- Science news
- Life sciences
- New path into bipolar disorder comes to light
New path into bipolar disorder comes to light

New research reveals a novel potential drug target for bipolar disorder and offers new insights into the underlying biology of this lifelong and devastating mental illness.
-By Publicase Comunicaçao Científica
Bipolar disorder (BD) is a multifactorial brain disorder in which patients experience radical shifts in mood and undergo periods of depression followed by periods of mania. It has been known for some time that both environmental and genetic factors play important roles in the disease. For instance, exposure to high levels of stress for long periods, especially during childhood, is one factor associated with development of BD.
New research published in Frontiers in Behavioral Neuroscience connects the dots between two genes involved in the brain’s response to environmental stimuli — called EGR3 and BDNF — and may explain the impaired resilience of BD patients to respond to events, including stress. The study not only provides new insights into the biology of BD, but also suggests that EGR3 could be a potential drug target.
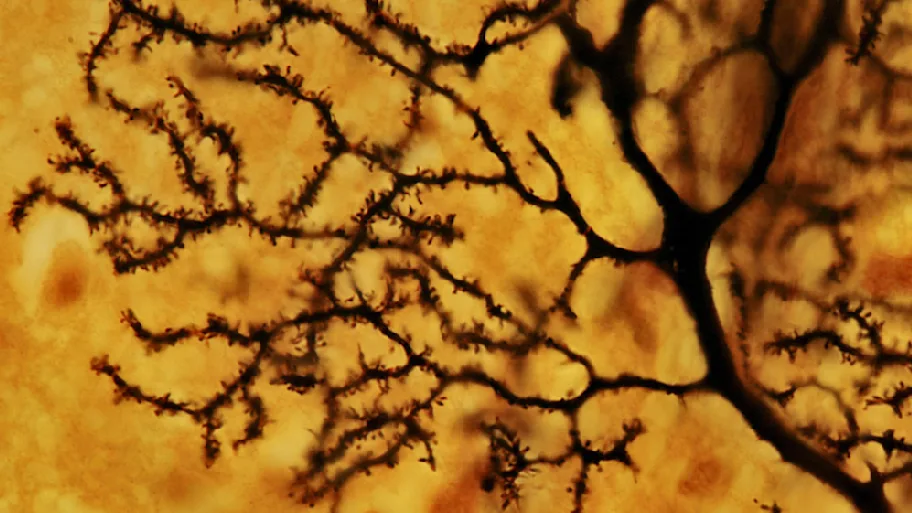
Immediate early genes (IEGs) are a class of genes that respond very rapidly to environmental stimuli, including stress. IEGs respond to a stressor by activating other genes that lead to neuronal plasticity — that is, a change in form and function o brain cells in response to changes in the environment. Ultimately, the process of neuronal plasticity gives the brain the ability to learn from and adapt to new experiences.
One type of protein induced by IEGs is the so-called Early Growth Response (EGR) proteins, which translate environmental influence into long-term changes in the brain. These proteins are found throughout the brain and are highly produced in response to environmental changes such as stressful stimuli and sleep deprivation. Without the action played out by these proteins, brain cells and the brain itself cannot appropriately respond to the many stimuli that are constantly received from the environment.
Effective neuronal plasticity also depends on regulatory factors called neurotrophins that promote development and survival of brain cells. Brain-derived neurotrophic factor (BDNF), the neurotrophin mostly found in the brain, has been extensively investigated in BD patients and has been suggested as a hallmark of BD. Indeed, some studies have shown that serum levels of BDNF are reduced in BD patients during periods of depression, hypomania, or mania. Other studies have shown that regardless of mood state, BD patients present reduced levels of BDNF. Overall, changes in BDNF levels seem to be a characteristic found in BD patients that may contribute to the pathophysiology of the disease.
The new study by an international team of researchers from Universidade Federal do Rio Grande do Sul in Brazil, University of Arizona College of Medicine in the United States and McMaster University in Canada connects the dots between these two players to explain the impaired cellular resilience observed in BD that in the grand scheme of things may relate to the impaired resilience presented by BD patients to respond to events, including stress.
In a previous study by the group in 2016, one type of IEG gene known as EGR3, that normally responds to environmental events and stressful stimuli, was found to be repressed in the brain of BD patients. This suggests that when facing a stressor, the EGR3 in BD patients does not respond to the stimulus appropriately. Indeed, BD patients are highly prone to stress and have more difficulties dealing with stress or adapting to it if compared to healthy individuals. The research group is now suggesting that both EGR3 and BDNF may each play a critical role in the impaired cellular resilience seen in BD, and that each of these two genes may affect each other’s expression in the cell.
“We believe that the reduced level of BDNF that has been extensively observed in BD patients is caused by the fact that EGR3 is repressed in the brain of BD patients. The two molecules are interconnected in a regulatory pathway that is disrupted in BD patients,” says Fabio Klamt, leading author of the article.
The authors also add that the fact that EGR3 responds very quickly to environmental stimuli renders the molecule a potential drug target. “It is possible to imagine that EGR3 may be modulated in order to increase its expression and that of BDNF, which may have a positive impact on BD patients,” says Bianca Pfaffenseller, a scientist working at Hospital de Clínicas de Porto Alegre, in Brazil, and the first author of the study.
The idea that mental disorders should be seen as any other chronic disease in which the underlying biology plays an important role has replaced the old descriptions of mental illnesses as the result of bad psychological influences. As Nobel prize laureate Eric Kandel has said, “all mental processes are brain processes and therefore all disorders of mental functioning are biological diseases.” The perspective article authored by Fabio Klamt and colleagues supports this view by offering new insights into the underlying biology of this lifelong and devastating mental disorder affecting millions of people worldwide.
Original article: EGR3 Immediate Early Gene and the Brain-Derived Neurotrophic Factor in Bipolar Disorder
Corresponding author: Dr. Bianca Pfaffenseller
REPUBLISHING GUIDELINES: Open access and sharing research is part of Frontier’s mission. Unless otherwise noted, you can republish articles posted in the Frontiers news blog — as long as you include a link back to the original research. Selling the articles is not allowed.






