- 1Department of Human Nutrition, Foods, and Exercise, Virginia Tech, Blacksburg, VA, United States
- 2Department of Psychology and Women and Gender Studies Program, George Mason University, Fairfax, VA, United States
- 3Virginia Cooperative Extension's Family Nutrition Program, Virginia Tech, Blacksburg, VA, United States
- 4Department of Public Health Sciences, School of Medicine, University of Virginia, Christiansburg, VA, United States
- 5Department of Population Health Sciences, Virginia Tech, Blacksburg, VA, United States
Introduction: Building household resiliency is one strategy that may help insulate households from the effects of food system volatility that contributes to in food insecurity. A stronger understanding of the relationship between food security and mental health is needed to identify potential factors for intervention to improve household resiliency to food system stressors. Because mothers often make household food decisions, they are an important population for building household resiliency. The purpose of this study was to develop and test a conceptual framework for the relationship between food security and mental health for low-income mothers and to identify potential targets for intervention.
Methods: A conceptual framework was developed based on the existing literature on mental health and food security, as well as factors that impact both constructs. This framework was tested by a path analysis using data from a 2021 cross-sectional survey of low-income Virginia mothers that used validated scales to assess food security status, indicators of mental and physical health, food coping strategies, and social support.
Results and discussion: The initial model was systematically adapted to develop the final retained model. The retained model did not include a direct effect of food security on mental health, but highlighted two significant mediators of the relationship, food coping strategies and social support. While the effect of social support was not practically significant, the effects of food coping strategies as a mediator from food security to perceived stress and life satisfaction were small (β = 0.21, 0.14, respectively; p < 0.001). The retained model provides a framework for understanding the relationship between food security and mental health and highlights potential targets for intervention. Notably, reducing the need for mothers to utilize food coping strategies should be targeted on multiple levels to reduce the impact on mental health and ultimately improve resiliency to future food system shocks.
1. Introduction
The COVID-19 pandemic exposed concerning vulnerabilities in the United States (U.S.) food system (Béné, 2020). Disruption in food supply chains, distribution challenges, and increased food prices all caused challenges for consumers, particularly those with fewer resources (Weersink et al., 2021). While efforts to build a more resilient/robust food system with fewer vulnerabilities are needed, improving household resiliency to volatility in the short term can help mitigate the negative effects of shocks to the food system for families and potentially improve their food security status.
Overall household resiliency defines a household's capacity to protect itself from and withstand stressors, such as an unexpected food supply issue. Households have a variety of both physical and intangible resources that impact resiliency, including financial resources, food coping strategies, and social support (Hobfoll et al., 2018). Shocks that result in a household experiencing food insecurity may result in long-term consequences caused by changes in dietary choices and stress, such as decreased diet quality, poor physical health, and mental distress (Ansah et al., 2019). Identifying strategies that build household resiliency can help insulate households from future shocks resulting from food system volatility and mutually address other concerns, such as the impact of food insecurity and other stressors on mental health status.
We focus on the understanding of this relationship in a United States (US) context because the lived experience of food insecurity differs between countries based on a number of factors including food-related norms, livelihood expectations, and food system stability (FAO, 2018). Smith et al. (2017) noted that because of some differences in predictors of food insecurity across World Bank development rankings, policies to address food insecurity should be country-specific. There is general evidence that shows a relationship between food insecurity and mental health in the US, with factors including physical health, behavioral food coping strategies, and social support associated with both components (Melchior et al., 2009; Gundersen and Ziliak, 2014; Pinard et al., 2016; Frongillo et al., 2017; Maynard et al., 2018; Arenas et al., 2019; Myers, 2020; Liebe et al., 2022). Poor physical health and behavioral food coping strategies, especially those that involve acquiring food in stigmatized ways, have both been correlated with food insecurity, negative mental health effects, and reduced quality of life (Weiser et al., 2011; Franklin et al., 2012; Gundersen and Ziliak, 2014, 2018; Jessiman-Perreault and McIntyre, 2017; Jones, 2017; Na et al., 2019; Elgar et al., 2021; Liebe et al., 2022). The literature suggests social support may mitigate some of the negative mental health outcomes for people experiencing food insecurity (Wehler et al., 2004; Siefert et al., 2007; Ajrouch et al., 2010; Hanson and Olson, 2012; Heberlein et al., 2016; Palar et al., 2018). Despite evidence suggesting these factors' involvement in the relationship between food security and mental health, more information is needed to elucidate potential causal pathways among mothers with children in their households in a US context.
Female heads of household (mothers) are a priority population for interventions designed to strengthen household resiliency to food systems shocks. Single-headed female households are more likely than any other household type to experience food insecurity (USDA Economic Research Service, 2021). Among households with children, mothers typically make food decisions to spare others within their household, such as reducing the quality or quantity of their diet (Myers, 2020). The existing research on the mental health of mothers experiencing food insecurity suggests that they are more likely to have a diagnosed mental illness or symptoms of mental illness than mothers who experience food security (Whitaker et al., 2006; Maynard et al., 2018; Tuthill et al., 2019; Zekeri, 2019; Cameron et al., 2020). Additionally, mothers experiencing food insecurity report higher levels of stress, anxiety, and depression than the U.S. average (Liebe et al., 2022). Stress associated with food insecurity may contribute to changes in parenting behavior that ultimately impact children in the household, such as reported increases in the children's risk of depression and anxiety (McIntyre et al., 2003; Ashiabi and O'Neal, 2008; Melchior et al., 2009; Nagata et al., 2019).
Given that mothers are more likely to experience food insecurity and negative mental health outcomes than average, the complex relationship between food insecurity and mental health needs to be better understood to identify opportunities to build household resiliency. This study aimed to develop a conceptual framework for understanding the pathways between food insecurity and mental health outcomes for low-income mothers. We sought to identify pathways including factors that may mediate this relationship as potential areas for future intervention.
2. Methods
A hypothesized conceptual framework of the relationship between food insecurity and mental health outcomes was developed based on a review of the existing literature (Figure 1). This conceptual framework was used to develop measures for a cross-sectional survey to understand the factors impacting the relationship between food security and mental health for low-income mothers in Virginia. Methods were approved by the Virginia Tech Institutional Review Board.
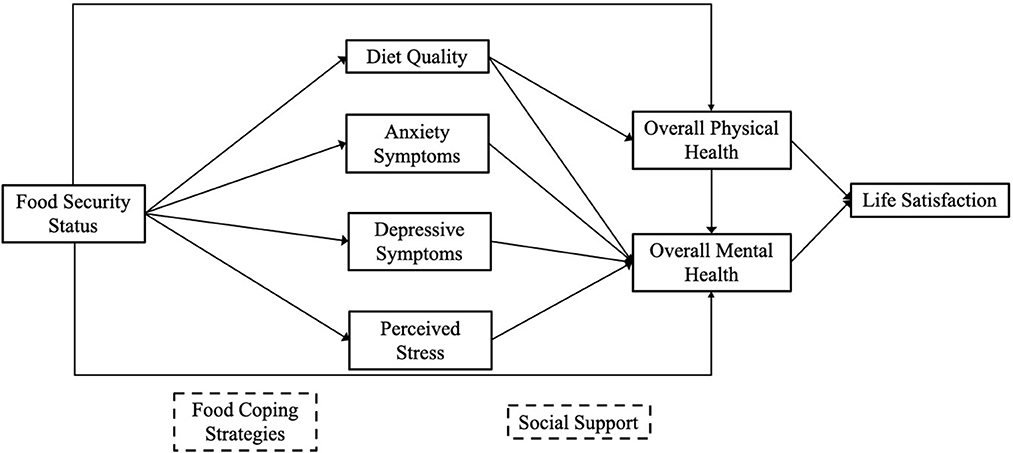
Figure 1. Hypothesized conceptual framework of the relationship between food insecurity and mental health for mothers. Solid lines indicate a path between two constructs. Dashed boxes indicate a strategy that may act as a mediator in the pathways directly above. For example, food coping strategies may mediate the relationship between food security status and diet quality, anxiety symptoms, depressive symptoms, and perceived stress. However, food security status was hypothesized to directly impact those outcomes.
2.1. Cross-sectional survey
A cross-sectional survey was self-administered via Qualtrics (Provo, Utah) from August through October 2021. The methods used to conduct the survey have been described in detail elsewhere (Liebe et al., 2022). The following sections provide a brief overview of the survey.
2.1.1. Participants
Qualtrics identified potential respondents using existing survey panels and listservs. Eligible respondents were low-income adults living in Virginia that identified their gender as a woman or non-binary with children under 18 years old living in their household, and English-speaking. The survey was pre-tested with fifty participants and minor alterations were made to improve the survey flow.
2.1.2. Measures
Food security status was assessed using the 18-item U.S. Department of Agriculture (USDA) Household Food Security Module (Bickel et al., 2000). Scores ranged from 0 to 18, with higher scores indicating worse food security status. Participants were categorized as high, marginal, low, or very low food security based on the thresholds outlined by Bickel and colleagues (Bickel et al., 2000). General physical health and diet quality were assessed with two single-item, validated questions (DeSalvo et al., 2005; Loftfield et al., 2015). Both were rated on a Likert-type scale from 1 (poor) to 5 (excellent).
Mental health and symptoms of mental illness were assessed using scales from the Patient Reported Outcome Measurement Information System (PROMIS). Overall mental health was assessed using the two-item Global Mental Health 2a Scale v1.2, anxiety symptoms were assessed using the four-item Emotional Distress v1.0—Anxiety—Short Form 4a, and depressive symptoms were assessed with Emotional Distress v1.0—Depression—Short Form 4a (Pilkonis et al., 2011, 2014; Hays et al., 2017). Perceived stress over the past month was measured with the National Institutes of Health (NIH) Toolbox Perceived Stress—Adults tool (Kupst et al., 2015). There was no specific timeframe for overall mental health. Anxiety and depression were measured over the past 7 days and perceived stress over the past 30 days. Raw scores from the PROMIS and NIH Toolbox measure were converted to T-scores in which 50 represents the mean for the U.S. general population, with a standard deviation of 10. Higher scores indicated more of the concept being measured (e.g., higher scores indicated greater overall mental health, higher scores indicated greater depressive symptomatology). The final mental health measure, life satisfaction (no specific timeframe), was assessed using the 5-item Satisfaction with Life Scale (Pavot and Diener, 2008). Each item was measured using a Likert-type scale from strongly disagree (1) to strongly agree (7) and scores were summed across all items for scores ranging from 5 to 35.
Social support was measured using a modified version of the 10-item Duke Social Support Inventory (Pachana et al., 2008). Higher scores indicated a greater level of total social support on a scale from 10 to 30. Food coping strategies were assessed using the Hunger Coping Scales (Pinard et al., 2016). This 15-item scale measures three types of strategies: tradeoffs, financial, and rationing. Scores on each subscale were summed to develop a total coping strategies score on a scale from 0 to 15. Demographic data were also collected with individual questions.
2.2. Analysis
A path analysis was performed using R version 4.1.2 (R Core Team, Vienna, Austria). The hypothesized model (Figure 1) was tested and adapted based on modification indices. The model was intended to provide an initial framework for the relationship between food security and mental health, as it is based on cross-sectional data. As outlined in the introduction, there is significant evidence to support that people experiencing food insecurity are more likely to experience poor mental health, which provides a theoretical justification for the proposed direction of the relationship between food security and mental health status. Although there is some evidence suggesting the relationship between depressive symptoms and food insecurity may be bidirectional (Maynard et al., 2018), it is unlikely that there would be an impact of reverse causality in this case because the time window measuring depression is so short (previous 7 days) compared to the time window for measuring food security status (previous 12-months). Therefore, based on the conceptual and statistical relationship, the direction of model flow is appropriate. Regression was used to determine if there was an interaction between food security and potential mediators.
Model fit was assessed using the Comparative Fit Index (CFI), Root Mean Square Error of Approximation (RMSEA), and Chi-Square. A CFI > 0.90 is considered an acceptable fit (Bentler and Bonett, 1980). RMSEA of 0.05 or less is considered a close fit, 0.08 or less as a reasonable fit, and >0.10 represents a model with poor fit (Browne and Cudeck, 1993). A non-significant chi-square test is indicative of good model fit, however, chi-square is sensitive to sample size, and thus this threshold is often not met with large samples (Smith and McMillan, 2001). Standardized regression coefficients (β) were reported for each relationship. Absolute values of β were used to estimate effects, and thresholds were set for small (>0.10), medium (>0.30), and large (>0.50) effects (Cohen, 1988). The threshold for statistical significance was set a priori at p ≤ 0.05.
3. Results
3.1. Survey respondent demographics
Survey participants (n = 1,029) were an average of 34.0 ± 9.8 years old but age ranged from 18 and 80 years old. Most respondents (77.6%, n = 799) reported their education as some college or less. More than two-thirds of respondents had experienced low or very low food security in the past 12 months. Almost two-thirds (65.0%, n = 673) identified as white and 23.4% (n = 242) identified as Black or African American. Additionally, 9.7% (n = 100) of respondents identified as Hispanic or Latino (see Table 1).
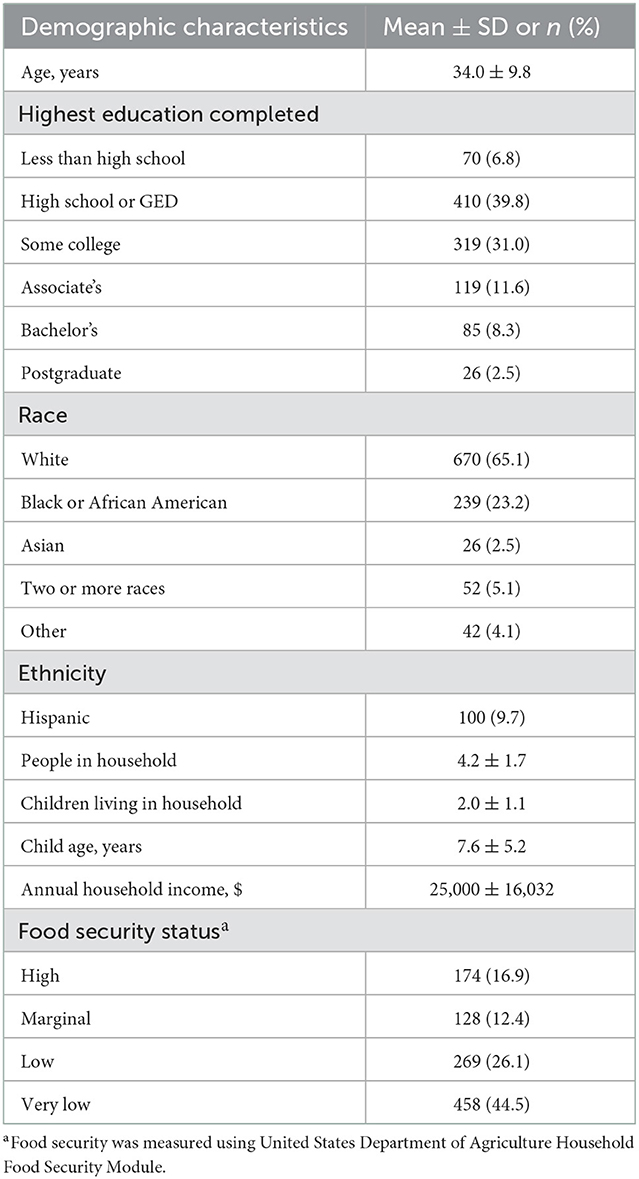
Table 1. Demographics of low-income Virginia mothers that completed the mental health and food security survey (n = 1,029).
3.2. Model selection
The proposed model (Figure 1) was a poor fit for the data [CFI = 0.59; RMSEA = 0.28; = 1,885.86, p < 0.001]. The poor fit may have been a result of the time frames of the mental health indicators. Overall mental health was measured without a specific time frame, whereas anxiety and depressive symptoms and stress were measured on specific timeframes (7 days and 1 month, respectively). Therefore, in the next model, mental health symptoms were switched so the model's specification was consistent with the measures' timeframes, with the most proximal mental health measures as outcomes. This reorganized mode was supported by the modification indices, which suggested this had the highest expected parameter change. This model had a CFI of 0.93 and RMSEA of 0.13, and = 349.40, p < 0.001 indicating a better, but still poor fit. In the next series of models, changes were made systematically based on the modification indices. The potential pathways from food security to mental health symptoms (anxiety, depression, and stress) and diet quality, independent of food coping strategies, were systematically removed. This model had a CFI of 0.93, an RMSEA of 0.14, and = 355.20, p < 0.001. Additionally, pathways from social support to diet quality and life satisfaction were added. The retained model (Figure 2 and Table 2) had a CFI of 0.97, an RMSEA of 0.086, and = 171.90, p < 0.00.
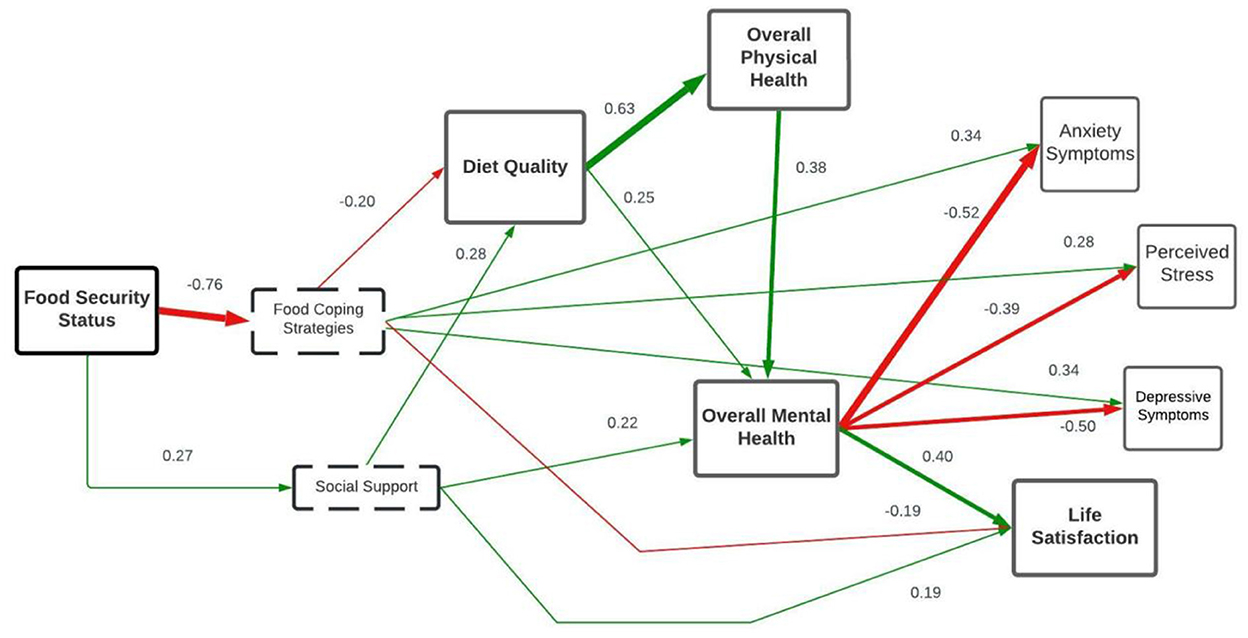
Figure 2. Path model with standardized regression coefficients for relationship between food insecurity and mental health among low-income mothers (n = 1,029). Figure is excluding pathways that had a negligible effect size (f2 < 0.02). Line thickness designates effect size, with a large effect indicated by the thickest lines. Line color indicates whether the relationship is positive (green) or negative (red). Dashed boxes represent strategies for addressing food insecurity. Tools used to assess measures: Food Security—United States Department of Agriculture Household Food Security Module; Social Support—Modified Duke Social Support Inventory; Food Coping Strategies—Hunger Coping Scales; overall mental health—Patient Reported Outcomes Measurement Information System (PROMIS) Global Mental 2a Scale v1.2; Anxiety—PROMIS Emotional Distress v1.0—Anxiety—Short Form 4a; Depression—PROMIS Emotional Distress v1.0—Depression—Short Form 4a. Stress—National Institutes of Health Toolbox Perceived Stress for Adults; Life Satisfaction—Satisfaction with Life Scale; Overall Physical Health—one-item Likert-type scale (DeSalvo et al., 2005); Diet Quality—one-item Likert-type scale (Loftfield et al., 2015).
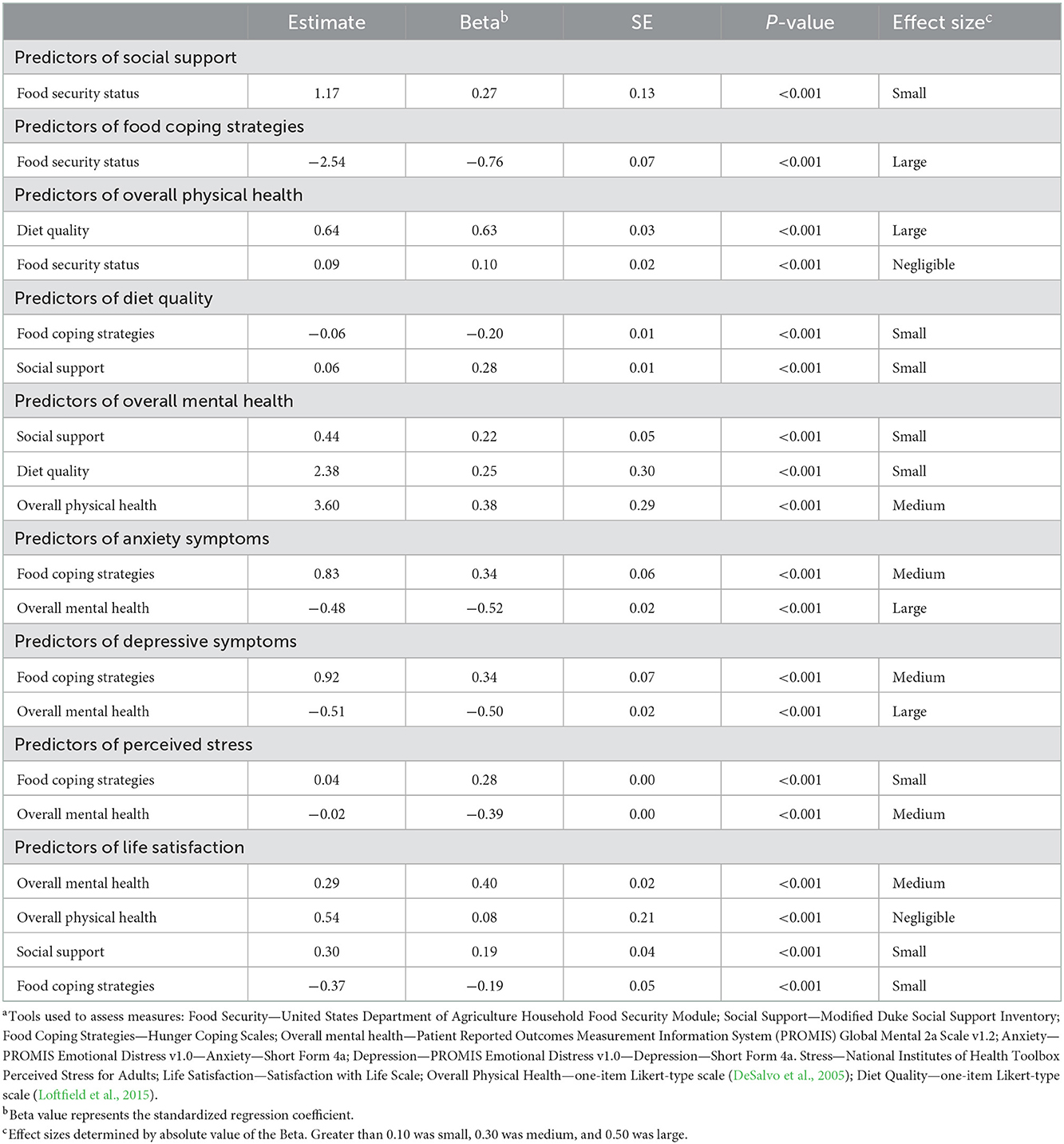
Table 2. Path model statistics for relationship between food insecurity and mental health among low-income mothers in Virginia (n = 1,029)a.
3.3. Retained model
In the retained model, food security had a large negative effect on food coping strategies (β = −0.76, p < 0.001) indicating that improved food security status was associated with fewer food coping strategies. Additionally, there was a small positive effect of food security status on social support (β = 0.27, p < 0.001). While food security was also associated with overall physical health, this relationship was practically insignificant (0.10, p < 0.001). Therefore, this pathway was not included in the retained model (Figure 2).
Two mediators in the relationship between food security and mental health outcomes emerged. No significant interactions were found between food security and either mediator for any of the pathways. Social support mediated the relationship between food security and overall mental health, but this effect was not practically significant (β = 0.06, p < 0.001). Similar results were seen for the effect on life satisfaction (β = 0.05, p < 0.001). The second mediator was food coping strategies, which impacted anxiety and depressive symptoms, perceived stress, and life satisfaction. The findings indicated food coping strategies mediated the relationship between food security and both anxiety and depressive symptoms, although these effects were small (β = 0.26 for both, p < 0.001). Food coping strategies also acted as a mediator on perceived stress and life satisfaction; these indirect effects were small (β = 0.21, 0.14, respectively; p < 0.001).
4. Discussion
The purpose of this study was to develop and test an initial conceptual framework of the relationship between food security and mental health for low-income mothers. Factors associated with the relationship had been identified in the literature, but potential pathways had not been explored. Importantly, the findings of this study suggest no direct effect of food security status on mental health outcomes, which was part of the initial framework based on the literature. We identified two mediators, with food insecurity impacting mental health through food coping strategies and social support. Understanding these pathways is critical because they can be targeted through future interventions to improve household resiliency for future food system instability.
4.1. Food coping strategies role in mental health
The findings of this study suggest reliance on food coping strategies is more common among people experiencing food insecurity and may potentially contribute to feelings of anxiety, depression, and perceived stress symptoms. These findings reflect previous literature suggesting mothers who utilize food coping strategies, compounded by poor mental health and stress, may also suffer from lower household resilience and other adverse consequences (Hobfoll et al., 2018; Ansah et al., 2019). Furthermore, as mothers experiencing food insecurity rely on more food coping strategies, they may also experience greater symptoms of mental illness and stress (Puddephatt et al., 2020).
People experiencing poor mental health may not be able to build the necessary resilience capacity to respond as effectively to future crises, which is problematic for overall food system stability as more households could remain food insecure (Ansah et al., 2019). The link between current resiliency and future food security status is supported by literature from countries other than the U.S. suggesting current household resiliency levels positively correlate with food security status during future shocks (Lokosang et al., 2014; d'Errico et al., 2018; Ansah et al., 2019). Furthermore, the current capacity to handle an unanticipated crisis is related to the ability of the household to adapt practices (e.g., seeking alternative income sources), to prevent future shocks from impacting the household (Ansah et al., 2019). Because mothers may be forced to rely on these strategies to prevent reductions in food quantity, mitigating the negative effects may depend on multi-level interventions. On a systemic level, increased monetary assistance may reduce the financial burden preventing mothers from building household resiliency. On an individual level, strategies to help build self-efficacy related to food resource management, through federally-funded nutrition education programs like Supplemental Nutrition Assistance Program-Education or the Expanded Food and Nutrition Education Program, may improve resiliency in response to future stressors (Kaiser et al., 2015; Ansah et al., 2019). These strategies may simultaneously improve resiliency and reduce the need for food-coping strategies in the future.
4.2. Psychosocial resources may provide iterative opportunities for intervention
Psychosocial resources, which include social support, life satisfaction, and optimism, have considerable overlap with personal resources known to impact household resiliency (Boehm et al., 2015; Ansah et al., 2019). Though the current model was not designed to assess this, these resources may provide an opportunity to improve future resilience capacity. Practices to promote mindfulness, such as meditation and yoga, may improve wellbeing and satisfaction with life and could be considered as potential strategies for future interventions targeting mothers experiencing food insecurity and negative mental health outcomes (Boehm et al., 2012).
4.2.1. Life satisfaction
The findings of this study suggested food coping strategies mediate the relationship between food security and life satisfaction for low-income mothers experiencing food insecurity. Individuals with low resources may tend to experience significantly more stressful experiences contributing to worse life satisfaction (Gallo, 2009). Chronic stress exposure can also impede a person's ability to restore the resources necessary for building household resilience capacity (Gallo et al., 2005; Boehm et al., 2015). Therefore, experiencing worse life satisfaction may contribute to less resilience to future shocks leading to future food insecurity, reliance on food coping strategies, and further worsening life satisfaction. Additionally, child life satisfaction is correlated with mother life satisfaction, suggesting the effects of food insecurity may also impact children in the household (Hoy et al., 2013). Interventions aiming to disrupt the pathway between chronic stress, negative mental health outcomes and less resilience to future shocks may not only improve resiliency but address disparities in life satisfaction contributing to health inequities (Boehm et al., 2015).
4.2.2. Social support
Although the effect of social support as a mediator in the relationship between food security and mental health was negligible, social support was associated with both greater food security and mental health in the current model. Mothers who can rely on the support of friends or family may be more prepared for future food systems shocks for several reasons. First, supportive environments foster personal resiliency through psychosocial resource development, such as greater self-efficacy and optimism (Boehm et al., 2015; Hobfoll et al., 2018). Mothers may then be able to rely on that social support and personal resiliency during a crisis to avoid significant resource loss. Secondly, as vulnerable mothers expend already limited resources to address a shock, they may experience greater stress (Hobfoll et al., 2018). Mothers experiencing food insecurity may be vulnerable to worsening mental health through other pathways as well. Since social support is correlated with positive mental health outcomes, efforts to increase social support may be warranted to improve mental health outcomes among those made vulnerable by food insecurity (Liebe et al., 2022).
4.3. Limitations
Several limitations of this study should be noted. First, participants in the cross-sectional survey were randomly selected from all members of the panels who met the eligibility criteria for the study. The representativeness of the sample to the state and national population of low-income mothers was not explored. However, the conceptual framework presented still highlighted pathways worthy of exploration at the national level. Secondly, all data collection occurred during the COVID-19 pandemic, and we were unable to isolate the effect of the pandemic on the survey findings given the sparsity of literature on the mental health of mothers experiencing food insecurity. Thirdly, a measure of depressive symptoms utilizing a 2-week timeframe would have been more in line with the current Diagnostic and Statistical Manual of Mental Disorders (DSM-V; American Psychiatric Association, 2013). However, the PROMIS scale utilized is a validated tool for assessing depressive symptoms. Finally, there are inherent challenges of a mediation model that is cross-sectional given that mediation implies an order of events. Despite the unknown effect of the pandemic and challenges with a cross-section mediation model, the study findings still suggest a mediating effect of food coping strategies and social support that warrants further exploration with longitudinal studies.
4.4. Framework implications and conclusions
The conceptual framework of the relationship between food security and mental health identified in this study suggests there are opportunities for intervention to improve household resiliency to unanticipated shocks. Interventions targeting household resiliency improvement may impact food system stability at the household level and contribute to greater food security and mental health for vulnerable mothers. This model can provide justification for research and practice targeting food coping strategies to improve the mental health of mothers experiencing food insecurity. Future research should explore potential variations in pathways by demographic characteristics to determine relevant intervention opportunities for different populations. Additionally, the role of other psychosocial resources and social determinants of health could be explored to strengthen the model. In the long term, the effect of interventions to improve resiliency by reducing the need to rely on food coping strategies should be explored to strengthen food system stability at the household level.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Virginia Tech Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
RL: conceptualization, data analysis, and writing—original draft preparation. LA and VH: conceptualization, methodology, and writing-review and editing. ES, KP, and NC: conceptualization and writing—review and editing. SM: conceptualization, methodology, supervision, project administration, and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by a College of Agriculture and Life Sciences, Virginia Tech Seed Grant.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ajrouch, K. J., Reisine, S., Lim, S., Sohn, W., and Ismail, A. (2010). Situational stressors among African-American women living in low-income urban areas: The role of social support. Women Health 50, 159–175. doi: 10.1080/03630241003705045
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. Arlington, VA: American Psychiatric Association.doi: 10.1176/appi.books.9780890425596
Ansah, I. G. K., Gardebroek, C., and Ihle, R. (2019). Resilience and household food security: A review of concepts, methodological approaches and empirical evidence. Food Secur. 11, 1187–1203. doi: 10.1007/s12571-019-00968-1
Arenas, D. J., Thomas, A., Wang, J., and DeLisser, H. M. (2019). A systematic review and meta-analysis of depression, anxiety, and sleep disorders in US adults with food insecurity. J. General Internal Med. 34, 2874–2882. doi: 10.1007/s11606-019-05202-4
Ashiabi, G. S., and O'Neal, K. K. (2008). A framework for understanding the association between food insecurity and children's developmental outcomes. Child Dev. Perspect. 2, 71–77. doi: 10.1111/j.1750-8606.2008.00049.x
Béné, C. (2020). Resilience of local food systems and links to food security – A review of some important concepts in the context of COVID-19 and other shocks. Food Secur. 12, 805–822. doi: 10.1007/s12571-020-01076-1
Bentler, P. M., and Bonett, D. G. (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bullet. 88, 588. doi: 10.1037/0033-2909.88.3.588
Bickel, G., Nord, M., Price, C., Hamilton, W., and Cook, J. (2000). Measuring Food Security in the United States: Guide to Measuring Household Food Security. Available online at: https://www.fns.usda.gov/guide-measuring-household-food-security-revised-2000 (accessed April 2, 2021).
Boehm, J. K., Chen, Y., Williams, D. R., Ryff, C., and Kubzansky, L. D. (2015). Unequally distributed psychological assets: Are there social disparities in optimism, life satisfaction, and positive affect? PLoS ONE 10, e0118066. doi: 10.1371/journal.pone.0118066
Boehm, J. K., Vie, L. L., and Kubzansky, L. D. (2012). The promise of well-being interventions for improving health risk behaviors. Curr. Cardiovasc. Risk Rep. 6, 511–519. doi: 10.1007/s12170-012-0273-x
Browne, M. W., and Cudeck, R. (1993). “Alternative ways of assessing model fit,” in Testing Structural Equation Models, eds K. A. Bollen and J. S. Long (Newbury Park, CA: SAGE), 136–162.
Cameron, E. E., Joyce, K. M., Delaquis, C. P., Reynolds, K., Protudjer, J. L. P., and Roos, L. E. (2020). Maternal psychological distress & mental health service use during the COVID-19 pandemic. J. Affect. Disord. 276, 765–774. doi: 10.1016/j.jad.2020.07.081
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences, 2nd Edn. New York, NY: Routledge.
d'Errico, M., Romano, D., and Pietrelli, R. (2018). Household resilience to food insecurity: Evidence from Tanzania and Uganda. Food Secur. 10, 1033–1054. doi: 10.1007/s12571-018-0820-5
DeSalvo, K. B., Fan, V. S., McDonell, M. B., and Fihn, S. D. (2005). Predicting mortality and healthcare utilization with a single question. Health Serv. Res. 40, 1234–1246. doi: 10.1111/j.1475-6773.2005.00404.x
Elgar, F. J., Pickett, W., Pförtner, T-K., Gariépy, G., Gordon, D., Georgiades, K., et al. (2021). Relative food insecurity, mental health and wellbeing in 160 countries. Soc. Sci. Med. 268, 113556. doi: 10.1016/j.socscimed.2020.113556
FAO IFAD, UNICEF, WFP, and WHO. (2018). The State of Food Security and Nutrition in the World 2018. Building Climate Resilience for Food Security and Nutrition. Licence: CC BY-NC-SA 3.0 IGO. Rome: FAO.
Franklin, B., Jones, A., Love, D., Puckett, S., Macklin, J., and White-Means, S. (2012). Exploring mediators of food insecurity and obesity: A review of recent literature. J. Commun. Health 37, 253–264. doi: 10.1007/s10900-011-9420-4
Frongillo, E. A., Nguyen, H. T., Smith, M. D., and Coleman-Jensen, A. (2017). Food insecurity is associated with subjective well-being among individuals from 138 countries in the 2014 gallup world poll. J. Nutr. 147, 680–687. doi: 10.3945/jn.116.243642
Gallo, L. C. (2009). The reserve capacity model as a framework for understanding psychosocial factors in health disparities. Appl. Psychol. 1, 62–72. doi: 10.1111/j.1758-0854.2008.01000.x
Gallo, L. C., Bogart, L. M., Vranceanu, A-M., and Matthews, K. A. (2005). Socioeconomic status, resources, psychological experiences, and emotional responses: A test of the reserve capacity model. J. Personal. Soc. Psychol. 88, 386. doi: 10.1037/0022-3514.88.2.386
Gundersen, C., and Ziliak, J. (2014). Childhood Food Insecurity in the US: Trends, Causes, and Policy Options. Available online at: https://files.eric.ed.gov/fulltext/EJ1042789.pdf (accessed December 10, 2022).
Gundersen, C., and Ziliak, J. (2018). Food insecurity research in the United States: Where we have been and where we need to go. Appl. Econ. Perspect. Pol. 40, ppx058. doi: 10.1093/aepp/ppx058
Hanson, K. L., and Olson, C. M. (2012). Chronic health conditions and depressive symptoms strongly predict persistent food insecurity among rural low-income families. J. Health Care Poor Underserv. 23, 1174–1188. doi: 10.1353/hpu.2012.0116
Hays, R. D., Schalet, B. D., Spritzer, K. L., and Cella, D. (2017). Two-item PROMIS® global physical and mental health scales. J. Patient Report. Outcomes 1, 2. doi: 10.1186/s41687-017-0003-8
Heberlein, E. C., Picklesimer, A. H., Billings, D. L., Covington-Kolb, S., Farber, N., and Frongillo, E. A. (2016). The comparative effects of group prenatal care on psychosocial outcomes. Archiv. Women's Mental Health 19, 259–269. doi: 10.1007/s00737-015-0564-6
Hobfoll, S. E., Halbesleben, J., Neveu, J. P., and Westman, M. (2018). Conservation of resources in the organizational context: The reality of resources and their consequences. Ann. Rev. Org. Psychol. Org. Behav. 5, 103–128. doi: 10.1146/annurev-orgpsych-032117-104640
Hoy, B. D., Suldo, S. M., and Mendez, L. R. (2013). Links between parents' and children's levels of gratitude, life satisfaction, and hope. J. Hap. Stud. 14, 1343–1361. doi: 10.1007/s10902-012-9386-7
Jessiman-Perreault, G., and McIntyre, L. (2017). The household food insecurity gradient and potential reductions in adverse population mental health outcomes in Canadian adults. SSM Popul. Health 3, 464–472. doi: 10.1016/j.ssmph.2017.05.013
Jones, A. D. (2017). Food insecurity and mental health status: A global analysis of 149 countries. Am. J. Prev. Med. 53, 264–273. doi: 10.1016/j.amepre.2017.04.008
Kaiser, L, Chaidez, V., Algert, S., Horowitz, M., Martin, A., Mendoza, C., et al. (2015). Food resource management education with SNAP participation improves food security. J. Nutr. Educ. Behav. 47, 374–378.e1. doi: 10.1016/j.jneb.2015.01.012
Kupst, M. J., Butt, Z., Stoney, C. M., Griffith, J. W., Salsman, J. M., Folkman, S., et al. (2015). Assessment of stress and self-efficacy for the NIH Toolbox for Neurological and Behavioral Function. Anxiety Stress Coping 28, 531–544. doi: 10.1080/10615806.2014.994204
Liebe, R. A., Adams, L. M., Hedrick, V. E., Serrano, E. L., Porter, K. J., Cook, N. E., et al. (2022). Understanding the relationship between food security and mental health for food-insecure mothers in Virginia. Nutrients 14, 71491. doi: 10.3390/nu14071491
Loftfield, E., Yi, S., Immerwahr, S., and Eisenhower, D. (2015). Construct validity of a single-item, self-rated question of diet quality. J. Nutr. Educ. Behav. 47, 181–187. doi: 10.1016/j.jneb.2014.09.003
Lokosang, L. B., Ramroop, S., and Zewotir, T. (2014). Indexing household resilience to food insecurity shocks: The case of South Sudan. Agrekon 53, 137–159. doi: 10.1080/03031853.2014.915486
Maynard, M., Andrade, L., Packull-McCormick, S., Perlman, C. M., Leos-Toro, C., and Kirkpatrick, S. I. (2018). Food insecurity and mental health among females in high-income countries. Int. J. Environ. Res. Public Health 15, 1424. doi: 10.3390/ijerph15071424
McIntyre, L., Glanville, N. T., Raine, K. D., Dayle, J. B., Anderson, B., and Battaglia, N. (2003). Do low-income lone mothers compromise their nutrition to feed their children? Can. Med. Assoc. J. 168, 686–691.
Melchior, M., Caspi, A., Howard, L. M., Ambler, A. P., Bolton, H., Mountain, N., et al. (2009). Mental health context of food insecurity: A representative cohort of families with young children'. Pediatrics 124, e564–e572. doi: 10.1542/peds.2009-0583
Myers, C. A. (2020). Food insecurity and psychological distress: A review of the recent literature. Curr. Nutr. Rep. 9, 107–118. doi: 10.1007/s13668-020-00309-1
Na, M., Miller, M., Ballard, T., Mitchell, D. C., Hung, Y. W., and Melgar-Quiñonez, H. (2019). Does social support modify the relationship between food insecurity and poor mental health? Evidence from thirty-nine sub-Saharan African countries. Public Health Nutr. 22, 874–881. doi: 10.1017/S136898001800277X
Nagata, J. M., Palar, K., Gooding, H. C., Garber, A. K., Whittle, H. J., Bibbins-Domingo, K., et al. (2019). Food insecurity is associated with poorer mental health and sleep outcomes in young adults. J. Adolesc. Health 65, 805–811. doi: 10.1016/j.jadohealth.2019.08.010
Pachana, N. A., Smith, N., Watson, M., McLaughlin, D., and Dobson, A. (2008). Responsiveness of the Duke Social Support sub-scales in older women. Age Ageing 37, 666–672. doi: 10.1093/ageing/afn205
Palar, K., Frongillo, E. A., Escobar, J., Sheira, L. A., Wilson, T. E., Adedimeji, A., et al. (2018). Food insecurity, internalized stigma, and depressive symptoms among women living with HIV in the United States. AIDS Behav. 22, 3869–3878. doi: 10.1007/s10461-018-2164-8
Pavot, W., and Diener, E. (2008). The Satisfaction With Life Scale and the emerging construct of life satisfaction. J. Positive Psychol. 3, 137–152. doi: 10.1080/17439760701756946
Pilkonis, P. A., Choi, S. W., Reise, S. P., Stover, A. M., Riley, W. T., Cella, D., et al. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment 18, 263–283. doi: 10.1177/1073191111411667
Pilkonis, P. A., Yu, L., Dodds, N. E., Johnston, K. L., Maihoefer, C. C., and Lawrence, S. M. (2014). Validation of the depression item bank from the Patient-Reported Outcomes Measurement Information System (PROMIS) in a three-month observational study. J. Psychiatr. Res. 56, 112–119. doi: 10.1016/j.jpsychires.2014.05.010
Pinard, C., Smith, T. M., Calloway, E. E., Fricke, H. E., Bertmann, F. M., and Yaroch, A. L. (2016). Auxiliary measures to assess factors related to food insecurity: Preliminary testing and baseline characteristics of newly designed hunger-coping scales. Prev. Med. Rep. 4, 289–295. doi: 10.1016/j.pmedr.2016.06.021
Puddephatt, J-A., Keenan, G. S., Fielden, A., Reaves, D. L., Halford, J. C. G., and Hardman, C. A. (2020). “Eating to survive”: A qualitative analysis of factors influencing food choice and eating behaviour in a food-insecure population. Appetite 147, 104547. doi: 10.1016/j.appet.2019.104547
Siefert, K., Finlayson, T. L., Williams, D. R., Delva, J., and Ismail, A. I. (2007). Modifiable risk and protective factors for depressive symptoms in low-income African American Mothers. Am. J. Orthopsychiatr. 77, 113–123. doi: 10.1037/0002-9432.77.1.113
Smith, M. D., Rabbitt, M. P., and Coleman-Jensen, A. (2017). Who are the world's food insecure? New evidence from the food and agriculture organization's food insecurity experience scale. World Dev. 93, 402–412. doi: 10.1016/j.worlddev.2017.01.006
Smith, T. D., and McMillan, B. F. (2001). “A primer of model fit indices in structural equation model,” in Paper Presented at the Annual Meeting of the Southwest Educational Research Association (New Orleans, LA).
Tuthill, E. L., Sheira, L. A., Palar, K., Frongillo, E. A., Wilson, T. E., Adedimeji, A., et al. (2019). Persistent food insecurity is associated with adverse mental health among women living with or at risk of HIV in the United States. J. Nutr. 149, 240–248, doi: 10.1093/jn/nxy203
USDA Economic Research Service (2021). Food Security and Nutrition Assistance. Available online at: https://www.ers.usda.gov/data-products/ag-and-food-statistics-charting-the-essentials/food-security-and-nutrition-assistance/#:~:text=Spending%20on%20USDA's%20food%20and,of%20%24122.8%20in%20FY%202020 (accessed December 9, 2022).
Weersink, A., von Massow, M., Bannon, N., Ifft, J., Maples, J., McEwan, K., et al. (2021). COVID-19 and the agri-food system in the United States and Canada. Agricult. Syst. 188, 103039. doi: 10.1016/j.agsy.2020.103039
Wehler, C., Weinreb, L. F., Huntington, N., Scott, R., Hosmer, D., Fletcher, K., et al. (2004). Risk and protective factors for adult and child hunger among low-income housed and homeless female-headed families. Am. J. Public Health 94, 109–115. doi: 10.2105/AJPH.94.1.109
Weiser, S. D., Young, S. L., Cohen, C. R., Kushel, M. B., Tsai, A. C., Tien, P. C., et al. (2011). Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am. J. Clin. Nutr. 94, 1729S−1739S. doi: 10.3945/ajcn.111.012070
Whitaker, R. C., Phillips, S. M., and Orzol, S. M. (2006). Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics 118, e859–e868. doi: 10.1542/peds.2006-0239
Keywords: food security, mental health, maternal health, conceptual framework, social support
Citation: Liebe RA, Adams LM, Hedrick VE, Serrano EL, Porter KJ, Cook NE and Misyak SA (2023) Developing a conceptual framework for the relationship between food security status and mental health among low-income mothers. Front. Sustain. Food Syst. 6:1078811. doi: 10.3389/fsufs.2022.1078811
Received: 24 October 2022; Accepted: 13 December 2022;
Published: 05 January 2023.
Edited by:
Ginny Lane, University of Idaho, United StatesReviewed by:
Edward Frongillo, University of South Carolina, United StatesMojtaba Shafiee, University of Saskatchewan, Canada
Copyright © 2023 Liebe, Adams, Hedrick, Serrano, Porter, Cook and Misyak. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah A. Misyak,  c21pc3lha0B2dC5lZHU=
c21pc3lha0B2dC5lZHU=
 Rachel A. Liebe
Rachel A. Liebe Leah M. Adams2
Leah M. Adams2 Valisa E. Hedrick
Valisa E. Hedrick Kathleen J. Porter
Kathleen J. Porter Sarah A. Misyak
Sarah A. Misyak