
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 17 July 2024
Sec. Pediatric Surgery
Volume 11 - 2024 | https://doi.org/10.3389/fsurg.2024.1369255
Introduction: Blunt diaphragmatic rupture (BTDR) is a rare condition that can occur in children following high-energy blunt thoracoabdominal trauma. In less than 1% of the cases, pericardial rupture can coexist with a BTDR. A coexistence of BTDR and pericardial rupture can result in displacement of the heart and is associated with high mortality. Clinical presentation is non-specific and requires a high index of suspicion for early management.
Case presentation: A 4-year-old child presented to the emergency unit of our hospital following high-energy trauma with severe respiratory distress. Initially, a left-side chest tube was inserted, but it resulted in no clinical improvement. A chest x-ray showed a collapse of the left lung with a herniation of bowel loops into the left hemithorax. An exploratory laparotomy was done, which revealed a 10 cm × 4 cm defect in the left hemidiaphragm with a medial extension involving the pericardium. The fundus of the stomach and left lobe of the liver were displaced into the pericardial space, pushing the cardiac apex posteriorly to the right side. Concomitantly, the transverse colon and small bowel were displaced into the left pleural space. After the reduction of the herniated abdominal viscera back into the peritoneal cavity, the pericardial sac was repaired by employing an interrupted resorbable suture, while the diaphragmatic defect was repaired by using a horizontal mattress. No other injuries were identified and the abdomen was closed in layers.
Conclusion: BTDR with pericardial rupture is an elusive condition with a high mortality rate that necessitates a high index of clinical suspicion. Early surgical repair of the defect with a reduction of herniated organs can reduce morbidity and mortality.
Diaphragmatic rupture following blunt abdominal trauma is a rare case scenario, with the rate of incidence ranging from 1% to 7% (1). Incidence is particularly low in children, with less than 1% of pediatric trauma resulting in diaphragmatic rupture (2, 3). Since most incidences of blunt traumatic diaphragmatic rupture (BTDR) result from high-energy traumas such as motor vehicle accidents or falls from height, patients often present with severe injuries to the other visceral organs (2, 4–7). Meanwhile, the coexistence of a pericardial rupture is very rare, with the rate of incidence ranging from 0.2% to 3.3% (4). Pericardial ruptures are associated with a high mortality rate (1, 8, 9). Communication between the abdominal cavity and the pericardial space through the tear can allow a herniation of abdominal organs into the chest cavity and pericardial space, resulting in cardiac tamponade, respiratory compromise, or gastrointestinal obstruction (1, 8). The management of choice is early reduction of hernia contents and repair of the defect (1, 4, 10). In this study, we report a rare case of a patient with BTDR with a herniation of the abdominal viscera into the chest cavity and an isolated pericardial rupture with a subluxation of the heart.
A 4-year-old male child presented to the emergency unit of our hospital after he was hit by a high-velocity vehicle. At the emergency unit, he showed signs and symptoms of respiratory distress with RR 66 breaths/min and an SpO2 of 66% at room air and 72% on a 10 L facemask. His blood pressure was 88/40 mmHg and pulse rate was PR 144 beats per minute and regular. The child showed no signs of head injury or a grossly visible fracture. A physical examination revealed absent air entry and hyperresonance on the left side of the chest with abrasion over his left chest wall and flank. The initial impression was a tension pneumothorax, following which a tube thoracostomy was done on the affected side. However, there was no gush of air or blood following tube thoracostomy nor any clinical improvement. Subsequently, a chest x-ray revealed left lung compression, herniation of bowel loops into the hemithorax, and mediastinal shift to the right side (Figure 1).

Figure 1 The yellow arrow indicates bowel loops with haustral markings and gas in the left hemithorax. The red arrow indicates a significant shift of the mediastinum to the right side. The image also shows significant tracheal deviation outlined by the yellow dashed line.
The patient was transferred to the operating room for an emergency exploration. A left transverse abdominal incision was performed. About 200 ml of blood in the peritoneal cavity with no gross contamination was identified. There was also a 10 cm × 4 cm left hemidiaphragmatic defect with medial extension resulting in a 4 cm × 2 cm pericardial sac defect (Figure 2).
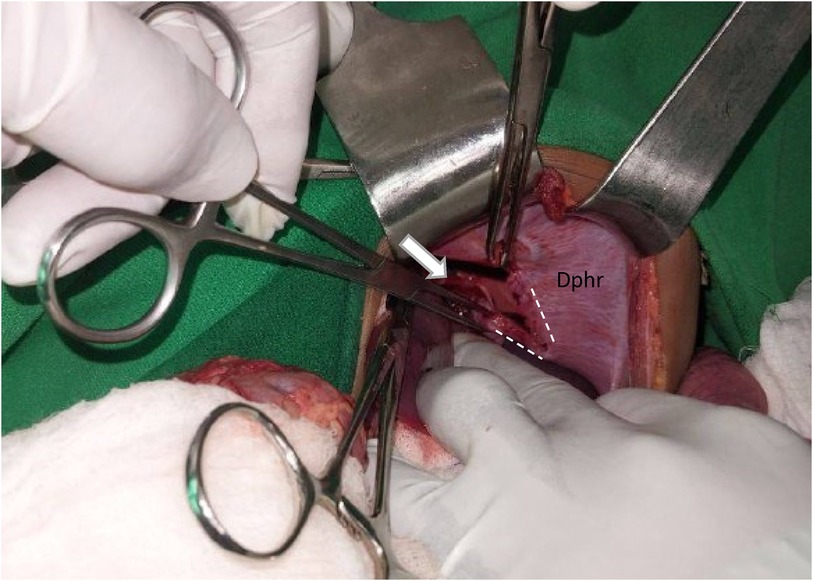
Figure 2 The white arrow indicates the pericardial sac tear. The white dashed line outlines the diaphragmatic defect. “Dphr” labels the left hemidiaphragm.
The transverse colon and proximal part of the small bowel herniated into the pleural cavity through the left hemi diaphragmatic defect with a contusion of the transverse colon at the level of the defect (Figure 3). However, there was no bowel perforation.
The edge of the left lobe of the liver and fundus of the stomach were uprooted into the pericardial space through the defect in the pericardium, pushing the cardiac apex posteriorly into the right side, but no myocardial contusion was seen. The herniated abdominal viscera were reduced into the peritoneal cavity. Recruitment of the collapsed left lung was done until there was complete expansion. No signs of air leak were evidenced post expansion. The pericardial defect was primarily closed with interrupted resorbable sutures. The diaphragmatic defect was primarily closed with an interrupted horizontal mattress. The integrity of the repair and diaphragmatic motion was then checked via large tidal volume administration. No other visceral injuries were identified, and the abdominal wall was closed in layers. A chest tube was kept in place for 48 h and removed after the evaluation of a control chest x-ray (Figure 4).
A traumatic diaphragmatic rupture is the loss of integrity of the diaphragm due to a sudden increase in intra-abdominal pressure from trauma (10–12). The most common site of rupture is at the junction of the muscle and tendon (3). Traumatic diaphragmatic rupture accounts for less than 0.5% of all trauma cases and 1.9% of all blunt traumas (11). The rate of incidence of BTDR is lower in the pediatric age group, standing at 0.18% of all pediatric traumas (2). Most BTDRs occur in the left posterolateral section of the diaphragm owing to the cushion effect of the liver on the right side (5, 8). A systematic review by Theodorou et al. showed a mortality rate of 2.8% among pediatric patients directly as a result of diaphragmatic rupture and associated herniation (2). The overall mortality rate was reported to be 33% among pediatric patients in studies by the National Trauma Data Bank (NTDB) (2). Patients with BTDR often present with injuries to the abdominal and chest organs (5). One study found that liver and spleen injuries occurred in 40%–60% of pediatric patients with BTDR (2).
Although injury to different organs is commonly associated with BTDR, a pericardial tear is very rare and is associated with a high mortality rate reaching up to 64% (4, 11). An isolated pericardial tear in a patient with BTDR is even rarer (12). However, the patient in this study presented with an isolated pericardial rupture with BTDR. Following blunt trauma, most pericardial ruptures occur in the left pleuropericardial region (12). Pericardial rupture is an elusive diagnosis, with most cases identified intraoperatively (5, 6). Similarly, the defect in the pericardial sac of our patient was identified intraoperatively. Most patients with pericardial rupture are asymptomatic and show signs and symptoms only when there is an associated herniation of the heart or when bleeding occurs (5). Large defects in the pericardium can result in dislocation or torsion of the heart (12). In our patient, there was a subluxation of the cardiac apex on the right side and the defect was closed, with herniated abdominal viscera preventing displacement of the heart out of the pericardial space through the defect.
The most common clinical symptoms of BTDR are signs and symptoms of respiratory distress followed by abdominal pain (2). Signs and symptoms of respiratory compromise can lead to a misdiagnosis of the pneumothorax, resulting in the insertion of a chest tube and iatrogenic injury to the herniated organ (12). In our patient, a similar misdiagnosis was made, and a chest tube was wrongfully inserted. Fortunately, there was no iatrogenic injury to the herniated bowel segments. Plain films of the chest and/or abdomen are the most common imaging methods used in acute cases, with sensitivity ranging from 27% to 73% (5). Findings on plain films associated with pericardial involvement include changes in the cardiac silhouette or axis, signs of pneumopericardium, and pericardial effusion (12). Computed tomography (CT) scans are more specific and sensitive than other imaging modalities to identify chest and abdominal injuries (5).
BTDR should be urgently repaired upon diagnosis, especially in left-sided diaphragmatic ruptures. Operative repair via the abdominal approach is the most common management for primary repair of the diaphragm, although the thoracic approach is recommended in cases of delayed diagnosis due to intra-abdominal adhesions from chronicity (2, 10, 11).
Diaphragmatic tear following blunt trauma is rare and is often associated with polytrauma. An isolated pericardial involvement is uncommon and difficult to detect before operation. As such, a high level of suspicion is required when evaluating patients with blunt trauma and respiratory distress. Emergent surgery with a reduction of herniated viscera and primary closure of diaphragmatic and pericardial defects can result in better patient outcomes.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the School of Medicine at the University of Gondar ethical board review. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
MK: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MA: Writing – original draft, Writing – review & editing. RA: Writing – original draft, Writing – review & editing. BA: Writing – original draft.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
2. Theodorou CM, Jackson JE, Beres AL, Leshikar DE. Blunt traumatic diaphragmatic hernia in children: a systematic review. J Surg Res. (2021) 268:253–62. doi: 10.1016/j.jss.2021.07.011
3. Burhamah W, Matcovici M, Hardy A, Awadalla S. Traumatic diaphragmatic rupture in children. J Pediatr Surg Case Rep. (2020) 61:101619. doi: 10.1016/j.epsc.2020.101619
4. Chellasamy RT, Rajarajan N, Pio Samy NM, Munusamy H. A rare case of traumatic pericardio-diaphragmatic injury following a road traffic accident. Cureus. (2023) 15(5):e39125. doi: 10.7759/cureus.39125
5. Özalp T, Küpeli M, Sönmezoğlu Y, Çakmak A, Akgül S, Fazlioğlu M, et al. Blunt diaphragmatic injuries: pericardial ruptures. Indian J Surg. (2017) 79(3):212–8. doi: 10.1007/s12262-016-1455-4
6. Gao R, Jia D, Zhao H, WeiWei Z, Yangming WF. A diaphragmatic hernia and pericardial rupture caused by blunt injury of the chest: a case review. J Trauma Nurs. (2018) 25(5):323–6. doi: 10.1097/JTN.0000000000000395
7. Davis PW. Traumatic herniation into the pericardial sac. Postgrad Med J. (1968) 44(517):875–8. doi: 10.1136/pgmj.44.517.875
8. Okamoto S, Maeyama H. Traumatic intrapericardial diaphragmatic hernia. Acute Med Surg. (2023) 10(1):e895. doi: 10.1002/ams2.895
9. Abou Hussein B, Khammas A, Kaiyasah H, Swaleh A, Al Rifai N, Al-Mazrouei A, et al. Pericardio-diaphragmatic rupture following blunt abdominal trauma: case report and review of literature. Int J Surg Case Rep. (2016) 19:168–70. doi: 10.1016/j.ijscr.2015.12.041
10. Öz N, Kargı AB, Zeybek A. Co-existence of a rare dyspnea with pericardial diaphragmatic rupture and pericardial rupture: a case report. Pol J Cardio-Thorac Surg. (2015) 2:173–5. doi: 10.5114/kitp.2015.52865
11. El Bakouri A, El Karouachi A, Bouali M, El Hattabi K, Bensardi FZ, Fadil A. Post-traumatic diaphragmatic rupture with pericardial denudation: a case report. Int J Surg Case Rep. (2021) 83:105970. doi: 10.1016/j.ijscr.2021.105970
Keywords: blunt trauma, diaphragmatic rupture, pericardial tear, pediatric trauma, heart subluxation
Citation: Kassie MT, Ayana MG, Abebe RB and Abebe BM (2024) Case Report: Surgical challenges and insights in a child with a blunt left diaphragmatic and pericardial rupture and heart subluxation. Front. Surg. 11: 1369255. doi: 10.3389/fsurg.2024.1369255
Received: 11 January 2024; Accepted: 27 June 2024;
Published: 17 July 2024.
Edited by:
Aydin Yagmurlu, Ankara University, TürkiyeReviewed by:
Ali Bilal Ulas, Atatürk University, Türkiye© 2024 Kassie, Ayana, Abebe and Abebe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melaku Tessema Kassie, bWVsZXRlc3NlbWExOEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.