
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Vet. Sci., 11 March 2025
Sec. Veterinary Emergency and Critical Care Medicine
Volume 12 - 2025 | https://doi.org/10.3389/fvets.2025.1558937
This article is part of the Research TopicEmerging Challenges in Companion Animal ToxicologyView all 8 articles
Paper wasp (Polistes rothneyi) envenomation is an emerging public threat in Asian countries, but its clinical manifestations are limited in veterinary medicine. A 2-year-old male Yorkshire Terrier was evaluated for symptoms including vomiting, melena, and anuria, and upon presentation, exhibited lethargy and signs of jaundice. The dog had a history of being stung multiple times by paper wasps (Polistes rothneyi) 3 days prior to admission. On blood examination, anemia, severe azotemia, hyperbilirubinemia, and significant elevation of creatine kinase were noted. Treatment was initiated with epinephrine, glucocorticoids, antihistamines, and fluid therapy. Despite these interventions, the condition worsened, necessitating the initiation of continuous renal replacement therapy. However, the dog subsequently developed bradycardia and hypotension, leading to cardiac arrest 48 h after presentation. This is the first case report describing the clinical manifestation of dogs envenomated by paper wasps (Polistes rothneyi). Massive paper wasp envenomation can cause multiple organ lesions, including renal, hepatic, and gastrointestinal damage.
The stings from members of the Hymenoptera order, including those from the Apoidea (bees), Vespoidea (wasps), and Formicidae (ants) families, present considerable potential health threats to dogs (1). This venom contains complex mixtures of allergenic proteins, active antigens, and peptides, which can lead to envenomation and potentially cause anaphylaxis (1). Hymenoptera stings are generally well tolerated and typically cause limited local reactions. However, in cases of massive envenomation, systemic reactions can occur, affecting multiple organs such as the kidneys, liver, nervous system, and lungs (2). Recently, wasps have successfully adapted to urban areas in many countries, leading to a significant increase in reported wasp stings, and they are now managed as a hazardous animal group (3). However, most reports on Hymenoptera stings in veterinary medicine focus on bee stings, with very limited documentation on wasp stings. The purpose of this report is to describe the clinical manifestations of a dog after massive paper wasp (Polistes rothneyi) envenomation.
A 2-year-old male Yorkshire Terrier weighing 4.88 kg referred to the emergency service for lethargy, vomiting, melena and anuria. The dog had a history of massive Hymenoptera envenomation, with over 100 stings, as reported by the owner, who directly witnessed the attack while the dog was urinating in the shrubs containing a nest 3 days before admission. The owner, who was also attacked by the Hymenoptera, called the emergency response center requesting nest removal. The nest was subsequently removed, and a taxonomist confirmed the Hymenoptera to be paper wasps (Polistes rothneyi) (Figure 1). The dog was reported to have had no prior health problems or medications before the envenomation and was fully vaccinated. The dog exhibited lethargy immediately after envenomation, followed by the onset of gastrointestinal signs, including vomiting and diarrhea, starting the next day. The condition progressively deteriorated, leading the owners to bring it to our hospital for further evaluation and treatment.
A general physical examination revealed facial swelling and jaundice, characterized by yellow discoloration throughout the body, including the ears, sclera, penis, and caudoventral abdomen (Figure 2). The patient was alert, auscultation was unremarkable, and the patient was normothermic with a temperature of 38.5°C. Other vital parameters were within normal limits, including a heart rate of 144 beats per minute, a respiratory rate of 36 breaths per minute, and a systolic blood pressure of 140 mmHg, measured using a Doppler ultrasonic flow detector. The mucous membranes were sticky, and skin turgor was mildly delayed, consistent with 5% dehydration. On blood examination, significant leukocytosis and elevated C-reactive protein (CRP) (169 mg/L; RI, 0–9 mg/L) were noted. Additionally, elevations in creatine kinase, bilirubin, alkaline phosphatase (ALKP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), and azotemia were observed. Serum symmetric dimethylarginine (SDMA) (57 μg/dL; RI, 0–14 μg/dL) was also increased. The complete blood count, serum biochemical, and venous blood gas results are summarized in Table 1. On coagulation examination, prothrombin time and activated partial thromboplastin time were both within the RI. However, the concentration of D-dimer was significantly elevated (4,360 ng/mL; reference interval, <250 ng/mL). Complete urinalysis obtained by cystocentesis revealed brown and turbid urine appearance with a specific gravity of 1.010, pH 7, 3+ protein, 3+ blood, and 2+ leukocyte. Hematuria was observed in the microscopic examination of the urine sediment, with no crystals or casts present. Thoracic and abdominal radiography revealed no remarkable findings. Abdominal ultrasonography was performed and revealed increased cortical echogenicity in both kidneys, hypoechoic echogenicity of the liver, hyperechoic pancreas with peripancreatic hyperechoic fat, gastric wall thickening, and decreased gastrointestinal motility. Severe multi-organ dysfunction, characterized by acute kidney injury [International Renal Interest Society acute kidney injury (AKI) grade 5], liver failure, and gastrointestinal failure, was suspected to result from direct toxins from massive paper wasp envenomation (4).

Figure 2. Yellow discoloration (jaundice) observed in the sclera, ears, and caudoventral abdomen of the paper wasp envenomated dog.
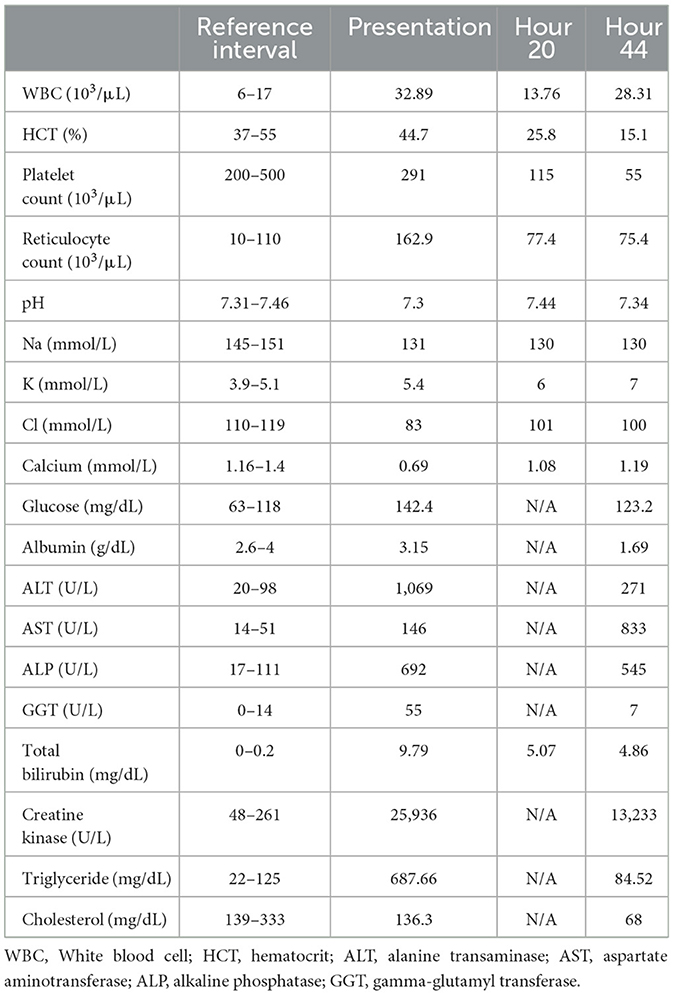
Table 1. Serial complete blood count, venous blood, and serum chemistry results from a dog with massive Paper wasp envenomation.
Initial therapeutics consisted of 10 ml/kg Ringer's lactate IV based on 70 mL/kg/day maintenance in addition to 5% dehydration aimed to be replaced over 8 h. Additionally, low dose epinephrine 0.01 mg/kg IV, dexamethasone 0.2 mg/kg IV, chlorpheniramine 0.2 mg/kg SC, maropitant 1 mg/kg SC, esomeprazole 1 mg/kg IV, ampicillin/sulbactam 12.5 mg/kg IV was added to the therapeutic plan. The dog was monitored in the intensive care unit after the placement of a urinary catheter. However, the dog remained anuric, with no urine output observed even after 8 h.
On day 1 of hospitalization, 8 h post-presentation, continuous venovenous hemodialysis was initiated using an automated renal replacement therapy and continuous fluid management unit. As the dog's condition continued deteriorate, diuretic therapy with furosemide or mannitol was not considered, and hemodialysis was prioritized for immediate management. Before use, an 8-Fr, 16-cm double lumen catheter was percutaneously placed in the right external jugular vein. The blood access lines and hemofilter were primed with heparinized saline. Unfractionated heparin was administered continuously as an anticoagulant dose ranging from 15 to 30 U/kg/h throughout the continuous renal replacement treatment (CRRT) procedure. A dialysate flow rate of 0–600 ml/h (0–123 ml/kg/h) and replacement rates of 50–100ml/h (10.2–20.5 ml/kg/h) and ultrafiltration rate of 20–50 ml/h (4.1–10.2 ml/kg/h) were utilized. There was no blood transfusion during the CRRT. A filtration fraction of 16.6%, measured Kt/V of 0.42, and calculated urea reduction ratio of 48.5% (5). Following the CRRT, BUN levels decreased from 181.7 mg/dL at admission to 93.5 mg/dL. Similarly, creatinine levels were reduced from 10.87 mg/dL to 4.04 mg/dL (Table 2).
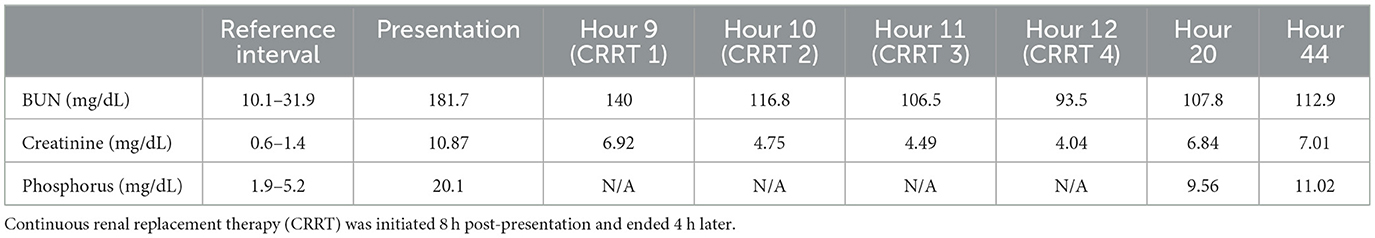
Table 2. Results of serial renal biochemical panels taken at various time points following the massive paper wasp envenomation.
By day 2 of hospitalization (20 h post-presentation), the dog remained persistently anuric, and its mental status deteriorated to a depressed state. The body weight increased from 4.88 kg to 5.5 kg, with the signs of overhydration including peripheral edema and increased skin turgor. The dog continued to show anorexia and dull mentation. The blood examination revealed that hyperbilirubinemia improved. However, azotemia progressed, with BUN at 107.8 mg/dL, creatinine at 6.84 mg/dL, and phosphorus at 9.56 mg/dL, compared to post-CRRT values. Venous blood gas analysis showed progressive hyperkalemia at 6 mmol/L. A second session of CRRT and blood transfusion were declined by the owner. On the second day, intravenous fluids were tapered and discontinued at 30 h post-presentation. Furosemide 2 mg/kg IV and Mannitol 1 g/kg IV were administered, but the patient remained anuric.
On day 3 of hospitalization, a venous blood gas revealed progressive hyperkalemia at 7 mmol/L. The chemistry panel showed a significant reduction in creatine kinase but progressive azotemia with BUN at 112.9 mg/dL, creatinine at 7.01 mg/dL, and phosphorus at 11.02 mg/dL. Administration of 1 ml/kg of 50% dextrose and 0.1 U/kg of regular insulin was initiated for the treatment of hyperkalemia. The patient progressively deteriorated, becoming stuporous, and showed bradycardia and hypotension at 48 h post-presentation, and cardiac arrest was observed. A post-mortem examination was declined by the owner.
This is the first case report describing the clinical characteristics of a dog envenomated by paper wasp (Polistes rothneyi). It confirms the occurrence of multi-organ lesions, including renal, hepatic, and gastrointestinal dysfunction, following massive paper wasp (Polistes rothneyi) envenomation. There are several reports of Hymenoptera stings in veterinary medicine, most of which involve bee stings, with other reports documenting stings by yellow jackets (Vespula spp) (6–10). Envenomation from paper wasps typically requires concern primarily for allergic reactions and cutaneous pain and inflammation which could result in fewer hospital visits in humans (11). Additionally, allergic reactions and fatalities are less common compared to yellowjacket stings, which may contribute to the limited information available on paper wasp envenomation (11).
The response to a Hymenoptera sting is classified into four categories: (1) local reactions, (2) uncomplicated allergic reactions, (3) anaphylactic reactions, and (4) direct systemic toxic reactions (12). During a sting, the wasp injects a proteinaceous liquid stored in its venom glands. The venom of Vespid wasps contains a variety of chemical constituents, including phospholipase A, antigen 5, hyaluronidase, acid phosphatase, biogenic amines, mast cell degranulating peptides, and kinins (1). These components can have myotoxic, hemolytic, neurotoxic, hepatotoxic, nephrotoxic, and vasodilatory effects (13).
A single wasp sting can cause an immunoglobulin E-mediated anaphylactic reaction, while mass envenomation from multiple stings can lead to systemic toxin-mediated cellular damage (14). In one study, acute kidney injury, rhabdomyolysis, hemolysis, liver injury, and coagulopathy were identified as the most frequent non-allergic manifestations of wasp stings (15). Additionally, high creatinine levels, presence of oliguria, anemia, and shock were recognized as risk factors for death (15). In this case, the dog was suspected to have direct systemic toxic reactions; however, the possibility of anaphylaxis could not be entirely ruled out, characterized by end-organ dysfunction and persistent gastrointestinal symptoms, including vomiting, melena, and facial swelling. Toxic reactions after Hymenoptera stings are uncommonly reported since most stinging events involve only one to a few stings, resulting in a small amount of toxin being injected into the body (2). However, in this study, the dog disturbed a shrub containing a paper wasp nest, leading to massive envenomation.
A severe acute kidney injury was observed in the dog at presentation, 3 days after massive envenomation. The pathophysiology of AKI following wasp envenomation is varied and includes secondary myoglobin release due to rhabdomyolysis, myoglobin-induced renal toxicity, intravascular hemolysis, direct nephrotoxicity from the wasp venom, allergic reactions, and inflammatory responses (16). The incidence of AKI following wasp envenomation is reported to be approximately 10 to 58% (17). In such patients, urinalysis often reveals various amounts of red and white blood cells with or without casts; the dog in our study showed similar results. Additionally, among those presenting with AKI, about 83% required dialysis (18). The dog in this study initially exhibited lethargy without significant symptoms after envenomation but later developed vomiting and diarrhea, which progressively worsened over time, eventually leading to an anuric state and hospitalization. It is crucial to recognize that even mild initial signs, such as lethargy, can progress to AKI. Additionally, the delay in presentation to the hospital may have contributed to the development of AKI and worsened the overall prognosis, highlighting the importance of timely medical intervention in similar cases.
Treatment for massive paper wasp envenomation was mainly supportive as there is no antivenom available for wasp stings (14). The patient underwent fluid resuscitation and received supportive treatment for toxin-related complications. A gastro-protectant, specifically a proton pump inhibitor, was administered, and neurokinin-1 receptor antagonist was prescribed to manage vomiting. Additionally, as anaphylaxis could not be ruled out, epinephrine was administered as the first-line drug, and antihistamines were given as adjunctive treatment (19). Continuous renal replacement therapy was initiated for the AKI, but the multi-organ dysfunction resulted in the patient remaining anuric and eventually cardiac arrest. Given that massive paper wasp envenomation can lead to systemic toxic reactions, including acute kidney failure, liver failure, and gastrointestinal failure, careful monitoring and fluid therapy could be considered as part of initial management. Although no established treatment guidelines exist for canine massive Hymenoptera envenomation, supportive care should be tailored to the patient's condition, and the potential benefits of additional treatments, such as anti-inflammatory or immunomodulatory therapies, warrant further investigation.
In humans, most victims of Hymenoptera stings sustain minor injuries and are treated as outpatients. In addition, if injuries are more serious, involving multiple stings by social wasps, patients tend to remain at medical facilities for ~4 days (3). In this case the dog experienced multiple stings but did not receive aggressive treatment initially. Despite later receiving intensive medication and dialysis, the patient eventually died.
In conclusion, this is the first report describing clinical manifestation of massive paper wasp envenomation in veterinary medicine. Multiple organ dysfunction is a possible consequence of massive paper wasp envenomation. Given the potential risk of paper wasp envenomation in urban parks, increased environmental awareness is advised for dog owners. Both owners and clinicians should be cautious of wasp nests and take preventive measures. Timely and appropriate treatment should be considered from the outset to improve outcomes.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethical approval was not required for the studies involving animals in accordance with the local legislation and institutional requirements because this manuscript describes cases of three client-owned animals in a retrospective nature. The owners consented to the care provided at the time of hospitalization. Written informed consent was obtained from the owners for the participation of their animals in this study. Written informed consent was obtained from the participants for the publication of this case report.
J-ML: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. S-KL: Data curation, Methodology, Writing – review & editing. S-TL: Data curation, Formal analysis, Resources, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to thank Jeong-Kyu Kim, PhD, a taxonomist, for their expertise.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Fitzgerald KT, Flood AA. Hymenoptera stings. Clin Tech Small Anim Pract. (2006) 21:194–204. doi: 10.1053/j.ctsap.2006.10.002
2. Castagnoli R, Giovannini M, Mori F, Barni S, Pecoraro L, Arasi S, et al. Unusual reactions to hymenoptera stings: current knowledge and unmet needs in the pediatric population. Front Med. (2021) 8:717290. doi: 10.3389/fmed.2021.717290
3. Choi MB, Kim TG, Kwon O. Recent trends in wasp nest removal and hymenoptera stings in South Korea. J Med Entomol. (2019) 56:254–60. doi: 10.1093/jme/tjy144
4. Cowgill L. Grading of Acute Kidney Injury. (2016). Available at: https://iris-kidney.com/guidelines/grading.html (accessed December 24, 2024).
5. Acierno MJ. Continuous renal replacement therapy in dogs and cats. Vet Clini North Am - Small Anim Pract. (2011) 41:135–46. doi: 10.1016/j.cvsm.2010.09.001
6. Nair R, Riddle EA, Thrall MA. Hemolytic anemia, spherocytosis, and thrombocytopenia associated with honey bee envenomation in a dog. Vet Clin Pathol. (2019) 48:620–3. doi: 10.1111/vcp.12747
7. Thomas E, Mandell DC, Waddell LS. Survival after anaphylaxis induced by a bumblebee sting in a dog. J Am Anim Hosp Assoc. (2013) 49:210–5. doi: 10.5326/JAAHA-MS-5833
8. Cowell AK, Cowell RL, Tyler RD, Nieves MA. Severe systemic reactions to Hymenoptera stings in three dogs. J Am Vet Med Assoc. (1991) 198:1014–6.
9. Oliveira EC, Pedroso PMO, Meirelles AEWB, Pescador CA, Gouvêa AS, Driemeier D. Pathological findings in dogs after multiple Africanized bee stings. Toxicon. (2007) 49:1214–8. doi: 10.1016/j.toxicon.2007.01.020
10. Caldwell DJ, Petras KE, Mattison BL, Wells RJ, Heffelman VL. Spontaneous hemoperitoneum and anaphylactic shock associated with Hymenoptera envenomation in a dog. J Vet Emerg Criti Care. (2018) 28:476–82. doi: 10.1111/vec.12751
11. Schmidt JO. Clinical consequences of toxic envenomations by Hymenoptera. Toxicon. (2018) 150:96–104. doi: 10.1016/j.toxicon.2018.05.013
12. Lee JH, Kim MJ, Park YS, Kim E, Chung HS, Chung SP. Severe systemic reactions following bee sting injuries in Korea. Yonsei Med J. (2023) 64:404–12. doi: 10.3349/ymj.2022.0532
13. Dewi PSL, Suardamana IK, A. Case report of anaphylactic shock due to hornet sting with multiple organ dysfunction complications. Open Access Maced J Med Sci. (2022) 10:252–6. doi: 10.3889/oamjms.2022.10487
14. Kaisbain N, Rajappan M, Lim WJ, Chang CY. Acute liver injury, rhabdomyolysis, and acute kidney injury following mass envenomation by wasps in Malaysia. Cureus. (2022). 14:e24369. doi: 10.7759/cureus.24369
15. Xie C, Xu S, Ding F, Xie M, Lv J, Yao J, et al. Clinical features of severe wasp sting patients with dominantly toxic reaction: analysis of 1091 cases. PLoS ONE. (2013) 8:e0083164. doi: 10.1371/journal.pone.0083164
16. Yu F, Wang L, Yuan H, Gao Z, He L, Hu F. Wasp venom-induced acute kidney injury: current progress and prospects. Ren Fail. (2023) 45:2259230. doi: 10.1080/0886022X.2023.2259230
17. Ruwanpathirana P, Priyankara D. Clinical manifestations of wasp stings: a case report and a review of literature. Trop Med Health. (2022) 50:8. doi: 10.1186/s41182-022-00475-8
18. Vikrant S, Pandey D, Machhan P, Gupta D, Kaushal SS, Grover N. Wasp envenomation-induced acute renal failure: a report of three cases. Nephrology. (2005) 10:548–52. doi: 10.1111/j.1440-1797.2005.00482.x
Keywords: acute kidney injury, canine, continuous renal replacement therapy, paper wasp, Polistes rothneyi
Citation: Lee J-M, Lee S-K and Lee S-T (2025) Case Report: Multi organ dysfunction in a dog following massive paper wasp (Polistes rothneyi) envenomation. Front. Vet. Sci. 12:1558937. doi: 10.3389/fvets.2025.1558937
Received: 11 January 2025; Accepted: 14 February 2025;
Published: 11 March 2025.
Edited by:
Kristin Opdal Seljetun, Norwegian Institute of Public Health (NIPH), NorwayReviewed by:
Adriano Carrasco, State University of Midwest Paraná, BrazilCopyright © 2025 Lee, Lee and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sun-Tae Lee, YmJpcmlyaTlAbmF2ZXIuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.