- 1Department of Internal Medicine Nursing, Faculty of Nursing, Hebei University of Chinese Medicine, Shijiazhuang, Hebei, China
- 2Faculty of Nursing, Hebei University of Chinese Medicine, Shijiazhuang, Hebei, China
Background: Colorectal cancer (CRC) is linked to obesity, particularly visceral fat. A more accurate measure of visceral fat accumulation is offered by a body shape index (ABSI). Currently, the direct application of the ABSI to populations with varying ethnic backgrounds might be restricted. Moreover, there is less evidence about the correlation between ABSI and CRC among individuals from different ethnical backgrounds.
Methods: A total of 40,998 individuals who took part in the National Health and Nutrition Examination Survey (NHANES) spanning from 2003 to 2023 were subjected to analysis. Logistic regression was utilized to examine the associations between the ABSI and the risk of CRC. In addition, restricted cubic spline curves (RCS) were utilized, and subgroup analyses along with interaction tests were also carried out. The receiver operating characteristic curve (ROC) was employed to predict the risk of CRC relying on various anthropometric indicators.
Results: After adjusting for covariates, ABSI demonstrated a positive association with the incidence of CRC (OR = 1.03 [95% CI: 1.01–1.05], p = 0.018). Individuals in the upper quartile of ABSI exhibited a greater prevalence of CRC than those in the lower quartile (OR = 1.88 [95% CI: 1.19–2.96], p = 0.006). RCS analysis indicated a nonlinear correlation between ABSI and CRC (P for nonlinear = 0.030). Subgroup analysis indicated a notable interaction between age and BMI subgroups (interaction p < 0.05), and ROC curves indicated that the ABSI was effective in predicting CRC risk (AUC = 0.658), demonstrating good sensitivity, particularly in individuals under 60 years of age.
Conclusion: A positive correlation exists between ABSI levels and the increased incidence of CRC among U.S. adults. This is especially true for people under 60 years of age (40–60 years), with a BMI below 25 kg/m2, and those with a BMI of 30 kg/m2 or beyond. ABSI can be used as a simple anthropometric predictor of CRC.
Introduction
Colorectal cancer (CRC), a malignant neoplasm, is witnessing an escalating prevalence on a global scale. Its morbidity and mortality figures stand among the highest in different kinds of cancers. In 2022, there were more than 1.9 million newly reported cases, and the number of fatalities reached 904,000 (1). The prevalence of colorectal cancer is rising in various nations, including China and the United States, with an increasingly younger demographic being impacted (2, 3). In light of this context, it is crucial to aggressively investigate more effective methods for the prevention and screening of CRC to significantly diminish its incidence rate.
The incidence of obesity has witnessed exponential growth on a global scale as a result of lifestyle alterations, impacting over 650 million individuals (4). In particular, it has been established that visceral obesity is a significant risk factor for CRC development (5, 6). However, it has been shown that traditional measures of obesity, like the body mass index (BMI), possess limitations when it comes to evaluating the risk of CRC, as they are unable to accurately reflect the characteristics of fat distribution (7, 8). Furthermore, the precision of BMI in gauging obesity has been cast in doubt on account of its inbuilt limitations (9). A body shape index (ABSI) was developed by Krakauer and his fellow researchers in 2012. With waist circumference (WC) being its basis, it is adjusted corresponding to height and weight. Under certain height and weight circumstances, if the ABSI is raised, it is more prone to suggest a larger portion of visceral (abdominal) fat rather than peripheral tissue (10). The index has demonstrated superior efficacy in predicting the health consequences of obesity, as elevations in the ABSI correlate with substantial increases in mortality, underscoring the insufficiency of standard obesity indicators in assessing health hazards (11). The ABSI effectively addresses some constraints inherent in relying solely on overall or central obesity markers, hence facilitating the investigation of relationships with cancer risk (12). Nonetheless, to date, only a restricted number of research have investigated the association between ABSI and the risk of CRC.
Therefore, this study sought to elucidate the relationship between ABSI and the incidence of CRC utilizing individual data from the National Health and Nutrition Examination Survey (NHANES) database. The objective was to investigate this correlation and formulate efficient preventative and screening measures for the incidence of CRC.
Materials and methods
Data sources
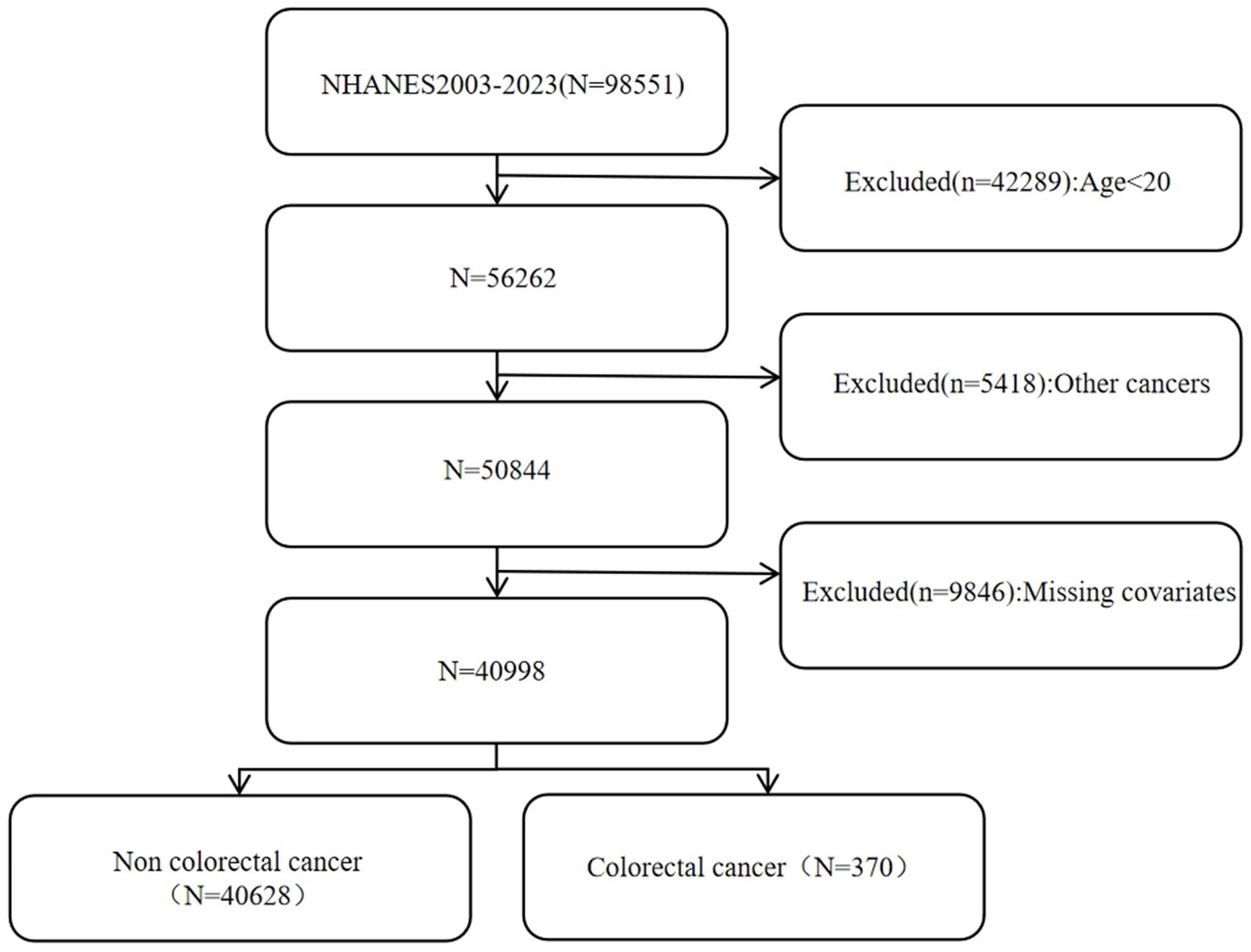
The NHANES is an ongoing cross-sectional survey that represents the nation as a whole. It employs a stratified, multistage random sampling approach and is conducted by the National Center for Health Statistics within the United States. Additionally, every participant has furnished written informed consent. All of the data can be conveniently retrieved from the NHANES website. This study analyzed 98,551 people from 2003 to 2023, removing individuals under 20 years of age, those with additional malignancies, and those missing critical covariate data. In total, 40,998 participants were incorporated into the study analysis according to stringent inclusion and exclusion criteria. The detailed steps of the specific inclusion process can be found in Figure 1.
Definition of ABSI and colorectal cancer
In this study, the exposure variable was the ABSI. The researchers collected basic anthropometric measurements from the participants, such as WC, height, and BMI. The formula for calculating the ABSI is ABSI = WC/(BMI⅔ × height½) (10, 13), with WC and height in meters.
Colorectal cancer was identified based on participants’ answers to the medical conditions questionnaire, “Have you ever been informed that you have cancer or a malignant tumor?” “What type of cancer was it?” Only participants who identified colon and rectal cancer were noted.
Temporal points for data collecting
Anthropometric data, including WC, height, and weight, were collected during participants’ visits to the Mobile Examination Center (MEC). These measurements were obtained at specific time points within the survey period. Information regarding colorectal cancer was collected through self-reported questionnaires. Notably, the time of cancer diagnosis was not directly correlated with the timing of the anthropometric data collection. Consequently, the study design operated under the assumption that the anthropometric data reflected the participants’ health status at the time of the survey. Any case of colorectal cancer diagnosed subsequent to the survey visit was regarded as a later-occurring event.
Covariates
This study evaluated covariates such as age, gender, ethnicity, BMI, ratio of family income to poverty (PIR), education level (≤high school, >high school), smoking, drinking status, exercise, and diabetes. Smoking: Classified as yes (smoked ≥100 cigs in life) or no based on the questionnaire. Drinking status: Divided into drinkers (affirmative to “consume 4/5 cups or more/day”) and non-drinkers. Exercise: Those doing vigorous exercise etc. for ≥10 min weekly are exercisers. Diabetes: Determined by self-report of diagnosis or blood sample with glycated Hb ≥ 6.5%. Data was collected via NHANES’ standardized questionnaires & interview protocols. The waist-to-height ratio (WHtR) was computed by taking the waist circumference, measured in centimeters, and dividing it by the height, which was also measured in the same unit of centimeters. In terms of the body roundness index (BRI), the following formula was employed to compute it: BRI = 364.2−365.5 × (1 − [wc(m)/2π]2 / [0.5 × height(m)]2)½ (14, 15).
Statistical analysis
Due to the multi-stage probability sampling in NHANES, sample weights were incorporated into the analytical procedure. At the outset, a univariate analysis was carried out to compare the individual baseline characteristics of the participants. The presentation of continuous variables was as the weighted mean ± standard deviation (SD). To evaluate the differences in average levels between groups, t-tests were used. Categorical variables, on the other hand, were expressed as actual frequencies and weighted percentages, and chi-square tests were utilized to compare their distributions among different groups. To analyze the connection between ABSI and CRC, logistic regression models were employed. The outcomes were presented as odds ratios (OR) and 95% confidence intervals (CI). Three separate models were devised: Model 1, which remained unadjusted for covariates; Model 2, which was adjusted for age, gender, and race; and Model 3, which was adjusted for all relevant elements. The same procedure was applied to look into the correlation among ABSI quartiles, considering the lowest quartile as the reference. We also used restricted cubic spline curves (RCS) to explore potential non-linear relationships. Furthermore, subgroup analyses were carried out with respect to diverse factors including age, gender, exercise, diabetes, and BMI. The aim of these subgroup analyses was to investigate the disparities and possible variations within different subgroups as well as to evaluate the interactions among them. Finally, after carrying out the adjustment for all covariates, an examination was conducted on the receiver operating characteristic (ROC) curves of the subjects. The area under the curve (AUC) of ABSI was compared with that of other factors such as the BRI, the WHtR, WC, BMI, and weight. Additionally, the AUC of ABSI was compared by categorizing the individuals based on age (≥60 and < 60). All of the statistical analyses were performed with the utilization of R (version 4.2.0) and EmpowerStats software (version 4.2). It was considered that a p value less than 0.05 signified a statistically significant difference.
Results
Baseline characterization
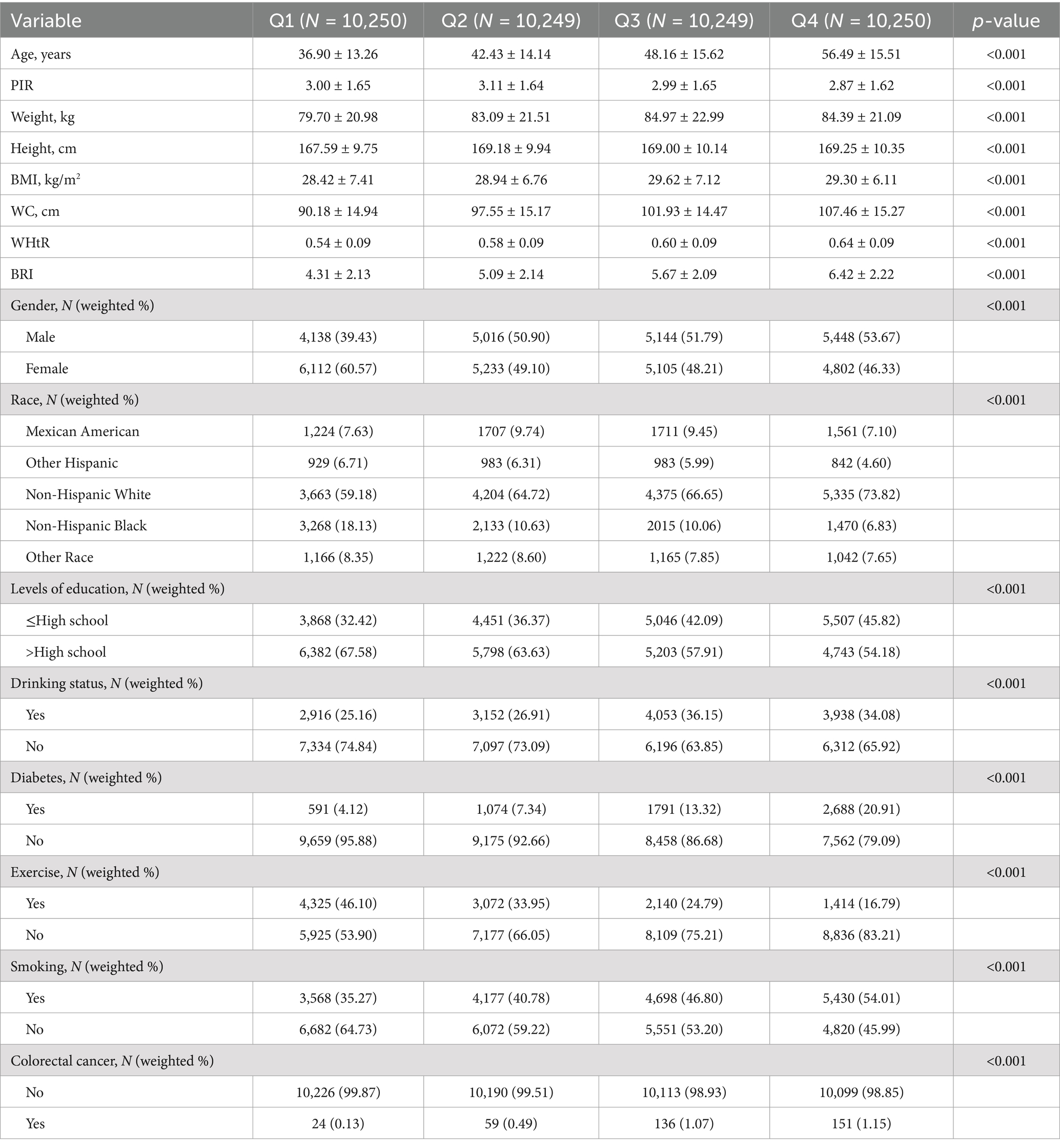
The baseline characteristics of the two groups of study participants divided according to whether they had colorectal cancer are shown in Table 1. The group without CRC had 40,628 participants, while the group with CRC included 370 participants. The mean age of the group with colorectal cancer was 67.40 ± 13.57 years. In the group free from colorectal cancer, the average ABSI was 0.081 ± 0.005, whereas in the group having colorectal cancer, it was 0.084 ± 0.004. Notable differences were observed between these two groups regarding a diverse range of factors, namely age, BMI, WC, WHtR, ABSI, BRI, ethnicity, education level, drinking habits, diabetes status, exercise frequency, and smoking status (all with p < 0.05). Table 2 is categorized based on the ABSI quartiles. The findings indicated a progressive rise in mean age from 36.90 ± 13.26 years in the Q1 group to 56.49 ± 15.51 years in the Q4 group. A substantial disparity existed among the four tertile groups regarding the presence or absence of CRC (p < 0.001). 0.13% (24) of the Q1 cohort had colorectal cancer; 0.49% (59) of the Q2 cohort had CRC; 1.07% (136) of the Q3 cohort had colorectal cancer; and 1.15% (151) of the Q4 cohort had CRC. With the rise in quartiles, there was a corresponding increase in the incidence of CRC cases. This may indicate that specific factors pertaining to the quartiles are maybe linked to the chance of acquiring CRC. Moreover, substantial disparities were seen among the ABSI quartile groups concerning other characteristics (all p < 0.001).
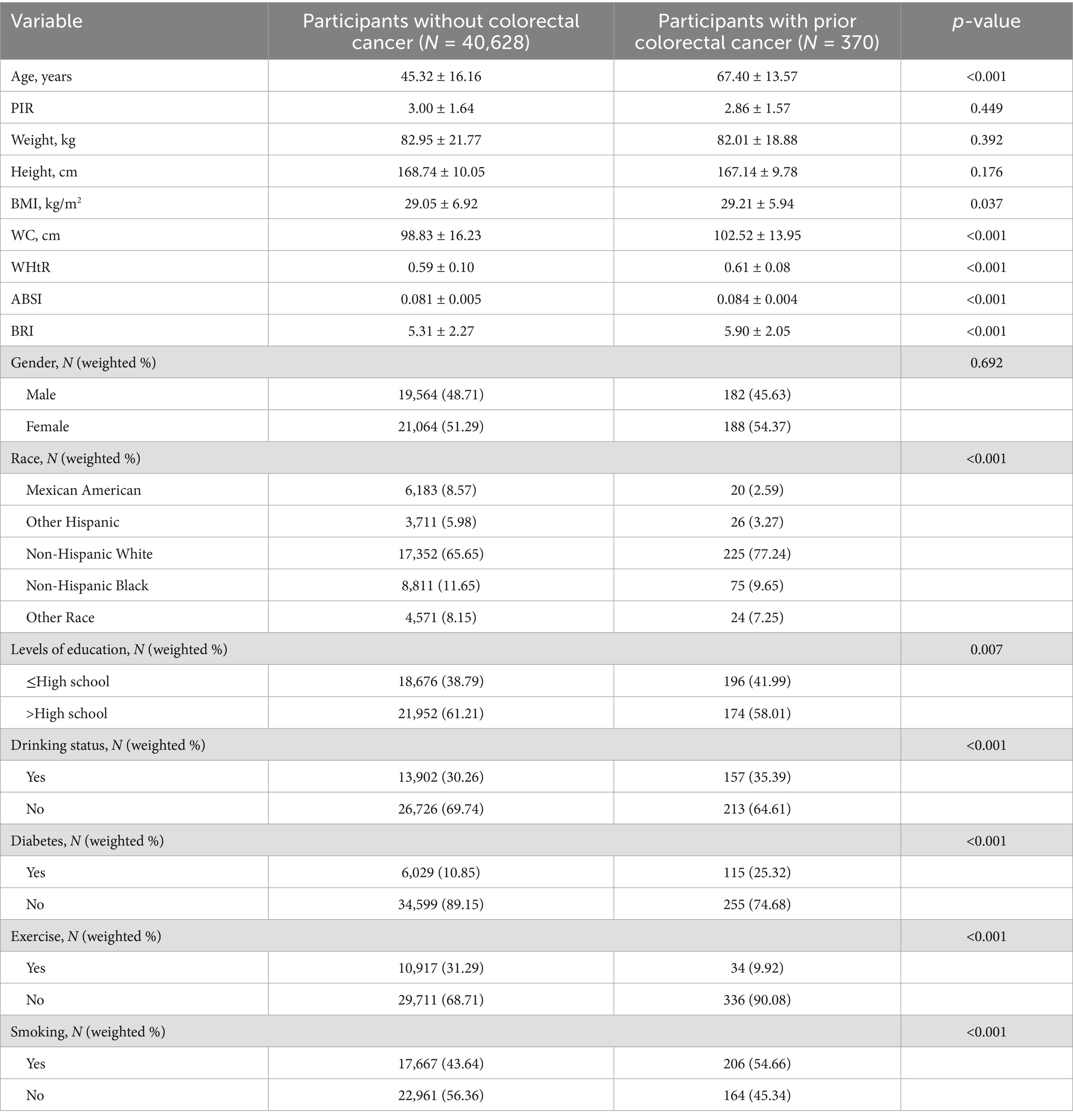
Table 1. Baseline characteristics of the study population classified according to colorectal cancer.
The relationship between ABSI and CRC
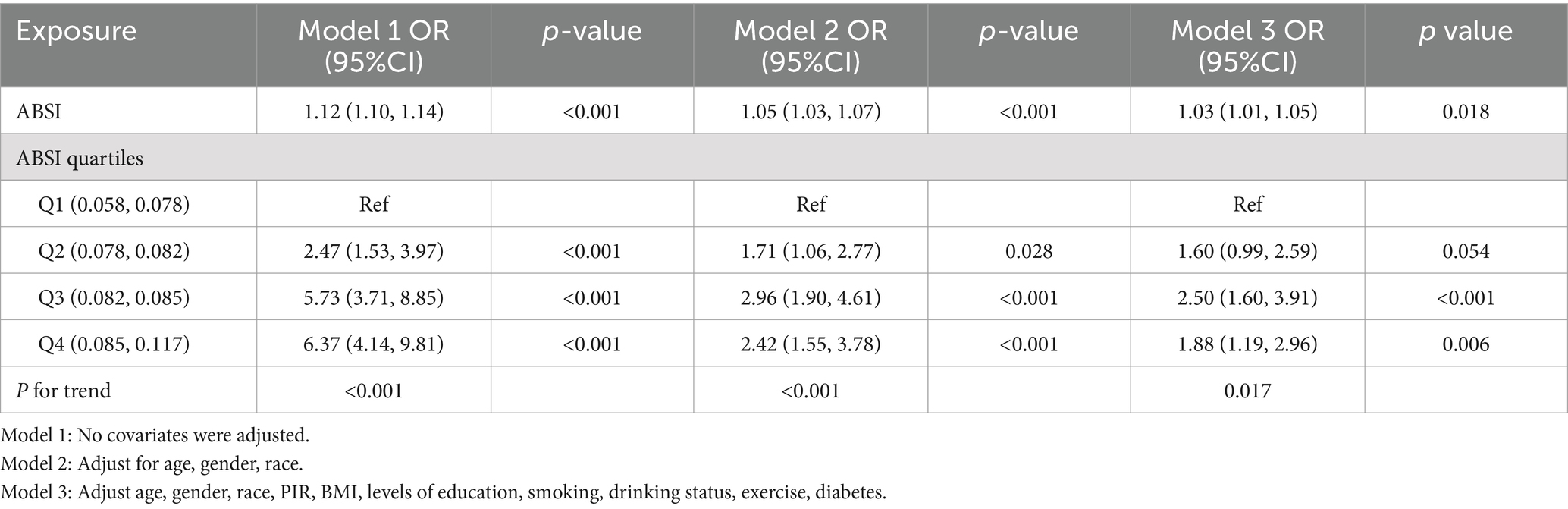
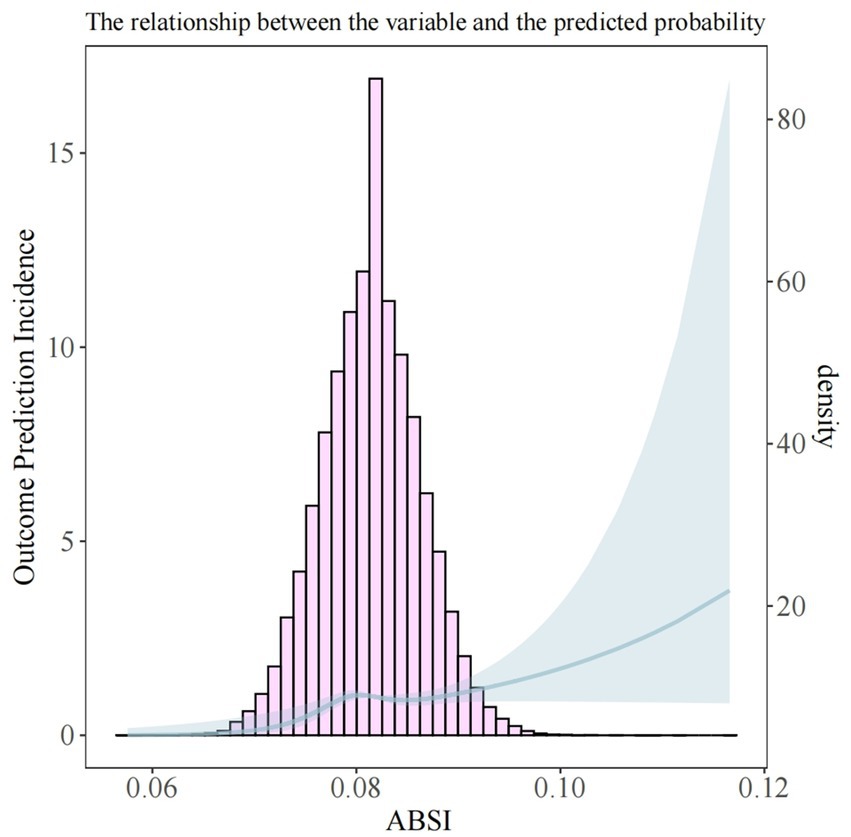
To evaluate the association between ABSI and CRC, we employed logistic regression analysis (Table 3). When ABSI was analyzed as a continuous variable without any adjustments, the OR for the association between ABSI and CRC was found to be 1.12 (95% CI: 1.10–1.14, and p < 0.001). In Model 2, after making adjustments for gender, age, and race, OR = 1.05 [95% CI: 1.03–1.07], and p < 0.001. After fully adjusting for covariables, OR = 1.03 [95% CI: 1.01–1.05], with p = 0.018. Each of the above-cited models showed a positive connection between ABSI and CRC. Furthermore, we converted ABSI into a four-category variable for the purpose of sensitivity analysis, which provided further support for this finding. In Model 3, compared to the Q1 group, the Q2 group had (OR = 1.60 [95% CI: 0.99–2.59], p = 0.054). The Q3 group had (OR = 2.50 [95% CI: 1.60–3.91], p < 0.001). And the Q4 group had (OR = 1.88 [95% CI: 1.19–2.96], p = 0.006). Trend analyses showed that all 3 models had statistical significance. In Model 1, the trend p value was <0.001. In Model 2, the trend p value was also <0.001. In Model 3, the trend p value was = 0.017. This further substantiates that when the ABSI quartiles rise, there may be a progressively increasing trend in the incidence of CRC. Furthermore, RCS analysis confirmed a significant non-linear correlation between ABSI and CRC. Figure 2 shows a significant overall trend (P for overall = 0.014) and a non-linear association (P for nonlinear = 0.030) between ABSI and CRC. When the ABSI value was approximately 0.082, the curve shifted from a relatively gentle upward trend to a steeper one. This indicates that as the ABSI value increases, the risk of CRC also rises.
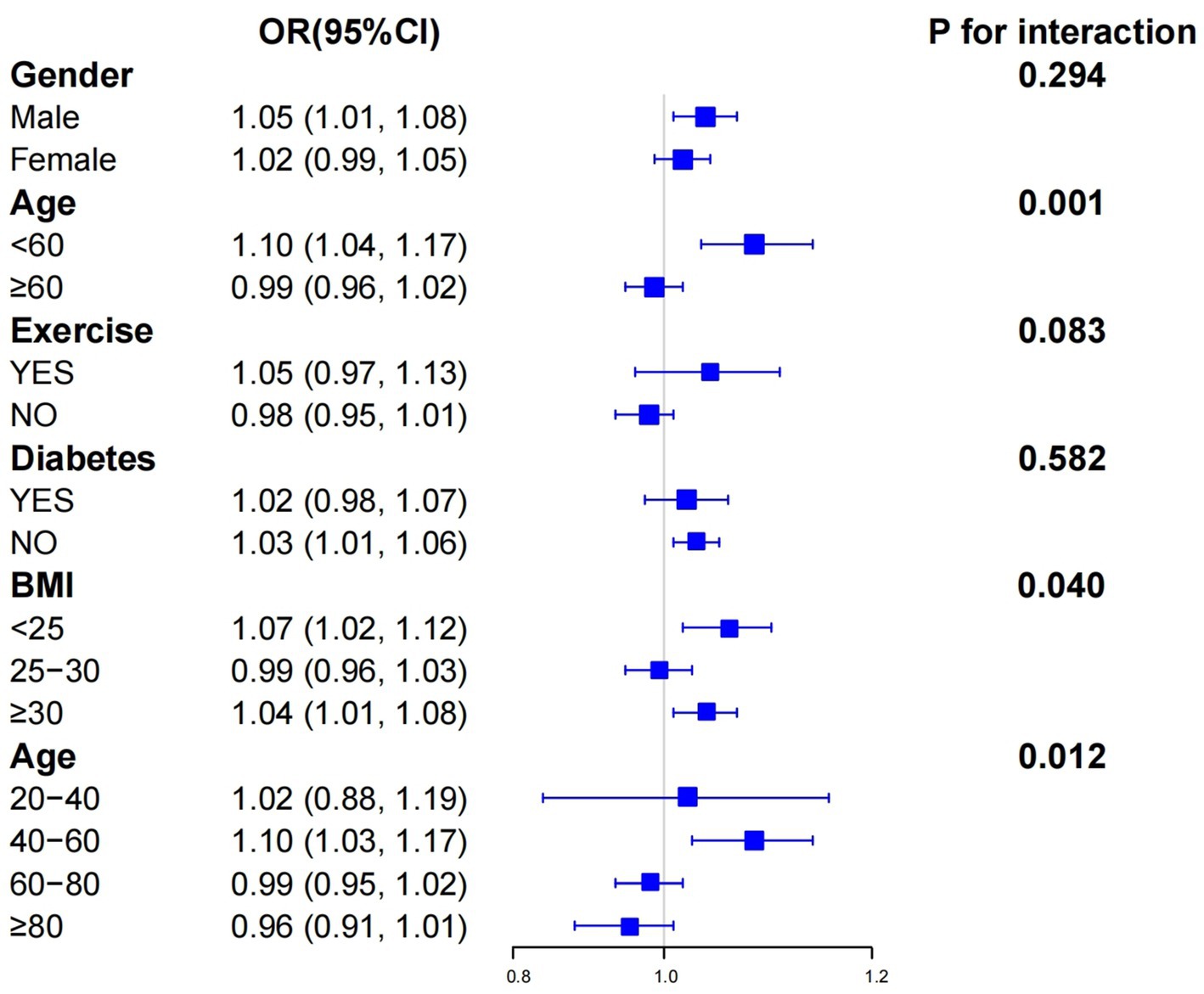
Subgroup analysis
In the subgroup analysis, we delved deeper into exploring how gender, age, exercise, diabetes, and BMI impact the relationship between ABSI and CRC, as depicted in Figure 3. A significant interaction was detected between different age subgroups and the correlation between ABSI and CRC. Specifically, for those with an age less than 60, the OR was 1.10 [with a 95% CI of 1.04–1.17]; while for those aged 60 or above, the OR was 0.99 [95% CI: 0.96–1.02], and the interaction p value was 0.001. This clearly shows that age has a substantial influence on the relationship between ABSI and CRC. To further explore the role of age, we conducted additional analyses using four age groups: 20–40 years old, 40–60 years old, 60–80 years old, and 80 years old and above. The findings indicated that the correlation between ABSI and CRC was most pronounced in the 40 to 60-year-old age demographic, exhibiting an OR of 1.10 [95% CI: 1.03–1.17] and an interaction p value of 0.012. Moreover, it is noteworthy that BMI also affects the relationship between ABSI and CRC, presenting a certain level of complexity. For individuals with a BMI less than 25, the OR was 1.07 [95% CI: 1.02–1.12]; and for those with a BMI of 30 or higher, the OR was 1.04 [95% CI: 1.01–1.08], with an interaction p value of 0.040. In contrast, no notable interactions were detected in the remaining categories since all of the interaction p values within these instances were higher than 0.05.
ROC curve analysis of ABSI vs. other anthropometric indicators
We compared the diagnostic efficacy of the ABSI with that of other anthropometric measures regarding the prevalence of CRC. The findings are shown in Figure 4. In the case of ABSI, the optimal cut-off value was determined to be 0.082, accompanied by a specificity of 0.5267 and a sensitivity of 0.7649. Additionally, it can be seen from Figure 4 that the performance of ABSI outperformed that of BRI, WHtR, WC, BMI, and Weight (AUC = 0.658). We further classified the subjects based on their age. For those who were younger than 60 years old, the value of 0.0801 was established as the optimal cut-off value of the ABSI. At this cut-off, the specificity was 0.4746 and the sensitivity was 0.7869. In the case of individuals who were 60 years old or older, the value of 0.0822 was established as the optimal cut-off value of the ABSI. Here, the specificity was 0.6684 and the sensitivity was 0.4369. The AUC of ABSI for those younger than 60 years old (AUC = 0.647) was significantly higher than that for those aged 60 years or older (AUC = 0.502), as depicted in Figure 4. The performance of various anthropometric indicators in predicting colorectal cancer differs. On the whole, ABSI holds certain value in predicting colorectal cancer, particularly demonstrating a relatively high sensitivity among individuals younger than 60 years old. Meanwhile, other indicators such as BRI, WHtR, WC, BMI, and Weight also possess some predictive capabilities for colorectal cancer to varying degrees (with AUC > 0.5).
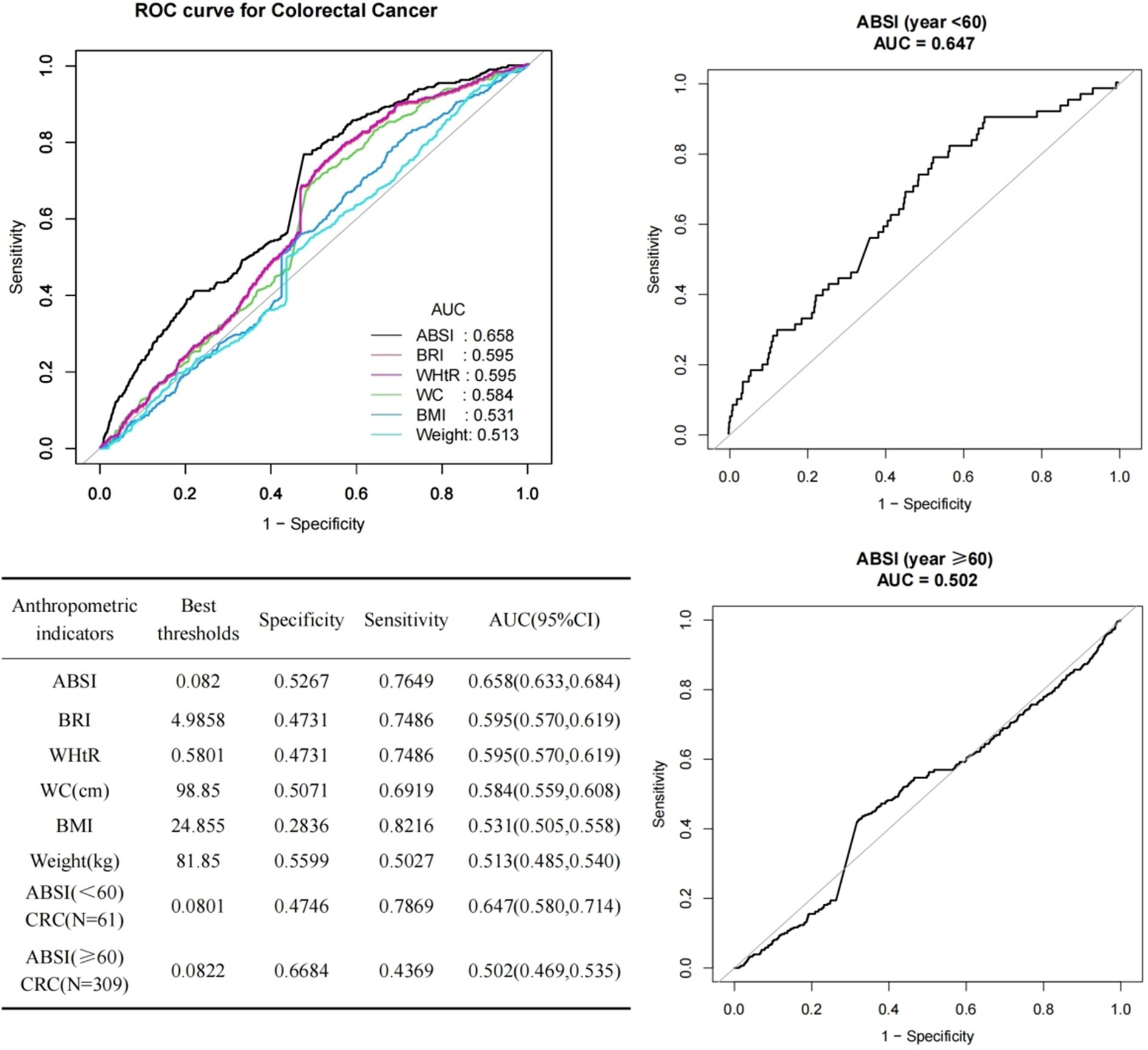
Figure 4. ROC curves for ABSI prediction of CRC with multiple anthropometric indices and age stratification.
Discussion
This study represents the first investigation to comprehensively analyze the relationship between ABSI and CRC in a broad population across the United States, leveraging the NHANES dataset. We additionally included and examined the most recent NHANES data from 2003 to 2023. The results indicated that ABSI is positively correlated with an increased incidence of CRC. This correlation remained significant even after taking all variables into account. In the subgroup analyses carried out according to age and BMI, a significant interaction between the ABSI and CRC was detected. In ROC analysis, we discovered that the association of ABSI with CRC exceeded that of other obesity indices, indicating that ABSI may be more precise than other obesity-related metrics in predicting CRC. The data revealed that the predictive capacity and accuracy of the ABSI for CRC were higher in individuals under 60 years of age than in those who were 60 years old or older. These findings suggest directions for further research and propose that, in clinical practice, ABSI should be considered as an auxiliary tool for risk assessment, especially for specific population subgroups such as those aged less than 60 years, and those with varying BMI categories. This would enable the formulation of more targeted preventive interventions.
Among the various factors associated with cancer development, visceral obesity is more likely to be a key carcinogenic factor than overall fat (16). Research has indicated that visceral obesity is a prevalent disease that is typically accompanied by low adiponectin levels. Moreover, it is a firmly recognized risk factor for CRC (17). This is because visceral obesity triggers a series of complex pathophysiological changes that further increase the risk of cancer (18–20). For instance, several pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) are secreted by visceral adipose tissue (5). These cytokines keep the immune system activated continuously, thereby leading to a state of chronic inflammation. Prolonged chronic inflammation can result in recurrent damage and repair of the colorectal mucosal epithelial cells, heightening the probability of genetic alterations and hence facilitating the onset and progression of colorectal cancer (21, 22). Furthermore, adipose tissue, especially the visceral fat within it, can cause the levels of insulin and insulin-like growth factor-I (IGF-I) in the serum to go up. It can also prompt the release of leptin and adiponectin. These alterations significantly contribute to the etiology of cancer (23). Computed tomography (CT) and magnetic resonance imaging (MRI) are commonly used to measure the distribution of visceral fat. Nevertheless, these techniques are expensive, take a lot of time, and are not appropriate for large-scale epidemiologic studies (24). Consequently, a straightforward clinical anthropometric index, the ABSI, is suggested for assessing visceral fat. The ABSI is founded on the notion of anisotropic growth in calculating BMI and has successfully developed BMI-independent alternatives to waist indices (10). From a statistical perspective, the ABSI has no dependence on height, BMI, and WC, and more accurately represents visceral adiposity than conventional anthropometric measures. Anthropometric measurements more accurately represent visceral obesity compared to conventional anthropometric assessments (25). In contrast to other novel anthropometric measures like the BRI, the ABSI has something to do with increased cancer risk in numerous spots (26), whereas the BRI has infrequently been connected with cancer (15). This suggests that the ABSI is more centered on measuring visceral fat, which is highly relevant to the incidence of cancer.
In recent years, the ABSI has gained increasing recognition for measuring visceral fat accumulation and its impact (27, 28). Studies have also demonstrated a positive relation between ABSI and the risk of neurological diseases (13), cardiovascular diseases (7), and all-cause mortality (29). Moreover, an increasing amount of research is exploring the connection between the ABSI and cancer risk. Studies regarding the UK Biobank cohort have shown that ABSI is markedly linked to a greater risk of five particular malignancies, among which are lung cancer and CRC, and the overall risk of developing cancer as well (26). A cohort research from the Guangzhou Biobank in China, with a 14-year follow-up, manifested a positive linkage between ABSI and an augmented risk of CRC (30). An analysis that combined and involved collaboration of 11 Australian cohorts showed that ABSI correlates with total cancer and CRC in both genders, but not with prostate cancer (31). Nevertheless, research on the American NHANES database finds that higher ABSI levels are closely linked to prostate cancer risk and its related death rates (25, 32). This indicates that ABSI may be subject to certain limitations when directly applied to populations with different ethical backgrounds, and the current evidence regarding the relationship of ABSI to CRC remains comparatively limited. Consequently, we undertook a comprehensive examination of the relationship between ABSI and CRC within the American populace. Our study results show that ABSI has a positive relation with a higher risk of CRC, particularly in specific demographics where this association is more significant. Furthermore, to explore the relationship between ABSI and CRC more comprehensively, we conducted an in-depth analysis and comparison of relevant studies. A study based on NHANES data from 1999 to 2018 investigated the association between ABSI and the risk of CRC among patients with metabolic syndrome. It was found that, in this patient group, a higher ABSI was significantly associated with an increased risk of developing CRC (33). In contrast, our study, based on a broader population in the United States, has further expanded the scope of research on the relationship between ABSI and CRC. Although the research subjects differ, both studies highlight the importance of ABSI in assessing the risk of CRC. Moreover, the results of our study, to some extent, corroborate those of the previous study, indicating that ABSI may be an important predictor of CRC, not restricted by the single factor of metabolic syndrome. Christakoudi et al. revealed the association between body shape phenotypes and imaging-based body composition measurements, as well as their relationship with colon cancer (34). Their research demonstrated that body shape phenotypes defined by ABSI and hip index (HI) were closely related to body composition and could reflect differences therein, such as variations in the distribution of visceral adipose tissue (VAT) and abdominal subcutaneous adipose tissue (ASAT). These differences were associated with the risk of colon cancer. Our study also detected an association between ABSI and CRC, further supporting the crucial role of body composition, especially abdominal fat distribution, in the pathogenesis of CRC. Rontogianni et al. provided new evidence for the causal relationship between body shape indices and the risk of CRC through a Mendelian randomization study (35). They discovered a potential positive causal correlation between the allometric index ABSI, waist-hip index (WHI), and CRC, which was independent of traditional waist-circumference indices and BMI. The results of our study echo theirs, further strengthening the reliability of ABSI as a risk predictor for CRC. Simultaneously, this also provides a direction for more in-depth research on causal mechanisms in the future.
In this study, we also found that the association between ABSI and CRC risk was more pronounced, especially in the subgroup of individuals under 60 years old (40–60 years old). The subgroup analysis accurately pinpointed the age range of 40–60 years old, where the association was significant, revealing the close connection between ABSI and CRC risk in this age group. In addition, the ROC analysis, as a supplementary tool for exploring the overall age-related trends in this study, showed that ABSI had a certain value in predicting CRC risk, especially in the population under 60 years old, where it exhibited high sensitivity. The results of these two analyses are closely related and refer to each other. From a more macroscopic perspective, that is, the grouping of ages ≥60 years old and < 60 years old, the ROC analysis helps us to grasp the overall trend of the predictive ability of ABSI with age, further confirming the findings of the subgroup analysis and emphasizing the importance of age as a modifying factor when considering the relationship between ABSI and CRC risk. This finding is consistent with what Krakauer et al. pointed out regarding the high correlation between ABSI and age, and is in line with previous research results, indicating that within this age range, ABSI might be an effective risk predictor (33). Specifically, the higher metabolic rate in younger people may amplify the impact of abdominal fat distribution on subsequent health outcomes (36). Additionally, unhealthy lifestyle behaviors, such as sedentary habits and poor dietary choices, are more prevalent among middle-aged individuals (37). This may further exacerbate the association between ABSI and the risk of CRC. As people age, the clinical manifestations of elderly patients tend to be more complex, often accompanied by multiple comorbidities. In this age group, the influence of ABSI still exists, but it may be masked by other factors, such as genetic factors and past medical history. Elderly patients may experience vague symptoms such as weight loss and decreased appetite, which are often attributed to aging rather than cancer (30). This thus influences the correlation between ABSI and CRC. These combined factors can explain the differences in the strength of the association between ABSI and CRC observed in different age subgroups.
To date, no study has explored the correlation between ABSI and the risk of CRC in the general population of the United States. The large sample size is another advantage of this study. However, we cannot overlook the limitations of the research. This study was conducted based on the cross-sectional survey data of NHANES. This approach may introduce temporal bias in the reference time points between anthropometric measurements and CRC. The relationship between anthropometric data and the risk of CRC may change over time, and the cross-sectional design restricts the ability to clarify causal relationships. Thus, it is impossible to rule out the possibility of reverse causation or bidirectional causation. Secondly, even after adjusting for some potential confounding variables in the statistical analysis, there may still be undetected confounding factors, which could affect the accuracy of the results. Finally, NHANES did not collect imaging and pathological data from its participants. Therefore, relying on self-reported CRC data may introduce information bias. Especially among the elderly population, due to memory decline, insufficient disease awareness, or limited access to medical care, they may not accurately report their CRC status, leading to an underestimation of the number of CRC cases and thus affecting the accuracy of the research results. Future research should adopt more objective cancer diagnosis methods, such as integrating clinical examination data and medical records, to reduce the bias caused by self-reporting. Meanwhile, more detailed survey plans can be designed for different age groups to improve the accuracy of the data.
Conclusion
This study finds that a bigger ABSI is tied to a higher CRC risk, especially for people under 60 years of age (40–60 years) and those with different BMI types. Compared to traditional anthropometric measurements, ABSI has a unique value in predicting CRC. Notably, it shows enhanced sensitivity in those aged less than 60 years. Future studies should the precise mechanisms of ABSI and CRC to formulate novel strategies for decreasing incidence rates. Furthermore, public health education must be enhanced to promote food regulation, consistent physical activity to diminish visceral fat buildup, and the endorsement of healthy lifestyles to mitigate the risk of CRC.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: http://www.cdc.gov/nchs/nhanes.htm.
Ethics statement
The studies involving humans were approved by NCHS Ethics Review Board (ERB) Approval. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HL: Conceptualization, Data curation, Formal analysis, Writing – original draft. JK: Data curation, Validation, Writing – review & editing. WL: Funding acquisition, Project administration, Supervision, Writing – review & editing. YS: Investigation, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Humanities and Social Sciences Research Planning Fund Project of the Ministry of Education in 2018 (18YJAZH074); the Teaching Reform Research Project of Postgraduate Education in 2024 (XYJG2024003); and the Project of Provincial Colleges and Universities’ Basic Scientific Research Operating Expenses Project in 2024 (TDSK2024001).
Acknowledgments
All authors thank the staff involved in the establishment and maintenance of the NHANES database. Additionally, the authors would like to express their gratitude to the Hebei Key Laboratory of Health Care with Traditional Chinese Medicine for their support and contributions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bray, F, Laversanne, M, Sung, H, Ferlay, J, Siegel, RL, Soerjomataram, I, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2024) 74:229–63. doi: 10.3322/caac.21834
2. Lui, RN, Tsoi, KKF, Ho, JMW, Lo, CM, Chan, FCH, Kyaw, MH, et al. Global increasing incidence of young-onset colorectal Cancer across 5 continents: a Joinpoint regression analysis of 1, 922, 167 cases. Cancer Epidemiol Biomarkers Prev. (2019) 28:1275–82. doi: 10.1158/1055-9965.EPI-18-1111
3. Siegel, RL, Fedewa, SA, Anderson, WF, Miller, KD, Ma, J, Rosenberg, PS, et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst. (2017) 109:27–32. doi: 10.1093/jnci/djw322
4. De Wit, DF, Hanssen, NMJ, Wortelboer, K, Herrema, H, Rampanelli, E, and Nieuwdorp, M. Evidence for the contribution of the gut microbiome to obesity and its reversal. Sci Transl Med. (2023) 15:eadg2773. doi: 10.1126/scitranslmed.adg2773
5. Tilg, H, and Moschen, AR. Mechanisms behind the link between obesity and gastrointestinal cancers. Best Pract Res Clin Gastroenterol. (2014) 28:599–610. doi: 10.1016/j.bpg.2014.07.006
6. Chaplin, A, Rodriguez, RM, Segura-Sampedro, JJ, Ochogavía-Seguí, A, Romaguera, D, and Barceló-Coblijn, G. Insights behind the relationship between colorectal Cancer and obesity: is visceral adipose tissue the missing link? Int J Mol Sci. (2022) 23:13128. doi: 10.3390/ijms232113128
7. Calderón-García, JF, Roncero-Martín, R, Rico-Martín, S, De Nicolás-Jiménez, JM, López-Espuela, F, Santano-Mogena, E, et al. Effectiveness of body roundness index (BRI) and a body shape index (ABSI) in predicting hypertension: a systematic review and Meta-analysis of observational studies. Int J Environ Res Public Health. (2021) 18:11607. doi: 10.3390/ijerph182111607
8. Moltrer, M, Pala, L, Cosentino, C, Mannucci, E, Rotella, CM, and Cresci, B. Body mass index (BMI), waist circumference (WC), waist-to-height ratio (WHtR) e waist body mass index (wBMI): which is better? Endocrine. (2022) 76:578–83. doi: 10.1007/s12020-022-03030-x
9. Donini, LM, Pinto, A, Giusti, AM, Lenzi, A, and Poggiogalle, E. Obesity or BMI paradox? Beneath the tip of the iceberg. Front Nutr. (2020) 7:53. doi: 10.3389/fnut.2020.00053
10. Krakauer, NY, and Krakauer, JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One. (2012) 7:e39504. doi: 10.1371/journal.pone.0039504
11. Sardarinia, M, Ansari, R, Azizi, F, Hadaegh, F, and Bozorgmanesh, M. Mortality prediction of a body shape index versus traditional anthropometric measures in an Iranian population: Tehran lipid and glucose study. Nutrition. (2017) 33:105–112. doi: 10.1016/j.nut.2016.05.004
12. Christakoudi, S, Tsilidis, KK, Muller, DC, Freisling, H, Weiderpass, E, Overvad, K, et al. A body shape index (ABSI) achieves better mortality risk stratification than alternative indices of abdominal obesity: results from a large European cohort. Sci Rep. (2020) 10:14541. doi: 10.1038/s41598-020-71302-5
13. Huang, W, Xiao, Y, Zhang, L, and Liu, H. Association between a body shape index and Parkinson's disease: a large cross-sectional study from NHANES. Heliyon. (2024) 10:e26557. doi: 10.1016/j.heliyon.2024.e26557
14. Thomas, DM, Bredlau, C, Bosy-Westphal, A, Mueller, M, Shen, W, Gallagher, D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity (Silver Spring). (2013) 21:2264–71. doi: 10.1002/oby.20408
15. Gao, W, Jin, L, Li, D, Zhang, Y, Zhao, W, Zhao, Y, et al. The association between the body roundness index and the risk of colorectal cancer: a cross-sectional study. Lipids Health Dis. (2023) 22:53. doi: 10.1186/s12944-023-01814-2
16. Silveira, EA, Kliemann, N, Noll, M, Sarrafzadegan, N, and de Oliveira, C. Visceral obesity and incident cancer and cardiovascular disease: an integrative review of the epidemiological evidence. Obes Rev. (2021) 22:e13088. doi: 10.1111/obr.13088
17. Cust, AE, Stocks, T, Lukanova, A, Lundin, E, Hallmans, G, Kaaks, R, et al. The influence of overweight and insulin resistance on breast cancer risk and tumour stage at diagnosis: a prospective study. Breast Cancer Res Treat. (2009) 113:567–76. doi: 10.1007/s10549-008-9958-8
18. Avgerinos, KI, Spyrou, N, Mantzoros, CS, and Dalamaga, M. Obesity and cancer risk: emerging biological mechanisms and perspectives. Metabolism. (2019) 92:121–35. doi: 10.1016/j.metabol.2018.11.001
19. Murphy, N, Jenab, M, and Gunter, MJ. Adiposity and gastrointestinal cancers: epidemiology, mechanisms and future directions. Nat Rev Gastroenterol Hepatol. (2018) 15:659–70. doi: 10.1038/s41575-018-0038-1
20. Deng, T, Lyon, CJ, Bergin, S, Caligiuri, MA, and Hsueh, WA. Obesity, inflammation, and Cancer. Annu Rev Pathol. (2016) 11:421–49. doi: 10.1146/annurev-pathol-012615-044359
21. Tarasiuk, A, Mosińska, P, and Fichna, J. The mechanisms linking obesity to colon cancer: an overview. Obes Res Clin Pract. (2018) 12:251–9. doi: 10.1016/j.orcp.2018.01.005
22. Iyengar, NM, Gucalp, A, Dannenberg, AJ, and Hudis, CA. Obesity and Cancer mechanisms: tumor microenvironment and inflammation. J Clin Oncol. (2016) 34:4270–6. doi: 10.1200/JCO.2016.67.4283
23. Donohoe, CL, Doyle, SL, and Reynolds, JV. Visceral adiposity, insulin resistance and cancer risk. Diabetol Metab Syndr. (2011) 3:12. doi: 10.1186/1758-5996-3-12
24. Kuriyan, R. Body composition techniques. Indian J Med Res. (2018) 148:648–58. doi: 10.4103/ijmr.IJMR_1777_18
25. Liu, X, Shi, H, Shi, Y, Wei, H, Yuan, X, Jiao, Z, et al. Association between a body shape index and prostate cancer: a cross-sectional study of NHANES 2001-2018. Int Urol Nephrol. (2024) 56:1869–77. doi: 10.1007/s11255-023-03917-2
26. Parra-Soto, S, Malcomson, FC, Ho, FK, Pell, JP, Sharp, L, Mathers, JC, et al. Associations of a body shape index (ABSI) with Cancer incidence, all-cause, and at 23 sites-findings from the UK biobank prospective cohort study. Cancer Epidemiol Biomarkers Prev. (2022) 31:315–24. doi: 10.1158/1055-9965.EPI-21-0591
27. Nagayama, D, Watanabe, Y, Yamaguchi, T, Maruyama, M, Saiki, A, Shirai, K, et al. New index of abdominal obesity, a body shape index, is BMI-independently associated with systemic arterial stiffness in real-world Japanese population. Int J Clin Pharmacol Ther. (2020) 58:709–17. doi: 10.5414/CP203778
28. Anoop, S, Krakauer, J, Krakauer, N, and Misra, A. A body shape index significantly predicts MRI-defined abdominal adipose tissue depots in non-obese Asian Indians with type 2 diabetes mellitus. BMJ Open Diabetes Res Care. (2020) 8:e001324. doi: 10.1136/bmjdrc-2020-001324
29. Kazemian, E, Mehran, L, Masoumi, S, Amouzegar, A, and Azizi, F. Association of trajectory of body shape index with all-cause and cause-specific mortality: 18 years follow-up. Front Endocrinol (Lausanne). (2023) 14:1259849. doi: 10.3389/fendo.2023.1259849
30. Wang, SY, Zhang, WS, Jiang, CQ, Jin, YL, Zhu, T, Zhu, F, et al. Association of novel and conventional obesity indices with colorectal cancer risk in older Chinese: a 14-year follow-up of the Guangzhou biobank cohort study. BMC Cancer. (2023) 23:286. doi: 10.1186/s12885-023-10762-0
31. Harding, JL, Shaw, JE, Anstey, KJ, Adams, R, Balkau, B, Brennan-Olsen, SL, et al. Comparison of anthropometric measures as predictors of cancer incidence: a pooled collaborative analysis of 11 Australian cohorts. Int J Cancer. (2015) 137:1699–708. doi: 10.1002/ijc.29529
32. Ku, HC, Cheng, E, and Cheng, CF. A body shape index (ABSI) but not body mass index (BMI) is associated with prostate cancer-specific mortality: evidence from the US NHANES database. Prostate. (2024) 84:797–806. doi: 10.1002/pros.24698
33. Kurexi, A, Peng, J, Yao, J, Wang, L, and Wang, Q. Association of "a body shape index" with the risk of developing colorectal cancer in U.S. patients with metabolic syndrome: evidence from the NHANES 1999–2018. BMC Gastroenterol. (2024) 24:447. doi: 10.1186/s12876-024-03537-9
34. Christakoudi, S, Tsilidis, KK, Evangelou, E, and Riboli, E. Association of body-shape phenotypes with imaging measures of body composition in the UK biobank cohort: relevance to colon cancer risk. BMC Cancer. (2021) 21:1106. doi: 10.1186/s12885-021-08820-6
35. Rontogianni, MO, Bouras, E, Aglago, EK, Freisling, H, Murphy, N, Cotterchio, M, et al. Allometric versus traditional body-shape indices and risk of colorectal cancer: a Mendelian randomization analysis. Int J Obes. (2024) 48:709–16. doi: 10.1038/s41366-024-01479-6
36. Marketou, ME, Buechler, NS, Fragkiadakis, K, Plevritaki, A, Zervakis, S, Maragkoudakis, S, et al. Visceral fat and cardiometabolic future in children and adolescents: a critical update. Pediatr Res. (2023) 94:1639–47. doi: 10.1038/s41390-023-02709-9
37. Ortiz, C, López-Cuadrado, T, Rodríguez-Blázquez, C, Pastor-Barriuso, R, and Galán, I. Clustering of unhealthy lifestyle behaviors, self-rated health and disability. Prev Med. (2022) 155:106911. doi: 10.1016/j.ypmed.2021.106911
Glossary
ABSI - A body shape index
CRC - Colorectal cancer
NHANES - National Health and Nutrition Examination Survey
BMI - Body mass index
WC - Waist circumference
OR - Odds ratio
CI - Confidence interval
ROC - Receiver operating characteristic
PIR - Ratio of family income to poverty
WHtR - Waist-to-height ratio
BRI - Body roundness index
TNF-α - Tumor necrosis factor-alpha
IL-6 - Interleukin-6
GF-I - Insulin-like growth factor-I
CT - Computed tomography
MRI - Magnetic resonance imaging
RCS - Restricted cubic spline
ASAT - Abdominal subcutaneous adipose tissue
VAT - Visceral adipose tissue
HI - Hip index
WHI - Waist-hip index
Keywords: ABSI, colorectal cancer, visceral fat, obesity, NHANES
Citation: Liu H, Kang J, Liu W and Shen Y (2025) Association between a body shape index and colorectal cancer in US population: a cross-sectional study based on NHANES. Front. Nutr. 12:1535655. doi: 10.3389/fnut.2025.1535655
Edited by:
José María Huerta, Carlos III Health Institute (ISCIII), SpainReviewed by:
Alessandro De Oliveira, Universidade Federal de São João del-Rei, BrazilAntonio José Molina De La Torre, University of León, Spain
Copyright © 2025 Liu, Kang, Liu and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Liu, MjczODYwNjkwbGl1d2VpQHNpbmEuY29t
 Hui Liu1
Hui Liu1 Wei Liu
Wei Liu