- 1Department of Community & Behavioral Health Sciences, Institute of Public and Preventative Health, Augusta University, Augusta, GA, United States
- 2School of Psychology, University College Dublin, Dublin, Ireland
- 3Centre for Motor Control, Faculty of Kinesiology & Physical Education, University of Toronto, Toronto, ON, Canada
- 4College of Health Professions, University of Montevallo, Montevallo, AL, United States
- 5Emory University School of Medicine Department of Medicine, Division of Geriatrics and Gerontology & Department of Rehabilitation, Atlanta, GA, United States
- 6Atlanta VA Center for Visual and Neurocognitive Rehabilitation, Decatur, GA, United States
- 7Birmingham/Atlanta VA Geriatric Research Education and Clinical Center, Decatur, GA, United States
Introduction
Dementia is a growing global public health priority, with 55 million people living with dementia (PLWD) worldwide (WHO, 2023). Approximately 45%−60% of dementia cases are preventable through modifiable risk factors (Calandri et al., 2024; Livingston et al., 2024). Much of the research on dementia focuses on prevention through lifestyle interventions, such as exercise (Kivipelto et al., 2020). Considerably less research has addressed treating dementia symptoms through lifestyle interventions, as PLWD are often excluded from intervention studies due to ineligibility criteria. Interventions must be tailored for PLWD because of their risk for recurrent falls (Jehu et al., 2021b) and distinct needs, such as forgetfulness (Jehu et al., 2024b), planning difficulties (Hauer et al., 2006), and apathy (Clarke et al., 2008). PLWD also commonly experience social isolation (Shen et al., 2022), poorer physical function (Jehu et al., 2024a), worsened behavioral and psychological symptoms (Cerejeira et al., 2012), poorer quality of life (Cerejeira et al., 2012), and reduced access to healthcare (Mitchell et al., 2016) compared to older adults without dementia. Designing efficacious interventions to improve health outcomes among PLWD is a frontline priority (Corriveau et al., 2017).
Potential benefits of dance interventions for PLWD
Dance can be particularly beneficial as a lifestyle intervention for PLWD through promoting social networking and enjoyment while boosting physical activity (Kshtriya et al., 2015). The aesthetic and creative aspects of dance may promote greater physiological arousal than aerobic exercise at a similar intensity (Fontanesi and DeSouza, 2020), but this should be confirmed by further studies with larger samples. Music and dance also encourage spontaneous rhythmic coupling between sensory and motor systems (Krotinger and Loui, 2021), and facilitate self-expression and the rediscovery of skills such as moving and singing as means of communicating (Hamill et al., 2012; Kshtriya et al., 2015).
Dementia is a progressive neurological disease that affects activities of daily living, while mild cognitive impairment is defined as cognitive decline greater than that expected for a person's age and education level, without significant functional impairment (Gauthier et al., 2006). Although dance has potential as a therapeutic intervention for PLWD, research on this population is scarce. A systematic review of dance interventions for PLWD (Karkou et al., 2023) found only one randomized controlled trial, which also included those with mild cognitive impairment (Ho et al., 2020), possibly masking between-group differences in responsiveness. This study found that dance improved loneliness, mood, physical functioning, and stress relative to a wait-list control group (Ho et al., 2020). Another randomized controlled trial comparing 2 months of Latin dance with a wait-list control found no differences in physical activity, fitness, or sedentary behavior, possibly due to the small sample size of n = 21 PLWD (Aguiñaga and Marquez, 2019). Other non-randomized controlled trials have indicated that dance is feasible in residential care facilities, but found no changes post-intervention, possibly due to small sample sizes (n < 30) (Hokkanen et al., 2008, 2003). One case study showed improved physical function following a 12-week salsa dance intervention in an individual with Alzheimer's disease (Abreu and Hartley, 2013). A quasi-experimental study comparing a 10-week dual-task intervention with an Iranian dance intervention found improvements in gait parameters among n=38 female PLWD (Ghadiri et al., 2022). Qualitative and non-randomized research has observed positive emotional reactions during dance among PLWD (Palo-Bengtsson and Ekman, 2002; Hamill et al., 2012; Guzmán-García et al., 2013; Bumanis and Yoder, 1988). Other research has indicated that PLWD exhibit procedural learning of the dance movements throughout the intervention (Rösler et al., 2002). Despite promising findings, there is a need to extend beyond feasibility studies and investigate dance interventions with adequate power and an active comparison group. General recommendations for exercise dosing exist for PLWD (Bushman, 2021), but further work should establish precise evidence-based exercise guidelines to improve outcomes in PLWD. No evidence-based dance guidelines exist to improve outcomes in PLWD. This opinion paper focuses on tailoring dance interventions for PLWD to increase uptake and improve treatment design.
Key considerations for dance for PLWD
Accessibility of dance
Researchers and dance instructors should make dance accessible, emphasizing participation over performance, to foster creativity and awareness of the body rather than accuracy (Hamill et al., 2012). PLWD may find dance easier in a partnered than group format because the former involves person-to-person interaction and connection (Abraham et al., 2024). Partnered dance involves leader and follower roles. The “leader” role, a proxy for internally generated movements, conveys direction, timing, and amplitude of steps with tactile cues, while the “follower” role, a proxy for externally generated movements, detects and responds to the leader's tactile cues (Abraham et al., 2024). The leader role is more cognitively demanding, requiring participants to remember specific movement sequences and choose appropriate next steps, while the follower role receives and responds to ongoing non-verbal cues. It may therefore be more beneficial to have PLWD in the less cognitively demanding follower role. Instructors should provide opportunities to engage in person-to-person contact and move together as a unit; such opportunities promote re-attachment and connection by overcoming communication difficulties, thereby building a socially cohesive environment (Hamill et al., 2012). Depending on dementia symptoms, such as agitation, PLWD may prefer non-partnered dance. Regardless of the dance type, participants should be encouraged to express themselves freely and spontaneously (Hamill et al., 2012). Instructors should wear name tags and simulate social interactions with group members while dancing (Hamill et al., 2012). We recommend regular reassurance, especially in times of confusion (Izquierdo et al., 2021). To foster meaningful progress in PLWD, we also recommend short and simple exercise instructions and mirroring techniques (i.e., performing dance moves with the PLWD enabling them to copy movements) (Izquierdo et al., 2021).
Individual adaptations
Adaptations to changing functional capacity levels should be considered throughout the intervention, to account for physical and functional limitations and secondary medical complications (Cipriani et al., 2020). Dementia is a non-linear progressive neurological disease that varies across individuals (Sachdev et al., 2014); thus, simpler instructions may be needed for PLWD as cognitive decline progresses. Cognitive, physical, and functional impairments may impact engagement and adherence levels; consequently, instructors should tailor dance programs to individuals' abilities. Conversely, PLWD may experience cognitive, physical, and functional improvements during interventions (Bracco et al., 2023); thus, complexity should be adjusted such that dance programs remain adequately challenging. Ongoing consultation with the PLWD's healthcare team (e.g., neuropsychologist), who are aware of the level of functional impairment, is important for appropriate dance prescription throughout the intervention (ACSM, 2021).
Caregiver support
Dance interventions seem to decrease caregiver burden (Wharton et al., 2021), and caregiver support is needed for PLWD to successfully engage in interventions. Reminders to attend classes can benefit PLWD who may lack an advocate and forget to attend (Portacolone et al., 2023), or may be aware of their own cognitive decline and avoid social activities due to embarrassment and stigmatization (Ho et al., 2021; Zhu et al., 2023). Partnered dance may be more beneficial for PLWD because a caregiver or instructor could act as a partner to cue for dance moves, help with spotting to reduce fall risk, and increase supervision for those who wander. However, partnered dance would likely increase intervention costs relative to group dance as each PLWD would need a cognitively intact partner (e.g., instructor/assistant).
Stakeholder input
Interventions should be designed with key stakeholders (e.g., caregivers, residential care facility staff, patients, and community advisory board) to ensure adequate training, resources, and support for PLWD in the community and residential care (Jehu et al., 2023b). Residential care facility staff have been hesitant to implement physical activity programs among PLWD due to therapeutic pessimism (Knaak et al., 2017), perceived risk, low belief in their utility, insufficient training and support, workload concerns, and high staff turnover (Wylie et al., 2022). Among PLWD, barriers to physical activity may be attitudinal or physical and include disliking physical activity, lacking experience of being physically active, pre-existing chronic conditions, sickness, holidays, and caregiver factors such as unavailability and health concerns (Suttanon et al., 2012). While residential care facility routines and negative attitudes about physical activity have reduced physical activity promotion in many facilities (Wylie et al., 2022), behavior change is possible among facility staff, caregivers, and PLWD (Low et al., 2015). For community-dwelling PLWD, it is important to support caregivers in delivering dance interventions to reduce burnout, such as providing educational resources, training, and regular phone calls (Jehu et al., 2023a). Several organizational factors should be considered when designing interventions, including ensuring that support (e.g., escorting PLWD to exercise, scheduling) and resources (e.g., staff) are available from the organization, as well as training researchers and dance instructors on the importance of dance interventions for PLWD, dance and dementia communication techniques, and safety (e.g., training for Cardiopulmonary Resuscitation and spotting) (Demers et al., 2015). Including PLWD and a community advisory board as members of the team can enable facilitators, avoid barriers, and promote generalizability to the larger population.
Considerations for choice of dance style and interventional targets
Selecting appropriate outcomes depending on individual needs, the type of dance, and dementia subtypes should be considered in the intervention design (Jehu et al., 2023a). For example, if the therapeutic target is to improve cardiovascular health, the current guidelines for prescribing exercise intensity should be followed (Riebe et al., 2015), and heart rate should be monitored throughout the intervention. Additional research is needed to identify optimal exercise intensities for improving health outcomes in specific populations, such as those with vascular dementia (Barnes and Corkery, 2018). If the therapeutic target is improving cognitive health, dance types involving visual-spatial cognition, memory, and planning, such as Argentinian Tango, may be appropriate, especially for people with Alzheimer's disease (Wharton et al., 2021). The dance style should be carefully selected for the target population, as even low-intensity dance could be challenging for deconditioned PLWD. The complexity of dance moves should be considered depending on dementia severity, as dance movements are generally more complicated than other types of exercise. To date, no studies have compared the effects of different doses of dance among PLWD for any outcome (Rice et al., 2024). Such research would provide insight into the frequency, intensity, and duration of dance required to achieve optimal benefits for PLWD.
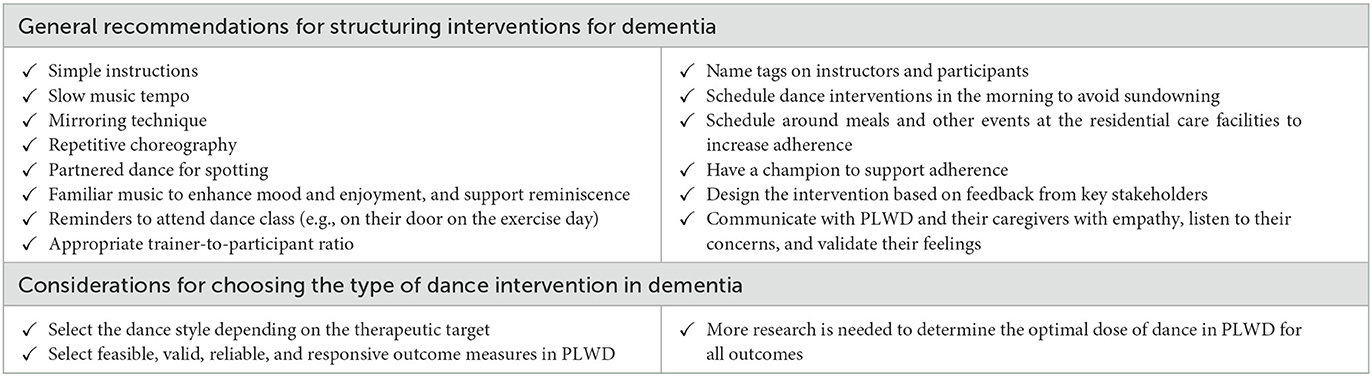
It is important to standardize person-centered valid and reliable outcome measures that are sensitive to change in dementia to increase comparability across studies. In a recent scoping review of more than 40 different types of dance intervention, over 50 cognitive measures and 30 mobility measures were identified, highlighting the lack of consistency in the standardization of outcomes (Rice et al., 2024). The outcome measures should also be feasible for PLWD. For example, previous work has documented substantial missing data due to poor adherence to wrist-worn activity monitors (Jehu et al., 2024b). Minor protocol changes (e.g., placing activity monitors on the lower back rather than the wrist) may increase adherence. A recent systematic review and consensus statement recommends a specific set of outcome measures for PLWD across cognition, activities of daily living, biological markers, neuropsychiatric symptoms, quality of life, and global domains (Webster et al., 2017). Dance researchers may want to provide similar recommendations in a consensus statement and add important measures such as balance, gait, falls, and social determinants of health (Jehu and Skelton, 2024, 2023; Jehu et al., 2021a). Researchers may also consider additional outcome measures depending on their research question, such as caregiver burden. Table 1 outlines a summary of our recommendations.
Future research directions
Preliminary research indicates potential cognitive, motor, and psychological benefits of dance interventions for PLWD (Balbim et al., 2022; Cezar et al., 2021). More rigorous research with larger sample sizes is needed. Involving PLWD, their caregivers, and clinicians in designing tailored and accessible dance interventions, as well as selecting appropriate outcomes, may increase relevance for this population. Dance intervention design should be tailored to neuropsychological and behavioral symptoms associated with specific dementia subtypes, such as addressing wandering for those with Alzheimer's disease or providing external cues for those with Parkinson's-related dementias. Our recommendations are more specifically for PLWD who are still able to follow instructions; further research is needed to involve those with more severe dementia. A better understanding of the impact of dance interventions on cognitive, motor, and psychological outcomes may inform targeted treatment and monitoring strategies in PLWD.
Author contributions
DJ: Conceptualization, Writing – original draft. JB: Writing – review & editing. CB: Writing – review & editing. MH: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. JB was supported by funding from the European Union's Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No. 101034345.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abraham, A., Hart, A., Bozzorg, A., Pothineni, S., Wolf, S. L., Schuh, K., et al. (2024). Comparison of externally and internally guided dance movement to address mobility, cognition, and psychosocial function in people with Parkinson's disease and freezing of gait: a case series. Front. Aging Neurosci. 16:1372894. doi: 10.3389/fnagi.2024.1372894
Abreu, M., and Hartley, G. (2013). The effects of Salsa dance on balance, gait, and fall risk in a sedentary patient with Alzheimer's dementia, multiple comorbidities, and recurrent falls. J. Geriatr. Phys. Ther. 36, 100–108. doi: 10.1519/JPT.0b013e318267aa54
ACSM (2021). American College of Sports Medicine's Guidelines for Exercise Testing and Prescription. Philadelphia, USA: Wolters Kluwer.
Aguiñaga, S., and Marquez, D. X. (2019). Impact of latin dance on physical activity, cardiorespiratory fitness, and sedentary behavior among latinos attending an adult day center. J. Aging Health 31, 397–414. doi: 10.1177/0898264317733206
Balbim, G. M., Falck, R. S., Barha, C. K., Starkey, S. Y., Bullock, A., Davis, J. C., et al. (2022). Effects of exercise training on the cognitive function of older adults with different types of dementia: a systematic review and meta-analysis. Br. J. Sports Med. 16:104955. doi: 10.1136/bjsports-2021-104955
Barnes, J. N., and Corkery, A. T. (2018). Exercise improves vascular function, but does this translate to the brain? Brain Plast 4, 65–79. doi: 10.3233/BPL-180075
Bracco, L., Pinto-Carral, A., Hillaert, L., and Mourey, F. (2023). Tango-therapy vs physical exercise in older people with dementia: a randomized controlled trial. BMC Geriatr. 23:693. doi: 10.1186/s12877-023-04342-x
Bumanis, A., and Yoder, J. W. (1988). Music and dance: tools for reality orientation. Activ. Adapt. Aging 10, 23–35. doi: 10.1300/J016v10n01_04
Bushman, B. P. M. (2021). Alzheimer's disease and physical activity. ACSM's Health Fitn. J. 25, 5–10. doi: 10.1249/FIT.0000000000000675
Calandri, I. L., Livingston, G., Paradela, R., Ossenkoppele, R., Crivelli, L., Allegri, R. F., et al. (2024). Sex and socioeconomic disparities in dementia risk: a population attributable fractions analysis in Argentina. Neuroepidemiology 58, 264–275. doi: 10.1159/000536524
Cerejeira, J., Lagarto, L., and Mukaetova-Ladinska, E. B. (2012). Behavioral and psychological symptoms of dementia. Front. Neurol. 3:73. doi: 10.3389/fneur.2012.00073
Cezar, N. O. C., Ansai, J. H., Oliveira, M. P. B., Da Silva, D. C. P., Gomes, W. L., Barreiros, B. A., et al. (2021). Feasibility of improving strength and functioning and decreasing the risk of falls in older adults with Alzheimer's dementia: a randomized controlled home-based exercise trial. Arch. Gerontol. Geriatr. 96:104476. doi: 10.1016/j.archger.2021.104476
Cipriani, G., Danti, S., Picchi, L., Nuti, A., and Fiorino, M. D. (2020). Daily functioning and dementia. Dement Neuropsychol. 14, 93–102. doi: 10.1590/1980-57642020dn14-020001
Clarke, D. E., Van Reekum, R., Simard, M., Streiner, D. L., Conn, D., Cohen, T., et al. (2008). Apathy in dementia: clinical and sociodemographic correlates. J. Neuropsychiatry Clin. Neurosci. 20, 337–347. doi: 10.1176/jnp.2008.20.3.337
Corriveau, R. A., Koroshetz, W. J., Gladman, J. T., Jeon, S., Babcock, D., Bennett, D. A., et al. (2017). Alzheimer's disease-related dementias summit 2016: national research priorities. Neurology 89, 2381–2391. doi: 10.1212/WNL.0000000000004717
Demers, M., Thomas, A., Wittich, W., and Mckinley, P. (2015). Implementing a novel dance intervention in rehabilitation: perceived barriers and facilitators. Disabil. Rehabil. 37, 1066–1072. doi: 10.3109/09638288.2014.955135
Fontanesi, C., and DeSouza, J. F. X. (2020). Beauty that moves: dance for Parkinson's effects on affect, self-efficacy, gait symmetry, and dual task performance. Front. Psychol. 11:600440. doi: 10.3389/fpsyg.2020.600440
Gauthier, S., Reisberg, B., Zaudig, M., Petersen, R. C., Ritchie, K., Broich, K., et al. (2006). Mild cognitive impairment. Lancet 367, 1262–1270. doi: 10.1016/S0140-6736(06)68542-5
Ghadiri, F., Bahmani, M., Paulson, S., and Sadeghi, H. (2022). Effects of fundamental movement skills based dual-task and dance training on single- and dual-task walking performance in older women with dementia. Geriatr. Nurs. 45, 85–92. doi: 10.1016/j.gerinurse.2022.03.003
Guzmán-García, A., Mukaetova-Ladinska, E., and James, I. (2013). Introducing a Latin ballroom dance class to people with dementia living in care homes, benefits and concerns: a pilot study. Dementia 12, 523–535. doi: 10.1177/1471301211429753
Hamill, M., Smith, L., and Röhricht, F. (2012). ‘Dancing down memory lane': circle dancing as a psychotherapeutic intervention in dementia—a pilot study. Dementia 11, 709–724. doi: 10.1177/1471301211420509
Hauer, K., Becker, C., Lindemann, U., and Beyer, N. (2006). Effectiveness of physical training on motor performance and fall prevention in cognitively impaired older persons: a systematic review. Am. J. Phys. Med. Rehabil. 85, 847–857. doi: 10.1097/01.phm.0000228539.99682.32
Ho, A., Nicholas, M. L., Dagli, C., and Connor, L. T. (2021). Apathy, cognitive impairment, and social support contribute to participation in cognitively demanding activities poststroke. Behav. Neurol. 2021:8810632. doi: 10.1155/2021/8810632
Ho, R. T. H., Fong, T. C. T., Chan, W. C., Kwan, J. S. K., Chiu, P. K. C., Yau, J. C. Y., et al. (2020). Psychophysiological effects of dance movement therapy and physical exercise on older adults with mild dementia: a randomized controlled trial. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 560–570.
Hokkanen, L., Rantala, L., Remes, A. M., Härkönen, B., Viramo, P., and Winblad, I. (2003). Dance/Movement Therapeutic methods in management of dementia. J. Am. Geriatr. Soc. 51, 576–577. doi: 10.1046/j.1532-5415.2003.51175.x
Hokkanen, L., Rantala, L., Remes, A. M., Härkönen, B., Viramo, P., and Winblad, I. (2008). Dance and movement therapeutic methods in management of dementia: a randomized, controlled study. J. Am. Geriatr. Soc. 56, 771–772. doi: 10.1111/j.1532-5415.2008.01611.x
Izquierdo, M., Merchant, R. A., Morley, J. E., Anker, S. D., Aprahamian, I., Arai, H., et al. (2021). International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J. Nutr. Health Aging 25, 824–853. doi: 10.1007/s12603-021-1665-8
Jehu, D. A., Davis, J. C., Barha, C. K., Vesely, K., Cheung, W., Ghag, C., et al. (2021a). Sex differences in subsequent falls and falls risk: a prospective cohort study in older adults. Gerontology 68, 272–279. doi: 10.1159/000516260
Jehu, D. A., Davis, J. C., Falck, R. S., Bennett, K. J., Tai, D., Souza, M. F., et al. (2021b). Risk factors for recurrent falls in older adults: a systematic review with meta-analysis. Maturitas 144, 23–28. doi: 10.1016/j.maturitas.2020.10.021
Jehu, D. A., Davis, J. C., Gill, J., Oke, O., and Liu-Ambrose, T. (2023a). The effect of exercise on falls in people living with dementia: a systematic review. J. Alzheimers Dis. 92, 1199–1217. doi: 10.3233/JAD-221038
Jehu, D. A., Dong, Y., Zhu, H., Huang, Y., Soares, A., Patel, C., et al. (2023b). The effects of strEngth aNd BaLance exercise on Executive function in people living with Dementia (ENABLED): study protocol for a pilot randomized controlled trial. Contemp. Clin. Trials 130:107220. doi: 10.1016/j.cct.2023.107220
Jehu, D. A., Langston, R., Sams, R., Young, L., Hamrick, M., Zhu, H., et al. (2024a). The impact of dual-tasks and disease severity on posture, gait, and functional mobility among people living with dementia in residential care facilities: a pilot study. Sensors 24:2691. doi: 10.3390/s24092691
Jehu, D. A., Pottayil, F., Dong, Y., Zhu, H., Sams, R., and Young, L. (2024b). Exploring the association between physical activity and cognitive function among people living with dementia. J. Alzheimers Dis. 2024:230594. doi: 10.3233/JAD-230594
Jehu, D. A., and Skelton, D. A. (2023). The measurement and reporting of falls: recommendations for research and practice on defining faller types. J. Frailty Sarcopenia Falls 8, 200–203. doi: 10.22540/JFSF-08-200
Jehu, D. A., and Skelton, D. A. (2024). The measurement and reporting of falls: recommendations for research on falls data collection and capturing social determinants of health. J. Frailty Sarcopenia Falls 9, 166–168. doi: 10.22540/JFSF-09-166
Karkou, V., Aithal, S., Richards, M., Hiley, E., and Meekums, B. (2023). Dance movement therapy for dementia. Cochr. Datab. Syst. Rev. 8:Cd011022. doi: 10.1002/14651858.CD011022.pub3
Kivipelto, M., Mangialasche, F., Snyder, H. M., Allegri, R., Andrieu, S., Arai, H., et al. (2020). World-wide FINGERS network: a global approach to risk reduction and prevention of dementia. Alzheimers. Dement. 16, 1078–1094. doi: 10.1002/alz.12123
Knaak, S., Mantler, E., and Szeto, A. (2017). Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc. Manage. Forum 30, 111–116. doi: 10.1177/0840470416679413
Krotinger, A., and Loui, P. (2021). Rhythm and groove as cognitive mechanisms of dance intervention in Parkinson's disease. PLoS ONE 16:e0249933. doi: 10.1371/journal.pone.0249933
Kshtriya, S., Barnstaple, R., Rabinovich, D. B., and Desouza, J. F. X. (2015). Dance and aging: a critical review of findings in neuroscience. Am. J. Dance Ther. 37, 81–112. doi: 10.1007/s10465-015-9196-7
Livingston, G., Huntley, J., Liu, K. Y., Costafreda, S. G., Selbæk, G., Alladi, S., et al. (2024). Dementia prevention, intervention, and care: 2024 report of the lancet standing commission. Lancet 404, 572–628. doi: 10.1016/S0140-6736(24)01296-0
Low, L. F., Fletcher, J., Goodenough, B., Jeon, Y. H., Etherton-Beer, C., Macandrew, M., et al. (2015). A systematic review of interventions to change staff care practices in order to improve resident outcomes in nursing homes. PLoS ONE 10:e0140711. doi: 10.1371/journal.pone.0140711
Mitchell, R., Harvey, L., Brodaty, H., Draper, B., and Close, J. (2016). Hip fracture and the influence of dementia on health outcomes and access to hospital-based rehabilitation for older individuals. Disabil. Rehabil. 38, 2286–2295. doi: 10.3109/09638288.2015.1123306
Palo-Bengtsson, L., and Ekman, S. L. (2002). Emotional response to social dancing and walks in persons with dementia. Am. J. Alzheimers. Dis. Other Demen. 17, 149–153. doi: 10.1177/153331750201700308
Portacolone, E., Nguyen, T. T., Bowers, B. J., Johnson, J. K., Kotwal, A. A., Stone, R. I., et al. (2023). Perceptions of the role of living alone in providing services to patients with cognitive impairment. JAMA Netw. Open 6:e2329913. doi: 10.1001/jamanetworkopen.2023.29913
Rice, P. E., Thumuluri, D., Barnstaple, R., Fanning, J., Laurita-Spanglet, J., Soriano, C. T., et al. (2024). Moving towards a medicine of dance: a scoping review of characteristics of dance interventions targeting older adults and a theoretical framework. J. Alzheimers Dis. 2024:230741. doi: 10.3233/JAD-230741
Riebe, D., Franklin, B. A., Thompson, P. D., Garber, C. E., Whitfield, G. P., Magal, M., et al. (2015). Updating ACSM'S recommendations for exercise preparticipation health screening. Med. Sci. Sports Exerc. 47, 2473–2479. doi: 10.1249/MSS.0000000000000664
Rösler, A., Seifritz, E., Kräuchi, K., Spoerl, D., Brokuslaus, I., Proserpi, S. M., et al. (2002). Skill learning in patients with moderate Alzheimer's disease: a prospective pilot-study of waltz-lessons. Int. J. Geriatr. Psychiatry 17, 1155–1156. doi: 10.1002/gps.705
Sachdev, P. S., Blacker, D., Blazer, D. G., Ganguli, M., Jeste, D. V., Paulsen, J. S., et al. (2014). Classifying neurocognitive disorders: the DSM-5 approach. Nat. Rev. Neurol. 10, 634–642. doi: 10.1038/nrneurol.2014.181
Shen, C., Rolls, E. T., Cheng, W., Kang, J., Dong, G., Xie, C., et al. (2022). Associations of social isolation and loneliness with later dementia. Neurology 99, e164–e175. doi: 10.1212/WNL.0000000000201564
Suttanon, P., Hill, K. D., Said, C. M., Byrne, K. N., and Dodd, K. J. (2012). Factors influencing commencement and adherence to a home-based balance exercise program for reducing risk of falls: perceptions of people with Alzheimer's disease and their caregivers. Int. Psychogeriatr. 24, 1172–1182. doi: 10.1017/S1041610211002729
Webster, L., Groskreutz, D., Grinbergs-Saull, A., Howard, R., O'brien, J. T., Mountain, G., et al. (2017). Core outcome measures for interventions to prevent or slow the progress of dementia for people living with mild to moderate dementia: systematic review and consensus recommendations. PLoS ONE 12:e0179521. doi: 10.1371/journal.pone.0179521
Wharton, W., Jeong, L., Ni, L., Bay, A. A., Shin, R. J., Mccullough, L. E., et al. (2021). A Pilot randomized clinical trial of adapted tango to improve cognition and psychosocial function in African American women with family history of Alzheimer's disease (ACT trial). Cereb. Circ. Cogn. Behav. 2:100018. doi: 10.1016/j.cccb.2021.100018
WHO (2023). Dementia [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed September 29, 2023).
Wylie, G., Kroll, T., Witham, M. D., and Morris, J. (2022). Increasing physical activity levels in care homes for older people: a quantitative scoping review of intervention studies to guide future research. Disabil. Rehabil. 45, 3160–3176. doi: 10.1080/09638288.2022.2118869
Keywords: dementia, dance, intervention, exercise, cognitive decline, mild cognitive impairment, physical activity
Citation: Jehu DA, Bek J, Bennett C and Hackney ME (2025) Group and partnered dance for people living with dementia: an overview of intervention design and measurement considerations. Front. Psychol. 16:1500688. doi: 10.3389/fpsyg.2025.1500688
Received: 23 September 2024; Accepted: 16 January 2025;
Published: 30 January 2025.
Edited by:
Christina E. Hugenschmidt, Wake Forest University, United StatesReviewed by:
Maura Crepaldi, University of Bergamo, ItalyAston McCullough, Northeastern University, United States
Copyright © 2025 Jehu, Bek, Bennett and Hackney. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Deborah A. Jehu, ZGplaHVAYXVndXN0YS5lZHU=
 Deborah A. Jehu
Deborah A. Jehu Judith Bek
Judith Bek Crystal Bennett
Crystal Bennett Madeleine E. Hackney
Madeleine E. Hackney