- 1Department of Internal Medicine, University of Maryland Capital Region Medical Center, Largo, MD, United States
- 2Bay Medical Centre, Castries, Saint Lucia
- 3Department of Internal Medicine, Indiana University School of Medicine, Fort Wayne, IN, United States
- 4Department of Internal Medicine, University of Miami at Holy Cross Hospital, Fort Lauderdale, FL, United States
- 5Department of Internal Medicine, University of the West Indies, Mona Campus, Kingston, Jamaica
- 6Department of Internal Medicine, University of the West Indies, St. Augustine Campus, St. Augustine
- 7Department of Internal Medicine, Eric Williams Medical Center, St. Augustine, Trinidad
- 8Bahamas Health and Healing Medical Center, Nassau, The Bahamas
- 9Comprehensive Orthopaedic global, St. Thomas, US Virgin Islands
- 10Department of Internal Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, United States
- 11Department of Internal Medicine, NEA Baptist Memorial Hospital, Jonesboro, AR, United States
Introduction: Systemic lupus erythematosus (SLE) is highly prevalent in the Caribbean, with limited access to specialist care. Primary care providers (PCPs) must play a key role in SLE management but lack specific knowledge on high-impact diagnostic and management strategies for the Caribbean SLE patient. The Caribbean Association for Rheumatology (CAR) supports PCPs with educational material tailored to the Caribbean but is limited by poor regional data on SLE educational needs. The aim of this project was to achieve consensus amongst CAR members on SLE educational priorities for PCPs based on individual experience.
Methods: The nominal group technique was used to achieve consensus. Participants were asked to generate, record, discuss and rank ideas, which were organized by emergent categories. Each participant assigned a score to their top ideas, generating a group-level score for each topic. A threshold of at least 70% agreement was set for consensus. Narrative comments from the discussion and ranking survey provided context for the consensus topics.
Results: 13 providers (9 rheumatologists and 4 internists), mostly female (92%), mean age 42.4 (8.2) years, participated. There was consensus on 15 topics which emphasized early diagnosis, early rheumatology referral and reproductive health. Of the top-ranked topics, there was a trend towards a primary care focus amongst internists.
Conclusion: Priority topics for PCP education focused on early diagnosis, early referral and reproductive health in SLE. Non-rheumatologists prioritized primary care interventions reflecting a misalignment in the perception of the Caribbean PCP's role in SLE, reinforcing the need for a focused educational program.
Introduction
Systemic Lupus Erythematosus is a systemic autoimmune disease with multiorgan involvement that primarily affects women of childbearing age. Significant disease burden and higher mortality have been described in persons of African ancestry (1, 2), which characterizes a large section of the Caribbean population, who experience more severe SLE disease, earlier onset and worse outcomes. In the Caribbean context, the lupus experience is exacerbated by high levels of poverty, nonadherence, cultural factors, and poor access to specialist care. Data from The Barbados Lupus and Rheumatology Registry (BLR), which can be extrapolated to other Caribbean countries due to similar populations, indicated higher incidence and prevalence of SLE (3) compared to other regionss (4, 5). While Caribbean SLE patients present most often with systemic symptoms, cutaneous manifestations and polyarthritis, they also have high morbidity and mortality rates with more severe renal disease, high infection rates and adverse pregnancy outcomes (6–10).
The Caribbean healthcare landscape is challenged by a lack of rheumatology specialists, compounded by variable and restricted access to disease-modifying therapies. Most countries have government-funded healthcare systems that provide primary, secondary, and tertiary care services. Though these systems offer universal access to healthcare, the quality and availability of services varies widely, and those who can afford private insurance or out of pocket payments may opt to be seen by private healthcare providers. Given that most Caribbean nations have fewer than two rheumatologists to serve the entire population of each island, these specialists, like other secondary healthcare providers, often work in both the public and private health sectors, assuming a significant workload. There have been no formal studies of the rheumatology workforce in the Caribbean, which has an estimated population of over 44 million (11). However, real-world data indicates that the current provider-to-population ratio is significantly below the optimal 2 providers per 100,000 persons (12), dropping to as low as 0.12 in some island nations, such as Trinidad and Tobago. Unfortunately, many Caribbean islands lack a rheumatologist, forcing patients to travel to neighboring islands for care, which adds further strain to an already burdened healthcare system. This translates into delayed diagnosis, inadequate treatment, and poor clinical outcomes in SLE. As such, primary care providers (PCPs) who serve as a crucial link to secondary and tertiary care, play an essential role in the early recognition and management of SLE.
Regional healthcare institutions have a major role in the education of PCPs, and rheumatic disease is included in medical school curricula, however, the primary focus of postgraduate and continuing medical education in primary care has been on reducing heart disease, cerebrovascular disease, cancer and diabetes, which accounts for almost 2/3 of all deaths in the Caribbean region (13). Caribbean public health policies target obesity, hypertension and diabetes as major causes of poor health outcomes. However, this has neglected the devastating effects of undiagnosed and undertreated inflammatory diseases, such as SLE.
The Caribbean Association for Rheumatology (CAR), founded by a pioneering team of Caribbean rheumatologists in 2007, is a medical professional organization committed to the advancement of rheumatology and improving health outcomes of Caribbean patients with rheumatic disease. CAR members comprise both rheumatologists and internists, with varied levels of experience. CAR has made a dedicated effort to educate both patients and PCPs to facilitate early diagnosis of SLE for timely initiation of therapy and to mitigate cumulative damage, disability, loss of work productivity and high morbidity.
An annual community education event led by CAR and hosted in a different Caribbean island each year, has been well received by providers but is limited in scope due to a lack of resources. Recognizing the detrimental impact of undertreated SLE in the Caribbean population, the CAR group met to determine the best strategy for educating PCPs on SLE, and the high impact topics of interest for inclusion in the annual education program. The goal of this project was to determine which topics should be prioritized in the educational forum for the greatest impact on SLE diagnosis and management within the unique context of the multicultural Caribbean region. Given the paucity of region-specific data, a nominal group technique was used to build consensus around priority topics for SLE education based on participant experience.
Methods
The nominal group technique (NGT) is a structured method for group brainstorming and decision making that allows a group of experts to anonymously submit ideas and solutions for discussion by the group at large (14). NGT has been used in healthcare and education to build consensus amongst experts. The strengths of this method include the generation of many ideas, equal participation by members and a democratic decision-making process. It is conducted in 4 phases—Phase I. Silent generation of ideas, Phase II. Recording of ideas, Phase III. Discussion and Phase IV. Voting and ranking. Numerical voting and ranking allow for the establishment of a prioritized list of ideas (14, 15).
Members of the expert panel were all members of CAR. In an executive meeting held in February 2024 to decide on a strategic plan for CAR's educational priorities for SLE in the region, it became evident that more information was needed to ensure the annual educational event is meeting the needs of the different island communities. Purposive sampling was used to select the expert panel, with a goal of having representation from each Caribbean island with an established rheumatology service. Members were emailed and invited to participate, including PCPs (who were also members of CAR) identified by the rheumatologists. In this study, PCPs are defined as healthcare professionals authorized to prescribe medications. In the Caribbean context, this group predominantly includes family medicine doctors, general practitioners and some internists.
The CAR executive committee met to discuss and refine the research focus and asked the question “When educating general practitioners and internists, what topics in SLE education would have the greatest impact on improving clinical outcomes for Caribbean patients with SLE?”. The nominal group technique, modified for an online format (16) was used to establish agreement on CAR's priorities for SLE education of PCPs in the Caribbean.
This project did not involve human subjects, and therefore, approval from Human Studies Committees was not required.
Data collection
Participants were invited to participate by email. One NGT session, modified for the online format, was implemented in the following phases:
I. Generation of Ideas—Participants were contacted by email and invited to submit responses to the question posed, with ideas stratified according to an established framework for education in SLE (17) including categories for medical knowledge, diagnosis, and management strategies (Supplementary Table S1).
II. Recording of Ideas—Submitted ideas were collated into a shared document. Participants were invited to review, edit, comment and/or add new ideas ahead of a scheduled online discussion. Responses were categorized into three emergent major themes—Diagnosis and Clinical Acumen, Management Strategies, and Management of Reproductive Health in SLE (Supplementary Table S3).
III. Discussion of Ideas—A 2.5 h virtual meeting was convened with all participants, where ideas were reviewed and clarified to ensure that participants understood the nature and intent of each idea.
IV. Voting on Ideas—Participants were given time to complete an electronic survey during the virtual meeting and were asked to rank their top priorities in each category. Ranking of the top 5 vs. the top 10 priorities was determined by the length of the list in each category (which included more than 20 ideas for the latter).
Data analysis
The ranks for each of the responses were summed across participants. A group-level rank and agreement on responses were calculated based on the number of participants who selected a response. The predetermined threshold for agreement was set at 70% based on accepted standards in consensus methodology (15).
Written narrative comments provided on completion of the ranking survey and verbalized comments made during the online discussion were compiled to give further context to the prioritized list.
Results
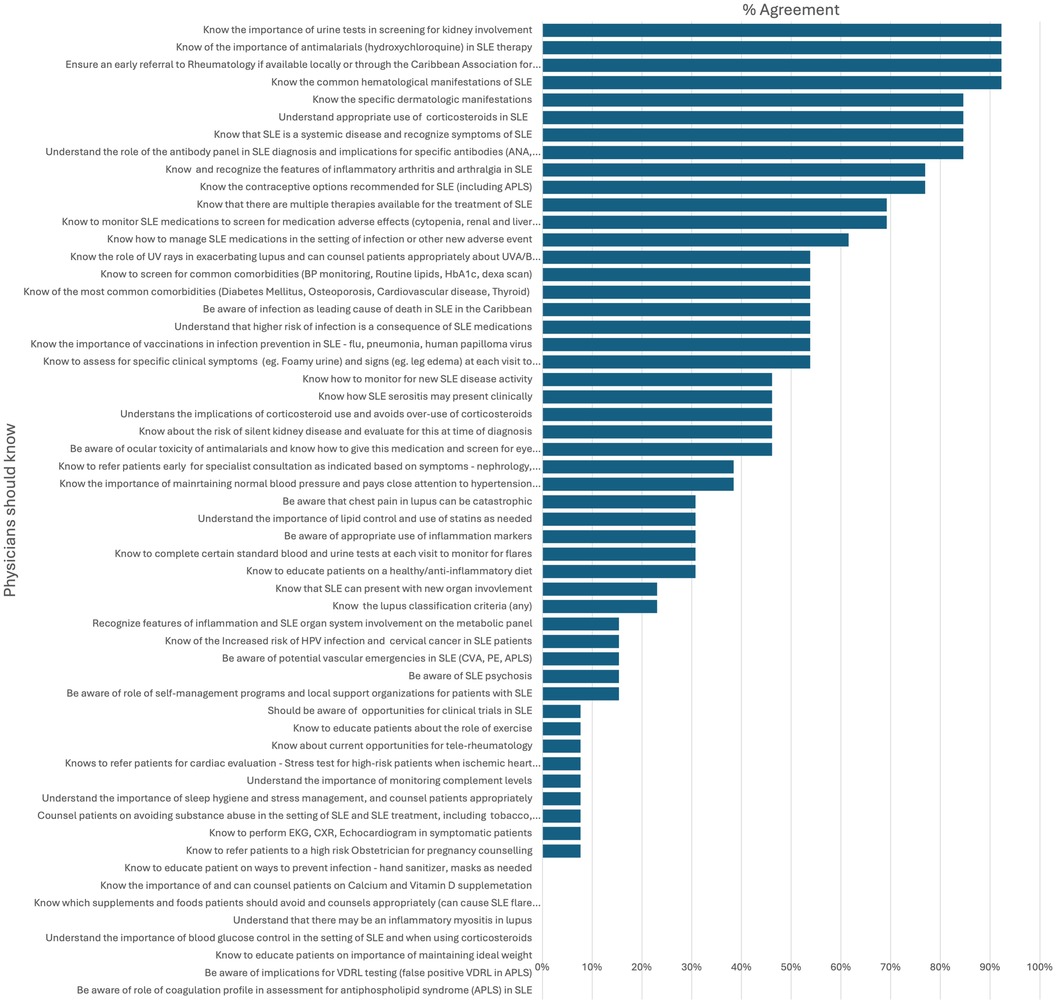
The study included 13 participants, 9 rheumatologists and 4 non-rheumatologists (2 internal medicine residents, 1 internist and 1 general practitioner) (Supplementary Table S2). Of these participants, 92% were female, had a mean age of 42.4 (8.2) years, and most were of Caribbean nationality (92%), and were practicing in the Caribbean. Participants ranged in experience (2–31 years) and clinical setting (private practice, public service, academic), and were representative of islands where rheumatology care is available to patients. Most participants held joint roles as practitioners and educators of medical trainees, were affiliated with regional academic institutions, and familiar with the local educational landscape and gaps in care in rheumatology. Sixty-nine ideas were generated in the initial phase, and refined to 66, after removal of duplicate and overlapping concepts. Three fundamental categories emerged: (1) Diagnosis and clinical acumen, (2) Management strategies and (3) Reproductive health. In the final prioritization exercise, participants voted on a total of 66 items across these 3 categories (.Figure 1).
Consensus
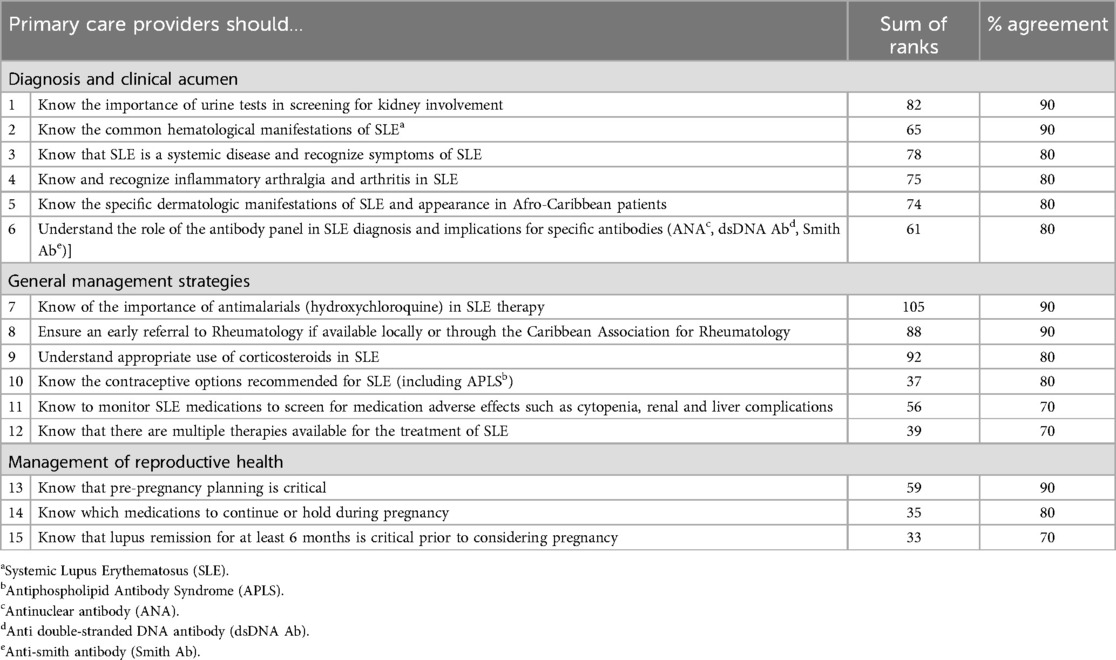
There was agreement on 15 responses (Table 1), with a focus on recognizing the systemic, dermatologic and musculoskeletal manifestations of SLE and early screening for kidney involvement. With respect to management strategies, priority areas were concentrated in pharmacological management. Participants agreed that education on the appropriate use of hydroxychloroquine (HCQ) and corticosteroids was critical, and rheumatologists should be involved in the care of suspected SLE patients. Education on contraception in SLE and medication monitoring was also ranked as important. In general, rheumatologists did not think that primary care providers should initiate therapy with disease modifying antirheumatic drugs (DMARD) other than HCQ but conceded that if patients were started on DMARD, medication monitoring for cytopenia and other adverse effects was critical. Pre-pregnancy planning with a focus on quiescent disease, medication management and high-risk obstetric counseling and care were also identified as priority areas.
Impact of experience and geographic region
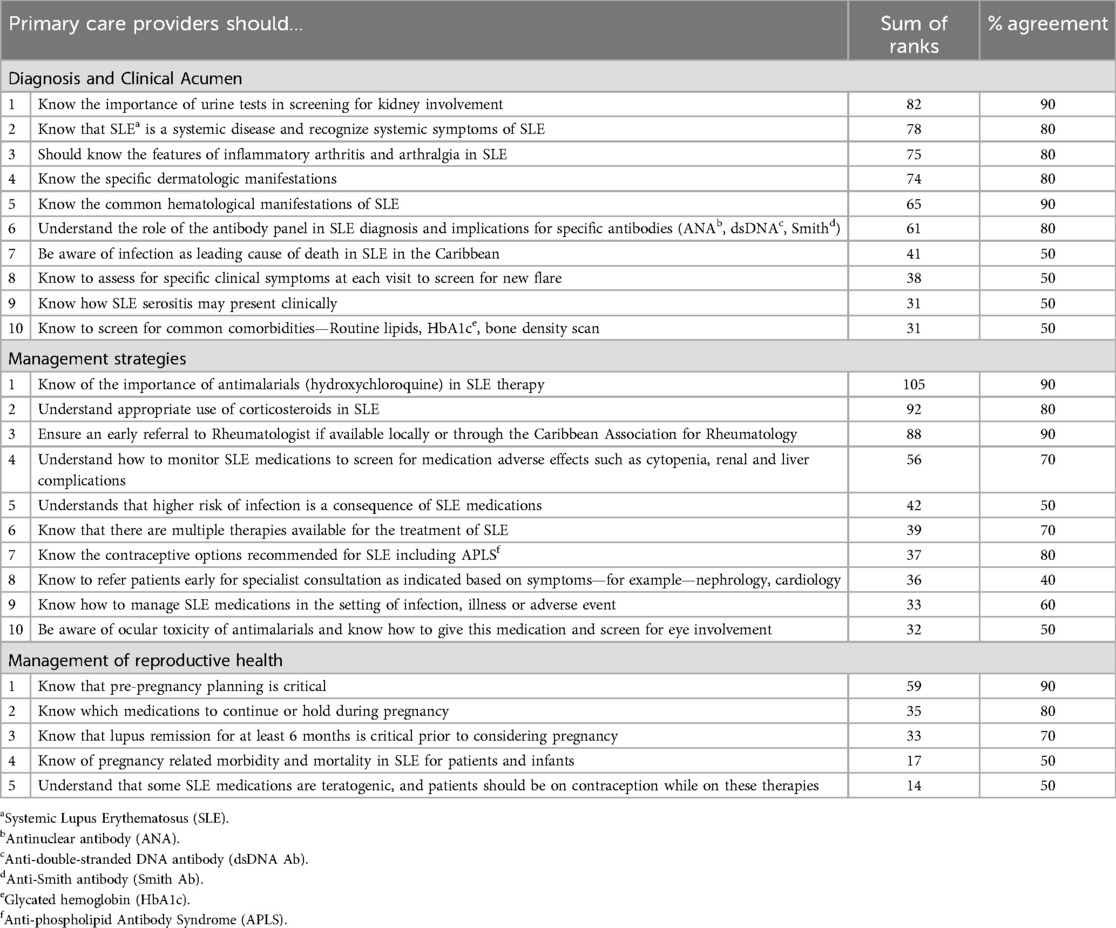
There was considerable overlap between years of experience and geographic location, with 71% (5/7) of providers in the Caribbean reporting more than 10 years of experience in their specialty, compared to 33% (2/6) of providers based elsewhere (Supplementary Table S2). Top scoring items were similar across all groups and in alignment with the identified top-ranking items (Table 2) with a few subtle differences. Providers within the Caribbean prioritized knowledge on ultraviolet A and B (UVA/B) protection, comorbid disease and infectious complications in patients with SLE, while providers outside of the Caribbean highlighted screening for ocular toxicity of HCQ and the role of vaccinations. The more experienced providers also emphasized the importance of understanding infectious complications, medication adverse effects and the need for UVA/B protection to prevent flares in patients with SLE.
Priorities for rheumatologists vs. Non-rheumatologists
There were a few differences between the responses ranked by rheumatologists and non-rheumatologists. Rheumatologists had high agreement on ensuring that PCPs were educated on the potentially fatal nature of infection in the Caribbean SLE patient, and in the online discussion, infection was highlighted as a primary cause of death. Internists however, prioritized knowledge about assessing new disease flares at clinical visits. Both agreed that it was important to educate PCPs about comorbidity management in SLE, with rheumatologists stressing general awareness while internists focused on performing specific screening procedures such as the annual lipid panel.
In management strategies, all agreed on the importance of HCQ use as standard therapy in all patients and appropriate corticosteroid use. Divergence occurred around the topic of infection with rheumatologists prioritizing knowledge of the risk of infection with certain SLE medications, compared to non-rheumatologists who focused on knowledge of vaccinations, early referral to appropriate specialists with new organ involvement, and medication management during illness.
In management of reproductive health, the top scoring topics among all participants included proactive pre-pregnancy planning, understanding medication safety during pregnancy, and achieving disease remission before conception. Rheumatologists and non-rheumatologists both emphasized the importance of comprehensive preconception planning and medication management, but rheumatologists particularly stressed the need for specialized care in high-risk clinics with obstetricians. Non-rheumatologists also highlighted the importance of understanding the risks associated with pregnancy in SLE patients and monitoring for incident lupus nephritis during pregnancy.
While there is some overlap in high scoring topics for both groups, rheumatologists demonstrate a heightened focus on specialized care. The top scoring topics (Table 2) reflect the items scored highly by both groups and were inclusive of items agreed on (crossing the 70% threshold) by rheumatologists only and non-rheumatologists only.
Insights from narrative comments
Participants had the opportunity to comment on ideas during the online clarifying discussion and the final ranking surveys. The main points of discussion included the impact of infection in SLE patients in the Caribbean and ensuring that the principles for steroid use were emphasized. Additionally, participants felt strongly that non-rheumatologists should not be expected to initiate advanced DMARD therapy in SLE but should be aware of the need to monitor for DMARD toxicity. There was specific reference to at least one occurrence of fatal Methotrexate-associated cytopenia. All agreed on the importance of preconception planning, with reference to a validated discussion aid that encouraged providers to initiate conversations around pregnancy. Participants believed this discussion aid to be concise yet comprehensive, and inclusive of essential topics around contraception and preconception planning in SLE. It was felt that this discussion aid should be adopted by CAR and utilized in PCP education. All 66 listed ideas were felt to be important, and participants emphasized that they should all be included in a comprehensive educational curriculum.
Discussion
The NGT process clarified the SLE educational priorities for Caribbean PCPs. Clear goals were to facilitate early recognition of SLE with monitoring for kidney involvement, early referral for management by a rheumatologist, and timely discussions about contraception and pregnancy for Caribbean SLE patients. Additionally, although PCPs are not expected to initiate advanced DMARD therapy, awareness of HCQ as the foundation of SLE therapy, minimizing corticosteroid use, and medication monitoring for adverse effects of DMARD therapy were stressed.
Early recognition of SLE
SLE is more prevalent and severe in the Caribbean than in the developed world (3). It accounts for significant morbidity in young women and contributes to high personal and governmental costs due to increased health system utilization for flares, infection and comorbid disease. Lupus is a leading cause of end-stage renal disease and mortality in young Afro-Caribbean women (18), with a high occurrence of proliferative glomerulonephritis and an associated poor prognosis. This may be mitigated by access to free specialized care as demonstrated in Martinique where reported renal outcomes are similar to those described in affluent White populations (19). Early recognition and prompt management are therefore particularly relevant to the Caribbean population. Barriers to diagnosis include lack of awareness in both health care systems and the public domains and lack of access to specialists (20), which is amplified in the Caribbean sphere. SLE educational materials for health care providers have traditionally lacked diversity in patient portrayals, with under-representation of skin of color. Cutaneous manifestations are a key presenting symptom of SLE but may be missed in skin of color. CAR's priorities focus on these dermatological manifestations in skin of color by highlighting the unique presentations in skin of color which lead to early recognition of pathology.
Early diagnosis is challenging due to the heterogeneous nature of the disease and varied clinical presentation. However, similar to other nations, patients in the Caribbean present most frequently with systemic, cutaneous and musculoskeletal features (3), awareness of which could influence early diagnosis. Delays in SLE diagnosis may also occur due to reliance on costly or specialized diagnostic tests, and CAR members emphasized the interpretation of readily available low-cost measures to support a lupus diagnosis. One measure with high agreement was the use of an in-office urinalysis to detect signs of kidney involvement at the time of diagnosis or with a lupus flare. Throughout the Caribbean, rheumatologists support the use of monthly at home urinalysis to detect kidney involvement in patients with SLE. The urinalysis gives an immediate and actionable result but does not supersede the random urine protein creatinine ratio, a more reliable and sensitive indicator of proteinuria, and the preferred test for healthcare encounters when available. Although knowledge of antibody panels was thought to be important, and highlighted as a priority, it was acknowledged that these test results are often delayed, and when suspicion is high based on clinical features, PCPs should initiate early referral and management strategies.
Early referral and management
Most Caribbean territories do not have enough rheumatologists to serve their populations adequately. There are widespread socioeconomic barriers to care, including availability and affordability of medications (10). The most cost-effective strategy of care, well recognized since the 1950's is early recognition and treatment of mild disease, emphasis on healthy lifestyle interventions, empowerment of patients as positive, adherent self-managers, and patient-team relationships built on trust. This is vital in the Caribbean to avoid the need for more expensive interventions. Despite recommendations that the rheumatologist is the ideal coordinator of the care team for a patient with rheumatic disease (21, 22), the Caribbean community must rely on PCPs to assume this role. CAR believes that PCPs can be trained to recognize the possibility of lupus, expedite specialist referrals and empower and support the SLE patient to manage life positively. CAR members did not believe that PCPs should initiate advanced DMARD therapy for SLE but were comfortable with HCQ as a staple in the PCPs treatment repertoire. Education on the indication, dosing, ocular toxicity monitoring and safe use in pregnancy was seen as a high priority and had the highest summed rank overall. Principles of corticosteroid use in SLE, and medication adverse effects were also areas of high priority, especially for the rheumatologists who referenced prior experience with fatal DMARD-associated cytopenia in unmonitored patients.
There was a stress on early referral to rheumatology, with high agreement from all participants. Despite the known lack of specialist care in some Caribbean islands, all believed that a rheumatologist should be involved in initiating and continuing management for newly diagnosed SLE patients. One potential way to institute this is via tele-rheumatology, which, recognized as important for access in the region and discussed by participants, was not considered a priority for PCP education and was one of the lowest ranking topics. Tele-rheumatology and tele-mentoring in rheumatology have been successfully used to reach underserved populations globally and to educate and support PCPs in the management of SLE patients (23, 24). The mismatch in expectation for specialist care and yet poor regional access to rheumatologists highlights a care gap that needs further development and an opportunity to engage PCPs in islands that lack rheumatology care.
Although the topics of infection and comorbid disease did not reach agreement, they received high ranks by multiple participants, and were identified priorities for Caribbean based providers In the Caribbean, severe, uncontrolled inflammation may fuel excessive corticosteroid use, and in the absence of appropriate prescribing and access to steroid-sparing medications, predisposes to infectious, cardiovascular and cerebrovascular complications, with premature loss of life, even when inflammation is no longer the primary problem. Sensitizing PCPs to the high rate of fatal infection in Caribbean SLE patients could affect the frequency of corticosteroid prescriptions, attention to recommended vaccinations and a greater vigilance for infection, with better outcomes for patients.
The PCP is the ideal person to encourage home monitoring of urine and blood pressure, educate the patient on the importance of adherence, manage emotional and physical well-being, and organize all appropriate screening for atherosclerotic disease and cardiovascular risk, metabolic bone disease and malignancy.
Reproductive health
Reproductive health was a priority for all participants, with high agreement on associated topics. SLE primarily affects women of childbearing age, who in the Caribbean, often head single-parent households. Hence, attention to reproductive health is critically important. Pregnancy in SLE patients is associated with poor maternal and fetal outcomes which is exacerbated in unplanned situations. The Caribbean region has one of the highest rates of unplanned pregnancy globally. Unplanned pregnancies coupled with high rates of poverty and lack of access to hormonal contraception (25) dramatically amplifies the risk of maternal and fetal complications. The importance of timely discussions about contraception and individualized family planning becomes paramount in the management of lupus in the Caribbean. Professional guidelines recommend routine use of contraception and engaging patients in early dialogue around a desire for conception. Pregnancy should only be considered when an SLE patient has been in remission for at least 6 months, after discontinuation of teratogenic medications, and with optimization of pregnancy-safe DMARDs (26). Four of the fifteen identified priorities for PCP education focused on reproductive health and included education on contraceptive options in SLE, preconception planning and medication management, and understanding the goal of quiescent disease prior to pregnancy, to mitigate the high risks of SLE pregnancy. Participants further endorsed a discussion aid shown to facilitate well-timed pregnancies for young women with SLE, and hence improve outcomes (27).
Rheumatologists vs. non-rheumatologists
Rheumatologists based in the Caribbean, who typically had more years of experience, emphasized the importance of education on infection prevention, comorbidity management, and UVA/B protection. These cost-effective measures can be readily implemented in resource-limited settings and likely represent clinical practice that does not depend heavily on healthcare infrastructure. There were few differences between rheumatologists and non-rheumatologists, but non-rheumatologists prioritized knowledge about general health, screening for comorbid disease and vaccinations. Whether PCPs perceive their role in SLE management as to be in areas that overlap with general medical care is unclear, but CAR's mandate is to empower and support PCPs as knowledgeable and proactive advocates for patients with SLE in the Caribbean.
Strengths and limitations
The NGT process facilitated equal representation of participants’ ideas by a democratic process, and with input from CAR core members, solidified the educational agenda for the annual educational forum. The online format, though less engaging than in-person interactions, enabled participation from providers across various geographical regions. The study was limited by the lack of perspective from islands without rheumatology access, potentially overlooking the unique educational needs of underserved areas. Additionally, the exclusion of primary care stakeholders other than rheumatologists and internists, limits the scope of insights into relevant SLE educational goals for the broader primary care ecosystem. Further research is essential to align educational goals with the needs of all Caribbean communities, especially for islands without rheumatology access. Engagement of a diverse range of primary care stakeholders will be crucial to understanding the specific SLE educational needs of underserved areas.
Conclusions
Guidance from professional organizations (21, 22) and global experience (28) is in alignment with the principal ideas emerging from the CAR NGT process. Given limited resources, CAR's initial focus for PCP education will comprise the 15 identified priorities, while advocating for a more nuanced SLE curriculum at regional medical institutions and organizations. A primary objective of CAR is to identify and educate PCPs willing to be rheumatology champions. A collaborative relationship with PCPs would greatly enhance the SLE patient experience and improve outcomes in the Caribbean through early recognition and referral for management of SLE and coordination of the multidisciplinary team.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
JL: Data curation, Visualization, Writing – original draft, Writing – review & editing. AK: Data curation, Writing – original draft, Writing – review & editing. NR: Data curation, Writing – review & editing. DH: Data curation, Writing – review & editing, Conceptualization, Project administration. SD: Data curation, Writing – review & editing, Conceptualization. KD-K: Data curation, Writing – review & editing, Conceptualization. TM: Data curation, Writing – review & editing. AR: Conceptualization, Data curation, Writing – review & editing. RM: Data curation, Writing – review & editing. SD: Conceptualization, Data curation, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to express sincere gratitude to CAR members whose contributions significantly enriched this work with their valuable insights and thoughtful discussion. Specifically, we thank Melissa Boyce MBBS, Cleopatra Altenor MBBS, and Marc Phillpotts MBBS for their support and expertise.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/flupu.2024.1446335/full#supplementary-material
References
1. Stojan G, Petri M. Epidemiology of systemic lupus erythematosus: an update. Curr Opin Rheumatol. (2018) 30(2):144–50. doi: 10.1097/bor.0000000000000480
2. Lau C-S, Feng P. Rheumatology without borders. Nat Clin Pract Rheumatol. (2007) 3(6):305. doi: 10.1038/ncprheum0509
3. Flower C, Hennis AJM, Hambleton IR, Nicholson GD, Liang MH, Group atTBNLR. Systemic lupus erythematosus in an African Caribbean population: incidence, clinical manifestations, and survival in the Barbados national lupus registry. Arthritis Care Res (Hoboken). (2012) 64(8):1151–8. doi: 10.1002/acr.21656
4. Pons-Estel GJ, Alarcón GS, Scofield L, Reinlib L, Cooper GS. Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum. (2010) 39(4):257–68. doi: 10.1016/j.semarthrit.2008.10.007
5. Tian J, Zhang D, Yao X, Huang Y, Lu Q. Global epidemiology of systemic lupus erythematosus: a comprehensive systematic analysis and modelling study. Ann Rheum Dis. (2023) 82(3):351–6. doi: 10.1136/ard-2022-223035
6. Molokhia M, Maconochie N, Patrick A, Doyle P. Cross-sectional analysis of adverse outcomes in 1,029 pregnancies of afro-Caribbean women in trinidad with and without systemic lupus erythematosus. Arthritis Res Ther. (2007) 9(6):R124. doi: 10.1186/ar2332
7. Gibson S, Johnson N, Simpson Brown S, Hartley S, Maloney K, Gossell-Williams M, et al. Pregnancy outcomes in systemic lupus erythematosus: experience from a Caribbean center. J Matern Fetal Neonatal Med. (2023) 36(1):2204392. doi: 10.1080/14767058.2023.2204392
8. Maloney KC, Ferguson TS, Stewart HD, Myers AA, De Ceulaer K. Clinical and immunological characteristics of 150 systemic lupus erythematosus patients in Jamaica: a comparative analysis. Lupus. (2017) 26(13):1448–56. doi: 10.1177/0961203317707828
9. Soyibo AK, DeCuelaer K, Miller RK, Smith R, Maloney K, Barton EN. Establishing the Jamaica lupus registry: report of patients with systemic lupus erythematosus attending a major referral hospital in Jamaica. West Indian Med J. (2012) 61(3):249–53. doi: 10.7727/wimj.2012.289
10. King A, Altenor C, Brown C, Hambleton I. LL-01 social determinants of treatment adherence and disease severity among people living with lupus in a small island developing state: a report from St. Lucia. Lupus Sci Med. 5(Suppl 2):A66. doi: 10.1136/lupus-2018-lsm.111
11. Worldometer. Caribbean population. Dover, Delaware: Worldometers.info (2024). Available online at: https://www.worldometers.info/world-population/caribbean-population/ (accessed July 14, 2024)
12. Battafarano DF, Ditmyer M, Bolster MB, Fitzgerald JD, Deal C, Bass AR, et al. 2015 American college of rheumatology workforce study: supply and demand projections of adult rheumatology workforce, 2015–2030. Arthritis Care Res (Hoboken). (2018) 70(4):617–26. doi: 10.1002/acr.23518
13. Razzaghi H, Martin DN, Quesnel-Crooks S, Hong Y, Gregg E, Andall-Brereton G, et al. 10-year trends in noncommunicable disease mortality in the Caribbean region. Rev Panam Salud Pública. (2019) 43:1–11. doi: 10.26633/rpsp.2019.37
14. Waggoner J, Carline JD, Durning SJ. Is there a consensus on consensus methodology? Descriptions and recommendations for future consensus research. Acad Med. (2016) 91(5):663–8. doi: 10.1097/ACM.0000000000001092
15. Nair R, Aggarwal R, Khanna D. Methods of formal consensus in classification/diagnostic criteria and guideline development. Semin Arthritis Rheum. (2011) 41(2):95–105. doi: 10.1016/j.semarthrit.2010.12.001
16. Michel DE, Iqbal A, Faehrmann L, Tadic I, Paulino E, Chen TF, et al. Using an online nominal group technique to determine key implementation factors for COVID-19 vaccination programmes in community pharmacies. Int J Clin Pharm. (2021) 43(6):1705–17. doi: 10.1007/s11096-021-01335-x
17. Wadey VM, Tang ET, Abelseth G, Dev P, Olshen RA, Walker D. Canadian multidisciplinary core curriculum for musculoskeletal health. J Rheumatol. (2007) 34(3):567–80.17183615
18. Hocaoglu M, Valenzuela-Almada MO, Dabit JY, Osei-Onomah SA, Chevet B, Giblon RE, et al. Incidence, prevalence, and mortality of lupus nephritis: a population-based study over four decades using the lupus midwest network. Arthritis Rheumatol. (2023) 75(4):567–73. doi: 10.1002/art.42375
19. Suzon B, Louis-Sidney F, Aglaé C, Henry K, Bagoée C, Wolff S, et al. Good long-term prognosis of lupus nephritis in the high-income afro-Caribbean population of Martinique with free access to healthcare. J Clin Med. (2022) 11(16):4860. doi: 10.3390/jcm11164860
20. S SZ, BGS CE, G-R J, Butts C, OC L. Increasing access to care and lupus treatments for individuals from underrepresented communities living with lupus: insights from qualitative interviews with patients, physicians, and payers. Lupus Sci Med. (2021) 8(Suppl 2):A1–A75. doi: 10.1136/lupus-2021-lupus21century.54
21. Guidelines for referral and management of systemic lupus erythematosus in adults. American college of rheumatology ad hoc committee on systemic lupus erythematosus guidelines. Arthritis Rheum. (1999) 42(9):1785–96. 10.1002/1529-0131(199909)42:9<1785::aid-anr1>3.0.co;2-#10513791
22. Fanouriakis A, Kostopoulou M, Andersen J, Aringer M, Arnaud L, Bae S-C, et al. EULAR recommendations for the management of systemic lupus erythematosus: 2023 update. Ann Rheum Dis. (2024) 83(1):15–29. doi: 10.1136/ard-2023-224762
23. Ferucci ED. Rural health care and telerheumatology. In: Peoples C, editor. Telerheumatology: Origins, Current Practice, and Future Directions. Switzerland: Springer International Publishing (2022). p. 201–7.
24. Zhao J, Mcglynn M, Bombardier C, Amanda JS. How echos amplify: the power of ECHO rheumatology for group practice to manage inflammatory arthritis & autoimmune disease. Ann Fam Med. (2023) 21(Supplement 1):4388. doi: 10.1370/afm.21.s1.4388
25. Langer A. El embarazo no deseado: impacto sobre la salud y la sociedad en américa Latina y el caribe. Rev Panam Salud Pública. (2002) 11(3):192–205. doi: 10.1590/s1020-49892002000300013
26. Sammaritano LR, Bermas BL, Chakravarty EE, Chambers C, Clowse MEB, Lockshin MD, et al. 2020 American college of rheumatology guideline for the management of reproductive health in rheumatic and musculoskeletal diseases. Arthritis Rheumatol. (2020) 72(4):529–56. doi: 10.1002/art.41191
27. Sims CA, Eudy AM, Doss J, Rogers JL, Sadun RE, Criscione-Schreiber L, et al. The impact of pregnancy planning and medical readiness on reproductive outcomes in women with systemic lupus erythematosus. Lupus. (2023) 32(14):1666–74. doi: 10.1177/09612033231216602
Keywords: systemic lupus erythematosus, education, Caribbean, primary care providers, access to care
Citation: Lawrence J, King A, Ramessar N, Henry D, Davis S, Davis-King K, McGhie T, Rolle A, Manno R and Dowell S (2024) Educational priorities for primary care providers on systemic lupus erythematosus in the Caribbean. Front. Lupus 2:1446335. doi: 10.3389/flupu.2024.1446335
Received: 9 June 2024; Accepted: 19 August 2024;
Published: 16 September 2024.
Edited by:
Cindy Hilary Flower, The University of the West Indies, BarbadosReviewed by:
Dzifa Dey, University of Ghana, GhanaChak Lau, The University of Hong Kong, Hong Kong SAR, China
Copyright: © 2024 Lawrence, King, Ramessar, Henry, Davis, Davis-King, McGhie, Rolle, Manno and Dowell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sharon Dowell, Sharon.dowell@awirgroup.org
†Present Address: Anishka Rolle,Doctors Hospital Health System, Department of Internal Medicine, Rheumatology, Nassau, The Bahamas; Western Atlantic University School of Medicine, Freeport, The Bahamas; Family Medical Center, Rheumatology, Nassau, The Bahamas
 Jannel Lawrence
Jannel Lawrence