
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol., 12 March 2025
Sec. Health Psychology
Volume 16 - 2025 | https://doi.org/10.3389/fpsyg.2025.1530311
This article is part of the Research TopicIntegrating Health Psychology in Practice: Enhancing Well-being and Improving Health Outcomes Across Diverse ContextsView all 12 articles
Objective: To explore effectiveness of non-pharmacological interventions in fear of childbirth.
Methods: All published literature were searched from three databases (Pubmed, Cochrane CENTRAL, and Web of Science) as of April 2024. The risk of bias of the included studies was assessed using the Cochrane Systematic Review Manual 2.0 bias risk assessment tool. The primary outcome was FOC, the secondary outcomes were depression, anxiety, stress, childbirth self-efficacy, and mode of delivery.
Results: This study included 32 randomized controlled trials, involving 17 interventions and 3,187 pregnant women. Compared with usual care, cognitive-behavioral therapy (SMD = −1.62, 95%CI –2.47 to −0.66), haptonomy (SMD = −1.43, 95%CI –2.63 to −0.24), motivational interview (SMD = −1.35, 95%CI –2.35 to −0.35), counseling therapy (SMD = −1.08, 95%CI –1.91 to −0.25) statistically and significantly improved fear of childbirth in gestational period. Emotional freedom technique (SMD = −3.13, 95%CI –5.00 to −1.26), counseling therapy (SMD = −1.81, 95%CI –2.97 to −0.80), haptonomy (SMD = −1.78, 95%CI –2.89 to −0.66), cognitive-behavioral therapy (SMD = −1.42, 95%CI –2.53 to −0.32), motivational interview (SMD = −1.28, 95%CI –2.37 to −0.19) statistically and significantly improved fear of childbirth in postnatal period. The cluster analysis showed that emotional freedom technique, haptonomy, motivational interview, cognitive-behavioral therapy, counseling therapy were considered to be more effective non-pharmacological interventions.
Conclusion: Several non-pharmacological interventions are promising in the daily care of pregnant women with fear of childbirth. Healthcare professionals should be encouraged to apply these non-pharmacological interventions for informal caregivers of pregnant women with fear of childbirth.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO, CRD42024536944.
Fear of childbirth (FOC), a prominent perinatal mental health challenge, has been shown to exert profound effects on both maternal and infant health outcomes (Chen et al., 2024). Defined as persistent anxiety and psychological distress associated with pregnancy and childbirth, FOC manifests through symptoms such as mood disorders, somatization, altered decision-making behaviors, and, in some cases, avoidance behaviors like opting for non-medically indicated cesarean sections or seeking active contraception (Alizadeh-Dibazari et al., 2024). Global epidemiological studies indicate that approximately 80% of pregnant women experience varying degrees of FOC, with 6.3 to 14.8% (Nilsson et al., 2018) meeting the diagnostic criteria for severe FOC, often classified as tokophobia. This specific fear disorder is significantly linked to an increased risk of postpartum depression, prolonged labor, and higher rates of neonatal NICU admissions (Horsch et al., 2024).
FOC has been found to be influenced by a range of factors, which can be categorized into four key domains: (1) psychological factors, such as anxiety, depression, stress, and low self-efficacy regarding childbirth (Dencker et al., 2019; Hildingsson et al., 2024; Zhang et al., 2023); (2) sociodemographic factors, including lower educational levels, economic disadvantage, and insufficient social support (Behmanesh et al., 2024; Dencker et al., 2019); (3) growth experiences and cultural perceptions, which encompass a history of emotional abuse or neglect during childhood, as well as cultural views that perceive childbirth as a high-risk medical event; and (Dencker et al., 2019; Porthan et al., 2023; Preis et al., 2018) (4) spiritual health, with higher levels of spiritual well-being being associated with a reduced risk of FOC (Behmanesh et al., 2024). Existing literature consistently reports that primigravid women tend to experience significantly higher levels of FOC compared to multiparous women (Badaoui et al., 2019; Behmanesh et al., 2024; Nieminen et al., 2017; Zhang et al., 2023).
FOC can trigger a cascade of stress responses in pregnant women, manifesting as physiological alterations including elevated heart rate, increased blood pressure, and heightened cortisol levels (Alder et al., 2011; Reissland and Kisilevsky, 2016). These physiological changes may induce uterine environmental modifications that elevate risks of intrauterine growth restriction, fetal distress, preterm delivery, and low birth weight infants (Van den Bergh et al., 2005). Concurrently, the emotional and psychological reactions associated with labor anxiety are clinically correlated with reduced breastfeeding intention and impaired postpartum role adaptation (Challacombe et al., 2021; Yin et al., 2024). Such emotional and psychological responses may adversely affect the establishment of early maternal–infant attachment (Seefeld et al., 2021) and ultimately compromise the physical and psychological development of the newborn.
FOC can significantly hinder the development of a maternal social support network (Zhang et al., 2023). It not only diminishes a woman’s positive expectations about childbirth but also influences the attitudes of her spouse and family towards the experience (Aguilera-Martín et al., 2021). Women experiencing FOC often feel isolated and reluctant to share their concerns with others. Furthermore, societal idealization of childbirth may lead to feelings of self-blame and shame among pregnant women, which can exacerbate their psychological distress (Nilsson et al., 2018).
FOC imposes a dual burden on both the healthcare system and the broader socio-economic landscape. Studies have demonstrated that women with severe FOC are more likely to seek frequent medical consultations for FOC-related symptoms, experience prolonged sick leave and postpartum hospitalization, and have higher rates of psychotropic medication use and a greater need for psychosocial interventions compared to those with lower levels of FOC (Nieminen et al., 2017). For instance, in Sweden, the average total social costs for women with severe FOC were 10,830.2 euros, which was 38% higher than the control group (Nieminen et al., 2017). Additionally, FOC is a significant driver of medically unindicated CS, with pregnant women requesting CS due to concerns such as distrust of healthcare providers, fear of labor pain (particularly when epidural analgesia is unavailable or unaffordable), fear of pelvic floor injuries and incontinence, an concerns about the potential negative impact on their sexuality or sexual relationships (Betrán et al., 2018). The global CS rate has increased from 7% in 1990 to 21% in 2018, with rates reaching as high as 50% in low- and middle-income countries, such as those in Asia and South America (Ana et al., 2021). In these regions, inadequate primary healthcare and pregnant women’s mistrust of healthcare workers often lead them to opt for cesarean delivery to avoid perceived poor-quality labor and delivery care (Etcheverry et al., 2024; Long et al., 2018). This overuse of CS is medically unjustified and results in the unnecessary consumption of healthcare resources (Betrán et al., 2018).
Non-pharmacological interventions are the preferred first-line treatments for FOC. Previous reviews have reported antenatal education, psychoeducation and midwifery counselling as effective interventions for reducing FOC (Akgün et al., 2020; Alizadeh-Dibazari et al., 2023; Alizadeh-Dibazari et al., 2024; Bakhteh et al., 2024). However, the evidence for the effectiveness of cognitive-behavioral therapy (CBT), mindfulness-based therapy and various newer alternative treatments remains unclear or conflicting (Aguilera-Martín et al., 2021; Badaoui et al., 2019; Neo et al., 2022; Striebich et al., 2018). Some meta-analyses included small sample sizes (Akgün et al., 2020; O'Connell et al., 2021) and incorporated non-randomized controlled trials (Akgün et al., 2020; Evans et al., 2022), which may compromise statistical power and evidence quality. Most studies (Aguilera-Martín et al., 2021; Alizadeh-Dibazari et al., 2024; O'Connell et al., 2021; Striebich et al., 2018) failed to measure psychological indicators closely related to FOC such as anxiety, depression, and childbirth self-efficacy, while also lacking follow-up assessments of postpartum and long-term psychological outcomes. Furthermore, most conventional meta-analyses only compared data between two interventions, failing to rank the effectiveness of multiple interventions. Consequently, it remains challenging to determine the optimal non-pharmacological intervention for reducing childbirth fear.
Network Meta-Analysis (NMA) is an advanced statistical method used to simultaneously compare the effects of multiple interventions, even when there are no direct comparative studies between them. By integrating both direct comparisons (e.g., A vs. B) and indirect comparisons (e.g., A vs. C inferred through A vs. B and B vs. C), NMA constructs a network structure. This allows for a unified ranking and comprehensive evaluation of all interventions (Dias and Caldwell, 2019).
This study is the first to apply NMA to systematically review and analyze existing evidence, including randomized controlled trials of non-pharmacological interventions for FOC. The study aims to assess the effectiveness of various non-pharmacological interventions on FOC and rank their effects. Additionally, it considers the effects of these interventions on CS rate and psychological outcomes closely related to FOC, such as anxiety, depression, stress, and childbirth self-efficacy. Our study addresses a gap in the existing literature and provides an evidence-based foundation for enhancing interventions aimed at alleviating FOC.
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (Hutton et al., 2015). The network meta-analysis was preregistered at PROSPERO (CRD42024536944).
We searched all published literature in four databases, Pubmed, Cochrane CENTRAL, and Web of Science, from the date of April 2014 to April 2024. Taking Pubmed as an example, our search strategy is “#1 Parturition [MeSH Terms] OR (Parturitions OR Birth OR Births OR Childbirth OR Childbirths OR Deliver* OR antenatal OR prenatal OR postpartum OR puerperium OR gestation OR postnatal OR Pregnan*) AND (in the last 10 years)[Filter] AND (Randomized Controlled Trial)[Filter] #2 (Fear of childbirth) OR FOC OR fear OR (fear of birth) AND (in the last 10 years)[Filter] AND (Randomized Controlled Trial)[Filter] #3 #1 AND #2.” In addition, reference lists of the included studies, and published systematic reviews and meta-analyses were hand searched to improve coverage. The specific search strategy is shown in the Supplementary material 1.
We defined the target trials according to the PICOS (population, interventions, comparisons, outcomes, study design) selection criteria.
1. Population: Age > 18 years, pregnant women, not pregnancy after infertility treatment, no high-risk pregnancy conditions, no clear indication for cesarean section; normal cognitive functioning, can read and write, no other clearly diagnosed illness or mental disorder.
2. Interventions: Non-pharmacological interventions that can improve pregnant women’s fear of childbirth.
3. Comparisons: Placebo, care as usual, antenatal education (lectures, online antenatal courses, online counseling, psycho-education).
4. Outcomes: Primary outcome indicator FOC must have been assessed, otherwise studies not included. Primary outcomes include improvement of pregnant women’s FOC [measurements including W-DEQ (Wijma Delivery Experience/Expectation Questionnaire), CAQ (Childbirth Attitude Questionnaire), FOBS (Fear Of Childbirth Scale), PRAQ (Pregnancy Related Anxiety Questionnaire)]. Secondary outcomes include mode of delivery (cesarean section, natural birth), depression, anxiety, stress, childbirth self-efficacy.
5. Type of included studies: RCT (Randomized Controlled Trail).
(1) Not RCT, (2) conference papers, abstracts, meta-analyses, or systematic reviews, (3) papers with incomplete data, (4) papers published not in English.
Endnote X9.3.3 was used to manage the literature. Duplicates were excluded using the duplicate literature filtering function of the software, and two authors (ZHOU & ZHU) independently screened the papers based on study titles and abstracts to obtain papers that met the criteria. We then independently extracted data from the included studies. Disagreements were resolved by discussion between the two reviewers, and a third reviewer (LI) was consulted if necessary. If a consensus could not be reached, predefined tiebreaker criteria, such as prioritizing the most recent or methodologically rigorous study, were applied to ensure an objective resolution.
During data extraction, the primary outcome measure was FOB scales and the secondary outcome measures were mode of delivery, depression, stress, anxiety and delivery self-efficacy scales. Details of the extracted data included RCT registration number, first author, year of publication, country, sample size, baseline characteristics of participants (mean age and gestational week), interventions, days of duration, outcome measure indicators. Outcome data included baseline and endpoint data on FOB, depression, stress, anxiety, and childbirth self-efficacy scales, including means and standard deviations. In addition, the number of people who chose different modes of delivery was extracted. If the outcome of a trial included several post-intervention and follow-up scores, only the score immediately after the end of the intervention phase was used.
Two reviewers (ZHOU & ZHU) independently examined the methodological quality of individual studies by using Cochrane risk of bias tool 2.0. The assessment domains included: bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in measurement of the outcome, bias in selection of the reported result, and overall bias. The overall risk of bias judgement would be “high risk,” “low risk,” or “unclear,” which could be obtained based on signaling questions and corresponding algorithms. Any discrepancy was resolved by discussion and made a consensus.
The network meta-analysis (NMA) was conducted using Stata (version 17) based on frequentist principles. For studies reporting outcomes as pre- and post-intervention measures, we applied methods from the Cochrane Handbook to calculate the mean change and its corresponding standard deviation (SD). Continuous outcome indicators were analyzed using the standardized mean difference (SMD) with a 95% confidence interval (95% CI) as the effect size. The incidence of cesarean section (CS) was expressed as an odds ratio (OR) with a 95% CI. Statistical significance was defined as a p-value of less than 0.05.
Global inconsistency tests and node-splitting tests were used to assess inconsistency. A consistency model was used only if neither of the two reported significant inconsistency (p > 0.05). If inconsistency was reported in any network, sensitivity analysis was performed to identify the source of inconsistency, and the study was excluded from the network. Network diagrams of the interventions were constructed to show the correlation between treatment options. Publication bias within each network was assessed using funnel plots. The relative effectiveness of interventions was ranked by the surface under the cumulative ranking curve (SUCRA). Funnel plots were used to detect potential publication bias and small-sample effects. To compare the effectiveness of non-pharmacological interventions for reducing cesarean section rates. Between-study heterogeneity was evaluated using the Cochrane Q test (with significance set at p < 0.1) and I2 statistics (with values above 50% indicating substantial heterogeneity). If heterogeneity was not significant, a fixed-effects model was used for statistical analysis; otherwise, a random-effects model was applied. To assess the effectiveness of non-pharmacological interventions in reducing fear of childbirth among primiparous women and those with severe FOC (W-DEQ-A score ≥ 85), subgroup analysis was performed.
A total of 2,830 articles were yielded by the search by keywords. An additional 4 articles were identified by searching the reference lists of the included studies. After eliminating 699 duplicate articles and screening the titles and abstracts, we retained 84 articles for full-text reading and review. Finally, 32 (Abdollahi et al., 2020; Alivand et al., 2023; Andaroon et al., 2017; Baas et al., 2023; Boz et al., 2021; Calpbinici and Yücel, 2022; Çankaya and Şimşek, 2021; Dai et al., 2021; Duncan et al., 2017; Emadi et al., 2023; Ghasemi et al., 2018; Gökbulut et al., 2024; Gönenç and Dikmen, 2020; Güney et al., 2022; Güven Santur and Özşahin, 2024; Kuo et al., 2022; Lee et al., 2023; Lida and Fariborz, 2017; Mortazavi and Mehrabadi, 2021; Navaee and Abedian, 2015; Ozbek and Pinar, 2022; Rondung et al., 2018; Rouhe et al., 2015; Sun et al., 2021; Thijssen et al., 2023; Toohill et al., 2017; Uludağ et al., 2022; Vakilian et al., 2023; Veringa-Skiba et al., 2022; Wang et al., 2023; Wilczyńska et al., 2023; Yesildag and Golbasi, 2024) articles were included in this meta-analysis. The study selection flow chart is shown in Figure 1.
The trials included a total of 3,187 pregnant women receiving 17 non-pharmacological interventions. The specific interventions are as follows: (1) motivational interview (MI) (n = 3), (2) high intensity interval training (n = 1), (3) prenatal education program (n = 11), (4) emotional freedom technique (EFT) (n = 2), (5) mindfulness-based interventions (n = 6), (6) deep relaxation exercise (n = 1), (7) acceptance and commitment therapy (n = 1), (8) breathing awareness training (n = 1), (9) haptonomy (n = 2), (10) CBT (n = 3), (11) simulation-based childbirth education (n = 3), (12) eye movement desensitization and reprocessing therapy (n = 1), (13) counseling therapy (n = 3), (14) dance and music therapy (n = 1), (15) music therapy (n = 1), (16) placebo (n = 6), (17) care as usual (n = 19). The table of basic characteristics of included literature can be found in Supplementary material 2.
In general, the randomized controlled trials included in our network meta-analysis showed an acceptable and relatively low risk of biases. Almost all the included trials reported randomization but did not describe the allocation concealment in sufficient detail and were judged to have an unclear risk bias. Seven studies were judged to have a high risk of bias with regard to “blinding of participants and personnel” domain. Six studies had a high risk of bias concerned in the “blinding of outcome assessment” domain. Most studies described in detail the loss of follow-up and excluded data. Most studies had an unclear risk of selective reporting bias. Other risk of bias was not identified in the included studies. Supplementary material 3 presents the results of the methodological quality evaluation of the included studies.
Separate network meta-analyses were conducted to evaluate improvements in FOB both immediately post-intervention (during the gestational period) and after delivery. During the gestational period, FOB was measured using the W-DEQ-A, CAQ, FOBS, PRAQ-R2, and the Childbirth Self-Efficacy Questionnaire (fear subscale). In the postnatal period, the W-DEQ-B and FOBS were used as measurement instruments.
Overall, 32 randomized controlled trials comprising of 2,765 participants assessed the effects of 17 non-pharmacological interventions on FOB during gestational period.
The main results of the network meta-analyses are shown in Figure 2. All interventions were compared pairwise. Compared with usual care, seven non-pharmacological interventions were statistically significantly effective in reducing FOB during pregnancy. These included dance and music therapy (SMD = −1.82, 95%CI –3.48 to −0.16), CBT (SMD = −1.62, 95%CI –2.47 to −0.66), haptonomy (SMD = −1.43, 95%CI –2.63 to −0.24), mindfulness-based intervention (SMD = −1.38, 95%CI –2.11 to −0.65), MI (SMD = −1.35, 95%CI –2.35 to −0.35), counseling therapy (SMD = −1.08, 95%CI –1.91 to −0.25), antenatal education program (SMD = −0.85, 95%CI –1.50 to −0.20). No statistically significant differences were found in the pairwise comparisons of the other interventions.
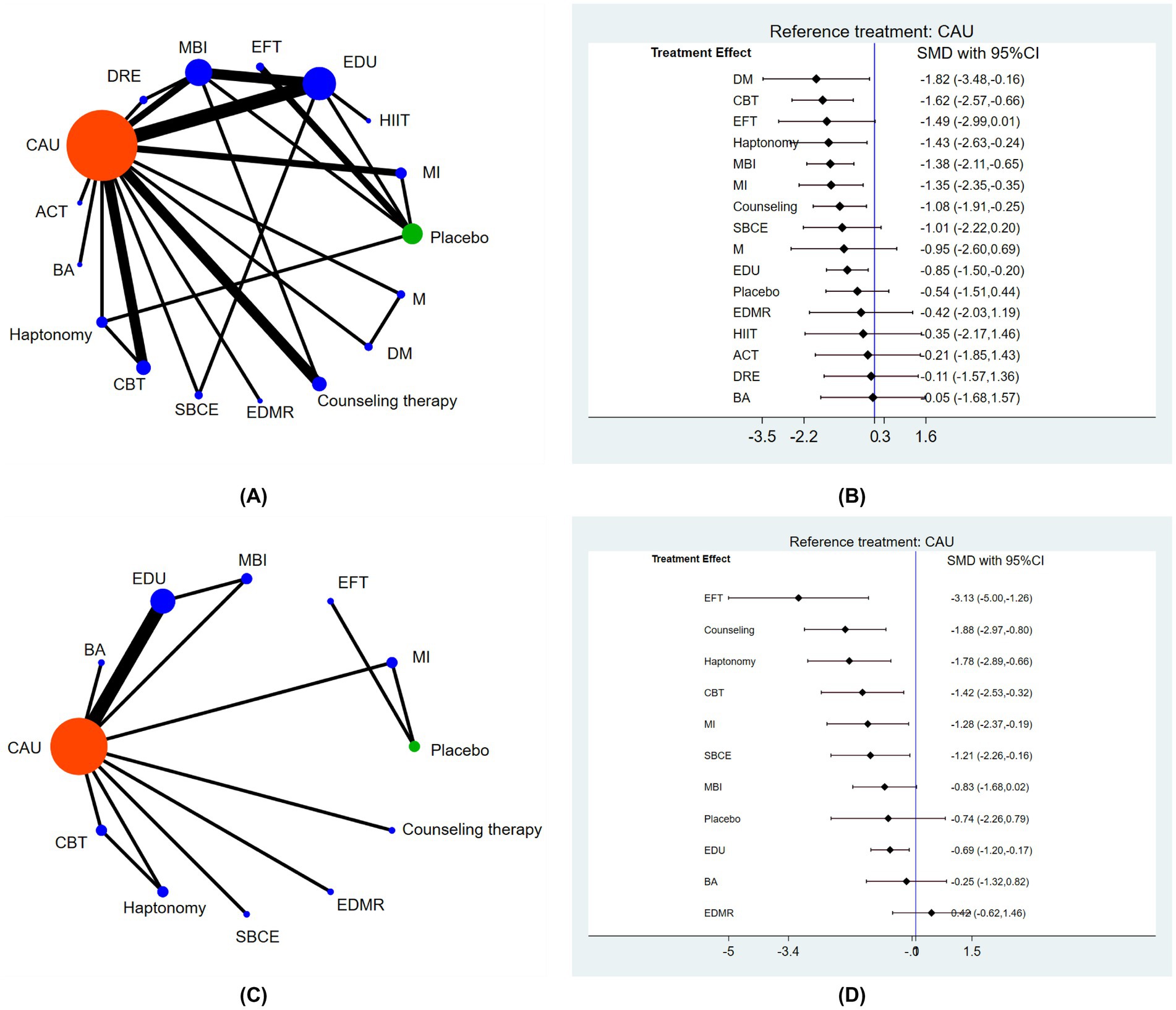
Figure 2. The main results of the network meta-analyses. (A) Network diagram of non-pharmacological interventions for fear of childbirth in the gestational period, (B) forest plot of pairwise comparisons between non-pharmacological interventions and usual care for reducing fear of childbirth in the gestational period, (C) network diagram of non-pharmacological interventions for fear of childbirth in the postnatal period, (D) forest plot of pairwise comparisons between non-pharmacological interventions and usual care for reducing fear of childbirth in the postnatal period. CAU = care as usual, ACT = acceptance commitment therapy, BA = breathing awareness training, CBT = cognitive behavior therapy, SBCE = simulation-based childbirth education, EDMR = eye movement desensitization and reprocessing therapy, DM = dance and music therapy, M = music therapy, MI = motivational interview, HIIT = high intensity interval training, EDU = prenatal education program, EFT = emotional freedom technique, MBI = mindfulness-based intervention, DRE = deep relaxation exercise.
A larger area in the SUCRA ranking chart for each intervention indicated a better intervention efficacy. The top three interventions were dance and music therapy (80.9), CBT (79.2) and EFT (72.6), as shown in Supplementary material 4.
Overall, 14 randomized controlled trials comprising of 1,388 participants assessed the effects of 12 non-pharmacological interventions on FOB during postnatal period.
The main findings of the network meta-analyses are shown in Figure 2. All intervention measures were compared pairwise. Compared with usual care, seven non-pharmacological interventions were statistically significantly effective in reducing fear of childbirth during postnatal period. They included EFT (SMD = −3.13, 95%CI –5.00 to −1.26), counseling therapy (SMD = −1.81, 95%CI –2.97 to −0.80), haptonomy (SMD = −1.78, 95%CI –2.89 to −0.66), CBT (SMD = −1.42, 95%CI –2.53 to −0.32), MI (SMD = −1.28, 95%CI –2.37 to −0.19), stimulate-based childbirth education (SMD = −1.21, 95%CI –2.26 to −0.16), antenatal education program (SMD = −0.69, 95%CI –1.20 to –0.17). No statistically significant differences were found in the pairwise comparisons of any other interventions.
According to the SUCRA ranking chart, the top three interventions were EFT (96.6), counseling therapy (79.4) and haptonomy (77.3), as shown in Supplementary material 4.
Seven randomized controlled trials comprising of 316 participants assessed the effects of 9 non-pharmacological interventions on FOB for primigravida during gestational period. All intervention measures were compared pairwise. Compared with placebo, three interventions were statistically significantly effective in reducing FOB of primigravida. They included MI (SMD = −0.57, 95%CI –1.04 to −0.11), EFT (SMD = −1.13, 95%CI –1.52 to −0.73), haptonomy (SMD = −1.21, 95%CI –2.26 to −0.16). Compared with usual care, two interventions including counseling therapy (SMD = −0.89, 95%CI –1.27 to −0.52) and simulate-based childbirth education (SMD = −0.88, 95%CI –1.43 to −0.33) were statistically significantly effective. The top intervention was EFT (SUCRA value: 98.8).
Nine randomized controlled trials comprising of 1,090 participants assessed the effects of 8 non-pharmacological interventions on severe fear of childbirth during gestational period. Compared with usual care, four interventions including CBT (SMD = −1.50, 95%CI –2.78 to −0.22), haptonomy (SMD = −1.67, 95%CI –2.95 to −0.38), mindfulness-based interventions (SMD = −1.58, 95%CI –3.01 to −0.16) and antenatal education program (SMD = − 1.15, 95%CI –1.89 to −0.41) were statistically significantly effective. The top intervention was haptonomy (SUCRA value: 77.9). The main results of subgroup analyses are shown in Supplementary material 4.
To better analyze the efficacy of different interventions in improving FOC during both gestational and postnatal periods and recommend more appropriate interventions for pregnant women, a cluster analysis was performed to combine the two outcome indicators to give a holistic evaluation. The different interventions were labeled using different colors. The more to the upper right the intervention, the better its efficacy, while the more to the lower left the intervention, the worse its efficacy. As shown in Figure 3, the five most effective interventions were EFT, counseling therapy, haptonomy, MI, and CBT.

Figure 3. The results of Cluster analyses. (A) Cluster analysis plot of the effect of non-pharmacological interventions on fear of childbirth in the gestational and postnatal period, (B) cluster analysis of the effectiveness of non-pharmacological interventions on fear of childbirth among primiparous women and those with severe childbirth fear.
We also conducted a cluster analysis of the effectiveness of different interventions among primigravida and pregnant women with severe FOC. The two most effective interventions were haptonomy and CBT.
After extracting the data on depression, stress, anxiety and childbirth self-efficacy from the included studies, the comparative effectiveness of interventions to improve these psychological symptoms was assessed by conducting pairwise meta-analyses using the random-effects model to directly compare the treatment effects of any two non-pharmacological interventions. Compared with usual care, counseling therapy was statistically significantly effective in reducing symptoms of depression, stress, and anxiety in pregnant women. No interventions are significantly better than other interventions at improving childbirth self-efficacy. Detailed results are provided in the Supplementary material 4.
Nine randomized controlled trials reported on the mode of delivery. As shown in Figure 4, The I2 statistic (0.0%) and p-value for heterogeneity (p = 0.576) indicate no significant heterogeneity among studies, meaning the results are consistent across studies. Two interventions demonstrated statistically significant effectiveness in reducing the cesarean section rate: haptonomy (OR = 3.10, 95% CI 1.05–9.11) and antenatal education programs (OR = 2.41, 95% CI 1.01–5.75).
Inconsistency of the data was detected according to the fit of the inconsistency model and node-splitting model, with closed-loop p > 0.05, suggesting no significant inconsistency between the results of direct comparison and indirect comparison. The Forest plots of consistency analyses are shown in Figure 5.
As shown in Figure 6, the scatter of points on the funnel plot has shown visually symmetrical in shape around the mean estimated treatment effect, indicating low risk of publication bias.
Our study included 32 randomized controlled trials, identifying 17 non-pharmacological interventions to address FOC in women through a network meta-analysis. We also extracted data on related outcomes, including depression, stress, anxiety, self-efficacy, and mode of delivery. This review demonstrated that dance and music therapy, CBT, and EFT were the top three interventions for reducing FOC. For alleviating FOC in postnatal period, EFT, counseling therapy, and haptonomy were the most effective.
Cluster analyses supported the recommendation of EFT, MI, haptonomy, counseling therapy, and CBT as effective non-pharmacological interventions for mitigating FOC. Subgroup analyses revealed that, compared with usual care, EFT was most effective for primigravida, while haptonomy had the greatest effect in women with severe FOC. Counseling therapy was found to be statistically significantly effective in reducing depression, stress, and anxiety symptoms in pregnant women compared to usual care. No single intervention showed a significant advantage over others in improving childbirth self-efficacy. However, haptonomy and antenatal education programs significantly reduced the cesarean section rate.
The study indicates that EFT can significantly reduce FOC. EFT, which blends cognitive and exposure therapies with acupressure, uses finger tapping on acupoints and is commonly known as “tapping” (Church et al., 2022). Clinical EFT is an evidence-based treatment for PTSD, with meta-analyses supporting its efficacy for depression, anxiety, and phobias (Clond, 2016; Sebastian and Nelms, 2017; Stapleton et al., 2023). EFT is accessible, easy to train, and safe, with remote instruction proving as effective as group sessions. This scalability makes it a promising, cost-effective intervention (Church et al., 2018). However, EFT has limited research in maternal health, and further high-quality studies are warranted, particularly for women with traumatic birth histories, to confirm EFT’ s efficacy in managing childbirth-related fears.
Haptonomy is an emerging intervention that fosters a positive emotional connection between mother and fetus through touch, potentially improving maternal mental health, preventing psychiatric disorders, and promoting strong mother-infant bonding (Fernandez, 2019; Ksycinski et al., 2010). Our findings suggest that haptonomy may help alleviate severe FOC and reduce cesarean section rates. However, it remains uncertain if the reduction in cesarean rates is clinically significant, given the limited studies and the influence of factors such as medical indications, partner preferences, and socio-economic and cultural considerations on delivery choice (Sebastião et al., 2016). Additionally, current trials focused only on primiparous women, and future research should include a wider population to confirm the effectiveness of haptonomy.
MI originated in addiction treatment and fosters a partnership between clinician and patient through an encouraging and guiding conversation style. It aims to evoke motivation for change by reinforcing and exploring the patient’s reasons for change, emphasizing patient autonomy, and prioritizing their needs (Miller and Rollnick, 2015). MI has proven to be an evidence-based approach for treating substance addictions, including alcohol, marijuana, and tobacco (Bischof et al., 2021). More recently, its use has expanded to mental health areas like anxiety and eating disorders (Romano and Peters, 2015), where MI has shown greater effectiveness as an adjunct to cognitive-behavioral therapy (CBT) compared to CBT alone (Marker and Norton, 2018). In the maternal health field, MI has been less extensively applied, this study suggests that MI holds potential as a primary or adjunctive method to reduce FOC.
This study found that both CBT and counseling therapy significantly reduce FOC. These interventions are commonly used to address psychological symptoms in pregnant women. While substantial evidence supports CBT’s effectiveness in improving sleep, anxiety, and depression during pregnancy (Shortis et al., 2020; Zheng et al., 2023), its impact on FOC is less studied or yields inconclusive results (Aguilera-Martín et al., 2021). CBT includes various formats. Some studies suggest face-to-face CBT is more effective than digital CBT due to adherence challenges (Larsson et al., 2017; Rondung et al., 2018), while others find no significant differences across formats or the opposite (Yunus et al., 2022). Our study did not distinguish between CBT types, suggesting future research should explore their specific effectiveness in reducing FOC. Counseling therapy, typically led by midwives, obstetricians, or psychologists, is a traditional psychological intervention (Souto et al., 2022). Although its effectiveness in reducing FOC is well-documented, some studies report limited impacts on FOC, childbirth experiences, and cesarean rates (Larsson et al., 2015).
Each intervention has different strengths and limitations in reducing fear of childbirth. EFT significantly reduces FOC and is easy to learn, safe, and cost-effective. However, there is limited research in maternal health, particularly for women with traumatic birth histories, and more high-quality studies are needed to confirm its effectiveness. Haptonomy may improve maternal mental health and reduce CS rates. However, current studies focus only on primiparous women, and the clinical significance of reduced cesarean rates remains uncertain. MI shows potential as an effective intervention for FOC, and further research is needed to explore its role in this context. CBT and counseling therapies are commonly used to reduce FOC. However, differences between CBT formats need further exploration. Counseling therapy is also effective in reducing FOC, though its impact on CS rates and childbirth experiences may be limited, suggesting a need for more effective alternatives. Further large-scale studies are needed to compare their efficacy and guide healthcare professionals in developing more effective strategies. Future research should compare the long-term effects of these interventions in larger samples and develop clinically practical, highly sensitive FOC assessment tools for rapid screening.
This study has several limitations requiring attention in future research. First, we did not conduct stratified analyses on sociodemographic factors that may influence FOC, such as age, gestational age, educational level, and income, nor did we account for variables such as treatment initiation and duration, which could introduce heterogeneity into the study. Second, some interventions, like music and dance therapy, were evaluated in only one study with small sample sizes, limiting result applicability and reliability. Third, the use of varying measurement scales with different structures, scoring criteria, and sensitivities may have introduced inconsistencies. Fourth, although all studies reported FOC outcomes, most did not assess related indicators such as depression, anxiety, stress, childbirth self-efficacy, or delivery methods. Fifth, many studies lacked adequate allocation concealment and blinding, risking bias and potential overestimation of intervention effects. Sixth, the inclusion of only English-language published literature introduces a potential risk of bias, as it may exclude relevant studies published in other languages.
Future research should compare the long-term effects of these interventions in larger samples and develop clinically practical, highly sensitive FOC assessment tools for rapid screening.
This study shows that EFT, haptonomy, MI, CBT, and counseling are significantly more effective than standard care in reducing prenatal and postpartum FOC. EFT was most effective for primiparous women, while haptonomy was most effective for women with severe FOC. Counseling significantly reduced depression, stress, and anxiety in pregnant women compared to usual care. No intervention showed a distinct advantage in improving childbirth self-efficacy. Based on these findings, EFT, haptonomy, MI, CBT, and counseling are recommended non-pharmacological interventions for FOC. Further research is needed to conduct high-quality investigations into the effectiveness of non-pharmacological interventions in addressing FOC.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
JZ: Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. ZZ: Data curation, Formal analysis, Methodology, Software, Writing – review & editing. RL: Data curation, Formal analysis, Methodology, Software, Writing – review & editing. XG: Conceptualization, Formal analysis, Methodology, Supervision, Writing – review & editing. DL: Conceptualization, Funding acquisition, Methodology, Resources, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2025.1530311/full#supplementary-material
Abdollahi, S., Faramarzi, M., Delavar, M. A., Bakouei, F., Chehrazi, M., and Gholinia, H. (2020). Effect of psychotherapy on reduction of fear of childbirth and pregnancy stress: a randomized controlled trial. Front. Psychol. 11:787. doi: 10.3389/fpsyg.2020.00787
Aguilera-Martín, Á., Gálvez-Lara, M., Blanco-Ruiz, M., and García-Torres, F. (2021). Psychological, educational, and alternative interventions for reducing fear of childbirth in pregnant women: a systematic review. J. Clin. Psychol. 77, 525–555. doi: 10.1002/jclp.23071
Akgün, M., Boz, İ., and Özer, Z. (2020). The effect of psychoeducation on fear of childbirth and birth type: systematic review and meta-analysis. J. Psychosom. Obstet. Gynaecol. 41, 253–265. doi: 10.1080/0167482X.2019.1689950
Alder, J., Breitinger, G., Granado, C., Fornaro, I., Bitzer, J., Hösli, I., et al. (2011). Antenatal psychobiological predictors of psychological response to childbirth. J. Am. Psychiatr. Nurses Assoc. 17, 417–425. doi: 10.1177/1078390311426454
Alivand, Z., Nourizadeh, R., Hakimi, S., Esmaeilpour, K., and Mehrabi, E. (2023). The effect of cognitive-behavioral therapy and haptonomy on fear of childbirth in primigravida women: a randomized clinical trial. BMC Psychiatry 23:929. doi: 10.1186/s12888-023-05414-3
Alizadeh-Dibazari, Z., Abdolalipour, S., and Mirghafourvand, M. (2023). The effect of prenatal education on fear of childbirth, pain intensity during labour and childbirth experience: a scoping review using systematic approach and meta-analysis. BMC Pregnancy Childbirth 23:541. doi: 10.1186/s12884-023-05867-0
Alizadeh-Dibazari, Z., Maghalain, M., and Mirghafourvand, M. (2024). The effect of non-pharmacological prenatal interventions on fear of childbirth: an overview of systematic reviews and meta-analysis. BMC Psychiatry 24:415. doi: 10.1186/s12888-024-05870-5
Ana, P. B., Jiangfeng, Y., Ann-Beth, M., João, P. S., and Jun, Z. (2021). Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob. Health 6:e5671. doi: 10.1136/bmjgh-2021-005671
Andaroon, N., Kordi, M., Kimiaei, S. A., and Esmaeily, H. (2017). The effect of individual counseling program by a midwife on fear of childbirth in primiparous women. J. Educ. Health Promot. 6:97. doi: 10.4103/jehp.jehp_172_16
Baas, M. A. M., Stramrood, C. A. I., Dijksman, L. M., Vanhommerig, J. W., de Jongh, A., and van Pampus, M. G. (2023). How safe is the treatment of pregnant women with fear of childbirth using eye movement desensitization and reprocessing therapy? Obstetric outcomes of a multi-center randomized controlled trial. Acta Obstet. Gynecol. Scand. 102, 1575–1585. doi: 10.1111/aogs.14628
Badaoui, A., Kassm, S. A., and Naja, W. (2019). Fear and anxiety disorders related to childbirth: epidemiological and therapeutic issues. Curr. Psychiatry Rep. 21:27. doi: 10.1007/s11920-019-1010-7
Bakhteh, A., Jaberghaderi, N., Rezaei, M., Naghibzadeh, Z. A., Kolivand, M., and Motaghi, Z. (2024). The effect of interventions in alleviating fear of childbirth in pregnant women: a systematic review. J. Reprod. Infant Psychol. 42, 5–21. doi: 10.1080/02646838.2022.2059458
Behmanesh, F., Alijanpour, M., Yahyavi, F., Nikpour, M., Haghighi, T., Karimnezhad Sorkhi, F., et al. (2024). Spiritual health, anxiety and fear of childbirth in Iran: is there any relationship? J. Relig. Health. 64, 400–412. doi: 10.1007/s10943-024-02067-8
Betrán, A. P., Temmerman, M., Kingdon, C., Mohiddin, A., Opiyo, N., Torloni, M. R., et al. (2018). Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet (London, England) 392, 1358–1368. doi: 10.1016/S0140-6736(18)31927-5
Bischof, G., Bischof, A., and Rumpf, H. (2021). Motivational interviewing: an evidence-based approach for use in medical practice. Dtsch. Arztebl. Int. 118, 109–115. doi: 10.3238/arztebl.m2021.0014
Boz, İ., Akgün, M., and Duman, F. (2021). A feasibility study of a psychoeducation intervention based on human caring theory in nulliparous women with fear of childbirth. J. Psychosom. Obstet. Gynaecol. 42, 300–312. doi: 10.1080/0167482X.2020.1752173
Calpbinici, P., and Yücel, C. (2022). The effect of the training program provided to primiparous pregnant women through the motivational interview method on their fear of childbirth, childbirth self-efficacy, and delivery mode: a randomized controlled trial. Curr. Psychol. 42, 21609–21623. doi: 10.1007/s12144-022-03285-7
Çankaya, S., and Şimşek, B. (2021). Effects of antenatal education on fear of birth, depression, anxiety, childbirth self-efficacy, and mode of delivery in primiparous pregnant women: a prospective randomized controlled study. Clin. Nurs. Res. 30, 818–829. doi: 10.1177/1054773820916984
Challacombe, F. L., Nath, S., Trevillion, K., Pawlby, S., and Howard, L. M. (2021). Fear of childbirth during pregnancy: associations with observed mother-infant interactions and perceived bonding. Arch. Womens Ment. Health 24, 483–492. doi: 10.1007/s00737-020-01098-w
Chen, C., Hussein, S. Z. B., Nasri, N. W. M., Yao, J., Qin, Y., Zhao, Z., et al. (2024). Fear of childbirth among pregnant women: a concept analysis. J. Adv. Nurs. 80, 4476–4487. doi: 10.1111/jan.16218
Church, D., Stapleton, P., Mollon, P., Feinstein, D., Boath, E., Mackay, D., et al. (2018). Guidelines for the treatment of ptsd using clinical eft (emotional freedom techniques). Healthcare 6:146. doi: 10.3390/healthcare6040146
Church, D., Stapleton, P., Vasudevan, A., and O'Keefe, T. (2022). Clinical eft as an evidence-based practice for the treatment of psychological and physiological conditions: a systematic review. PubMed. 13:951451. doi: 10.3389/fpsyg.2022.951451
Clond, M. (2016). Emotional freedom techniques for anxiety: a systematic review with meta-analysis. J. Nerv. Ment. Dis. 204, 388–395. doi: 10.1097/NMD.0000000000000483
Dai, L., Shen, Q., Redding, S. R., and Ouyang, Y. (2021). Simulation-based childbirth education for chinese primiparas: a pilot randomized controlled trial. Patient Educ. Couns. 104, 2266–2274. doi: 10.1016/j.pec.2021.02.036
Dencker, A., Nilsson, C., Begley, C., Jangsten, E., Mollberg, M., Patel, H., et al. (2019). Causes and outcomes in studies of fear of childbirth: a systematic review. Women Birth 32, 99–111. doi: 10.1016/j.wombi.2018.07.004
Dias, S., and Caldwell, D. M. (2019). Network meta-analysis explained. Archives of disease in childhood. Fetal Neonatal 104, F8–F12. doi: 10.1136/archdischild-2018-315224
Duncan, L. G., Cohn, M. A., Chao, M. T., Cook, J. G., Riccobono, J., and Bardacke, N. (2017). Benefits of preparing for childbirth with mindfulness training: a randomized controlled trial with active comparison. BMC Pregnancy Childbirth 17:140. doi: 10.1186/s12884-017-1319-3
Emadi, S. F., Hekmat, K., Abedi, P., and Maraghi, E. (2023). Effect of emotional freedom technique on the fear of childbirth in iranian primiparous women: a randomized controlled trial. Front. Psychol. 14:1145229. doi: 10.3389/fpsyg.2023.1145229
Evans, K., Rennick-Egglestone, S., Cox, S., Kuipers, Y., and Spiby, H. (2022). Remotely delivered interventions to support women with symptoms of anxiety in pregnancy: mixed methods systematic review and meta-analysis. J. Med. Internet Res. 24:e28093. doi: 10.2196/28093
Fernandez, M. (2019). Childbirth education: Comparative analysis. Childbirth. IntechOpen. doi: 10.5772/intechopen.88021
Ghasemi, F., Bolbol Haghighi, N., Mottaghi, Z., Hosseini, S., and Khosravi, A. (2018). The effect of group counseling with cognitive-behavioral approach on self-efficacy of pregnant women’s choice of vaginal delivery. Iran J. Psychiatry Behav. Sci. 12:e7632. doi: 10.5812/ijpbs.7632
Gökbulut, N., Cengizhan, S. Ö., Akça, E. I., and Ceran, E. (2024). The effects of a mindfulness-based stress reduction program and deep relaxation exercises on pregnancy-related anxiety levels: a randomized controlled trial. Int. J. Nurs. Pract. 30:e13238. doi: 10.1111/ijn.13238
Gönenç, İ. M., and Dikmen, H. A. (2020). Effects of dance and music on pain and fear during childbirth. J. Obstetric Gynecologic Neonatal Nurs. 49, 144–153. doi: 10.1016/j.jogn.2019.12.005
Güney, E., Cengizhan, S. Ö., Karataş Okyay, E., Bal, Z., and Uçar, T. (2022). Effect of the mindfulness-based stress reduction program on stress, anxiety, and childbirth fear in pregnant women diagnosed with COVID-19. Complement. Ther. Clin. Pract. 47:101566. doi: 10.1016/j.ctcp.2022.101566
Güven Santur, S., and Özşahin, Z. (2024). The effects of emotional freedom techniques implemented during early pregnancy on nausea-vomiting severity and anxiety: a randomized controlled trial. J. Integr. Complement Med. 30, 858–868. doi: 10.1089/jicm.2023.0586
Hildingsson, I., Nordin-Remberger, C., Wells, M. B., and Johansson, M. (2024). Cluster analysis of fear of childbirth, anxiety, depression, and childbirth self-efficacy. J. Obstetric Gynecologic Neonatal Nursing 53, 522–533. doi: 10.1016/j.jogn.2024.04.004
Horsch, A., Garthus-Niegel, S., Ayers, S., Chandra, P., Hartmann, K., Vaisbuch, E., et al. (2024). Childbirth-related posttraumatic stress disorder: definition, risk factors, pathophysiology, diagnosis, prevention, and treatment. Am. J. Obstet. Gynecol. 230, S1116–S1127. doi: 10.1016/j.ajog.2023.09.089
Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., et al. (2015). The prisma extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Intern. Med. 162, 777–784. doi: 10.7326/M14-2385
Ksycinski, W., Hartman-Ksycińska, A., and Pszeniczna, E. (2010). Prenatal baby's behaviour with the use of haptonomic techniques and the relevant experiences and reactions of the parents. Early Hum. Dev. 86:S125. doi: 10.1016/j.earlhumdev.2010.09.328
Kuo, T., Au, H., Chen, S., Chipojola, R., Lee, G. T., Lee, P., et al. (2022). Effects of an integrated childbirth education program to reduce fear of childbirth, anxiety, and depression, and improve dispositional mindfulness: a single-blind randomised controlled trial. Midwifery 113:103438. doi: 10.1016/j.midw.2022.103438
Larsson, B., Karlström, A., Rubertsson, C., and Hildingsson, I. (2015). The effects of counseling on fear of childbirth. Acta Obstet. Gynecol. Scand. 94, 629–636. doi: 10.1111/aogs.12634
Larsson, B., Karlström, A., Rubertsson, C., Ternström, E., Ekdahl, J., Segebladh, B., et al. (2017). Birth preference in women undergoing treatment for childbirth fear: a randomised controlled trial. Women Birth 30, 460–467. doi: 10.1016/j.wombi.2017.04.004
Lee, Y., Kim, S., and Choi, S. (2023). Effectiveness of mobile-based intervention self-care for pregnant women at work: a randomized controlled trial. J. Occup. Health 65:e12402. doi: 10.1002/1348-9585.12402
Lida, A., and Fariborz, B. (2017). The effectiveness of educating mindfulness on anxiety, fear of delivery, pain catastrophizing and selecting caesarian section as the delivery method among nulliparous pregnant women. Nurs. Pract. Today 4:52–63. Available at: https://npt.tums.ac.ir/index.php/npt/article/view/23.
Long, Q., Kingdon, C., Yang, F., Renecle, M. D., Jahanfar, S., Bohren, M. A., et al. (2018). Prevalence of and reasons for women's, family members', and health professionals' preferences for cesarean section in China: a mixed-methods systematic review. PLoS Med. 15:e1002672. doi: 10.1371/journal.pmed.1002672
Marker, I., and Norton, P. J. (2018). The efficacy of incorporating motivational interviewing to cognitive behavior therapy for anxiety disorders: a review and meta-analysis. Clin. Psychol. Rev. 62, 1–10. doi: 10.1016/j.cpr.2018.04.004
Miller, W. R., and Rollnick, S. (2015). Motivierende gesprächsführung: motivational interviewing: 3. Lambertus-Verlag: Auflage des standardwerks in deutsch.
Mortazavi, F., and Mehrabadi, M. (2021). Effectiveness of solution-focused counseling therapy on pregnancy anxiety and fear of childbirth: A randomized clinical trial. Nursing Practice Today. 8. doi: 10.18502/npt.v8i3.5939
Navaee, M., and Abedian, Z. (2015). Effect of role play education on primiparous women's fear of natural delivery and their decision on the mode of delivery. Iran. J. Nurs. Midwifery Res. 20, 40–46. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4325412/
Neo, H. S., Tan, J. H., Ang, W. H. D., and Lau, Y. (2022). Internet-delivered psychological interventions for reducing depressive, anxiety symptoms and fear of childbirth in pregnant women: a meta-analysis and meta-regression. J. Psychosom. Res. 157:110790. doi: 10.1016/j.jpsychores.2022.110790
Nieminen, K., Wijma, K., Johansson, S., Kinberger, E. K., Ryding, E., Andersson, G., et al. (2017). Severe fear of childbirth indicates high perinatal costs for swedish women giving birth to their first child. Acta Obstet. Gynecol. Scand. 96, 438–446. doi: 10.1111/aogs.13091
Nilsson, C., Hessman, E., Sjöblom, H., Dencker, A., Jangsten, E., Mollberg, M., et al. (2018). Definitions, measurements and prevalence of fear of childbirth: a systematic review. BMC Pregnancy Childbirth 18:28. doi: 10.1186/s12884-018-1659-7
O'Connell, M. A., Khashan, A. S., Leahy-Warren, P., Stewart, F., and O'Neill, S. M. (2021). Interventions for fear of childbirth including tocophobia. Cochrane Database Syst. Rev. 2021:CD013321. doi: 10.1002/14651858.CD013321.pub2
Ozbek, H., and Pinar, S. E. (2022). The effect of haptonomy applied to pregnant women on perceived stress, fear of childbirth, and prenatal attachment: randomized controlled experimental study. Curr. Psychol. 42, 23313–23322. doi: 10.1007/s12144-022-03388-1
Porthan, E., Lindberg, M., Härkönen, J., Scheinin, N. M., Karlsson, L., Karlsson, H., et al. (2023). Childhood trauma and fear of childbirth: findings from a birth cohort study. Arch. Womens Ment. Health 26, 523–529. doi: 10.1007/s00737-023-01328-x
Preis, H., Benyamini, Y., Eberhard-Gran, M., and Garthus-Niegel, S. (2018). Childbirth preferences and related fears - comparison between Norway and Israel. BMC Pregnancy Childbirth 18:362. doi: 10.1186/s12884-018-1997-5
Reissland, N., and Kisilevsky, B.S. (2016). Fetal development: Research on brain and behavior, environmental influences, and emerging technologies. Springer eBooks. Cham: Springer. doi: 10.1007/978-3-319-22023-9
Romano, M., and Peters, L. (2015). Evaluating the mechanisms of change in motivational interviewing in the treatment of mental health problems: a review and meta-analysis. Clin. Psychol. Rev. 38, 1–12. doi: 10.1016/j.cpr.2015.02.008
Rondung, E., Ternström, E., Hildingsson, I., Haines, H. M., Sundin, Ö., Ekdahl, J., et al. (2018). Comparing internet-based cognitive behavioral therapy with standard care for women with fear of birth: randomized controlled trial. Jmir. Ment. Health 5:e10420. doi: 10.2196/10420
Rouhe, H., Salmela-Aro, K., Toivanen, R., Tokola, M., Halmesmäki, E., Ryding, E., et al. (2015). Group psychoeducation with relaxation for severe fear of childbirth improves maternal adjustment and childbirth experience--a randomised controlled trial. J. Psychosom. Obstet. Gynaecol. 36, 1–9. doi: 10.3109/0167482X.2014.980722
Sebastian, B., and Nelms, J. (2017). The effectiveness of emotional freedom techniques in the treatment of posttraumatic stress disorder: a meta-analysis. Explore 13, 16–25. doi: 10.1016/j.explore.2016.10.001
Sebastião, Y. V., Womack, L., Vamos, C. A., Louis, J. M., Olaoye, F., Caragan, T., et al. (2016). Hospital variation in cesarean delivery rates: contribution of individual and hospital factors in Florida. Am. J. Obstet. Gynecol. 214, 123.e1–123.e18. doi: 10.1016/j.ajog.2015.08.027
Seefeld, L., Weise, V., Kopp, M., Knappe, S., and Garthus-Niegel, S. (2021). Birth experience mediates the association between fear of childbirth and mother-child-bonding up to 14 months postpartum: findings from the prospective cohort study dream. Front. Psych. 12:776922. doi: 10.3389/fpsyt.2021.776922
Shortis, E., Warrington, D., and Whittaker, P. (2020). The efficacy of cognitive behavioral therapy for the treatment of antenatal depression: a systematic review. J. Affect. Disord. 272, 485–495. doi: 10.1016/j.jad.2020.03.067
Souto, S. P. A. D., Silva, R. C. G. D., Prata, A. P., Guerra, M. J., Couto, C., and Albuquerque, R. S. D. (2022). Midwives' interventions for reducing fear of childbirth in pregnant women: a scoping review. JBI Evid Synth 20, 2867–2935. doi: 10.11124/JBIES-21-00382
Stapleton, P., Kip, K., Church, D., Toussaint, L., Footman, J., Ballantyne, P., et al. (2023). Emotional freedom techniques for treating post traumatic stress disorder: an updated systematic review and meta-analysis. PubMed. 14:1195286. doi: 10.3389/fpsyg.2023.1195286
Striebich, S., Mattern, E., and Ayerle, G. M. (2018). Support for pregnant women identified with fear of childbirth (foc)/tokophobia - a systematic review of approaches and interventions. Midwifery 61, 97–115. doi: 10.1016/j.midw.2018.02.013
Sun, Y., Li, Y., Wang, J., Chen, Q., Bazzano, A. N., and Cao, F. (2021). Effectiveness of smartphone-based mindfulness training on maternal perinatal depression: randomized controlled trial. J. Med. Internet Res. 23:e23410. doi: 10.2196/23410
Thijssen, K. M. J., Kierkels, J. J. M., van Meurs, A., Verhoeven, C. J., Der, V., Hout-van der Jagt, M. B., et al. (2023). Visualization of contractions: evaluation of a new experience design concept to enhance the childbirth experience. Birth 50, 1025–1033. doi: 10.1111/birt.12754
Toohill, J., Callander, E., Gamble, J., Creedy, D. K., and Fenwick, J. (2017). A cost effectiveness analysis of midwife psycho-education for fearful pregnant women - a health system perspective for the antenatal period. BMC Pregnancy Childbirth 17:217. doi: 10.1186/s12884-017-1404-7
Uludağ, E., Serçekuş, P., Vardar, O., Özkan, S., and Alataş, S. E. (2022). Effects of online antenatal education on worries about labour, fear of childbirth, preparedness for labour and fear of COVID-19 during the covid-19 pandemic: a single-blind randomised controlled study. Midwifery 115:103484. doi: 10.1016/j.midw.2022.103484
Vakilian, K., Rahmati, F., Khorsandi, M., and Majidi, A. (2023). Counseling by acceptance and commitment therapy approach on fear of childbirth: A randomized clinical trial. Open Public Health J, 16:e187494452306130. doi: 10.2174/18749445-v16-e230711-2022-191
Van den Bergh, B. R. H., Mulder, E. J. H., Mennes, M., and Glover, V. (2005). Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. Neurosci. Biobehav. Rev. 29, 237–258. doi: 10.1016/j.neubiorev.2004.10.007
Veringa-Skiba, I. K., de Bruin, E. I., van Steensel, F. J. A., and Bögels, S. M. (2022). Fear of childbirth, nonurgent obstetric interventions, and newborn outcomes: a randomized controlled trial comparing mindfulness-based childbirth and parenting with enhanced care as usual. Birth 49, 40–51. doi: 10.1111/birt.12571
Wang, S. L., Sun, M. Y., Huang, X., Zhang, D. M., Yang, L., Xu, T., et al. (2023). Benefits of mindfulness training on the mental health of women during pregnancy and early motherhood: a randomized controlled trial. Biomed. Environment. Sci. 36, 353–366. doi: 10.3967/bes2023.041
Wilczyńska, D., Walczak-Kozłowska, T., Santos-Rocha, R., Laskowski, R., and Szumilewicz, A. (2023). Stress is not so bad-cortisol level and psychological functioning after 8-week hiit program during pregnancy: a randomized controlled trial. Front. Public Health 11:1307998. doi: 10.3389/fpubh.2023.1307998
Yesildag, B., and Golbasi, Z. (2024). Effects of the web-based birth preparation programme and motivational interviews on primigravida women: randomized-controlled study. Int. J. Nurs. Pract. 30:e13207. doi: 10.1111/ijn.13207
Yin, A., Shi, Y., Heinonen, S., Räisänen, S., Fang, W., Jiang, H., et al. (2024). The impact of fear of childbirth on mode of delivery, postpartum mental health and breastfeeding: a prospective cohort study in shanghai, China. J. Affect. Disord. 347, 183–191. doi: 10.1016/j.jad.2023.11.054
Yunus, W. M., Matinolli, H., Waris, O., Upadhyaya, S., Vuori, M., Korpilahti-Leino, T., et al. (2022). Digitalized cognitive behavioral interventions for depressive symptoms during pregnancy: systematic review. J. Med. Internet Res. 24:e33337. doi: 10.2196/33337
Zhang, T., Liu, M., Min, F., Wei, W., Liu, Y., Tong, J., et al. (2023). Fear of childbirth and its determinants in pregnant women in the third trimester: a cross-sectional study. BMC Psychiatry 23:574. doi: 10.1186/s12888-023-05070-7
Keywords: non-pharmacological interventions, fear of childbirth, FOC, pregnant women, network meta-analysis
Citation: Zhou J, Zhu Z, Li R, Guo X and Li D (2025) Comparative efficacy of non-pharmacological interventions on fear of childbirth for pregnant women: a systematic review and network meta-analysis. Front. Psychol. 16:1530311. doi: 10.3389/fpsyg.2025.1530311
Received: 18 November 2024; Accepted: 19 February 2025;
Published: 12 March 2025.
Edited by:
Paul Greenman, University of Quebec in Outaouais, CanadaReviewed by:
Alessia Renzi, Sapienza University of Rome, ItalyCopyright © 2025 Zhou, Zhu, Li, Guo and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dehua Li, NTYyMzcyMTYyQHFxLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.