Explore article hub
- 1ISEM, Université de Montpellier, CNRS, IRD, EPHE, Montpellier, France
- 2Santa Fe Institute, Santa Fe, NM, United States
A Viewpoint on the Frontiers in Science Lead Article
The future of evolutionary medicine: sparking innovation in biomedicine and public health
Introduction
Illness and disease are among the most preoccupying challenges facing humanity. The causes are many and varied, including frailty associated with lifespan extension, modern day living and lifestyle choices, and greater contact with wildlife and with each other. With ever fewer new antimicrobial and cancer drugs and inertia in the development and uptake of the spectrum of alternative medicines, future progress will require change in our perception of how science can better contribute to health.
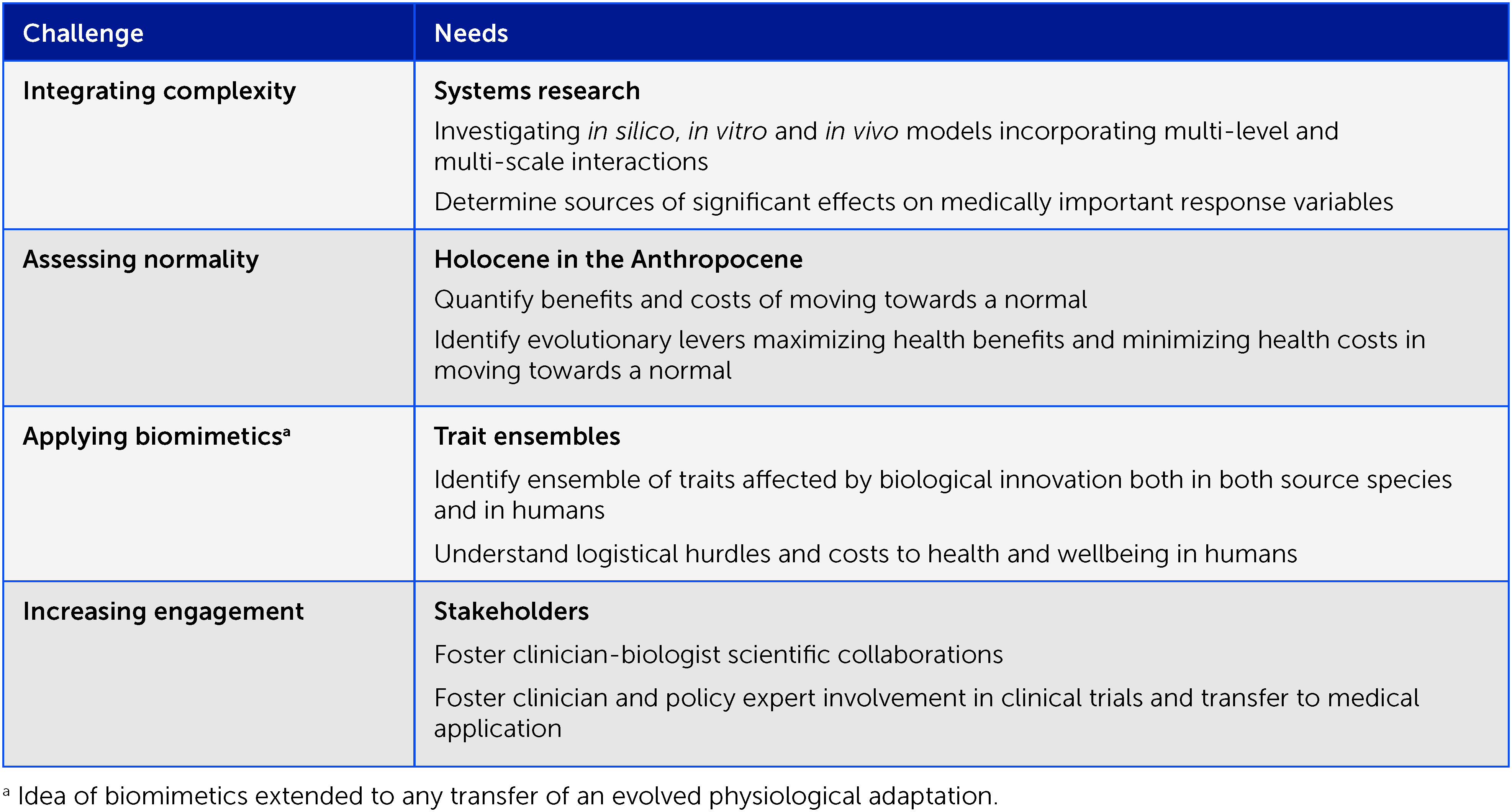
Natterson-Horowitz and colleagues (1) present the promise of evolutionary medicine to meet health challenges in the 21st century. Like all emerging fields, evolutionary medicine has its proponents and sceptics. While many evolutionary biologists are aware of evolutionary medicine, few would view their research as useful to it. In contrast and, arguably, more disconcertingly, too few clinicians and public health policymakers are sufficiently familiar with evolutionary medicine; of those who are, too few see it as a serious alternative to mainstream medicine. Correspondingly, evolutionary medicine’s successes have largely been in better public understanding of illness and disease, education of medical students, and experimental proof of evolutionary concepts. In terms of clinical trials and concrete application, evolutionary medicine is seeing its most impressive successes in targeted therapies against drug-resistant cancers and bacterial infections. Although these are important accomplishments, echoing Natterson-Horowitz and colleagues, I believe that evolutionary medicine’s future progress will depend on whether several challenges can be addressed (Box 1).
Challenges
Integrating complexity
Complexity science aims to elucidate responses of system components to one another and to whole system behaviors. Simple systems are characterized by small numbers of linear interactions. Complex systems have sufficient numbers of non-linear interactions to make the overall behavior difficult to predict without an understanding of the underlying structure of the interaction network. Homeostasis and organ system remediation following injury or disease are examples of how multiple systems interact to maintain or achieve normality (2).
Some of the greatest potentials of evolutionary medicine are in preventing or managing resistance in distinct therapeutic targets, such as bacterial pathogens or cancer cells. Complexity in these systems involves a number of interactions: the responses of cell variants to the impacts of drugs, cell-cell competition, interactions with non-target host cells, microbiota, and host organ systems such as the immune system; interactions with one or more drugs or replicating agents (e.g., bacteriophage); and therapeutic contingencies based on patient condition and monitored effects of the therapy (3). For example, the common belief that antibiotics alone are responsible for clearing bacterial infections is likely erroneous, since some degree of immune competence is necessary for remediating damaged tissue and contributing to (and possibly dominating) the elimination of the pathogen itself.
An outstanding question in evolutionary medicine is the extent to which complexity needs to be understood and incorporated into strategic medical decisions. This will surely differ on a case-by-case basis, since it is not intuitively clear whether, for example, there is more complexity linking lifestyle to type 2 diabetes and its treatment than linking hospital-acquired infection by Klebsiella pneumoniae (or a biofilm producing vs non-producing bacterium) to pneumonia and its treatment. There are potentially an enormous number of precursors, intermediaries, and contexts in each. Should we simplify systems and work from the bottom-up, or start with maximal complexity and work from the top-down, or take a more knowledge-based approach and add or subtract factors as justified? How do we account for lacuna in understanding of the environmental and contextual idiosyncrasies that may generate complications? Arguably, the choice of any treatment strategy comes down to the likelihood of success and options in cases of failure. The flexibility of evolutionary medicine to account for system complexity may prove to be superior to conventional therapies, particularly when treatment resistance is a factor.
Assessing normality
Evolutionary process provides an explanation as to why life systems tend toward optimum states. Environments change over different time scales, and populations tend to evolutionarily track those environmental components persisting long enough for a selective response and associated changes in phenotypic (e.g., life history) traits. A trait approaches the normal for a given environment as it increasingly matches the evolutionary optimum for that environment. This is unless that environment is evolutionarily novel, in which case the trait is mismatched, should the trait not have previously evolved the capacity of adaptive plasticity in response to novel environments. The Anthropocene has produced unprecedented physical and social environmental changes. Even if cultural evolution can reduce certain mismatches, modern lifestyles and altered habitats can push individual health away from evolved normal states, resulting in diverse health conditions, including increased risk of cancers, diabetes, and psychological disorders. An important question is the extent to which certain pathologies attributed to mismatches alone are in fact also associated with aging due to longer life spans, the latter being promoted by progress in hygiene and medicine.
A challenge to evolutionary medicine is discovering the extent to which nudging life systems and/or associated environments somewhere between states of the Anthropocene and Holocene will result in improved health and wellbeing, while accounting for the costs of nudging strategies. Physiological and behavioral traits are interwoven and, to some extent, individual-specific. It is not clear how guiding either or both toward norms associated with our hunter-gatherer ancestors affects the diverse facets of health and wellbeing. For example, although primary prevention such as never-smoking or balanced diets has undeniable benefits, reactive strategies such as periodic ceasing of tobacco use or repetitive crash-dieting could have psychological and/or physiological consequences. To the extent that certain present-day behaviors produce health problems, complex pathologies are best mitigated if the target behavior is prevented in the first place.
Applying biomimetics
Biomimetics holds the prospect of using the fruits of macro-evolution in the tree of life for the betterment of human health and wellbeing. Biomimetics has shown some success, but as much as capitalizing on what other species have achieved, the question remains whether extrapolating to humans is logistically feasible and whether application has underappreciated downstream negative effects. These concerns are based on the embedding of traits in a larger, coevolved, interactive life system, and the fact that the trait ensemble could be specific to the species in which it evolves.
The impacts of transfers of useful adaptations to humans are largely unknown (antibiotics in microbes being a very notable exception) and generally evaluated through experiments on murine models and clinical trials on human subjects. Concerns notwithstanding, there are justifications for adapting biological innovations such as very-high-molecular-mass hyaluronan for human use, given this molecule is involved in deterring tumor development and limiting physiological aging in the naked mole rat, Heterocephalus glaber. A reasonable (but unverified) hypothesis is that this innovation has coevolved with other traits to both incorporate the molecule’s positive effects and minimize any negative fitness effects in H. glaber. Even should use of this beneficial molecule have unintended negative effects in humans (e.g., possible detriment to embryonic development; V. Gorbunova, pers. comm.) – as for innovation transfers from other species – research should focus on whether and how this biological innovation could be adapted so that its medical benefits far outweigh any costs.
Increasing engagement
Medicine employs established, time-tested methods with the aim of positive outcomes at manageable risk. A consequence of this conservatism is inertia to change and, in particular, the uptake of controversial evolution-instructed approaches. Evolutionary medicine uptake is also slowed due to hesitancy by Big Pharma, challenges in executing clinical trials, and both doctor and patient reticence to apply unconventional medicine. A prime example of reticence is the idea that bacterial pathogens and cancers should sometimes be managed rather than cured and the use of replicating microbes, such as viruses, rather than drugs to this effect. As a consequence, evolution-informed targeted medicine has found much of its application in last resort (e.g., antibiotic-resistant) and compassionate cases.
To the extent that evolutionary medicine research has produced a wealth of knowledge and first steps toward application to improve health and wellbeing, its progress depends on funding by governments and industry, and the education and engagement of clinicians (especially physicians) and public health policymakers. Most physicians will have had no more than an undergraduate-level introduction to evolutionary biology and, as above, are not expected to deviate from the mantra of approved, time-tested prescription of drugs to eliminate signs and symptoms of disease. The challenge to achieving more inclusive medicine lies both with the medical education establishment and with commitment and implementation by doctors themselves in situations where evolutionary strategy and tactics are approved and present a viable alternative to conventional practices.
Ways forward
The evolutionary medicine community is aware of these and other challenges but, in my view, greater future emphasis is needed specifically in the following areas (see expanded list in Box 1).
Systems research
Evolutionary medicine needs more emphasis on complex systems thinking. Medicine is part of a larger ecosystem with many levels and scales, and both fundamental research and its application need to better account for the diversity of significant players, their interactions, and feedback affecting health and wellbeing. This is a daunting proposal since there are many potential influences, from molecules to organ systems, individual behaviors and disease-causing agents, to clinicians, medical options, and public health authorities. Method, such as starting with a few central, direct features/interactions and incrementally building up as necessary, is needed, as is distinguishing conserved system levers from unknowns and special circumstances. A greater understanding of the significant players, their interactions, and non-linear feedbacks (4) will contribute to both the effective application of evolutionary medicine and its uptake by clinicians and the public. Moreover, evolutionary medicine needs a better understanding of the strengths and limitations of comparisons at different scales, for example, between somatic evolution and species evolution and how control measures – cancer and pests, respectively – are optimized in each (e.g., https://cancerevolution.org).
Involvement
Evolutionary medicine needs more engagement from clinicians and policymakers. This can happen in several ways. The annual meeting of the International Society of Evolutionary Medicine and Public Health is a venue for both the latest research in evolutionary medicine and a valuable opportunity for discussions and possible projects involving evolutionary biologists and clinicians. Engagement is not limited to formal conferences; progress also results from evolutionary medicine courses, virtual seminars and discussion platforms (in particular ClubEvMed), and through the growth of collaborative research publications involving clinicians and biologists (5), such as the journal Evolutionary Medicine and Public Health. It is just a matter of time until these outlets and curricula given to medical students worldwide produce the next generation of physicians, more scientific collaboration and clinical trials, and a greater reach of evolutionary insights into medicine. Government agencies and industry will need to provide the financial resources for engagement, necessities, and opportunities to be realized.
Compendia
More than anything else, evolutionary medicine needs to understand why it works or fails. Existing assessments are sometimes limited by unintentional biases in reporting successes over failures, and by difficulties in accessing the huge variety of publishing venues and diverse terminology. Among the challenges are classifying like with like and applying statistics to disparate and often limited data, especially given the many possible caveats associated with individual interventions. Compendia should not only include the intentional application of ecological and evolutionary principles, such as in treating bacterial infections with combinations of antibiotics and bacteriophage, but also those that imply evolution, such as routine phage therapy as practiced in Georgia, Poland, and Russia. Finally, compendia are needed not only for direct, targeted medicine, such as treating microbial infections and cancers, but also for preventive medicine at a public health level, increasing lifestyle awareness of disease.
Conclusion
Enthusiasm for evolutionary medicine is amply warranted given the spectrum of its application and the possibilities of producing innovation in diverse medical applications. Nonetheless, this field is still young and facing challenges. Only scientific research and communication between biologists and clinicians can assess when evolutionary significance translates into medical significance and when it does not, and whether correlations and epidemiology supported (or not) by evolutionary insights are sufficient to make wise medical decisions and policy choices. In this regard, evolutionary medicine aimed at pathogenic microbes and cancer needs to realize its potential beyond special cases to the spectrum of resistance prevention and management situations. Despite its challenges, evolutionary medicine stands as the most promising science-based framework to confront growing health challenges in the 21st century.
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Funding
MEH acknowledges the Fondation ARC pour la recherche sur le cancer: Programmes labellisés 2021 (Project #ARCPGA12021010002850_3574) for funding.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Natterson-Horowitz B, Aktipis A, Fox M, Gluckman P, Low FM, Mace R, et al. The future of evolutionary medicine: sparking innovation in biomedicine and public health. Front Sci (2023) 1:997136. doi: 10.3389/fsci.2023.997136
2. Torres BY, Oliveira JHM, Tate AT, Rath P, Cumnock K, Schneider DS. Tracking resilience to infections by mapping disease space. PloS Biol (2016) 14:e1002436. doi: 10.1371/journal.pbio.1002436
3. Burmeister AR, Hansen E, Cunningham JJ, Rego EH, Turner PE, Weitz JS, et al. Fighting microbial pathogens by integrating host ecosystem interactions and evolution. BioEssays (2021) 43:e2000272. doi: 10.1002/bies.202000272
4. Roach DR, Leung CY, Henry M, Morello E, Singh D, Di Santo JP, et al. Synergy between the host immune system and bacteriophage is essential for successful phage therapy against an acute respiratory pathogen. Cell Host Microbe (2017) 22:38–47.e4. doi: 10.1016/j.chom.2017.06.018
Keywords: biomedicine, biomimetics, complexity, evolutionary medicine, mismatch, stakeholders, systems science, traits
Citation: Hochberg ME. Addressing challenges in evolutionary medicine: three priorities. Front Sci (2023) 1:1123806. doi: 10.3389/fsci.2023.1123806
Received: 14 December 2022; Accepted: 26 January 2023;
Published: 28 February 2023.
Edited and Reviewed by:
Henry H. Heng, Wayne State University, United StatesCopyright © 2023 Hochberg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael E. Hochberg, bWljaGFlbC5ob2NoYmVyZ0B1bW9udHBlbGxpZXIuZnI=
 Michael E. Hochberg
Michael E. Hochberg