- 1Department of Surgery, Division of Urology, The University of Vermont Medical Center, Burlington, VT, United States
- 2Department of Surgery, King Abdulaziz University, Rabigh, Saudi Arabia
- 3Department of Urology, Northwestern University, Chicago, IL, United States
Objective: To combat alarming postoperative opioid prescribing in the United States (U.S.), many surgical specialties implement pathways to limit routine use of opioids with the goal of zero opioid prescribing. We sought to examine outcomes after implementing non-opioid post ureteroscopy (URS) pathways at two academic centers in the U.S.
Materials and Methods: We examined patients who underwent URS utilizing a non-opioid postoperative pathway from November 1, 2016 – March 31, 2020. Primary outcomes included adverse events (Emergency Department (ED) presentation, and office phone calls for postoperative genitourinary symptoms).
Results: In total, 699 patients underwent URS with stent placement. Of these, 652 (89.4%) were discharged without opioids and 74 (10.6%) received opioids. Of those discharged without opioids, 484 (77.4%) received non-steroidal anti-inflammatory medications. Compared to patients discharged without opioids, patients prescribed opioids were more likely to present to the ED (67 (10.7%) vs 14 (19.9%), p=0.037) and call the clinic (102 (16.3%) vs 22 (29.7%), p=0.004). In a multivariate analysis, patients prescribed opioids post URS (OR 1.9, 95% CI 1.1 – 3.5, p=0.024) and patients who had an opioid prescription preop (OR 2.2, 95% CI 1.1 – 4.5, p=0.032) were associated with higher odds of calling the clinic. Older patients (OR 0.98, 95% CI 0.97 – 0.99, p=0.006) were less likely to call.
Conclusions: The study highlights almost 90% of patients can be discharged safely without opioids following URS. In our cohort, patients prescribed opioids experienced higher postoperative healthcare interactions. We hope our results encourage consideration of non-opioid pathways.
Introduction
The United States (US) is one of many countries struggling to control the opioid misuse epidemic sweeping the globe. Drug overdose deaths has increased in 2019 with 80% of these deaths involving ≥1 opioid (1). Despite these statistics and a growing awareness of the risks of prescribing opioids in the medical field, physicians in the US continue to prescribe large amounts of opioids, particularly postoperatively (2, 3). Concerted efforts by numerous surgical specialties are being made to mitigate the reflexive post-operative opioid prescribing by implementing opioid-free post-surgical care pathways. The American Urological Association (AUA) have issued a position statement and white paper on opioid use intended to guide urologists on pain management and opioid prescribing to reduce annual opioid prescribing. The AUA specifically encourages patient education, the use of non-opioid pain control adjuncts, and prescribing the fewest number and lowest potency of opioids when required (4, 5).
In the last two decades, thanks in part to technology advancements, there has been a global trend for increased ureteroscopy (URS) for the treatment of urolithiasis (6). Post URS a ureteric stent is often placed, particularly in the US. Although stents are useful for many situations, they can be associated with variable postoperative discomfort and widespread utilization of stents post-URS can significantly impair an overall large number of patient’s quality of life (QOL), particularly those with recurrent stone episodes. Unfortunately, very few modern advancements have succeeded in mitigating this patient reported discomfort despite a wide range of stent designs, surgical/stent placement techniques, or postoperative medications (7). Translational research has demonstrated that nonsteroidal anti-inflammatory drugs (NSAIDs) may relieve renal colic by inhibiting ureteric smooth muscle (8). This information has been supported clinically with NSAIDs in eligible patients often provided adequate pain management. Similarly, NSAIDs have been used for management of stent discomfort and many urologists implement post-operative NSAID prescribing into their practice along with various adjunct medications (anticholinergic, alpha blockers). However, despite the growing awareness about the opioid epidemic, many urologists still routinely reflexively prescribe opioids post-URS especially in the US and Canada compared to the rest of the world (2). Unfortunately, many individuals first exposure to opioids in the postoperative setting leads to long term negative health effects, including 6% persistent opioid use (9, 10).
To decrease physician over-prescribing, surgeons from both institutions began implementing post URS opioid-free pathways in 2016 (KS) and 2018 (AK). These pathways were focused on using a combination of pre- and postop counselling along with NSAIDs and adjunct non-opioid medications for stent tolerance. In previously published feasibility studies, these initial efforts demonstrated most patients can be discharged without opioids and avoid additional postoperative events or outpatient resource utilization (Emergency Department (ED) visits, patient phone calls) (11, 12). However, these studies were limited by small sample sizes, and it was unclear whether the opioid-free pathways would be maintained long term after their initial feasibility implementation or whether care teams would relapse to increased opioid prescribing. Therefore, we sought to perform a multicentered study that examined long term outcomes of established opioid-free post-URS pathways and determine their effectiveness. We hypothesize that our established opioid-free pathways will continue to manage patient expectations and postoperative pain without increasing unplanned office calls and ED visits while minimizing narcotic prescribing. Secondarily, we hope to encourage other urologists to implement post URS opioid-free pathways.
Materials and Methods
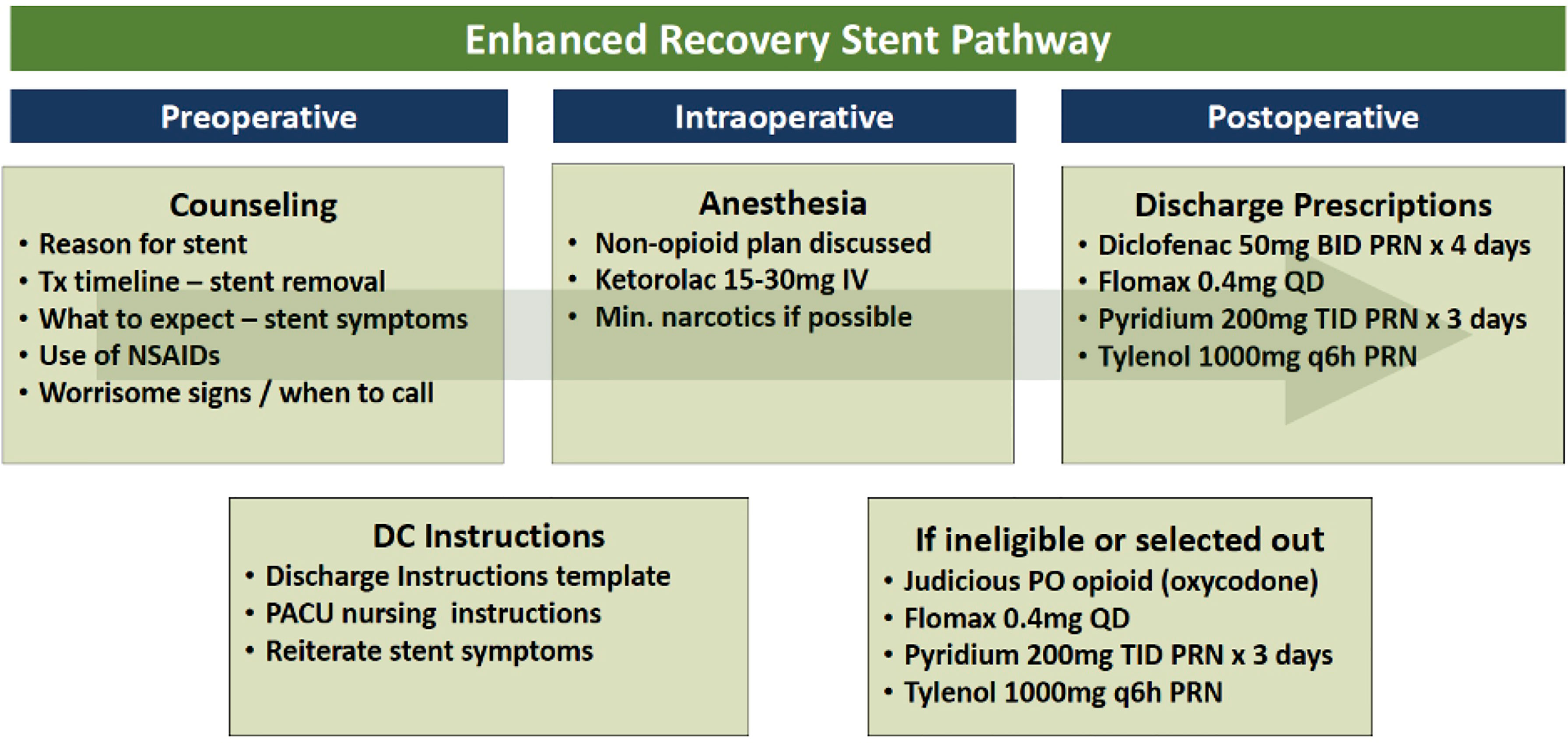
After obtaining institutional review board approvals, we retrospectively reviewed all adult (≥18 years old) patients undergoing URS with ureteric stent placement performed by two fellowship trained surgeons (KS, AK) at two academic medical centers in the United States from the start of instituting an opioid-free pathway (Nov 1, 2016 - KS & Feb 1, 2018 - AK) until March 1, 2020. A concerted effort was made during this period to determine the likelihood of a safe discharge post-URS without opioids for all patients. Details of the opioid-free pathways can be found in our institutions initial feasibility publications (11, 12). Briefly, a similar algorithm was used by both institutions to include patients in the opioid-free pathway (Figure 1). The post-URS opioid-free pathway included pre- and postop counselling which included patient handouts of common ureteric stent related symptoms. Additionally, the handouts provided education on the intent and rationale for NSAIDs use, intraoperative Ketorolac administration by anesthesia in patients without Chronic Kidney Disease (CKD) stage ≥2 or NSAIDs allergy, and postoperative prescription of NSAIDs and/or adjunct medications such as acetaminophen, phenazopyridine, and alpha blockers (Figure 1). In select patients whom providers felt may require opioids for pain control they were prescribed a limited (<10) quantity of either hydromorphone, oxycodone or tramadol. Opioid dependence was defined as a patient who filed ≥120-day supply of opioids or ≥3 opioid prescriptions in the year period preoperatively.
Predictor Variables
Bilateral URS procedures were included as a single patient encounter. We excluded patients who did not have ureteric stents placed post-URS or underwent any other combined procedures with URS (ex. Transurethral resection of bladder tumor, cystolitholopaxy). We collected patient’s demographics (Age, Body Mass Index (BMI), medical comorbidities (identified through Electronic Medical Record (EMR) International Classification of Diseases (ICD) diagnosis codes), urinary tract stone history), procedure characteristics (Operative time, ureter stent characteristics, utilization of laser) and prescribed postoperative medications (Opioid and non-opioid adjuncts).
Outcome Variables
Our primary outcomes were adverse event rates with the post-URS ureteric stent in place between the opioid-free and opioid prescribed cohorts. Adverse events for health care utilization were defined as post-operative visits to the ED or unplanned telephone calls to the clinic for genitourinary-related symptoms. Secondary outcomes were patient and operative factors associated with post-operative ED visits and telephone calls as well as factors associated with providers prescribing opioids post-URS.
Statistical Analysis
Statistical analysis was preformed using STATA v14 (College Station, TX, USA) (13). Patient demographics, procedure characteristics and adverse events by prescription cohort were compared using Chi-square test for categorical variables, Student’s t-test for continuous variables, and Wilcoxon rank-sum test for non-parametric continuous variables. Multivariate logistic regression analyses were used for binomial outcomes. Confounding factors were chosen a priori for each analysis and included in the multivariate model. All tests were two sided and a p-value ≤0.05 was considered statistically significant.
Results
Patient Characteristics
In total, 699 patients underwent URS with ureteric stent placement during the study period and were included in our analysis. Of these patients, 652 (89.4%) were discharged without opioids and 74 (10.6) received opioids postoperatively. Of those discharged without opioids, 484 (77.4%) received NSAIDs. Most patients were prescribed adjunct medications (acetaminophen, phenazopyridine, and/or alpha blockers) upon discharge (Table 1). This was not different between the two groups.
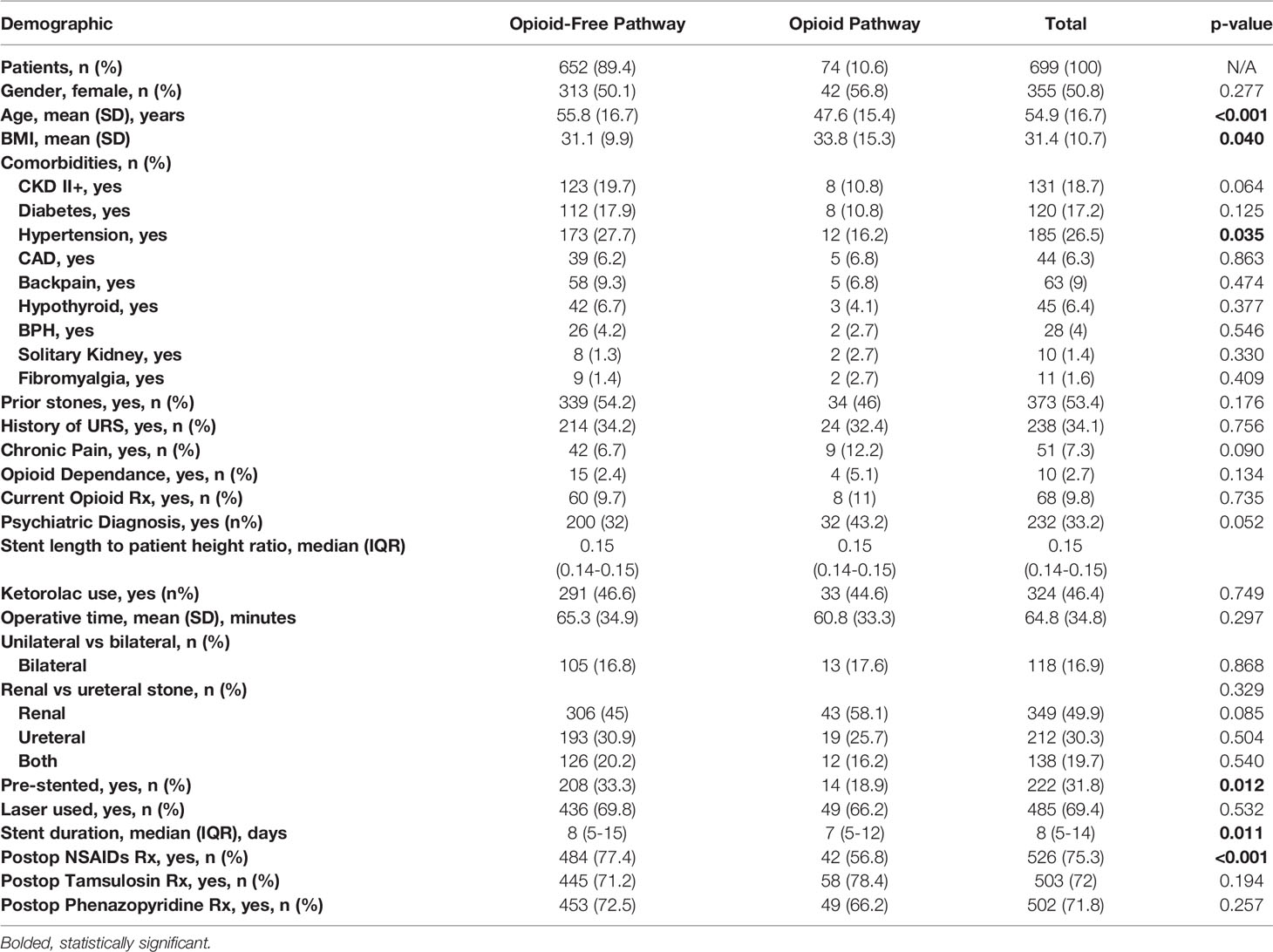
Patients in the opioid and opioid-free cohorts were similar across most patient demographics and procedure characteristics as outlined in Table 1. Overall average age was 54.9 years with BMI 31.4. The five most common comorbidities within the opioid-free, opioid prescribed and total cohorts were: psychiatric/mental health diagnosis (33.2%), hypertension (26.5%), chronic kidney disease grade ≥2 (18.7%) and diabetes (17.2%). Over half (53.4%) of patients were recurrent kidney stone formers with a third (34.1%) having undergone prior ureteroscopy.
The two cohorts differed with respect to patients who were prescribed opioids were younger, had higher body mass indexes, were less likely to have a diagnosis of hypertension, more likely to have a psychiatric diagnosis, less likely to be pre-stented before their procedures and less likely to receive NSAIDs postoperatively (Table 1).
Baseline Opioid Use
Overall, 7.3% of patients had a diagnosis of chronic pain with 2.7% of patients having opioid dependance prior to surgery and no difference detected between these rates in our two cohorts (opioid-free vs. opioid prescribed) (all p>0.05). There were 68/699 (9.8%) of patients who were actively on an opioid for pain management leading up to their planned surgical stone intervention with no difference detected between cohorts (p=0.735).
Stone Surgery
Average operative time was 64.8 minutes (Table 1) with no difference detected between the opioid-free and opioid prescribed cohorts (p=0.297). Bilateral URS was performed in 16.9% of our patients with stone distribution as follows: 49.9% renal, 30.3% ureteric, 19.7% both. There was a significant difference in the proportion that were pre-stented (18.9% opioid prescribed vs. 33.3% opioid-free, p=0.012) but no difference detected in rate of laser use intraoperatively or stent length to patient height ratio (all p>0.05). Average post-operative stent duration was 8 days (8 days opioid-free vs. 7 days opioid prescribed, p=0.011).
Factors Associated With Opioid Prescribing
In multivariate analysis, older age (OR 0.97, 95% CI 0.95 – 0.99, p=0.001), and being pre-stented (OR 0.5, 95% CI 0.3 – 0.9, p=0.042) were both associated with decreased odds of opioids prescribed post-URS by urologists at our institutions (Table 2). Characteristics included in this multivariate analysis included: gender, age, BMI, history of stones, URS, chronic pain, opioid dependence, current opioid use, psychiatric diagnosis, unilateral vs. bilateral, stone location, presence of pre-operative stent and use of the laser.
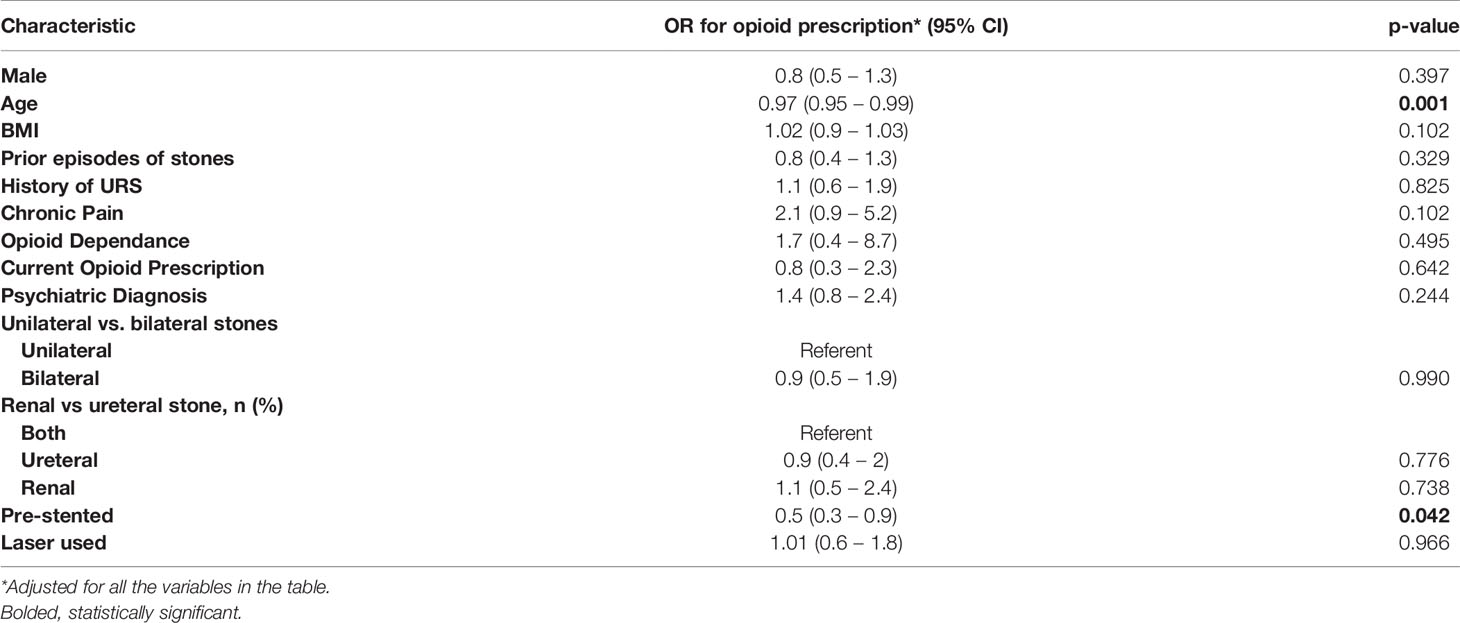
Table 2 Multivariate logistic regression analysis for factors associated with being provided an opioid prescription post-URS by providers at our institutions.
Post-URS Healthcare Interactions
Compared to patients discharged without opioids, patients who were prescribed opioids were more likely to present to the ED [67 (10.7%) vs 14 (19.9%), p=0.037] and call the clinic postoperatively for genitourinary symptoms [102 (16.3%) vs 22 (29.7%), p=0.004] (Figure 2). In multivariate analysis, no factors were associated with higher odds of ED visits (Table 3). Characteristics included in this multivariate analysis for ED presentations and clinic calls included: gender, age, BMI, history of stones, URS, chronic pain, opioid dependence, current opioid use, psychiatric diagnosis, unilateral vs. bilateral, stone location, presence of pre-operative stent, use of the laser and intraoperative NSAID use. However, patients prescribed opioids post-URS (OR 1.9, 95% CI 1.1 – 3.5, p=0.024) and patients who had an opioid prescription preop (OR 2.2, 95% CI 1.1 – 4.5, p=0.032) were associated with higher odds of calling the clinic for genitourinary symptoms. Older patients (OR 0.98, 95% CI 0.97 – 0.99, p=0.006) were less likely to call the clinic for genitourinary symptoms (Table 4).
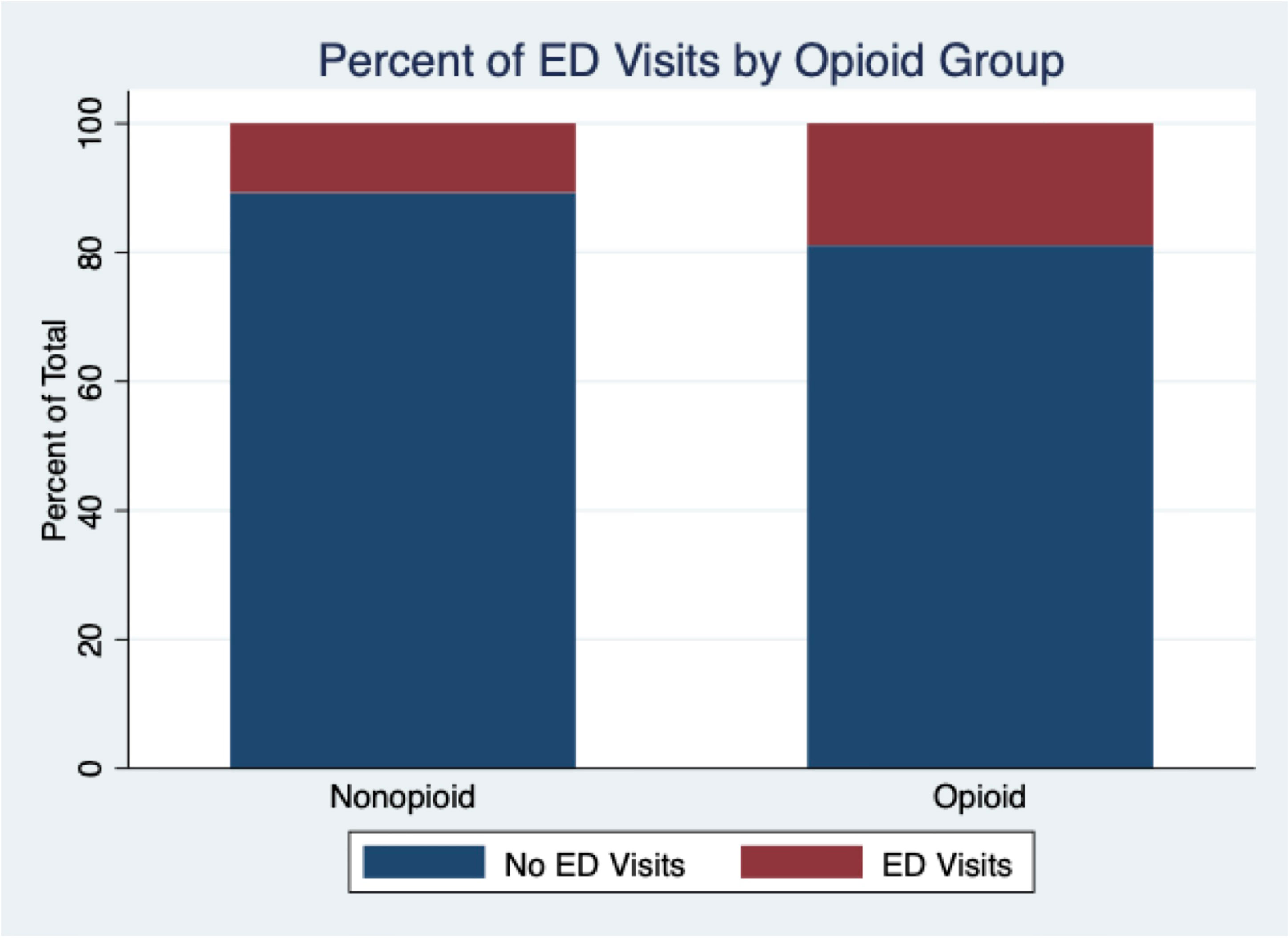
Figure 2 Proportion of patients in opioid-free prescribing pathway and opioid prescribing pathway that presented to ED following URS (p=0.037).
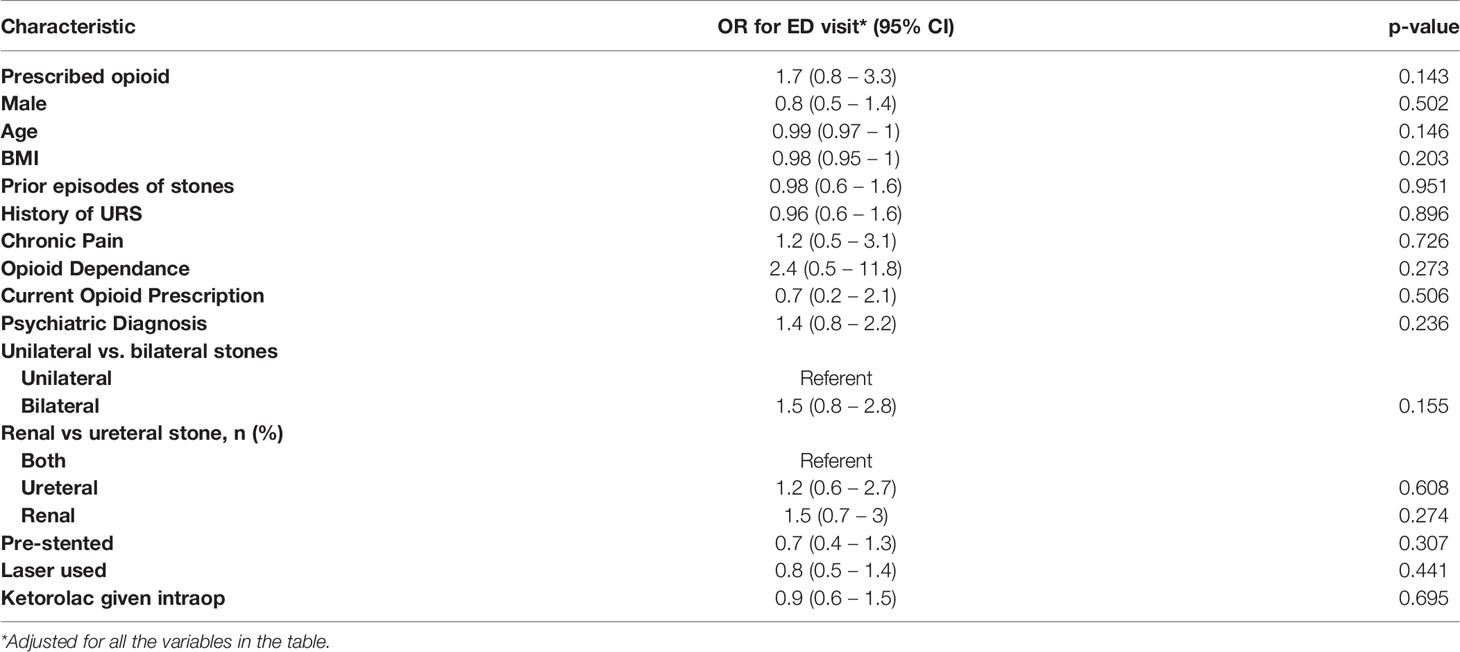
Table 3 Multivariate logistic regression analysis for factors associated with ED visits for genitourinary symptoms post-URS.
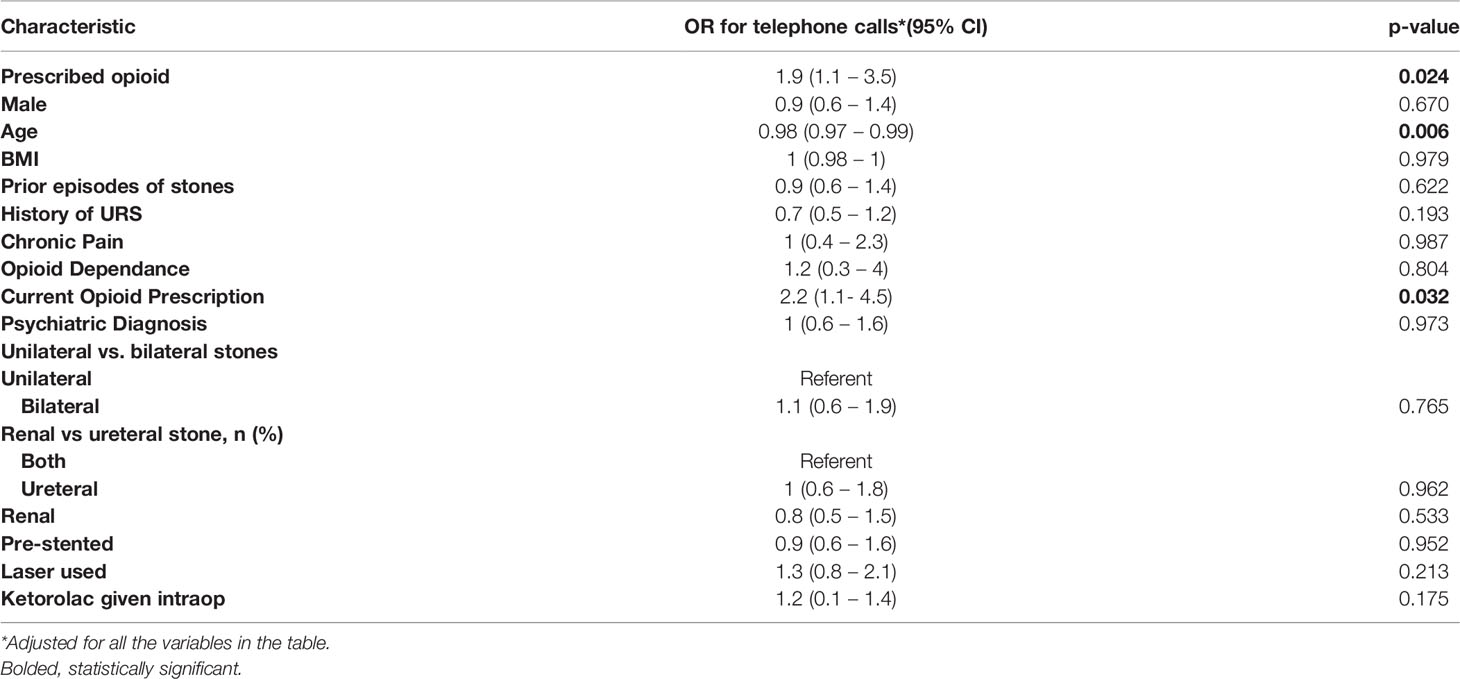
Table 4 Multivariate logistic regression analysis for factors associated with telephone calls to clinic for genitourinary symptoms post-URS.
Discussion
After establishing opioid-free post-URS pathways at two US academic centers we were able to maintain and achieve close to 90% opioid-free prescribing practices for patients leaving hospital postoperatively with a ureteric stent indwelling. A combination of urologic team and patient education on the postoperative expectations after ureteroscopy and stent placement along with preferential utilization of NSAIDs in eligible patients allowed for this transition. We demonstrated the long-term durability (>2years) of these opioid-free pathways without reverting to reflexive opioid prescribing. After establishing the opioid-free pathways at these two centers in 2016 and 2017, the first 6-month period at each institution saw a 73% and 50% opioid-free prescribing rate after ureteroscopy, respectively (11, 12). After >2years of establishing the pathways, the opioid-free prescribing rate has improved further achieving 85-90% over the most recent 6-month period.
Our primary outcome was to examine health care utilization (ED visits and unplanned office phone calls) postoperatively between our two patient cohorts. We found that patients who were prescribed opioids at the time of discharge from their surgery were significantly more likely to both present to the ED and to initiate unplanned phone calls to the urology office for genitourinary symptoms concerns. This highlights a unique cohort of patients who we can work to further educate and improve post-operative stent colic education in before leaving the hospital. One study examined that reflex opioid prescribing often provides medications that patients are not even utilizing (67% of postsurgical opioids remained unused in a urologic population) (14).
A recent study by our group examined the true rate of opioid free prescribing and detected 14-16% of patients failed opioid-free URS by seeking opioid prescriptions from other providers (PCP, ED, other urologists) (15). In some of these situations, patients’ pain may warrant further analgesic, however further education for other providers on preferred pain adjuncts to tolerate ureteric stents may help us further reduce this rate and represents an area for future research. Even accounting for this possible cohort of patients who seek opioid prescriptions from other providers along with those that were prescribed opioids by our teams at discharge, over 75% of patients can undergo URS with stent placement without utilizing opioids.
One important difference that we detected between the patients in the opioid-free pathway was higher rates of utilization of NSAIDs on discharge prescriptions compared to those who received opioids, despite equal rates of chronic kidney disease and no difference in contraindications to NSAID use among the groups. This represents an area for ongoing improvement in education for our care teams. In many situations, patients who utilized opioids preoperative for either urinary calculi pain management or concurrent medical conditions there can be a patient and provider perception that using a “perceived” weaker NSAID isn’t worth prescribing. However as mentioned above, NSAIDs may provide unique benefits for ureteric/stent colic symptoms and should be considered in eligible patients even those with opioid dependence to provide adjunct management. Many of these adjuncts have shown to be beneficial for stent colic symptoms in some patients, including alpha blockers, or methylprednisolone tapers and should be offered to patients with ongoing stent symptoms (16).
Other studies have found correlation between opioid misuse and younger age, mental health illnesses, prior stone surgeries and preoperative opioid use, however the vast majority of patients in these studies were receiving postop opioids in contrast to our predominately opioid-free post-URS cohort (17). Our study did not identify that prior episodes of stones, stone surgeries, preop opioid dependence, chronic pain or current opioid use was associated with rate of prescribing opioids post-URS. Also, similar to the literature, older patients were less likely to be prescribed opioids.
One limitation of our study is the retrospective nature of the study design and inability to control for all patient and operative characteristics between the opioid prescribed and opioid-free pathway patients. We did not confirm if patients had a pre-operative opioid prescribed by their PCP or received post-op opioids from an alternative prescriber. Additionally, we did not confirm that prescribed and filled prescription medications were physically taken by patients. Moving forward it would be useful to create a patient reported survey for the 10% of patients who were prescribed opioids postoperatively to further understand the amount of their prescription that they took, if any. This would also help provide our centers with a better ability to target the AUA recommended minimal number of opioid tablets to manage patients who need them at the time of discharge. We did not control for postop complication and resultant hospital admissions post-URS which may affect analgesic use, although the vast majority were performed as uncomplicated day surgeries. We did not find significant factors associated with postoperative ED presentations on multivariate analysis which may be secondary to our low (n=81) postop ED presentation rate. This represents an area for future study with a prospective design. One difference we found within the opioid prescribed patient cohort was a lower rate of preoperative stent placement (18.9% vs. 33.3%). Although we controlled for this difference within our analysis, preop stenting may theoretically reduce ureter trauma although there is no evidence to support uniformly pre-stenting all patients prior to URS from a stone free success rate or health care resource utilization perspective. There is evidence that pre-operative stent placement has resulted in ureteral aperistalsis in porcine models and this may contribute to less pain and subsequently less opioid prescriptions in this cohort (18). Despite the difference in preop-stent placement, the overall rate of prior history of stones, URS and stents was not different between groups so the proportion of patients experiencing a ureteric stent for the first time following their OR was equal between the cohorts.
Conclusion
The study highlights almost 90% of patients can be discharged safely without opioids following URS. After establishing opioid-free pathways our centers were able to maintain low-opioid prescribing rates for >2 years without reverting to reflexive opioid prescribing practices. In our cohort, patients prescribed opioids experienced higher postoperative healthcare interactions (both ED visits and unplanned office phone calls). We hope our results encourage other urologists to consider establishing opioid-free pathways.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Indiana University HRPP University of Vermont IRB. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
Each named author has substantially contributed to conducting the underlying research and drafting of this original research article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
AK is a consultant for Boston Scientific, Lumenis, Virtuoso, Ambu and on the data safety monitoring board for Sonomotion.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. O’Donnell JG,M, Mattson CL, Hunter T, Davis NL. Vital Signs: Characteristics of Drug Overdose Deaths Involving Opioids and Stimulants - 24 States and the District of Columbia, January - June 2019. Morbid Mortal Weekly Rep (2020) 69:1189–97. doi: 10.15585/mmwr.mm6935a1
2. Kaafarani HMA, Han K, El Moheb M, Kongkaewpaisan N, Jia Z, El Hechi MW, et al. Opioids After Surgery in the United States Versus the Rest of the World: The International Patterns of Opioid Prescribing (iPOP) Multicenter Study. Ann Surg (2020) 272(6):879–86. doi: 10.1097/SLA.0000000000004225
3. Awad MA, Sober DW, Chew BH, Breyer BN, Plante MK, et al. Patterns of Opioid Prescription Post Ureteroscopy Among Members of the Endourological Society. Trans Androl Urol (2021) 10:851. doi: 10.21037/tau-20-1121
4. Directors ABo. AUA Position Statement: Opioid Use (2019). Available at: https://www.auanet.org/guidelines/opioid-use.
5. Robles J, Abraham NE, Brummett C, Davies B, Graff V, Gupta R, et al. Rationale and Strategies for Reducing Urologic Post-Operative Opioid Prescribing (2021). American Urol Assoc Educ Res. (2021) 1–14.
6. Geraghty RM, Jones P, Somani BK. Worldwide Trends of Urinary Stone Disease Treatment Over the Last Two Decades: A Systematic Review. J Endourol (2017) 31(6):547–56. doi: 10.1089/end.2016.0895
7. Fischer KM, Louie M, Mucksavage P. Ureteral Stent Discomfort and Its Management. Curr Urol Rep (2018) 19(8):64. doi: 10.1007/s11934-018-0818-8
8. Chaignat V, Danuser H, Stoffel MH, Z'Brun S, Studer UE, Mevissen M. Effects of a Non-Selective COX Inhibitor and Selective COX-2 Inhibitors on Contractility of Human and Porcine Ureters In Vitro and In Vivo. Br J Pharmacol (2008) 154(6):1297–307. doi: 10.1038/bjp.2008.193
9. Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg (2017) 152(6):e170504. doi: 10.1001/jamasurg.2017.0504
10. Tam CA, Dauw CA, Ghani KR, Gunaseelan V, Kim T, Leavitt DA, et al. New Persistent Opioid Use After Outpatient Ureteroscopy for Upper Tract Stone Treatment. Urology (2019) 134:103–8. doi: 10.1016/j.urology.2019.08.042
11. Sobel DW, Cisu T, Barclay T, Pham A, Callas P, Sternberg K. A Retrospective Review Demonstrating the Feasibility of Discharging Patients Without Opioids After Ureteroscopy and Ureteral Stent Placement. J Endourol (2018) 32:1044–9. doi: 10.1089/end.2018.0539
12. Large T, Heiman J, Ross A, Blake A, Krambeck A. Initial Experience With Narcotic-Free Ureteroscopy: A Feasibility Analysis. Journal of Endourology. J Endourol(2018) 32:907–11. doi: 10.1089/end.2018.0459
14. Bates C, Laciak R, Southwick A, Bishoff J. Overprescription of Postoperative Narcotics: A Look at Postoperative Pain Medication Delivery, Consumption and Disposal in Urological Practice. J Urol (2011) 185(2):551–5. doi: 10.1016/j.juro.2010.09.088
15. Lee MS, Assmus M, Agarwal D, Rivera ME, Large T, Krambeck AE. Opioid Free Ureteroscopy: What Is the True Failure Rate? Urology (2021) 154:89–95. doi: 10.1016/j.urology.2021.03.011
16. Hamidi N, Ozturk E, Yikilmaz TN, Atmaca AF, Basar H. The Effect of Corticosteroid on Postoperative Early Pain, Renal Colic and Total Analgesic Consumption After Uncomplicated and Unstented Ureteroscopy: A Matched-Pair Analysis. World J Urol (2018) 36(6):979–84. doi: 10.1007/s00345-018-2210-1
17. Kang C, Shu X, Herrell DS, Miller NL, Hsi RS. Opiate Exposure and Predictors of Increased Opiate Use After Ureteroscopy. J Endourol (2019) 33:480–5. doi: 10.1089/end.2018.0796
Keywords: pain, opioid, ureteroscopy, stent, care pathway
Citation: Awad MA, Assmus MA, Berg AN, Lee MS, Hallgarth LA, Krambeck AE and Sternberg KM (2022) Outcomes of Opioid-Free Pathways Post-Ureteroscopy: Joint Analysis From Two Academic Centers. Front. Urol. 2:893161. doi: 10.3389/fruro.2022.893161
Received: 10 March 2022; Accepted: 29 March 2022;
Published: 28 April 2022.
Edited by:
Marlon Perera, Memorial Sloan Kettering Cancer Center, United StatesReviewed by:
Liang Qu, University of Melbourne, AustraliaMahesh R Desai, Muljibhai Patel Urological Hospital, India
Copyright © 2022 Awad, Assmus, Berg, Lee, Hallgarth, Krambeck and Sternberg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark A. Assmus, bWFyay5hc3NtdXNAbm0ub3Jn
†These authors have contributed equally to this work and share first authorship
 Mohannad A. Awad1,2†
Mohannad A. Awad1,2† Mark A. Assmus
Mark A. Assmus Adrian N. Berg
Adrian N. Berg Matthew S. Lee
Matthew S. Lee Kevan M. Sternberg
Kevan M. Sternberg