- 1Department of Maternal-Infant and Urological Sciences, “Sapienza” University of Rome, Policlinico Umberto I Hospital, Rome, Italy
- 2Department of Urology, “Villa Tiberia Hospital”, Rome, Italy
- 3Department of Urology, “S. Eugenio Hospital”, Rome, Italy
- 4Department of Urology, Viterbo Hospital, Viterbo, Italy
Objectives: To evaluate the effectiveness and safety of the Allium™ ureteral stent as a curative treatment of benign ureteral strictures.
Materials and methods: We retrospectively reviewed the electronic database of the two centers of patients who underwent ureteral Allium™ positioning for different types of stenosis (benign or malignant). Between April 2017 and May 2021, 151 patients were treated with the Allium™ stent for ureteral strictures including benign and malignant stenosis. In total, 83 of them met the inclusion criteria for benign ureteral stricture and were included in final analysis.
Results: About the etiology of strictures, 79 (95.18%) were secondary to ureteroscopy or impacted stones and 4 (4.82%) were secondary to pelvic surgery. The median operating time was 47.9 ± 15.53 min, and the median length of strictures was 2.51 ± 0.84 (1-4) cm. The median time of follow-up was 18 months (range 1–48 months), the overall success rate was 85.5% (71/83), and no intraoperative or perioperative major complications were recorded. Among patients with failure (12 pts, 14.5%): 10 (83.33%) presented ureteral strictures again; among them, 8/10 were patients with a stricture length between 2 and 4 cm, 2 (16.67%) patients with pyelus–ureteral junction stenosis experienced the migration of the stent. All patients who experienced failure were treated surgically either with a robotic or laparoscopic approach.
Conclusions: In our preliminary experience, the Allium™ stent seems to be an effective and safe surgical treatment for benign ureteral stricture. Further analysis and prospective trials are necessary to better define the role of the Allium™ stent in the treatment of benign ureteral strictures.
Introduction
Ureteral strictures are caused by the narrowing of the ureteral lumen. Apart from counting congenital strictures, which are involved in the majority of cases of ureteral pelvic junction, benign pathology including the sequelae of impacted stone and iatrogenic trauma represent the most common causes (80%) of benign ureteral strictures (1). Among these type of strictures, pelvic surgery accounts for 82% of all iatrogenic ureteral injuries, from which 73% are of gynecologic origin (2), while colorectal surgery accounts for more than 9%, and urological procedures for another 14% (3). Regardless of the etiology, the management of ureteral strictures remains a challenge for urologists (4). Among the endoscopic treatments available, balloon dilation often represents the first therapeutic approach (5); however, its effectiveness depends mainly on the length and location of the stenosis with a short-term success rate (3 months) of 60% ± 10% and a long-term success rate (6–12 months) of 54% ± 14% (6). Metallic ureteral stents represent an emerging mini-invasive therapeutical approach, and, in this group, the most commonly utilized devices are Uventa™, Memokath™, and the Allium™ stent (7). This group of dispositives come with the intent of going beyond the limits of double-J stents as the high percentages of encrustation, dislocation, periodic substitutions, and infectious complications. Actually, there is still lacking knowledge about long-term results and the effectiveness of this type of stents and many of these were born with the rationale of a permanent stent with fewer side effects than a double-j stent rather than a surgical technique with curative intent (7). Preliminary experiences with the Allium stent™ have shown promising results in the treatment of benign stenosis; however, many of these have limited and often mixed populations including patients with different types of stenosis, making it difficult to interpret the results (8–10). Based on these considerations, the aim of our study was to evaluate the effectiveness and safety of the Allium™ stent as a curative treatment of benign ureteral strictures since this device may represent a definitive therapeutical solution to ureteral stenosis because of its unique design and application (9)
Material and methods
We retrospectively reviewed the electronic database of patients referred to two clinical centers who underwent ureteral Allium™ positioning for different types of stenosis (benign or malignant) between April 2017 and May 2021. A total of 151 patients were treated with Allium™ stents for ureteral strictures including benign and malignant stenosis during this period, but only 83 of them met the inclusion criterion for benign ureteral stricture and were included in final analysis. The patients’ characteristics including the age, gender, etiology of stenosis, and length and site of the stenosis were recorded. The details of surgery including the surgical time and early and late complications were also recorded. The effectiveness of the procedure was defined as the disappearance of clinical symptoms such as backache and nausea and improved hydronephrosis by imaging during follow-up. Safety was evaluated by the postoperative presence of moderate or severe lower urinary tract symptoms, recurrent urinary infection, pain, stent displacement, encrustation and reobstruction. During follow-up, an abdominal X-ray was performed on the first day after surgery to determine whether the position of the ureteric stent was normal. Subsequently, all patients were evaluated 1 month after surgery with X-ray and ultrasound to assess the stent position and hydronephrosis status and then every 3 months with ultrasound for hydronephrosis evaluation.
We considered as failure criteria stent migration observed during follow-up and persistent hydronephrosis assessed through ultrasound images, in particular after stent removal, independently from the time frame after the stent was removed.
Surgical technique
Allium™ stent positioning
The Allium™ stent is a newly developed ureteral stent, which can be inserted in the strictures of a small diameter and spontaneously expands and preserves a large caliber. The stent is coated with a biochemical copolymer that prevents tissue ingrowth and encrustation, and it can be inserted endoscopically with an intraoperative X-ray guidance. Furthermore, according to the site of the stenosis, when it involves the distal segment of the ureter, the Allium™ stent designed with the intravesical anchor should be placed in order to avoid the migration of the device during the time it remains in place. The first step of the surgical technique is to assess the site and length of the stenosis through ureteroscopy and retrograde pyelography (Figure 1). After establishing the characteristics of the stenosis, a safety guidewire must be placed beyond the stenosis and a ureteral balloon device should be placed through a 24 F cystoscope in the center of the stenosis and then inflated to 20 atm for approximately 3 min according to the manufacturer’s recommendations (Figures 2A, B). After fluoroscopy confirms the disappearance or significant diminution of the ‘‘waist,’’ the Allium™ stent may be inserted into the ureter either by a retrograde or anterograde approach and its position fluoroscopically confirmed (Figure 2C). The tricks for this step consist of positioning the device with the medial portion in the most narrowed part of the stricture in order to obtain the maximum strength to maintain dilatation and to avoid migration.
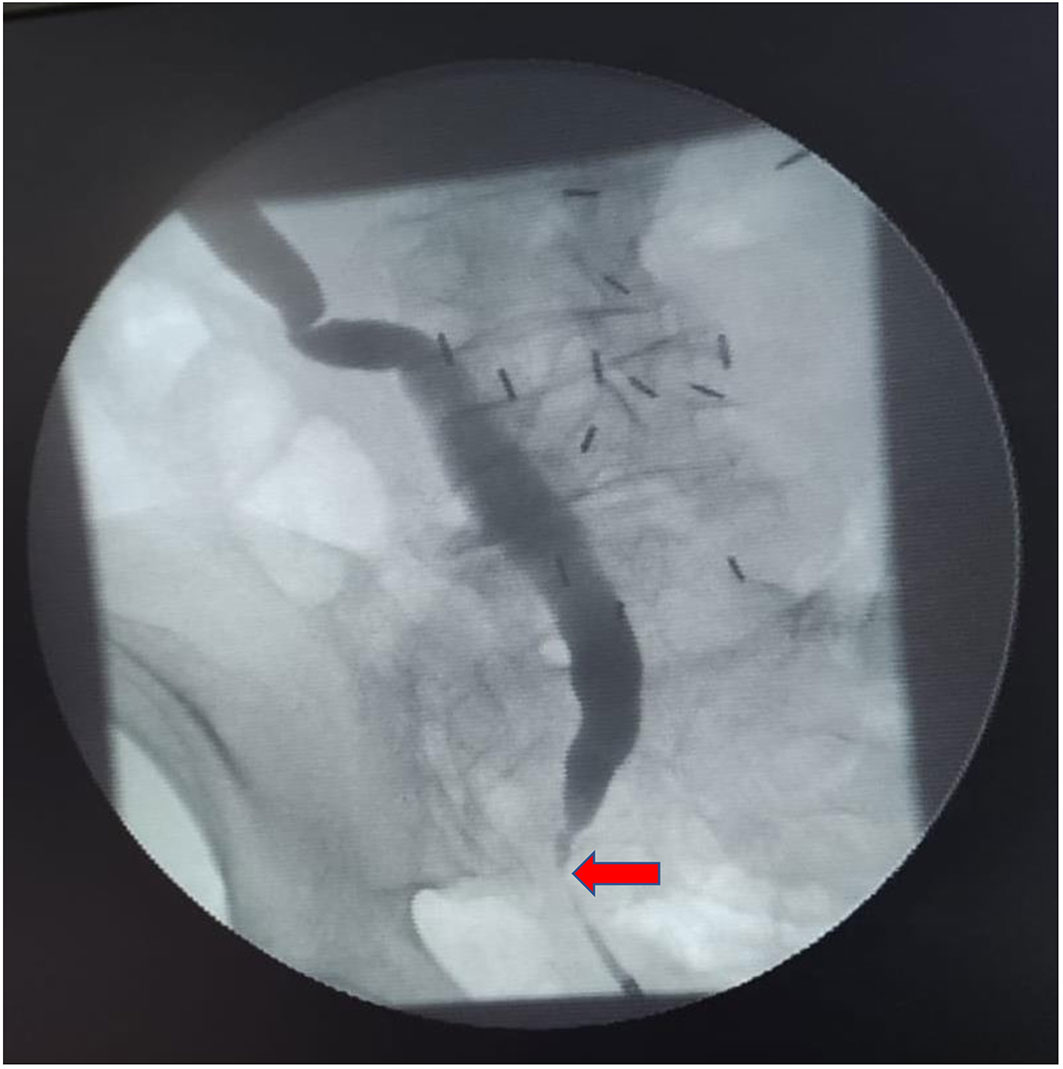
Figure 1 Retrograde pyelography showing low ureteral stenosis in a 65-year-old patient with right ureteral stenosis secondary to impacted stone. The length of stenosis was 2 cm. Red arrow shows the location of the stricture.
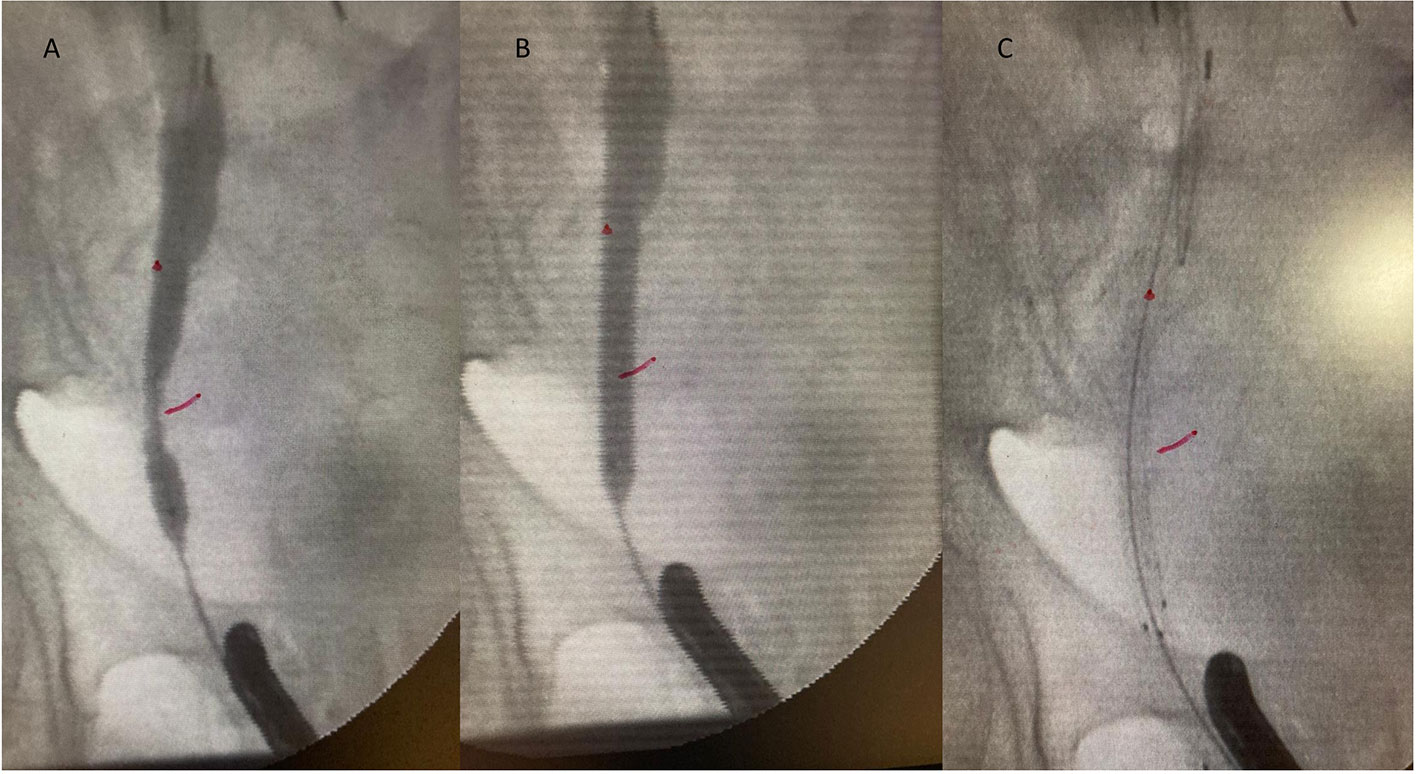
Figure 2 Balloon dilation of the stenosis (A, B). The red line shows the point of maximum shrinkage. Allium ureteral stent implanted (C) (Note: the Allium™ stent was implanted with the median portion in the most narrowed part of the stricture [red line] to obtain the maximum strength, to maintain the dilatation, and finally, to avoid the migration of the stent.
Allium™ stent removing
According to the position of the Allium™ stent, it can be removed either by a ureteroscopy or cystoscopy approach; in the case of the intravesical anchor, the Allium™ stent is removed by grasping the anchor with endoscopic forceps. The keys to safe and successful removal are the following: first, a retrograde pyelography should be obtained and a guidewire should be positioned into the Allium™ under endoscopic and X-ray control; secondly, the anchor or the distal part of the Allium™ should be catched by endoscopic forceps. Finally, the Allium should be gently removed obtaining the unraveling of the nytinol wire under fluoroscopic control. After stent removal, ureteroscopy can be performed in order to assess the condition of the ureter and stricture.
Statistical analysis
Continuous variables are expressed as the mean ± SD or median (range expressed as min–max), and categorical variables are expressed as numbers and percentages. The statistical comparisons of the continuous data were performed using the rank-sum test, and a P-value <0.05 was considered to indicate statistically significant differences. Statistical analysis was performed using STATA software version 17.0.
Results
Between April 2017 and May 2021, 151 patients were treated with Allium™ stents for ureteral strictures including benign and malignant stenosis. In total, 83 of them met the inclusion criteria for benign ureteral stricture and were included in final analysis. About the etiology of strictures, 79 (95.18%) were secondary to ureteroscopy or impacted stones and 4 (4.82%) were secondary to pelvic surgery. The general characteristics of the patients are listed in Table 1. The median operating time was 47.9 ± 15.53 min, and the median length of strictures was 2.51 ± 0.84 (1-4) cm. Regarding hospital stay, all patients were treated as 1-day surgery. The location of the stenosis was as follows: 28 (33.73%) upper ureter, 24 (28.92%) medial ureter, and 31 (37.35%) lower ureter. After surgery in the postoperative period, two (2.4%) patients needed analgesic therapy due to persistent pain in the surgical area, one (1.2%) patient developed fever, and three (3.61%) patients developed hematuria. No intraoperative or perioperative major complications were recorded according to the Clavien–Dindo classification (only grade I complications were reported from patients). Stent removal was performed after an average time of 6 months (range min–max, 3–12 months). The overall success rate was 85.5% (71/83) with a median follow-up of 18 months (range 1–48 months) (Table 2). A total of 12 (14.5%) patients experienced failure: in 10 patients (83.33%), stricture relapses were observed, 8 out of 10 presented preoperative stricture length between 2 and 4 cm, and 2 (16.67%) patients with preoperative pyelus–ureteral junction stenosis experienced stent migration in the renal pelvis at the first month of follow-up, which was observed after X-ray control with persistent hydronephrosis confirmed with ultrasound images. All patients who experienced failure were treated surgically either with a robotic or laparoscopic approach.
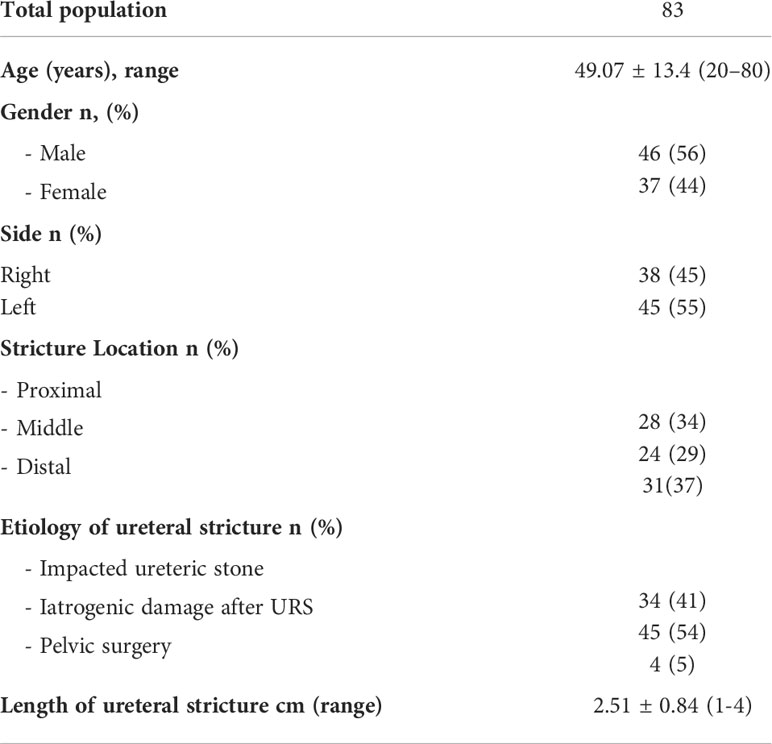
Table 1 Demographic and clinical characteristics of the population (quantitative data presented as mean ± SD).
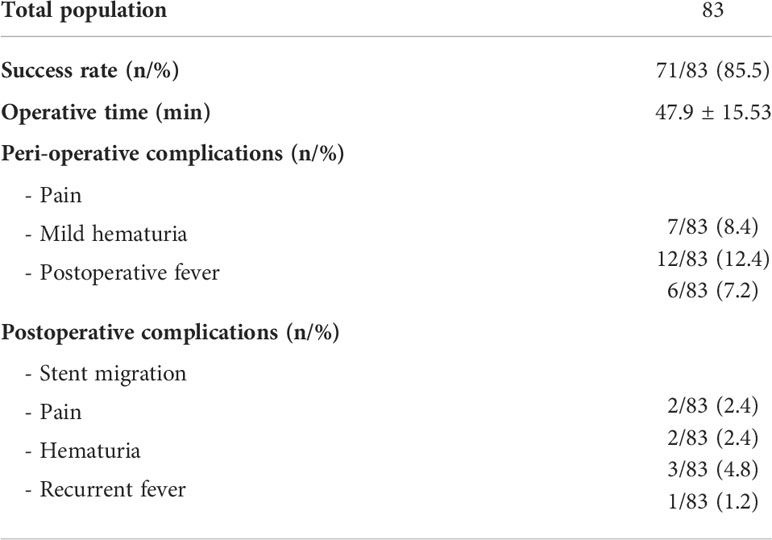
Table 2 Main outcomes and procedure-related characteristics (quantitative data presented as mean ± SD).
Discussion
The management of ureteral strictures is a great challenge for urologists. Traditionally, the surgical treatment of ureteral strictures included uretero-ureteral anastomosis, ileal substitution, autotransplant, or, in some cases, an indwelling stent or nephrostomy tube (11). Thanks to technological evolution, endoscopic treatments such as balloon dilation, cold knife incision, and laser endoureterotomy are more becoming more common, including the new types of ureteral metallic stent placement (12). The Allium™ stent is a newly developed ureteral stent, which can be inserted in structures of a small diameter and spontaneously expands and preserves a large caliber. The Allium™ (Allium Medical, Caesarea, Israel) is a self-expanding large-caliber stent made of a super elastic Nitinol alloy covered by a polymeric material that prevents tissue ingrowth and early encrustation (9). In this study, we present our experience with the Allium™ stent positioned as a curative treatment of benign ureteral strictures. Previous experiences with the Allium™ stent have shown encouraging results (8–10). However, many of these studies included small samples, mixed populations with malignant and benign strictures and, most importantly, in all these studies, the use of the Allium™ stent was mainly evaluated as a permanent device rather than active and temporary treatment. To our knowledge, our study is the first to analyze the effectiveness and safety of the Allium™ stent as a curative treatment in a specific population presenting benign ureteral strictures. Compared with previous studies in which the Allium™ stent was used as a permanent device with the aim of overcoming the limitations of the double-j stent, in this study, we evaluated the effectiveness of the Allium™ stent as definitive minimally invasive therapy. We observed a success rate of 85.5% with a good safety profile. The rationale of our study is mainly based on the etiopathogenesis of benign ureteral stenosis (13, 14). Impacted stones and the iatrogenic damage of the ureteral wall seem to have the same mechanism leading to scar formation, which includes a cascade of events that finally lead to stenosis: ureteral stones cause persistent irritation that leads to edema and fibrosis in the ureteral mucosa. There are some histological findings showing the occurrence of chronic interstitial fibrosis and urothelial hypertrophy at the stone impaction area, decreased blood flow due to prolonged physical pressure, or an immunological response toward stone material causing severe and chronic inflammation at the ureteral mucosa (15). After balloon dilation, the Allium™ stent, due to its unique properties, could act as a scaffold to rebuild a normal epithelium around the stent and avoid scar formation. In this context, the main question still open is when we can consider the remodeling process finished and, consequently, when we can remove the stent. In this first experience, the Allium™ stent was removed after a median time of 6 months and the overall success rate achieved (85.5%) supported this timing. With a similar concept Gao X et al. recently proposed a new technique of ureteric bypass using the Allium™ stent (16). They observed an overall success rate of 92% with a favorable safety profile. Similarly to Gao, in our experience, we have observed a good safety profile that supports its use in clinical practice as a mini-invasive strategy. In fact, we did not observe major complications according to the Clavien–Dindo classification during stent positioning and removal. We know that the removal of an indwelling stent attached to the wall could be a dangerous maneuver; however, due to its favorable properties, we suggest to gently remove the Allium™ by unravelling the nytinol wire in order to perform a safe procedure. The retrospective nature of our study did not allow us to identify the predictive factors of success. Indicatively, among the population of our study, 12 patients experienced failure, 10 (83.33%) patients presented ureteral strictures again, and, in particularm we noticed that 8 of them presented a stenosis between 2- and 4-cm long suggesting that the length of the stenosis could be the main predictor of failure. Moreover, since only four patients presented a stricture secondary to pelvic surgery, it did not allow us to perform a robust analysis in order to estimate the effectiveness and safety of the Allium™ stent in this group of patients. Our study presents some other limitations: firstly, we did not know which is the role of Allium™ stent over balloon dilation alone since this procedure is a key step performed before Allium™ stent positioning. Therefore, a randomized study comparing balloon dilation alone vs. balloon dilation plus the Allium™ stent should be performed in order to better define the added value of the Allium™ stent. However, a recent metanalysis on the functional outcomes of balloon dilation clearly showed that the effectiveness of the procedure decreases significantly during follow-up (12 months) with a median success rate of 54% (6). Our results (85.5% of success rate) with a median follow-up of 18 months support the hypothesis that guiding tissue remodeling around the Allium™ device may be the key to success. Many minimally invasive techniques currently available including balloon dilation and incision are often characterized by the recurrence and formation of exuberant scar tissue (6). In our opinion, the innovation of our approach lies precisely in the fact of exploiting the properties of the stent allium in guiding the tissue remodeling around the walls of the Allium™ stent in order to avoid excessive scarring that leads to the recurrence of the stenosis. Another important limitation of our study was the definition of “success.” In this context, there is a wide range of definitions that make it difficult to compare the results of the different studies. In this study, during follow-up, we used only ultrasound imaging to monitor hydronephrosis without any data on renal function or functional imaging such as mercaptoacetyltriglycine-3 diuretic renal scan. To date, among the studies involving the Allium™ stent, only Gao et al. reported longitudinal data on renal function such as creatinine, urea serum levels, and glomerular filtration rate (GFR) and they observed a significant decline between preoperative and during follow-up only for urea nitrogen levels (5.68 mmol/L ± 1.26 vs. 5.11 ± 1.42, p 0.007) and for the hydronephrosis volume (17.88 volume/cm3 ± 14.55 vs. 8.97 ± 7.82, p 0.014) but not for creatinine levels and GFR (16). Despite the lack of data about renal function that represents a clear limitation of our study, we believe that the results observed by Gao et al. support the use of “hydronephrosis reduction” as a marker of success for this type of surgery. Moreover, there are several studies that clearly suggest a degree of association between the hydronephrosis grade and renal cortical damage (17, 18). In conclusion, in our preliminary experience, an Allium™ stent may be considered as an effective and safe surgical treatment for benign ureteral stricture. Further analysis and prospective trials are necessary to better define the role of the Allium™ stent in the treatment of benign ureteral strictures.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Reviewer Board (PROTOC #61.22_12_21.1), Department of Maternal-Infant and Urological Sciences, “Sapienza” University of Rome, Policlinico Umberto I Hospital, Rome, Italy. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wolf JS Jr., Elashry OM, Clayman RV. Long-term results of endoureterotomy for benign ureteral and ureteroenteric strictures. J Urol (1997) 158:759–64. doi: 10.1016/S0022-5347(01)64308-8
2. Liapis A, Bakas P, Giannopoulos V, Creatsas G. Ureteral injuries during gynecological surgery. Int Urogynecol J (2001) 12:391–4. doi: 10.1007/PL00004045
3. Tyritzis SI, Wiklund NP. Ureteral strictures revisited … trying to see the light at the end of the tunnel: a comprehensive review. J Endourol (2015) 29(2):124–36. doi: 10.1089/end.2014.0522
4. Paffenholz P, Heidenreich A. Modern surgical strategies in the management of complex ureteral strictures. Curr Opin Urol (2021) 31(2):170–6. doi: 10.1097/MOU.0000000000000849
5. Lucas JW, Ghiraldi E, Ellis J, Friedlander JI. Endoscopic management of ureteral strictures: an update. Curr Urol Rep (2018) 19(4):24. doi: 10.1007/s11934-018-0773-4
6. Lu C, Zhang W, Peng Y, Li L, Gao X, Liu M, et al. Endoscopic balloon dilatation in the treatment of benign ureteral strictures: A meta-analysis and systematic review. J Endourol (2019) 33(4):255–62. doi: 10.1089/end.2018.0797
7. Corrales M, Doizi S, Barghouthy Y, Kamkoum H, Somani B, Traxer O. A systematic review of long-duration stents for ureteral stricture: which one to choose? World J Urol (2021) 39(9):3197–205. doi: 10.1007/s00345-020-03544-x
8. Guandalino M, Droupy S, Ruffion A, Fiard G, Hutin M, Poncet D, et al. Stent allium urétéral dans la prise en charge des sténoses urétérales. Étude rétrospective multicentrique [The allium ureteral stent in the management of ureteral stenoses, a retrospective, multicenter study]. Prog Urol (2017) 27(1):26–32. doi: 10.1016/j.purol.2016.11.005
9. Moskovitz B, Halachmi S, Nativ O. A new self-expanding, large-caliber ureteral stent: results of a multicenter experience. J Endourol (2012) 26(11):1523–7. doi: 10.1089/end.2012.0279
10. Bahouth Z, Meyer G, Halachmi S, Nativ O, Moskowitz B. Multicenter experience with allium ureteral stent for the treatment of ureteral stricture and fistula. Harefuah (2015) 154(12):753–6:806.
11. Gild P, Kluth LA, Vetterlein MW, Engel O, Chun FKH, Fisch M. Adult iatrogenic ureteral injury and stricture-incidence and treatment strategies. Asian J Urol (2018) 5(2):101–6. doi: 10.1016/j.ajur.2018.02.003
12. Sampogna G, Grasso A, Montanari E. Expandable metallic ureteral stent: indications and results. Minerva Urol Nefrol (2018) 70(3):275–85. doi: 10.23736/S0393-2249.18.03035-7
13. Roberts WW, Cadeddu JA, Micali S, Kavoussi LR, Moore RG. Ureteral stricture formation following removal of impacted calculi. J Urol (1998) 159:723–6. doi: 10.1097/00005392-199904020-00505
14. Doddamani D, Kumar R, Hemal AK. Stone granuloma–not to be forgotten as a delayed complication of ureteroscopy. Urol Int (2002) 68(2):129–31. doi: 10.1159/000048434
15. Yamaguchi K, Minei S, Yamazaki T, Kaya H, Okada K. Characterization of ureteral lesions associated with impacted stones. Int J Urol (1999) 6:281–5. doi: 10.1046/j.1442-2042.1999.00067.x
16. Gao X, Chen J, Wang W, Peng L, Di X, Xiao K, Li H, Wei X, et al. Step-by-step technique for the endoscopic treatment of ureteric stricture. BJU Int (2021) 128(6):692–6. doi: 10.1111/bju.15558
17. Konda R, Sakai K, Ota S, Abe Y, Hatakeyama T, Orikasa S. Ultrasound grade of hydronephrosis and severity of renal cortical damage on 99m technetium dimercaptosuccinic acid renal scan in infants with unilateral hydronephrosis during followup and after pyeloplasty. J Urol (2002) 167(5):2159–63. doi: 10.1016/S0022-5347(05)65118-X
Keywords: ureteral stenosis, urolithiaisis, ureteral stricture, Allium stent, metallic ureteral stent
Citation: Salciccia S, De Marco F, Sciarra A, Moriconi M, Alfarone A, Polese M, Maggi M, Del Giudice F, Gentilucci A, De Berardinis E and Ricciuti GP (2022) Allium stent as a curative treatment for benign ureteral strictures: Preliminary experience, surgical technique, and functional results. Front. Urol. 2:984719. doi: 10.3389/fruro.2022.984719
Received: 02 July 2022; Accepted: 29 August 2022;
Published: 21 September 2022.
Edited by:
Nicolomaria Buffi, Humanitas University, ItalyReviewed by:
Amelia Pietropaolo, University Hospital Southampton NHS Foundation Trust, United KingdomLorenzo Masieri, Meyer Children’s Hospital, Italy
Copyright © 2022 Salciccia, De Marco, Sciarra, Moriconi, Alfarone, Polese, Maggi, Del Giudice, Gentilucci, De Berardinis and Ricciuti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stefano Salciccia, stefano.salciccia@uniroma1.it
†These authors have contributed equally to this work
 Stefano Salciccia
Stefano Salciccia