
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 09 January 2023
Sec. Heart Valve Disease
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.1047715
 Tie Zheng†
Tie Zheng† Yichen Zhao†
Yichen Zhao† Qing Ye
Qing Ye Shuai Zheng
Shuai Zheng Fei Meng
Fei Meng Qiuming Hu
Qiuming Hu Haibo Zhang
Haibo Zhang Jie Han
Jie Han Baiyu Tian
Baiyu Tian Junming Zhu*
Junming Zhu* Jiangang Wang*
Jiangang Wang*Objective: To determine whether different changes of pulmonary artery systolic pressure (PASP) after surgeries have an impact on the long-term outcomes in patients with rheumatic and degenerative mitral valve (MV) disease and atrial fibrillation.
Methods: Between 2004 and 2016, 1,188 patients with rheumatic and degenerative MV disease undergoing MV and Cox-Maze procedure were identified. Clinic outcomes, as well as rhythm state and echocardiography indices in long-term follow-up were recorded. Patients were grouped by the changes of PASP (persistently normal, persistently increased, increased, and decreased) from preoperative estimation to follow-up.
Results: A complete echocardiography was performed at baseline and after 5 years. During follow-up, free of death and atrial fibrillation (AF) off antiarrhythmic drugs was 90 and 61%, 78 and 41% at 5 and 10 years, respectively. Survival rate was higher in patients with persistently normal and became worse in patients with persistently increased and increased PASP (log-rank 166.0, P < 0.0001). Moreover, the patients with persistently normal PASP had a lowest risk of recurrent AF (SHR: 0817; CI: 0.765–0.872; P < 0.0001) after considering death as a competing risk. A persistently normal PASP at follow-up and degenerative MV disease were associated with improved survival and sinus rhythm (SR) maintenance at multivariable Cox regression analysis (P < 0.05).
Conclusion: Patients with degenerative MV disease or have persistently normal PASP during follow-up have better survival and SR maintenance rate than patients with either rheumatic MV disease or persistently abnormal PASP.
How are the impacts of pulmonary arterial systolic pressure on patients with mitral valve disease combined with atrial fibrillation?
A persistently normal PASP at follow-up and degenerative MV disease were associated with improved survival and sinus rhythm maintenance.
For patients with rheumatic mitral diseases, more active interventions for valve disease and atrial fibrillation should be considered if PASP had obvious abnormity.
Pulmonary hypertension (PH) was known as one of serious complications of mitral valve (MV) disease, was originally reported in patients with rheumatic MV disease (RMVD) (1, 2). Recent studies have also showed that significant PH was present in patients with severe degenerative MV disease (DMVD) (3). More importantly, with more increasing evidences supporting the independent role of PH on negative long-term prognostic implications (4), the importance of PH deserves more attention.
Among patients with RMVD or DMVD, nearly 50% of them present with atrial fibrillation (AF), who needs to be treated with Cox-Maze procedure during cardiac operation according to the current guideline (5). Although Prof. Damiano found that the patients with RMVD or DMVD who underwent Cox-Maze procedure showed similar outcomes in terms of restoring sinus rhythm (SR) during a 41-month follow-up (6), some investigators suggested that the Cox-Maze procedure was less effective in patients with RMVD (7). Therefore, our study was aimed at to characterizing the clinical features and the significance of PH regarding prognosis in a large cohort of patients with RMVD or DMVD after Cox-maze procedure.
This study was approved by the institutional review board (20180723) of Beijing Anzhen Hospital, Capital Medical University. Patients with MV disease and concomitant AF requiring MV and Cox maze procedure were identified with a review of our center’s medical records from 2004 to 2016. Among 1,689 patients initially screened for inclusion, 1,188 patients with rheumatic and degenerative MV disease who discharged alive were included in our study cohort. All patients with non-rheumatic/non-degenerative mitral valve (MV) disease were excluded, which encompassed patients with MV disease secondary to annular dilation or calcification, infectious endocarditis, ischemic heart disease, congenital heart disease and prosthetic valve dysfunction. Patients who underwent tricuspid valve surgeries before were also excluded in this study.
Rheumatic MV disease was determined by the history of acute rheumatic fever. Echocardiographic and intraoperative findings of leaflet thickening, nodularity, and commissural fusion, resulting in narrowing of the valve, were considered as rheumatic MV disease. According to the guidelines, patients could be diagnosed as long-standing persistent AF when their rhythm kept AF for more than 12 months. All patients referred in this study gave informed consent.
MV repair and replacement were performed using standard cardiopulmonary bypass. All the patients underwent a Cox-Maze procedure as described in our previous study, with the bipolar radiofrequency clamp (8). Tricuspid valve (TV) annuloplasty was subsequently performed for patients with moderate or higher TR or tricuspid annular diameter (TAD) more than 40 mm. Details on Cox-maze procedure were shown in Supplementary material.
All echocardiography examinations were conducted in accordance with current guidelines (9). Based on the preoperative PASP, patients were divided into three groups: normal PH, mild PH (35–44 mm Hg), and moderate-to-severe PH (≥ 45 mm Hg) (10). At follow-up, based on changes of PASP changes from baseline to follow-up evaluated by echocardiography, patients were than divided into four groups: (1) persistently normal PASP; (1) decreased PASP (PASP decreased at least one category from baseline); (3) increased PASP (PASP increased least one category from baseline); and (4) persistently increased PASP (Figure 1). Echocardiographic images including standard 2D and Doppler were completed in the parasternal and apical views by trained cardiac sonographers. The measurement of PASP was based on the modified Bernoulli equation which composed of the trans-tricuspid Doppler signal and RA pressure. PASP were acquired by averaging values of at least three times measurements. RA pressure was evaluated based on inferior vena cava diameter (IVCd) and the collapsible index of inferior vena cava (IVC). IVCd was measured from the longitudinal subxiphoid view with M-mode, at end-expiration and end-inspiration, respectively. Then the collapsible index of IVC was calculated [collapsible index of IVC = (IVCd at end-expiration - IVCd at end-inspiration)/IVCd at end-expiration]. After acquiring the IVCd and collapsible index, RA pressure could be divided into three grades (3, 8, and 15 mmHg) according to the ASE recommendations (11).
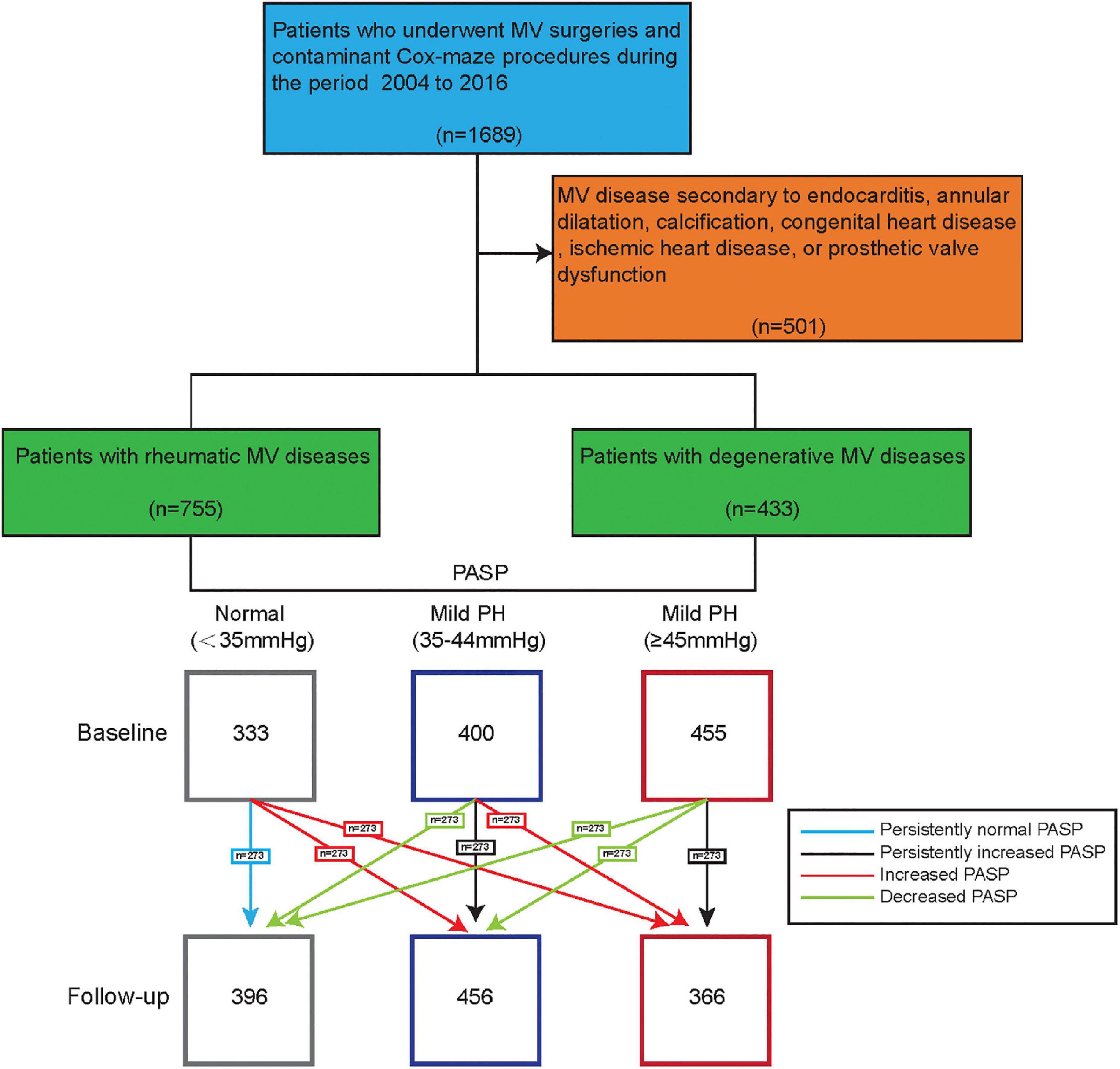
Figure 1. Individual changes of pulmonary artery systolic pressure (PASP) from baseline to 5-year follow-up.
The patients’ clinical profiles and postoperative outcomes were extracted from the hospital medical records. Patients were followed at 3 months, 12 months, and then every year. Recurrent arrhythmia was evaluated by a 24-h Holter. According to the HRS guidelines, late recurrence could be diagnosed when patients meet the following conditions: atrial arrhythmia including AF, atrial flutter or atrial tachycardia which could last more than 30 s and occurred after 3 months following surgery. Sinus rhythm maintenance was defined when the cardiac rhythm was sinus rhythm at each echocardiography evaluation during follow-up. Long-term outcomes were acquired by questionnaires, physician clinical visits during follow-up.
Class I or III antiarrhythmic drugs (AADs) and warfarin were used routinely postoperatively unless contraindicated. If SR could be maintained for 3 months postoperatively, patients would discontinue AADs. Once patients were diagnosed as recurrent AF, they would be informed to restart AADs. Considering the importance of rate control in AF, patients with persistent AF also took other agents, including beta-blockers, digoxin, non-dihydropyridine calcium-channel blockers (CCBs) and so on. Patients’ hemodynamic features, symptoms and heart failure would be taken into consideration when cardiologist determine which agents to use.
The international normalized ratio (INR) were requested to maintain between 2.0 and 2.5 when patients taken oral anticoagulation in the first 6 months after surgery, and those who had mechanical prosthesis or persistent AF were requested to take oral anticoagulation for life.
Categorical variables were presented as frequencies and percentages. Normal distributed continuous variables were presented as mean ± standard deviation (SD). Data among 3 or 4 groups were compared with one way analysis of variance, or Kruskal- Wallis test. Survival analysis were completed with Kaplan- Meier analysis and Cox regression models. The incidence of recurrent AF were compared with competing risk model. A PASP cut-off value for even-free survival were acquired with the analysis of time-dependent receiver operating characteristic curve. Statistical analyses were performed using R 3.6.2 or Stata/SE version 15.
Table 1 showed the clinical and echocardiographic features of the study population (1,188 patients), as shown in Table 1. The mean age of all the patients was 48 (39–57) years; Patients with rheumatic MV disease accounted for 64% of cases, and 36% of patients presented with DMVD. Significant mitral stenosis (mitral valve area: 1.02 ± 0.31 cm2) were observed among all patient with RMVD, and 42% of which showed over moderate mitral regurgitation preoperatively. Patients with RMVD who underwent mitral valve replacement accounted for 14%, and 86% of whom received mitral valve repair. Similarly, 11% of patients with DMVD underwent mitral valve replacement, and 89% of them received mitral valve repair. No significant differences in terms of procedures were observed between the two groups.
Considering the whole population, PASP significantly decreased at 5-year follow-up (from 42 ± 9 to 39 ± 9 mmHg, P < 0.001); however, it remained almost unchanged in patients with RMVD (from 41 ± 9 to 42 ± 9 mmHg, P = 0.512), while it significantly decreased in patients with DMVD (from 42 ± 9 to 35 ± 6 mmHg, P < 0.001). The baseline clinical and echocardiographic features of patients who were grouped based on the PASP changes during follow-up were shown in Table 2. Compared with patients showed normal PASP persistently, other three groups patients had higher prevalence of etiology of RMVD, more MV replacement and TV repair procedure, and higher baseline PASP values.
During a mean follow-up of 8 years (4–12 years), a total of 173 deaths were observed, of which 106 were of cardiovascular origin. Overall survival of the total population was 90% (95% CI, 92–98) at 5 years and 78% (95% CI, 75–81) at 10 years. During follow-up, 76 patients had reoperation, 35 had a stroke, and 7 patients had implanted pacemaker. In total population, AF freedom on and off AAD was 69% (95% CI, 66–72) and 61% (95% CI, 57–65) at 5 years; 48% (95% CI, 45–52) and 41% (95% CI, 36–46) at 10 years, respectively (Figure 2).
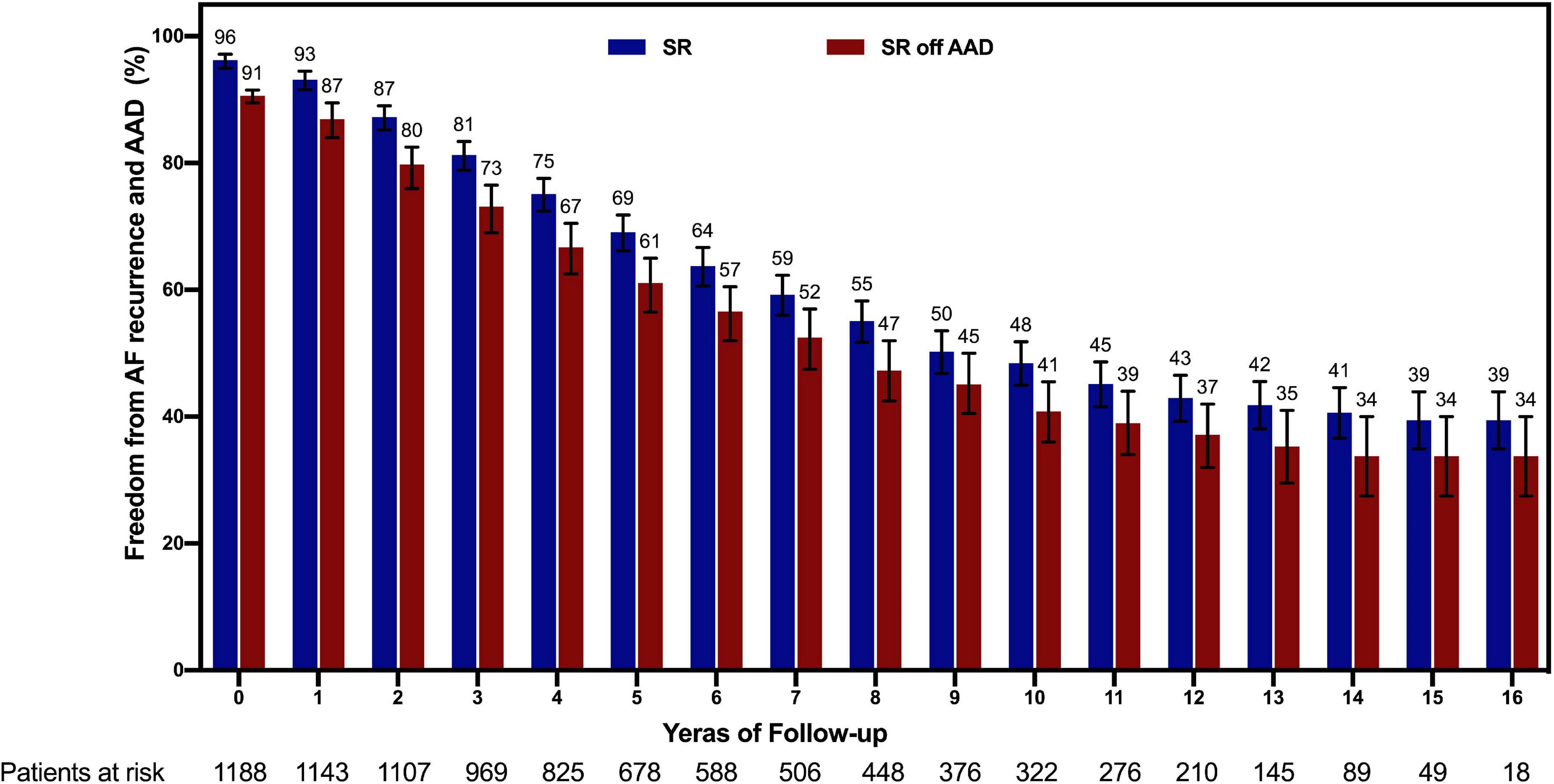
Figure 2. Follow-up showing freedom from recurrence of AF both on and off AADs with 95% confidence intervals. AF, atrial fibrillation; AAD, antiarrhythmic drug; SR, sinus rhythm.
Etiology, MV procedure, and PASP changes at follow-up were significant univariable predictors for both death and AF recurrence. Furthermore, LAD, PASP at baseline, and TV repair were significant univariable predictors of AF recurrence. While etiology and PASP changes at follow-up in death-free and AF recurrence free survival remained significant after multivariable adjustment (Table 3). Details of univariate regression were shown in Supplementary material.
Patients with DMVD had the significantly better death-free survival compared with patients with RMVD (log-rank 37.8, P < 0.0001, Figure 3A). Meanwhile, compared with RMVD, the patients with DMVD also had a lower risk of AF recurrence (SHR: 1.239; CI: 1.082–1.419; P = 0.002, Figure 3B) after considering death as a competing risk. Moreover, when patients were stratified according to the PASP changes at 5-year follow-up, a higher survival rate was observed among patients with persistently normal and decreased PASP (log-rank 166.0, P < 0.0001, Figure 4A). Likewise, the patients with persistently normal PASP had a lowest risk of recurrent AF (SHR: 0.817; CI: 0.765–0.872; P < 0.0001, Figure 4B) in the competing model that death was seen as a competing event.

Figure 3. (A) Kaplan–Meier survival analysis, and (B) cumulative incidence analysis of probability of recurrence of AF according to the MV etiology. CI, confidence interval; DMVD, degenerative mitral valve disease; RMVD, rheumatic mitral valve disease; SHR, sub-hazard ratio.
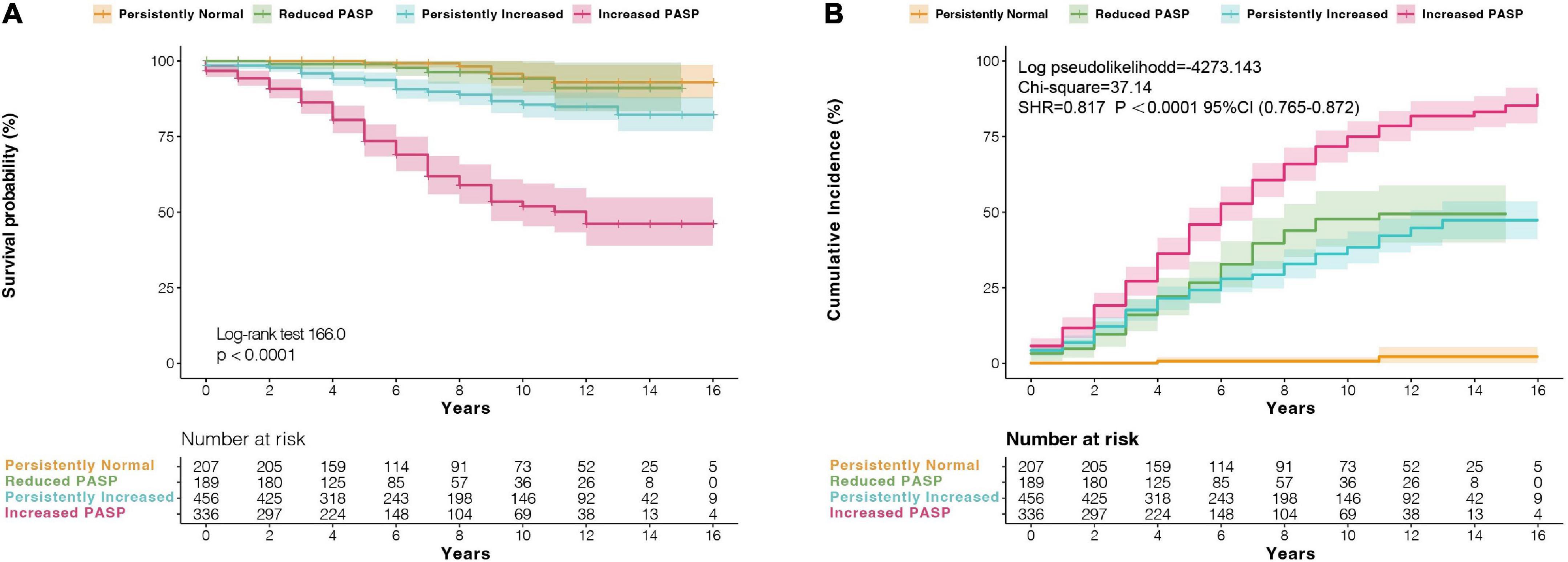
Figure 4. (A) Kaplan–Meier survival analysis, and (B) cumulative incidence analysis of probability of recurrence of AF according to changes of pulmonary artery systolic pressure (PASP) at follow-up. CI, confidence interval; SHR, sub-hazard ratio.
The Time-dependent ROC curve indicated that PASP of 35 mmHg at follow-up discriminated predicting 5-(sensitivity 89%, specificity of 54%, AUC 0.70), and 10-(sensitivity 88%, specificity of 42%, AUC 0.66) year death-free survival patients, respectively (Figure 5A). Similarly, a value of 35 mmHg at follow-up discriminated predicting 5-(sensitivity 71%, specificity of 62%, AUC 0.65), and 10-(sensitivity 76%, specificity of 63%, AUC 0.71) year recurrent AF-free survival patients, respectively (Figure 5B).
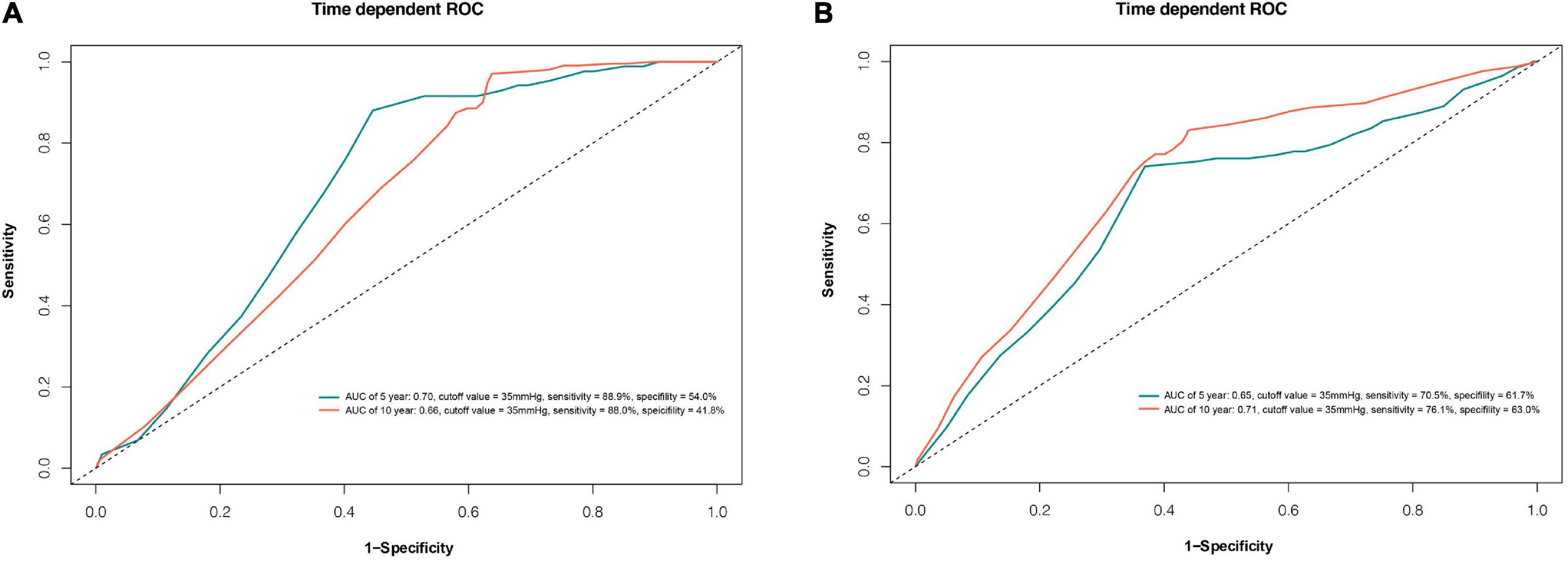
Figure 5. Time-dependent receiver operating characteristic (ROC) curve for pulmonary artery systolic pressure (PASP) at follow-up with optimal cut-off point best predicting death (A) and AF recurrence (B). AUC, area under curve.
Figure 6 demonstrated PASP was significantly higher in patients with RMVD, which was accompanied by a lower SR maintenance rate.
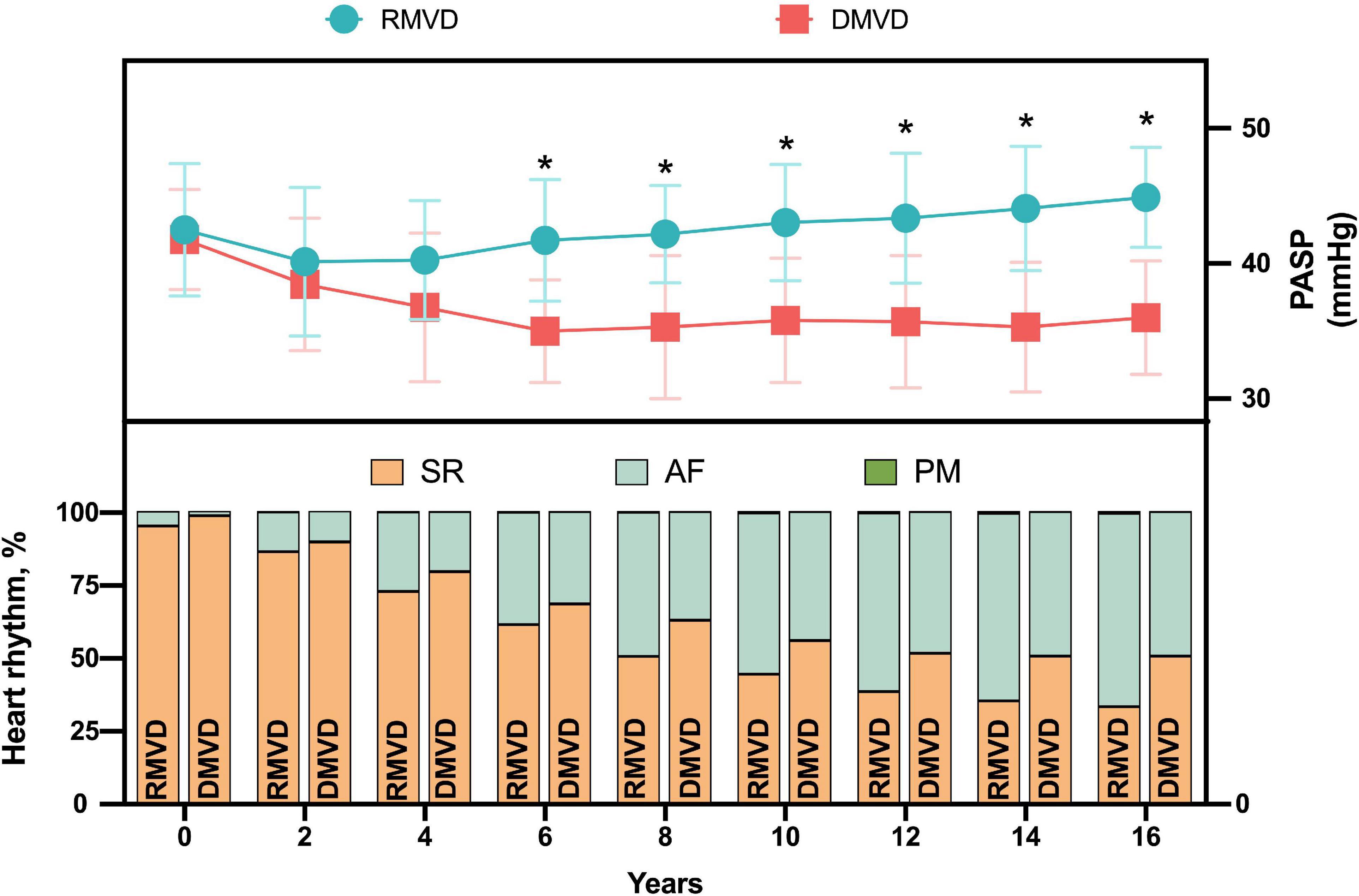
Figure 6. Heart rhythm according to the changes of PASP during follow-up in patients with MV disease. AF, atrial fibrillation; DMVD, degenerative mitral valve disease; PASP, pulmonary artery systolic pressure; PM, pacemaker; RMVD, rheumatic mitral valve disease; SR, sinus rhythm. *P < 0.05 vs. DMVD.
To our knowledge, our study is the first one that demonstrates the association between MV etiology and PASP with improved survival in patients with MV disease with AF. Our results illustrated that the improvement of PH during follow-up may directly affect the clinical outcomes of patients after MV procedure and Cox-Maze procedure. These observations also highlight the important contributions of MV etiology and PH in maintaining clinical compensation.
AF is a common sequela of MV disease that is frequently present in patients referred to MV surgery (12, 13). MV disease may lead to the development of AF via affecting LA volume and pressure overload, causing progressive atrial fibrosis, LA structural remodeling and electrical remodeling (14). The Cox-Maze procedure, using a bipolar radiofrequency device, has been shown to be the most effective surgical treatment of AF (15, 16). However, the outcomes of the Cox-Maze procedure in treating AF associated with different etiology of MV disease remained controversial. Labin et al. reported that compared with patients with DMVD with a longer duration of AF and larger LAD, despite representing a sicker patient population, patients with RMVD may equally benefit from the Cox-Maze procedure up to 5 years of follow-up (6). Nevertheless, our results showed significantly worse event-free survival in patents with RMVD during a 15-years follow-up.
Hemodynamic evaluation of patients with DMVD associated PH reveals that the increase of pulmonary arterial pressure of these patients were positioned in the incipient stage, which were mainly caused by the increase of left atrial pressure (17). In this stage, the resistance of pulmonary vessel showed normal function. Patients may show a high transpulmonary pressure gradient but this status could usually be reversed after successful mitral interventions (18, 19). Although, the pathology mechanism of pulmonary vessel among patients with DMVD could be affected by a lot of factors that are not fully understood yet (20), the fact is that many patients with severe DMVD in the real world have not been observed any elevations of pulmonary artery pressure (21).
However, in patients with RMVD (long-standing course MV disease), PASP had a lower possibility of decreasing PASP though their LAP and PH may maintain normal postoperatively (2, 22), which indicated that the irreversibility of PH caused by pulmonary vascular remodeling may led to worse clinical outcomes. The above persistence of significant PH after surgery in patients with RMVD may be the result of persistent microvascular changes.
As with other retrospective studies, several limitations of this study are as follows. First, PH was defined as mean PAP of more than 20 mm Hg measured with right heart catheterization (RHC). RHC is an invasive procedure with associated risk, which limits the utility for routine evaluation of PH during follow-up. However, echocardiography has been an effective and relatively precise tool to evaluate PASP since the correlation was found between RHC and echocardiography, and 35 mmHg is the most used threshold value to estimate PH via echocardiography (23). Second, the occurrence of missing data is also one of the limitations. Not all patients had rhythm status and echocardiography available for each time point.
Our data indicated that patients with DMVD or have persistently normal PASP during follow-up have better survival and SR maintenance, while patients with RMVD or have an abnormal PASP during follow-up have worse outcome. For patients with rheumatic mitral diseases, more active surgical interventions should be considered if PASP had obvious abnormity.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study has been approved by the Institutional Review Board (20180723) at Beijing Anzhen Hospital, Capital Medical University. The patients/participants provided their written informed consent to participate in this study.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
This study was supported by the National Natural Science Foundation of China (Grant No. 82170311).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.1047715/full#supplementary-material
1. Coutinho GF, Correia PM, Branco C, Antunes MJ. Long-term results of mitral valve surgery for degenerative anterior leaflet or bileaflet prolapse: analysis of negative factors for repair, early and late failures, and survival. Eur J Cardiothorac Surg. (2016) 50:66–74. doi: 10.1093/ejcts/ezv470
2. Yang B, DeBenedictus C, Watt T, Farley S, Salita A, Hornsby W, et al. The impact of concomitant pulmonary hypertension on early and late outcomes following surgery for mitral stenosis. J Thorac Cardiovasc Surg. (2016) 152:394–400. doi: 10.1016/j.jtcvs.2016.02.038
3. Genuardi M, Shpilsky D, Handen A, VanSpeybroeck G, Canterbury A, Lu M, et al. Increased mortality in patients with preoperative and persistent postoperative pulmonary hypertension undergoing mitral valve surgery for mitral regurgitation: a cohort study. J Am Heart Assoc. (2021) 10:e018394. doi: 10.1161/JAHA.120.018394
4. Enter D, Zaki A, Duncan B, Kruse J, Andrei A, Li Z, et al. A contemporary analysis of pulmonary hypertension in patients undergoing mitral valve surgery: is this a risk factor? J Thorac Cardiovasc Surg. (2016) 151:1288–97. doi: 10.1016/j.jtcvs.2015.12.063
5. January C, Wann L, Alpert J, Calkins H, Cigarroa J, Cleveland J, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of cardiology/American heart association task force on practice guidelines and the heart rhythm society. Circulation. (2014) 130:e199–267. doi: 10.1161/CIR.0000000000000041
6. Labin J, Haque N, Sinn L, Schuessler R, Moon M, Maniar H, et al. The Cox-Maze IV procedure for atrial fibrillation is equally efficacious in patients with rheumatic and degenerative mitral valve disease. J Thorac Cardiovasc Surg. (2017) 154:835–44. doi: 10.1016/j.jtcvs.2017.03.152
7. Kim K, Cho K, Kim Y, Sohn D, Kim K. Long-term results of the Cox-Maze III procedure for persistent atrial fibrillation associated with rheumatic mitral valve disease: 10year experience. Eur J Cardiothorac Surg. (2007) 31:261–6. doi: 10.1016/j.ejcts.2006.11.017
8. Wang J, Han J, Li Y, Ye Q, Meng F, Luo T, et al. Impact of surgical ablation of atrial fibrillation on the progression of tricuspid regurgitation and right-sided heart remodeling after mitral-valve surgery: a propensity-score matching analysis. J Am Heart Assoc. (2016) 5:e004213. doi: 10.1161/JAHA.116.004213
9. Zoghbi W, Enriquez-Sarano M, Foster E, Grayburn P, Kraft C, Levine R, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and doppler echocardiography. J Am Soc Echocardiogry. (2003) 16:777–802. doi: 10.1016/S0894-7317(03)00335-3
10. Zlotnick D, Ouellette M, Malenka D, DeSimone J, Leavitt B, Helm R, et al. Effect of preoperative pulmonary hypertension on outcomes in patients with severe aortic stenosis following surgical aortic valve replacement. Am J Cardiol. (2013) 112:1635–40. doi: 10.1016/j.amjcard.2013.07.025
11. Rudski L, Lai W, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American society of echocardiography endorsed by the European association of echocardiography, a registered branch of the European society of cardiology, and the Canadian society of echocardiography. J Am Soc Echocardiogr. (2010) 23:685–788. doi: 10.1016/j.echo.2010.05.010
12. Halas M, Kruse J, McCarthy P. Concomitant treatment of atrial fibrillation during mitral valve surgery. J Cardiovasc Electrophysiol. (2021) 32:2873–8. doi: 10.1111/jce.15019
13. John B, Lau C. Atrial fibrillation in valvular heart disease. Card Electrophysiol Clin. (2021) 13:113–22. doi: 10.1016/j.ccep.2020.11.007
14. De Jong A, Maass A, Oberdorf-Maass S, Van Veldhuisen D, Van Gilst W, Van Gelder I. Mechanisms of atrial structural changes caused by stretch occurring before and during early atrial fibrillation. Cardiovasc Res. (2011) 89:754–65. doi: 10.1093/cvr/cvq357
15. Damiano R, Schwartz F, Bailey M, Maniar H, Munfakh N, Moon M, et al. The Cox maze IV procedure: predictors of late recurrence. J Thorac Cardiovasc Surg. (2011) 141:113–21. doi: 10.1016/j.jtcvs.2010.08.067
16. Ruaengsri C, Schill M, Khiabani A, Schuessler R, Melby S, Damiano R. The Cox-maze IV procedure in its second decade: still the gold standard? Eur J Cardiothorac Surg. (2018) 53:i19–25. doi: 10.1093/ejcts/ezx326
17. Patel H, Desai M, Tuzcu E, Griffin B, Kapadia S. Pulmonary hypertension in mitral regurgitation. J Am Heart Assoc. (2014) 3:e000748. doi: 10.1161/JAHA.113.000748
18. Kulik T. Pulmonary hypertension caused by pulmonary venous hypertension. Pulm Circ. (2014) 4:581–95. doi: 10.1086/678471
19. Guazzi M, Borlaug B. Pulmonary hypertension due to left heart disease. Circulation. (2012) 126:975–90. doi: 10.1161/CIRCULATIONAHA.111.085761
20. Austin E, Loyd J. The genetics of pulmonary arterial hypertension. Circ Res. (2014) 115:189–202. doi: 10.1161/CIRCRESAHA.115.303404
21. Maeder M, Weber L, Buser M, Gerhard M, Haager P, Maisano F, et al. Pulmonary hypertension in aortic and mitral valve disease. Front Cardiovasc Med. (2018) 5:40. doi: 10.3389/fcvm.2018.00040
22. Borde D, Asegaonkar B, Khade S, Puranik M, George A, Joshi S. Impact of preoperative pulmonary arterial hypertension on early and late outcomes in patients undergoing valve surgery for rheumatic heart disease. Indian J Anaesth. (2018) 62:963–71. doi: 10.4103/ija.IJA_374_18
Keywords: mitral valve, atrial fibrillation, pulmonary hypertension, Cox-Maze procedure, pulmonary artery systolic pressure
Citation: Zheng T, Zhao Y, Ye Q, Zheng S, Meng F, Hu Q, Zhang H, Han J, Tian B, Zhu J and Wang J (2023) Impact of pulmonary arterial systolic pressure on patients with mitral valve disease combined with atrial fibrillation. Front. Cardiovasc. Med. 9:1047715. doi: 10.3389/fcvm.2022.1047715
Received: 18 September 2022; Accepted: 14 December 2022;
Published: 09 January 2023.
Edited by:
Jane Grande-Allen, Rice University, United StatesReviewed by:
Peng Zhu, Southern Medical University, ChinaCopyright © 2023 Zheng, Zhao, Ye, Zheng, Meng, Hu, Zhang, Han, Tian, Zhu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiangang Wang,  jiangangwang@ccmu.edu.cn; Junming Zhu,
jiangangwang@ccmu.edu.cn; Junming Zhu,  anzhenzjm@163.com
anzhenzjm@163.com
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.