
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CURRICULUM, INSTRUCTION, AND PEDAGOGY article
Front. Public Health , 17 February 2025
Sec. Public Health Education and Promotion
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1493331
This article is part of the Research Topic Vaccine Education and Promotion View all 30 articles
 Eseosa Olive Osaghae1*
Eseosa Olive Osaghae1* Greta Sirek2
Greta Sirek2 Tonya Roberson3
Tonya Roberson3 Mia Chandler4
Mia Chandler4 Ariel Childs5
Ariel Childs5 Monica Crespo-Bosque6
Monica Crespo-Bosque6 Gina Curry7
Gina Curry7 Amar Dhand8
Amar Dhand8 Mary Dollear9
Mary Dollear9 Alice Eggelston10
Alice Eggelston10 Nnenna Ezeh11
Nnenna Ezeh11 Dieufort Fleurissaint12
Dieufort Fleurissaint12 Denice Garrett13
Denice Garrett13 Gail Granville14
Gail Granville14 Muriel Jean-Jacques15
Muriel Jean-Jacques15 Elena Losina16,17
Elena Losina16,17 Holly Milaeger1
Holly Milaeger1 Lutfiyya Muhammad18
Lutfiyya Muhammad18 Mary Ann Nelson19
Mary Ann Nelson19 Chisa Nosamiefan20
Chisa Nosamiefan20 Bisola Ojikutu12,16,21
Bisola Ojikutu12,16,21 Neil Pillai1
Neil Pillai1 Mary Beth Son2
Mary Beth Son2 Marie Jacques Toussaint22
Marie Jacques Toussaint22 Ana Valle2
Ana Valle2 Jessica N. Williams23
Jessica N. Williams23 Michael York6
Michael York6 Karen Mancera-Cuevas24
Karen Mancera-Cuevas24 Candace H. Feldman2,16
Candace H. Feldman2,16 Rosalind Ramsey-Goldman1
Rosalind Ramsey-Goldman1Despite the efficacy of the COVID-19 vaccine in reducing mortality and illness severity, racial inequities in vaccination uptake persist. Among individuals with rheumatologic conditions who are often immunocompromised, the impact of disparities in preventive care threatens to widen existing inequities in adverse outcomes related to COVID-19 infection. There exists an urgent need to develop interventions that reduce COVID-19 vaccine hesitancy and promote vaccine uptake. We leveraged long-standing community-academic partnerships in two cities to develop a curriculum that will be part of an intervention to decrease COVID-19 vaccine hesitancy within Black communities. We describe the collaborative efforts that resulted in the creation of two interactive virtual curricula with similar core content but different theoretical lenses. One lens uses a racial justice approach to acknowledge the effects of historical and current structural racism on vaccine hesitancy, the other utilizes a traditional biomedical lens. In a future trial, we will compare the efficacy of these curricula to empower Black individuals identified as Popular Opinion Leaders (POLs), or trusted community members with large social networks, to disseminate health information to promote COVID-19 vaccine uptake. Strategies to reduce racial inequities in COVID-19 vaccine uptake must begin with accurately identifying and empathetically acknowledging the root causes of vaccine hesitancy, as well as addressing nuanced concerns that drive vaccine avoidance among Black individuals. Community engagement and collaboration are central in creating interventions to develop and test culturally relevant strategies, as observed with our curricula, that bridge scientific efforts with community concerns and practices.
With an estimated death toll of 14.8 million globally and approximately 1.1 million lives lost along with 6.4 million hospitalizations in the United States alone, the COVID-19 pandemic profoundly impacted the world on an unprecedented scale and specifically revealed many shortcomings present within the United States healthcare system (1, 2). Currently, historically marginalized populations remain disproportionately affected by the COVID-19 pandemic. Accounting for nearly 13% of the United States population, individuals of African ancestry, here after referred to as Black, are more likely to contract COVID-19 and experience adverse long-term outcomes (3–5). With higher hospitalization rates, these individuals are more likely to require intensive care unit admission, mechanical ventilation, and have an 11% higher mortality rate than their white counterparts (3, 6, 7). It is essential to note that there is significant heterogeneity within the Black population and many statistics related to COVID-19 do not specifically address ancestry (5). Yet, despite the efficacy of the COVID-19 vaccine and its subsequent boosters, we continue to see this population have lower COVID-19 vaccination rates and report more hesitancy to get vaccinated or receive a booster (8–10). As one of the top threats to global health as described by the World Health Organization, vaccination hesitancy refers to “a delay or refusal to accept vaccination despite its availability (11).” At the height of the pandemic, misinformation and the rise of anti-vaccination movements bolstered an increase in global vaccine hesitancy and avoidance (12). Though U.S.-based Black individuals were not exempt from this phenomenon, the roots of vaccination hesitancy in this group extend past misinformation and harken back to historical instances of unethical and unjust practices in the healthcare system that have ultimately bred mistrust and avoidance (12).
The pervasiveness of vaccination hesitancy within this population is concerning as certain rheumatic conditions like systemic lupus erythematosus (SLE) disproportionately affect Black individuals, and require immunosuppressive therapies, which heighten risk of severe infection (13, 14). Studies have demonstrated reduced efficacy of the COVID-19 vaccine in immunosuppressed individuals, highlighting the importance both of booster vaccinations and of advocacy to vaccinate not only individuals with rheumatic conditions but also their close contacts (15). Thus, our future intervention trial focuses on addressing and ultimately, decreasing vaccine hesitancy among Black individuals with rheumatic conditions.
In this paper, we describe the process of developing two virtual curricula, informed by the racial justice and biomedical models, respectively, with collaboration between longstanding academic and community partners in two cities. These curricula contain similar core content with two different lenses and objectives (Figure 1; Table 1). We ultimately aim to use these curricula to train Popular Opinion Leaders (POLs), or trusted community leaders, to disseminate health information to their social network members. Our forthcoming trial utilizes the POL model, an evidence-based and community-based approach previously used to reduce HIV stigma and increase SLE awareness (16, 17). Grounded in the social network and diffusion of innovation theories, the POL model trains community leaders to engage their social network members in health-related discussions that ultimately lead to adoption of positive health norms and behaviors (17, 18). Thus, our primary goals are to influence the content of these discussions through developing curricular material that trains POLs while determining the efficacy of two distinct curricular perspectives - biomedical versus racial justice – in training these POLs to effectively disseminate information concerning the COVID-19 vaccine. This dissemination is intended to decrease COVID-19 vaccine hesitancy and increase vaccine uptake among their social network members. This paper’s objective is to illustrate our community-engaged, iterative approach to design these two curricula and their relevant pre- and post-tests for use in this planned NIH-funded randomized clinical trial (Northwestern University Institutional Review Board (IRB, ID #STU00217038) and Mass General Brigham IRB (#2022P000633 and #2023P000686) (19).
To decrease COVID-19 vaccine hesitancy, current strategies commonly emphasize educating individuals about COVID-19 through development of innovative training materials. These teaching materials are often framed with a biomedical lens highlighting the vaccine as an individual-level tool to prevent serious infection. This model proposes that illness primarily arises as an outcome of abnormal biology or deviations from normal physiological function with psychological or sociological factors having less significant roles (20). With the biomedical approach, the COVID-19 vaccine is placed among other trusted preventative health practices with vaccine hesitancy addressed primarily by acknowledging and addressing scientific concerns. An example of a strategy utilizing the biomedical model involved the creation of a digital intervention through individualized motivational interviewing techniques that addressed COVID-19 vaccine misinformation and provided education about its development following a systematic literature review and qualitative interviews with public health experts (21).
Previously published work that involved semi-structured interviews with physicians and community leaders to determine barriers toward COVID-19 vaccination for Black individuals identified strategies that differed from the biomedical model to decrease COVID-19 vaccine hesitancy (22). These strategies emphasized the importance of acknowledging racial, ethnic and socioeconomic injustices, using compassionate and motivational messaging, and addressing misinformation, that is, taking a racial justice-oriented approach (22). Unlike the biomedical approach, the racial justice model recognizes and openly acknowledges the role of current and historical racial and social inequities in poor health outcomes, focusing on population-level motivations and goals as opposed to individual-level objectives (23). This model contends that acknowledging and addressing the psychological and sociological health of Black communities is an essential factor to reduce health inequities. We see this strategy utilized by Peteet et al. (24) with the development of a webinar for Black churchgoers that discussed the psychology behind the fear of the COVID-19 vaccine by acknowledging medical mistrust. Another study reported the development of a vaccine education campaign focused on transparency and having culturally sensitive discussions regarding COVID-19 vaccine hesitancy with Black employees of nursing homes and their social networks (25). Though both interventions successfully decreased COVID-19 vaccine hesitancy in their respective populations, neither study compared racial justice-focused strategies to the norm, a biomedical-based educational approach to understand if there was a difference in efficacy between these two models. Therefore, to develop innovative strategies to reduce COVID-19 vaccine hesitancy among Black individuals, it is necessary to determine which educational model is more successful in changing health attitudes and behaviors.
Diffusion of innovation theory, the foundation of the POL model, focuses on the process of how and why innovative ideas and behaviors are adopted in a population (18). It proposes that searching for and creating new methods that better fit existing ideals and needs of hesitant individuals is necessary for behavioral change (18). This theory describes early adopters as individuals who embrace change and cautiously adopt new behaviors, and early and late majorities as individuals who are hesitant, and require more information and time for deliberation (18). Thus, when considering our approach to decrease COVID-19 vaccine hesitancy among Black individuals, we aimed to develop educational materials that were informative and both culturally relevant and sensitive such that Black individuals or POLs who are “early adopters” of the COVID-19 vaccine can influence members of their communities and social networks who might then become part of the “early and late majorities” (18).
These curricula were created to be delivered to Black individuals who are older than 18 years, have a rheumatic and musculoskeletal condition, speak English, and have received at least one COVID-19 vaccine. These individuals will receive curricula training virtually over Zoom meetings.
To develop our curricula, we utilized longstanding collaborations between our research team and academic and community partners from Boston and Chicago. This group consisted of racially and ethnically diverse academic clinicians and researchers, rheumatic disease, infectious disease, and general medicine healthcare providers, neighborhood organization and community leaders, advocacy groups, social workers, and experts in public health. POLs from our previous studies were also significant members in this group. These individuals met monthly through Zoom meetings within and across both cities since summer 2022 and continue to meet.
To create our curricula, we leveraged findings from previous work where a series of semi-structured interviews with physician and community stakeholders focused on finding strategies to address COVID-19 vaccine hesitancy among Black individuals with rheumatic condition (22). Combining information from this work with the lived experiences and expertise of our community and academic partners, we planned to develop curricula that would accomplish the objectives as seen in Figure 1 (22).
Following the development of the learning objectives, we used multiple methods to review existing literature to understand inequities in vaccine uptake and adverse COVID-19 outcomes, as well as historical racial injustices. Meeting with our community and academic partners to discuss the concerns and questions they had heard about the COVID-19 vaccine from their patients and community members informed further literature review and our curricula drafts.
After creating the curricula’s initial drafts, developed using Microsoft PowerPoint, we sent the materials to our community and academic partners for review. Each partner also received a worksheet that allowed them to reflect and comment on their thoughts and concerns after reviewing the slides. This worksheet contained guided questions such as, “please list any slides you found confusing,” “suggest how the slides can be improved,” and “were the goals of this module clear?” After the partners completed their review, our research team met with them over Zoom meetings to discuss any suggestions and feedback. This process was repeated numerous times during the development of our curricula to ensure the curricula met our objectives. Throughout this iterative process to develop educational materials that accurately accomplished our learning objectives, the primary challenges we repeatedly encountered were addressing the curricula’s content, accessibility, and tone (Figure 2).
Developing both curricula content involved multiple methods to broaden our understanding of COVID-19 incidence and prevalence, vaccine development, vaccination recommendations, and common misconceptions regarding vaccination. Various sources were reviewed and utilized including data from the Centers for Disease Control and Prevention (CDC), articles from the lay press, and peer-reviewed published manuscripts in PubMed indexed journals. Creating the material for the curriculum with a racial justice lens required extensive research about data on bias and mistrust in medicine and historical and current treatment of Black individuals in the health care system and general society. Furthermore, upon receiving feedback from some of our partners regarding tailoring the curriculum content specifically to the sites where we will ultimately deliver the curriculum, we searched for distinct examples of how the healthcare systems in both cities addressed mistrust and medical bias. Additional content to inform the biomedical lens involved review of health screening and preventative guidelines for people with rheumatic conditions (15). Some of our public health experts provided several examples of teaching materials focused on preventative care which were incorporated into our curriculum.
Given the collaborative nature of the curricular development, at times, our community and academic partners had differing perspectives on the curricula’s content. To address these conflicts, we integrated the varying ideas into our curricula drafts and, as part of the iterative process, invited our partners to evaluate which approach best aligned with our overall goals.
During meetings with our community and academic partners, we identified certain language used in our curricula drafts that was too scientific or contained medical jargon, which would limit accessibility of our curricula to a broad audience (Figure 3). To enhance the materials’ comprehensibility and create an approachable learning environment, we revised the language used, replacing technical terminology with understandable terms (Figure 3). Several strategies were used to check on the literacy of the materials including having the curricula reviewed by individuals blinded to the curricula or intervention’s goals. A literacy check was conducted to ensure the language met the desired comprehension level of an 8th-grade student (26). Based on feedback and comments about challenges understanding biomedical terminology, we also created a glossary to define terms such as “beneficence” or “variant” to further achieve this goal.
In our meetings, we frequently discussed the tone of the curricula, particularly the version with the racial justice lens. Initially, the feedback from our community and academic partners was that this curriculum lens could be perceived as disheartening and demoralizing notably when discussing racial bias or discrimination Black individuals encounter. In response, we made this curriculum’s language empowering and removed images that elicited feelings of disillusionment identified by community members as problematic (Figure 4). We changed the language used in the curriculum from having an individualized perspective, removing any individualized culpability and instead, created a sense of collective responsibility. For example, rather than stating, “here’s what you need to do to become healthier,” we revised the curriculum to describe a collective “we” as in “here’s how we can be healthier.” In addition, we added information about current initiatives within the healthcare system that address issues such as medical mistrust and bias to further decrease feelings of frustration or defeat for curricula learners.
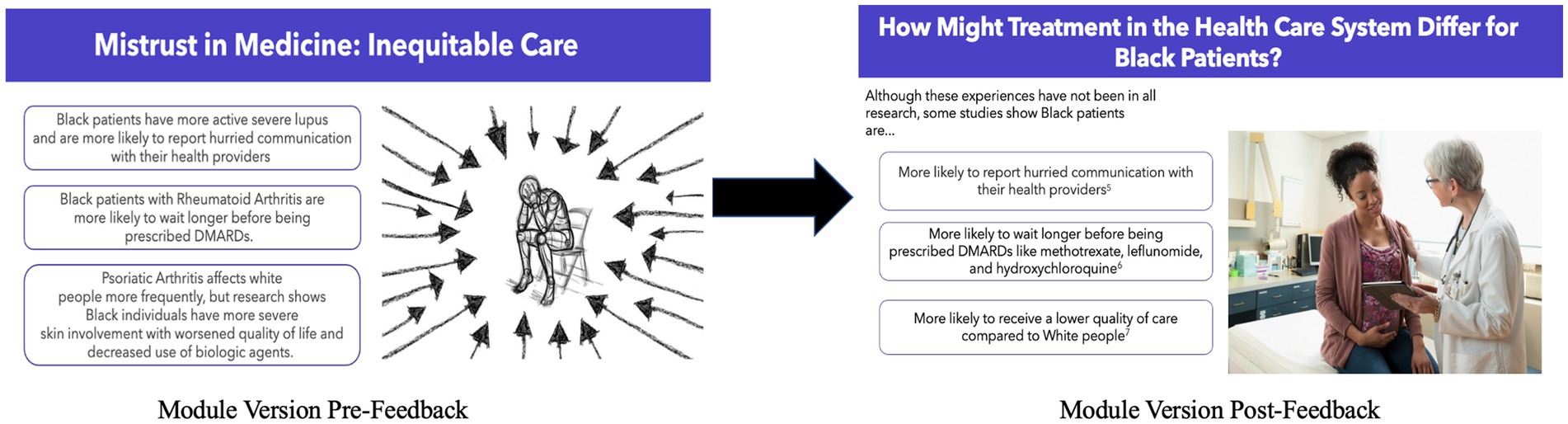
Figure 4. Curricula outcome of addressing feedback about tone. Image 1 is reprinted with permission from “Stress Burnout Despair” by Gerd Altman, licensed under Content License. Image 2 is reprinted with permission from “Gynecologist with digital tablet comforting pregnant patient” by Jose Luis Pelaez under a Royalty-free license.
We addressed feedback about the lecture-based tone of both curricula by making the modules more interactive with content checks and multiple choice/true or false questions, and specifically created a module to practice anticipated conversations using role play.
To assess POLs curricular knowledge retention following training, we followed the format of previous research where a curriculum was developed for POLs to promote familiarity of clinical trials and research methods to Black individuals with Lupus (27). Similar to that study, each module in our curricula contained pre- and post-test questionnaires to assess POLs’ knowledge acquisition. Each curriculum had similar questions testing core competencies, but also contained additional questions specific to that curriculum’s lens. These test questions had a format of multiple choice, short answer, and true or false per feedback from the previous POL study suggesting only utilizing a multiple-choice format was intimidating (27). These questions, along with the curricula slides, were sent to our community and academic partners to review. They were asked to assess the clarity and simplicity of the questions with space to offer suggestions for improvement, which were then incorporated into the pre- and post-tests (Supplementary Table 1).
Following an iterative process with our community and academic partners over a period of a year, we developed two virtual curricula with shared core content, but two different theoretical lenses. Each curriculum contained five distinct modules as described below. The curricula both provide education about the development of the COVID-19 vaccine and address COVID-19 misinformation. The modules with a racial justice lens describe the origins of vaccine hesitancy among the Black population and the health care system’s role informing this belief, whereas the curriculum with a biomedical lens explores the importance of preventative care and highlights the COVID-19 vaccine as a tool in reducing an individual’s adverse health outcomes.
Module I: We described the role of POLs as trusted individuals within their social networks. These modules discussed how these individuals will influence and promote healthy behaviors in their communities.
Module II: We discussed the mechanism and development of the COVID-19 vaccine, detailing its side effects and safety profile (Figure 3). These modules included information about COVID-19 risks, current epidemiology data, and education regarding various rheumatic disease presentations. The curriculum with the racial justice lens differed from the biomedical lens by specifically detailing COVID-19 risk in Black populations and provided trial data about Black individuals’ participation in the development of the COVID-19 vaccine.
Module III: We described common myths and provided evidence-based discussions to dispel misinformation about the COVID-19 vaccine. Some myths discussed were concerns that the COVID-19 vaccine could cause COVID-19 infection and beliefs that there was an increased possibility or likelihood of getting severe side effects from the COVID-19 vaccine such as stroke, infertility, and sudden death. Other myths addressed included concerns about how quickly the COVID-19 vaccine was developed, beliefs about the presence of dangerous ingredients within the vaccine, and notions that the vaccine was a government ploy. The curriculum framed with the racial justice lens also addressed concerns regarding the diversity of individuals involved in developing and participating in the COVID-19 research clinical trials.
Module IV: The racial justice framed curriculum defined structural racism, discussed etiologies of current inequities in the COVID-19 infection risk and severity for the Black population, and addressed healthcare mistrust by acknowledging past injustices within the health care system and current methods for preventing recurrence (Figure 4). Short video recordings and visual art played prominent roles in this module to explain difficult and emotionally charged concepts. The module from the curriculum framed with the biomedical lens discussed general preventative care strategies including highlighting the importance of nutrition, physical activity, cancer screenings, and vaccinations for individuals with rheumatic conditions. The objective of this module was to describe the COVID-19 vaccine as a form of preventative care.
Module V: We emphasized the role POLs play as community researchers. We discussed data collection procedures, highlighting HIPAA and confidentiality.
Module VI: We provided a summary of the prior modules, revisiting any key information previously discussed. These modules included role play to reinforce previous teaching and allow POLs to practice having difficult conversations.
As of December 2024, we have recruited our POLs at both cities and randomized them to either receive the racial justice or biomedical framed curriculum for their training (19). We will begin teaching the POLs virtually mid- December and pre and post-tests will be administered for each module to ensure that the teaching is effective. POLs will then be asked to disseminate the information they learned through their social networks and COVID-19 vaccine uptake among network members will be assessed.
Inequities in COVID-19 vaccination uptake have often been attributed to poorer access to the vaccine and misinformation regarding vaccine safety and testing (28). However, a critical factor is the strained relationship between the United States’ healthcare system and Black communities due to longstanding discrimination and societal and healthcare injustices. Prior studies document that Black individuals are more likely to report hurried communication with their health providers and feel less cared for or listened to by their physicians (29, 30). These experiences coupled with historical and contemporary examples of racism and mistreatment have led to medical mistrust which ultimately play a key role in COVID-19 vaccine hesitancy (31). To address COVID-19 vaccine hesitancy and improve vaccine uptake among Black individuals, we have developed two virtual curricula that will equip community leaders across two cities who identify as Black to disseminate information about the COVID-19 vaccine and acknowledge concerns about the vaccine to hesitant Black individuals given prior and current racial injustices. The objectives of these curricula are to acknowledge the historical and current racial discrimination Black individuals encounter in the healthcare system, address the role these interactions have on COVID-19 vaccine hesitancy, and ultimately empower Black individuals to teach members of their social networks, through transparent and informative discussions, about the importance of getting vaccinated.
One of the innovative aspects of creating these curricula is the utilization of community and academic partnerships at every step of the developmental process to shape the curricula’s content, accessibility, and tone. From previous work involving focus groups with community leaders and physician partners, we know that strategies to improve COVID-19 vaccine uptake in Black populations with rheumatic conditions must be motivational while acknowledging and addressing racial and social injustices (22). Prior studies have described the need for a social justice framework in public health education that adequately recognizes the effects of social inequities on health outcomes (23). Many researchers have developed anti-racist curricula to educate health professionals and equip them with tools to address health inequities (32–34). With our curricula, created by a diverse group of individuals motivated by the common mission to reduce inequities, we step outside of the health system into the community and focus attention on the individuals affected by these inequities to create materials that are directly informed by their perspectives and experiences.
Another benefit of community engaged collaboration is the creative environment these interactions form that leads to the development and implementation of innovative ideas. Currently, the literature is lacking data on which curricular approach, the traditional biomedical or the racial justice model, is more successful for improving COVID-19 vaccine uptake among Black individuals. Creating two adjacent curricula with these two lenses addresses this gap by allowing for direct comparison to determine which perspective leads to knowledge acquisition and which leads to more effective knowledge dissemination to reduce inequities in COVID-19 vaccination. Independent of curricula perspective, developing these curricula addresses the urgent need for researchers in public health to find strategies that reduce COVID-19 vaccination inequities for Black individuals. However, creating a racial justice curriculum specifically acknowledges the population that lives with these inequities and establishes materials that directly caters to this group on a sociological, psychological, and cultural level. The COVID-19 pandemic only highlighted known racial and ethnic health inequities that are deeply rooted in our society. The iterative process used to develop these curricula acknowledges and addresses these inequities while providing useful information for future curricula development and interventions that address other health issues where we find similar inequities.
As with any curricula development, there were notable challenges in this process. One such challenge involved resolving conflicting ideas and suggestions between team members which is inevitable within collaborative efforts. Being cognizant of the etiologies of these suggestions along with the role life experiences played in each person’s perspective led to learning opportunities that enriched this work and future perspectives. Though our curricula discuss concerns Black individuals have about the COVID-19 vaccine, we recognize the great heterogeneity within the United States Black population and note that our curricula do not represent the entirety of diverse perspectives and concerns within this group (5). However, due to structural racism, there are commonalities regarding concerns about the COVID-19 vaccine and the health care system generally that stem from similar experiences of racism that we hope to acknowledge and represent. Moreover, for our future intervention, we plan to recruit a diverse group of POLs to capture aspects of the diversity within the Black population.
Addressing COVID-19 vaccination uptake and decreasing vaccine hesitancy among Black individuals is essential. Strategies to improve health outcomes for Black individuals are most successful when trusted members from their communities are included in the development of these interventions. This collaboration, which can be replicated in other cities and countries, lays the groundwork for transparency and trust which increases the likelihood of creating impactful, effective, and culturally sensitive work.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
EO: Writing – original draft, Writing – review & editing. GS: Writing – review & editing. TR: Writing – review & editing. MC: Writing – review & editing. AC: Writing – review & editing. MC-B: Writing – review & editing. GC: Writing – review & editing. AD: Writing – review & editing. MD: Writing – review & editing. AE: Writing – review & editing. NE: Writing – review & editing. DF: Writing – review & editing. DG: Writing – review & editing. GG: Writing – review & editing. MJ-J: Writing – review & editing. EL: Writing – review & editing. HM: Writing – review & editing. LM: Writing – review & editing. MN: Writing – review & editing. CN: Writing – review & editing. BO: Writing – review & editing. NP: Writing – review & editing. MT: Writing – review & editing. MS: Writing – review & editing. AV: Writing – review & editing. JW: Writing – review & editing. MY: Writing – review & editing. KM-C: Writing – review & editing. CF: Writing – review & editing. RR-G: Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institute of Health under award number R01 AR080089-01A1 to Northwestern (MPIs: Ramsey-Goldman; contact PI and Feldman).
Rosalind Ramsey-Goldman served as Chair of the Collaborative Initiatives Committee for the American College of Rheumatology. She consults for Merck, Biogen, Cabaletta, Exagen Diagnostics, Ampel Solutions, Clarivate, Upstart Research all less than $10 K. She has consults for Duke University and the State University of New York, Syracuse. She is supported by the John P. Gallagher Research Professor of Rheumatology at Northwestern University, and she serves on the Medical and Scientific Advisory Council of the Lupus Foundation of America and on the Site Selection & Evaluation Committee for Lupus Therapeutics, an arm of the Lupus Research Alliance. She has received honoraria for lectures from Georgetown University, AstraZeneca, and the International Lupus meeting in Korea. Candace Feldman serves on the DEI Task Force for the Arthritis Foundation and the DEI Committee for the American College of Rheumatology. She consults for OM1, Inc., Bain Capital, LP, the Lupus Foundation of America, and the American College of Rheumatology, and previously consulted for Harvard Pilgrim and the University of Alabama. She serves on the Editorial Board of Arthritis Care & Research, as an Associate Editor for Lupus Science & Medicine and on the Medical and Scientific Advisory Council of the Lupus Foundation of America. Chisa Nosamiefan serves as a consultant with The Light Collective and is a member of the Brigham and Women’s Hospital Patient Advisory Board.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can befound online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1493331/full#supplementary-material
1. CDC. COVID-19 Update for the United States [Internet]. Cdc.gov. (2023). Available at: https://stacks.cdc.gov/view/cdc/136367
2. Msemburi, W, Karlinsky, A, Knutson, V, Aleshin-Guendel, S, Chatterji, S, and Wakefield, J. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature. (2023) 613:130–7. doi: 10.1038/s41586-022-05522-2
3. Magesh, S, John, D, Li, WT, Li, Y, Mattingly-App, A, Jain, S, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and Meta-analysis. JAMA Netw Open. (2021) 4:e2134147. doi: 10.1001/jamanetworkopen.2021.34147
4. Jacobs, MM, Evans, E, and Ellis, C. Racial, ethnic, and sex disparities in the incidence and cognitive symptomology of long COVID-19. J Natl Med Assoc. (2023) 115:233–43. doi: 10.1016/j.jnma.2023.01.016
5. Dorsey, R, Wilson-Frederick, SM, Ejike-King, L, and González, G In: S Elswick, editor. Data collection: Methods, ethical issues and future directions. Memphis, Tennessee: Nova Science Publishers, Inc (2017). 195.
6. Mirajkar, A, Oswald, A, Rivera, M, Logan, G, Macintosh, T, Walker, A, et al. Racial disparities in patients hospitalized for COVID-19. J Natl Med Assoc. (2023) 115:436–40. doi: 10.1016/j.jnma.2023.06.006
7. Asch, DA, Islam, MN, Sheils, NE, Chen, Y, Doshi, JA, Buresh, J, et al. Patient and hospital factors associated with differences in mortality rates among black and White US Medicare beneficiaries hospitalized with COVID-19 infection. JAMA Netw Open. (2021) 4:e2112842. doi: 10.1001/jamanetworkopen.2021.12842
8. Willis, DE, Andersen, JA, Bryant-Moore, K, Selig, JP, Long, CR, Felix, HC, et al. COVID-19 vaccine hesitancy: race/ethnicity, trust, and fear. Clin Transl Sci. (2021) 14:2200–7. doi: 10.1111/cts.13077
9. Pfizer and BioNTech Announce Vaccine Candidate Against COVID-19 Achieved Success in First Interim Analysis from Phase 3 Study. (2020). Available at: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-announce-vaccine-candidate-against
10. Kelly, JD, Leonard, S, Hoggatt, KJ, Boscardin, WJ, Lum, EN, Moss-Vazquez, TA, et al. Incidence of severe COVID-19 illness following vaccination and booster with BNT162b2, mRNA-1273, and Ad26.COV2.S vaccines. JAMA. (2022) 328:1427–37. doi: 10.1001/jama.2022.17985
11. MacDonald, NE, and Hesitancy, SW. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
12. Savoia, E, Masterson, E, Olander, DR, Anderson, E, Mohamed Farah, A, and Pirrotta, L. Determinants of vaccine Hesitancy among African American and black individuals in the United States of America: a systematic literature review. Vaccines (Basel). (2024) 12, 1–28. doi: 10.3390/vaccines12030277
13. Grainger, R, Kim, AHJ, Conway, R, Yazdany, J, and Robinson, PC. COVID-19 in people with rheumatic diseases: risks, outcomes, treatment considerations. Nat Rev Rheumatol. (2022) 18:191–204. doi: 10.1038/s41584-022-00755-x
14. Nowell, WB, Barnes, EL, Venkatachalam, S, Kappelman, MD, Curtis, JR, Merkel, PA, et al. Racial and ethnic distribution of rheumatic diseases in health Systems of the National Patient-Centered Clinical Research Network. J Rheumatol. (2023) 50:1503–8. doi: 10.3899/jrheum.2022-1300
15. Curtis, JR, Johnson, SR, Anthony, DD, Arasaratnam, RJ, Baden, LR, Bass, AR, et al. American College of Rheumatology Guidance for COVID-19 vaccination in patients with rheumatic and musculoskeletal diseases: version 5. Arthritis Rheum. (2023) 75:E1–E16. doi: 10.1002/art.42372
16. Li, L, Guan, J, Liang, LJ, Lin, C, and Wu, Z. Popular opinion leader intervention for HIV stigma reduction in health care settings. AIDS Educ Prev. (2013) 25:327–35. doi: 10.1521/aeap.2013.25.4.327
17. Phillip, CR, Mancera-Cuevas, K, Leatherwood, C, Chmiel, JS, Erickson, DL, Freeman, E, et al. Implementation and dissemination of an African American popular opinion model to improve lupus awareness: an academic-community partnership. Lupus. (2019) 28:1441–51. doi: 10.1177/0961203319878803
18. Dearing, JW. Applying diffusion of innovation theory to intervention development. Res Soc Work Pract. (2009) 19:503–18. doi: 10.1177/1049731509335569
19. Sirek, G, Erickson, D, Muhammad, LN, Losina, E, Chandler, MT, Son, MB, et al. Community-engaged randomised controlled trial to disseminate COVID-19 vaccine-related information and increase uptake among black individuals in two US cities with rheumatic conditions. BMJ Open. (2024) 14:e087918. doi: 10.1136/bmjopen-2024-087918
20. Engel, GL. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196:129–36. doi: 10.1126/science.847460
21. Knight, H, Jia, R, Ayling, K, Bradbury, K, Baker, K, Chalder, T, et al. Understanding and addressing vaccine hesitancy in the context of COVID-19: development of a digital intervention. Public Health. (2021) 201:98–107. doi: 10.1016/j.puhe.2021.10.006
22. Ezeh, N, Sirek, G, Ulysse, SN, Williams, JN, Chandler, MT, Ojikutu, BO, et al. Understanding Stakeholders' perspectives to increase COVID-19 vaccine and booster uptake among black individuals with rheumatic conditions. Arthritis Care Res. (2023) 75:2508–18. doi: 10.1002/acr.25172
23. Munala, L, Allen, E, Beall, OM, and Phi, KM. Social justice and public health: a framework for curriculum reform. Pedagogy in Health Promotion. (2022) 9:231–3. doi: 10.1177/23733799221143375
24. Peteet, B, Watts, V, Tucker, E, Brown, P, Hanna, M, Saddlemire, A, et al. Faith, fear, and facts: a COVID-19 vaccination Hesitancy intervention for black church congregations. Vaccines (Basel). (2022) 10:1–11. doi: 10.3390/vaccines10071039
25. Feifer, RA, Bethea, L, and White, EM. Racial disparities in COVID-19 vaccine acceptance: building trust to protect nursing home staff and residents. J Am Med Dir Assoc. (2021) 22:1853–1855.e1. doi: 10.1016/j.jamda.2021.07.006
26. Flesch Kincaid Calculator. Available from: https://goodcalculators.com/flesch-kincaid-calculator/ (Accessed December 13, 2023).
27. Arneson, LC, Taber, KA, Williams, JN, Ulysse, SN, Erickson, DL, Chmiel, JS, et al. Use of popular opinion leader models to disseminate information about clinical trials to black individuals with lupus in two US cities. Arthritis Care Res. (2023) 75:44–52. doi: 10.1002/acr.24889
28. Sekimitsu, S, Simon, J, Lindsley, MM, Jones, M, Jalloh, U, Mabogunje, T, et al. Exploring COVID-19 vaccine Hesitancy amongst black Americans: contributing factors and motivators. Am J Health Promot. (2022) 36:1304–15. doi: 10.1177/08901171221099270
29. Martin, KJ, Stanton, AL, and Johnson, KL. Current health care experiences, medical trust, and COVID-19 vaccination intention and uptake in black and White Americans. Health Psychol. (2023) 42:541–50. doi: 10.1037/hea0001240
30. Sun, K, Eudy, AM, Criscione-Schreiber, LG, Sadun, RE, Rogers, JL, Doss, J, et al. Racial differences in patient-provider communication, patient self-efficacy, and their associations with systemic lupus erythematosus-related damage: a cross-sectional survey. J Rheumatol. (2021) 48:1022–8. doi: 10.3899/jrheum.200682
31. Williamson, LD, and Bigman, CA. A systematic review of medical mistrust measures. Patient Educ Couns. (2018) 101:1786–94. doi: 10.1016/j.pec.2018.05.007
32. Hagopian, A, West, KM, Ornelas, IJ, Hart, AN, Hagedorn, J, and Spigner, C. Adopting an anti-racism public health curriculum competency: the University of Washington experience. Public Health Rep. (2018) 133:507–13. doi: 10.1177/0033354918774791
33. Afolabi, T, Borowsky, HM, Cordero, DM, Paul, DW Jr, Said, JT, Sandoval, RS, et al. Student-led efforts to advance anti-racist medical education. Acad Med. (2021) 96:802–7. doi: 10.1097/ACM.0000000000004043
Keywords: community academic partnerships, COVID-19, African American/black, community health promotion, health equity, rheumatic and autoimmune disease, vaccine hesitancy
Citation: Osaghae EO, Sirek G, Roberson T, Chandler M, Childs A, Crespo-Bosque M, Curry G, Dhand A, Dollear M, Eggelston A, Ezeh N, Fleurissaint D, Garrett D, Granville G, Jean-Jacques M, Losina E, Milaeger H, Muhammad L, Nelson MA, Nosamiefan C, Ojikutu B, Pillai N, Son MB, Toussaint MJ, Valle A, Williams JN, York M, Mancera-Cuevas K, Feldman CH and Ramsey-Goldman R (2025) Community-engaged curriculum development using racial justice and biomedical lenses to address COVID-19 vaccine hesitancy in black individuals with rheumatologic conditions. Front. Public Health. 12:1493331. doi: 10.3389/fpubh.2024.1493331
Received: 09 September 2024; Accepted: 24 December 2024;
Published: 17 February 2025.
Edited by:
Carlos Alberto De Oliveira Magalhães Júnior, State University of Maringá, BrazilReviewed by:
Erica De Vita, University of Pisa, ItalyCopyright © 2025 Osaghae, Sirek, Roberson, Chandler, Childs, Crespo-Bosque, Curry, Dhand, Dollear, Eggelston, Ezeh, Fleurissaint, Garrett, Granville, Jean-Jacques, Losina, Milaeger, Muhammad, Nelson, Nosamiefan, Ojikutu, Pillai, Son, Toussaint, Valle, Williams, York, Mancera-Cuevas, Feldman and Ramsey-Goldman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eseosa Olive Osaghae, b2xpdmUub3NhZ2hhZUBub3J0aHdlc3Rlcm4uZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.