- Department of Physiology and Comprehensive Alcohol-HIV/AIDS Research Center, Louisiana State University Health Sciences Center, New Orleans, LA, United States
Introduction: Alcohol use disorder (AUD) is a psychiatric disease that affects approximately 10% of the population. Individuals suffer from a myriad of causes and consequences of AUD, and team-based management of patients is often required for given the chronic and complex nature of the disease. Interprofessional education (IPE) for biomedical science and health professional students that incorporates patient-centered cases focused on AUD and adjacent stress-related disorders may improve future collaboration in managing these conditions and community outcomes related to wellbeing.
Methods: This study assessed the impact of a single, 90-minute IPE exercise on improving confidence in possessing the knowledge and skills required for screening and management of patients at risk for AUD, the role of social determinants in health and stress-related diseases, and the importance of supporting the mental health of professionals to improve patient care. The exercise was provided to three groups of post-baccalaureate students (physician assistant [PA], physical therapy [PT], and biomedical sciences [BMS] graduate programs) within a human physiology course. Pre- and post-test surveys were administered via web-based platform before and after the session.
Results: We found significant improvements in responses to seven of the eight assessment questions, including improved knowledge of one’s role in biomedical research or brief interventions for alcohol misuse, increased confidence in advising patients and community members about responsible alcohol drinking, and improved understanding of the role of all three professions (PA, PT, and BMS) in managing, treating, or researching stress-related disorders.
Discussion: These findings suggest that a single focused IPE session is impactful for improving student knowledge and understanding of stress-related disorders. IPE may represent an important educational strategy to bring together future scientists and health professionals to reflect upon unique and shared knowledge bases as well as integrative care principles for both patient and professional wellbeing.
Introduction
The majority of healthcare settings increasingly rely on interprofessional teams and collaboration when managing patients in order to provide optimal care. In concert with this growing need, interprofessional education (IPE) has grown as both a key program accreditation standard and a critical component of the early curriculum for health professions students for improving the skills and understanding required to work as a successful member of a healthcare team. The treatment of stress-related psychiatric disorders, including alcohol use disorder (AUD), incorporates several professions, with optimal patient care requiring contributions from various healthcare domains including primary care, psychiatry, nursing, physical therapy, and physician assistants. Importantly, even more points of care are involved in screening for alcohol use and AUD risk (e.g., as part of routine dental screening). As treatments for AUD are limited, the preclinical work of biomedical scientists is also critical to better understand the pathophysiology underlying this and other stress-related conditions to improve therapeutic options for treating these vulnerable patient populations.
AUD is a chronic, relapsing psychiatric disorder characterized by a lack of control over alcohol consumption and the emergence of negative affective symptoms over time (Nehring et al., 2024). It affects approximately 10% of the population in the United States and is a life-long condition that must be carefully managed to prevent relapse (Grant et al., 2017). Beyond its psychiatric manifestation, AUD can also produce systematic adverse consequences, resulting in pathophysiology in nearly every organ system throughout the body (Simon et al., 2021). Thus, it is important that all healthcare professionals are aware of the screening process for at-risk drinking and AUD and feel comfortable discussing alcohol consumption with their patients. The United States Preventive Services Task Force (USPSTF) recommends screening for unhealthy alcohol use in adults 18 or older in primary care settings and providing counseling to those who engage in hazardous drinking (US Preventive Services Task Force et al., 2018). Even though individuals welcome a discussion from their health care providers about responsible alcohol use (Miller et al., 2006a, 2006b; Broyles et al., 2012), screening and brief intervention strategies are underutilized in clinical practice (Bazzi and Saitz, 2018).
Social determinants of health, such as relative economic stability, education access and quality, and health care access and quality, can also influence the development and severity of many stress-related disorders. These disorders encompass psychiatric conditions, including substance use disorders, generalized anxiety disorder, and major depressive disorder, along with somatic manifestations of chronic stress such as cardiovascular disease and metabolic syndrome (Alegría et al., 2018; Satyjeet et al., 2020). Together, these social determinants influence an individual’s allostatic load, which encompasses the cumulative burden of stress and maladaptive physiological responses to the stress (Guidi et al., 2021). Management of patients thus necessitates consideration of these social determinants and the allostatic load that may be contributing to patients’ adverse health outcomes. Thus, the patient case in our study included discussion on social determinants of health and their contribution to health outcomes in a patient at risk for AUD. Furthermore, while biomedical scientists are typically not directly patient-facing, they play an important role in conceptualizing and modeling stress-related disorders and advancing our understanding of the pathophysiology underlying these conditions for the development of better therapeutics, underscoring the need for heightened translational relevance of their work.
Louisiana State University Health Sciences Center at New Orleans (LSUHSC-NO) established the Office for Interprofessional Education and Collaborative Practice (IPECP) in 2015 to support student learning and faculty training in IPE. Its primary mission is to increase interprofessional learning for students across all six schools (Allied Health, Dentistry, Graduate Studies, Medicine, Nursing, and Public Health) by assisting faculty in the development, implementation, and assessment of meaningful IPE experiences. The establishment of this office led to several studies evaluating the effectiveness of either single IPE sessions or longitudinal IPE course participation. Previous work from our group has focused on the introduction of a single IPE session into the renal and/or endocrine blocks of a graduate-level human physiology course at LSUHSC consisting of physician assistant (PA), physical therapy (PT), and biomedical sciences (BMS) graduate students. These studies found that IPE sessions improve student understanding and interprofessional competence following either single (Edwards et al., 2017, 2018; Harrison-Bernard et al., 2017) or multiple (Harrison-Bernard et al., 2019) IPE sessions. However, the present study is the first to introduce a case focused on AUD and team-based management of stress-related disorders in vulnerable populations.
This study also addressed provider burn out, an important topic that is often neglected in the formal curriculum of healthcare professional students. Introduced by Berwick and colleagues in 2008, the Triple Aim is a system of goals aimed at improving population health, improving the experience of the patient, and reducing costs associated with healthcare (Ryan et al., 2016). More recently, this model has been updated to include a fourth aim—improving the work life of health care providers (Bodenheimer and Sinsky, 2014). Thus, our session also incorporated discussion regarding burnout and stress management in different healthcare careers, including patient-facing and non-patient facing biomedical science careers.
Overall, the goal of this study was to assess the impact of a single interprofessional session on the knowledge and skills required for screening and managing patients with AUD and the role of stress and social determinants of health in disease. This study targeted three different groups of healthcare professional students (physical therapy, physician assistant, and biomedical graduate studies) in a single physiology course.
Materials and methods
An overarching goal of our IPE curriculum is to quantify the impact of interprofessional interactions among several health professional students during their formative years of education at LSUHSC. For purposes of the current study, students were assigned to small teams comprised of all three health professions and provided class time to discuss a simulated patient case, along with additional training materials to facilitate learning and discussion that included an alcohol fact sheet (see Supplementary material) and literature commentaries on burnout from PA (Tetzlaff et al., 2020), PT (Pugliese et al., 2023), and biomedical science (Nagy et al., 2019) perspectives in addition to an introduction to the Quadruple Aim (Bodenheimer and Sinsky, 2014). Web-based survey assessments of their knowledge and perceptions regarding the role of each profession in stress-related disease research or care, the role of social determinants of health and stress in health and disease, and confidence in their own abilities to counsel patients about their alcohol drinking were given before and after the session.
Participants
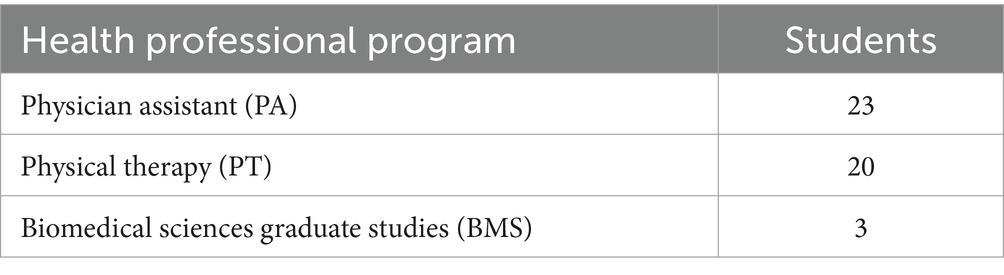
A total of 77 first-year students representing three health professions at LSUHSC-NO were given the opportunity to participate in the voluntary 90-min IPE exercise in March 2024. They were organized into 7 small, professionally diverse groups (11 members per group, n = 5 physician assistant [PA], n = 5 physical therapy [PT], and n = 1 biomedical sciences [BMS]). Responses were only evaluated from students who completed both the pre- and post-tests (n = 46, 60% response rate). Table 1 shows the distribution of students across the three professions. The authors (one MD/PhD student and one course instructor) served as facilitators and were available to answer questions about the exercise and to provide encouragement and direction. This educational study was conducted with LSUHSC-NO IRB approval (IRB #7002).
Program and study design
For the present study, we designed and presented a 90-min IPE training module to provide students with training on an interprofessional approach to screening patients for alcohol use and managing patients with stress-related disorders. The objectives of this case were to: (1) identify the characteristics of binge drinking and heavy drinking, as defined by the National Institute of Alcohol Abuse and Alcoholism (NIAAA); (2) describe the role of stress in promoting alcohol use disorder (AUD); (3) understand how to assess sources of psychosocial stress in vulnerable populations; (4) discuss methods for reducing burnout in your chosen profession (PA, PT, Biomedical Sciences); and (5) explain the role of PA, PT, and Biomedical Sciences professionals in combating stress-related diseases. A simulated patient case (see Supplementary material) was presented to facilitate discussion surrounding care for a patient presenting with multiple comorbidities, including AUD and human immunodeficiency virus (HIV) infection, and how these may be exacerbated by psychosocial stress factors as guided by discussion of the PRAPARE Protocol for Responding to & Assessing Patients’ Assets, Risks & Experiences (PRAPARE®) tool, a national patient risk screening tool for assessing social determinants of health (Weir et al., 2020). This also led to discussion about the unique roles of biomedical scientists, physician assistants, and physical therapists in the research and care process.
The learning objectives of the session also corresponded to the following competencies established by the Interprofessional Education Collaborative (IPEC, 2023): (1) Values and Ethics (VE11)—Support a workplace where differences are respected, career satisfaction is supported, and well-being is prioritized; (2) Roles and Responsibilities (RR3)—Incorporate complementary expertise to meet health needs including the determinants of health; and (3) Roles and Responsibilities (RR4)—Differentiate each team member’s role, scope of practice, and responsibility in promoting health outcomes.
Data collection and analysis
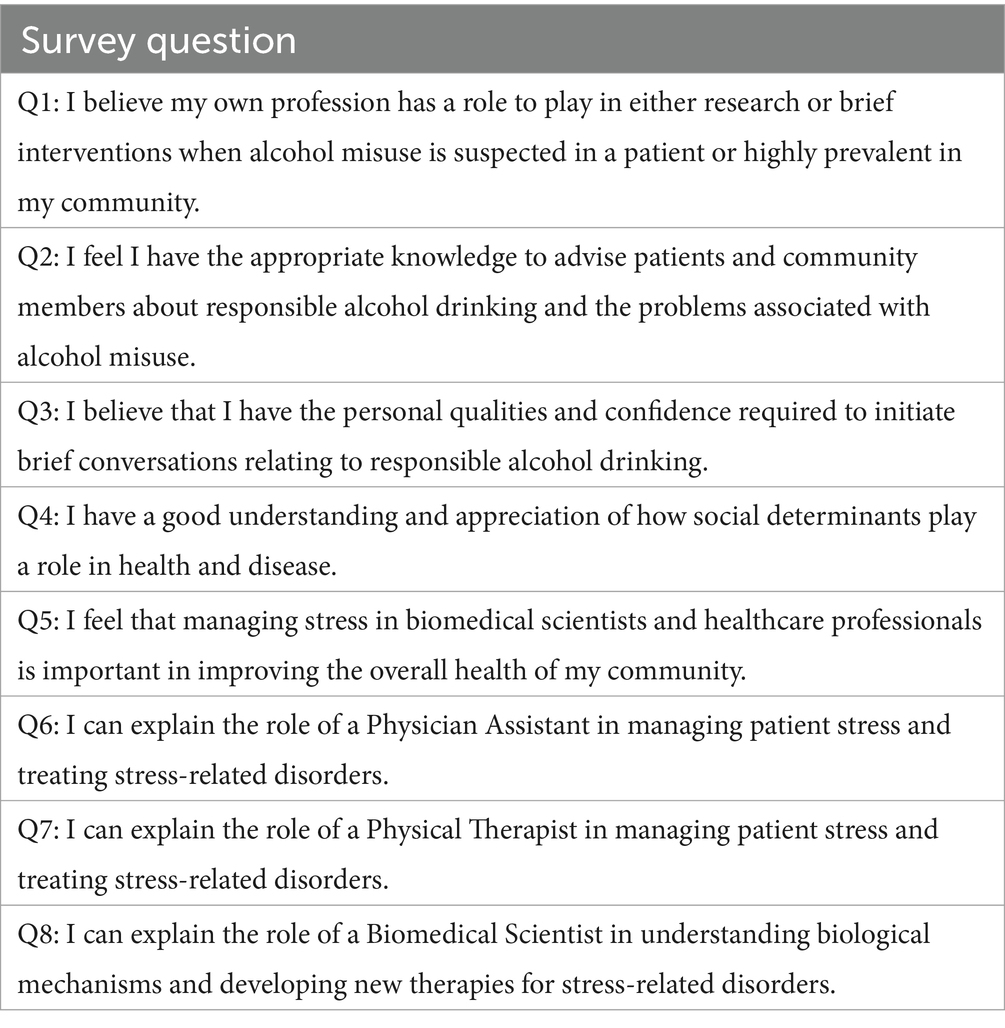
Anonymous and voluntary survey questionnaires were made available online via a web-based platform (Moodle) before and after the 90-min session (Table 2). Responses to questions used a 5-point Likert-scale with responses ranging from 1 (strongly disagree) to 5 (strongly agree), and changes in response before and after the session (n = 46) were analyzed using the Wilcoxon matched-pairs signed-rank testing. The Wilcoxon sum of signed ranks (W) was calculated, and a p-value less than 0.05 was used to indicate statistical significance. All analyses were performed using GraphPad Prism 9 for macOS (San Diego, CA, USA).
Results
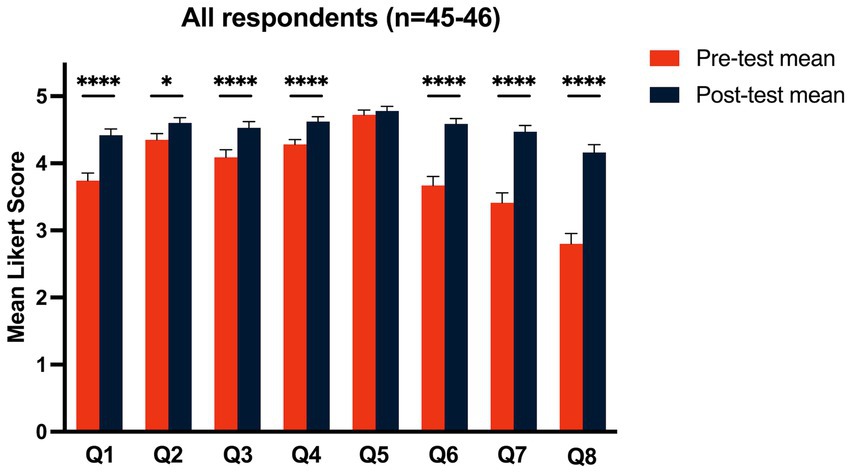
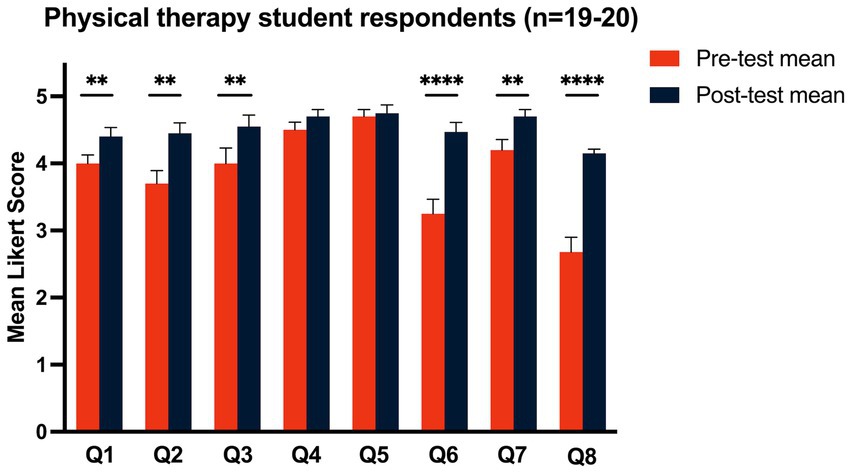
Overall, 60% of students (n = 46) participated in both the pre- and post-test surveys across all three programs. Paired data was collected from 23 physician assistant (PA), 20 physical therapy (PT), and three biomedical science (BMS) students (Table 1). Eight questions addressed knowledge (Q2 and Q4), perceptions (Q1, Q3, Q5), and confidence (Q6–Q8) explaining the roles of the three health professions in managing stress-related disorders, including AUD (Table 2). Survey responses to the eight survey questions across all three programs (n = 46) are shown in Figure 1 where we compared means observed before and after the training exercise. We found significant increases in scores for seven of the eight questions, with the largest increases in Q6 (reflecting increased ability to explain the role of a PA in managing patient stress and treating stress-related disorders), Q7 (reflecting increased ability to explain the role of a PT in managing patient stress and treating stress-related disorders), and Q8 (reflecting increased ability to explain the role of a biomedical scientist in understanding biological mechanisms and developing new therapies for stress-related disorders). Additional significant improvements were seen in Q1 (reflecting increased understanding of the role of their own profession in research or interventions for patients with alcohol misuse), Q3 (reflecting increased confidence in the personal qualities required to initiate conversations regarding responsible alcohol drinking), Q4 (reflecting increased understanding and appreciation of the role of social determinants in health and disease), and Q2 (reflecting increased knowledge to advise patients and community members about responsible alcohol drinking and the risks of alcohol misuse). We did not see significant changes in the response to Q5, which addressed the importance of managing stress in biomedical scientists and healthcare professionals for improving the health of the community. Notably, baseline scores for Q5 were high (4.72) in the pre-test and increased slightly (4.78) in the post-test, reflecting a high appreciation for this concept in students even before the exercise.
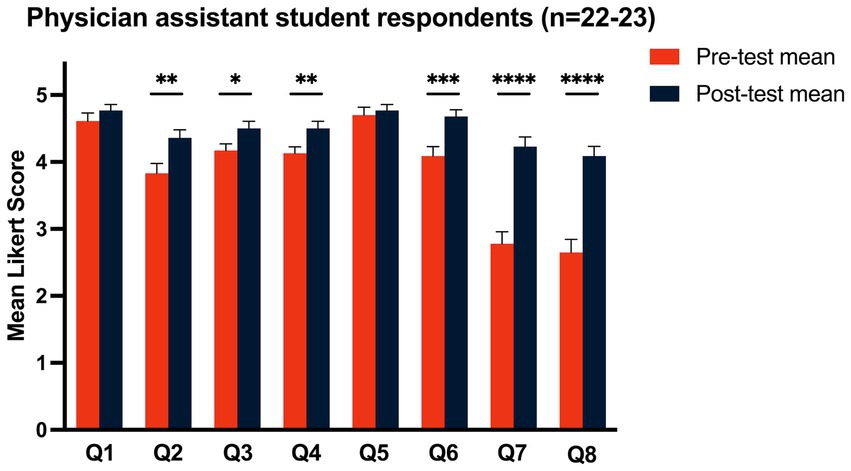
We next examined how changes in survey responses compared between PA and PT students. Unfortunately, we could not include BMS students due to the low response rate and insufficient power to detect group differences (n = 3). Figures 2, 3 show the responses for PA and PT students, respectively. Among PA students, we found significant increases in Likert scores for all questions except Q1 and Q5 (Figure 2). Interestingly, the most significant increases were seen in Q7 and Q8, reflecting an increase in PA students understanding of the role of the two other healthcare professional programs (PT and BMS). PT students showed significant increases in Likert scores for all questions except Q4 and Q5. Similar to the PA students, the PT students had the greatest increases in scores for questions regarding their ability to explain the role of the other two professions (PA and BMS, Q6 and Q8) (Figure 3). They also showed a large significant increase in their scores for Q2, reflecting a robust increase in their confidence in their knowledge to advise patients about responsible alcohol drinking and the problems associated with alcohol misuse.
Discussion
This study sought to engage students representing three professions in a discussion regarding screening for at-risk alcohol use and consideration of the role of social determinants of health in the development of stress-related disorders. Importantly, the interprofessional focus of the 90-min exercise allowed students to work as a team and learn from other students about the role of researchers and distinct healthcare professionals. Overall, we found significant improvements in Likert scores on seven of the eight assessment questions across when tabulated across all three healthcare professional students (Figure 1). These improvements included increased knowledge of one’s role in research or brief interventions for alcohol misuse, increased confidence in advising patients and community members about responsible alcohol drinking, and improved understanding of the role of all three professions (PA, PT, and biomedical scientist) in managing, treating, or researching stress-related disorders. Indeed, the most robust improvements were seen in confidence in explaining the roles of the three professions, highlighting the importance of the interprofessional nature of these sessions (Figure 1, Q6–Q8).
In addition to at-risk alcohol use, the case also incorporated discussion on the role of psychosocial stress and social determinants of health in vulnerable populations. This included examination of the Protocol for Responding to & Assessing Patients’ Assets, Risks & Experiences (PRAPARE®) tool, a national patient risk screening tool for assessing social determinants of health (Weir et al., 2020). Students discussed the practicality of this instrument, along with its limitations. For example, limited time allotted for interacting with the patient may limit the feasibility of using the PRAPARE® tool. Another consideration is the intimate nature of the questions listed in the instrument. Nonetheless, exposure to this tool early in healthcare students’ training may improve their understanding of the multitude of factors that can contribute to a patient’s overall health and lead to future use of instruments like the PRAPARE® tool. A limitation of the current study is our inability to know how this training will impact future translational research and collaborative care of AUD and other stress-related disorders in vulnerable populations. Few studies have examined the long-term impact of early exposure to IPE experiences, although two recent studies have shown positive qualitative and quantitative changes in knowledge, understanding and interest in social determinants of health following either a 13-week longitudinal IPE experience or a single asynchronous online workshop (Rulli et al., 2023; Peeters et al., 2024). Additional studies are necessary to better understand how these IPE experiences during training can impact future practice as a healthcare professional or biomedical scientist.
Through the case and discussion of the PRAPARE® instrument, our results demonstrated significant improvements in understanding and appreciation of the role of social determinants in health and disease across all three professions (Figure 1, Q4). Interestingly, scores to this question were significantly increased in PA students but not PT students (Figures 2, 3, Q4). This difference may be due to a higher baseline score to this question in the PT group, which may be attributed to differences in preexisting training or educational stage at the time of the IPE session. Importantly, PT students participated in this session during their third semester, while PA students were in their first semester. Thus, it is possible that PA students have not yet learned about social determinants of health in their own curriculum, while PT students may have already been exposed to this concept. Unfortunately, only three biomedical science graduate students participated in the survey and thus we could not analyze their data separately due to insufficient statistical power.
Although we could not separately analyze data from the biomedical science graduate students, we found significant improvements in recognizing the role of a biomedical scientist in understanding biological mechanisms and developing new therapies for stress-related disorders, both overall and among PA and PT students. Despite that fact that graduate students are not directly patient-facing, inclusion of biomedical science graduate students in IPE sessions is essential for facilitating conversations between preclinical researchers and healthcare providers and improving the translatability of their work. Additionally, understanding the biology and hormonal systems that are implicated or dysregulated in stress-related disorders is critical for optimizing patient care (Fitzpatrick-Schmidt and Edwards, 2023). For graduate students, it is important to understand the limits of how different diseases can be modeled and the limitations on translational validity of these models. Thus, the overall goal for inclusion of these students in the session is to highlight the translational relevance of the work of biomedical scientists and facilitate conversations with patient-facing healthcare workers early in both students’ careers. Reasons for the relative lack of engagement in biomedical sciences students in the present work may be due to their drastic under-representation on the student groups (limiting psychological safety), and future studies are encouraged to include groups with greater balance among professions when possible.
Importantly, this study was the first to incorporate an interprofessional AUD-based training exercise into our institution’s PA curriculum. Previous work at our institution from Edwards and colleagues assessed changes in attitudes about alcohol and confidence in screening and AUD prevention across 10 different healthcare professions, including PT students, after a single IPE session, although PA students were not included (Edwards et al., 2023). In the present study, we saw significant improvements in PA student knowledge and confidence in addressing AUD and stress-related disorders (Figure 2). Another recent study (Karagiannis et al., 2024) discovered attitudinal improvements in PA and other student populations after a half-day IPE event focused on opioid use disorder, suggesting that early educational strategies aimed at team-based care to prevent misuse of other substances is also viable. Our findings in PT students from the present study are consistent with our previous work conducted in a larger setting, which also showed significant improvements in knowledge and confidence advising patients regarding responsible alcohol consumption.
Finally, this study sought to introduce the concept of the Quadruple Aim, an expansion of the Triple Aim that includes well-being of the healthcare team. Recently, the Quadruple Aim has been suggested to facilitate improved health outcomes at lower costs, while advocating for the mental health of healthcare workers. Indeed, the recent coronavirus (COVID-19) pandemic has resulted in additional stress and challenges for a spectrum of healthcare professionals (Leo et al., 2021). We propose here that exposure to the Quadruple Aim early in the training curriculum may result in a greater appreciation of well-being of fellow healthcare workers, especially given the rise of burnout in the COVID-19 era. Interestingly, we did not see a significant improvement in scores for question 5, which addressed the importance of managing stress in biomedical scientists and healthcare professionals, either overall or in PA or PT students alone; however, baseline scores for this question were higher than baseline scores for all the other questions, which may preclude our ability to detect significant improvements in the post-test responses. This result may even be interpreted as encouraging since students appear already focused on culturing wellness and self-care as they embark on their future careers.
Limitations of the present study include the small sample size, particularly for the biomedical science graduate students, and the lack of validated assessments, which are not readily available for this field. The small sample size extends from the relatively small class size, but future studies plan to extend this work to larger interprofessional classes with more students. Although we did intentionally re-use some of the questions from a previous study to directly compare across cohorts (Edwards et al., 2023), one of our future aims is to work with other alcohol research centers to develop a validated questionnaire for use across multiple centers and studies.
In conclusion, we demonstrate that a single IPE session for PA, PT, and biomedical science graduate students improves knowledge of one’s role in research or brief interventions for at-risk alcohol use, confidence in advising patients and community members about responsible alcohol drinking, and improved understanding of the role of three distinct professions (PA, PT, and biomedical scientist) in managing, treating, or researching stress-related disorders. Importantly, we found the most robust improvements in confidence in explaining the roles of the three professions, further emphasizing the utility of the interprofessional focus of these sessions. We believe that introduction to tools such as the PRAPARE® instrument and the Quadruple Aim early in the didactic curriculum for these healthcare and graduate students may improve comfort with incorporating these tools into their clinical practice or research, increase the likelihood of successful team collaborations, and increase confidence in diagnosing or researching stress-related disorders including AUD.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the LSU Health-New Orleans IRB (#7002). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TF-S: Conceptualization, Data curation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing. SE: Conceptualization, Formal analysis, Funding acquisition, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was generously supported by the following training and research grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA): F30AA030941, P60AA009803, and T32AA007577.
Acknowledgments
We would like to acknowledge Dr. Tina Gunaldo and the Office of Interprofessional Education and Collaborative Practice at LSU Health-New Orleans for their support of IPE and training of the authors. The authors would also like to thank the American Physiological Society (APS) Teaching of Physiology Section for their generous support of TFS through a William Galey Professional Skills Scholarship Award.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2024.1431409/full#supplementary-material
References
Alegría, M., NeMoyer, A., Falgàs Bagué, I., Wang, Y., and Alvarez, K. (2018). Social determinants of mental health: where we are and where we need to go. Curr. Psychiatry Rep. 20:95. doi: 10.1007/s11920-018-0969-9
Bazzi, A., and Saitz, R. (2018). Screening for unhealthy alcohol use. JAMA 320, 1869–1871. doi: 10.1001/jama.2018.16069
Bodenheimer, T., and Sinsky, C. (2014). From triple to quadruple aim: care of the patient requires care of the provider. Ann. Fam. Med. 12, 573–576. doi: 10.1370/afm.1713
Broyles, L. M., Rosenberger, E., Hanusa, B. H., Kraemer, K. L., and Gordon, A. J. (2012). Hospitalized patients’ acceptability of nurse-delivered screening, brief intervention, and referral to treatment. Alcohol. Clin. Exp. Res. 36, 725–731. doi: 10.1111/j.1530-0277.2011.01651.x
Edwards, S., Ferguson, T. F., Gasparini, S., Mercante, D. E., Molina, P. E., and Gunaldo, T. P. (2023). Interprofessional education as a potential foundation for future team-based prevention of alcohol use disorder. BMC Med. Educ. 23:126. doi: 10.1186/s12909-023-04100-y
Edwards, S., Molina, P. E., McDonough, K. H., Mercante, D. E., and Gunaldo, T. P. (2017). Integrating an interprofessional education experience into a human physiology course. J. Physician Assist. Educ. 28, 146–148. doi: 10.1097/JPA.0000000000000132
Edwards, S., Molina, P. E., McDonough, K. H., Mercante, D. E., and Gunaldo, T. P. (2018). The potential of interprofessional education to translate physiology curricula effectively into future team-based healthcare. Adv. Physiol. Educ. 42, 354–359. doi: 10.1152/advan.00183.2017
Fitzpatrick-Schmidt, T., and Edwards, S. (2023). Cortisol as a risk biomarker to guide recovery from substance use disorders. Alcohol Clin. Exp. Res. 47, 435–437. doi: 10.1111/acer.15018
Grant, B. F., Chou, S. P., Saha, T. D., Pickering, R. P., Kerridge, B. T., Ruan, W. J., et al. (2017). Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry 74, 911–923. doi: 10.1001/jamapsychiatry.2017.2161
Guidi, J., Lucente, M., Sonino, N., and Fava, G. A. (2021). Allostatic load and its impact on health: a systematic review. Psychother. Psychosom. 90, 11–27. doi: 10.1159/000510696
Harrison-Bernard, L. M., Naljayan, M. V., Eason, J. M., Mercante, D. E., and Gunaldo, T. P. (2017). Effectiveness of interprofessional education in renal physiology curricula for health sciences graduate students. Adv. Physiol. Educ. 41, 594–598. doi: 10.1152/advan.00120.2017
Harrison-Bernard, L. M., Naljayan, M. V., Mercante, D. E., Gunaldo, T. P., and Edwards, S. (2019). Longitudinal interprofessional education in a graduate physiology course. Adv. Physiol. Educ. 43, 241–245. doi: 10.1152/advan.00007.2019
IPEC (2023). Core competencies for interprofessional collaborative practice: Version 3. Washington, DC: Interprofessional Education Collaborative.
Karagiannis, C., Liang, J., Pierre, S. S., Brody, C., and Kinnevey, C. (2024). Evaluating attitudes among healthcare graduate students following interprofessional education on opioid use disorder. J. Osteopath Med. 124, 85–93. doi: 10.1515/jom-2023-0132
Leo, C. G., Sabina, S., Tumolo, M. R., Bodini, A., Ponzini, G., Sabato, E., et al. (2021). Burnout among healthcare workers in the COVID 19 era: a review of the existing literature. Front. Public Health 9:750529. doi: 10.3389/fpubh.2021.750529
Miller, P. M., Ravenel, M. C., Shealy, A. E., and Thomas, S. (2006a). Alcohol screening in dental patients: the prevalence of hazardous drinking and patients’ attitudes about screening and advice. J. Am. Dent. Assoc. 137, 1692–1698. doi: 10.14219/jada.archive.2006.0115
Miller, P. M., Thomas, S. E., and Mallin, R. (2006b). Patient attitudes towards self-report and biomarker alcohol screening by primary care physicians. Alcohol Alcohol. 41, 306–310. doi: 10.1093/alcalc/agl022
Nagy, G. A., Fang, C. M., Hish, A. J., Kelly, L., Nicchitta, C. V., Dzirasa, K., et al. (2019). Burnout and mental health problems in biomedical doctoral students. CBE Life Sci. Educ. 18:ar27. doi: 10.1187/cbe.18-09-0198
Nehring, S. M., Chen, R. J., and Freeman, A. M. (2024). “Alcohol use disorder” in StatPearls (Treasure Island (FL): StatPearls Publishing).
Peeters, M. J., D’Amico, A., Khadka, S., Cleary, H. M., and Singh, S. (2024). Interacting within an asynchronous online interprofessional education workshop focused on social determinants of health. Curr. Pharm. Teach. Learn. 16, 196–201. doi: 10.1016/j.cptl.2023.12.031
Pugliese, M., Brismée, J.-M., Allen, B., Riley, S., Tammany, J., and Mintken, P. (2023). Mentorship and self-efficacy are associated with lower burnout in physical therapists in the United States: a cross-sectional survey study. J. Educ. Eval. Health Prof. 20:27. doi: 10.3352/jeehp.2023.20.27
Rulli, D., Smith, L. J., Escalera-Torres, A., and Anderson, O. S. (2023). Experiential interprofessional education rooted in the social determinants of health and ecological model fosters interprofessional socialization. J. Allied Health 52, 172–179
Ryan, B. L., Brown, J. B., Glazier, R. H., and Hutchison, B. (2016). Examining primary healthcare performance through a triple aim lens. Healthc. Policy 11, 19–31. doi: 10.12927/hcpol.2016.24521
Satyjeet, F., Naz, S., Kumar, V., Aung, N. H., Bansari, K., Irfan, S., et al. (2020). Psychological stress as a risk factor for cardiovascular disease: a case-control study. Cureus 12:e10757. doi: 10.7759/cureus.10757
Simon, L., Edwards, S., and Molina, P. E. (2021). Pathophysiological consequences of at-risk alcohol use; implications for comorbidity risk in persons living with human immunodeficiency virus. Front. Physiol. 12:758230. doi: 10.3389/fphys.2021.758230
Tetzlaff, E. D., Coplan, B., Bernard, K., Sierra, T., and Dominguez, D. (2020). Addressing PA burnout. JAAPA 33, 10–11. doi: 10.1097/01.JAA.0000668840.02042.2c
US Preventive Services Task ForceCurry, S. J., Krist, A. H., Owens, D. K., Barry, M. J., Caughey, A. B., et al. (2018). Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US preventive services task force recommendation statement. JAMA 320, 1899–1909. doi: 10.1001/jama.2018.16789
Keywords: interprofessional education, alcohol use screening, stress, physician assistant, physical therapist, biomedical sciences graduate students
Citation: Fitzpatrick-Schmidt T and Edwards S (2024) Interprofessional education to support alcohol use screening and future team-based management of stress-related disorders in vulnerable populations. Front. Educ. 9:1431409. doi: 10.3389/feduc.2024.1431409
Edited by:
Meriem Khaled Gijón, University of Granada, SpainReviewed by:
José Gijón Puerta, University of Granada, SpainSoledad Domene Martos, Sevilla University, Spain
Copyright © 2024 Fitzpatrick-Schmidt and Edwards. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Scott Edwards, c2Vkd2E1QGxzdWhzYy5lZHU=
†ORCID: Scott Edwards, orcid.org/0000-0002-0865-7758
 Taylor Fitzpatrick-Schmidt
Taylor Fitzpatrick-Schmidt Scott Edwards*†
Scott Edwards*†