hector ortega
Prana Therapies
San Diego, CA, United States
1,466
Total downloads
15k
Total views and downloads
Submission closed
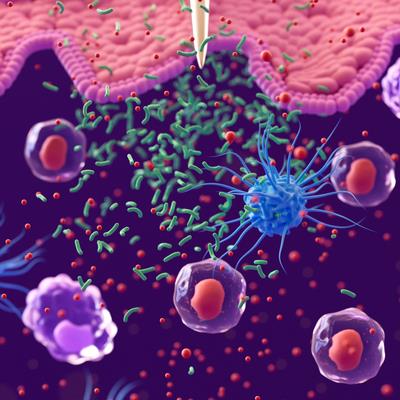
Studies have demonstrated a critical role of the cytokines thymic stromal lymphopoietin (TSLP), IL-33, and IL-25, produced by epithelial and other cells at mucosal surfaces in response to a wide range of environmental stimuli, in activating ILC2s to produce Th2-type cytokines, and in inducing Th2-type differentiation of CD4+ T cells directly or by suitable priming of Ag presenting dendritic cells. These alarmins are likely involved in innate and adaptive immune responses initiated by the interaction of epithelial cells with the external environment in diseases such as asthma, COPD, chronic rhinosinusitis with nasal polyps and atopic dermatitis.
Pre-clinical studies have shown that local topical administration or lung-specific transgenic expression of TSLP, IL-25, or IL-33 alone is sufficient to induce a complete spectrum of asthma-associated pathogenetic features, including airway inflammation, eosinophil infiltration, goblet cell hyperplasia, and airway hyperresponsiveness, in the airways of animal surrogates of asthma.
Elevated expression of these cytokines and their receptors has also been observed in bronchial biopsies of asthmatic patients compared with controls. Increased concentrations of TSLP, IL-33 and IL-25 have also been documented in bronchoalveolar lavage fluid (BALF) of patients with asthma and COPD. A large body of evidence is available demonstrating the clinical benefit of anti-TSLP treatment in asthma while more limited evidence is available in COPD. With regards to anti-IL-33 inhibition (including its receptor, ST2) the evidence in asthma and COPD is still growing while large clinical studies are ongoing in patients with COPD.
The goal of this research topic is to provide a comprehensive review of the three key epithelial alarmins (TSLP, IL-33 and IL-25) in asthma and COPD. Despite the evidence of the role of these alarmins in some clinical studies, there is still relatively little information about the redundancy of the expression of these alarmins in the airways, their complementary role, their effect on disease modification, the potential utility of biomarkers, the spectrum of modulation in the context of Type 2 vs. non-Type 2 inflammation, remodelling and the potential utility of dual inhibition with bispecifics.
We welcome manuscript submissions on themes including, but not limited to:
- Biology and mechanism of action of epithelial alarmins
- Models to inform on the pleotropic role of alarmins
- Use of in vivo models beyond airways
- Biological implications of the short and long thymic stromal lymphopoietin isoforms in inflammation
- The use of biomarkers for selecting a target population
- Type 2 vs. non-type 2 inflammation (eosinophilic vs. neutrophilic)
- Current clinical evidence in asthma and COPD with anti-TSLP inhibition
- Current clinical evidence in asthma and COPD with anti_IL-33 inhibition
- Current clinical evidence in asthma and COPD with anti_IL-25 inhibition
- Disease modification and remodelling
- New insights on the next generation of biotherapeutics with bispecifics
Topic Editor Dr. Hector Ortega, MD, ScD is employed by Uniquity Bio. The other Topic Editors report no competing interests related to this Research Topic.
Keywords: Alarmin, Asthma, Airway epithelium, Cytokines, COPD, Inflammation, Monoclonal antibodies, Remodelling
Important note: All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Share on WeChat
Scan with WeChat to share this article
