- 1School of Medicine, Nankai University, Tianjin, China
- 2Graduate School of Tianjin Medical University, Tianjin, China
- 3Department of Spine Surgery, Tianjin Union Medical Center, Tianjin, China
Objective: This study aims to evaluate the clinical efficacy and safety between Discover cervical disc arthroplasty (DCDA) and anterior cervical discectomy and fusion (ACDF) in Cervical degenerative disc diseases.
Methods: Two researchers independently conducted a search of PubMed, EMBASE, and Cochrane Central Register of Controlled Trails (CENTRAL) for randomized controlled trials (RCTs) following the Cochrane methodology guidelines. A fixed-effects or random-effects model was applied based on different heterogeneity. Review Manager (Version 5.4.1) software was used to perform data analysis.
Results: A total of 8 RCT studies were included in this meta-analysis. The results indicate that the DCDA group had a higher incidence of reoperation (P = 0.03) and a lower incidence of ASD (P = 0.04) than the CDA group. There was no significant difference between two groups regarding NDI score (P = 0.36), VAS ARM score (P = 0.73), VAS NECK score (P = 0.63), EQ-5D score (P = 0.61) and dysphagia incidence (0.18).
Conclusion: DCDA and ACDF have similar results in terms of NDI scores, VAS scores, EQ-5D scores, and dysphagia. In addition, DCDA can reduce the risk of ASD but increases the risk of reoperation.
1. Introduction
Spinal degeneration is very common in the population. Some studies have shown that at age 50, about 80%–90% of people will show disk degeneration on magnetic resonance imaging (MRI) (1, 2). Degeneration of the cervical spine may further affect the cervical nerve roots and the cervical spinal cord, ultimately causing clinical symptoms.(3) The number of patients requiring surgical treatment for symptomatic cervical degenerative disease has increased in recent years. In the study by Kazuyoshi et al. (4), the number of patients who eventually required surgery for CDDD increased 1.9 times over 12 years. Previous research on this type of disease is extensive, and its treatment is varied.(5–7) Among them, ACDF is a recognized and effective means for treating this disease (8, 9). The success rate of ACDF and its clinical efficacy have been well demonstrated (10–12). However, ACDF can also cause some adverse effects. The complications that have been previously reported include postoperative development of angulation deformity, dysphagia, bone graft or instrumentation extrusion, adjacent segment degeneration, and postoperative mechanical instability of the cervical spine (13–15). In addition, biomechanical studies have also shown an increased incidence of disc degeneration at the level adjacent to the spinal fusion segment (16, 17). Hilibrand et al. (18) reported that approximately 25% of patients would develop further degeneration of the adjacent segment within 10 years after ACDF surgery. The emergence of CDA is to address some of the complications caused by ACDF. The theoretical advantage of cervical arthroplasty is its ability to preserve more segmental mobility, reducing the incidence of adjacent segmental degeneration and avoiding some of the limitations of ACDF (19, 20). However, CDA is not a perfect substitute for ACDF, as heterotopic ossification and implant migration or subsidence are common complications of CDA (21, 22). Multiple studies have compared the clinical efficacy and adverse events of CDA and ACDF, but the conclusions drawn from these studies are inconsistent (23, 24). Many meta-analyses integrate data from related articles in order to obtain more accurate results. Still, the type of prosthesis is often not taken into account in these articles (25–27). However, a meta-analysis by MD et al. (28) revealed that the clinical efficacy and the incidence of adjacent segmental disorders differed between the different classes of prostheses. Therefore, this article is dedicated to comparing one of the prostheses (Discover disc prosthesis) with ACDF.
2. Materials and methods
2.1. Search strategy
We performed a systematic review and meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. To make an exhaustive search of all relevant literature, we conducted a search of PubMed, EMBASE, and Cochrane Central Register of Controlled Trails (CENTRAL) for randomized controlled trials (RCTs) following the Cochrane methodology guidelines. We located studies with the following search terms: cervical disc arthroplasty, cervical disc replacement, CDA, CDR, artificial disc replacement, anterior cervical discectomy and fusion, ACDF, Discover. We did not restrict the language of the articles, and the literature search results were last updated on August 1, 2022. We also searched the reference lists of the included literature in case any relevant articles were missed. We obtained the full text of all potential articles. Two independent reviewers screened the titles and abstracts of these articles and finally determined the literature that met the criteria for this meta-analysis.
2.2. Criteria for selected trials
Articles that met the following criteria were included in our study: (1) An RCT comparing ACDF with Discover artificial disc replacement for cervical degenerative diseases. (2) The article contains information on at least one of the outcome indicators such as NDI score, VAS score, EQ-5D score, reoperation rate, dysphagia incidence, and ASD incidence. (3) The age of the individuals involved in the article should be older than 18 years; (4) The follow-up period in the literature should be at least >24 months. The exclusion criteria for the literature were as follows: (1) the articles were observational studies, reviews, or case reports. (2) Articles with incomplete data or continuous variables for which standard deviations were not available. (3) Repeated publication of the same data.
2.3. Data extraction
Two independent reviewers extracted data from the included literature. When we encountered discrepancies, we would reach a consensus by discussion. If necessary, we will combine the opinions of a third reference to make a final decision. The essential information extracted from the inclusive article includes the study design, sample size, sex distribution, age, experimental and control interventions, duration of follow-up, and outcomes. In this literature, the outcome indicators we analyzed included the NDI score, EQ-5D score, VAS score, and the number of patients presenting with dysphagia, reoperation, and ASD.
2.4. Quality of evidence assessment
Two researchers applying the Cochrane Collaboration tool evaluated the included literature. The content of the device consists of the following aspects: (1) random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessment; (5) incomplete outcome data; (6) selective reporting; (7) other bias. Each item is judged by high risk, low risk, or unclear risk. Disagreements will be resolved by discussion or by consulting a third author.
2.5. Statistical analysis
RevMan 5.4.1 (Cochrane, London, UK) was used to perform a combined analysis of the extracted data. The standardized mean difference (SMD) and its 95% confidence interval (CI) were calculated for the continuous data, and the risk ratio (RR) and its 95% CI were calculated for the dichotomous data. The heterogeneity of studies was estimated using the I2 tests: low heterogeneity (I2 < 25%), moderate heterogeneity (25% < I2 < 50%), and substantial heterogeneity (I2 > 50%). Due to the possible difference in disease severity of patients before surgery, all patients adopt random effect model. The possibility of publishing bias was not researched because of the limited number of included studies. We defined the follow-up period of fewer than 3 years as short-term follow-up and the follow-up period of more than 5 years as long-term follow-up. The statistically significant level was set at P < 0.05.
3. Results
3.1. Search results
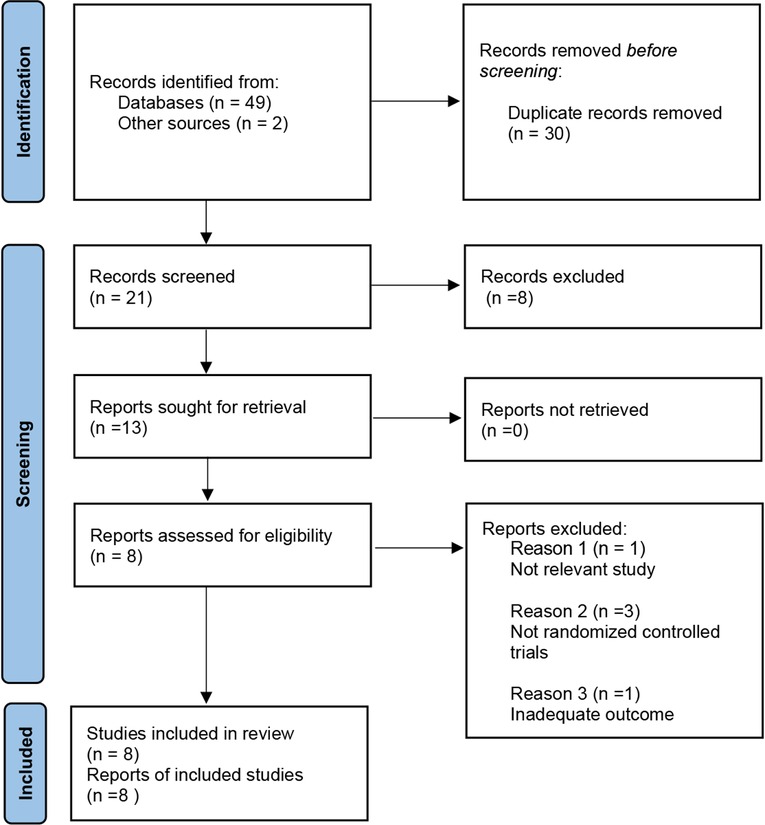
A total of 51 articles from PubMed, Embase, Cochrane Library, and reference lists were initially identified. 17 papers were found in PubMed, 11 were from Embase, 21 were found in Cochrane library, and 2 were from the reference lists. 30 articles were excluded because they were duplicates. By screening the titles and abstracts, 8 articles were excluded because they did not meet our indicated inclusion criteria for the literature. 5 of the remaining articles were excluded by analysis of the full text. Ultimately, 8 pieces were enrolled in this meta-analysis for qualitative and quantitative analyses (Figure 1).
3.2. Study characteristics
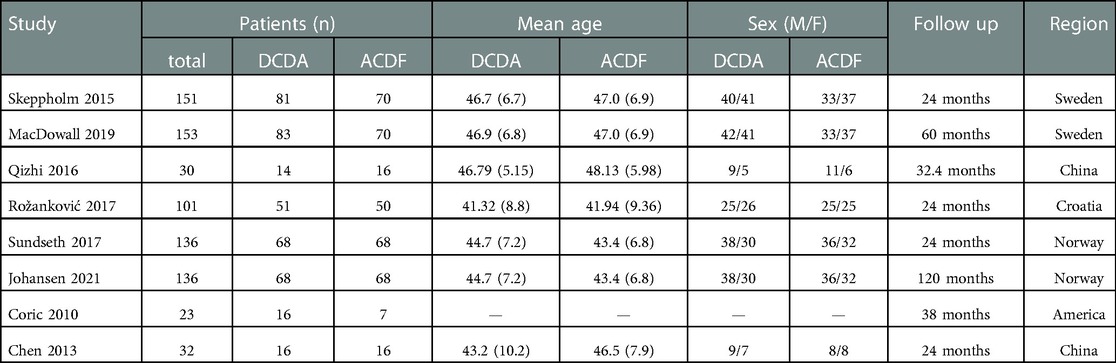
8 RCT studies (29–36) published between 2010 and 2021 were included in the present study. Except for the two data sets that differed in follow-up time, a total of 475 patients were involved in the 8 studies. The DCDA group was 227 patients, and the ACDF group was 248. Four of the included papers had a 2-year follow-up, two articles had a 5-year follow-up, and the remaining two articles had a mean follow-up of 32.4 and 38 months respectively. The characteristics of included studies are presented in Table 1.
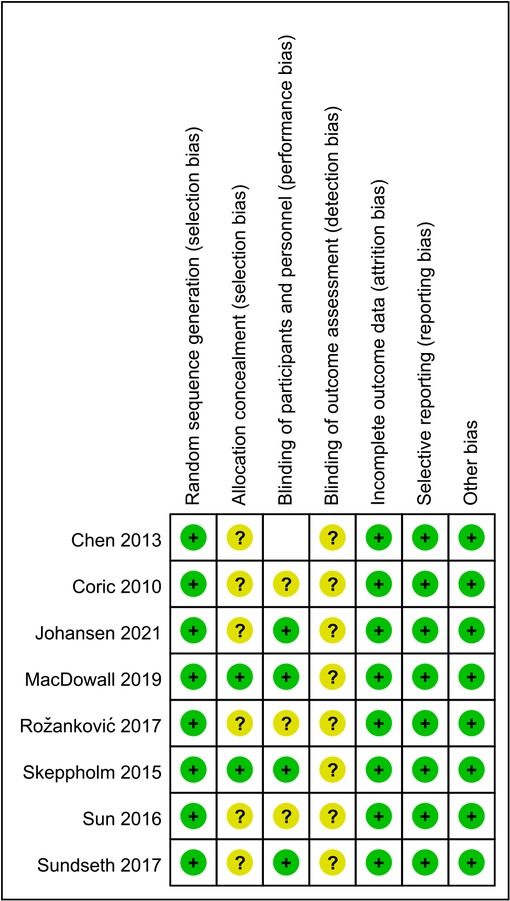
3.3. Risk of bias in included studies
Among the literature included in this study, eight articles had a low risk of bias for random sequence generation. 2 of the studies described allocation concealment. The remaining six articles do not provide a detailed description of whether allocation concealment was performed. Four studies described the blinding of participants and personnel. None of the included studies described blinding to outcome assessment (Figure 2).
3.4. Clinical indices
3.4.1. Neck disability index
A total of 7 articles compared the NDI scores of the DCDA and ACDF groups. Five of these articles (29, 31, 32, 35, 36) had a 2-year follow-up period, and the other two (30, 33) had a 5-year follow-up period. In comparing short-term outcomes, the NDI score was lower in the experimental group than in the control group, but the difference was not statistically significant. (SMD, −0.29; 95% CI: −0.96–0.38, P = 0.40). In comparing long-term outcomes, DCDA and ACDF also did not show statistically significant differences. (SMD, −0.01; 95% CI: −0.26–0.24, P = 0.96) (Figure 3).
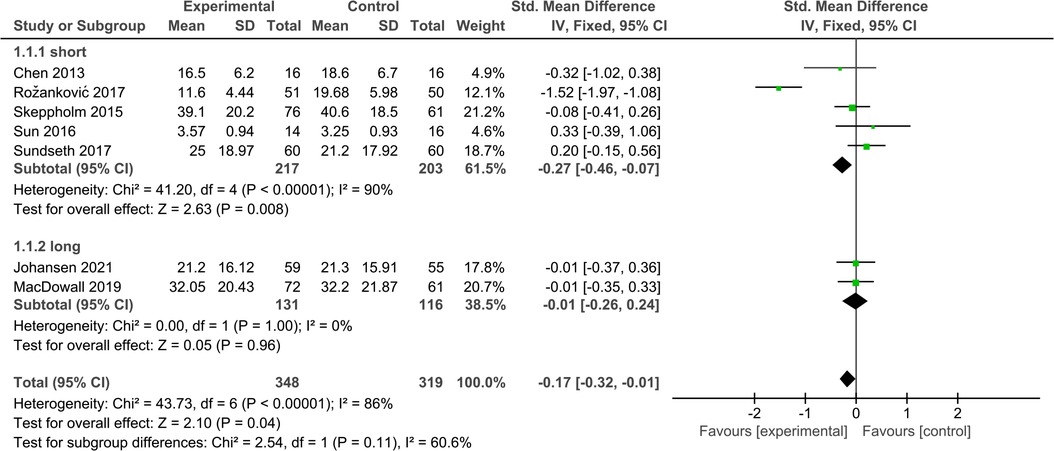
Figure 3. Comparison of NDI score between the discover cervical disc arthroplasty (DCDA, “experimental”) group and the anterior cervical discectomy and fusion (ACDF, “control”) group.
3.4.2. VAS NECK
Four studies (31, 32, 35, 36) reported mean neck pain VAS scores within the DCDA and ACDF groups, respectively. There was significant heterogeneity between the two groups (P < 0.00001, I2 = 89%). The results showed no statistically significant difference in neck pain VAS score between the two groups. (SMD, −0.26; 95% CI: −1.04–0.53, P = 0.53) (Figure 4).
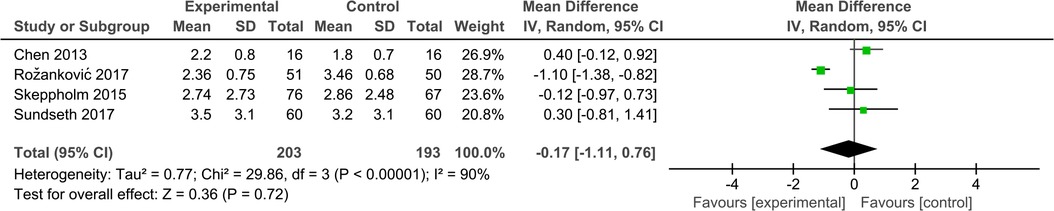
Figure 4. Comparison of VAS NECK score between the discover cervical disc arthroplasty (DCDA, “experimental”) group and the anterior cervical discectomy and fusion (ACDF, “control”) group.
3.4.3. VAS ARM
Three studies (31, 35, 36) contributed to the analysis of the arm pain VAS score. There was significant heterogeneity between the two groups (P < 0.00001, I2 = 93%). No significant difference was found when comparing the arm pain scores between the two groups (SMD, −0.20; 95% CI: −1.01–1.61, P = 0.63) (Figure 5).
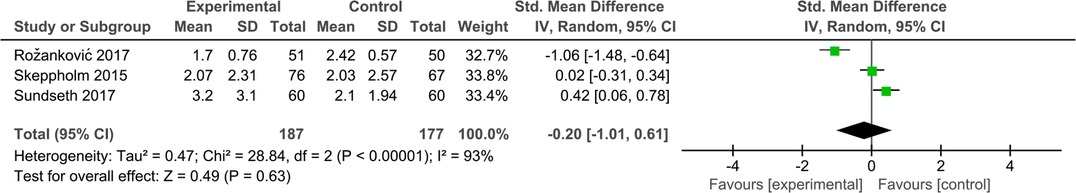
Figure 5. Comparison of VAS ARM score between the discover cervical disc arthroplasty (DCDA, “experimental”) group and the anterior cervical discectomy and fusion (ACDF, “control”) group.
3.4.4. EQ-5D
EQ-5D score was reported in four studies (30, 33, 35, 36). Two of these articles compare short-term results, while the other two compare long-term results. The pooled results indicated that the DCDA and ACDF groups were not showing statistical differences in either long-term or short-term outcomes. (short-term, SMD, −0.02; 95% CI: −0.26–0.22, P = 0.88 long-term SMD, −0.09; 95% CI: −0.49–0.30, P = 0.64) (Figure 6).
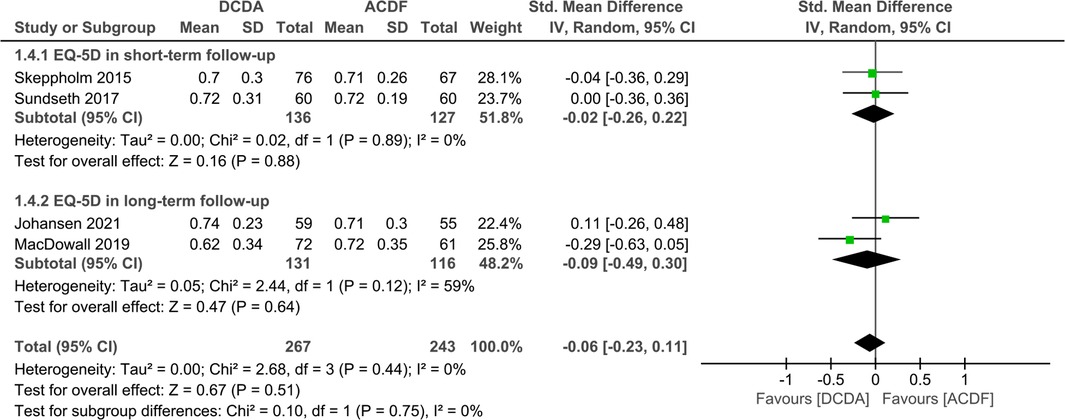
Figure 6. Comparison of EQ-5D score between the discover cervical disc arthroplasty (DCDA, “experimental”) group and the anterior cervical discectomy and fusion (ACDF, “control”) group.
3.5. Adverse events
3.5.1. Dysphagia
Three studies with 113 patients were included to assess the incidence of dysphagia. All patients had only short-term follow-up results. There were no significant difference in short-term follow-up between DCDA and ACDF (RR: 0.60, 95% CI: 0.29–1.25, P = 0.17). The results were consistent across the studies (I2 = 0%, P = 0.79) (Figure 7).
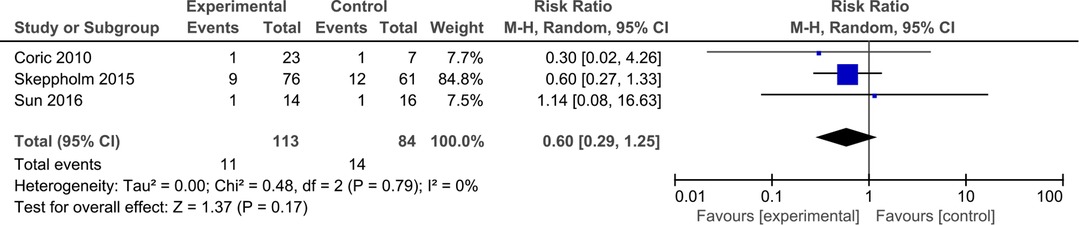
Figure 7. Comparison of dysphagia between the discover cervical disc arthroplasty (DCDA, “experimental”) group and the anterior cervical discectomy and fusion (ACDF, “control”) group.
3.5.2. Reoperation
Six studies reported reoperations at the final follow-up. There was no significant heterogeneity between the two groups (short-term P = 0.28; I2 = 22%; long-term P = 0.31; I2 = 3%). The results showed that the reoperation rate of the DCDA group was higher than the ACDF groups, with no statistical difference in short-term and long-term outcomes. In the comparison of total outcomes, the probability of secondary surgery was higher in DCDA, and this value was statistically significant. (total, RR = 1.65, 95% CI: 1.01–2.70, P = 0.05; short-term, RR = 1.99, 95% CI: 0.63–6.33, P = 0.24; long-term, RR = 1.53, 95% CI: 1.01–2.70, P = 0.43) (Figure 8).
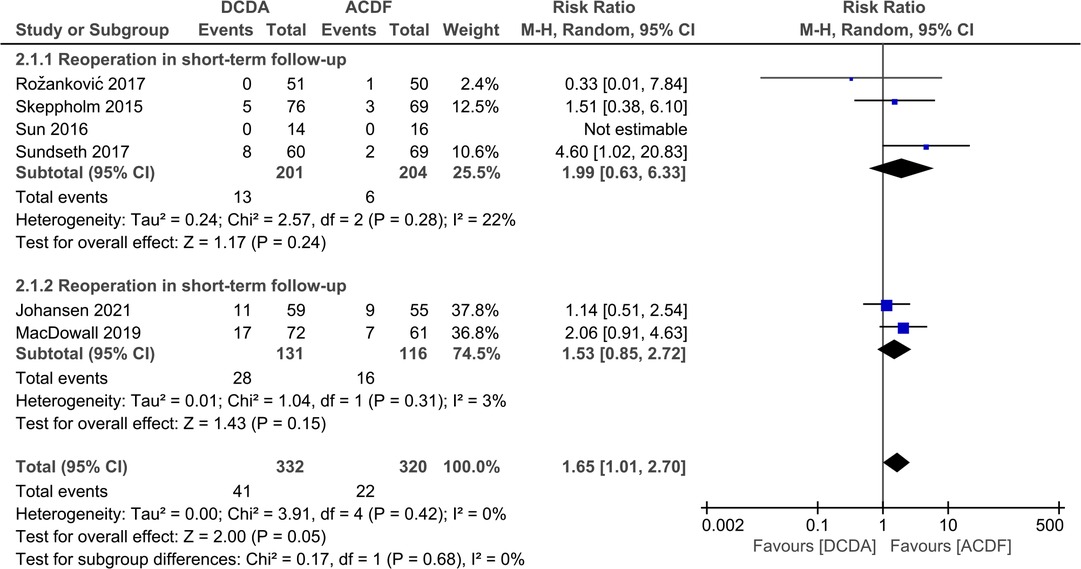
Figure 8. Comparison of reoperation between the discover cervical disc arthroplasty (DCDA, “experimental”) group and the anterior cervical discectomy and fusion (ACDF, “control”) group.
3.5.3. ASD
Four articles compared the incidence of ASD, and the follow-up period for these articles ranged from 24 to 120 months. Ultimately, the results revealed that the ASD rate of the DCDA group was lower than that of the ACDF group. (RR: 0.16, 95% CI: 0.03–0.88, P = 0.03) (Figure 9).
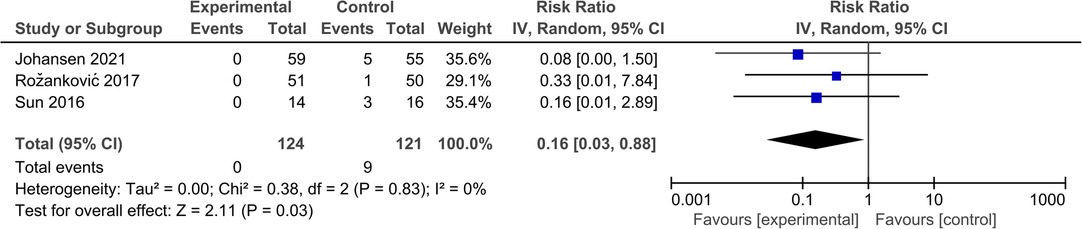
Figure 9. Comparison of ASD between the discover cervical disc arthroplasty (DCDA, “experimental”) group and the anterior cervical discectomy and fusion (ACDF, “control”) group.
3.6. Sensitivity analysis
Sensitivity analysis was conducted to determine whether the general trend would be significantly affected by deleting each study. Except for NDI and VAS ARM scores, no altered results were observed after each study was eliminated.
4. Discussion
Many meta-analyses have previously been performed comparing ACDF and CDA. Some studies (37–39) found that CDA was superior to ACDF in the comparison of NDI and EQ-5D scores and had better clinical efficacy. In addition, some other studies (40, 41) noted that the CDA and ACDF groups did not show a statistically significant difference in the incidence of ASD. However, all these studies regard CDA as a whole when comparing CDA and ACDF. In fact, CDA is a relatively broad concept, and the prostheses utilized in different studies are variable. Based on the article by Phillips et al. (42), artificial cervical discs can be classified by material into metal-on-metal, metal-on-polymer, ceramic-on-metal and ceramic-on-ceramic types. If classified according to biomechanics, the cervical prosthesis can also be further divided into three types — non-constrained,semi-constrained and constrained. Different types of prostheses have their own advantages, such as metal-to-metal types that produce less debris and metal-to-polymer prostheses that are better at simulating disc physiology and MR imaging. Coban et al. (28) have reported the differences in ASD between metal-on-metal and metal-on-polymer. In summary, comparing different prostheses with ACDF or between the various types of prostheses is reasonable. The clinical application of the Discover cervical artificial disc was first reported by Greiner–Perth et al. (43) in 2009. DISCOVER prosthesis is both a metal-on-polymer type and a non-constrained type of prosthesis, which may have advantages in terms of the incidence of heterotopic ossification and ASD. That is why we conducted a meta-analysis of eight RCTs to determine whether DCDA was superior to ACDF. The results suggest ACDF was superior to DCDA with a significantly lower incidence of secondary surgical procedures. However, the DCDA group had significantly better results in terms of the occurrence of ASD compared with the ACDF group.
The NDI is a very common and essential index used to evaluate the clinical efficacy of cervical spine surgery. Previous studies (38, 44) have found that CDA has a lower NDI score than ACDF. Meanwhile, other studies (29, 45) have also found no significant difference between DCDA and ACDF in the comparison of postoperative NDI. When applying the random effects model, the NDI between the two groups in this study did not show significant differences in both long- and short-term outcomes. In addition, the results showed a significant difference after removing the article by Rožanković et al. (31) The patients included in this article have (NDI) score of ≥30%, which was not described in the other enrolled articles. This may be the reason for the unstable results and the high heterogeneity of the index. And in the comparison of long-term outcomes, only two articles (30, 33) provided data for the 5-year follow-up period, so more high-quality long-term follow-up data need to be further investigated.
In previous articles (46, 47), the CDA and ACDF groups had similar effects in relieving arm and neck pain. Such results are also consistent with this meta-analysis. Kan et al. (48) indicated that the CDA group had lower VAS ARM and VAS NECK scores than the ACDF group. However, such differences may not have clinical significance, and patients may not be able to perceive subtle differences in scores. The results presented in this article are not robust due to the high heterogeneity. VAS focuses on the degree of pain, so patients with cervical spondylotic radiculopathy may have greater preoperative and postoperative differences. In addition, although the VAS scoring methods are all based on visual assessment, there are differences in the actual scoring details. And this difference is often not described in the articles. In the article by Skeppholm et al. (35), the VAS score is larger than the score of the standard scoring method. Therefore, we adjusted the VAS score of this article according to the standard score. All of the above reasons will have an impact on the current results. Hence, with the initiation of additional high-quality studies with longer follow-up, the VAS scores should be studied more rigorously. In the EQ-5D scores, the two groups did not show significant differences. The EQ-5D is a standardized set of scales that measure health status. The scale assesses a person's state of health through three levels on five dimensions. However, because of the small number of levels delineated, the scale is less sensitive to changes in small and medium health levels. Therefore, the application of the more accurate EQ-5D-5l scale in subsequent studies may be able to demonstrate more accurately whether there are differences between the two groups.
In the comparison of adverse events, Yao et al. (49) and Jiang et al. (50) found no significant difference in dysphagia incidence between the two groups. However, the study by McAfee et al. (51) showed that CDA was superior to ACDF in terms of dysphagia because CDA does not require strict retraction of the esophagus past the midline during the surgery procedure. Moreover, the occurrence of dysphagia is also influenced by other factors. Topical or intravenous steroid administration may also impact dysphagia rates (52). Hence, research on this issue still needs to limit more confounding factors to more accurately explore the advantages and disadvantages of DCDA and ACDF. Besides, the DCDA group showed more secondary procedures in this study. Such a result is not consistent with some previous studies. Many studies (53–55) have shown that the secondary surgical procedure for CDA is less than ACDF. Degeneration of the adjacent segment, implant events and persisting radiculopathy can all lead to reoperation.(53) Further refinement of the cause analysis may be more helpful in understanding the actual situation. In addition, this study found that the rate of ASD in the DCDA group was lower than that in the ACDF group. There are many relevant studies supporting such results. For example, a biomechanical study by Eck et al. (17) found that CDA may have less impact on adjacent segments. This biomechanical variation is why CDA is less likely to cause ASD. Reducing the effects on adjacent segments is also one of the reasons why the CDA technique has been developed. The ASD data reported in this article are based on the last follow-up visit. Therefore, high-quality studies with more extended follow-up periods are needed to prove this view.
This meta-analysis has several limitations. First, the sample sizes of part of the included articles were small. Studies with a small sample size are more likely to overestimate clinical effects. Second, although the same procedure was performed on patients in both the experimental and control groups, differences in the surgeon's experience, the extent of the patient's pathology, and scoring instruments in different studies still led to high heterogeneity in some of the indicators. Finally, the research was based on the statistics from published studies. The publication bias was unavoidable because of the limitations of a comprehensive review. The above conclusions may be not applicable to all patients.
5. Conclusion
This study shows that DCDA and CDA have similar results in terms of NDI scores, VAS scores, and EQ-5D scores. Also, they did not show significant differences in dysphagia. However, DCDA had a higher incidence of reoperation and fewer ASD than CDA. More high-quality studies are needed to provide more reliable data to compare the two treatments.
Author contributions
Conceptualization: ZW. Data curation: ZW, GL. Formal analysis: ZW, GL, HY. Funding acquisition: TS. Investigation: ZW, GL, HY. Methodology: ZW, GL. Project administration: ZW, GL, HY. Supervision: HZ, TL, HY. Validation: HZ, TL, HY. Visualization: ZW. Writing – original draft: ZW, TS. Writing –review & editing: ZW, TS. All authors contributed to the article and approved the submitted version.
Funding
Funded by Tianjin Key Medical Discipline (Specialty) Construction Project (grant no. TJYXZDXK-064B).
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. (2015) 36(4):811–6. doi: 10.3174/ajnr.A4173
2. Teraguchi M, Yoshimura N, Hashizume H, Muraki S, Yamada H, Minamide A, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama spine study. Osteoarthr Cartil. (2014) 22(1):104–10. doi: 10.1016/j.joca.2013.10.019
3. Voorhies RM. Cervical spondylosis: recognition, differential diagnosis, and management. Ochsner J. (2001) 3(2):78–84.21765723
4. Kobayashi K, Ando K, Nishida Y, Ishiguro N, Imagama S. Epidemiological trends in spine surgery over 10 years in a multicenter database. Eur Spine J. (2018) 27(8):1698–703. doi: 10.1007/s00586-018-5513-4
5. Binder AI. Cervical spondylosis and neck pain. Br Med J. (2007) 334(7592):527–31. doi: 10.1136/bmj.39127.608299.80
6. Kjaer P, Kongsted A, Hartvigsen J, Isenberg-Jørgensen A, Schiøttz-Christensen B, Søborg B, et al. National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy. Eur Spine J. (2017) 26(9):2242–57. doi: 10.1007/s00586-017-5121-8
7. Fehlings MG, Tetreault LA, Riew KD, Middleton JW, Aarabi B, Arnold PM, et al. A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Global Spine J. (2017) 7(3 Suppl):70S–83S. doi: 10.1177/2192568217701914
8. Lied B, Roenning PA, Sundseth J, Helseth E. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). BMC Surg. (2010) 10:10. doi: 10.1186/1471-2482-10-10
9. Eastlack RK, Garfin SR, Brown CR, Meyer SC. Osteocel plus cellular allograft in anterior cervical discectomy and fusion: evaluation of clinical and radiographic outcomes from a prospective multicenter study. Spine (Phila Pa 1976). (2014) 39(22):E1331–7. doi: 10.1097/BRS.0000000000000557
10. Fehlings MG, Barry S, Kopjar B, Yoon ST, Arnold P, Massicotte EM, et al. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine (Phila Pa 1976). (2013) 38(26):2247–52. doi: 10.1097/BRS.0000000000000047
11. Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. (2004) 17(2):79–85. doi: 10.1097/00024720-200404000-00001
12. Emery SE, Bohlman HH, Bolesta MJ, Jones PK. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am. (1998) 80(7):941–51. doi: 10.2106/00004623-199807000-00002
13. Bertalanffy H, Eggert HR. Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir. (1989) 99(1-2):41–50. doi: 10.1007/BF01407775
14. Fielding JW. Complications of anterior cervical disk removal and fusion. Clin Orthop Relat Res. (1992) 284:10–3. doi: 10.1097/00003086-199211000-00003
15. Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine (Phila Pa 1976). (1982) 7(6):536–9. doi: 10.1097/00007632-198211000-00004
16. Hwang SH, Kayanja M, Milks RA, Benzel EC. Biomechanical comparison of adjacent segmental motion after ventral cervical fixation with varying angles of lordosis. Spine J. (2007) 7(2):216–21. doi: 10.1016/j.spinee.2006.05.018
17. Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976). (2002) 27(22):2431–4. doi: 10.1097/00007632-200211150-00003
18. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. (1999) 81(4):519–28. doi: 10.2106/00004623-199904000-00009
19. Goffin J, Van Calenbergh F, van Loon J, Casey A, Kehr P, Liebig K, et al. Intermediate follow-up after treatment of degenerative disc disease with the Bryan cervical disc prosthesis: single-level and bi-level. Spine (Phila Pa 1976). (2003) 28(24):2673–8. doi: 10.1097/01.BRS.0000099392.90849.AA
20. Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, et al. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976). (2009) 34(2):101–7. doi: 10.1097/BRS.0b013e31818ee263
21. Leung C, Casey AT, Goffin J, Kehr P, Liebig K, Lind B, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery. (2005) 57(4):759–63; discussion 759–763. doi: 10.1093/neurosurgery/57.4.759
22. Pickett GE, Sekhon LHS, Sears WR, Duggal N. Complications with cervical arthroplasty. J Neurosurg Spine. (2006) 4(2):98–105. doi: 10.3171/spi.2006.4.2.98
23. Grasso G. Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J. (2015) 24(Suppl 7):842–8. doi: 10.1007/s00586-015-4281-7
24. Sasso RC, Anderson PA, Riew KD, Heller JG. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. Orthopedics. (2011) 34(11):889. doi: 10.3928/01477447-20110922-24
25. Peng Z, Hong Y, Meng Y, Liu H. A meta-analysis comparing the short- and mid- to long-term outcomes of artificial cervical disc replacement (ACDR) with anterior cervical discectomy and fusion (ACDF) for the treatment of cervical degenerative disc disease. Int Orthop. (2022) 46(7):1609–25. doi: 10.1007/s00264-022-05318-z
26. Wahood W, Yolcu YU, Kerezoudis P, Goyal A, Alvi MA, Freedman BA, et al. Artificial discs in cervical disc replacement: a meta-analysis for comparison of long-term outcomes. World Neurosurg. (2020) 134:598–613.e5. doi: 10.1016/j.wneu.2019.10.032
27. Badhiwala JH, Platt A, Witiw CD, Traynelis VC. Cervical disc arthroplasty versus anterior cervical discectomy and fusion: a meta-analysis of rates of adjacent-level surgery to 7-year follow-up. J Spine Surg. (2020) 6(1):217–32. doi: 10.21037/jss.2019.12.09
28. Coban D, Pompliano M, Changoor S, Dunn C, Sinha K, Hwang KS, et al. Metal-on-metal versus metal-on-plastic artificial discs in two-level anterior cervical disc replacement: a meta-analysis with follow-up of 5 years or more. Spine J. (2021) 21(11):1830–8. doi: 10.1016/j.spinee.2021.04.018
29. Qizhi S, Lei S, Peijia L, Hanping Z, Hongwei H, Junsheng C, et al. A comparison of zero-profile devices and artificial cervical disks in patients with 2 noncontiguous levels of cervical spondylosis. Clin Spine Surg. (2016) 29(2):E61–6. doi: 10.1097/BSD.0000000000000096
30. MacDowall A, Canto Moreira N, Marques C, Skeppholm M, Lindhagen L, Robinson Y, et al. Artificial disc replacement versus fusion in patients with cervical degenerative disc disease and radiculopathy: a randomized controlled trial with 5-year outcomes. J Neurosurg Spine. (2019) 30(3):323–31. doi: 10.3171/2018.9.SPINE18659
31. Marjan R, Mihailovič MS, Miroslav V. Cervical disc replacement with discover versus fusion in a single level cervical disc disease: a prospective single center randomized trial with a minimum two-year follow – up.:30.
32. Chen Y, Wang X, Lu X, Yang H, Chen D. Cervical disk arthroplasty versus ACDF for preoperative reducible Kyphosis. Orthopedics. (2013) 36(7):8. doi: 10.3928/01477447-20130624-29
33. Johansen TO, Sundseth J, Fredriksli OA, Andresen H, Zwart JA, Kolstad F, et al. Effect of arthroplasty vs fusion for patients with cervical radiculopathy: a randomized clinical trial. JAMA Netw Open. (2021) 4(8):e2119606. doi: 10.1001/jamanetworkopen.2021.19606
34. Coric D, Boltes MO. Prospective study of cervical arthroplasty in 98 patients involved in 1 of 3 separate investigational device exemption studies from a single investigational site with a minimum 2-year follow-up. J Neurosurg. (2010) 13(6):715–21. doi: 10.3171/2010.5.SPINE09852
35. Skeppholm M, Lindgren L, Henriques T, Vavruch L, Löfgren H, Olerud C. The discover artificial disc replacement versus fusion in cervical radiculopathy—a randomized controlled outcome trial with 2-year follow-up. Spine J. (2015) 15(6):1284–94. doi: 10.1016/j.spinee.2015.02.039
36. Sundseth J, Fredriksli OA, Kolstad F, Johnsen LG, Pripp AH, Andresen H, et al. The Norwegian Cervical Arthroplasty Trial (NORCAT): 2-year clinical outcome after single-level cervical arthroplasty versus fusion—a prospective, single-blinded, randomized, controlled multicenter study. Eur Spine J. (2017) 26(4):1225–35. doi: 10.1007/s00586-016-4922-5
37. Toci GR, Canseco JA, Patel PD, Divi SN, Goz V, Shenoy K, et al. The incidence of adjacent segment pathology after cervical disc arthroplasty compared with anterior cervical discectomy and fusion: a systematic review and meta-analysis of randomized clinical trials. World Neurosurg. (2022) 160:e537–48. doi: 10.1016/j.wneu.2022.01.072
38. Byvaltsev VA, Stepanov IA, Riew DK. Mid-term to long-term outcomes after total cervical disk arthroplasty compared with anterior diskectomy and fusion: a systematic review and meta-analysis of randomized controlled trials. Clin Spine Surg. (2020) 33(5):192–200. doi: 10.1097/BSD.0000000000000929
39. Zhang Y, Lv N, He F, Pi B, Liu H, Chen AC, et al. Comparison of cervical disc arthroplasty and anterior cervical discectomy and fusion for the treatment of cervical disc degenerative diseases on the basis of more than 60 months of follow-up: a systematic review and meta-analysis. BMC Neurol. (2020) 20(1):143. doi: 10.1186/s12883-020-01717-0
40. Dong L, Wang D, Chen X, Liu T, Xu Z, Tan M, et al. A comprehensive meta-analysis of the adjacent segment parameters in cervical disk arthroplasty versus anterior cervical discectomy and fusion. Clin Spine Surg. (2018) 31(4):162–73. doi: 10.1097/BSD.0000000000000552
41. Dong L, Xu Z, Chen X, Wang D, Li D, Liu T, et al. The change of adjacent segment after cervical disc arthroplasty compared with anterior cervical discectomy and fusion: a meta-analysis of randomized controlled trials. Spine J. (2017) 17(10):1549–58. doi: 10.1016/j.spinee.2017.06.010
43. Greiner-Perth R, Allam Y, Silbermann J, Simank HG. First experience and preliminary clinical results with the cervical disc replacement DISCOVER. Z Orthop Unfall. (2009) 147(5):582–7. doi: 10.1055/s-0029-1185897
44. Zhang Y, Liang C, Tao Y, Zhou X, Li H, Li F, et al. Cervical total disc replacement is superior to anterior cervical decompression and fusion: a meta-analysis of prospective randomized controlled trials. PLoS One. (2015) 10(3):e0117826. doi: 10.1371/journal.pone.0117826
45. Qian Y, Xue F, Sheng X, Lu J, Chen B. Early effectiveness of discover cervical artificial disc replacement in treatment of cervical spondylosis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. (2012) 26(3):277–83.22506461
46. Chang HK, Huang WC, Tu TH, Fay LY, Kuo CH, Chang CC, et al. Radiological and clinical outcomes of 3-level cervical disc arthroplasty. J Neurosurg Spine. (2019) 32(2):174–81. doi: 10.3171/2019.8.SPINE19545
47. Lavelle WF, Riew KD, Levi AD, Florman JE. Ten-year outcomes of cervical disc replacement with the BRYAN cervical disc: results from a prospective, randomized, controlled clinical trial. Spine (Phila Pa 1976). (2019) 44(9):601–8. doi: 10.1097/BRS.0000000000002907
48. Kan SL, Yuan ZF, Ning GZ, Liu FF, Sun JC, Feng SQ. Cervical disc arthroplasty for symptomatic cervical disc disease: traditional and Bayesian meta-analysis with trial sequential analysis. Int J Surg. (2016) 35:111–9. doi: 10.1016/j.ijsu.2016.09.088
49. Yao Q, Liang F, Xia Y, Jia C. A meta-analysis comparing total disc arthroplasty with anterior cervical discectomy and fusion for the treatment of cervical degenerative diseases. Arch Orthop Trauma Surg. (2016) 136(3):297–304. doi: 10.1007/s00402-015-2337-0
50. Jiang H, Zhu Z, Qiu Y, Qian B, Qiu X, Ji M. Cervical disc arthroplasty versus fusion for single-level symptomatic cervical disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg. (2012) 132(2):141–51. doi: 10.1007/s00402-011-1401-7
51. McAfee PC, Cappuccino A, Cunningham BW, Devine JG, Phillips FM, Regan JJ, et al. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech. (2010) 23(1):1–8. doi: 10.1097/BSD.0b013e31819e2ab8
52. Zhong ZM, Li M, Han ZM, Zeng JH, Zhu SY, Wu Q, et al. Does cervical disc arthroplasty have a lower incidence of dysphagia than anterior cervical discectomy and fusion? A meta-analysis. Clin Neurol Neurosurg. (2016) 146:45–51. doi: 10.1016/j.clineuro.2016.04.002
53. Turkov D, Job A, Iturriaga C, Verma RB. Current concepts of cervical disc arthroplasty. Int J Spine Surg. (2021) 15(6):1174–83. doi: 10.14444/8149
54. Núñez JH, Escudero B, Omiste I, Martínez-Peñas J, Surroca M, Alonzo-González F, et al. Outcomes of cervical arthroplasty versus anterior cervical arthrodesis: a systematic review and meta-analysis of randomized clinical trials with a minimum follow-up of 7-year. Eur J Orthop Surg Traumatol. (2022) 20. doi: 10.1007/s00590-022-03365-1. [Epub ahead of print]
Keywords: anterior cervical discectomy and fusion, discover cervical disc arthroplasty, meta-analysis, randomized controlled trial, degenerative disc diseases
Citation: Wang Z, Luo G, Yu H, Zhao H, Li T, Yang H and Sun T (2023) Comparison of discover cervical disc arthroplasty and anterior cervical discectomy and fusion for the treatment of cervical degenerative disc diseases: A meta-analysis of prospective, randomized controlled trials. Front. Surg. 10:1124423. doi: 10.3389/fsurg.2023.1124423
Received: 15 December 2022; Accepted: 1 February 2023;
Published: 21 February 2023.
Edited by:
Tingkui Wu, Sichuan University, ChinaReviewed by:
Osvaldo Mazza, Bambino Gesù Children’s Hospital (IRCCS), ItalyMark Lambrechts, Rothman Institute, United States
© 2023 Wang, Luo, Yu, Zhao, Li, Yang and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tianwei Sun MTI5MDY4NDAwMUBxcS5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Abbreviations ACDF, anterior cervical discectomy and fusion; ASD, adjacent segment degeneration; CDA, cervical disc arthroplasty; CDDD, cervical degenerative disc diseases; DCDA, discover cervical disc arthroplasty; NDI, neck disability index; VAS, visual analogue scale
 Ziqi Wang
Ziqi Wang Gan Luo2
Gan Luo2 Hongwei Yu
Hongwei Yu Tianwei Sun
Tianwei Sun