- 1Department of Thoracic Surgery, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
- 2Department of Medical Education, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
- 3School of Clinical and Basic Medical Sciences, Shandong First Medical University, Jinan, Shandong, China
Background: The flipped classroom teaching method has been increasingly adopted in recent years for teaching clinical medical specialties in medical schools around the world. However, the outcomes of this approach have not been systematically and quantitatively assessed. This meta-analysis aims to rigorously compare the effects of flipped classroom (FC) and traditional classroom (TC) teaching models on students’ learning in clinical medicine.
Methods: We conducted a systematic search for all randomized and quasi-randomized controlled trials (RCTs/Q-RCTs) comparing traditional classrooms and flipped classrooms in the context of clinical medical education. The literature search included the Cochrane Library, PubMed, Embase, and Web of Science, with the final retrieval conducted on October 26, 2024. We screened the literature based on predefined inclusion and exclusion criteria. The quality of each study was assessed using RevMan (Version 5.4). The outcome indicators included theoretical scores, composite scores, skills scores, and student satisfaction. Data extraction and subsequent meta-analysis were performed using Stata 17.0 software.
Results: A total of 12 studies were included in the analysis. The meta-analysis revealed that the flipped classroom (FC) group exhibited significantly higher theoretical scores (SMD = 0.481, 95% CI: 0.214 to 0.748, p = 0.000), composite scores (SMD = 0.642, 95% CI: 0.273 to 1.011, p = 0.001), and skills scores (SMD = 0.660, 95% CI: 0.312 to 1.008, p = 0.000) compared to the traditional classroom (TC) group. However, no statistically significant difference was observed in student satisfaction (SMD = −0.195, 95% CI: −1.081 to 0.691, p = 0.667).
Conclusion: The flipped classroom teaching method is more effective in enhancing the theoretical scores, composite scores, and skill scores of clinical medicine students compared to the traditional classroom teaching method. However, there was no statistically significant difference in student satisfaction between the two teaching approaches. Due to the limitations of the included studies, further robust randomized controlled trials (RCTs) across diverse educational contexts are necessary to validate these findings.
1 Introduction
The earliest iteration of the flipped classroom can be traced back to the peer-to-peer teaching method introduced by Eric Mazur in the early 1990s (Mazur, 1991). In 2007, Bergmann and Sams formalized the flipped classroom approach, whereby content traditionally delivered in the classroom is instead presented through videos and other formats outside of class, while classroom time is dedicated to student-driven, teacher-supported activities that reinforce prior learning (Lopez, 2022). Active learning is essential for effective teaching and learning, with strategies to engage students including pre-class preparation and active participation in discussions with peers (Freeman et al., 2014; Prober and Heath, 2012; Mehta et al., 2013). The flipped classroom exemplifies an “active learning” model in education (Freeman et al., 2014). Unlike traditional teaching methods, the flipped classroom prioritizes student engagement, fostering interaction and communication among students, while enhancing their independent learning capabilities. Due to these attributes, the flipped classroom is increasingly utilized across various domains of medical education, with growing confidence in its efficacy (Prober and Khan, 2013).
Students benefit from the flexibility of self-paced learning in the flipped classroom model, which enhances retention of material and increases engagement in learning (Bishop et al., 2013; Tucker, n.d.). This approach also positively influences students’ attitudes toward learning and fosters the development of critical thinking skills (Chen et al., 2017). However, clinical medicine, as a discipline demanding high levels of comprehensive ability, necessitates that students possess both theoretical knowledge and practical skills to effectively navigate complex clinical environments. Consequently, the effectiveness of the flipped classroom method may vary across different medical fields. This variability is supported by diverse research findings regarding students’ test scores and satisfaction levels (Jones-Bonofiglio et al., 2018), as well as the uncertain impact on skill development (Xu et al., 2019). The heterogeneity in the existing literature on the application of flipped classroom pedagogy in clinical medicine, along with the ambiguity surrounding its effectiveness, underscores the need for this meta-analysis. While the flipped classroom approach has demonstrated positive outcomes in basic medical education (e.g., pulmonary, renal, and cardiovascular physiology), its application in applied clinical disciplines remains limited (Tune et al., 2013; Morgan et al., 2015). This article aims to synthesize randomized controlled trials across various clinical topics, utilizing composite outcome metrics that could inform other clinical disciplines yet to adopt the flipped classroom model.
2 Methods
The meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Liberati et al., 2009). The study protocol has been registered with the International Prospective Systematic Evaluation Registry (PROSPERO) under the identifier CRD42024519911.1 As this meta-analysis utilized data from previously published studies, obtaining consent and ethical approval from the participants involved was not necessary (Hu et al., 2018).
2.1 Search strategy
To identify relevant studies, a comprehensive search was conducted across multiple databases, including PubMed, Cochrane Library, Embase, and Web of Science. Additionally, the references of the retrieved studies were manually reviewed to ensure the inclusion of potentially relevant literature. The retrieval strategy employed both Medical Subject Headings (MeSH) and keywords, specifically “flipped classroom” and “clinical medicine.” The final search was conducted on October 26, 2024. All duplicate entries were eliminated using Endnote X 9.3.3. No language restrictions were applied during the article selection process.
2.2 Selection criteria
Inclusion criteria were as follows: (1) Participants: Students studying clinical medicine courses [according to the Ministry of Health of China, clinical medicine is a primary discipline under the field of medicine, which includes secondary clinical application disciplines such as internal medicine, surgery, obstetrics and gynecology, pediatrics, among others (Ministry of Education, Ministry of Health, 2008)]; (2) Interventions: implementation of the flipped classroom teaching methodology; (3) Controls: application of the traditional teaching model; (4) Outcome measures: theoretical scores, composite scores, skill scores, and student satisfaction; (5) Study designs: randomized controlled trials (RCTs) or quasi-randomized controlled trials (Q-RCTs).
Exclusion criteria were as follows: (1) The course types studied in the article include basic medicine (such as subdisciplines like physiology, biochemistry, human anatomy, etc.), pharmacology, radiology, and other non-clinical application disciplines or clinical auxiliary disciplines; (2) Articles with incomplete data or lacking relevant target data; (3) Non-primary research publications, including reviews, meta-analyses, repeated studies, expert opinions, and conference summaries.
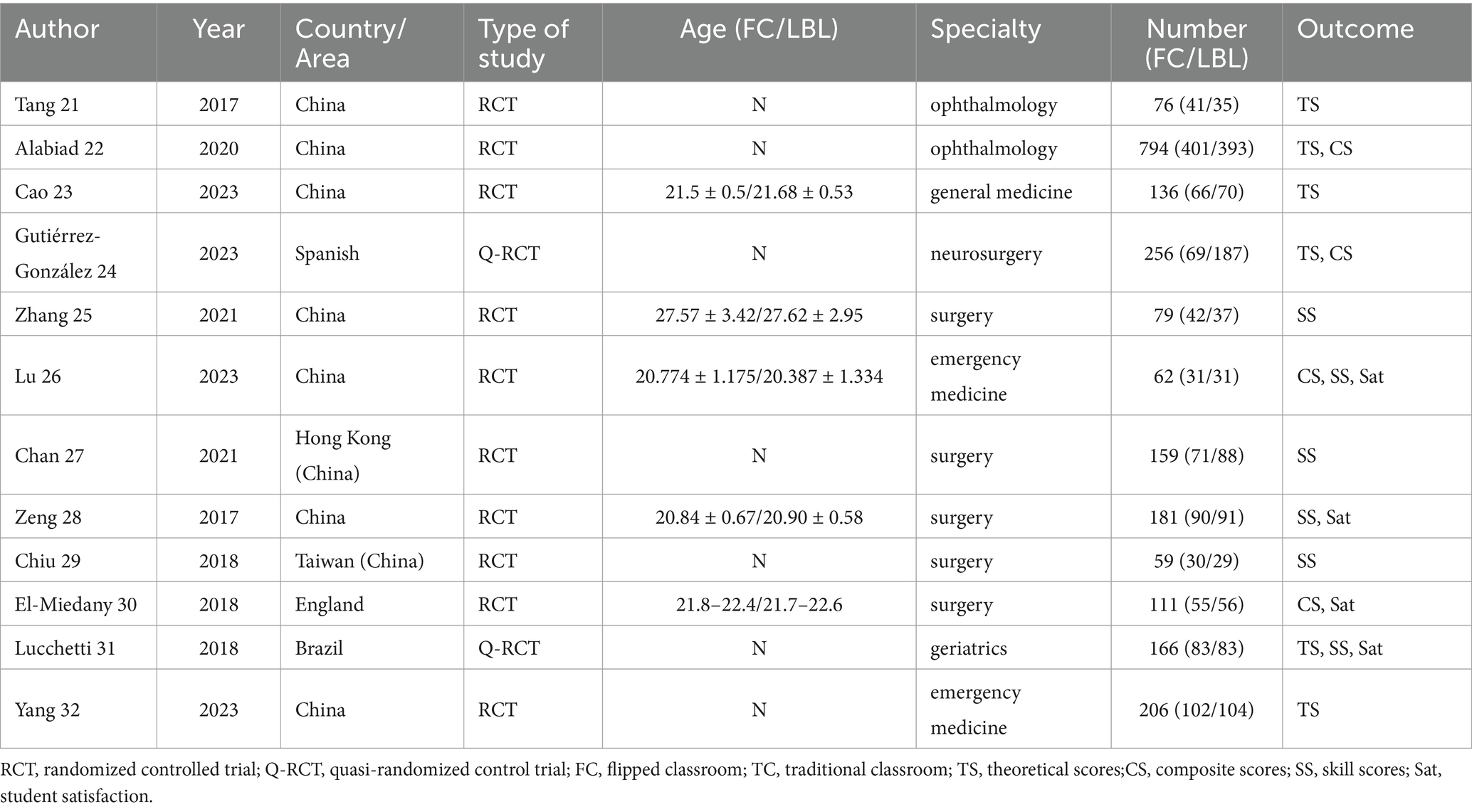
2.3 Data extraction
Data were independently collected by two authors from the literature that met the established inclusion and exclusion criteria, following the prior design of a data extraction form. The information extracted from the included studies encompassed the following variables: (a) Author, (b) Year of publication, (c) Country of origin, (d) Type of study, (e) Age of participants (FC/TC), (f) Specialty, (g) Sample size (FC/TC), and (h) Outcomes measured. Composite scores, theoretical scores, and skill scores served as objective outcome indicators, while student satisfaction was classified as a subjective outcome indicator.
2.4 Assessment of study quality
Two authors independently evaluated the methodological quality and risk of bias of the included studies. Any disagreements were discussed and resolved with the involvement of a third author. The assessment utilized Cochrane’s collaboration (Higgins et al., 2011) tool and was based on seven criteria: (1) random sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding of participants and personnel (performance bias), (4) blinding of outcome assessment (detection bias), (5) incomplete outcome data (attrition bias), (6) selective reporting (reporting bias), and (7) other biases. Each study was categorized under these criteria as “low risk,” “high risk,” or “unclear risk.” Additionally, efforts were made to obtain any missing data by contacting the authors of the relevant studies.
2.5 Statistical analysis
Data were entered and subsequently analyzed using Stata 17.0 software, including meta-analysis and heterogeneity testing. The Standardized Mean Difference (SMD) and 95% Confidence Interval (CI) were utilized for statistical analysis, with a significance level set at p < 0.05. Effect sizes were expressed using Hedges’ g to account for potential small sample sizes. The chi-square test was conducted, and the I2 statistic was calculated to assess the heterogeneity of the included studies (Higgins et al., 2003). An I2 value of less than 50% and a p-value greater than 0.10 indicated low heterogeneity, allowing for a meta-analysis using a fixed-effects model; conversely, a random-effects model was employed when heterogeneity was present. In cases of identified heterogeneity, sensitivity analyses were performed to exclude certain studies, and the remaining data were re-evaluated to determine the significance of the exclusions. Funnel plots and Egger’s test (Egger et al., 1997) were utilized to assess potential publication bias, small study effects, and evidence of asymmetry (Guyatt et al., 2011). The impact of publication bias on the overall effect size was further evaluated using the trim-and-fill method.
3 Results
3.1 Studies selection and basic characteristics
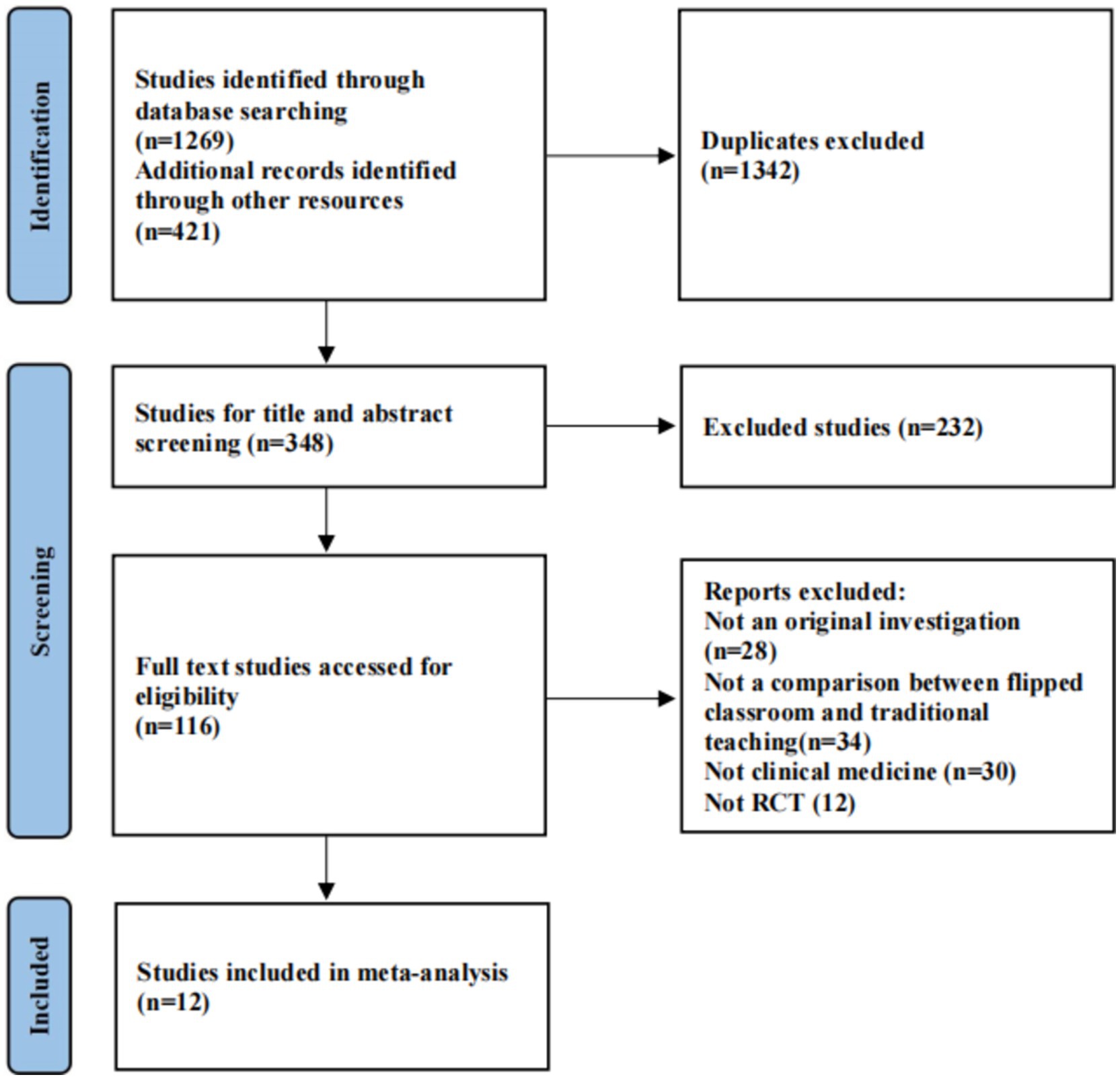
A total of 1,269 documents were retrieved from multiple databases, with an additional 421 documents obtained through manual searches. Following the removal of 1,342 duplicates, 348 documents were screened based on the established inclusion and exclusion criteria. Ultimately, 12 papers were included in the final analysis (Tang et al., 2017; Alabiad et al., 2020; Cao et al., 2023; Gutiérrez-González et al., 2023; Zhang et al., 2022; Lu et al., 2024; Chan et al., 2021; Rui et al., 2017; Chiu et al., 2018; El-Miedany et al., 2019; Granero Lucchetti et al., 2018; Yang et al., 2023). Baseline information for the included studies is presented in Table 1, and the literature selection process is illustrated in Figure 1.
3.2 Risk of bias and methodological quality assessment of included documents
The risk of bias in the included studies was evaluated using the Cochrane Risk of Bias Tool. Figure 2 illustrates the bias assessment for the 12 studies included in the review. One study (Granero Lucchetti et al., 2018) presented unclear grouping methods. In two studies (Alabiad et al., 2020; El-Miedany et al., 2019), the researchers recruited medical students from a specific grade level for the experimental group, referred to as the flipped classroom instruction group. Additionally, three studies (Zhang et al., 2022; Lu et al., 2024; El-Miedany et al., 2019) provided participants with detailed information regarding the study objectives, research procedures, and the curriculum model, facilitating informed consent and ensuring participants’ understanding of the course content. These studies were classified as high risk under the relevant criteria. All included studies reported complete data, thereby minimizing the potential for reporting bias. No instances of selective reporting or other biases were identified. Overall, the majority of the included literature demonstrated a low risk of bias.
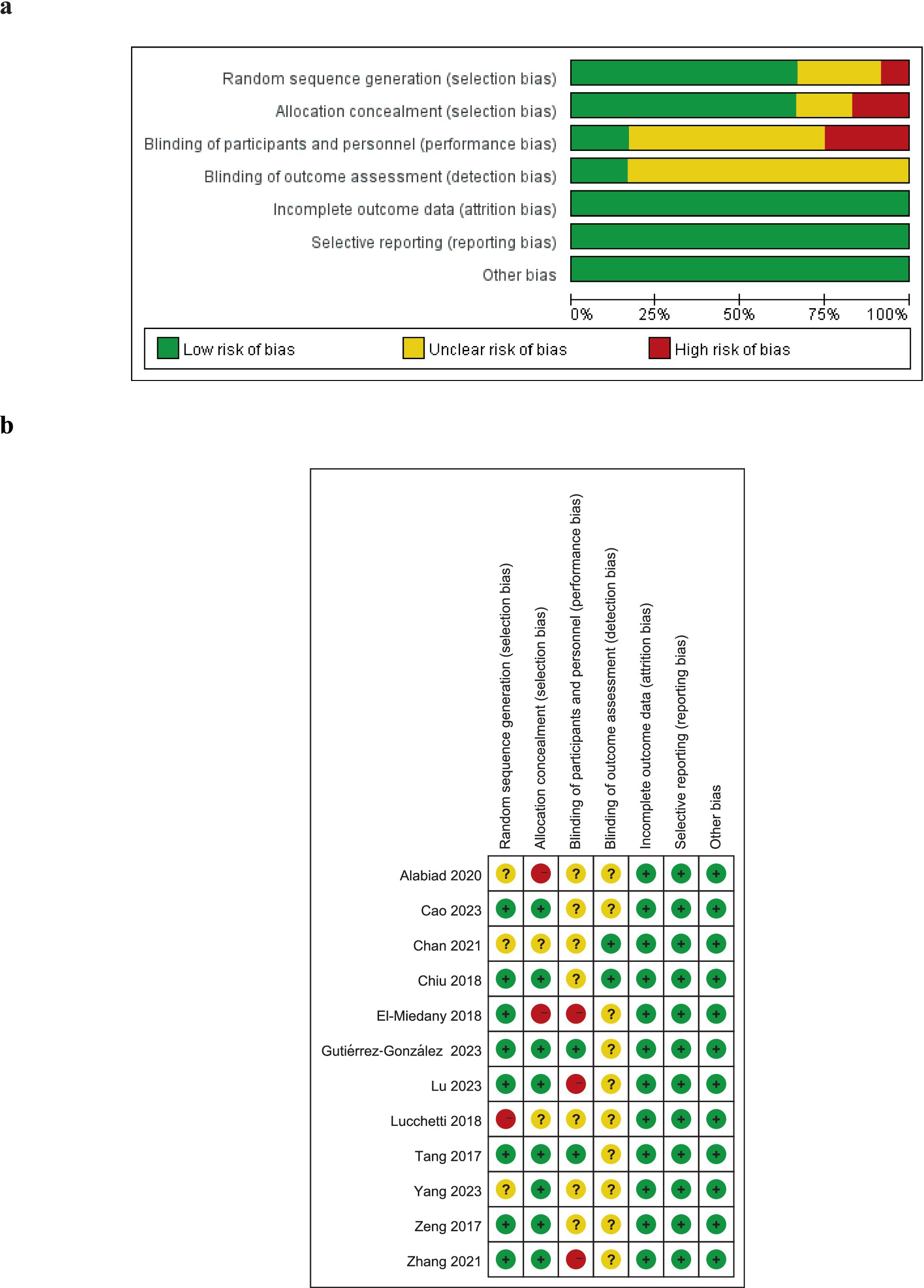
Figure 2. Risk-of-bias assessment. (A) Risk of bias graph as percentages for 11 included documents; (B) Risk of bias summary for each included document.
3.3 Meta-analysis results
3.3.1 Theoretical scores
A total of 1,006 students were included across six studies, with 444 in the flipped classroom group and 562 in the traditional teaching group. Analysis revealed significant statistical heterogeneity among the studies (I2 = 75.6%, p = 0.001). Consequently, a meta-analysis was conducted using a random effects model. The combined effect sizes indicated a statistically significant difference in theoretical scores between the two groups (SMD = 0.481, 95% CI: 0.214 to 0.748, p = 0.000) (Figure 3A). Students in the flipped classroom group demonstrated superior theoretical knowledge compared to those in the traditional teaching group.
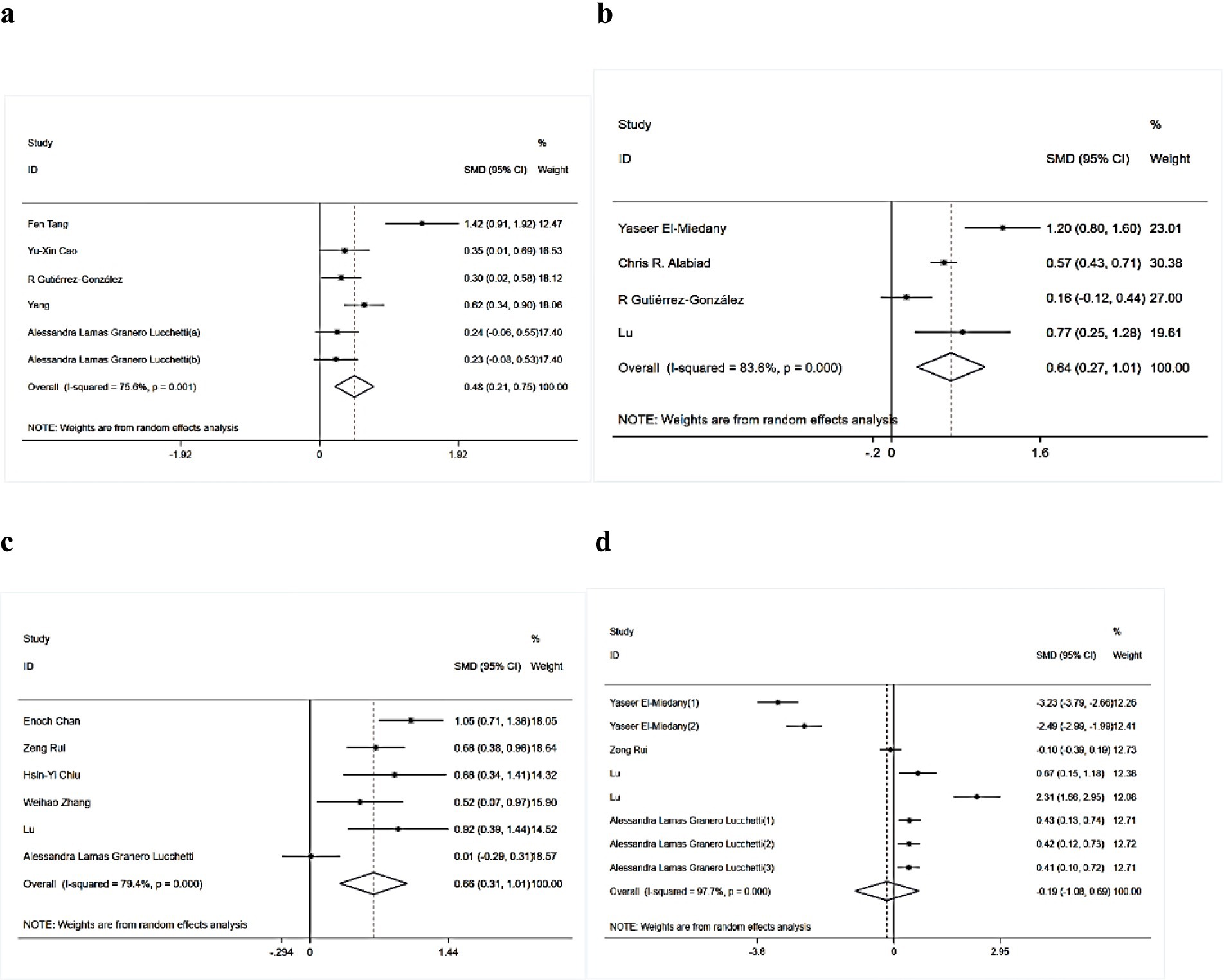
Figure 3. Forest plots for this meta-analysis: (A) theoretical scores, (B) composite scores, (C) skill scores, (D) student satisfaction.
3.3.2 Composite scores
A total of 1,223 students from four studies were analyzed, comprising 556 students in the flipped classroom group and 667 in the traditional teaching group. Significant statistical heterogeneity was observed among the studies (I2 = 83.6%, p = 0.000). Consequently, a meta-analysis was performed using a random effects model. The combined effect sizes revealed a statistically significant difference in composite scores between the two groups (SMD = 0.642, 95% CI: 0.273 to 1.011, p = 0.001) (Figure 3B). Students in the flipped classroom group exhibited superior performance in general competence compared to those in the traditional teaching group.
3.3.3 Skill scores
A total of 706 students across six studies were assessed for skill scores, with 347 participants in the flipped classroom group and 359 in the traditional teaching group. Analysis revealed significant statistical heterogeneity among the studies (I2 = 79.4%, p = 0.000). Therefore, a meta-analysis was conducted using a random effects model. The combined effect sizes demonstrated a statistically significant difference in skill scores between the two groups (SMD = 0.66, 95% CI: 0.312 to 1.008, p = 0.000) (Figure 3C). Students in the flipped classroom instruction group exhibited superior skill manipulation compared to those in the traditional instruction group.
3.3.4 Student satisfaction
A total of 1,028 students across eight studies participated in a survey assessing their satisfaction with both the flipped classroom and traditional classroom approaches, with 511 students in the flipped classroom group and 517 in the traditional teaching group. Significant statistical heterogeneity was identified among the study results (I2 = 97.7%, p = 0.000). Consequently, a meta-analysis was conducted using a random effects model. The combined effect sizes indicated no statistically significant difference in satisfaction between the two groups (SMD = −0.195, 95% CI: −1.081 to 0.691, p = 0.667) (Figure 3D). These findings suggest that students have varied and mixed perceptions of the flipped classroom and traditional teaching methods.
3.4 Sensitivity analysis
Due to the substantial heterogeneity observed among the studies, sensitivity analyses were conducted. Initially, each study was individually excluded from the analysis of each outcome indicator, and the remaining studies were then combined for reevaluation, as depicted in Figure 4. The results indicate that the four combined effect sizes, after the exclusion of each study, remain within the 95% confidence interval of their initial combined effect sizes. Furthermore, the new combined effect sizes, whether statistically significant or not, are consistent with the original findings, suggesting a relative stability in our results. To further assess stability, we also performed analyses after excluding the studies that exerted the greatest influence on each outcome metric prior to conducting the combined analysis. Following the exclusion of the study with the largest effect on theoretical scores (Gutiérrez-González et al., 2023), the combined effect size for the remaining studies in this outcome metric was SMD = 0.529 (95% CI: 0.199–0.860, p = 0.002), which did not alter the outcome of the original combined effect size. Similarly, after removing the study with the largest effect on composite scores (Alabiad et al., 2020), the combined effect size for the remaining studies remained at SMD = 0.695 (95% CI: 0.015–1.375, p = 0.045), with no change to the original result. Upon excluding the study with the largest effect on skill scores (Rui et al., 2017), the combined effect size for the remaining studies was SMD = 0.660 (95% CI: 0.210–1.111, p = 0.004), again consistent with the original finding. Finally, after deleting the study with the largest effect on student satisfaction (Rui et al., 2017), the combined effect size for the remaining studies was SMD = −0.210 (95% CI: −1.289–0.869, p = 0.703), which did not affect the original outcome. These sensitivity analyses collectively affirmed the reliability of our outcome indicators.
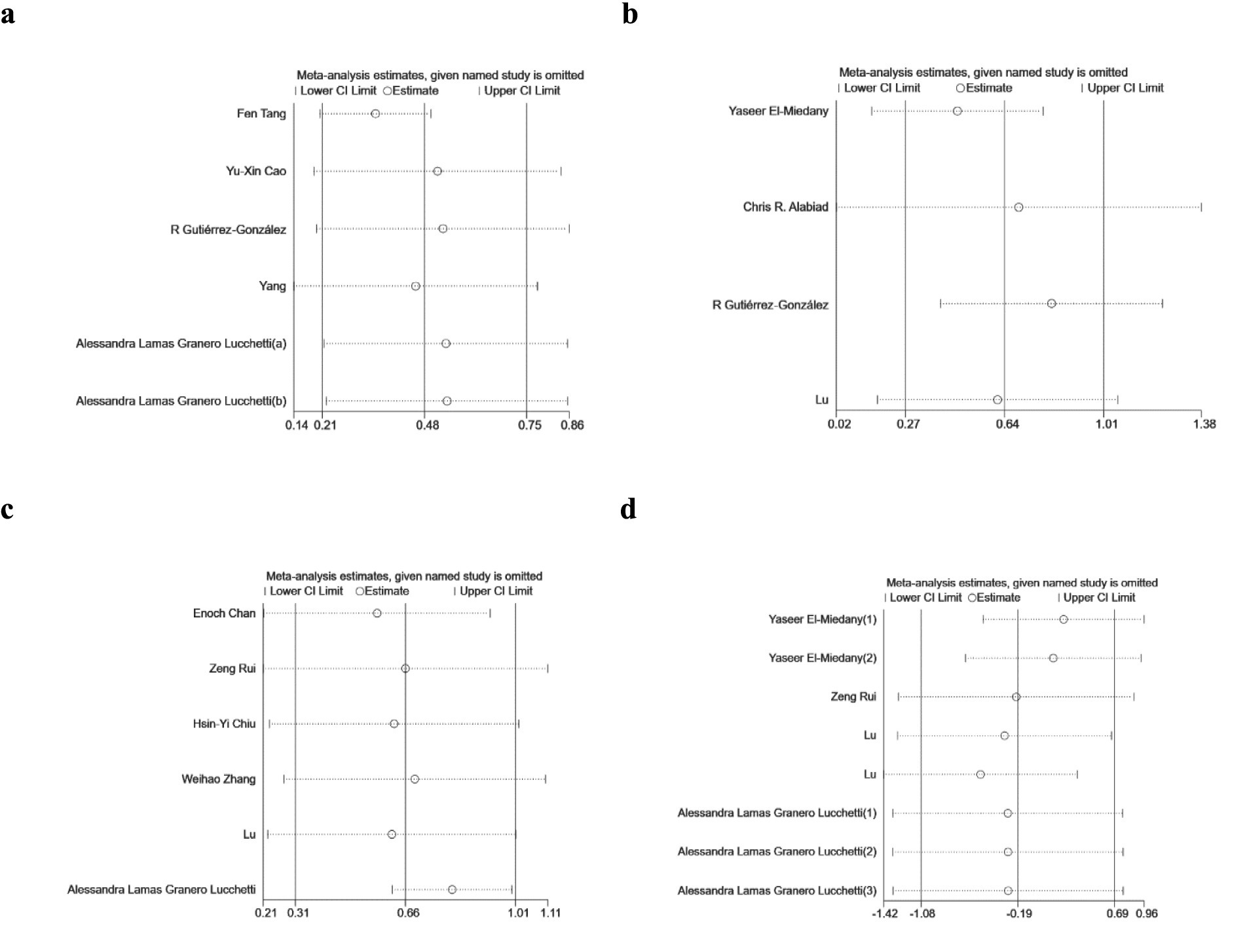
Figure 4. Sensitivity analysis of this meta-analysis: (A) theoretical scores, (B) composite scores, (C) skill scores, (D) student satisfaction.
3.5 Publication bias
Funnel plots were utilized to assess publication bias for the outcome metrics in the included studies (Figures 5A–D). The observed funnel plots exhibited relative symmetry; however, it is important to note that this assessment is inherently visual and somewhat subjective. Moreover, the determination of true funnel plot symmetry is complicated by the limited number of studies included for each combined outcome indicator (Sterne et al., 2011). Consequently, publication bias was quantitatively evaluated using the Egger linear regression test for each of the four combined effect sizes. The results were as follows: theoretical scores (P > |t| = 0.089), composite scores (P > |t| = 0.693), skill scores (P > |t| = 0.482), and student satisfaction (P > |t| = 0.466). These findings indicated no evidence of publication bias for any of the four outcome indicators. Additionally, the application of the cut-and-patch method revealed that the exclusion of individual studies did not significantly alter the original combined effect sizes. Collectively, these analyses suggest that the results are robust.
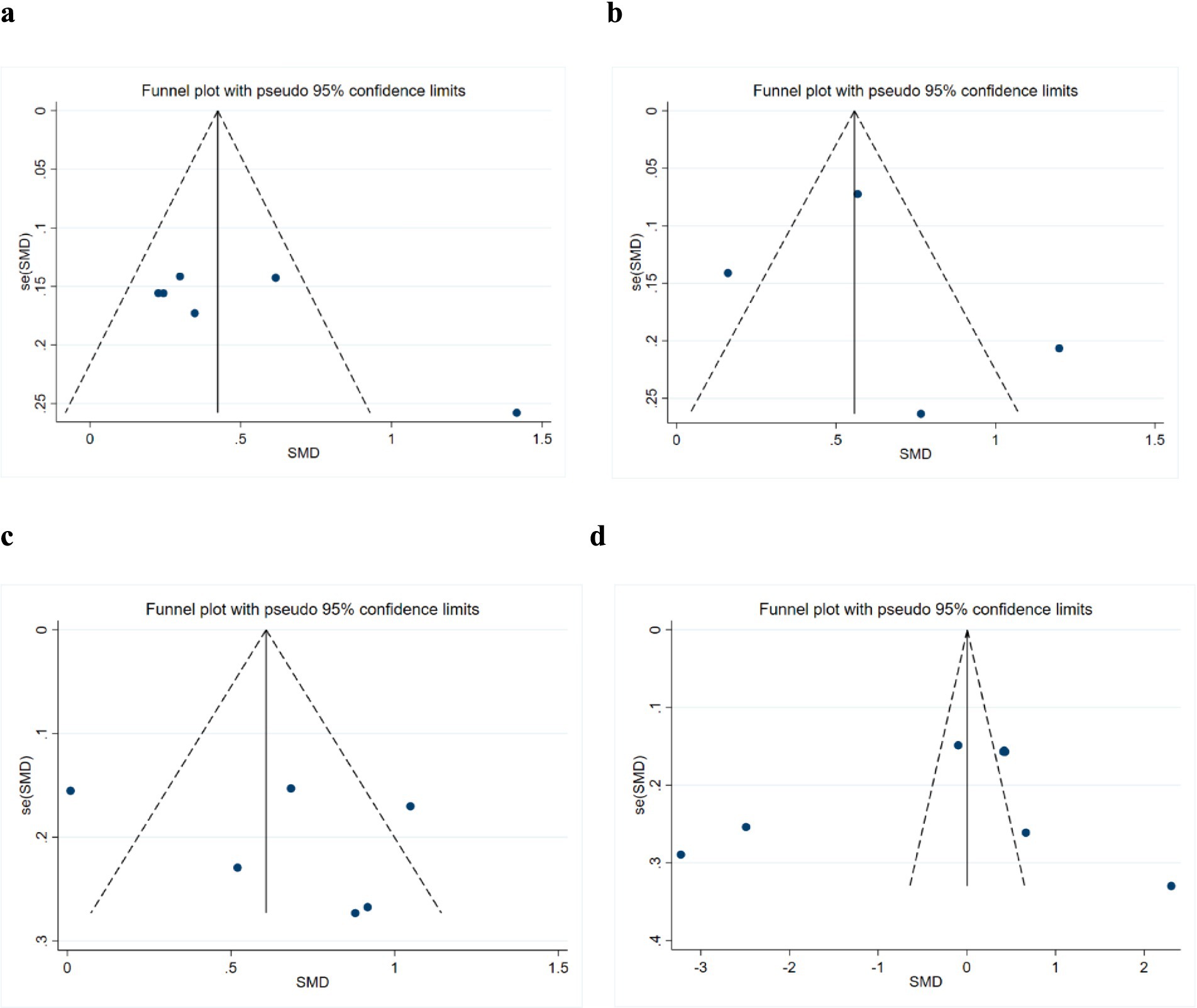
Figure 5. Funnel plot of this meta-analysis: (A) theoretical scores, (B) composite scores, (C) skill scores, (D) student satisfaction.
4 Discussion
4.1 Summary of main findings
According to the standards of the Ministry of Health of China, both clinical medicine and basic medicine are classified as primary disciplines (Ministry of Education, Ministry of Health, 2008). Clinical medicine is divided into 12 secondary disciplines, including major fields such as internal medicine, surgery, obstetrics and gynecology, and pediatrics, while basic medicine is divided into 6 secondary disciplines, including key areas such as human anatomy and histology, immunology, and pathology. Clinical medicine is based on the knowledge acquired from basic medicine to diagnose and treat patients, and their relationship is akin to that between basic and applied sciences. Both basic and clinical medicine share the mission of understanding human life processes and uncovering their underlying principles, with clinical medicine being the primary means for diagnosing diseases. Most medical students, especially in China, choose the medical profession with the primary goal of becoming clinical doctors. Therefore, to accurately assess the applicability and potential of the flipped classroom teaching method, we selected clinical application disciplines of significant clinical value. These disciplines are highly representative within the scope of the research questions, are closely aligned with the core focus of the study, and their case types, treatment methods, and other factors sufficiently meet the analytical needs of this research, providing strong support for the study’s conclusions.
This meta-analysis provides a comprehensive evaluation of the effectiveness of flipped classroom pedagogy among clinical medical students, utilizing four primary outcome metrics: theoretical scores, skill scores, composite scores, and student satisfaction. An extensive literature search was conducted to identify studies comparing flipped classroom pedagogy with traditional teaching methods regarding their effectiveness in clinical specialties. A total of 12 studies meeting the inclusion criteria were analyzed, all employing flipped classroom pedagogy for the experimental group and traditional pedagogy for the control group. The findings indicate that the flipped classroom approach significantly enhances theoretical knowledge, practical skills, and overall competencies in clinical medical students compared to traditional methods. However, student feedback revealed varied attitudes toward the two pedagogical approaches.
The enhanced effectiveness of flipped classrooms compared to traditional classrooms in fostering student achievement can be attributed to several key factors. Central to the flipped classroom model is the student. First, by distributing teaching videos in advance, students have the opportunity to revisit the material post-class, allowing them to analyze key concepts and address difficulties at their own pace. This promotes personalized learning, empowering students to take responsibility for their own education (Shiau et al., 2018). Such an approach acknowledges individual differences among learners and demonstrates a more student-centered, humane educational framework than traditional methods. Additionally, the student-centered nature of flipped classrooms is evident during in-class activities. In this environment, instructors guide students in tackling challenging problems and assessing their independent learning progress. Upon achieving an understanding or mastery of the knowledge presented in this course, students demonstrate increased confidence and actively engage with both the instructor and their peers in discussions, sharing their insights. This interaction fosters a dynamic classroom atmosphere and enhances teamwork, enabling students to acquire more skills and knowledge compared to traditional teaching methods (Hu et al., 2018). Furthermore, this approach improves students’ interest in learning by facilitating the practice of their expression and communication skills. In contrast, the predominant teaching system in many countries remains traditional, teacher-centered, where students passively receive information, significantly hindering their motivation to learn (Gong and Dong, n.d.). The implementation of the flipped classroom model addresses this issue by providing students with a sense of immediacy and rekindling their interest in learning (Hu et al., 2018). Additionally, the flipped classroom model supports the retention of students’ abilities to recognize clinical signs and symptoms as well as to perform essential clinical skills (El-Miedany et al., 2019).
The increased interest in learning and improved academic performance naturally lead to a generally positive perception of the flipped classroom among students. However, it is noteworthy that some students express a preference for traditional instructional methods. This preference may stem from their previous experiences, which predominantly involved traditional lecture-based teaching, resulting in a reliance on this approach. Additionally, certain students may struggle with self-directed learning and possess limited self-efficacy. Insufficient preparation prior to class can hinder their ability to keep pace with the instructor and peers, ultimately undermining their self-confidence. Secondly, some students perceive traditional teaching as more systematic in terms of knowledge transfer compared to the flipped classroom model. Despite achieving higher grades with the flipped classroom approach, certain students remain ambivalent about its effectiveness. This ambivalence is largely due to the challenge of shifting away from their dependence on the instructor and altering their passive information reception habits. Furthermore, the flipped classroom necessitates substantial out-of-class time, which can increase the overall learning burden on students. This additional workload may contribute to the reluctance of some students to fully embrace this teaching method, even in light of their improved academic performance. Notably, there were no statistically significant differences in the attitudes of the various student groups, preventing a conclusive determination of their overall impressions of the two instructional approaches.
In a flipped classroom model, the role of the teacher is no longer merely that of a knowledge transmitter but instead becomes that of a guide and facilitator. For teachers, allowing students to watch instructional videos multiple times before class can help mitigate the issue of students falling behind in traditional classroom settings, thus avoiding the need for supplementary lessons or the revision of teaching plans for students with varying levels of comprehension. In class, less time is spent on theoretical learning, allowing for more time to engage in case discussions, practical exercises, and interactive communication, which helps develop students’ clinical reasoning and hands-on skills while also enhancing classroom dynamics. However, teachers also face several challenges. The preparation required for flipped classroom teaching demands substantial time and effort, and places high demands on the teacher’s capabilities (Cao et al., 2023). Additionally, some students may lack self-management skills, particularly in clinical internships, where time is constrained and tasks are heavy, making it difficult for them to effectively organize pre-class learning. This could impact the subsequent classroom teaching process and increase the teacher’s workload. Overall, despite these challenges, the flipped classroom approach has the potential to improve teaching quality when these obstacles are overcome.
4.2 Strengths and limitations of the review
Firstly, our search was comprehensive, utilizing MeSH terms and keywords across multiple databases relevant to the flipped classroom and clinical medicine. Secondly, sensitivity analyses and the assessment of publication bias confirmed the robustness and credibility of the results of this meta-analysis. Additionally, our outcome measures are notably comprehensive, incorporating both objective indicators—specifically, students’ theoretical scores, skills scores, and composite scores—as well as the subjective measure of student satisfaction.
Our study does have some limitations as well. We did not search for unpublished literature, which may have resulted in the omission of relevant data. The included studies also have several limitations. Their teaching curricula, duration, and examination criteria could not be standardized, leading to significant heterogeneity. Additionally, the methodological quality of some studies was suboptimal, characterized by inaccurate randomization methods and lack of allocation concealment. Some studies also had small sample sizes. This study systematically evaluated the flipped classroom teaching model exclusively through students’ objective grades and subjective opinions, omitting an analysis of teachers’ subjective experiences. Teachers invest considerable time and effort in creating pre-course learning materials, such as instructional videos, and their participation is crucial to the flipped classroom approach. This oversight raises questions regarding the objectivity and comprehensiveness of the study’s findings.
It is worth noting that although we did not specifically search for studies from China in these databases, it is indisputable that research from China constitutes three-quarters of all studies included in our analysis. In clinical medical education in China, most basic disciplines, such as physiology, pathology, and anatomy, typically adopt traditional lecture-based teaching, which is teacher-centered. Only clinical application disciplines, directly related to diagnosing and treating diseases in clinical practice, tend to employ emerging teaching methods such as Flipped Classroom (FC), Case-Based Learning (CBL), and Problem-Based Learning (PBL), as these approaches are well-suited for case discussions that foster the development of students’ clinical thinking and skills. However, this is not yet widespread in most medical schools in China, where such teaching methods may be implemented only once every 2 weeks. As a result, Chinese researchers are actively conducting experiments to demonstrate the effectiveness and applicability of the flipped classroom approach in clinical application disciplines. Most medical students are expected to enter hospitals and become clinicians, and their clinical competencies reflect the quality of their medical education. The courses that develop their clinical abilities primarily come from clinical application disciplines such as internal medicine and surgery. Exploring the effectiveness of flipped classrooms in these disciplines can provide valuable insights for educators in medical schools worldwide. A substantial number of high-quality studies from China align closely with the needs of our research, which is why we included a relatively large proportion of studies from China. However, this inevitably affects the comprehensiveness and objectivity of our findings, and further high-quality international studies are needed to validate our conclusions.
4.3 Implications for future research
This study highlights the promising application of the flipped classroom model in clinical medical education. Indeed, numerous innovative teaching methods have demonstrated advantages over traditional approaches. With the ongoing reform and evolution of educational models, methodologies such as problem-based learning (PBL), case-based learning (CBL), and team-based learning (TBL) have been implemented in medical education and have garnered positive feedback. For instance, one study indicated that the integration of the flipped classroom and PBL methods proved to be more effective than traditional teaching in the context of hyperthyroidism instruction during endocrinology clerkships (Hu et al., 2019). One study indicated that a combined approach utilizing the flipped classroom and case-based learning (CBL) effectively complemented medical morphology instruction (Hu et al., 2023). Research has also demonstrated that integrating the flipped classroom with team-based learning (TBL) is widely regarded as an advantageous strategy in the training of clinical interns, particularly in enhancing students’ clinical competencies with significant benefits (Shuai et al., 2023). Thus, the integration of various teaching methods with the flipped classroom model may yield synergistic effects, suggesting that “1 + 1 > 2.” Further experimental research is needed to investigate the full potential of the flipped classroom teaching model.
5 Conclusion
The numerous advantages of the flipped classroom teaching model have contributed to its growing adoption in medical education globally. This study conducted an initial evaluation of the effectiveness of the flipped classroom model within clinical medical education. The findings indicated that the flipped classroom approach was more effective than traditional teaching in enhancing students’ theoretical knowledge, clinical skills, and overall competencies, although it did not demonstrate a significant advantage in terms of student satisfaction. This meta-analysis underscores the urgent need to promote the flipped classroom teaching method within clinical medical education to enhance the medical literacy of students. However, as discussed, the limitations of this study highlight the necessity for additional high-quality research with larger sample sizes across diverse educational contexts to further corroborate these findings. Additionally, implementing a blended teaching methodology that integrates various innovative teaching approaches within the flipped classroom framework is both feasible and essential.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
X-YS: Writing – original draft, Writing – review & editing. QY: Writing – review & editing. Q-WW: Writing – review & editing. B-RL: Writing – review & editing. G-XL: Writing – review & editing. S-HH: Writing – review & editing. Z-GS: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Research Project on Undergraduate Teaching Reform in Higher Education in Shandong Province (Grant No. M2023352), Shandong First Medical University Campus Education and Teaching Reform Research Project Approval Project in 2022 (Grant No. XM2022159) and Shandong First Medical University Course Ideological and Political Education Research Project in 2024 (No. KZ2024014 and No. KZ2024015).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Alabiad, C. R., Moore, K. J., Green, D. P., Kofoed, M., Mechaber, A. J., and Karp, C. L. (2020). The flipped classroom: an innovative approach to medical education in ophthalmology. J. Acad. Ophthalmol. 12, e96–e103. doi: 10.1055/s-0040-1713681
Bishop, J, Verleger, M, Aeronautical, ER, and Beach, D. (2013). The flipped classroom: a survey of the research. 2013 ASEE annual conference exposition proceedings
Cao, Y. X., Xia, S. L., Zhu, Z. Y., Zeng, F. R., Li, H. N., Zhang, T. T., et al. (2023). Exploring lemology teaching with “internet plus” flipped classroom pedagogy. BMC Med. Educ. 23:341. doi: 10.1186/s12909-023-04309-x
Chan, E., Botelho, M. G., and Wong, G. T. C. (2021). A flipped classroom, same-level peer-assisted learning approach to clinical skill teaching for medical students. PLoS One 16:e0258926. doi: 10.1371/journal.pone.0258926
Chen, F., Lui, A. M., and Martinelli, S. M. (2017). A systematic review of the effectiveness of flipped classrooms in medical education. Med. Educ. 51, 585–597. doi: 10.1111/medu.13272
Chiu, H. Y., Kang, Y. N., Wang, W. L., Huang, H. C., Wu, C. C., Hsu, W., et al. (2018). The effectiveness of a simulation-based flipped classroom in the Acquisition of Laparoscopic Suturing Skills in medical students—a pilot study. J. Surg. Educ. 75, 326–332. doi: 10.1016/j.jsurg.2017.07.007
Egger, M., Smith, G. D., Schneider, M., and Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634. doi: 10.1136/bmj.315.7109.629
El-Miedany, Y., El-Gaafary, M., El-Aroussy, N., and Youssef, S. (2019). Flipped learning: can rheumatology Lead the shift in medical education? Curr. Rheumatol. Rev. 15, 67–73. doi: 10.2174/1573397114666180416170156
Freeman, S., Eddy, S. L., McDonough, M., Smith, M. K., Okoroafor, N., Jordt, H., et al. (2014). Active learning increases student performance in science, engineering, and mathematics. Proc. Natl. Acad. Sci. USA 111, 8410–8415. doi: 10.1073/pnas.1319030111
Gong, L, and Dong, R. The application of cooperative learning in English study. In Proceedings of the 6th international conference on electronic, mechanical, information and management society 2016; 1062–1064. doi: 10.2991/emim-16.2016.218
Granero Lucchetti, A. L., Ezequiel, O., de Oliveira, I. N., Moreira-Almeida, A., and Lucchetti, G. (2018). Using traditional or flipped classrooms to teach “geriatrics and gerontology”? Investigating the impact of active learning on medical students’ competences. Med. Teach. 40, 1248–1256. doi: 10.1080/0142159X.2018.1426837
Gutiérrez-González, R., Zamarron, A., Royuela, A., and Rodriguez-Boto, G. (2023). Flipped classroom applied to neurosurgery in undergraduate medical education. BMC Med. Educ. 23:170. doi: 10.1186/s12909-023-04158-8
Guyatt, G. H., Oxman, A. D., Montori, V., Vist, G., Kunz, R., Brozek, J., et al. (2011). GRADE guidelines: 5. Rating the quality of evidence—publication bias. J. Clin. Epidemiol. 64, 1277–1282. doi: 10.1016/j.jclinepi.2011.01.011
Higgins, J. P. T., Altman, D. G., Gotzsche, P. C., Juni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. doi: 10.1136/bmj.d5928
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Hu, R., Gao, H., Ye, Y., Ni, Z., Jiang, N., and Jiang, X. (2018). Effectiveness of flipped classrooms in Chinese baccalaureate nursing education: a meta-analysis of randomized controlled trials. Int. J. Nurs. Stud. 79, 94–103. doi: 10.1016/j.ijnurstu.2017.11.012
Hu, X. M., Li, Z. X., Deng, J., Han, Y., Lu, S., Zhang, Q., et al. (2023). Integration of theory and practice in medical morphology curriculum in postgraduate training: a flipped classroom and case-based learning exercise. Curr. Med. Sci. 43, 741–748. doi: 10.1007/s11596-023-2759-9
Hu, X., Zhang, H., Song, Y., Wu, C., Yang, Q., Shi, Z., et al. (2019). Implementation of flipped classroom combined with problem-based learning: an approach to promote learning about hyperthyroidism in the endocrinology internship. BMC Med. Educ. 19:290. doi: 10.1186/s12909-019-1714-8
Jones-Bonofiglio, K. D., Willett, T., and Ng, S. (2018). An evaluation of flipped e-learning experiences. Med. Teach. 40, 953–961. doi: 10.1080/0142159X.2017.1417577
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gotzsche, P. C., Ioannidis, J. P. A., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. doi: 10.1136/bmj.b2700
Lopez, S. Book review–Flip your classroom: reach every student in every class every day by Jonathan Bergmann and Aaron Sams. Electronic journal of social and strategic studies (2022); 3:258–264.
Lu, F., Luo, Z., Huang, T., Lv, X., Wang, H., Wang, Y., et al. (2024). Effectiveness evaluation of flipped classroom in emergency medicine online teaching for medical undergraduates. Med. Teach. 46, 689–696. doi: 10.1080/0142159X.2023.2273780
Mehta, N. B., Hull, A. L., Young, J. B., and Stoller, J. K. (2013). Just imagine: new paradigms for medical education. Acad. Med. 88, 1418–1423. doi: 10.1097/ACM.0b013e3182a36a07
Ministry of Education, Ministry of Health. (2008). Notice on the issuance of "undergraduate medical education standards — clinical medicine program (trial)" by the Ministry of Education and the Ministry of Health. Gazette of the Ministry of Health of People’s republic of China. 12, 27–37
Morgan, H., McLean, K., Chapman, C., Fitzgerald, J., Yousuf, A., and Hammoud, M. (2015). The flipped classroom for medical students. Clin. Teach. 12, 155–160. doi: 10.1111/tct.12328
Prober, C. G., and Heath, C. (2012). Lecture halls without lectures--a proposal for medical education. N. Engl. J. Med. 366, 1657–1659. doi: 10.1056/NEJMp1202451
Prober, C. G., and Khan, S. (2013). Medical education reimagined. Acad. Med. 88, 1407–1410. doi: 10.1097/ACM.0b013e3182a368bd
Rui, Z., Lian-rui, X., Rong-zheng, Y., Jing, Z., Xue-hong, W., and Chuan, Z. (2017). Friend or foe? Flipped classroom for undergraduate electrocardiogram learning: a randomized controlled study. BMC Med. Educ. 17:53. doi: 10.1186/s12909-017-0881-8
Shiau, S., Kahn, L. G., Platt, J., Li, C., Guzman, J. T., Kornhauser, Z. G., et al. (2018). Evaluation of a flipped classroom approach to learning introductory epidemiology. BMC Med. Educ. 18:63. doi: 10.1186/s12909-018-1150-1
Shuai, L., Huiwen, W., Shihao, D., and Li, J. (2023). The application of flipped classroom combined with team-based learning in the orthopedic clinical teaching. Medicine (Baltimore) 102:e35803. doi: 10.1097/MD.0000000000035803
Sterne, J. A. C., Sutton, A. J., Ioannidis, J. P. A., Terrin, N., Jones, D. R., Lau, J., et al. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002. doi: 10.1136/bmj.d4002
Tang, F., Chen, C., Zhu, Y., Zuo, C., Zhong, Y., Wang, N., et al. (2017). Comparison between flipped classroom and lecture-based classroom in ophthalmology clerkship. Med. Educ. Online 22:1395679. doi: 10.1080/10872981.2017.1395679
Tucker, B. The flipped classroom: Online instruction at home frees class time for learning. Education Next 12:82. Available at: https://api.semanticscholar.org/CorpusID:220762283
Tune, J. D., Sturek, M., and Basile, D. P. (2013). Flipped classroom model improves graduate student performance in cardiovascular, respiratory, and renal physiology. Adv. Physiol. Educ. 37, 316–320. doi: 10.1152/advan.00091.2013
Xu, P., Chen, Y., Nie, W., Wang, Y., Song, T., Li, H., et al. (2019). The effectiveness of a flipped classroom on the development of Chinese nursing students’ skill competence: a systematic review and meta-analysis. Nurse Educ. Today 80, 67–77. doi: 10.1016/j.nedt.2019.06.005
Yang, C., Zhou, Z. W., Jin, L., Jiang, L., and Han, S. J. (2023). Emergency medicine education via the micro-course and flipped classroom-reform of medical education during the COVID-19 pandemic. Medicine (Baltimore) 102:e36459. doi: 10.1097/MD.0000000000036459
Keywords: clinical medicine, flipped classroom, FC, traditional classroom, TC, education
Citation: Shi X-Y, Yin Q, Wang Q-W, Lu B-R, Li G-X, Huang S-H and Sun Z-G (2025) Is the flipped classroom more effective than the traditional classroom in clinical medical education: a systematic review and meta-analysis. Front. Educ. 9:1485540. doi: 10.3389/feduc.2024.1485540
Edited by:
Mei Tian, Xi’an Jiaotong University, ChinaReviewed by:
Jürgen Schlegel, Technical University of Munich, GermanyLei Qi, The First Affiliated Hospital of Xi’an Jiaotong University, China
Copyright © 2025 Shi, Yin, Wang, Lu, Li, Huang and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhi-Gang Sun, c3Vuc3pnQDEyNi5jb20=; Shu-Hong Huang, c2h1aG9uZ2h1YW5nQHNkZm11LmVkdS5jbg==
 Xu-Ying Shi
Xu-Ying Shi Qing Yin2
Qing Yin2 Guo-Xiang Li
Guo-Xiang Li Shu-Hong Huang
Shu-Hong Huang Zhi-Gang Sun
Zhi-Gang Sun