Explore article hub
A Viewpoint on the Frontiers in Science Lead Article
The future of evolutionary medicine: sparking innovation in biomedicine and public health
The concept of evolutionary medicine was created about 40 years ago at the University of Michigan’s Museum of Zoology when the psychiatrist Randy Nesse walked into the office of Bill Hamilton with a new theory about senescence that was quite wrong. The field thus had a precarious early childhood but was soon guided into strapping adolescence by two works: the 1991 treatise ‘Dawn of Darwinian Medicine’ by George Williams and Nesse and the 1993 book ‘Evolution of Infectious Disease’ by Paul Ewald. A string of landmark successes followed: a brilliant monograph on ‘Why We Get Sick’ by Nesse and Williams, an international society, a thriving Oxford journal, a ‘Club EvMed’ seminar series led by Charlie Nunn, and a dedicated textbook co-authored by Steve Stearns. It was a paradigm of cross-disciplinary insights, with Randy Nesse tirelessly rallying the troops and Darwin himself taking point. What could possibly go amiss?
I was drawn to evolutionary medicine by my interest in human social behavior, sparked by Bill Hamilton and Dick Alexander, which led me to the realization that autism was a disorder of evolved, adaptive human sociality, but was studied virtually bereft of evolutionary theory. I found that, amazingly, one could study both evolution and human disease in one fell swoop, with hopes to both help alleviate human suffering and attempts to make a name for oneself in the pantheons of biology. This unique quality of evolutionary medicine has, I think, drawn many creative researchers to the field; among them are the authors of Natterson-Horowitz et al., 2023 (1). One of the field’s brightest stars, David Haig, developed a novel theory for genomic conflicts in the 1990s that has had direct and immediate implications for the major disorders of human pregnancy (2)—or so he and I thought at the time. The theory was well supported by diverse data but neglected, misunderstood, or disbelieved by most of the geneticists and molecular biologists who studied the genes involved. It was also virtually ignored by the physicians and medical researchers who studied pre-eclampsia, gestational diabetes, and the other disorders of pregnancy—those who could obviously help patients using Haig’s insights. What had gone wrong?
I write this not just to praise evolutionary medicine but also to help save it from potentially grievous futures. The field and its adherents have performed brilliantly where its subject is inherently evolutionary: the adaptation of infectious diseases to antibiotics (and other human defenses) in real time, the evolution of cancer in the body, and the use of phylogenies or phages to understand and fight pathogens. Here, though, one can easily see the variation, the natural selection, and the evolutionary change that drive the disease risks and processes. For other fields ostensibly in the purview of evolutionary medicine, among which are gynecology, cardiology, physiology, dentistry, neurology, immunology, emergency medicine, life history, and most of psychiatry, all that we have are hypotheses, theory, and a few tentative, toe-in-the-lake applications to show for our Darwinian labors. Why?
Perhaps it is a matter of time. After all, it took decades, and many thousands of maternal deaths, for the insight of the Hungarian doctor Ignaz Semmelweis—that handwashing by physicians could prevent lethal ‘childbirth fever’—to enter the mainstream. Medical practice is inherently conservative: the motto of medicine is primum non nocere (“first do no harm”), and this is nowadays often reinforced by malpractice suits and lawyers.
But the causes may be deeper and more complex. The greatest strength of evolutionary medicine, its relentless interdisciplinarity, appears also to be its greatest vulnerability. Imagine a landscape and a path from evolutionary theory to clinical applications (Figure 1). The pathway is riven by three great divides : (1) between theory and empirical evidence from academics, (2) between academia (as a whole) and the domains of medicine (as a whole), and (3) between academic and medical researchers and the clinicians who actually see patients and conduct trials of therapies. The divides must be traversed, from computers to clinics, for evolutionary medicine to have a material impact on human health. At present, the main bridges in place comprise a widespread but unsystematic network of undergraduate and graduate courses in evolutionary medicine, and perhaps a few hours of instruction for exhausted medical students, where most have little to none of the background needed to appreciate it. I have written papers for the flagship journal in the field, Evolution, Medicine, and Public Health, thinking that they would instigate a revolution in thinking about a disease, with direct implications for research and therapy. Such hopeful yet hopeless naïveté highlights a focus on just what the impediments are to the successful crossing of the great divides from academic theory to clinical application and how they might be overcome.
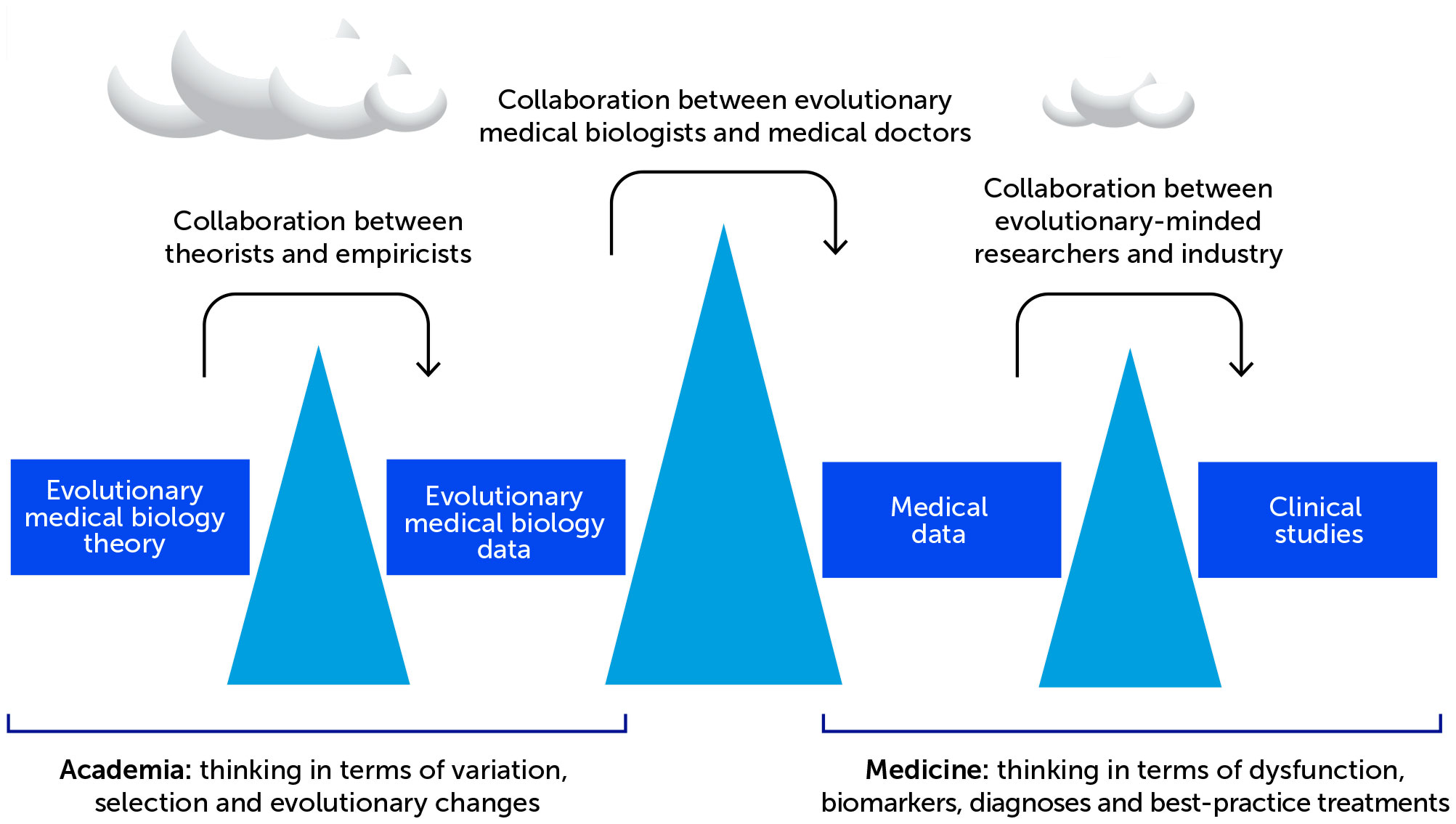
Figure 1 The great divides separating evolutionary medicine from ‘conventional’ medicine. Evolutionary medicine is separated from ‘conventional’ medicine by three great divides created by diversity and specialization in training, differences in ways of thinking and collaborating, and political-economic exigencies. Surmounting the divides is crucial for evolutionary medicine to provide the practical health benefits that can follow naturally from its promise.
The first divide, from theory to data within evolutionary biology, should be the easiest to traverse. After all, a primary strength of evolutionary medicine is that it tells us what new data to collect to address key questions that may have hitherto been unrecognized as such. But most theoreticians, and mathematicians (with some important exceptions), neither collaborate with empiricists nor present their work with an eye to specifying the critical tests motivated by their formal insights. Evolutionary processes are inherently mathematical, but many, or most, data-collecting evolutionary biologists are not. The only obvious answer here is fostering of collaborations between theorists and empiricists in evolutionary medicine—or at least insistence, by reviewers, editors, and grants panels, that data always connect to theory and that theorists always describe ways and means of putting their equations to use. The detail, depth, and complexity of both theory and medical questions make crossing this divide especially challenging.
The second divide, from academic training, institutions, and domains to medical ones, is by far the greatest of the three. Evolutionary biologists and doctors have both been trained in biology, but they think and act on their information entirely differently. How?
Card-carrying evolutionary-medical biologists think in terms of variation at the levels of genes, haplotypes, phenotypes, healthy individuals, patients, populations, species, and phylogenies. They think about natural selection, tradeoffs, extremes, the body’s own evolved defenses, coevolution, environments, and mismatches impacting upon the variation, often leading to disease. They develop hypotheses that they test themselves using data from the literature or lab.
By stark contrast, medical researchers and clinicians think in terms of dysfunctions, biomarkers, proximate mechanisms, categorical diagnoses, and standardized ‘best-practice’ treatments. They tend to be data-driven because hypotheses may be flawed or incorrect, and they are at their best admitting the anathema of uncertainty. Data collection, in turn, is often driven by recent advances in technology (e.g., single-cell genomics or whole suites of -omics in concert) rather than ideas because grants panels and reviewers require it. The outcome is commonly a massive stand of trees (much data) but no forest (little to no meaning) and no real hypothesis that has been rejected or offered support.
There is no philosophical, political, or practical necessity for this greatest of divides—this isolation of evolutionary medicine from medical sciences. I once spent over an hour of intense conversation with a brilliant young medical neuroscientist trying to explain the concept of a tradeoff that could explicate one of their key findings. It was astonishing to see the light bulb turn on when they ‘got’ the idea. Bridging this divide is just a matter of openness to new ideas and, for evolutionary biologists, the extremely hard work required to learn enough about cancer (or endometriosis or microbiomes) to hold one’s own with a medical specialist or in a medical journal article. Ultimately, a robust crossing will probably come most directly from collaborations between M.D.s and Ph.D.s where the two cultures can find common purpose and synergy (e.g. 3). But such collaboration is, so far, so rare that its absence is hardly noticed. Indeed, the only well-flagged trail connecting this divide is in the field of cancer biology, where evolutionary research findings are directly helping physicians and patients and where discoveries regarding cancer evolution are also feeding back to provide novel insights concerning evolutionary processes themselves.
The third divide, the separation of medical researchers (and the academic domain) from the world of clinical trials and drug companies, has been generated by economics, politics, and society more broadly. This divide thus differs qualitatively from the others, and its consideration raises dire questions about the consequences of turning human health into a profit-driven business. But opportunities are raised as well: can evolutionary-minded researchers infiltrate big pharma with its big budgets to help steer evolutionary insights and approaches towards their clinical applications? There are certainly reasons to think that therapies derived from evolutionary paradigms should be more effective, and thus more profitable, than those derived from non-evolutionary medicine, whatever that may be. And as evidenced by the health crises due to antibiotic resistance, metabolic syndrome, and emerging and resurging infectious diseases, big pharma needs all the help it can get whatever its political-economic bent.
I used to think that the future of evolutionary medicine was unconditionally bright. Now, however, for me (as for the immortal Yogi Berra), ‘the future ain’t what it used to be.’ An ideal future would involve evolutionary thinking becoming so fully and deeply integrated into medicine that the field would, as a discrete discipline, simply disappear by assimilation. Evolutionary medicine could, however, also fade away for the worst of reasons: because its core group of first-generation researchers and champions passes into history without enough leaders to take their places by sustaining its identity and purpose. It is perhaps most likely, for the foreseeable future, that the field will, through reviews like the one published here, continue to inspire many of the next generation of researchers who want to combine their love of evolution with devotion to the betterment of human well-being. In this way, evolutionary medicine can hopefully, through the crossing of these divides, enjoy a long lifespan, and an expanding pedigree, from which we all gain in fitness and health.
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Acknowledgments
I thank the editors of Frontiers in Science for inviting me to write this article and Henry Heng for helpful comments.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Natterson-Horowitz B, Aktipis A, Fox M, Gluckman PD, Low FM, Mace R, et al. The future of evolutionary medicine: Sparking transformation in biomedical innovation and public health. Front Sci (2023) 1:997136. doi: 10.3389/fsci.2023.997136
2. Haig D. Genetic conflicts in human pregnancy. Quart Rev Biol (1993) 68:495–532. doi: doi: 10.1086/418300
Keywords: evolutionary medicine, infectious disease, cancer, natural selection, medicine
Citation: Crespi BJ. The possible futures of evolutionary medicine. Front Sci (2023) 1:1124128. doi: 10.3389/fsci.2023.1124128
Received: 14 December 2022; Accepted: 26 January 2023;
Published: 28 February 2023.
Edited and Reviewed by:
Henry H. Heng, Wayne State University, United StatesCopyright © 2023 Crespi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bernard J. Crespi, Y3Jlc3BpQHNmdS5jYQ==
 Bernard J. Crespi
Bernard J. Crespi