- Section of Rheumatology, Department of Medicine, University of Santo Tomas, Manila, Philippines
SLE is a chronic autoimmune disease with a wide range of manifestations and potential to affect several organ systems. Complications arise from both disease and medications especially glucocorticoids, significantly contributing to overall morbidity and mortality. SLE predominantly affects patients during their prime productive years resulting in substantial economic burden on the patient, caregivers and society due to direct, indirect and intangible costs. In developing countries with limited resources, efficient healthcare delivery for most lupus patients remains elusive. This is magnified by the increasing shortage of rheumatologists and lupus specialists. Physician education starting in medical school as well as practical referral pathways and physician networking in clinical practice ensure continuity of and coordinated care for every lupus patient. Likewise, education of allied health professionals, patient empowerment and self-help programs help improve overall outcomes in SLE.
Introduction
Systemic lupus erythematosus (SLE) predominantly affects young individuals and interfere with their potential to be productive members of the societal workforce. Additionally, SLE as a disease significantly increases healthcare utilization with higher overall expenditures. Consequently, the burden of SLE impacts the patient, family, community and society. More than 85% of the world's population live in low to middle income countries (LMIC), usually in developing countries, where SLE has been associated with several unfavourable outcomes including higher disease activity, damage accrual, work disability and mortality (1, 2). Infections, notably tuberculosis (TB) are an important cause of mortality and morbidity in SLE particularly in low socioeconomic status (SES) settings, with TB infection closely linked to glucocorticoid use (3) further incurring additional healthcare costs in LMIC (4). These are compounded by the increasing patient load and globally dwindling rheumatology workforce which are largely responsible for many of the health disparities, resulting in diagnostic delay and severe organ damage, and contributing to overall SLE illness burden (5). Aside from the development and implementation of public policy measures to improve healthcare delivery in SLE (6), physician education is fundamental to mitigating the effects of these health disparities. This article proposes various strategies to strengthen lupus education and enhance coordinated care especially in resource-limited settings or developing countries.
Strategies for physician education and coordinated care in lupus
Integrating SLE in the medical curriculum and residency training program
“Start them early”. Medical education lays the foundation for capacity building of competent specialists in Rheumatology. Many rheumatology fellowship applicants develop an interest in rheumatology during medical school and internal medicine residency training, particularly in institutions with strong academic rheumatology orientation. Strategies should thus focus on increasing exposure to rheumatology in both medical school and residency (7).
Educational resources have been developed through The Lupus Initiative (TLI) of the American College of Rheumatology (ACR) to foster increased awareness of lupus among educators and students. These include presentations, videos, interactive case studies etc., appropriate for teaching on health disparities, management of chronic disease, and coordination of care. In particular, the ACR Medical School Outreach Project offers complimentary lupus educational resources to medical schools to help increase the number of healthcare providers who are knowledgeable about diagnosing and treating lupus (8).
Furthermore, the existing exchange programs which offer opportunities for young rheumatologists from LMICs in Asia Pacific League of Associations for Rheumatology (APLAR) to learn from APLAR Centers of Excellence (9) as well as engage and collaborate with colleagues at the annual ACR and European League Against Rheumatism (EULAR) meetings (10, 11) may be expanded to deserving and highly motivated medical students or residents with special interest in rheumatology.
Patient educators enrich the learning experience
“Patients are our best teachers”. Involving patients as educators more effectively hones patient-centric skills than if taught by physician-educators (12). The participation of “patient partners” with deforming rheumatoid arthritis who have been trained and certified in the demonstration and instruction of musculoskeletal physical examination has been adapted and consistently highly rated by students and trainees in developing countries like the Philippines (13). This innovative learning program has now been locally expanded to involve lupus patients with good communication skills to share their SLE journey, actively engaging students and trainees to better understand and integrate the knowledge of SLE from the patient's perspective.
Dedicated lupus clinics
“Tell me and I forget, teach me and I may remember, involve me and I learn” (quote from Benjamin Franklin). Students and residents learn best when the learning experience is interactive and pertinent to the necessary skills to best perform their tasks in clinical practice. A dedicated lupus clinic performs better in terms of quality measure compared with the general rheumatology clinic, by optimally leveraging the subspecialist's experience, care processes, interdisciplinary networks, and increased awareness of disease-pertinent guidelines (14).
A significant proportion of SLE cases are childhood in onset, thus dedicated pediatric lupus clinics are just as important as internal medicine (IM) lupus clinics. This poses an even greater challenge considering the global shortage of pediatric rheumatologists (15). Furthermore, due to earlier diagnosis and better disease control in children in the past decade, the number of patients with childhood SLE surviving into adulthood has rapidly increased, and the vulnerable transition period has been associated with disease flares and poor adherence (16). This compels the need for transition clinics to facilitate the seamless transfer of patients from pediatric to IM rheumatology (17). In developing countries with a more pronounced shortage of pediatric rheumatologists, the expanded role and training of the internist-rheumatologist in the care of children and adolescents with lupus becomes more crucial.
Notwithstanding the existing barriers, these dedicated clinics effectively allow focused patient interaction with the healthcare team composed of rheumatology fellows, internal medicine or pediatric residents, postgraduate interns and medical students, under the supervision of a rheumatology consultant who encapsulates the current patient status and facilitates the individualized patient disposition with the team, ranging from urgent or priority treatment measures to long-term management plans (18). Knowledge retention is thus enhanced by making the trainee and medical student an integral team member in the evaluation and treatment of these patients, as well as an active participant in their learning (19). This hands-on participation also helps develop and reinforce their interest to pursue rheumatology as a subspecialty.
Lupus education in primary care
Disruption points in optimizing patient pathways in SLE were systematically identified in a study of SLE patients, healthcare providers and other stakeholders. These disruption points included the need for a dedicated consultation and access to an SLE care coordinator, and cited the general undertraining of (primary care) physicians in autoimmune diseases like SLE, as well as lack of coordinated care from various healthcare providers (20).
The Applied Rheumatology Made Simple (ARMS) educational program conducted in some Asian countries facilitates implementation of a shared Model of Care for musculoskeletal conditions by targeting workforce capacity building and empowering the primary care practitioner (PCP) (13). Aligned with the ARMS program is the establishment of a systematic networking relationship between the lupus specialist e.g., rheumatologist and the non-lupus specialist e.g., PCP or general internist in the individualized care of an SLE patient at various stages of illness (Figure 1). With the increasing patient load and current lack of trained lupus specialists, this coordinated care model requires commitment to continuing physician education (21).
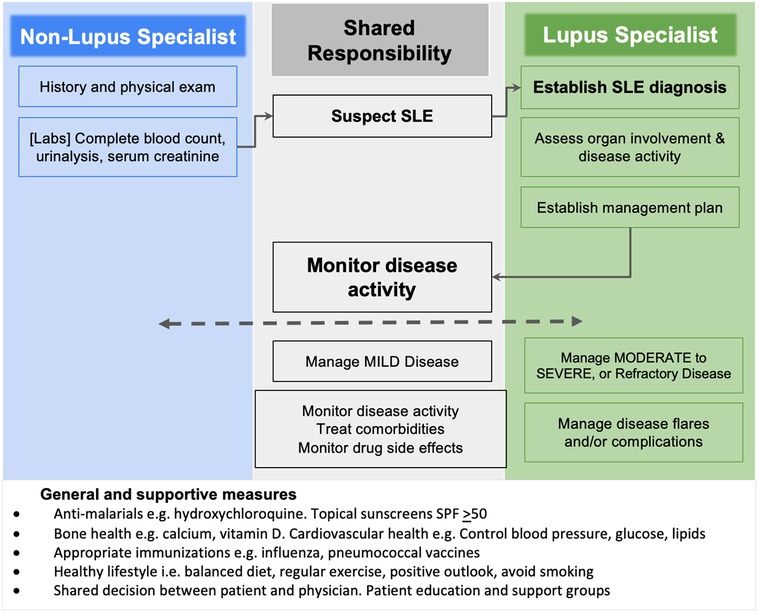
Figure 1. Algorithm in the coordinated care of a lupus patient throughout the disease course. Blue lines and blue box fill: roles of the non-lupus specialist including primary care and family physicians, internists, pediatricians. Green lines and green box fill: roles of the lupus specialist including rheumatologists and other subspecialists proficient in the care of lupus patients. Black lines and gray box fill: Shared roles and responsibilities between non-lupus specialist and lupus specialist.
Finally, the revival and widespread practice of telehealth propelled by the COVID-19 pandemic has had the most positive impact in helping underserved populations not only providing better healthcare access, but also strengthening collaboration opportunities among medical disciplines caring for a lupus patient especially in remote areas. Similarly, the surge of applications in digital technology has made it easier and efficient to organize virtual meetings and conferencing and dramatically increased access to cost-effective, inclusive, innovative and engaging learning opportunities including simulation scenarios, case management conferences and SLE updates for medical students and clinicians at all levels.
Summary and future directions
The heterogenous manifestations, organ involvement and variable clinical course of SLE, compounded by the shortage of lupus specialists pose a veritable barrier to early recognition and timely management. Physician education and practical referral guidelines are crucial to ensure early access to competent and efficient healthcare. Strategies for strengthening lupus education and enhancing coordinated care in developing countries include:
• Integrate and reinforce SLE in the undergraduate medical curriculum and residency training programs.
• Educate and empower primary care physicians, general internists and other non-lupus specialists who serve as first line of evaluation for patients, and assist them in deciding which patients need specialist care.
• Set up dedicated lupus clinics including transition (childhood to adult) clinics which actively deploy internal medicine or pediatric residents, interns and medical students.
• Establish networking relationships among healthcare providers in remote areas, led by a lupus specialist (in-person or virtually) to facilitate coordinated care of an individual lupus patient and conduct regular continuing medical education programs in lupus.
These strategies also well apply to allied health professionals e.g., nurses, physician assistants, counsellors. Alongside these strategies, we must continue to empower patients and reinforce patient self-help or peer-mentoring programs and other support group projects. Indeed, as lupus education and coordinated patient referral systems prosper especially in remote geographical areas, patients gain increased and earlier access to competent and efficient healthcare with improved quality of life, and society ultimately stands to reap the benefits of an overall reduced burden of SLE.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
SN: Writing – original draft.
Funding
The author declares that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tikly M, Navarra S. Lupus in the developing world—is it any different? Best Pract Res Clin Rheumatol. (2008) 22(4):643–55. doi: 10.1016/j.berh.2008.05.003
2. He X, Lloyd E, Cooper S, Li L, Chauhan D, Juliao P, et al. Healthcare costs and utilization for patients with systemic lupus erythematosus in China: a national claims database study. Value Health Reg Issues. (2023) 37:88–96. doi: 10.1016/j.vhri.2023.03.007
3. Darmawan G, Liman LMS, Wibowo SAK, Hamijoyo L, Apriani L, Atik N, et al. Global tuberculosis disease and infection in systemic lupus erythematosus patients: a systematic review and meta-analysis. Lupus. (2024) 33(6):555–73. doi: 10.1177/09612033241239504
4. Huang SP, DerSarkissian M, Gu YM, Duh MS, Wang M, Benson J, et al. Health care costs with sustained oral corticosteroid use in systemic lupus erythematosus. Clin Ther. (2023) 45(7):619–26. doi: 10.1016/j.clinthera.2023.04.013
5. Bruce IN. Health inequalities and systemic lupus erythematosus: a global challenge. Rheumatology. (2023) 62(Supplement_1):i1–3. doi: 10.1093/rheumatology/kead058
6. Mendoza-Pinto C, Etchegaray-Morales I, Ugarte-Gil MF. Improving access to SLE therapies in low and middle-income countries. Rheumatology. (2023) 62(Supplement_1):i30–5. doi: 10.1093/rheumatology/keac530
7. Miloslavsky EM, Bolster MB. Addressing the rheumatology workforce shortage: a multifaceted approach. Semin Arthritis Rheum. (2020) 50(4):791–6. doi: 10.1016/j.semarthrit.2020.05.009
8. The Lupus Initiative of American College of Rheumatology. (2024). Available online at: https://thelupusinitiative.org/educators-students/schools-2 (Accessed August 24, 2024).
9. APLAR-CoE Exchange Program. (2024). Available online at: https://aplar.org/collaboration/center-of-excellence/exchange-programe-application/ (Accessed August 24, 2024).
10. ACR-APLAR Exchange program. (2024). Available online at: https://www.ryumachi-jp.com/jcr_wp/media/2024/05/2024_ACR-APLAR_Application_and_Information.pdf (Accessed August 24, 2024).
11. APLAR-EULAR Exchange Program. (2024). Available online at: https://aplar.org/collaboration/aplar-eular-exchange-program/ (Accessed August 24, 2024).
12. McMahon GT. Learning together: engaging patients as partners in CPD. J Contin Educ Health Prof. (2021) 41(4):268–72. doi: 10.1097/CEH.0000000000000388
13. Lim KK, Chan M, Navarra S, Haq SA, Lau CS. Development and implementation of models of care for musculoskeletal conditions in middle-income and low-income Asian countries. Best Pract Res Clin Rheumatol. (2016) 30(3):398–419. doi: 10.1016/j.berh.2016.08.007
14. Arora S, Nika A, Trupin L, Abraham H, Block J, Sequeira W, et al. Does systemic lupus erythematosus care provided in a lupus clinic result in higher quality of care than that provided in a general rheumatology clinic? Arthritis Care Res. (2018) 70(12):1771–7. doi: 10.1002/acr.23569
15. Correll CK, Klein-Gitelman MS, Henrickson M, Battafarano DF, Orr CJ, Leonard MB, et al. Child health needs and the pediatric rheumatology workforce: 2020–2040. Pediatrics. (2024) 153(Supplement 2):e2023063678R. doi: 10.1542/peds.2023-063678R
16. Son MB, Sergeyenko Y, Guan H, Costenbader K. Disease activity and transition outcomes in a childhood-onset systemic lupus erythematosus cohort. Lupus. (2016) 25(13):1431–9. doi: 10.1177/0961203316640913
17. Sadun RE, Schanberg LE. Transition and transfer of the patient with paediatric-onset lupus: a practical approach for paediatric and adult rheumatology practices. Lupus Sci Med. (2018) 5(1):e000282. doi: 10.1136/lupus-2018-000282
18. Navarra SV, Zamora LD, Collante M. Lupus education for physicians and patients in a resource-limited setting. Clin Rheumatol. (2020) 39(3):697–702. doi: 10.1007/s10067-019-04795-9
19. Fett NM, Fiorentino D, Werth VP. Practice and educational gaps in lupus, dermatomyositis, and morphea. Dermatol Clin. (2016) 34(3):243–50. doi: 10.1016/j.det.2016.02.006
20. Schlencker A, Messer L, Ardizzone M, Blaison G, Hinschberger O, Dahan E, et al. Improving patient pathways for systemic lupus erythematosus: a multistakeholder pathway optimisation study. Lupus Sci Med. (2022) 9(1):e000700. doi: 10.1136/lupus-2022-000700
Keywords: lupus (SLE), education, coordinated care, developing countries, low to middle income country (LMIC)
Citation: Navarra SV (2024) Strengthening lupus education and coordinated care in developing countries. Front. Lupus 2:1462111. doi: 10.3389/flupu.2024.1462111
Received: 9 July 2024; Accepted: 19 August 2024;
Published: 2 September 2024.
Edited by:
Cindy Hilary Flower, The University of the West Indies, BarbadosReviewed by:
Sarfaraz Ahmed Hasni, National Institutes of Health (NIH), United StatesCopyright: © 2024 Navarra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sandra V. Navarra, c2FuZHJhX25hdmFycmFAeWFob28uY29t
 Sandra V. Navarra
Sandra V. Navarra