EDITORIAL
Published on 15 Nov 2021
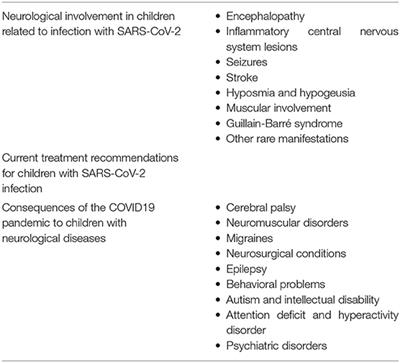
Editorial: Consequences of the COVID-19 Pandemic on Care for Neurological Conditions
doi 10.3389/fneur.2021.788912
- 1,461 views
- 2 citations
114k
Total downloads
526k
Total views and downloads
EDITORIAL
Published on 15 Nov 2021
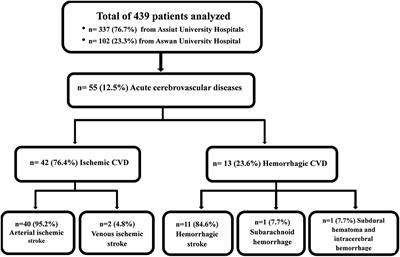
BRIEF RESEARCH REPORT
Published on 03 Sep 2021
ORIGINAL RESEARCH
Published on 09 Apr 2021
CASE REPORT
Published on 08 Apr 2021
MINI REVIEW
Published on 24 Mar 2021
ORIGINAL RESEARCH
Published on 22 Mar 2021
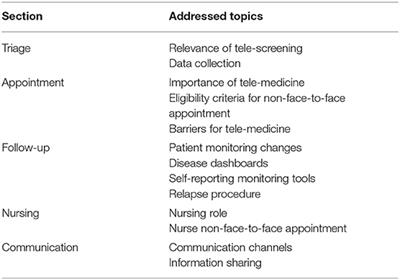
PERSPECTIVE
Published on 08 Mar 2021
BRIEF RESEARCH REPORT
Published on 26 Feb 2021

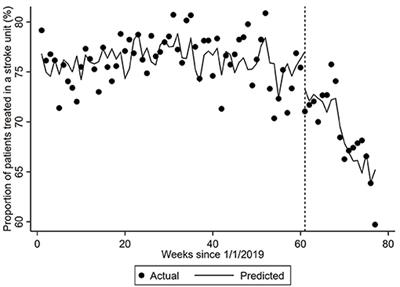
BRIEF RESEARCH REPORT
Published on 26 Feb 2021
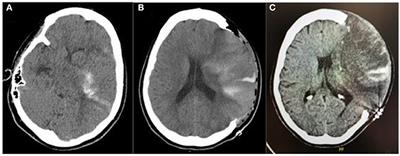
CASE REPORT
Published on 22 Feb 2021
REVIEW
Published on 18 Feb 2021
ORIGINAL RESEARCH
Published on 11 Feb 2021

