
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Comput. Sci., 30 November 2022
Sec. Human-Media Interaction
Volume 4 - 2022 | https://doi.org/10.3389/fcomp.2022.926649
This article is part of the Research TopicInbodied InteractionView all 6 articles
Introduction: A goal of inbodied interaction is to explore how tools can be designed to provide external interactions that support our internal processes. One process that often suffers from our external interactions with modern computing technology is our breathing. Because of the ergonomics and low-grade-but-frequent stress associated with computer work, many people adopt a short, shallow breathing pattern that is known to have a negative effect on other parts of our physiology. Breathing guides are tools that help people match their breathing patterns to an external (most often visual) cue to practice healthy breathing exercises.However, there are two leading protocols for how breathing cues are offered by breathing guides used in non-clinical settings: simple paced breathing (SPB) and Heart Rate Variability Biofeedback (HRV-b). Although these protocols have separately been demonstrated to be effective, they differ substantially in their complexity and design. Paced breathing is a simpler protocol where a user is asked to match their breathing pattern with a cue paced at a predetermined rate and is simple enough to be completed as a secondary task during other activities. HRV-b, on the other hand, provides adaptive, real-time guidance derived from heart rate variability, a physiological signal that can be sensed through a wearable device. Although the benefits of these two protocols have been well established in clinical contexts, designers of guided breathing technology have little information about whether one is better than the other for non-clinical use.
Methods: To address this important gap in knowledge, we conducted the first comparative study of these two leading protocols in the context of end-user applications. In our N=28 between-subject design, participants were trained in either SPB or HRV-b and then completed a 10-minute session following their training protocol. Breathing rates and heart rate variability scores were recorded and compared between groups.
Results and discussion: Our findings indicate that the exercises did not significantly differ in their immediate outcomes – both resulted in significantly slower breathing rates than their baseline and both provided similar relative increases in HRV. Therefore, there were no observed differences in the acute physiological effects when using either SPB or HRV-b. Our paper contributes new findings suggesting that simple paced breathing – a straightforward, intuitive, and easy-to-design breathing exercise – provides the same immediate benefits as HRV-b, but without its added design complexities.
Guided breathing exercises – where the breath is actively controlled – have been shown to lead to both immediate and long-term benefits for health, including reduction in the symptoms of chronic stress (Kennedy and Parker, 2018), lower blood pressure in individuals with hypertension (Schein et al., 2001), increased resistance to relapse in depression (Caldwell and Steffen, 2018), increased effectiveness of substance dependence treatments (Eddie et al., 2015), and increased cognitive executive functioning (Prinsloo et al., 2011; Sutarto et al., 2013). Guided breathing exercises work because our breathing influences the state of our body. When we control our breath, we create change throughout the entire body, which, like other forms of exercise, can positively benefit health and wellness.
Given the documented health benefits observed during clinical use (see Gevirtz, 2013 for a review), it is not surprising that many commercial products have been developed to support guided breathing exercises outside of clinical settings. For example, clinically backed guided breathing tools such as HeartMath's EmWave1 and MindMedia's BioTrace+2 (Figure 1-left) are marketed based on the promise of health benefits that can be achieved with continued use. Similarly, a wide variety of breathing guides are readily available at minimal cost on mobile app stores (e.g., casual use by healthy individuals is not well understood. To address this gap in knowledge, we compare the relative effectiveness of the two most prominent protocols used in existing guided breathing technologies: heart rate variability biofeedback (HRV-b) – a comparatively more complex protocol that employs real-time sensing and feedback to guide breathing – and, paced breathing – a simpler protocol that guides breathing in a consistent and rhythmic pattern (that is not based upon sensed physiological data). Although research has established that HRV-b may be more effective in clinical contexts (Brown and Gerbarg, 2005; Logtenberg et al., 2007; Gevirtz, 2013; Critchley et al., 2015; Ma et al., 2017; Russell et al., 2017; Steffen et al., 2017), it is not yet well-understood how the effectiveness of each protocol differs during casual use and, in turn, how best to balance any differences in effectiveness with each protocol's inherent differences in design complexity.
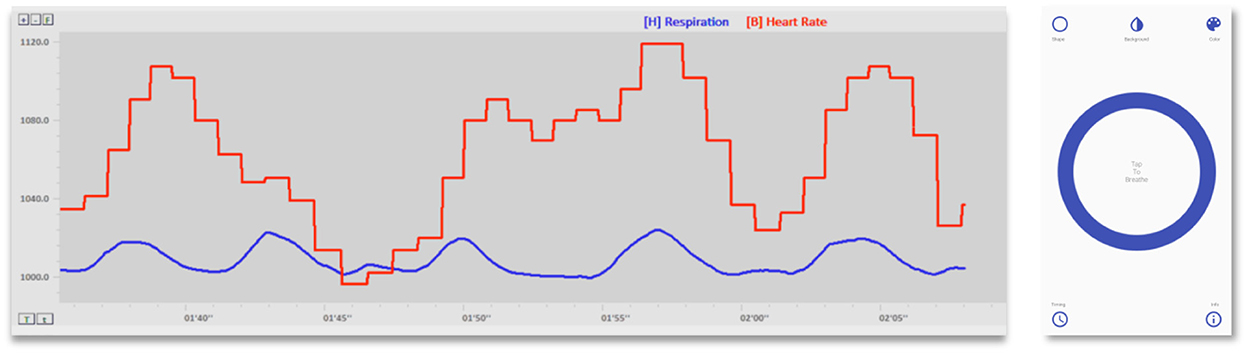
Figure 1. Commercially available Heart Rate Variability Biofeedback (HRV-b) and Paced Breathing tools. (Left) Biotrace+ Clinical HRV-b Software (Mind Media): Clinical populations align their breathing (blue) with a real-time representation of their heart rate (red), with the goal of creating smooth, large waves in their heart rate signal. (Right) Breathe Easy (Mood Tools): Users time their inhales and exhales with the rhythmic expansion and contraction of the onscreen circle (blue). This app employs a simple paced breathing protocol – users select a constant, predetermined breathing rate at the start of each session.
Heart rate variability biofeedback works by using a sensing technology (such as ECG) to capture changes in heart rate variability (i.e., HRV - a measure of the natural variations in timing between consecutive heart beats; Shaffer et al., 2014). HRV-b systems typically use a visual representation to show the user how their heart rate rises and falls in relation to their breathing (see Figure 1-left). The user is instructed to align their inhalations with increases in their heart rate, and exhalations with decreases in their heart rate. Although this may initially seem abstract, with some guidance and practice, and because changes in heart rate are relatively rhythmic, users can typically learn to follow HRV-b guidance quickly. This specific process amplifies HRV and is believed to maximize physiological benefits (Lehrer, 2013; Lehrer and Gevirtz, 2014). The HRV-b protocol is described in greater detail below.
In contrast, paced breathing is somewhat simpler. A paced breathing system provides a rhythmic guidance cue. For example, this cue could be a circle displayed on a mobile phone that slowly and rhythmically grows and shrinks; users breathe in as the circle grows and breathe out as the circle shrinks (Figure 1-right). Importantly, paced breathing systems do not typically use a sensing technology to provide adaptive guidance, everyone gets the same guidance based on a pre-determined breathing rate (typically, six breaths per minute, Eddie et al., 2015). This is believed to work for a similar reason as HRV-b, as breathing in a slow rhythmic way approximates the beneficial physiological conditions created by HRV-b.
The main distinction between these approaches is that HRV-b is adaptive and paced breathing is not. However, to provide this adaptivity, HRV-b requires both a sensing technology to collect heartbeat data and close attention for users to observe and adapt their breathing in real time. Paced breathing does not have these requirements, and because it is static and predictable, it has been suggested that it can even be practiced while performing other tasks; for example, during information work (Moraveji et al., 2011; Ghandeharioun and Picard, 2017; Tabor et al., 2021) or while driving (Paredes et al., 2018).
Importantly, there are clear differences in how systems that support either HRV-b or paced breathing can be designed. However, it has not been established whether the added complexity of HRV-b translates to greater physiological benefit in non-clinical settings. For clinical populations, HRV-b has often been treated as the gold standard because it provides the real-time, full-resolution biofeedback with which to align breathing (Lehrer and Gevirtz, 2014). This may not necessarily be the case during non-clinical use of breathing exercises (e.g., commodity grade sensors may not be capable of providing adequate feedback; untrained users may not be able to fully operationalize the feedback provided), which leads to a key gap in design knowledge. On the one hand, if the “cheaper and easier” paced breathing protocol leads to benefits that are comparable with HRV-b in this context, designers could rely on a much simpler protocol when integrating breathing exercise into their tools without the need for specialized equipment. On the other hand, if HRV-b holds clear benefit above and beyond paced breathing, designers and users may accept the additional overheads of HRV-b, deeming them necessary to receive the maximum benefit for their time and effort.
In our work, we present the first study that directly compares the acute physiological benefits of paced breathing with HRV-b in a non-clinical setting. In a between-subjects study consisting of 28 participants, we demonstrate that both exercises created measurable physiological markers of benefit, and that the magnitude of these effects do not differ significantly between the two exercises. That is, both exercises led to comparable decreases in respiration rate and increases in heart rate variability, which are the immediate goals of the exercises.
Our findings suggest that, in non-clinical use cases, the simpler paced breathing exercise is as an effective alternative to HRV-b. Although our current work does not examine longer-term positive health effects achieved through continued practice, our findings can immediately inform the design of guided breathing technologies that target the acute benefits of guided breathing exercise. Our work provides new directions for future research in the design of technology that supports breathing exercise for everyday use. Further, we provide essential information for the design of inbodied interactions (schraefel, 2020) that leverage breathing as a means to “tune” our physiological processes for positive health benefits (schraefel, 2020).
We organize our related work by first presenting relevant background on the physiology of guided breathing exercises, then summarizing previous research in HCI that has explored the design of tools that make use of breathing and heart rate variability sensing and systems that provide support for guided breathing exercise.
Our heart is often conceptualized as beating in a constant and uniform pattern. However, in reality, the beat-to-beat timing between each successive heartbeat varies – a phenomenon known as heart rate variability (HRV). In the context of breathing exercises, HRV is often visualized as the waveform created by plotting a sequence of rr-intervals – the elapsed time in milliseconds between each pair of consecutive heart beats (Shaffer et al., 2014). In the remainder of this paper, we refer to this representation of HRV as a heart rate wave, which is visible in Figure 1-left, but described in greater detail in Figure 3.
Heart rate variability occurs because our heart rate is governed by many physiological processes that are frequently in contention with one another. Respiratory sinus arrhythmia (RSA) and the baroreflex are two of these processes relevant to guided breathing exercise. RSA causes our heart rate to oscillate in unison with our breathing – inhales lead to faster heart beats to streamline gas exchange, whereas exhales lead to slower heart beats to conserve energy as the lungs expel spent fuel (Yasuma and Hayano, 2004). RSA oscillations occur at an individual's current breathing rate, which typically range from 8 to 24 cycles per minute during spontaneous (i.e., unguided/natural) breathing (Calais-Germain, 2006). Conversely, the baroreflex causes our heart rate to oscillate in a way that maintains a stable blood pressure (i.e., a negative feedback loop) (Chapleau, 2012). Although the exact rate varies by individualized traits such as height, weight, and gender, baroreflex oscillation typically occur proximate to six cycles per minute (Lehrer, 2013).
Research has demonstrated that, with sustained practice, guided breathing exercise can lead to a wide range of health and wellness benefits (e.g., a survey of documented benefits is presented in Gevirtz, 2013). As is the case with many forms of exercise, these benefits are contingent on the effectiveness of each practice session, which is characterized by the creation of high-amplitude, low-frequency oscillations in HRV (Lehrer and Gevirtz, 2014). This is accomplished by slowing the breathing to match the frequency of the baroreflex, which causes the influences of the RSA and baroreflex to come into alignment and resonate (see Figure 3). Although the theoretical underpinnings of why this leads to health and wellness benefits is beyond the scope of the current paper, a detailed explanation can be found in Lehrer and Gevirtz (2014), Eddie et al. (2015), or Tabor et al. (2019).
Due in part to the physiological benefits attainable through breathing exercise, many technology-mediated breathing guides have been developed. As outlined in the remainder of this section, it is common for designs to target either a heart rate variability biofeedback (HRV-b) or simple paced breathing (SPB) protocol – often motivating the added complexity of HRV-b based on the promise of more fully realizing exercise benefits.
Heart rate variability biofeedback (HRV-b) is often considered the gold-standard slow breathing exercise in clinical settings (Lehrer et al., 2000; Gevirtz, 2013; Lehrer, 2013). Originally designed as a clinical exercise for reducing blood pressure in people with hypertension (Lehrer et al., 2000), HRV-b uses visual feedback to display the patient's heart rate wave, breathing rate, and other physiological signals in real time (Lehrer, 2013; Lehrer and Gevirtz, 2014) (visible in Figure 1-left). Supported by guidance and instruction from a trained clinician, the patient uses this feedback to align their breathing with the on-screen heart rate wave to create the desired high-amplitude, low-frequency waveform (Lehrer, 2013; Shaffer et al., 2014; Steffen et al., 2017).
Since its inception, HRV-b has been demonstrated to be both an effective standalone and supplemental treatment of a wide range of adverse conditions and illnesses (Gevirtz, 2013). In addition to clinical use, commercially available tools now exist that allow HRV-b to be also used in non-clinical settings (e.g., BreatheSync3, HeartMath EmWave4). Adaptations of the exercise have also been proposed in research including the use of different modalities of feedback (Weffers and Alina, 2010; Bergstrom et al., 2014; Yu and Song, 2015; Yu et al., 2015, 2018a,b,c; Frey et al., 2018) and even into more engaging game-like settings (Kuikkaniemi et al., 2010; Al Rihawi et al., 2014; Qin et al., 2014; Sonne and Jensen, 2016; Patibanda et al., 2017; Sonne et al., 2017).
Many of these HRV-based designs motivate the added protocol complexity based on the promise of maximizing exercise benefits. However, despite its effectiveness, HRV-b has several limitations that prevent it from being a widely accessible and easily deployable exercise. While the biofeedback provided in HRV-b helps people breathe in a way that maximizes physiological effects (known as one's coherent or resonant frequency breathing rate, which generally ranges between 4.5 and 6.5 bpm, Lehrer, 2013), this feedback is derived from real-time sensor readings. This means that users are required to wear a sensor when practicing the exercise. For example, the EmWave5 system uses a smartphone attached PPG ear-clip to monitor HRV, providing biofeedback visualizations during exercise. Further, focused attention is required to continuously monitor and respond to real-time changes in physiology, which means HRV-b is best practiced while solely focused on the exercise (and would be difficult to sustain while actively engaged in another work task). Although HRV sensing has also recently been shown to be achievable using the camera and flash on a mobile phone (Plews et al., 2017; Bánhalmi et al., 2018), (i.e., bypassing the need for external/dedicated sensors), users still must actively use the sensor and focus on adapting their breathing to the provided feedback (e.g., BioZen, 2019; Breathmix - Biofeedback Breath Pacer, 2019; HRV Biofeedback, 2019).
In an attempt to mitigate the design complexities inherent to HRV-b, research has suggested that simpler breathing exercises – that do not exhibit the attentional or real-time sensing requirements of HRV-b – can still lead to physiological benefits. For example, Song and Lehrer (2003) found that regulated breathing at 6.0 bpm (irrespective of each participant's “optimal” breathing rate identified through HRV-b) led to the desirable exercise effects. This is an important finding for the design of technology-mediated breathing guides as it suggests that the benefits of these exercises may be attainable without the requirements for real-time sensing and constant attention that accompany HRV-b. Conversely, however, a study conducted by Steffen et al. (2017) suggests that breathing exactly at one's individualized resonance frequency is critical for the full benefits of guided breathing exercise to occur. In this study, the magnitude of exercise benefits was diminished when breathing rates deviated from resonance frequency by as little as one breath-per-minute (Steffen et al., 2017). This conflicting evidence is a key motivator for our study and is likely a contributing factor to the prevalence of both HRV-b and SPB protocols in current guided breathing technologies. In our research, we aim to better understand the relative effectiveness and design tradeoffs between these two protocols during non-clinical use.
To date, many guided breathing system designs have been proposed both in research and commercially. Although these designs employ a wide variety of guiding approaches and stimulus modalities, these systems can largely be organized into two categories according to the underlying exercise protocol employed (i.e., HRV-b or SPB). Table 1 presents an illustrative sample of the wide variety of existing breathing guide designs. We organize this table by guidance protocol (i.e., whether the design employed HRV-b, SPB, or both), intended salience (i.e., whether the design was intended to require active user focus or serve as a subtle ambient/environmental cue), target setting (i.e., whether the design was intended for general-purpose relaxation or was tailored for a specific setting such as information work), and stimulus modality (i.e., whether the employed visual, auditory, haptic, or a combination of guidance stimuli). Although research has presented designs that satisfy many different configurations of these design parameters to date, there is still little information about how these designs compare in utility and effectiveness. We believe that studying how the influence of factors such as salience, setting, and modality influence (such as our work comparing different guidance modalities in an office environment, Tabor et al., 2021) will uncover valuable findings for the design of breathing exercise technologies.
The use of sensed breathing and heart rate variability has a lengthy history in HCI research. We organize our presentation of HCI research employing breathing (or breathing rate) and heart rate (or heart rate variability) around the four main motivations for the use of these physiological signals: (1) to identify user state, (2) as an input to control interactive systems, (3) to support mindfulness practices, and (4) to support therapeutic exercise.
Physiological input, in general, has received growing attention from the HCI community as sensors become commoditized and more reliable. Heart rate, HRV, and respiration have been explored for some time to identify user state in HCI such as, stress, fatigue, and anxiety (see Cowley et al., 2016 for a review). The motivation for identifying state is that, with an understanding of state, systems can adapt their behavior to best suit the user (Rowe et al., 1998). For example, Spire6 monitors breathing rate during normal daily activities through a wearable stone and alerts user with real-time coping strategies when “stressful” breathing patterns are detected.
Breathing has been widely used for direct control of interactive systems. Much of the work that leverages breath as an input modality has involved blowing (by forcefully pushing air out) for general computer control or control of assistive devices. Notably, sip-and-puff interfaces (which operate using both the intake and exhalation of air) have been used to control powered wheelchairs for many years (for example, to assist those with a cervical injury, Fehr et al., 2000). Additionally, sip-and-puff interfaces have been developed for the control of mouse pointers (Kitto and Bellingham, 1993) and music players (Jones et al., 2008) with accessibility applications in mind.
Research has also explored the use of blowing as an additional input channel for general computer use. Patel and Abowd (2007) demonstrated the use of commodity microphones to create “BLUIs” (Blowable User Interfaces). Breathing has been explored more frequently for entertainment applications as a means of improving engagement (e.g., Schnädelbach et al., 2010; Tennent et al., 2011; Sra et al., 2018).
Heart rate and HRV have been explored less frequently to control interactive systems. Unlike with breathing, we have very little direct volitional control over our heart rate7. Nacke et al. (2011) generalize this difference and draw a distinction between direct (e.g., breathing) and indirect (e.g., heart rate or HRV) sources of physiological input, stating that, in games, direct physiological sensors can be mapped to actions in a virtual world, while indirect sensors are better suited to alter features in the game world rather than as a control (e.g., influencing music or lighting). In agreement, Kuikkaniemi et al. (2010) found that direct physiological controls (e.g., breathing or muscle input) benefited player experience, while indirect (i.e., heart rate) did not. Furthermore, while we largely have some degree of control over breathing, Marshall et al. (2011) point out that it can also be involuntary in certain situations, and this can be leveraged for thrilling experiences (e.g., they mapped the control of a mechanical bull's movements to breathing). In a different application of indirect physiological input, Stach et al. (2009) found that scaling game difficulty according to heart rate in exergames was an effective means for balancing competition between players of different physical abilities.
HCI research has also explored the relationship between breathing and heart rate in activities for mindfulness. Inspired by yogic practice, Patibanda et al. (2017) and Zhu et al. (2017) explored tools designed to develop breathing awareness inspired by mindfulness activities. Similarly, Roo et al. (2017) provide indirect biofeedback of “cardiac coherence” in a playful activity meant to support mindfulness through directed focus on the breath. See Terzimehić et al. (2019) for a full review of HCI research into mindfulness.
Although these projects illustrate the common connection made between practices of mindfulness and the breath, guided breathing can also be considered and practiced independently from meditation or mindfulness practices. In meditation, the breath is both a convenient and complimentary object to direct attention toward during meditation (i.e., since our breath is readily available to us at all times, and is tightly coupled with our heart rate and autonomic state) – we can volitionally alter our breathing without meditating, and we can practice meditation by directing attention toward objects other than our breath (e.g., toward various body parts during a “body-scan” meditation, Terzimehić et al., 2019). Furthermore, in this study, we focus strictly on the physiological effects of guided breathing, and therefore do not explore the many important psychological factors at play in both meditation and mindfulness practices.
HCI researchers have also focused on the potential physiological and therapeutic benefits of breathing exercises. In many cases, this research has focused on improving user engagement by incorporating game-like elements into existing forms of breathing exercise. For example, Sonne and Jensen (2016) found that their breathing game for children with ADHD had consistent effects on HRV compared to traditional breathing focused exercises and was much preferred as an activity. Rovers et al. (2009) have synthesized the design lessons that have been uncovered through such games and provide a model to assist in the design of biofeedback games more generally.
HCI has also focused on designing technology that facilitates the integration of therapeutic breathing exercise into everyday life, and several recent projects have looked at various ways to provide paced guidance for breathing using visual cues and sounds (Moraveji et al., 2011; Moraveji and Soesanto, 2012). The results of this work suggest that while people could successfully follow paced breathing cues during information work, they quickly returned to normal breathing when the cues were removed (Moraveji et al., 2011). This research also found evidence that subjective calm was reported as being lower in a visually-paced breathing condition than a sound-paced condition (Moraveji and Soesanto, 2012), suggesting that additional cognitive demands of splitting visual attention between the two tasks “… may counter the calming effects of slow breathing” (Moraveji and Soesanto, 2012). This line of work did not, however, explicitly investigate physiological effects such as HRV.
To summarize, while work on the use of breathing for therapeutic benefit has been motivated by reliable findings and benefits, much of the work described above does not consider whether the adapted breathing activity still led to physiological markers of benefit (with the notable exception of Sonne and Jensen, 2016). In our study, we quantify these physiological markers of benefits to directly compare the effects of two commonly employed protocols for breathing exercise.
Although HRV-b has been proposed as a gold standard in clinical contexts (Brown and Gerbarg, 2005; Logtenberg et al., 2007; Lehrer and Gevirtz, 2014; Critchley et al., 2015; Ma et al., 2017; Russell et al., 2017; Steffen et al., 2017), it is currently unclear if the added complexities of HRV-b translate to increased benefit over simple paced breathing during non-clinical use. To better understand any potential differences in immediate effects between these two exercises, we conducted a between-subject study. We hypothesized that both treatments would create physiological effects [as has been shown many times in previous research (Prinsloo et al., 2011; Critchley et al., 2015; Russell et al., 2017; Steffen et al., 2017)] and, importantly, that the magnitude of those effects would not be significantly different.
Specifically, we proposed three main hypotheses.
First, previous research has established that both SPB (e.g., Song and Lehrer, 2003) and HRV-b (e.g., Eddie et al., 2015) increase HRV scores. We expect our experimental protocol to replicate these outcomes. Thus, we hypothesize that:
• H1: Both breathing exercises will lead to reductions in breathing rate and increases in HRV scores compared to baseline measures.
Second, the key difference between HRV-b and SPB is that the adaptive, real-time feedback provided during HRV-b allows users to further refine their breathing patterns and reach an optimal “resonant frequency breathing rate” (Lehrer, 2013) that maximizes physiological effects. This rate varies according to physical traits such as height, weight, and physical fitness. However, we believe that the influence of these individual differences will be minimal during non-clinical exercise use and, in turn, the physiological effects of our SPB protocol (which only approximates each participant's resonant frequency rate) will be similar to those provided by HRV-b. Thus, we hypothesize that:
• H2: The magnitude of the HRV effects will not be significantly different between HRV-b and SPB (i.e., HRV-b will not lead to significantly larger effects than SPB).
Third, previous research has suggested that the magnitude of HRV effects created is related to baseline state, with larger magnitude effects anticipated in individuals who are “farther out of breathing alignment” to begin with (Kennedy and Parker, 2018). Therefore, in our analysis we also test for correlations between baseline breathing rate and the magnitude of effects created. We hypothesize that:
• H3: Effects will be most pronounced in participants with higher baseline breathing rates (i.e., the magnitude of HRV effects will positively correlate with baseline breathing rate).
Two guided breathing applications were developed in Processing 3.0. Each tool was developed based on examples from published literature on paced breathing (Moraveji et al., 2011; Wongsuphasawat et al., 2012) and HRV-b (Lehrer et al., 2000; Lehrer and Gevirtz, 2014; Eddie et al., 2015). Both tools are publicly available at https://github.com/hcilab/BreathingGuides.
The paced breathing stimulus consisted of a circle with rhythmically oscillating diameter and opacity (Figure 2). Participants were instructed to inhale as the circle increased in size and became darker (Figure 2-left) and exhale as it got smaller and lighter (Figure 2-right). Participants were told that the circle represented the expansion and contraction of their stomach during each cycle of breath, which was calibrated to guide breathing a constant rate of six breaths per minute (i.e., 10-s cycles).
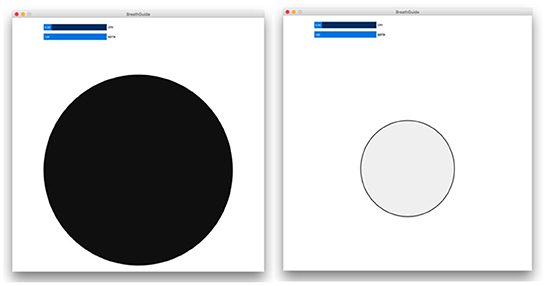
Figure 2. The breath pacing stimulus that guided participants at a constant six breaths per minute breathing rate. Participants were instructed to inhale as the circle grew and became darker (left), and exhale as it got smaller and lighter in color (right).
The heart rate variability biofeedback (HRV-b) tool consisted of a scrolling real-time line graph depicting the participant's heart rate wave. Heart rate was displayed numerically on the vertical-axis of the graph, and the graph presented a 45-s history of the signal. Participants were instructed to align their breathing with the heart rate wave (i.e., the biofeedback) by timing their inhales with the rise of the wave and their exhales with the fall of the wave – with the goal of achieving a heart rate wave with maximal amplitude and smoothness. A detailed description of the coaching cues and instructions are provided in Procedure. Figure 3 depicts the HRV-b tool and illustrates a heart rate wave during normal breathing (left) and during HRV-b (right).
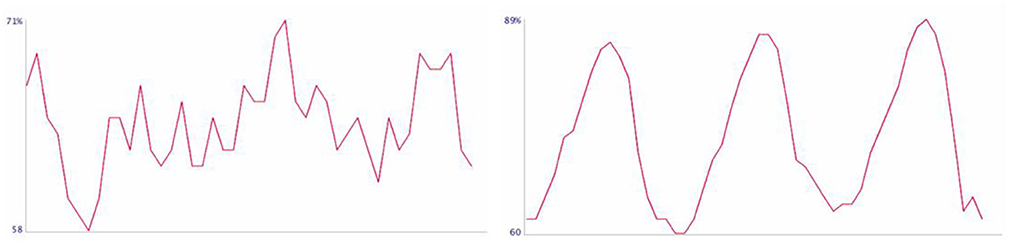
Figure 3. The Heart Rate Variability Biofeedback (HRV-b) tool used during the experiment. The scrolling line graph depicts the most recent 45-s of the user's heart rate wave, with the vertical-axis representing their heart rate derived from each RR interval. (Left) A typical heart rate wave during spontaneous/unguided breathing. (Right) A high-amplitude, low-frequency heart rate wave created by aligning the breath with the feedback during the HRV-b exercise.
Breathing and heart rate variability signals were logged during the experiment. Outcome measures were computed from the two 10-min data logs collected during the baseline and breathing exercise portions of the session (see below).
Respiration was monitored continuously using a nasal thermistor and the BioRadio wireless physiology monitoring kit8. Sensor readings were recorded at 1,000 Hz, smoothed using a sixth-order Butterworth low-pass filter (0.75 Hz, corresponding to 45b pm), and down sampled to 10 Hz for further analysis. Breathing rate was computed by counting zero-crossing occurrences in the respiration signal in each 15-s contiguous data-window of the recording.
RR-intervals were recorded using the Polar H10 chest strap9. As presented above, the goal of guided breathing exercise is to create high-amplitude, low-frequency heart rate waves. In this experiment, we use two standardized outcome measures (Shaffer and Ginsberg, 2017) to characterize these signal qualities from the captured rr-interval log: HRV amplitude – a measure of the height of each wave in beats per minute; and low-frequency HRV power (LF) – a measure of the degree to which the heart rate wave is oscillating in the desired frequency band. HRV amplitude was computed using the opensource heartpy analysis toolkit (van Gent et al., 2019), while LF was computed using the Kubios HRV Analysis Software v3.5 (Tarvainen et al., 2014). Note that, in order to satisfy the statistical requirements of our analysis, a log transformation was applied to measured LF scores (see below).
The experiment was conducted according to the following procedure. A summary of experimental activities is presented in Figure 4.
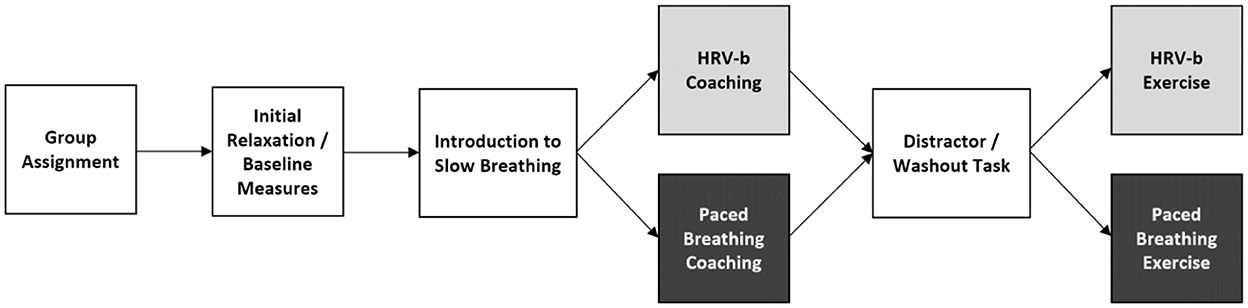
Figure 4. A block diagram summarizing the experiment procedure. White blocks were completed by all participants. Gray blocks were completed by participants assigned to the HRV-b exercise protocol condition, whereas black blocks were completed by those in the Paced Breathing condition.
Each session was 2 h in duration. All participants read and signed an informed consent form before beginning the experiment (UNB REB 2018-112) and withheld from caffeine, tobacco, alcohol, vigorous exercise, and large amounts of food intake in the 3-h preceding the experiment, any of which are known to influence HRV (Shaffer and Ginsberg, 2017). Each participant was assigned to one of two exercise protocol conditions (Paced Breathing or HRV-b) to balance groups by age and gender (since these traits are known to systematically influence HRV, Shaffer and Ginsberg, 2017). The experiment proceeded identically for both groups except for the breathing exercise condition that was completed, as described below.
The session began with physiological sensor placement. The Polar H10 was positioned in the center of the chest according to manufacturer guidelines10, while the nasal thermistor was positioned securely at the base of the nostrils. Once positioned, the experimental data collection began. This began with 10-min of controlled relaxation, during which the participant sat quietly and relaxed with no explicit queues about breathing provided. This allowed breathing and HRV to stabilize and was the 10-min data log used to compute each participant's baseline breathing rate and HRV scores.
Participants received a short introduction to abdominal breathing, which was modeled on published coaching instructions (Lehrer et al., 2000; Calais-Germain, 2006). In this introduction, participants first practiced distinguishing between chest and abdominal breathing by resting their hands on their chest and stomach and feeling each hand rise and fall as they inhaled and exhaled. Once comfortable with abdominal breathing, all participants then practiced slowing their inhales and exhales to a count that approximated six breaths per minute.
Following the introduction, participants were introduced to the specific breathing exercise they had been assigned to, either:
• HRV-b Instructions: Our delivery of HRV-b was based on published best practices for the clinical form of the exercise (Lehrer et al., 2000). Participants in the HRV-b group were given a short introduction to heart rate variability. Specifically, they were told that the timing between each consecutive heartbeat varies, and that this variation is natural, normal, and healthy as it reflects our ability to constantly adapt to the many bodily processes that influence our heart rate at any point in time. To illustrate this, the experimenter opened the HRV-b tool and explained how the scrolling line graph (Figure 5) depicts this variability. Finally, participants were told that the goal of this exercise was to align their breathing with the waves visible in their heart rate wave by breathing in a way that was similar to the practice they had just completed, but slightly adjusting the timing of their breathing to make the waves as big and smooth as possible.
• Paced Breathing Instructions: Participants in the paced breathing group were introduced to the breath pacing guide (Figure 4) and instructed to align their breathing appropriately (as explained in Paced Breathing Guide).
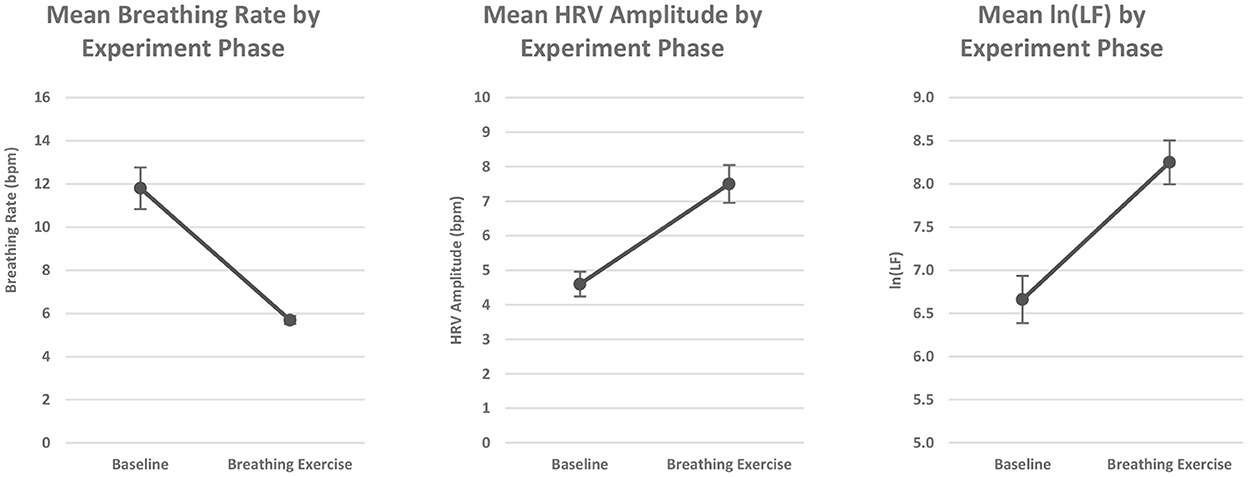
Figure 5. Grand mean outcome measures scores broken down by experiment phase. (Left) Breathing rate; (Middle) HRV amplitude; (Right) ln(LF). Error bars depict standard error of mean (SEM).
Both groups were given several minutes to practice their respective breathing exercises and reminded to breathe in a rhythmic and regular manner through their nose and into their abdomen. Instructions and coaching cues were repeated as necessary.
Before proceeding to the 10-min monitored breathing exercise, participants completed a distractor task to washout any effects from the practice. In this task, participants used a search engine to populate information in a spreadsheet of countries (e.g., population, capital city), which was selected as it is simple, straightforward, easy to explain, and requires active engagement to complete the search queries, which directed attention away from the breath.
Following the distractor task, participants in each group then performed a timed 10-min session of their respective breathing exercises. Outcome measures were computed from the 10-min data log collected during this phase of the experiment. Before beginning, participants were reminded of the exercise protocol, reminded to breathe rhythmically and regularly through their nose and into their abdomen.
A total of 30 participants were recruited for the study. However, two participants were excluded from analysis due to sensor error (i.e., breath sensor receded from nostrils – one participant from each experimental group). This resulted in an analysis composed of 28 participants, 14 per group.
According to established best practice (e.g., Voss et al., 2015), participants were systematically assigned to treatment groups to balance age and sex as sessions occurred. These demographic factors are known to substantially influence baseline HRV. As a result, both groups were composed of six self-reported males and eight self-reported females, with mean age of 40.6 years (SD = 18.9) for the paced breathing group and 38.7 years (SD = 16.3) for the HRV-b group.
All analyses were conducted in JASP 0.10.2. For hypotheses H1 and H2, outcome measures were analyzed using a 2 × 2 repeated measures ANOVA with within-subjects factor experiment phase (baseline, breathing exercise), and between-subjects factor exercise protocol (HRV-b, paced breathing). To satisfy the normality requirements of this analysis, a natural-log transformation was applied to measured LF scores – this outcome measure is presented as ln(LF) throughout the results section below. For hypothesis H3, mean-difference transformed HRV scores were compared with baseline breathing rates using a Pearson correlation analysis. All effects were considered significant for p-values ≤0.05, and no significant interaction effects were detected unless explicitly stated.
T-tests confirm that baseline outcome measures (i.e., breathing rate, ln(LF), and hrv amplitude) were not significantly different between treatment groups (p > 0.25).
Signal profiles are presented in the results section, below. These profiles were generated by iteratively recomputing outcome measures in each contiguous 30-s window of the data log.
We organize results around our experimental hypotheses presented in Section A direct comparison of the acute physiological effects of HRV-b and simple-paced breathing.
In agreement with H1, significant reductions in breathing rate and increases in HRV (both ln(LF) and hrv amplitude) were observed during the breathing exercise phase of the experiment compared to baseline measures. Figure 5 presents a summary of these findings.
ANOVA results indicate a main effect of experiment phase (F1,26 = 41.9, p < 0.01). Grand mean breathing rates were significantly lower when completing the breathing exercises (5.7b pm, SD = 0.99) compared to baseline measures (11.8b pm, SD = 5.1). Figure 5-left presents grand mean breathing rates by experiment phase.
ANOVA results indicate a main effect of experiment phase (F1,26 = 56.9, p < 0.01). Grand mean HRV amplitude was significantly higher during breathing exercise (amplitude = 7.5, SD = 2.9) compared to baseline measures (amplitude = 4.6, SD = 1.9). Figure 5-middle presents grand mean hrv amplitude scores by experiment phase.
ANOVA results indicate a main effect of experiment phase (F1,26 = 81.7, p < 0.01). Grand mean ln(LF) scores were significantly higher during breathing exercise (ln(LF) = 8.3, SD = 1.4) compared to baseline measures (ln(LF) = 6.7, SD = 1.5). Figure 5-right presents grand mean ln(LF) scores by experiment phase.
Observations also support H2 – no significant differences in the magnitude of effects were observed between treatment groups. Figures 6, 7 present a summary of these findings.
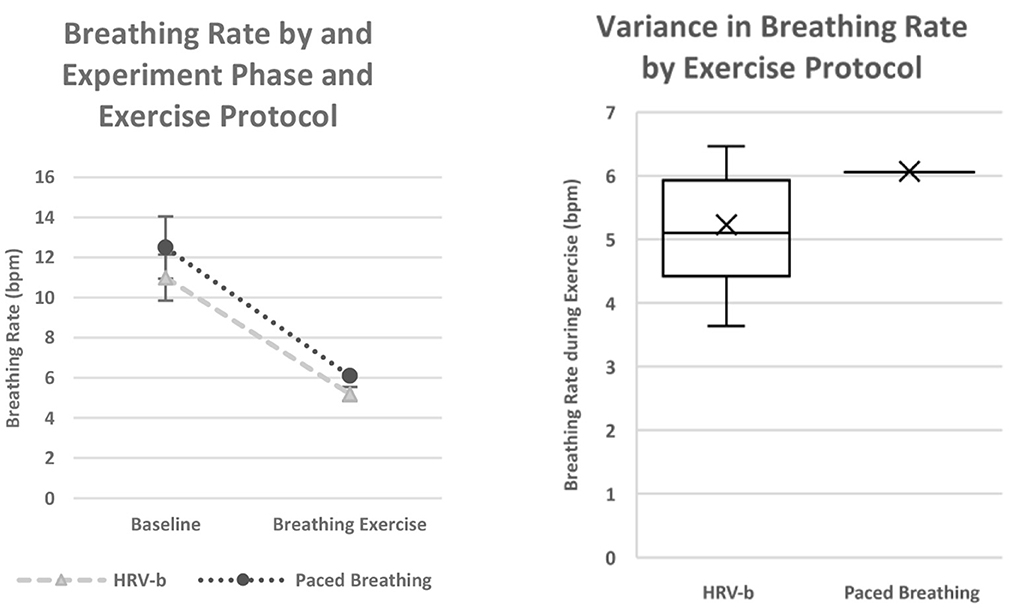
Figure 6. Observed breathing rates during the experiment. (Left) Average breathing rates broken down by experiment phase and exercise protocol. Error bars indicate standard error of mean (SEM). (Right) Per-participant mean breathing rates while completing breathing exercises, broken down by exercise protocol. The box-and-whisker plots denote per-quartile median (i.e., “box” → 25th, 50th, and 75th quartile, “whiskers” → minimum and maximum values). The “X” markers indicate per-protocol mean. A markedly larger variance in breathing rate was observed in the HRV-b group compared to Paced Breathing.
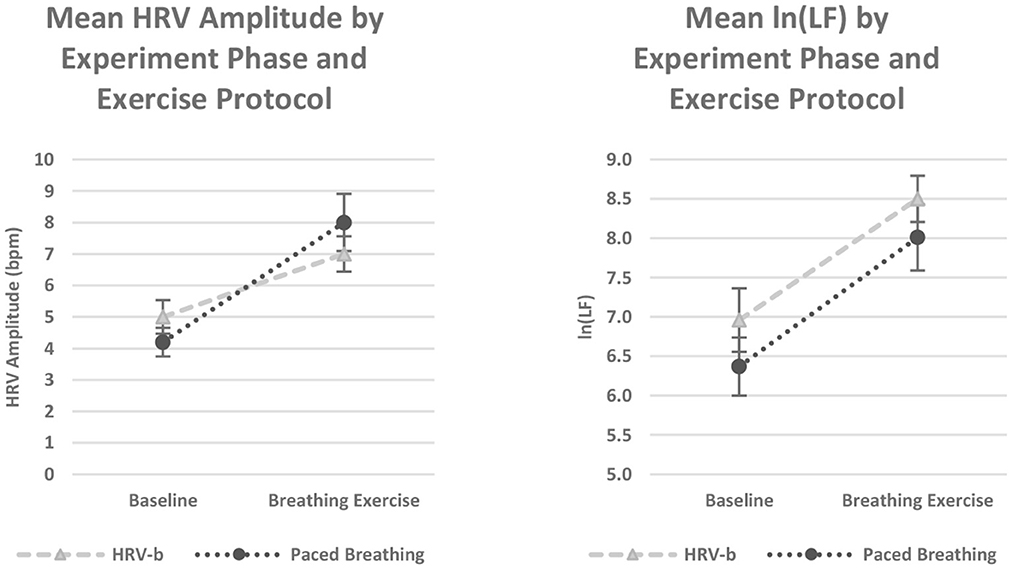
Figure 7. HRV Scores broken down by Experiment Phase and Exercise Protocol (HRV-b – gray dashed lines; Paced Breathing – black dotted lines). (Left) HRV Amplitude; (Right) ln(LF). No significant differences were detected between the two protocols. However, a significant experiment phase x exercise protocol interaction was detected with HRV amplitude. Error bars depict standard error of mean (SEM).
Participants who completed HRV-b achieved reductions in mean breathing rate from 11.0 bpm (SD = 4.3) during baseline down to 5.2 bpm (SD = 1.3) during treatment. Meanwhile, participants who completed paced breathing achieved reductions from a baseline rate of 12.5 bpm (SD = 5.8) down to 6.1 bpm (SD = 0.03) during treatment. ANOVA results were not significant for this comparison (F1,26 = 1.32, p = 0.26). Figure 6-left presents breathing rates by experiment phase and exercise protocol. We interpret these observations as evidence that a comparable reduction in breathing rate was achieved with both breathing exercise protocols.
Although a significant difference in mean breathing rates was not detected between exercise protocols, a markedly higher variance was observed in the HRV-b group compared to Paced Breathing (Figure 6-right). This difference is likely reflective of the key distinction between the two exercise protocols – the paced breathing protocol provided guidance at a predetermined rate of 6.0bpm, whereas the HRV-b feedback did not impose a specific breathing rate during exercise.
Participants who completed HRV-b achieved an increase in hrv amplitude from 5.0 (SD = 2.0) during baseline to 7.0 (SD = 2.1) during the breathing exercise. Meanwhile, participants who completed paced breathing achieved a comparable increase from 4.2 (SD = 1.7) during baseline to 8.0 (SD = 3.4) during the breathing exercise. ANOVA results were not significant for this comparison (F1,26 < 1.0, p = 0.90). Figure 7-left presents hrv amplitude scores by experiment phase and exercise protocol. We interpret these observations as evidence that a comparable increase in hrv amplitude was achieved with both breathing exercise protocols. However, a significant experiment phase * breathing protocol interaction was also detected (F1,26 = 5.5, p = 0.03).
Participants who completed HRV-b achieved an increase in ln(LF) from 7.0 (SD = 1.5) during baseline to 8.5 (SD = 1.1) during the breathing exercise. Meanwhile, participants who completed paced breathing achieved a comparable increase from 6.4 (SD = 1.4) during baseline to 8.0 (SD = 1.6) during the breathing exercise. ANOVA results were not significant for this comparison (F1,26 = 1.18, p = 0.29). Figure 7-right presents ln(LF) scores by experiment phase and exercise protocol. We interpret these observations as evidence that a comparable increase in ln(LF) was achieved with both breathing exercise protocols.
Evidence supports the previously claimed relationship between baseline breathing rate and the magnitude of exercise effects (e.g., Kennedy and Parker, 2018). Our findings suggest that, although all participants were able to align their breathing to the desired frequency, increases in HRV amplitude was more pronounced in individuals with higher baseline breathing rates. A summary of these findings is presented in Figure 8.
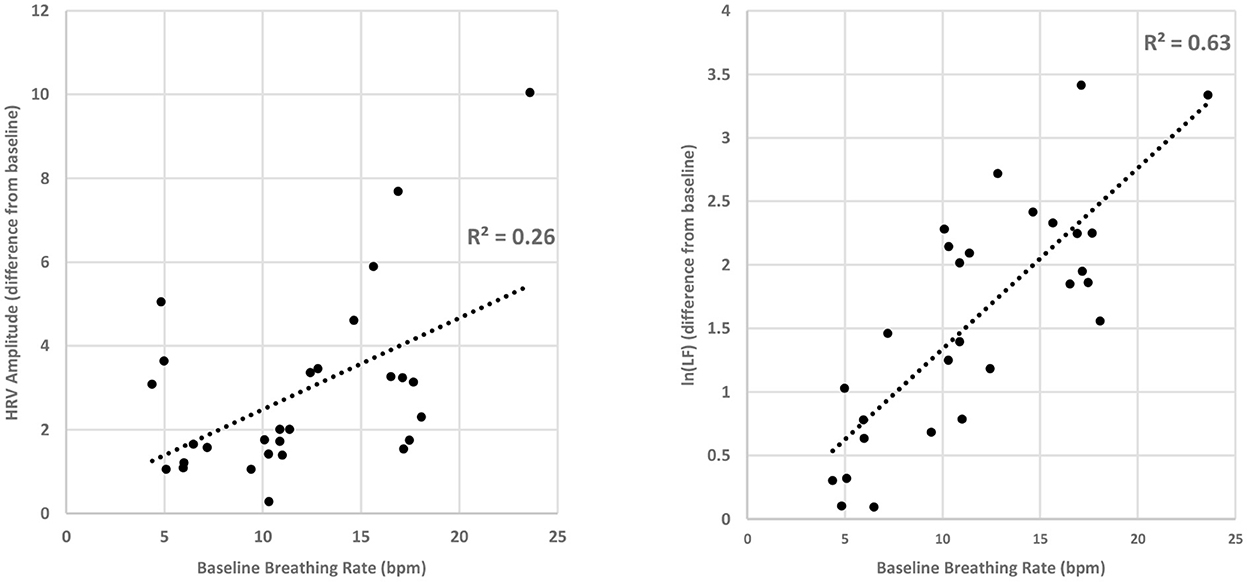
Figure 8. Correlation plots between baseline breathing rates and mean-difference transformed HRV scores. (Left) Mean-difference transformed HRV amplitude by baseline breathing rate. (Right) Mean difference transformed ln(LF) scores by baseline breathing rate. Consistently across both measures of HRV, a significant Pearson correlation was found. This suggests that larger magnitude increases in HRV scores were created by individuals with higher baseline breathing rates.
A significant, positive correlation was found between baseline breathing rate and HRV amplitude (r2 = 0.26, p < 0.01) – participants with higher baseline breathing rates attained larger increases in HRV amplitude during breathing exercise. Figure 8-left presents hrv amplitude scores attained during the exercise phase of the experiment against baseline breathing rate.
Similarly, a significant, positive correlation was also found between baseline breathing rate and ln(LF) (r2 = 0.63, p < 0.01) – participants with high baseline breathing rates attained larger increases in ln(LF) during breathing exercise. Figure 8-right presents ln(LF) scores attained during the exercise phase of the experiment against baseline breathing rate.
To consider whether one approach may allow people to reach lower breathing rates or HRV increases more quickly, we visually inspected data over the 10-min exercise. Figure 9 presents profiles of outcome measures over the course of the 10-min breathing exercise. This analysis reveals that the onset of exercise effects was largely consistent between HRV-b and paced breathing.
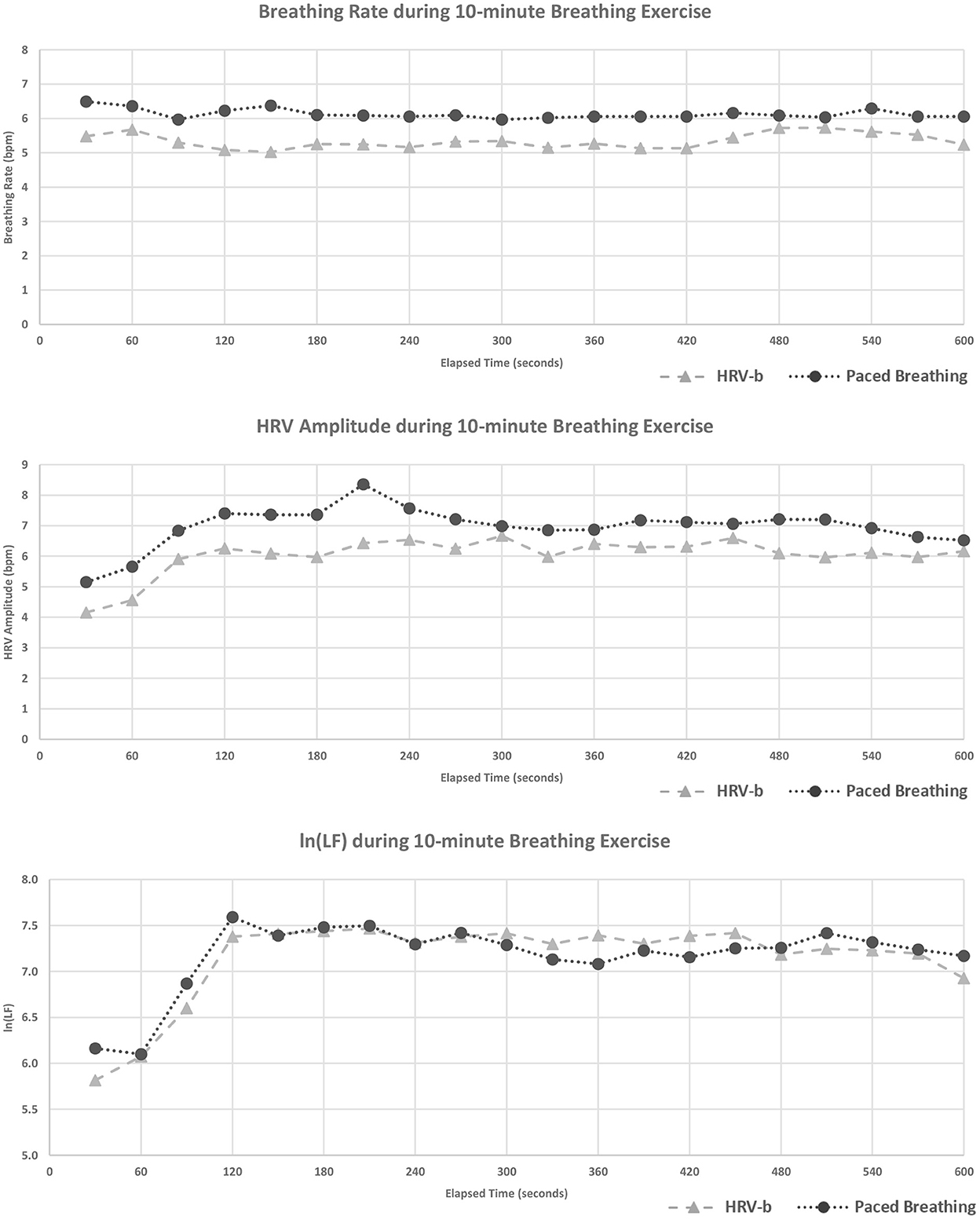
Figure 9. Profiles of breathing rate (top), hrv amplitude (middle), and ln(LF) (bottom) during the 10-min guided breathing exercise. Plotted values indicate the end of each 30-s computation window. Data is broken down by exercise protocol (Paced Breathing, black dotted lines; HRV-b, gray dashed lines). Visual inspection suggests that reductions in breathing rate and increases in HRV scores occurred in a similar fashion with both exercise protocols.
In this section, we summarize the findings just presented, highlighting how they relate to our initial hypotheses and how they might be generalized and applied to the design of guided breathing technology more broadly.
In our experiment, we observed the physiological markers of health benefits across both guided breathing treatment groups. Both groups successfully reduced their breathing rates, which translated to higher-amplitude, lower-frequency heart rate waves – the maker of effective guided breathing exercise.
We did not include a control group in our study design because the effectiveness of both HRV-b and paced breathing compared to control is well-established in the literature (e.g., Sherlin et al., 2009; Prinsloo et al., 2014; Critchley et al., 2015; Steffen et al., 2017). However, since our findings align with well-established previous results, we have full confidence that the exercises completed in our study were what led to observed increases in HRV amplitude and low-frequency power. Our results support H1.
In addition to observing physiological markers of benefit across participants in both guided breathing treatment groups, we found that the effects of paced breathing did not differ significantly from those of the more sophisticated HRV-b exercise. Participants in both treatment groups achieved comparable reductions in breathing rate and increases in HRV scores. Further, the way these effects materialized over the course of the 10-min exercise (i.e., the onset of the effects) was also consistent between exercises.
This is an important finding for design because HRV-b is a more sophisticated, involved, and costly protocol to integrate into tools that support guided breathing. Since similar immediate effects can be achieved from either breathing exercise, our findings suggest that paced breathing can be used in place of HRV-b when designing guided breathing technologies for non-clinical use. Our results support H2.
Previous research (e.g., Kennedy and Parker, 2018) has suggested that the magnitude of the effects created during guided breathing depend on baseline state – larger magnitude effects are anticipated to occur in individuals who are “further out of breathing alignment” to begin with. Our findings corroborate this conjecture – all participants in our study were able to reduce their breathing to the desired rates during exercise and larger increases in HRV amplitude and low-frequency power were observed in those with higher baseline breathing rates.
Again, this finding is important for the design of guided breathing tools because it suggests that designers may be able to rely on a simple and uniform exercise irrespective of the targeted user group (i.e., additional design consideration is not needed to help individuals who are “out of breathing alignment” complete the exercise effectively). Despite the widely varying demographic backgrounds of the participants that completed our studies (e.g., with ages ranging from those in their 20's through those into their 80's; individuals with widely varying levels of physical fitness), the guided breathing exercises completed led to the anticipated physiological effects.
Although many system designs have previously been proposed for guided breathing based upon both HRV-b approaches (Yu and Song, 2015; Liang et al., 2018) and simple-paced breathing (Moraveji et al., 2011; Ghandeharioun and Picard, 2017), we argue that there is a fundamental knowledge gap that inbodied interaction helps to expose. That is whether there are fundamental differences between the outcomes of these practices. Inbodied interaction argues that HCI systems that aim to support and optimize human performance need to rely upon a sound understanding of physiology to best inform design (schraefel, 2019; Andres et al., 2020). With this in mind, our paper provides both a valuable primer that should be accessible to HCI researchers and critical information about the physiological effects of two leading exercises that improve health and well-being. Although our work is preliminary from a physiological point of view, it provides a valuable first step toward building a deeper understanding of a critical issue for designing guided breathing technologies. Further, we articulate and evidence the need for further research into both HRV-b and paced breathing exercises.
In clinical use, HRV-b is typically practiced continually over the course of several months to achieve lasting/permanent physiological (e.g., reduced BP, Schein et al., 2001) and psychological benefits [e.g., decreased effects of chronic stress (Kennedy and Parker, 2018) and reduced rates of relapse in depression (Caldwell and Steffen, 2018)]. While we have demonstrated consistent effects across the two breathing exercises in a single 10-min session, we cannot speak to the effects of sustained or continued practice. However, it is important to note that even though it is currently unclear whether a single 10-min session of guided breathing can create meaningful, real-world performance benefits, research suggests that these early and acute physiological effects are indicative of the benefits that will be achieved with continued practice of guided breathing (Gevirtz, 2013; Lehrer and Gevirtz, 2014). Therefore, it seems likely that paced breathing would provide long term benefits similar to those demonstrated with HRV-b.
Given the potential benefits of guided breathing technology, we hope our findings and other explorations of paced breathing guides (e.g., Tabor et al., 2021) provides important next steps for further study. In particular, an improved understanding of real-world, long-term use will be beneficial from both a user experience and physiological outcomes point of view.
A critical question that still exists for the use and design of future breathing guidance technology in how long sessions should (or need to) be. Previous research has suggested that sessions of at least 10-min in duration are needed to fully achieve the benefits of guided breathing (Lehrer et al., 2000; Lehrer and Gevirtz, 2014). This is based on maximizing the neuro-plastic effects created by the breathing exercises (Lehrer et al., 2003) and has been the protocol used in many studies to date (e.g., Prinsloo et al., 2013; Critchley et al., 2015; Steffen et al., 2017; Kennedy and Parker, 2018). However, in our study, we observed that the changes in HRV occurred largely within the first 2 min of both breathing exercises – well before completing the full 10 min of practice. This early shift could suggest that some of the benefits of the exercises might be attainable with a shorter duration of treatment, which could make guided breathing more appealing and attainable when designing tools for certain contexts [e.g., in an information workplace setting (Moraveji et al., 2011), where interruptions are known to occur frequently (Czerwinski et al., 2004)]. Our recent study found some indication that guide designs may influence peoples' preferences after being interrupted (but not in physiologically measurable way; Tabor et al., 2021). Although we cannot confirm whether shorter, more frequent bouts of guided breathing would lead to the benefits of a more traditional practice, clearly understanding the tradeoffs between duration, frequency, and physiological benefits will be an important direction for future research in guided breathing technologies.
In many current non-clincal guided breathing technologies, progress and performance metrics have been derived from the user's HRV during guided breathing exercise. For example, the Heart Math EmWave (see text footnote 5). uses an ear-clip to monitor HRV and provides users with a metric called coherence (see McCraty et al., 2009 for details). Similarly, BreatheSync (see text footnote 3), an iPhone breathing app, monitors HRV by having users rest their finger over their phones camera during the breathing exercise and reports a metric derived from this data known as wellness quotient (WQ). While the specific details of these measures may differ between products, their purpose is to provide a quantifiable sense of performance during the breathing exercise and for tracking progress over time. However, if designers follow our results and design according to the simpler paced breathing protocol, it raises the question of how performance and progress can be tracked, assessed, and quantified. We discuss several ideas below.
First, with continuing improvements in both camera technology and computer vision, it is becoming feasible to monitor physiological signals using a standard RGB video feed. For example, research has demonstrated that heart rate, breathing rate, and RR intervals can be monitored in this way (Fei et al., 2005; Pavlidis et al., 2007; Poh et al., 2010; AL-Khalidi et al., 2011; Dcosta et al., 2016), albeit with individuals seated at their desk under ideal lighting and environmental conditions. Further exploring the feasibility and robustness of such an approach under non-ideal lighting, with moving participants, or in a mobile setting could allow performance to be monitored during guided breathing without the need for specialized sensing equipment.
Furthermore, it may be possible to assess performance and progress through markers other than those traditionally associated with guided breathing exercises, such as HRV. For example, perceived levels of stress/anxiety (Prinsloo et al., 2013; Goessl et al., 2017; Ma et al., 2017) and cognitive acuity (Sherlin et al., 2009; Prinsloo et al., 2011; Purwandini Sutarto et al., 2012; Sutarto et al., 2013; Dessy et al., 2018) are also both measurable characteristics that have been shown to be influenced by guided breathing exercise that do not require real-time heart rate sensing. Should designers choose to assess performance and demonstrate progress through measures like perceived stress and cognitive state, it may also have the added benefit of helping to motivate continued use as these measures more directly demonstrates the tangible benefits that manifest from guided breathing. Designing performance assessment tools that demonstrate the improvements achieved during guided breathing that are quick to complete, responsive to change, and robust over time is an interesting direction for future research in this area.
Finally, depending on the context of the design, it may not be important or even necessary to demonstrate performance or progress over time. For example, research exploring the design of peripheral breathing guides (Moraveji et al., 2011; Ghandeharioun and Picard, 2017; Tabor et al., 2021) suggests that users may be able to adhere to a paced breathing stimulus without constant attention to their breath, partially mitigating the need to motivate the practice through measures of performance and progress.
In this section, we discuss the limits and scope of our findings, and explain how the results of our study can inform further research in the future.
We have argued that HRV-b is a more sophisticated and involved protocol compared to paced breathing, especially in non-clinical use cases. This raises an interesting question: did we administer HRV-b correctly/to its fullest potential? Although our results demonstrate effects that are not significantly different between paced breathing and HRV-b, we also acknowledge that HRV-b can be challenging – especially for beginners. Is it possible that, had we administered HRV-b in a “better” way, we would have observed greater improvement? In preparing for the study, we took great care to match our testing protocol with those reported in previous literature. We made heavy use of the guide provided by Lehrer et al. (2000) that provides a detailed protocol for HRV-b. Additionally, our exercise and coaching instructions were informed based on the materials of an HRV-b course taught by Dr. Richard Gevirtz11 as well as interviews with an HRV-b clinician in our local area. We, therefore, have no reason to believe that our protocol differed in any meaningful way from those in previous work and, in short, we are confident that the HRV-b protocol was administered correctly. Therefore, the physiological benefits achieved in our HRV-b protocol are representative of those anticipated in unsupervised, real-world practice, as would be the case with at-home use of commercially available HRV-b tools.
Previous research has demonstrated that many of the benefits associated with guided breathing are achieved with continued practice over a period of weeks or months (Wheat and Larkin, 2010; Gevirtz, 2013; Michael et al., 2017; Kennedy and Parker, 2018; De Witte et al., 2019). For example, the lowered levels of blood pressure (Schein et al., 2001), decreased symptoms of depression (Caldwell and Steffen, 2018), and reduced rates of relapse in substance dependence (Eddie et al., 2015) presented in previous research were all observed following sustained practice of guided breathing over an 8 week period or longer. While we have demonstrated that the early, acute physiological markers of these benefits occur consistently in paced breathing and HRV-b, we will investigate whether this similarity remains with sustained practice of the exercises in future research.
Although we did not delineate between chest and abdominal breathing in our experiment, nor did we measure the depth of each breath (i.e., the tidal volume, or quantity of air that was displaced with each inhale and exhale), we did coach participants to breathe into and out of their “bellies” during both exercises and informally ensured adherence to this method of breathing. However, both of these properties (i.e., location and depth) can play a role in the effectiveness of breathing exercise (Calais-Germain, 2006). It is possible to measure and quantify these aspects of breathing using an instrument known as a respiratory induced plethysmography belt (or RIP belt, for short) (Chadha et al., 1982), albeit with an additional calibration step (Sackner et al., 1989). Future work could further explore how other such properties of breathing can influence the effectiveness and ease of use of guided breathing exercises like paced breathing and HRV-b, and how other new breathing technologies can provide guidance for them.
Early research is beginning to suggest that a single 10-min session of guided slow breathing can have measurable effects of aspects of cognitive function such as response time and decision making abilities (e.g., Prinsloo et al., 2011). Although we did not collect data pertaining to cognitive function in our work, exploring these other potential differences between guided breathing technologies could be an interesting area for future research, especially when considering wider application of breathing exercises (e.g., how breathing exercise could support performance in information or creative work).
In this paper, we have demonstrated that paced breathing can create early physiological markers of benefit that are not significantly different from those using Heart Rate Variability Biofeedback (HRV-b), a more sophisticated breathing exercise that requires real-time sensing and feedback. This finding is important for the design of guided breathing technologies because it suggests that these tools can confidently be designed to employ the simpler paced breathing protocol. Our findings can allow designed of paced breathing technology to avoid the complications associated with HRV-b without sacrificing the potential benefits that their users can achieve.
With clear connections to health, wellbeing, and bodily performance, guided breathing is an important topic of research. In this paper, we contribute foundational knowledge to the growing body of HCI research inspired by an inbodied interaction approach to the design of technology for improving health well-being and performance. Our work provides a better understanding of human physiology and illustrate how this can make the benefits of guided breathing exercises more accessible and effective through the design of new technology.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by University of New Brunswick Research Ethics Board (UNB REB 2018-112). The patients/participants provided their written informed consent to participate in this study.
AT led all the work. SB, ES, and MS supported all aspects of the research and contributed to writing the paper. All authors contributed to the article and approved the submitted version.
We acknowledge funding support from NSERC, New Brunswick Innovation Foundation, EPSRC Health Resilience Interactive Technology, ReFresh and GetAMoveOn (EP/T007656/1, EP/K021907/1, and EP/N027299/1).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
2. ^mindmedia.com/en/products/biotrace-software
5. ^store.heartmath.com/emwave2
7. ^Recent research suggests that with specific focus and training it may actually be possible to volitionally influence our heart rate (Abukonna et al., 2013), however, outside of these special circumstances our heart rate is typically considered to be a non-volitional/autonomically mediated process.
9. ^polar.com/ca-en/products/accessories/h10_heart_rate_sensor
10. ^support.polar.com/e_manuals/H10_HR_sensor/Polar_H10_user_manual_English/manual.pdf
11. ^shop.stensacademy.com/products/e-course-heart-rate-variability
Abtahi, F., Berndtsson, A., Abtahi, S., Seoane, F., and Lindecrantz, K. (2014). “Development and preliminary evaluation of an android based heart rate variability biofeedback system,” in 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (Chicago, IL), 3382–3385. doi: 10.1109/EMBC.2014.6944348
Abukonna, A., Yu, X., Zhang, C., and Zhang, J. (2013). Volitional control of the heart rate. Int. J. Psychophysiol. 90, 143–148. doi: 10.1016/j.ijpsycho.2013.06.021
Al Rihawi, R. G., Ahmed, B., and Gutierrez-Osuna, R. (2014). “Dodging stress with a personalized biofeedback game,” in Proceedings of the First ACM SIGCHI Annual Symposium on Computer-Human Interaction in Play, 399–400. CHI PLAY'14. New York, NY: ACM. doi: 10.1145/2658537.2661310
AL-Khalidi, F. Q., Saatchi, R., Burke, D., Elphick, H., and Tan, S. (2011). Respiration rate monitoring methods: a review. Pediatr. Pulmonol. 46, 523–529. doi: 10.1002/ppul.21416
Andres, J., Schraefel, M. C., Patibanda, R., and Mueller, F. F. (2020). “Future InBodied: a framework for inbodied interaction design,” in Proceedings of the Fourteenth International Conference on Tangible, Embedded, and Embodied Interaction (Sydney, NSW: ACM), 885–888. doi: 10.1145/3374920.3374969
Ban, Y., Karasawa, H., Fukui, R., and Warisawa, S. I. (2018). “Relaxushion: controlling the rhythm of breathing for relaxation by overwriting somatic sensation,” in SIGGRAPH Asia 2018 Emerging Technologies. SA'18 (New York, NY: Association for Computing Machinery), 1–2. doi: 10.1145/3275476.3275492
Bánhalmi, A., Borbás, J., Fidrich, M., Bilicki, V., Gingl, Z., Rudas, L., et al. (2018). Analysis of a pulse rate variability measurement using a smartphone camera. J. Healthc. Eng. 2018, 4038034. doi: 10.1155/2018/4038034
Bergstrom, I., Seinfeld, S., Arroyo-Palacios, J., Slater, M., and Sanchez-Vives, M. V. (2014). Using music as a signal for biofeedback. Int. J. Psychophysiol. Appl. Neurosci. 93, 140–149. doi: 10.1016/j.ijpsycho.2013.04.013
BioZen (2019). Available online at: http://play.google.com/store/apps/details?id=com.t2 (accessed November 15, 2022).
Breathmix - Biofeedback Breath Pacer (2019). Available online at: http://play.google.com/store/apps/details?id=com.breathmix (accessed November 15, 2022).
Brown, R. P., and Gerbarg, P. L. (2005). Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: Part II—clinical applications and guidelines. J. Altern. Complement. Med. 11, 711–717. doi: 10.1089/acm.2005.11.711
Bumatay, A. L., and Seo, J. H. (2015). “Investigating the role of haptic stimulation in mobile meditation tools,” in HCI International 2015 - Posters' Extended Abstracts, Vol. 529, eds C. Stephanidis (Cham: Springer International Publishing), 451–456. doi: 10.1007/978-3-319-21383-5_75
Calais-Germain, B. (2006). Anatomy of Breathing. Seattle, WA: Eastland Press. Available online at: http://trove.nla.gov.au/version/38995666 (accessed November 15, 2022).
Caldwell, Y. T., and Steffen, P. R. (2018). Adding HRV biofeedback to psychotherapy increases heart rate variability and improves the treatment of major depressive disorder. Int. J. Psychophysiol. 131, 96–101 doi: 10.1016/j.ijpsycho.2018.01.001
Chadha, T. S., Watson, H., Birch, S., Jenouri, G. A., Schneider, A. W., Cohn, M. A., et al. (1982). Validation of respiratory inductive plethysmography using different calibration procedures. Am. Rev. Respir. Dis. 125, 644–649. doi: 10.1164/arrd.1982.125.6.644
Chapleau, M. W. (2012). “Chapter 33 - Baroreceptor reflexes,” in Primer on the Autonomic Nervous System, 3rd ed, eds D. Robertson, I. Biaggioni, G. Burnstock, P. A. Low, and J. F. R. Paton (San Diego, CA: Academic Press), 161–165. doi: 10.1016/B978-0-12-386525-0.00033-0
Cowley, B., Filetti, M., Lukander, K., Torniainen, J., Henelius, A., Ahonen, L., et al. (2016). Tihe Psychophysiology Primer: A Guide to Methods and a Broad Review with a Focus on Human–Computer Interaction, Vol. 9. Foundations and Trends® in Human–Computer Interaction, 151–308. doi: 10.1561/1100000065
Critchley, H. D., Nicotra, A., Chiesa, P. A., Nagai, Y., Gray, M. A., Minati, L., et al. (2015). Slow breathing and hypoxic challenge: cardiorespiratory consequences and their central neural substrates. PLoS ONE 10:,e0127082. doi: 10.1371/journal.pone.0127082
Czerwinski, M., Horvitz, E., and Wilhite, S. (2004). “A diary study of task switching and interruptions,” in: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. CHI'04 (New York, NY: ACM), 175–182. doi: 10.1145/985692.985715
Dcosta, M., Shastri, D., Tsiamyrtzis, P., and Pavlidis, I. (2016). “Turning security monitoring into an engaging high performance task,” in 2016 IEEE Symposium on Technologies for Homeland Security (HST) (Waltham, MA), 1–2. doi: 10.1109/THS.2016.7568926
De Witte, N. A., Buyck, I., and Van Daele, T. (2019). Combining biofeedback with stress management interventions: a systematic review of physiological and psychological effects. Appl. Psychophysiol. Biofeedback 44, 71–82. doi: 10.1007/s10484-018-09427-7
Dessy, E., Van Puyvelde, M., Mairesse, O., Neyt, X., and Pattyn, N. (2018). Cognitive performance enhancement: do biofeedback and neurofeedback work? J. Cogn. Enhanc. 2, 12–42. doi: 10.1007/s41465-017-0039-y
Eddie, D., Vaschillo, E., Vaschillo, B., and Lehrer, P. (2015). Heart rate variability biofeedback: theoretical basis, delivery, and its potential for the treatment of substance use disorders. Addict. Res. Theory 23, 266–272. doi: 10.3109/16066359.2015.1011625
Fehr, L., Langbein, W. E., and Skaar, S. B. (2000). Adequacy of power wheelchair control interfaces for persons with severe disabilities: a clinical survey. J. Rehabil. Res. Dev. 37, 353–360.
Fei, J., Zhu, Z., and Pavlidis, I. (2005). “Imaging breathing rate in the CO2 absorption band,” in 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference (Shanghai), 700–705.
Frey, J., Grabli, M., Slyper, R., and Cauchard, J. R. (2018). “Breeze: sharing biofeedback through wearable technologies,” in Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems. CHI'18. (New York, NY: ACM), 645, 1–645, 12. doi: 10.1145/3173574.3174219
Gevirtz, R. (2013). The promise of heart rate variability biofeedback: evidence-based applications. Biofeedback 41, 110–120. doi: 10.5298/1081-5937-41.3.01
Ghandeharioun, A., and Picard, R. (2017). “BrightBeat: effortlessly influencing breathing for cultivating calmness and focus,” in Proceedings of the 2017 CHI Conference Extended Abstracts on Human Factors in Computing Systems - CHI EA'17 (Denver, CO: ACM Press), 1624–1631. doi: 10.1145/3027063.3053164
Goessl, V. C., Curtiss, J. E., and Hofmann, S. G. (2017). The effect of heart rate variability biofeedback training on stress and anxiety: a meta-analysis. Psychol. Med. 47, 2578–2586. doi: 10.1017/S0033291717001003
Hair, A., and Gutierrez-Osuna, R. (2017). “Deep breaths: an internally- and externally-paced deep breathing guide,” in 2017 Seventh International Conference on Affective Computing and Intelligent Interaction Workshops and Demos (ACIIW), 85–87. doi: 10.1109/ACIIW.2017.8272594
Hamon, M., Ramadour, R., and Frey, J. (2018). Exploring biofeedback with a tangible interface designed for relaxation. arXiv. doi: 10.48550/arXiv.1808.08711
Harris, J., Vance, S., Fernandes, O., Parnandi, A., and Gutierrez-Osuna, R. (2014). “Sonic respiration: controlling respiration rate through auditory biofeedback,” in CHI'14 Extended Abstracts on Human Factors in Computing Systems. CHI EA'14. (New York, NY: Association for Computing Machinery), 2383–2388. doi: 10.1145/2559206.2581233
HRV Biofeedback (2019). Available online at: http://play.google.com/store/apps/details?id=com.achimsapps.hrv (accessed November 15, 2022).
Jones, M., Grogg, K., Anschutz, J., and Fierman, R. (2008). A sip-and-puff wireless remote control for the apple IPod. Assist. Technol. 20, 107–110. doi: 10.1080/10400435.2008.10131937
Kennedy, L., and Parker, S. H. (2018). Biofeedback as a stress management tool: a systematic review. Cogn. Technol. Work 21, 161–190. doi: 10.1007/s10111-018-0487-x
Kitto, K. L., and Bellingham, W. (1993). Development of a Low Cost Sip and Puff Mouse. Association for the Advancement of Rehabilitation Technology. p. 465.
Kuikkaniemi, K., Laitinen, T., Turpeinen, M., Saari, T., Kosunen, I., Ravaja, N., et al. (2010). The Influence of Implicit and Explicit Biofeedback in First-Person Shooter Games. New York, NY: ACM Press, 859. doi: 10.1145/1753326.1753453
Lehrer, P. (2013). How does heart rate variability biofeedback work? Resonance, the baroreflex, and other mechanisms. Biofeedback 41, 26–31. doi: 10.5298/1081-5937-41.1.02
Lehrer, P. M., and Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work? Front. Psychol. 5, 756. doi: 10.3389/fpsyg.2014.00756
Lehrer, P. M., Vaschillo, E., and Vaschillo, B. (2000). Resonant frequency biofeedback training to increase cardiac variability: rationale and manual for training. Appl. Psychophysiol. Biofeedback 25, 177–191. doi: 10.1023/a:1009554825745
Lehrer, P. M., Vaschillo, E., Vaschillo, B., Lu, S. E., Eckberg, D. L., Edelberg, R., et al. (2003). Heart rate variability biofeedback increases baroreflex gain and peak expiratory flow. Psychosom. Med. 65, 796. doi: 10.1097/01.PSY.0000089200.81962.19
Leslie, G., Ghandeharioun, A., Zhou, D., and Picard, R. W. (2019). “Engineering music to slow breathing and invite relaxed physiology,” in 2019 8th International Conference on Affective Computing and Intelligent Interaction (ACII) (Cambridge), 1–7. doi: 10.1109/ACII.2019.8925531
Liang, R. H., Yu, B., Xue, M., Hu, J., and Feijs, L. M. (2018). “BioFidget: biofeedback for respiration training using an augmented fidget spinner,” in Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems. CHI'18. (New York, NY: ACM), 613, 1–613, 12. doi: 10.1145/3173574.3174187
Logtenberg, S. J., Kleefstra, N., Houweling, S. T., Groenier, K. H., and Bilo, H. J. (2007). Effect of device-guided breathing exercises on blood pressure in hypertensive patients with type 2 diabetes mellitus: a randomized controlled trial. J. Hypertens. 25, 241–246. doi: 10.1097/HJH.0b013e32801040d5
Ma, X., Yue, Z. Q., Gong, Z. Q., Zhang, H., Duan, N. Y., Shi, Y. T., et al. (2017). The effect of diaphragmatic breathing on attention, negative affect and stress in healthy adults. Front. Psychol. 8, 874. doi: 10.3389/fpsyg.2017.00874
Marshall, J., Rowland, D., Rennick Egglestone, S., Benford, S., Walker, B., McAuley, D., et al. (2011). “Breath control of amusement rides,” in Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. CHI'11 (New York, NY: ACM), 73–82. doi: 10.1145/1978942.1978955
McCraty, R., Atkinson, M., Tomasino, D., and Bradley, R. T. (2009). The Coherent Heart Heart–Brain Interactions, Psychophysiological Coherence, and the Emergence of System-Wide Order, Vol. 5, 106.
Michael, S., Graham, K. S., and Davis, G. M. (2017). Cardiac autonomic responses during exercise and post-exercise recovery using heart rate variability and systolic time intervals—a review. Front. Physiol. 8, 301. doi: 10.3389/fphys.2017.00301
Mladenović, J., Frey, J., and Cauchard, J. R. (2018). “Dišimo: anchoring our breath,” in Extended Abstracts of the 2018 CHI Conference on Human Factors in Computing Systems - CHI'18 (Montreal, QC: ACM Press), 1–4. doi: 10.1145/3170427.3186517
Moraveji, N., Olson, B., Nguyen, T., Saadat, M., Khalighi, Y., Pea, R., et al. (2011). Peripheral Paced Respiration: Influencing User Physiology during Information Work. New York, NY: ACM Press, 423. doi: 10.1145/2047196.2047250
Moraveji, N., and Soesanto, C. (2012). “Towards stress-less user interfaces: 10 design heuristics based on the psychophysiology of stress,” in CHI'12 Extended Abstracts on Human Factors in Computing Systems. CHI EA'12 (New York, NY: ACM), 1643–1648. doi: 10.1145/2212776.2223686
Nacke, L. E., Kalyn, M., Lough, C., and Mandryk, R. L. (2011). “Biofeedback game design: using direct and indirect physiological control to enhance game interaction,” in Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. CHI'11 (New York, NY: ACM), 103–112. doi: 10.1145/1978942.1978958
Papadopoulou, A., Berry, J., Knight, T., and Picard, R. (2019). “Affective sleeve: wearable materials with haptic action for promoting calmness,” in Distributed, Ambient and Pervasive Interactions, eds N. Streitz, and S. Konomi. Lecture Notes in Computer Science (Cham: Springer International Publishing), 304–319. doi: 10.1007/978-3-030-21935-2_23
Paredes, P., and Chan, M. (2011). “CALM-ME-NOW - An Exploratory Study and Design of Stress Mitigating Interventions,” in Proceedings of the 2011 CHI Conference on Human Factors in Computing Systems (Vancouver, BC: ACM).
Paredes, P. E., Zhou, Y., Hamdan, N. A., Balters, S., Murnane, E., Ju, W., et al. (2018). “Just breathe: in-car interventions for guided slow breathing,” in Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies, Vol. 2, 1–23. doi: 10.1145/3191760
Patel, S. N., and Abowd, G. D. (2007). “Blui: low-cost localized blowable user interfaces,” in Proceedings of the 20th Annual ACM Symposium on User Interface Software and Technology. UIST'07 (New York, NY: ACM), 217–220. doi: 10.1145/1294211.1294250
Patibanda, R., Mueller, F. F., Leskovsek, M., and Duckworth, J. (2017). Life Tree: Understanding the Design of Breathing Exercise Games. In, 19–31. ACM Press. doi: 10.1145/3116595.3116621
Pavlidis, I., Dowdall, J., Sun, N., Puri, C., Fei, J., Garbey, M., et al. (2007). Interacting with human physiology. Comput. Vis. Image Underst. 108, 150–170. doi: 10.1016/j.cviu.2006.11.018
Plews, D. J., Scott, B., Altini, M., Wood, M., Kilding, A. E., Laursen, P. B., et al. (2017). Comparison of heart-rate-variability recording with smartphone photoplethysmography, polar H7 chest strap, and electrocardiography. Int. J. Sports Physiol. Perform. 12, 1324–1328. doi: 10.1123/ijspp.2016-0668
Poh, M. Z., McDuff, D. J., and Picard, R. W. (2010). Non-contact, automated cardiac pulse measurements using video imaging and blind source separation. Optics Express 18, 10762. doi: 10.1364/OE.18.010762
Prinsloo, G. E., Derman, W. E., Lambert, M. I., and Rauch, H. G. (2013). The effect of a single episode of short duration heart rate variability biofeedback on measures of anxiety and relaxation states. Int. J. Stress Manag. 20, 391–411. doi: 10.1037/a0034777
Prinsloo, G. E., Rauch, H. L., and Derman, W. E. (2014). A brief review and clinical application of heart rate variability biofeedback in sports, exercise, and rehabilitation medicine. Phys. Sportsmed. 42, 88–99. doi: 10.3810/psm.2014.05.2061
Prinsloo, G. E., Rauch, H. L., Lambert, M. I., Muench, F., Noakes, T. D., Derman, W. E., et al. (2011). The effect of short duration heart rate variability (HRV) biofeedback on cognitive performance during laboratory induced cognitive stress. Appl. Cogn. Psychol. 25, 792–801. doi: 10.1002/acp.1750
Purwandini Sutarto, A., Abdul Wahab, M. N., and Mat Zin, N. (2012). Resonant breathing biofeedback training for stress reduction among manufacturing operators. Int. J. Occup. Saf. Ergon. 18, 549–561. doi: 10.1080/10803548.2012.11076959
Qin, Y., Vincent, C. J., Bianchi-Berthouze, N., and Shi, Y. (2014). “AirFlow: designing immersive breathing training games for COPD,” in CHI'14 Extended Abstracts on Human Factors in Computing Systems. CHI EA'14. (New York, NY: ACM), 2419–2424. doi: 10.1145/2559206.2581309
Ren, X. (2019). LightSit: an unobtrusive health-promoting system for relaxation and fitness microbreaks at work. Sensors 19, 2162. doi: 10.3390/s19092162
Roo, J. S., Gervais, R., Frey, J., and Hachet, M. (2017). “Inner garden: connecting inner states to a mixed reality sandbox for mindfulness,” in Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems. CHI'17 (New York, NY: ACM), 1459–1470. doi: 10.1145/3025453.3025743
Rovers, A. F., Feijs, L. M., Van Boxtel, G. J., and Cluitmans, P. J. (2009). Flanker Shooting Game; Model-Based Design of Biofeedback Games. Compiegne, France, 12.
Rowe, D. W., Sibert, J., and Irwin, D. (1998). “Heart rate variability: indicator of user state as an aid to human-computer interaction,” in Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. CHI'98 (New York, NY: ACM Press/Addison-Wesley Publishing Co.), 480–487. doi: 10.1145/274644.274709
Russell, M. E., Scott, A. B., Boggero, I. A., and Carlson, C. R. (2017). Inclusion of a rest period in diaphragmatic breathing increases high frequency heart rate variability: implications for behavioral therapy. Psychophysiology 54, 358–365. doi: 10.1111/psyp.12791
Sackner, M. A., Watson, H. E., Belsito, A. S., Feinerman, D. R., Suarez, M. A., Gonzalez, G. E., et al. (1989). Calibration of respiratory inductive plethysmograph during natural breathing. J. Appl. Physiol. 66, 410–420. doi: 10.1152/jappl.1989.66.1.410
Schein, M. H., Gavish, B., Herz, M., Rosner-Kahana, D., Naveh, P., Knishkowy, B., et al. (2001). Treating hypertension with a device that slows and regularises breathing: a randomised, double-blind controlled study. J. Hum. Hypertens. 15, 271–278. doi: 10.1038/sj.jhh.1001148
Schnädelbach, H., Glover, K., and Irune, A. A. (2010). “ExoBuilding: breathing life into architecture,” in Proceedings of the 6th Nordic Conference on Human-Computer Interaction: Extending Boundaries. NordiCHI'10 (New York, NY: ACM), 442–451. doi: 10.1145/1868914.1868965
schraefel, M. C. (2019). “In5: a model for inbodied interaction,” in Extended Abstracts of the 2019 CHI Conference on Human Factors in Computing Systems (Glasgow Scotland Uk: ACM), 1–6. doi: 10.1145/3290607.3312977
schraefel, M. C. (2020). Inbodied Interaction: Introduction. Interactions Magazine. Available online at: https://interactions.acm.org/archive/view/march-april-2020/introduction22 (accessed November 15, 2022).
Shaffer, F., and Ginsberg, J. P. (2017). An overview of heart rate variability metrics and norms. Front. Public Health 5, 258. doi: 10.3389/fpubh.2017.00258
Shaffer, F., McCraty, R., and Zerr, C. L. (2014). A healthy heart is not a metronome: an integrative review of the heart's anatomy and heart rate variability. Front. Psychol. 5, 40. doi: 10.3389/fpsyg.2014.01040
Sherlin, L., Gevirtz, R., Wyckoff, S., and Muench, F. (2009). Effects of respiratory sinus arrhythmia biofeedback versus passive biofeedback control. Int. J. Stress Manag. 16, 233–248. doi: 10.1037/a0016047
Song, H. S., and Lehrer, P. M. (2003). The effects of specific respiratory rates on heart rate and heart rate variability. Appl. Psychophysiol. Biofeedback 11, 13–23. doi: 10.1023/A:1022312815649
Sonne, T., and Jensen, M. M. (2016). “Evaluating the chillfish biofeedback game with children with ADHD,” in Proceedings of the The 15th International Conference on Interaction Design and Children. IDC'16 (New York, NY: ACM), 529–534. doi: 10.1145/2930674.2935981
Sonne, T., Merritt, T., Marshall, P., Lomholt, J. J., Müller, J., Grønbæk, K., et al. (2017). “Calming children when drawing blood using breath-based biofeedback,” in Proceedings of the 2017 Conference on Designing Interactive Systems - DIS'17 (Edinburgh: ACM Press), 725–737. doi: 10.1145/3064663.3064742
Sra, M., Xu, X., and Maes, P. (2018). “BreathVR: leveraging breathing as a directly controlled interface for virtual reality games,” in Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems. CHI'18 (New York, NY: ACM), 340, 1–340, 12. doi: 10.1145/3173574.3173914
Stach, T. C., Nicholas, G., Yim, J., and Rhodes, R. E. (2009). “Heart rate control of exercise video games,” in Proceedings of Graphics Interface 2009 (GI '09) (Kelowna, BC: Canadian Information Processing Society), 125–132.
Steffen, P. R., Austin, T., DeBarros, A., and Brown, T. (2017). The impact of resonance frequency breathing on measures of heart rate variability, blood pressure, and mood. Front. Public Health 5, 222. doi: 10.3389/fpubh.2017.00222
Sutarto, A. P., Wahab, M. N., and Zin, N. M. (2013). Effect of biofeedback training on operator's cognitive performance. Work 44, 231–243. doi: 10.3233/WOR-121499
Tabor, A., Bateman, S., and Scheme, E. (2019). Breathing Physiology and Guided Breathing Exercise: A Primer. Technical Report. University of New Brunswick, New Brunswick. Available online at: https://www.cs.unb.ca/tech-reports/documents/TR19-241.pdf (accessed November 15, 2022).
Tabor, A., Bateman, S., Scheme, E., Sadprasid, B., and schraefel, M. (2021). “Understanding the design and effectiveness of peripheral breathing guide use during information work,” in Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems (Yokohama: ACM), 1–13. doi: 10.1145/3411764.3445388
Tarvainen, M. P., Niskanen, J. P., Lipponen, J. A., Ranta-Aho, P. O., and Karjalainen, P. A. (2014). Kubios HRV – heart rate variability analysis software. Comput. Methods Programs Biomed. 113, 210–220. doi: 10.1016/j.cmpb.2013.07.024
Tennent, P., Rowland, D., Marshall, J., Egglestone, S. R., Harrison, A., Jaime, Z., et al. (2011). “Breathalising games: understanding the potential of breath control in game interfaces,” in Proceedings of the 8th International Conference on Advances in Computer Entertainment Technology. ACE'11. (New York, NY: ACM), 58, 1–58, 8. doi: 10.1145/2071423.2071496
Terzimehić, N., Häuslschmid, R., Hussmann, H., and Schraefel, M. C. (2019). “A review and analysis of mindfulness research in HCI: framing current lines of research and future opportunities,” in Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. CHI'19 (New York, NY: ACM), 457, 1–457, 13. doi: 10.1145/3290605.3300687
van Gent, P., Farah, H., Van Nes, N., and Van Arem, B. (2019). HeartPy: a novel heart rate algorithm for the analysis of noisy signals. Transp. Res. Part F Traffic Psychol. Behav. 66, 368–78. doi: 10.1016/j.trf.2019.09.015
Voss, A., Schroeder, R., Heitmann, A., Peters, A., and Perz, S. (2015). Short-Term heart rate variability—influence of gender and age in healthy subjects. PLoS ONE 10, e0118308. doi: 10.1371/journal.pone.0118308
Weffers, E. O., and Alina, D. (2010). Breathe With the Ocean: A System for Relaxation Using Audio, Haptic and Visual Stimuli. Amsterdam: EuroHaptics. p. 47–60.
Wheat, A. L., and Larkin, K. T. (2010). Biofeedback of heart rate variability and related physiology: a critical review. Appl. Psychophysiol. Biofeedback 35, 229–242. doi: 10.1007/s10484-010-9133-y
Wollmann, T., Abtahi, F., Eghdam, A., Seoane, F., Lindecrantz, K., Haag, M., et al. (2016). User-centred design and usability evaluation of a heart rate variability biofeedback game. IEEE Access 4, 5531–5539. doi: 10.1109/ACCESS.2016.2601882
Wongsuphasawat, K., Gamburg, A., and Moraveji, N. (2012). “You Can'T force calm: designing and evaluating respiratory regulating interfaces for calming technology,” in Adjunct Proceedings of the 25th Annual ACM Symposium on User Interface Software and Technology. UIST Adjunct Proceedings'12 (New York, NY: ACM), 69–70. doi: 10.1145/2380296.2380326
Yasuma, F., and Hayano, J. I. (2004). Respiratory sinus arrhythmia: why does the heartbeat synchronize with respiratory rhythm?” Chest 125, 683–690. doi: 10.1378/chest.125.2.683
Yu, B., Feijs, L., Funk, M., and Hu, J. (2015). Breathe with touch: a tactile interface for breathing assistance system,” in Human-Computer Interaction – INTERACT 2015, eds by J. Abascal, S. Barbosa, M. Fetter, T. Gross, P. Palanque, and M. Winckler. Lecture Notes in Computer Science. (New York, NY: Springer International Publishing), 45–52. doi: 10.1007/978-3-319-22698-9_4
Yu, B., Funk, M., Hu, J., and Feijs, L. (2018a). Unwind: a musical biofeedback for relaxation assistance. Behav. Inform. Technol. 37, 800–814. doi: 10.1080/0144929X.2018.1484515
Yu, B., Hu, J., Funk, M., and Feijs, L. (2018b). DeLight: biofeedback through ambient light for stress intervention and relaxation assistance. Pers. Ubiquitous Comput. 22, 787–805. doi: 10.1007/s00779-018-1141-6
Yu, B., Hu, J., Funk, M., Liang, R. H., Xue, M., Feijs, L., et al. (2018c). RESonance: lightweight, room-scale audio-visual biofeedback for immersive relaxation training. IEEE Access 6, 38336–38347. doi: 10.1109/ACCESS.2018.2853406
Yu, B., Song, Y., and Feijs, L. (2015). “Light bird: An animated biofeedback interface for coherent breathing,” in 9th International Conference on Design and Semantics of Form and Movement (Milano: Politecnico di Milano).
Zepf, S., El Haouij, N., Lee, J., Ghandeharioun, A., Hernandez, J., Picard, R. W., et al. (2020). “Studying personalized just-in-time auditory breathing guides and potential safety implications during simulated driving,” in Proceedings of the 28th ACM Conference on User Modeling, Adaptation and Personalization (New York, NY: Association for Computing Machinery), 275–283. doi: 10.1145/3340631.3394854
Keywords: guided breathing, simple paced breathing, heart rate variability biofeedback (HRV-b), heart rate variability (HRV), guided breathing technology
Citation: Tabor A, Bateman S, Scheme EJ and schraefel mc (2022) Comparing heart rate variability biofeedback and simple paced breathing to inform the design of guided breathing technologies. Front. Comput. Sci. 4:926649. doi: 10.3389/fcomp.2022.926649
Received: 22 April 2022; Accepted: 10 November 2022;
Published: 30 November 2022.
Edited by:
Bruno Bonnechère, Universiteit Hasselt, BelgiumReviewed by:
Liliya Poskotinova, N. Laverov Federal Center for Integrated Arctic Research of the Ural Branch of the Russian Academy of Sciences, RussiaCopyright © 2022 Tabor, Bateman, Scheme and schraefel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aaron Tabor, YWFyb24udGFib3JAdW5iLmNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.