EDITORIAL
Published on 05 May 2022
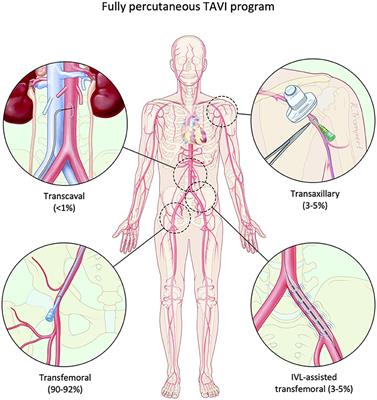
Editorial: Transcatheter Aortic Valve Implantation: All Transfemoral? Update on Vascular Acccess and Closure
doi 10.3389/fcvm.2022.907445
- 1,637 views
- 1 citation
6,704
Total downloads
26k
Total views and downloads
EDITORIAL
Published on 05 May 2022
MINI REVIEW
Published on 04 Mar 2022
ORIGINAL RESEARCH
Published on 21 Jan 2022

ORIGINAL RESEARCH
Published on 15 Nov 2021

CASE REPORT
Published on 20 Oct 2021
REVIEW
Published on 29 Sep 2021
ORIGINAL RESEARCH
Published on 22 Sep 2021
ORIGINAL RESEARCH
Published on 22 Sep 2021
ORIGINAL RESEARCH
Published on 21 Jul 2021