- Department of Seafood Science and Technology, Institute of Marine Industry, Gyeongsang National University, Tongyeong, South Korea
The coronavirus disease 2019 (COVID-19) pandemic, which began in 2019, has far-reaching ramifications, including economic losses and health challenges that still affect various parts of the world. During our review, we learned that the entire world is working to stop the spread of the SARS-CoV-2 outbreak. We explore ways that may lower the danger of SARS-CoV-2 contamination and useful strategies to avoid the possibility of SARS-CoV-2 spreading through food. While hygienic protocols are required in the food supply sector, cleaning, disinfection, and the avoidance of cross-contamination across food categories and other related goods at different stages of the manufacturing process remain especially important because the virus can survive for long periods of time on inert materials such as food packaging. Furthermore, personal hygiene (regular washing and disinfection), wearing gloves and using masks, garments, and footwear dedicated to maintaining hygiene provide on-site safety for food sector personnel, supply chain intermediaries, and consumers. Restrictions imposed in response to the pandemic (e.g., closure of physical workplaces, canteens, cafes, restaurants, schools, and childcare institutions), changes in household grocery shopping frequency, individuals' perceived risk of COVID-19, income losses due to the pandemic, and sociodemographic factors are among the factors. The conclusions drawn from this study consider the implications of healthy diets, food system resilience, behavior change, and nutritional imbalance for policymakers and food supply chain participants, as well as the antimicrobial effects of vitamins and nutrients. During a public health crisis, people should eat less, necessitating preventive policies and nutritional advice to deal with this.
Introduction
The World Health Organization (WHO) confirmed the coronavirus disease 2019 (COVID-19), which began in China (Wuhan Province) and quickly spread throughout the country and subsequently to other countries worldwide; it was confirmed by the World Health Organization (WHO) as pandemic on March 11, 2020, despite widespread global attention (WHO, 2019; Clemente-Suarez et al., 2021). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was named by the International Committee on Virus Taxonomy (ICTV) (Hui et al., 2020). Even though COVID-19 has a lower fatality rate than SARS, it has a higher transmission rate due to mutation and increased recombination of genes in the SARS-CoV-2 receptor-binding domain S protein (Shereen et al., 2020).
In this study, over 633 million cases have been confirmed in over 230 countries, resulting in over 6.5 million deaths (CoronaBoard, 2019; Wu et al., 2020; Galvan et al., 2021). Despite this, unpaid particular antiviral medicines continue to spread new infections daily (outbreak worldwide presented in Figure 1). Furthermore, SARS-CoV-2 infection has a negative effect on each country's economy and causes marketing issues throughout the food supply chain. The precise source of COVID-19 is currently unknown. Phylogenetic comparisons show that SARS-CoV-2 is 96% similar to SARS-CoV, implying that bats are its natural hosts (Zhou et al., 2020; Han et al., 2021). However, no intermediate host has yet been identified to assist this virus in crossing the species barrier and infecting humans. This virus is known to be easily transmitted by respiratory droplets in human-to-human contact, and food surfaces are viral transporters (Mullis et al., 2012). The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) have stated that there is no evidence of SARS-CoV-2 transmission or direct contamination of food or water (CDC, 2021). The virus, conversely, can be disseminated by consuming food prepared and packaged on dirty surfaces or through transmission by an infected person during food handling or sharing (Galanakis, 2020; Han et al., 2021). In January 2020, at a conference, researchers infected a few people with COVID-19 via physical contact and shared meals (Pung et al., 2020), implying that food could be a possible SARS-CoV-2 infection channel. Using scientific information to find new ways to stop the virus from spreading quickly and to update international standards, it is important to find out how the virus spreads, including whether it can be spread through food.
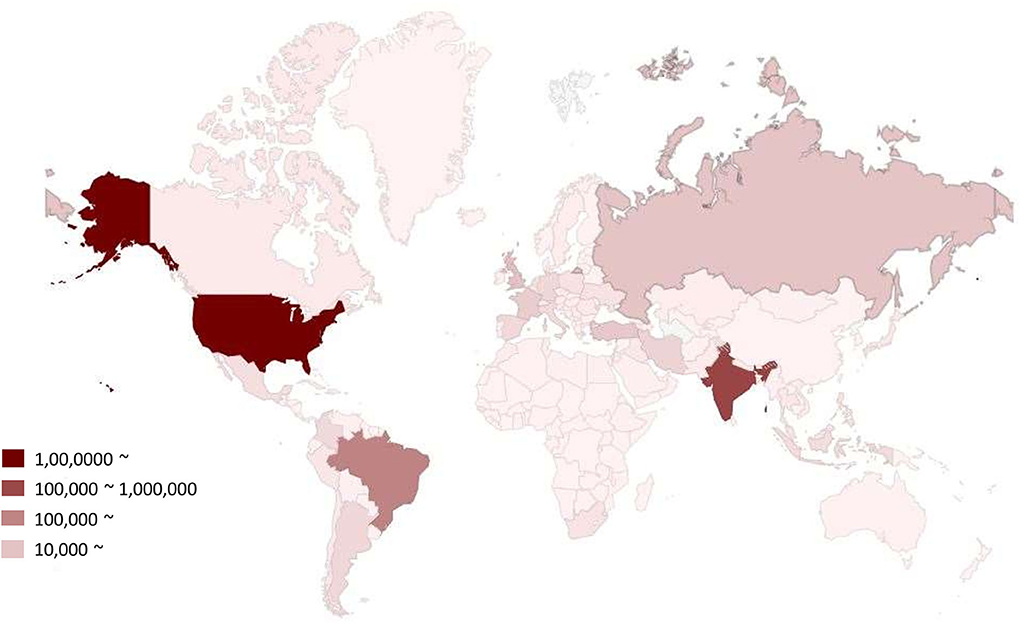
Figure 1. COVID-19 outbreak all over the world. Different color indicated number of infected populations.
Despite being a viral disease, the new coronavirus disease (COVID-19) is often treated with several antimicrobials (Wu et al., 2020; Ng et al., 2021). Healthcare professionals (HCP) use an empirical approach to treat COVID-19 patients regardless of the laboratory parameters due to the ambiguity of a successful treatment strategy (Fathi et al., 2021). The choice to begin antibiotics is typically made in response to clinical manifestations that resemble bacterial pneumonia (Lau et al., 2011; Bertuzzi and DiRita, 2020). The HCP is considering antibiotics as a treatment option due to concerns about community-acquired pneumonia, nosocomial bacterial superinfection in longer hospitalized patients, and high mortality due to COVID-19 among risk groups, including those over 60 and those with underlying medical problems (Li et al., 2005; Fathi et al., 2021). Worldwide, up to 72% of COVID-19 patients were treated with antibiotics (Lau et al., 2011; Bertuzzi and DiRita, 2020), but only 1–16% of these patients also had a bacterial co-infection (Lau et al., 2011). Broad-spectrum antibiotics were frequently used to treat various microorganisms (Lau et al., 2011; WHO, 2020; Fathi et al., 2021).
Additionally, COVID-19 was treated with antivirals (Li et al., 2005; Czarniecka-Skubina et al., 2021; Memon et al., 2021), antimalarials like hydroxychloroquine (Kassir, 2020), and antiparasitic medications like ivermectin (Kassir, 2020; Celorio-Sardà et al., 2021). Antibiotic use has increased and been sustained as a result of COVID-19 treatment. Antimicrobial resistance (AMR) is silently and gradually increasing due to empiric antibiotic use, becoming a major global threat (Assiri et al., 2013; Cockrell et al., 2016; Backer et al., 2020; Chan et al., 2020; Wu et al., 2020). As a result, there will probably be more cases of sickness and mortality both during and after the pandemic. The World Health Organization (WHO) has voiced concern that the COVID-19 pandemic will worsen the AMR situation, which is already a pressing problem (Mahase, 2020; Filip et al., 2021).
The actual pandemic directly affected people's daily lives worldwide, with limited policies such as lockdowns, the use of face masks, and restrictions on individual movement (Clemente-Suarez et al., 2021; Tornero-Aguilera and Clemente-Suarez, 2021). Fever, sore throat, headache, dry cough, weariness, dyspnea, and infrequent intestinal indications are prevalent clinical symptoms, asymptomatic to acute respiratory distress syndrome and multi-organ dysfunction (Singhal, 2020; Zhao et al., 2021). The common indications include fever, headaches, sore throats, dry coughs, lethargy, myalgia, shortness of breath, and gastrointestinal symptoms (Zhao Q. W. et al., 2020). The contagion can devolve into respiratory failure, pneumonia, and mortality by the end of the first week (Singhal, 2020). In addition, the eosinophilic cell blood count appears to have a significant role in COVID-19 analysis and prediction (Clemente-Suarez et al., 2020). COVID-19 has been studied in relation to many characteristics such as socioeconomic position, age, sex, nutrition, and race (Dastoli et al., 2020; Fuentes-Garcia et al., 2020; Golestaneh et al., 2020). Nutrition plays a crucial role in immunological conditions and sickness. The nutritional intervention has demonstrated various approaches with varying outcomes. The COVID-19 pandemic caused changes in food hygiene, lifestyle, and diet in various parts of the world. However, with the current development of SARS-CoV-2, changes are still occurring, and much more information is being acquired. Ultimately, determining the wider health effects of COVID-19 depends on how the pandemic influences the world's population's mental, social, and physical health compared to pre-pandemic conditions. This review aimed to offer current nutritional attention to the current COVID-19 situation. This review scenario aims to gather issues about dietary patterns, nutrition, nutritional deficiencies, vitamin involvement, physical activity, and the antimicrobial activity of nutritional elements (Han et al., 2021).
Methodology and data collection approaches
This review study is based on evidence from reputable journals on Google Scholar, LISTA (EBSCO), the Web of Science Core Collection, and PubMed. Key phrases such as SARS-CoV-2, COVID-19, food supply, dietary patterns, nutrition, health, and publication date were also evaluated when searching for papers on the web. Most works published in 2020 and during COVID-19 (2019–present) were considered. A few studies published before 2020 and websites updating situation reporting are also acknowledged as documenting earlier viral outbreaks. This review study provided a broad and brief overview of the COVID-19 pandemic research landscape, which could be helpful for getting a general understanding of the subject.
Food supply during the COVID-19 pandemic
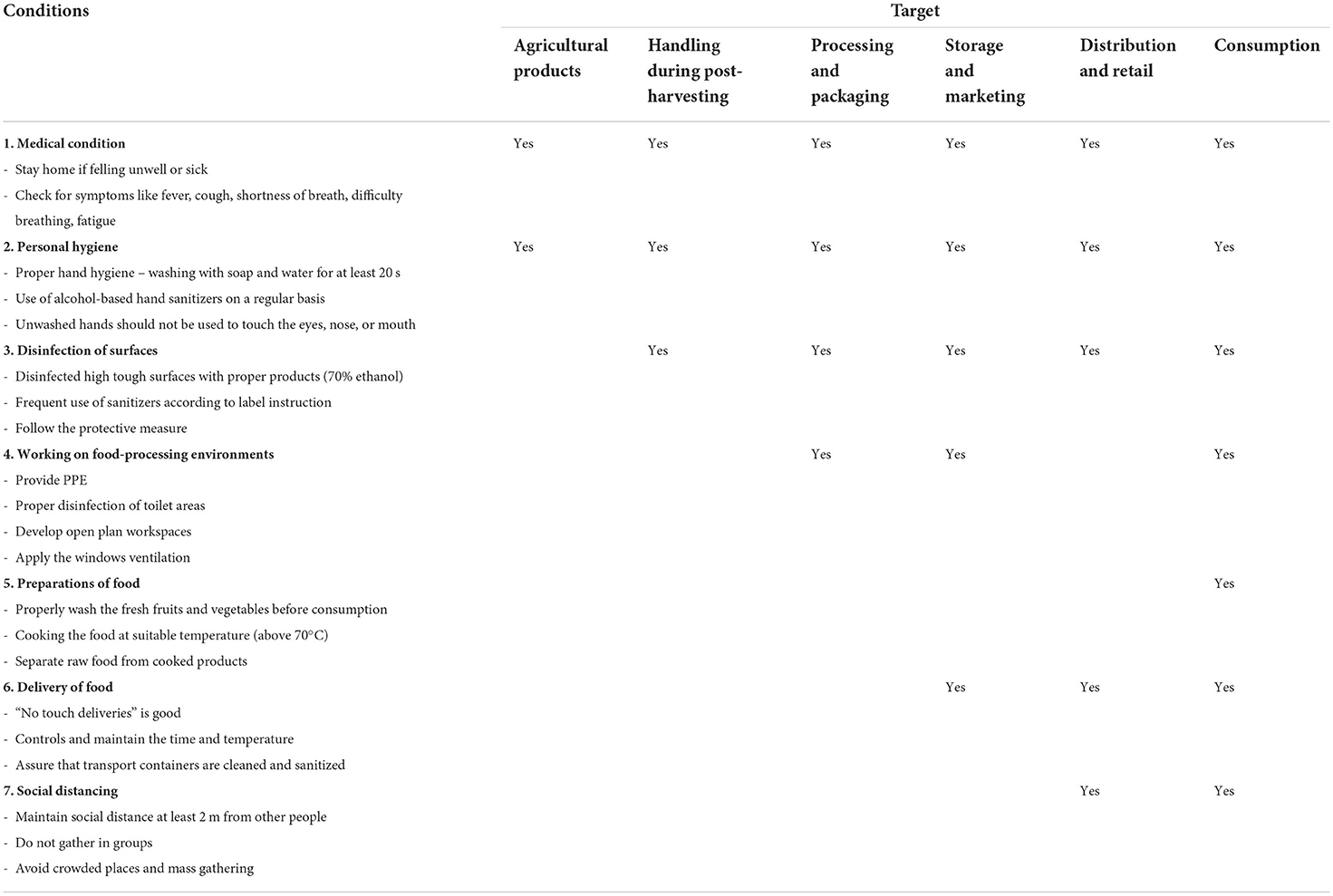
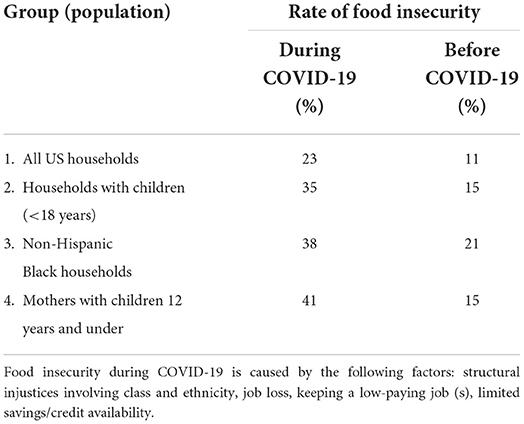
The food system is broad, multifaceted, interdependent, and capable of handling food security, safety, nourishment, quality, and industrial distribution (Clancy, 2017; Han et al., 2021). Food items frequently need components for multi-element preparations that are not readily available in the region; the absence of such substances can pose a substantial problem for food manufacturers, ranging from manufacturing to local, state, national, and worldwide points (Bhunnoo, 2019). However, it is essential to manage food worldwide to manage the crisis (Lima et al., 2018). According to the Food and Agriculture Organization (FAO), COVID-19 has a two-pronged impact on agriculture: supply and demand are directly tied to food safety (FAO, 2020). The food supply chain connects farm operations to customer tables through production, packing, supply, and stowing (Chen et al., 2020). All segments of the food supply chain—fruit, bakery items, fresh vegetables, and food products—were severely harmed (Ivanov and Dolgui, 2020). The main pillar of four pillars (production, packing, supply, and stowing) of the food safety scheme has been significantly harmed by COVID-19 (Galanakis, 2020). Table 1 illustrates the suggested food safety processes for food subdivisions from farmhouses to users. Workers are classified according to their treatment circumstances, individual cleanliness, apparent cleansing, work environment hygiene, food preparation and distribution, and communal separation (Galanakis, 2020). Despite all the safety regulations across the food supply chain, consumption necessitates the most thorough safety considerations at the consumer level. Many food supply chains stopped selling rare steak and beef during the crisis to avoid contamination (Euractiv, 2021; Obayelu et al., 2021; Pravst et al., 2022). Furthermore, certain industries (meat processing) in the United States were completely shut down during the COVID-19 outbreak (Reiley, 2020). Therefore, food insecurity factors were involved during the COVID-19 pandemic (Table 2) (Leone et al., 2020).
Food demand refers to interest in and willingness to pay for food during a particular time period (Mankiw, 2014). Due to uncertainty and dwindling consumer power, food demand has declined marginally. Furthermore, these conditions may worsen due to a lack of money and employment losses (FAO, 2020). Because of the COVID-19 pandemic, there is an increasing demand for food and beverages from virtual sources. Food shortages are unavoidable under such stringent lockdown circumstances, during which the maximum logistical supply has ceased. Due to the risk of getting sick, one cannot order food from online food delivery services such as Tomato and Twiggy (Narayanan et al., 2020).
Food poverty is increasing because of the financial crisis due to COVID-19, and the number of individuals facing global food uncertainty may quadruple by the end of 2020 (WFP, 2022). Owing to heightened food uncertainty during the COVID-19 pandemic, developing and developed countries are in a similar scenario, with helpless and low-income populations suffering the most (Fitzpatrick et al., 2020). Authorities must play a crucial role. Everyone must have unfettered access to food that satisfies their basic needs for food security to encourage access to wholesome foods. An impending food crisis that disproportionately impacts the most vulnerable communities is signaled by a failure to act swiftly (Rosales and Mercado, 2020). FAO (2021) reported ~820 million people are the most helpless group, being affected by long-lasting hunger and not consuming sufficient nutrients to live a decent lifespan. Due to their lack of resources and access to food, the effects of the virus spreading farther across nations could be disastrous. Small farmers are a second vulnerable group who might be prohibited from working on their property or traveling to markets to sell their harvests or buy seeds and other necessary goods. Last but not least, low-income families' children are largely fed through communal programs; program interruptions due to the pandemic risk their food safety and nutrition, decreasing their ability to cope with illnesses. Therefore, to stop the spread of viruses, each country needs to keep up with programs that help people work together to take the necessary precautions.
Dietary patterns during the COVID-19 pandemic
The COVID-19 pandemic has affected people's eating habits and nutrition patterns. Therefore, there have been differences in the category and period of family internment, the traditional and communal trends of the nations, the age of the trial investigated, and existing obesity, which have resulted in disparate assumptions. In Spain, it was found that the food consumed during the pandemic had higher energy consumption and lower nutritional quality than pre-COVID-19 consumption patterns (Batlle-Bayer et al., 2020). Furthermore, a 6% increase in daily intake was observed during the COVID-19 home confinement compared to 2019 (Batlle-Bayer et al., 2020). Similarly, a study in Poland revealed that people consumed snacks more throughout the lockdown, with this behavior being more common in bulky and obese people (Sidor and Rzymski, 2020). One possible explanation for this was that staying at home directly affected day-to-day food practices, resulting in increased energy consumption and demand for comfort food (Muscogiuri et al., 2020; Rodriguez-Perez et al., 2020; Zhao A. et al., 2020). Governments must assess how dietary changes that affect food quality (such as an increased intake of high-calorie meals) and a decrease in the consumption of wholesome foods (such as vegetables and fruits) may increase the prevalence of chronic diseases (Rundle et al., 2020). COVID-19 alters the rate of consumption of some foods as well as the amount consumed by others in terms of dietary composition (Rundle et al., 2020; Rodriguez-Besteiro et al., 2021). These results confirmed that staying at home and communal isolation had an adverse effect on adherence to vigorous eating practices (Rundle et al., 2020). In particular, a prior study found that Spanish people consumed fewer beverages, somewhat more eggs, and red meat and consumed much more plant-based foods, such as almonds, pasta, processed vegetables, or rice, than in 2019 (Rodriguez-Besteiro et al., 2021). Despite these modifications, red meat consumption remains higher than the suggested dietary requirements, whereas plant-based foods remain within the required choices (Rodriguez-Besteiro et al., 2021). Conversely, during COVID-19, the dietary patterns of the Chinese shifted, with a fall in the consumption of garden-fresh vegetables and fruit, poultry, rice, pork, and soybean foods (Jia et al., 2021).
Interestingly, another report (Ruiz-Roso et al., 2020) found that COVID-19 confinement resulted in a healthy dietary adjustment in a teenage population from Chile, Brazil, Colombia, Italy, and Spain, increasing the incidence of vegetable, fruit, and legume consumption during the lockdown. Thus, the proportion of adolescents consuming the suggested weekly portions of fruits and legumes during the lockdown increased by 8 and 7.7%, respectively, compared to before the lockdown. Numerous factors could support these pattern alterations. First, sales of fruits and legumes have surged since incarceration started, and second, people have more time to prepare meals at home (Ruiz-Roso et al., 2020). Several studies, for example, examined populations with innate eating tendencies. Furthermore, authorities in each country imposed distinct levels of lockdown, varying degrees of severity, and population limits. These reasons may be the root of the inconsistencies observed in previous studies (Opichka et al., 2019; Ruiz-Roso et al., 2020).
Surprisingly, in all the categories affected by the COVID-19 pandemic, bulky and obese individuals had the worst dietary patterns and behaviors. These populations exhibit more troublesome eating patterns, such as food intake without feeling hungry and frequent overeating (Opichka et al., 2019). Because of a longer stay at home and typically limitless food access, bulky and obese people started eating and snacking more throughout their home confinement (Blaszczyk-Bebenek et al., 2020). Furthermore, participants with a higher body mass index consumed fewer vegetables, fruits, and legumes throughout the lockdown and consumed more meat, dairy, and fast foods throughout the lockdown (Blaszczyk-Bebenek et al., 2020). Furthermore, the lockdown altered the nutrition patterns of overweight children and teenagers, considerably boosting their use of sugary drinks, red meat, and potato chips compared with 2019 (Pietrobelli et al., 2020). These lifestyle modifications have the potential to increase fat mass (Larsen and Heitmann, 2019).
The long-term consequences of the negative dietary changes reported during the lockdown may include the development of unhealthy eating habits (Poobalan et al., 2014; Serra-Majem et al., 2020). During the lockdown, negative emotions such as boredom and worry increased the development of poor eating habits (Moynihan et al., 2015; Araiza and Lobel, 2018). Owing to the immunomodulatory effects of several macro-, micro-, and phytonutrients (Bhaskaram, 2002; Fernandez et al., 2021), a nutritious and balanced diet is a vital aspect of the personal hazard management plan during the COVID-19 pandemic (Gasmi et al., 2020). Furthermore, dietary deficits have been associated with increased host vulnerability to virus-related contagion and a more severe clinical course of sickness (Bhaskaram, 2002; Fernandez et al., 2021). As a result, while a healthy diet cannot entirely prevent illness, it can play a significant role in the host's response to an infectious agent (Blaszczyk-Bebenek et al., 2020). Surprisingly, other unhealthy habits followed the same pattern as food patterns. Thus, an increase in alcohol intake (15%) among alcohol addicts and an increase in smoking (Blaszczyk-Bebenek et al., 2020). Therefore, more investigation is needed to determine how food patterns changed during the COVID-19 pandemic and provide the necessary guidelines to endorse good behavior throughout probable future pandemics.
Effects of vitamin ingredients as antimicrobial agents during the COVID-19 pandemic
The COVID-19 pandemic has been related to other documented epidemics in the last 20 years, such as SARS and MERS (lower respiratory diseases), with comparable clinical symptoms in the early infection stages (fever and cough), resulting in significant fatalities among susceptible people (Das, 2020; Han et al., 2021). Consuming vitamins and functional foods can boost the immune system and aid in virus suppression (Gibson et al., 2012). Vitamin C boosts the immune system and is required for body tissue growth and repair due to its antimicrobial and anti-inflammatory properties (Li et al., 2020). Furthermore, vitamin A is a fat-soluble molecule that plays an important role in immune function and lowers infection susceptibility (Huang et al., 2018; Shirvani et al., 2019). Isotretinoin is a cellular protein that regulates the downregulation of angiotensin-converting enzyme 2 (ACE2), which is essential for SARS-CoV-2 entry (Sinha et al., 2020).
Furthermore, vitamins D and E can boost resistance to SARS-CoV-2 (Im et al., 2016). Bioactive lipids (arachidonic acid and other unsaturated fatty acids) can also boost resistance. Natural polyphenols such as hesperidin and rutin are effective against COVID-19 primary protease inhibitors and are key targets for therapeutic medicines (Adem et al., 2020). Herbal and Chinese medicines have been used to treat viral diseases. Ginseng root, for example, can be used to treat respiratory virus infections (Im et al., 2016). Astragalus membranaceus is widely used to treat colds and upper respiratory infections (Luo et al., 2020), but Pelargonium sidoides is an efficient herbal treatment (Kolodziej, 2011). Chinese herbal formulae are used as an alternative route to COVID-19 treatment and prevention (Pietrobelli et al., 2020). Some bioactive foods (quercetin) suppress the enzymatic activity of SARS 3-chymotrypsin-like protease (3CLpro). This is required for SARS-CoV-2 replication and can be used to treat COVID-19 patients (Yang et al., 2020). Dietary supplements (vitamins, botanicals, bioactive lipids, and flavonoids) may help the human immune system.
Nonetheless, there is no evidence that such bioactive compounds can sufficiently increase immune function to prevent or cure COVID-19 (Han et al., 2021). Furthermore, in the novel era of the COVID-19 pandemic, researchers are looking for suitable medications to enhance the immune system in the future. Nutritional deficiencies in macro- and micronutrients can have an effect on immune function and infection resistance (Filip et al., 2021). Several functional foods, including pepper, garlic, turmeric, and onion, may have immunomodulatory and antiviral effects (Table 3).
Health conditions
This section studied the associations between body compositions. The following issues are addressed: (a) body composition variations, (b) the correlation between body composition and changes (e.g., physical activity and nutrition), and (c) body composition as a risk factor.
Physical activity was marked by a sharp decrease at the pandemic's beginning (Ding et al., 2021). Those with a higher body fat percentage had less physical activity due to a lower fat proportion (Poobalan et al., 2014). Body composition was assessed by measures of fatness (Neovius et al., 2005), bioimpedance analysis (Ding et al., 2021), or BMI to investigate alterations between underweight, overweight, and normal-weight people (Gwynn et al., 2011; Bell et al., 2018). Obesity people are at an increased risk for COVID-19 (Freuer et al., 2021). For example, obesity class II increased the hazard of COVID-19 in individuals over 65 years; however, BMI has a linear relationship with the virus in adults aged 65 (Christensen et al., 2021).
Furthermore, visceral fat was found in patients with COVID-19 who required critical care (Favre et al., 2021). In COVID-19, body composition was assessed using the waist circumference/paravertebral muscle circumference ratio. It was proposed as a predictor of a poor clinical outcome on low-dose computed tomography of the chest (Kottlors et al., 2020). Additionally, abdominal obesity in COVID-19 patients with respiratory symptoms was found to be an independent risk factor for respiratory distress as determined by the waist-to-hip ratio (van Zelst et al., 2020). Obesity may also have an impact on immune responses to viruses, inflammatory reactions, and metabolic and respiratory issues (Coelho-Ravagnani et al., 2021; Sinska et al., 2021). It could be explained by its effect on immunity, which alters the etiology of ARF (acute renal failure) and pneumonia (Rebello et al., 2020). In COVID-19, obesity and morbid obesity were identified as major risk factors for ICU admission (Foldi et al., 2020). Obese patients with a higher BMI should be constantly monitored and may require medication assistance sooner to treat colds and upper respiratory infections (Zhao X. et al., 2020). Obesity or BMI should be considered key indicators, and obese COVID-19 patients should be considered a high-risk group (Tamara and Tahapary, 2020; Yang et al., 2021). Regarding energy balance, the negative changes in body composition during a pandemic should be endorsed to match changes in physical activity and diet, indicating a decrease in energy expenditure and an increase in caloric absorption (Huber et al., 2021). Furthermore, obesity reduces vaccine efficacy in people suffering from rabies, hepatitis B, tetanus, and influenza; thus, immunization conditions and constraints on the efficiency of COVID-19 inoculation should be considered (Liu et al., 2017).
Nutrition at multilevel and health conditions
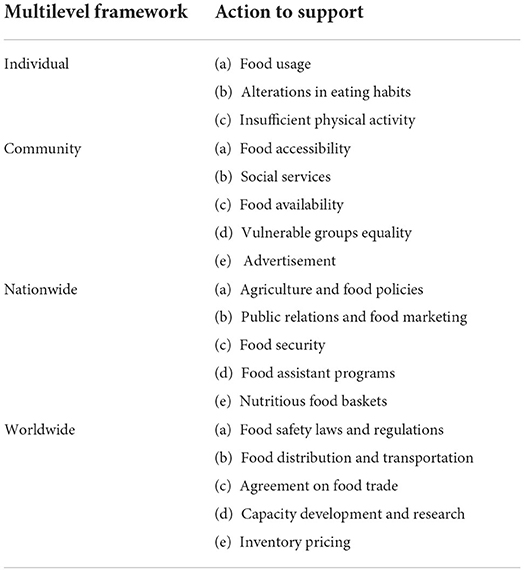
Previous pandemics have shown that as a pandemic progresses, it is critical to expanding community health efforts through clinical supervision to include basic supervision concepts and optimize resource usage. Since the COVID-19 pandemic, personal and social resilience have emerged as valuable resources and continue to be the first line of defense in crisis response. Indeed, mental and behavioral countermeasures at both the personal and communal levels are critical factors in accomplishing public health ingenuities in the face of a pandemic with the magnitude of COVID-19 (Reissman et al., 2006). Individual nutritional status has long been considered a prognosticator of flexibility and instability (Cobb, 2011). The ecology of difficulty and flexibility indicates that significant stresses, such as deprivation of nourishment, can have long-term repercussions on health (Yousafzai et al., 2013). Deprived nutrition eminence is related to both corporeal and psychological health problems (Hislop et al., 2006). Optimal nutrition and dietary consumption are resources that extend beyond the personal and communal to have a worldwide impact (Ma and Lee, 2012). In response to the COVID-19 pandemic, this article suggests a plan of action (Table 4) for maintaining good nutrition on a personal, community, national, and international level.
The common denominator that drives most nutrition and dietary advice to treat viral infections, including COVID-19, is the relationship between food and immunity. Existing research indicates that nutrition significantly impacts the immune system and illness susceptibility. Specific food or nutritive element combinations influence the immune system via cell activation, signaling molecule synthesis changes, and gene expression (Valdes-Ramos et al., 2010). Furthermore, nutritional elements are important factors in gut infectious arrangements and, as a result, can determine the nature of the body's immunological responses (Wypych et al., 2017). Low immune function and increased sensitivity to infection have been linked to protein, energy, and micronutrient shortages. Maintaining immune function requires a diet rich in iron, zinc, and vitamins A, E, B6, and B12 (Nieman, 2020). So, the best way to keep an immune system that works is to avoid dietary deficiencies needed for immune cells to activate, interact, differentiate, or show how they work.
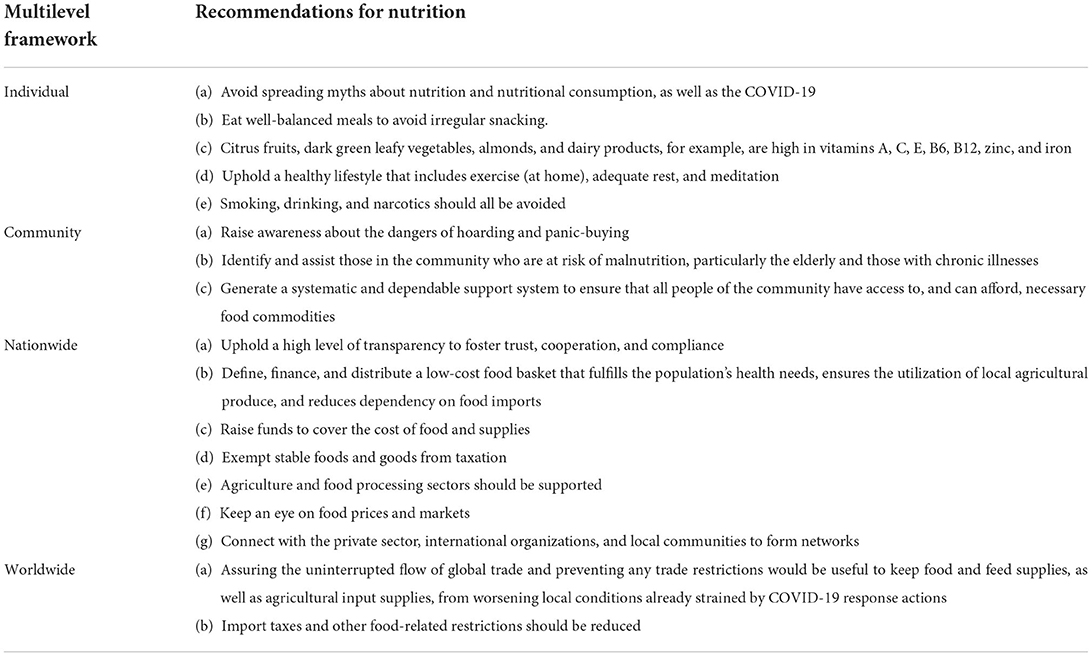
Pandemics cause consumer demand to be unclear and volatile, making it especially difficult to manage food supplies in a just-in-time economy (Vo and Thiel, 2006). A study of the effect of an outbreak on behavior found that stockpiling supplies, food, and water was the most common response (Kohn et al., 2012). Therefore, it is critical to raise community awareness of panic buying. Furthermore, during the COVID-19 pandemic, older people and patients with chronic illnesses were especially vulnerable to nutritional imbalances. Existing data indicates that people aged 60 years and older and patients with pre-existing medical disorders, particularly heart disease, lung illness, diabetes, or cancer, are more likely to suffer severe or even fatal coronavirus infections. Second, given their sensitivity, the instructions to stay at home and practice social distancing explicitly targeted these populations. Third, due to their weakened health and reduced purchasing power, the elderly and patients with chronic conditions may already be vulnerable to malnutrition. So, at the community level, it is very important to find these vulnerable groups and help them get food by setting up a structured and reliable support system.
While boundary safety is essential to protect the health of individuals, it can cause major disturbances in trade, travel, and tourism and infringe on civil liberties (Gostin, 2006). Therefore, ensuring the smooth flow of global trade and fully using international markets as a crucial weapon for guaranteeing global food supplies and eliminating food insecurity is critical. The worldwide nature of COVID-19, in which no country is immune to its spread and devastation, illustrates a fundamental lesson: a global threat necessitates global action. Each country's preventative measures should be complemented by global collaboration and coordination to ensure that humanity survives this epidemic with as few losses as possible. In summary, while there is still much to learn about COVID-19, its effect on nutrition and food consumption has already gone well beyond the individual and communal levels, reaching national and global levels. This outbreak underlined the interconnectedness of these numerous levels, as an individual's health directly resulted from his understanding and choices, community togetherness, government readiness, and, eventually, global action in response to this threat. From this perspective, a framework for action and recommendations are offered at each of these levels. Table 5 summarizes these recommendations.
Conclusions
This study shows that the COVID-19 pandemic has a deleterious impact on people's diets and physical and mental health. During the COVID-19 pandemic, people's eating habits were, on average, less healthy, especially during a lockdown, which was linked to weight gain. According to this study, there was a significant prevalence of food and nutrition-related worries throughout the COVID-19 pandemic lockdown period. These worries were linked to a higher likelihood of reporting changes in dietary behaviors, such as food preparation and consumption. The capacity of the current dietary recommendations to manage dietary issues during a public health emergency is limited, and it is possible that they do not have the precision to offer dietary advice to various people. Age, weight, and income are among the sociodemographic factors linked to higher levels of food, nutrition, and health concerns, indicating the need for appropriate programs and policies to support disadvantaged people and lifestyle recommendations to encourage healthy eating. This study also sheds insight on probable explanations for this shift, such as depression, decreased shopping frequency, which is linked to lower fresh food consumption, and increasing fast food marketing. We also encourage scientists to anticipate future pandemic food and nutrition priorities as well as to build a more resilient food system that better integrates critical factors such as the food supply chain, nutritional security, healthy food accessibility, health, and food safety and preparation communication in the event of long quarantines. Developing long-term “exit strategies” and goals to prepare for future pandemics is vital. As a result, as also stated, a global food, nutrition, and associated science advisory council is needed to prepare for future pandemics and provide advice. The advising scientific body's recommendations must be shared and embraced by decision-makers to ensure successful and long-term program execution. It is important to practice food hygiene and eat a balanced diet rich in fresh fruits and vegetables to maintain a healthy lifestyle and an effective immune system that can fight off infection and disease. Although there is no proof that the coronavirus may spread directly through food, packages may be contaminated with SARS-CoV-2 and could do so. Packaging may be required to contain bioactive substances that neutralize infectious contaminants to lower the risk of transmission. We essentially want to prevent more outbreaks that tax the healthcare system, given the possibility that SARS-CoV-19 will continue to spread throughout the population. Further research should be conducted on the psychological and physiological impacts of prolonged lockdowns, the probable persistence of altered behaviors, and their effects on personal and societal health in the post-lockdown and post-pandemic eras.
Author contributions
Conceptualization, software, validation, formal analysis, investigation, resources, writing—original draft preparation, and visualization: PR. Methodology and data curation: PR and MS. Writing—review and editing: PR, MS, EJ, and SK. Supervision, project administration, and funding acquisition: SP. All authors have carefully read, reviewed, edited, and agreed to publish the manuscript.
Funding
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education, Grant Number 2021R1I1A3A04037468.
Acknowledgments
We are grateful to the Food Safety Laboratory for its excellent support while writing this review manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adem, S., Eyupoglu, V., Sarfraz, I., Rasul, A., and Ali, M. (2020). Identification of potent COVID-19 main protease (Mpro) inhibitors from natural polyphenols: an in silico strategy unveils a hope against CORONA. doi: 10.20944/preprints202003.0333.v1
Araiza, A. M., and Lobel, M. (2018). Stress and eating: definitions, findings, explanations, and implications. Soc. Personal Psychol. 12, e12378. doi: 10.1111/spc3.12378
Assiri, A., Al-Tawfiq, J. A., Al-Rabeeah, A. A., Al-Rabiah, F. A., Al-Hajjar, S., Al-Barrak, A., et al. (2013). Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect. Dis. 13, 752–761. doi: 10.1016/S1473-3099(13)70204-4
Backer, J. A., Klinkenberg, D., and Wallinga, J. (2020). Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance 25, 2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062
Batlle-Bayer, L., Aldaco, R., Bala, A., Puig, R., Laso, J., Margallo, M., et al. (2020). Environmental and nutritional impacts of dietary changes in Spain during the COVID-19 lockdown. Sci. Total Environ. 748, 141410. doi: 10.1016/j.scitotenv.2020.141410
Bell, R. A., Chen, H. Y., Saldana, S., Bertoni, A. G., Effoe, V. S., Hairston, K. G., et al. (2018). Comparison of measures of adiposity and cardiovascular disease risk factors among African American adults: the jackson heart study. J. Racial Ethn. Health 5, 1230–1237. doi: 10.1007/s40615-018-0469-y
Bertuzzi, S., and DiRita, V. J. (2020). After COVID-19 we will need a new research system. we need to start planning now. mBio 11, 1–4. doi: 10.1128/mBio.03251-20
Bhaskaram, P. (2002). Micronutrient malnutrition, infection, and immunity: an overview. Nutr. Rev. 60, S40–45. doi: 10.1301/00296640260130722
Bhunnoo, R. (2019). The need for a food-systems approach to policy making. Lancet 393, 1097–1098. doi: 10.1016/S0140-6736(18)32754-5
Blaszczyk-Bebenek, E., Jagielski, P., Boleslawska, I., Jagielska, A., Nitsch-Osuch, A., Kawalec, P., et al. (2020). Nutrition behaviors in Polish adults before and during COVID-19 lockdown. Nutrients 12, nu12103084. doi: 10.3390/nu12103084
CDC (2021). COVID-19. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/index.html
Celorio-Sardà, R., Comas-Basté, O., Latorre-Moratalla, M., Zerón-Rugerio, M., Urpi-Sarda, M., Illán-Villanueva, M., et al. (2021). Effect of COVID-19 lockdown on dietary habits and lifestyle of food science students and professionals from Spain. Nutrients 13, 1494. doi: 10.3390/nu13051494
Chan, J. F.-W., Yuan, S., Kok, K-. H., To, K. K-. W., Chu, H., Yang, J., et al. (2020). A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395, 514–523. doi: 10.1016/S0140-6736(20)30154-9
Chen, S. E., Brahma, S., Mackay, J., Cao, C. Y., and Aliakbarian, B. (2020). The role of smart packaging system in food supply chain. J. Food Sci. 85, 517–525. doi: 10.1111/1750-3841.15046
Christensen, R. A. G., Sturrock, S. L., Arneja, J., and Brooks, J. D. (2021). Measures of adiposity and risk of testing positive for SARS-CoV-2 in the UK biobank study. J. Obes. 2021, 8837319. doi: 10.1155/2021/8837319
Clancy, K. (2017). Digging deeper bringing a systems approach to food systems: transdisciplinary and systems approaches to food security. J. Agric. Food Syst. 7, 13–16. doi: 10.5304/jafscd.2017.074.012
Clemente-Suarez, V. J., Hormeno-Holgado, A., Jimenez, M., Benitez-Agudelo, J. C., Navarro-Jimenez, E., Perez-Palencia, N., et al. (2020). Dynamics of population immunity due to the herd effect in the COVID-19 pandemic. Vaccines-Basel 8, 623. doi: 10.3390/vaccines8020236
Clemente-Suarez, V. J., Navarro-Jimenez, E., Jimenez, M., Hormeno-Holgado, A., Martinez-Gonzalez, M. B., Benitez-Agudelo, J. C., et al. (2021). Impact of COVID-19 pandemic in public mental health: an extensive narrative review. Sustainability-Basel 13, su13063221. doi: 10.3390/su13063221
Cobb, T. D. (2011). Reclaiming Our Food: How the Grassroots Food Movement is Changing the Way We Eat. North Adams, CA: Storey Publishing.
Cockrell, A. S., Yount, B. L., Scobey, T., Jensen, K., Douglas, M., Beall, A., et al. (2016). mouse model for MERS coronavirus-induced acute respiratory distress syndrome. Nat. Microbiol. 2, 16226. doi: 10.1038/nmicrobiol.2016.226
Coelho-Ravagnani, C. D., Corgosinho, F. C., Sanches, F. L. Z., Prado, C. M. M., Laviano, A., Mota, J. F., et al. (2021). Dietary recommendations during the COVID-19 pandemic. Nutr. Rev. 79, 382–393. doi: 10.1093/nutrit/nuaa067
CoronaBoard (2019). COVID 19 Dashboard. Available online: https://coronaboard.com/global/ko/ (accessed on November 2, 2019).
Czarniecka-Skubina, E., Pielak, M., Sałek, P., Głuchowski, A., Kobus-Cisowska, J., Owczarek, T., et al. (2021). Use of food services by consumers in the SARS-CoV-2 PANDEMIC. How the eating habits of consumers changed in view of the new disease risk factors? Nutrients 13, 2760. doi: 10.3390/nu13082760
Das, U. N. (2020). Can bioactive lipids inactivate coronavirus (COVID-19)? Arch. Med. Res. 51, 282–286. doi: 10.1016/j.arcmed.2020.03.004
Dastoli, S., Bennardo, L., Patruno, C., and Nistico, S. P. (2020). Are erythema multiforme and urticaria related to a better outcome of COVID-19? Dermatol. Ther. 33, 13681. doi: 10.1111/dth.13681
Ding, D., Cheng, M. N., Cruz, B. D., Lin, T., Sun, S. Y., Zhang, L., et al. (2021). How COVID-19 lockdown and reopening affected daily steps: evidence based on 164,630 person-days of prospectively collected data from Shanghai, China. Int. J. Behav. Nutr. Phys. 18, 1–10. doi: 10.1186/s12966-021-01106-x
Euractiv (2021). No Evidence of COVID-19 Transmission Through Food, Says EFSA. Available online at: https://www.euractiv.com/section/coronavirus/news/no-evidence-of-covid-19-transmission-through-food-says-efsa/
FAO (2020). QandA: COVID-19 Pandemic-Impact on Food and Agriculture. Available online at: http://www.fao.org/2019-ncov/q-and-a/impact-on-food-and-agriculture/en/
Fathi, M., Vakili, K., Sayehmiri, F., Mohamadkhani, A., Hajiesmaeili, M., Rezaei-Tavirani, M., et al. (2021). The prognostic value of comorbidity for the severity of COVID-19: a systematic review and meta-analysis study. PLoS ONE 16, e0246190. doi: 10.1371/journal.pone.0246190
Favre, G., Legueult, K., Pradier, C., Raffaelli, C., Ichai, C., Iannelli, A., et al. (2021). Visceral fat is associated to the severity of COVID-19. Metabolism 115, e154440. doi: 10.1016/j.metabol.2020.154440
Fernandez, M. L., Raheem, D., Ramos, F., Carrascosa, C., Saraiva, A., Raposo, A., et al. (2021). Highlights of current dietary guidelines in five continents. Int. J. Environ. Res. Public Health 18, 2814. doi: 10.3390/ijerph18062814
Filip, R., Anchidin-Norocel, L., Gheorghita, R., Savage, W. K., and Dimian, M. (2021). Changes in dietary patterns and clinical health outcomes in different countries during the SARS-CoV-2 pandemic. Nutrients 13, 3612. doi: 10.3390/nu13103612
Fitzpatrick, K., Harris, C., and Drawve, G. (2020). Assessing US food insecurity in the United States during COVID-19 pandemic. J Hunger Environ Nutr. 16, 1–18. doi: 10.1080/19320248.2020.1830221
Foldi, M., Farkas, N., Kiss, S., Zadori, N., Vancsa, S., Szako, L., et al. (2020). Obesity is a risk factor for developing critical condition in COVID-19 patients: a systematic review and meta-analysis. Obes. Rev. 21, e13095. doi: 10.1111/obr.13095
Freuer, D., Linseisen, J., and Meisinger, C. (2021). Impact of body composition on COVID-19 susceptibility and severity: a two-sample multivariable Mendelian randomization study. Metab. Clin. Exp. 118, 154732. doi: 10.1016/j.metabol.2021.154732
Fuentes-Garcia, J. P., Patino, M. J. M., Villafaina, S., and Clemente-Suarez, V. J. (2020). The effect of COVID-19 confinement in behavioral, psychological, and training patterns of chess players. Front. Psychol. 11, 1812. doi: 10.3389/fpsyg.2020.01812
Galanakis, C. M. (2020). The food systems in the era of the coronavirus (COVID-19) pandemic crisis. Foods 9, 523. doi: 10.3390/foods9040523
Galvan, D., Effting, L., Cremasco, H., and Conte-Junior, C. A. (2021). The spread of the COVID-19 outbreak in Brazil: an overview by Kohonen self-organizing map networks. Medicina 57, 235. doi: 10.3390/medicina57030235
Gasmi, A., Noor, S., Tippairote, T., Dadar, M., Menzel, A., Bjorklund, G., et al. (2020). Individual risk management strategy and potential therapeutic options for the COVID-19 pandemic. Clin. Immunol. 215, 108409. doi: 10.1016/j.clim.2020.108409
Gibson, A., Edgar, J. D., Neville, C. E., Gilchrist, S. E. C. M., McKinley, M. C., Patterson, C. C., et al. (2012). Effect of fruit and vegetable consumption on immune function in older people: a randomized controlled trial. Am. J. Clin. Nutr. 96, 1429–1436. doi: 10.3945/ajcn.112.039057
Golestaneh, L., Neugarten, J., Fisher, M., Billett, H. H., Gil, M. R., Johns, T., et al. (2020). The association of race and COVID-19 mortality. Eclinicalmedicine 25, 100455. doi: 10.1016/j.eclinm.2020.100455
Gostin, L. (2006). Public health strategies for pandemic influenza—ethics and the law. JAMA-J. Am. Med. Assoc. 295, 1700–1704. doi: 10.1001/jama.295.14.1700
Gwynn, R. C., Berger, M., Garg, R. K., Waddell, E. N., Philburn, R., Thorpe, L. E., et al. (2011). Measures of adiposity and cardiovascular disease risk factors, New York City Health and Nutrition Examination Survey, 2004. Prev. Chronic Dis. 15, 785–795. doi: 10.1038/oby.2007.593
Han, S., Roy, P. K., Hossain, M. I., Byun, K. H., Choi, C., Ha, S. D., et al. (2021). COVID-19 pandemic crisis and food safety: implications and inactivation strategies. Trends Food Sci. Tech. 109, 25–36. doi: 10.1016/j.tifs.2021.01.004
Hislop, T. G., Bajdik, C. D., Balneaves, L. G., Holmes, A., Chan, S., Wu, E., et al. (2006). Physical and emotional health effects and social consequences after participation in a low-fat, high-carbohydrate dietary trial for more than 5 years. J. Clin. Oncol. 24, 2311–2317. doi: 10.1200/JCO.2005.04.3042
Huang, Z., Liu, Y., Qi, G., Brand, D., and Zheng, S. G. (2018). Role of vitamin A in the immune system. J Clin Med. 7, 258. doi: 10.3390/jcm7090258
Huber, B. C., Steffen, J., Schlichtiger, J., and Brunner, S. (2021). Altered nutrition behavior during COVID-19 pandemic lockdown in young adults. Eur. J. Nutr. 60, 2593–2602. doi: 10.1007/s00394-020-02435-6
Hui, D. S., Azhar, E. I., Madani, T. A., Ntoumi, F., Kock, R., Dar, O., et al. (2020). The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—the latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. IJID 91, 264–266. doi: 10.1016/j.ijid.2020.01.009
Im, K., Kim, J., and Min, H. (2016). Ginseng, the natural effectual antiviral: protective effects of Korean Red Ginseng against viral infection. J. Ginseng Res. 40, 309–314. doi: 10.1016/j.jgr.2015.09.002
Ivanov, D., and Dolgui, A. (2020). Viability of intertwined supply networks: extending the supply chain resilience angles towards survivability. A position paper motivated by COVID-19 outbreak. Int. J. Prod. Res. 58, 2904–2915. doi: 10.1080/00207543.2020.1750727
Jia, P., Liu, L., Xie, X. F., Yuan, C. Z., Chen, H., Guo, B., et al. (2021). Changes in dietary patterns among youths in China during COVID-19 epidemic: the COVID-19 impact on lifestyle change survey (COINLICS). Appetite 158, 105015. doi: 10.1016/j.appet.2020.105015
Kassir, R. (2020). Risk of COVID-19 for patients with obesity. Obes. Rev. 21, e13034. doi: 10.1111/obr.13034
Kohn, S., Eaton, J. L., Feroz, S., Bainbridge, A. A., Hoolachan, J., Barnett, D. J., et al. (2012). Personal disaster preparedness: an integrative review of the literature. Disaster Med. Public Health Prep. 6, 217–231. doi: 10.1001/dmp.2012.47
Kolodziej, H. (2011). Antimicrobial, antiviral and immunomodulatory activity studies of Pelargonium sidoides (EPs® 7630) in the context of health promotion. Pharmaceuticals. 4, 1295–1314. doi: 10.3390/ph4101295
Kottlors, J., Zopfs, D., Fervers, P., Bremm, J., Abdullayev, N., Maintz, D., et al. (2020). Body composition on low dose chest CT is a significant predictor of poor clinical outcome in COVID-19 disease—a multicenter feasibility study. Eur. J. Radiol. 132, 109274. doi: 10.1016/j.ejrad.2020.109274
Larsen, S. C., and Heitmann, B. L. (2019). More frequent intake of regular meals and less frequent snacking are weakly associated with lower long-term gains in body mass index and fat mass in middle-aged men and women. J. Nutr. 149, 824–830. doi: 10.1093/jn/nxy326
Lau, S. K. P., Lee, P., Tsang, A. K. L., Yip, C. C. Y., Tse, H., Lee, R. A., et al. (2011). Molecular epidemiology of human coronavirus OC43 reveals evolution of different genotypes over time and recent emergence of a novel genotype due to natural recombination. J. Virol. 85, 11325–11337. doi: 10.1128/JVI.05512-11
Leone, L. A., Fleischhacker, S., Anderson-Steeves, B., Harper, K., Winkler, M., Racine, E., et al. (2020). Healthy food retail during the COVID-19 pandemic: challenges and future directions. Int. J. Environ. Res. Public Health 17, 7397. doi: 10.3390/ijerph17207397
Li, Q., Guan, X., Wu, P., Wang, X., Zhou, L., Tong, Y., et al. (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 382, 1199–1207. doi: 10.1056/NEJMoa2001316
Li, W., Shi, Z., Yu, M., Ren, W., Smith, C., Epstein, J. H., et al. (2005). Bats are natural reservoirs of SARS-like coronaviruses. Science 310, 676–679. doi: 10.1126/science.1118391
Lima, D. P., Padula, J. C., Pumi, A. D., and The impact, G. (2018). of Chinese imports of soybean on port infrastructure in Brazil: a study based on the concept of the “Bullwhip Effect”. J Commodity Markets 9, 55–76. doi: 10.1016/j.jcomm.2017.11.001
Liu, F., Guo, Z. R., and Dong, C. (2017). Influences of obesity on the immunogenicity of Hepatitis B vaccine. Hum. Vacc. Immunother. 13, 1014–1017. doi: 10.1080/21645515.2016.1274475
Luo, H., Tang, Q. L., Shang, Y. X., Liang, S. B., Yang, M., Robinson, N., et al. (2020). Can Chinese medicine be used for prevention of corona virus disease 2019 (COVID-19)? A review of historical classics, research evidence and current prevention programs. Chin. J. Integr. Med. 26, 243–250. doi: 10.1007/s11655-020-3192-6
Ma, Y. J., and Lee, H. H. (2012). Understanding consumption behaviours for fair trade non-food products: focusing on self-transcendence and openness to change values. Int. J. Consum. Stud. 36, 622–634. doi: 10.1111/j.1470-6431.2011.01037.x
Mahase, E. (2020). Coronavirus: COVID-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ 368, m641. doi: 10.1136/bmj.m641
Memon, S., Pawase, V., Pavase, T., and Soomro, M. (2021). Investigation of COVID-19 impact on the food and beverages industry: China and India perspective. Foods 10, 1069. doi: 10.3390/foods10051069
Moynihan, A. B., van Tilburg, W. A. P., Igou, E. R., Wisman, A., Donnelly, A. E., Mulcaire, J. B., et al. (2015). Eaten up by boredom: consuming food to escape awareness of the bored self. Front Psychol. 6, 369. doi: 10.3389/fpsyg.2015.00369
Mullis, L., Saif, L. J., Zhang, Y., Zhang, X., and Azevedo, M. S. (2012). Stability of bovine coronavirus on lettuce surfaces under household refrigeration conditions. Food Microbiol. 30, 180–186. doi: 10.1016/j.fm.2011.12.009
Muscogiuri, G., Barrea, L., Savastano, S., and Colao, A. (2020). Nutritional recommendations for CoVID-19 quarantine. Eur. J. Clin. Nutr. 74, 850–851. doi: 10.1038/s41430-020-0635-2
Narayanan, L., Pandit, M., Basu, S., Karmakar, A., Bidhan, V., Kumar, H., et al. (2020). Impact of lockdown due to COVID-19 outbreak: lifestyle changes and public health concerns in India. Int. J. Indian Psychol. 8, 1385–1411. doi: 10.20944/preprints202006.0129.v1
Neovius, M., Linne, Y., and Rossner, S. (2005). BMI waist-circumference and waist-hip-ratio as diagnostic tests for fatness in adolescents. Int. J. Obes. 29, 163–169. doi: 10.1038/sj.ijo.0802867
Ng, W. H., Tipih, T., Makoah, N. A., Vermeulen, J-. G., Goedhals, D., Sempa, J. B., et al. (2021). Comorbidities in SARS-CoV-2 patients: a systematic review and meta-analysis. MBio 12, 1–12. doi: 10.1128/mBio.03647-20
Nieman, D. C. (2020). Effects of exercise training on immune function and implications for nutrition support. Altern Ther Health 26, 17–19.
Obayelu, A. E., Obayelu, O. A., Bolarinwa, K. K., and Oyeyinka, R. A. (2021). Assessment of the immediate and potential long-term effects of COVID-19 outbreak on socioeconomics, agriculture, security of food and dietary intake in Nigeria. Food Ethics 6, 5. doi: 10.1007/s41055-021-00085-w
Opichka, K., Smith, C., and Levine, A. S. (2019). Problematic eating behaviors are more prevalent in African American women who are overweight or obese than African American women who are lean or normal weight. Fam. Commun. Health 42, 81–89. doi: 10.1097/FCH.0000000000000222
Pietrobelli, A., Pecoraro, L., Ferruzzi, A., Heo, M., Faith, M., Zoller, T., et al. (2020). Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity 28, 1382–1385. doi: 10.1002/oby.22861
Poobalan, A. S., Aucott, L. S., Clarke, A., and Smith, W. C. S. (2014). Diet behaviour among young people in transition to adulthood (18–25 year olds): a mixed method study. Health Psychol. Behav. Med. 2, 909–928. doi: 10.1080/21642850.2014.931232
Pravst, I., Raats, M. M., and Chang, B. P. I. (2022). Editorial: The effects of the COVID-19 outbreak on food supply, dietary patterns, nutrition, and health: volume 1. Front. Nutr. 9, 845374. doi: 10.3389/fnut.2022.845374
Pung, R., Chiew, C. J., Young, B. E., Chin, S., Chen, M. I., Clapham, H. E., et al. (2020). Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet 395, 1039–1046. doi: 10.1016/S0140-6736(20)30528-6
Rebello, C. J., Kirwan, J. P., and Greenway, F. L. (2020). Obesity, the most common comorbidity in SARS-CoV-2: is leptin the link? Int. J. Obes. 2020, 1-8. doi: 10.1038/s41366-020-0640-5
Reiley, L. (2020). Meat processing plants are closing due to COVID-19 outbreaks. Beef shortfalls may follow. Washington Post, 16.
Reissman, D. B., Watson, P. J., Klomp, R. W., Tanielian, T. L., and Prior, S. D. (2006). Pandemic influenza preparedness: adaptive responses to an evolving challenge. J. Homel Secur. Emerg. 3:1–26. doi: 10.2202/1547-7355.1233
Rodriguez-Besteiro, S., Tornero-Aguilera, J. F., Fernandez-Lucas, J., and Clemente-Suarez, V. J. (2021). Gender differences in the COVID-19 pandemic risk perception, psychology, and behaviors of Spanish University students. Int. J. Environ. Res. Public Health 18. doi: 10.3390/ijerph182010918
Rodriguez-Perez, C., Molina-Montes, E., Verardo, V., Artacho, R., Garcia-Villanova, B., Guerra-Hernandez, E. J., et al. (2020). Changes in dietary behaviours during the COVID-19 Outbreak Confinement in the Spanish COVIDiet study. Nutrients 12, 1730. doi: 10.3390/nu12061730
Rosales, G., and Mercado, W. (2020). Effect of changes in food price on the quinoa consumption and rural food security in Peru. Sci. Agropec. 11, 83–93. doi: 10.17268/sci.agropecu.2020.01.10
Ruiz-Roso, M. B., Carvalho Padilha, d. e., Mantilla-Escalante, P., Ulloa, D. C., Brun, N., Acevedo-Correa, P., et al. (2020). Covid-19 confinement and changes of adolescent's dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 12, 1807. doi: 10.3390/nu12061807
Rundle, A. G., Park, Y., Herbstman, J. B., Kinsey, E. W., and Wang, Y. C. (2020). COVID-19 related school closings and risk of weight gain among children. Obesity 28, 1008. doi: 10.1002/oby.22813
Serra-Majem, L., Tomaino, L., Dernini, S., Berry, E. M., Lairon, D., de la Cruz, J. N., et al. (2020). Updating the mediterranean diet pyramid towards sustainability: focus on environmental concerns. Int. J. Environ. Res. Public Health 17, 8758. doi: 10.3390/ijerph17238758
Shereen, M. A., Khan, S., Kazmi, A., Bashir, N., and Siddique, R. (2020). COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 24, 91–98. doi: 10.1016/j.jare.2020.03.005
Shirvani, S. S., Nouri, M., Sakhinia, E., Babaloo, Z., Mohammadzaeh, A., Alipour, S., et al. (2019). The molecular and clinical evidence of vitamin D signaling as a modulator of the immune system: role in Behcet's disease. Immunol. Lett. 210, 10-19. doi: 10.1016/j.imlet.2019.03.017
Sidor, A., and Rzymski, P. (2020). Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients 12, 1657. doi: 10.3390/nu12061657
Singhal, T. A. (2020). Review of coronavirus disease-2019 (COVID-19). Indian J. Pediatr. 87, 281–286. doi: 10.1007/s12098-020-03263-6
Sinha, S., Cheng, K., Aldape, K., Schiff, E., and Ruppin, E. (2020). Systematic cell line-based identification of drugs modifying ACE2 expression. doi: 10.20944/preprints202003.0446.v1
Sinska, B., Jaworski, M., Panczyk, M., Traczyk, I., and Kucharska, A. (2021). The Role of resilience and basic hope in the adherence to dietary recommendations in the polish population during the COVID-19 pandemic. Nutrients 13, 2108. doi: 10.3390/nu13062108
Tamara, A., and Tahapary, D. L. (2020). Obesity as a predictor for a poor prognosis of COVID-19: a systematic review. Diabetes Metab. Synd. 14, 655–659. doi: 10.1016/j.dsx.2020.05.020
Tornero-Aguilera, J. F., and Clemente-Suarez, V. J. (2021). Cognitive and psychophysiological impact of surgical mask use during university lessons. Physiol. Behav. 234, 113342. doi: 10.1016/j.physbeh.2021.113342
Valdes-Ramos, R., Martinez-Carrillo, B. E., Aranda-Gonzalez, I. I., Guadarrama, A. L., Pardo-Morales, R. V., Tlatempa, P., et al. (2010). Diet, exercise and gut mucosal immunity. Proc Nutr Soc 69, 644–650. doi: 10.1017/S0029665110002533
van Zelst, C. M., Janssen, M. L., Pouw, N., Birnie, E., Cabezas, M. C., Braunstahl, G. J., et al. (2020). Analyses of abdominal adiposity and metabolic syndrome as risk factors for respiratory distress in COVID-19. BMJ Open Respir Res. 7, e000792. doi: 10.1136/bmjresp-2020-000792
Vo, T. L. H., and Thiel, D. (2006). A system dynamics model of the chicken meat supply chain faced with bird flu. Nantes, France: University of Nantes.
WFP (2022). COVID-19 Will Double Number of People Facing Food Crises Unless Swift Action is Taken. Media release.
WHO (2019). Coronavirus Disease (COVID-19) Pandemic. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov (accessed September 10, 2021).
WHO (2020). Water, Sanitation, Hygiene, and Waste Management for SARS-CoV-2, the Virus that Causes COVID-19. Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-WASH-2020.4 (accessed August 20, 2022).
Wu, Y.-C., Chen, C. S., and Chan, Y. J. (2020). The outbreak of COVID-19: an overview. JCMA 83, 217–220. doi: 10.1097/JCMA.0000000000000270
Wypych, T. P., Marsland, B. J., and Ubags, N. D. J. (2017). The impact of diet on immunity and respiratory diseases. Ann. Am. Thorac. Soc. 14, S339–S347. doi: 10.1513/AnnalsATS.201703-255AW
Yang, J., Hu, J. H., and Zhu, C. Y. (2021). Obesity aggravates COVID-19: a systematic review and meta-analysis. J. Med. Virol. 93, 257–261. doi: 10.1002/jmv.26237
Yang, Y., Islam, M. S., Wang, J., Li, Y., and Chen, X. (2020). Traditional Chinese medicine in the treatment of patients infected with 2019-new coronavirus (SARS-CoV-2): a review and perspective. Int. J. Biol. Sci. 16, 1708–1717. doi: 10.7150/ijbs.45538
Yousafzai, A. K., Rasheed, M. A., and Bhutta, Z. A. (2013). Annual research review: improved nutrition-a pathway to resilience. J. Child Psychol. Psychiatry 54, 367–377. doi: 10.1111/jcpp.12019
Zhao, A., Li, Z. Y., Ke, Y. L., Huo, S. S., Ma, Y. D., Zhang, Y. M., et al. (2020). Dietary Diversity among Chinese Residents during the COVID-19 Outbreak and Its Associated Factors. Nutrients 12. doi: 10.3390/nu12061699
Zhao, Q. W., Meng, M., Kumar, R., Wu, Y. L., Huang, J. F., Deng, Y. L., et al. (2020). Lymphopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a systemic review and meta-analysis. Int. J. Infect. Dis. 96, 131–135. doi: 10.1016/j.ijid.2020.04.086
Zhao, X., Gang, X. K., He, G. Y., Li, Z., Lv, Y., Han, Q., et al. (2020). Obesity increases the severity and mortality of influenza and COVID-19: a systematic review and meta-analysis. Front. Endocrinol. 11, 595109. doi: 10.3389/fendo.2020.595109
Zhao, X., Lei, Z. H., Gao, F. W., Xie, Q. Y., Jang, K., Gong, J., et al. (2021). The impact of coronavirus disease 2019 (COVID-19) on liver injury in China A systematic review and meta-analysis. Medicine 100, e24369. doi: 10.1097/MD.0000000000024369
Keywords: COVID-19, food supply, dietary patterns, nutrition, health
Citation: Roy PK, Song MG, Jeon EB, Kim SH and Park SY (2022) Effects of dietary intake behavior, food supply, nutrition, and health during the COVID-19 outbreak. Front. Sustain. Food Syst. 6:1032750. doi: 10.3389/fsufs.2022.1032750
Received: 31 August 2022; Accepted: 03 November 2022;
Published: 24 November 2022.
Edited by:
Roberta Selvaggi, University of Catania, ItalyReviewed by:
Seydi Yikmiş, Namik Kemal University, TurkeyGiuseppina Rizzo, University of Palermo, Italy
Copyright © 2022 Roy, Song, Jeon, Kim and Park. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shin Young Park, c3lwYXJrQGdudS5hYy5rcg==
 Pantu Kumar Roy
Pantu Kumar Roy Min Gyu Song
Min Gyu Song Eun Bi Jeon
Eun Bi Jeon Shin Young Park
Shin Young Park