
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 05 February 2025
Sec. Health Psychology
Volume 16 - 2025 | https://doi.org/10.3389/fpsyg.2025.1440054
The present research assessed the psychometric properties of the Patient Health Questionnaire-9 (PHQ-9) through an examination of its internal structure, invariance analysis, and standardization. Social distribution analyses of the measure were conducted using linear and binomial logistic regression. The sample consisted of 10,069 adults from all 27 states in Brazil. The data were obtained through four collections across different years of the COVID-19 pandemic (2020, 2021, 2022, and 2023), using independent samples. Confirmatory Factor Analysis (CFA) indicated that the measure is unidimensional with satisfactory fit indices. The model was invariant in relation to the variables investigated at four different levels (configural, metric, scalar, and strict). The standardization supported hypothetical cut scores indicating the severity of depressive symptoms, categorized as very low (0 to 6), low (7 to 13), moderate (14 to 19), high (20 to 23), and very high (≥ 24). We found that sex/gender, skin color/ethnicity, age, education level, and year of the pandemic were predictors of depressive symptoms in the adjusted linear regression analysis. The logistic regression showed variables with higher chances for a positive screening diagnosis of depression, with adjusted Odds Ratio as follows: years 2021 (ORadj = 1.275) and 2023 (ORadj = 1.409), women (ORadj = 1.900), Pardos individuals (ORadj = 1.252), education up to high school (ORadj = 1.272), being a northeast region resident (ORadj = 2.127), and younger people (ORadj = 1.716). The findings of this study indicate the suitability of the PHQ-9 for assessing depression in the population and recommend its use for monitoring depressive symptoms in the coming years in Brazil. Clinical implications include developing interventions to address the psychological impact of this and any future health crises.
Every decade, the world prepares for a hypothetical pandemic-like health crisis—a phenomenon closely monitored by the World Health Organization (WHO). The European Commission’s Chief Scientific Advisory Group (ECCCSAG) is a dedicated committee that actively monitors and manages these proposals. Beginning in 2020, the global community experienced unique stressors due to the COVID-19 pandemic, one of the most devastating pandemics in recent history (Hiscott et al., 2020; Piret and Boivin, 2021; Smallwood, 2023). COVID-19 could be on its way to becoming an historic event, joining the larger pandemics of past centuries such as the Spanish flu, which have been extensively studied for their far-reaching effects (Demertzis and Eyerman, 2020; Moura et al., 2022; Nii-Trebi et al., 2023).
Given the magnitude of the COVID-19 outbreak, various delayed effects of the adaptive strain that people have endured over the battles of previous years are expected primarily for survival (Ashby et al., 2022; Kira et al., 2021). A significant increase in fatigue, loneliness (Mansueto et al., 2021) covid-anxiety syndrome (Alhakami et al., 2023; Mansueto et al., 2022) distress (Brailovskaia et al., 2021) as well as a decrease on well-being (Mansueto et al., 2024) have been observed across different samples and across different countries during COVID-19 pandemic. Due to the accumulation of stressors and organic as well as mental strains at various levels, vulnerabilities to certain diseases or disorders emerge (Haight et al., 2023). Previous findings in disaster Psychology provide evidence of the challenging times that follow in attempting to return to the new normal or even establishing new parameters for psychological adjustment. These adjustments involve incorporating new difficulties as part of daily life from then onwards (Nielsen et al., 2019). While we are moving towards declaring the end of the pandemic, there are still anticipated effects related to the pandemic especially concerning psychological adjustment and the mental health of the population (Gradidge et al., 2023; Kazlauskas and Quero, 2020). Health Psychology has fundamental contributions to understanding what impacted the population during this period, under what conditions, how it influenced their behaviors towards the pandemic, and how they stand today in terms of mental health and psychological adjustment. This focus frames the primary aims of this study.
Health Psychology contributes to studies aimed at assisting in planning actions that structure necessary care using an epidemiological perspective (Taylor, 2018). Actions such as addressing vaccine refusal are already being tackled by health belief models (Limbu et al., 2022; Suess et al., 2022) as well as modifying behaviors (Smail et al., 2021). Recommendations or protocols for identifying and managing depressive symptoms are also incorporated as they are a clinical condition often linked to adjustment difficulties during the pandemic (Lakhan et al., 2020). All these actions demonstrate potential applications to deal with post-COVID-19 crisis aspects as well as future demands (Esterwood and Saeed, 2020) requiring a current understanding of what transpired over the past years. Monitoring aspects of the population’s mental health throughout the pandemic contributes to understanding acute or chronic effects, potentially cumulative, that exacerbate the burden of psychological adjustment (Breslau et al., 2021). Research with this objective will help clarify the primary long-term impact on mental health across different individuals and groups.
Depressive symptoms are among the most studied mental health outcomes of the pandemic (Renaud-Charest et al., 2021). In various countries, depression has been monitored since 2020 (Dettmann et al., 2022; Mahmud et al., 2023; McPherson et al., 2021; Salari et al., 2020) given its association with greater strain and behavioral efforts to cope with the constant shocks that emerged daily with the pandemic’s grim news. The country’s major TV networks provided 24/7 coverage, seven days a week of all COVID-19 movements and statistics. Undoubtedly, it was the largest social network (or coverage) surrounding a disaster in human history. Never had there been such immediate, widespread transmission of so much misinformation in such a short time period.
The public health measures adopted to mitigate the spread of the coronavirus have had significant impacts on mental health protective structures, such as social support, routine, and access to resources like food, leisure, and performance (Shader, 2020). These changes in social dynamics are expected to induce alterations in people’s behavior, including modifications in sleep patterns, eating habits, substance use, and social interaction (Wu et al., 2021); aspects directly linked to depressive symptoms (Turna et al., 2021). Other factors contributed to an increase in depression in the population, such as high unemployment rates (Lee et al., 2021), loss of loved ones (Reitsma et al., 2021), financial insecurity (Wilson et al., 2020), social isolation (Gorenko et al., 2021), among others. Research in various countries reported high rates of depression during the COVID-19 outbreak. A study conducted in China with 14,493 individuals found that one in 20 adults had a suggestive depression score with a prevalence of 6.3% (Liu et al., 2022). The authors also noted that urban residents and nurses were more likely to be in the symptomatic group. A systematic review with meta-analysis investigated the prevalence of stress, anxiety, and depression in the general population during the first year of the pandemic across different continents (Salari et al., 2020). The prevalence of depression in 14 studies with a sample size of 44,531 was 33.7%. Additionally, Asia had the highest symptom rate at 35.3% (Salari et al., 2020).
A longitudinal study in Germany assessed changes in mental health symptoms, including depression, before and during the first and second waves of COVID-19. In the descriptive course, clinically relevant depression symptoms were more often reported in the first wave (13.9%), slightly decreasing in the second wave (12.1%), but did not reach pre-pandemic levels (9.7%). Depressive symptoms increased mainly in the younger individuals aged18 and 29 years (Hettich et al., 2022). Evidence has showed to other variables as relevant to understanding vulnerability to depressive symptomatology in the pandemic context, such as sex/gender (Qian et al., 2024), skin color/ethnicity (Maciel et al., 2023), and level of education (Zhu et al., 2023). Geographic region (Deng et al., 2021; Layton et al., 2021) and pandemic year (Grineski et al., 2024; Shen et al., 2024) are variables that have also been given attention and seem to predict the occurrence of depression.
Another study aimed to document the prevalence of depression in the adult population of the United States in the first year and 5 months of the pandemic based on data reported in peer-reviewed literature (Ettman et al., 2023). The overall mean prevalence reported over the first 17 months of the outbreak was 36.0% for mild depression, 26.0% for moderate depression, and 12.9% for severe depression. The researchers pointed out that the Patient Health Questionnaire-9 (PHQ-9) was the most used instrument to measure depressive symptoms and severity levels (n = 36; 76%; Ettman et al., 2023). These findings underscore the need to continue mapping the presence of depression in the population using context-adjusted measures so that with appropriate psychological strategies, techniques, and interventions, the mental wellbeing of the population can be maintained and improved.
The post-pandemic period challenges research to better understand the events during the phenomenon and rely on valid and reliable measures that accurately represent the dynamics of what is being studied. Thus, evaluating the psychometric and predictive qualities of a measure becomes fundamental to verify its behavior (or functioning) during the pandemic. This process not only allows us to understand any necessary changes due to the context, if applicable, but also to ensure that its indicators have evidence of validity and can be used safely. The change in context requires identification and modification of measures adjusted to the period given the unique externalities of the experienced adversities (Hernández et al., 2020). Some groups or individuals may have been more likely to present significant symptomatology, and certain symptoms may have been more characteristic (Ettman et al., 2023). The ability of psychological and/or psychiatric instruments to capture this variability with necessary and validated robustness is essential to understand the dimensions of the pandemic’s impact on psychological adjustment.
To estimate the validity evidence of a measure – in this case, the PHQ-9 (Kroenke et al., 2001), one of the most common instruments for measuring depressive symptoms globally (Costantini et al., 2021) – specific predictors for depression screening in the population can be sought with greater reliability. This estimation would facilitate the formulation of a more complete assessment of the indicators. There is also the possibility of using the data in a metric manner (PHQ-9 scores), categorical levels (diagnoses for screening), or even stratification of symptom severity in a population. All of these uses are subject to different interests and applications in basic community clinics, individual clinical settings, or systemic interventions. Investing and refining the measure and its indicators can be considered a pertinent contribution to the study of depression during the pandemic and in the following years.
The PHQ-9 is one of the most used depression scale worldwide, having been adapted into multiple languages, including Spanish, Japanese, Russian, Portuguese, among others (Lamela et al., 2020). Its factorial structure has been extensively evaluated in different countries such as Norway (Wisting et al., 2021), Chile (Aslan et al., 2020), Argentina (Urtasun et al., 2019), Germany (Reich et al., 2018), even in the context of the COVID-19 pandemic, including the United States (Shaff et al., 2024), Brazil (Nunes and Faro, 2021), China (Gao and Liu, 2024). Most validity studies have found support for a single-factor structure, reinforcing the greater plausibility for the measure’s unidimensional model. The evidence demonstrates good psychometric quality of the instrument, proving it a robust measure with potential for cross-country result comparisons (Odero et al., 2023; Rahman et al., 2022).
This study aims to investigate different aspects related to the instrument, measure, and indicators of depression in the Brazilian population during the COVID-19 pandemic years 2020, 2021, 2022, and 2023. The first aim seeks to validate the use of the PHQ-9 in the pandemic, a widely disseminated measure for measuring depressive symptoms. The PHQ-9 has been used in different countries during the pandemic [China (Choi et al., 2020), Israel (Palgi et al., 2020), France (Peretti-Watel et al., 2020), the United Kingdom (Kotabagi et al., 2020), Australia (Stocker et al., 2021), USA (Sekimitsu et al., 2022), Japan (Fukase et al., 2021), among others], demonstrating its breadth of application. In Brazil, we relied on the study performed by (Nunes and Faro, 2022), which only covered the 2020. In recent years, other studies involving Brazilian participants have been conducted, but they have primarily focused on specific demographics, such as undergraduate students (Rufino et al., 2024), or were limited to a single city (Lua et al., 2022). These studies did not address the broader population during the pandemic period. Since that data collection, the pandemic has gone through different phases which can be understood as differentiated periods within each year. These periods could have altered aspects of psychometric equivalence of the measure. As a result, the variation requires a new study with these new characteristics and more recent data, thus we performed a confirmatory factor analysis (CFA) and multi-group CFA of the PHQ-9 of the Brazilian population considering samples from four different time periods of the pandemic. This analysis will evaluate the potential effect of the pandemic year on the outcome along with a larger and more diversified geographic sample.
The second aim assesses the potential to standardize the PHQ-9 scores in the sample using novel data. This analysis will allow other studies to have parameters to weigh their findings and thus assist in clinical, policy, or governmental decision-making. Although it is not a randomized sample, the number of participants (over 10,000) and regional diversity (around 1,500 cities) helps the purpose of comparison not for diagnostic strata but for establishing general cut score based on an extensive sample.
The third aim seeks to conduct predictive testing of the PHQ-9 to enhance the findings of the study including information about the vulnerability of certain groups or individuals to depression in Brazil. These data are novel considering the proposed national design. The regression models (linear and logistic) seek to estimate vulnerability of certain groups dependent on specific conditions providing greater direction for current and future public health interventions.
The study had a successive cross-sectional and a non-probabilistic design based on independent samples by convenience method. Inclusion criteria included adults aged 18 years or more, and agreement to participate through a consent form. The exclusion criterion was an incomplete questionnaire response. The data were collected in four moments, one per year, in different years and distinct samples: the first from June 2 to June 6, 2020 (Epidemiological Week [EW], 23); at that moment, the restriction measures included social isolation and quarantine for the general population and at-risk groups, curfews, suspension of events and classes, transportation restrictions, mandatory mask-wearing, and economic shutdown. The second one was from March 18 to April 5, 2021 (EW 11, 12, and 13). In 2021, in addition to the previously mentioned measures, beach and park closures, prohibition of religious gatherings, collective sports activities, and food takeout from bars and restaurants were in effect. At that time, schools remained open only for meal distribution and provision of materials to students in need. Furthermore, national holidays were brought forward to encourage social isolation. The third data-collection was from March 17 to March 24, 2022 (EW 11 and 12). In 2022, the mandatory use of masks ceased in several states, such as Rio de Janeiro, Rio Grande do Sul, the Federal District, among others. All the others restriction measures were finished. The fourth data-collection was from March 17 to March 31, 2023 (EW 11, 12, and 13). In 2023, the use of masks was already optional nationwide and other restrictions were not in effect at the time.
10,069 adults comprised the full sample. Participants were from all 27 Brazilian states and approximately 1,500 cities. The majority of the total sample was collected in 2020 (47.6%; n = 4,793), followed by 2023 (22.2%; n = 2,238). 2021 and 2022 had roughly the same number of participants (15.1%; n = 1,522; n = 1,516, respectively). Females constituted the majority (88.2%; n = 8,880), as well as people who identified as White individuals (54.4%; n = 5,481), and those who had higher educational attainment (undergraduate and graduate, 81.6%; n = 8,218). The age group with the most participants was 18–24 years old (27.0%; n = 2,722), while the smallest group was those over 55 years old (13.3%; n = 1,342). The Northeast and Southeast regions were the most represented (39.2%; n = 3,951 and 38.6%; n = 3,891, respectively), with the North having the smallest proportion in the sample (3.1%; n = 311). Based on a screening cut score (> 10), almost two-thirds of the sample presented some level of significant depressive symptomatology (63.2%; n = 6,362) (Table 1).
The PHQ-9 is a self-administered questionnaire used for screening the presence and severity of depressive symptoms over the last 2 weeks, based on the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V) criteria (Kroenke et al., 2001). The PHQ-9 consists of nine items, with responses using a four-point Likert scale (0 = never, 1 = several days, 2 = more than half the days, 3 = nearly every day). According to the original study, a score higher than 10 indicates the presence of depressive symptoms. Previous research has demonstrated good psychometric properties of the scale (pre-pandemic studies), even during the pandemic period (Kroenke et al., 2001; Nunes and Faro, 2022; Odero et al., 2023; Sun et al., 2020). The Cronbach’s alpha (α) and McDonald’s omega (Ω) found in the current study were 0.90, indicating excellent internal consistency.
The Generalized Anxiety Disorder Screener (GAD-7) is a brief self-report measure that assesses the frequency of anxiety signs and symptoms over the past two weeks (Spitzer et al., 2006). The instrument consists of seven items rated on a four-point scale ranging from 0 (not at all) to 3 (nearly every day). The total score is obtained by summing the item responses, ranging from 0 to 21 points, with a score of 10 or higher considered a probable indicator of Generalized Anxiety Disorder (GAD). In its original study, the GAD-7 demonstrated excellent internal consistency (Cronbach’s α = 0.92). In this study, reliability was 0.90. A sociodemographic questionnaire was administered to collect data regarding the sample characteristics. Participants provided information about their age (in years, but later stratified into age groups), the year of the survey (2020, 2021, 2022 or 2023), sex/gender (male, female or other option) skin color/ethnicity (White, Black, Parda [mixed race], Yellow or Indigenous individuals, or other options), region of the country in which they reside (North, Northeast, Midwest, South, and Southeast), and education level (up to High school and Higher school).
This study was authorized by the Brazilian Research Ethics Committee with Human Subjects (National Council of Ethics and Research [CONEP], n° 3.955.180). For 4 years, data collection was done by approaching participants through invitations on digital platforms such as WhatsApp and Instagram. The questionnaire was created using the Survey Monkey platform and made available to individuals who accepted the invitations. It was not possible to estimate how many individuals did not agree to participate due to the method of randomly boosting the invitations in the social media platform. A consent form was presented on the first page of the questionnaire. Participants were granted access to the research questionnaires only after consent.
For the CFA and measurement invariance (MI), the Robust Diagonally Weighted Least Squares (RDWLS) estimation method was adopted. These analyses were performed using JASP Software (Version 0.18.0). The fit indices included the Comparative Fit Index (CFI; expected >0.95), Tucker-Lewis Index (TLI; expected >0.95), Root Mean Square Error of Approximation (RMSEA; expected ≤0.050, CI [95%] between 0 and 0.08; p-close >0.05) and Standardized Root Mean Residual (SRMR; expected ≤0.080). The testing for MI was executed at four levels: configural, metric, scalar, and strict (Cheung and Rensvold, 2002). The criteria of ΔCFI <0.010 and ΔRMSEA <0.015 were set for sequential models to assess invariance (Chen, 2007). Reliability was analyzed using Cronbach’s alpha (expected >0.60) and McDonald’s omega (expected >0.70) (Hair et al., 2014). The T Score (T = 50 + 10Z) of the PHQ-9 scores was also calculated.
Hierarchical linear regression (LinR) and binomial logistic regression (LogR) were executed through JAMOVI software (The jamovi project, 2022). The PHQ-9 score was the dependent variable in two types: score (LinR) and screening diagnosis (LogR). Sociodemographic and pandemic-related variables were added as independent variables in progressive blocks, as follows: pandemic year (2020, 2021, 2022 and 2023), sex/gender (male and female), skin color/ethnicity (White individuals, Black individuals and Parda [mixed race] individuals), education level (high school and higher school), Region (North, Northeast, Midwest, South and Southeast), and age group (18–24, 25–34, 35–44, 45–54 and more than 55 years old). Yellow, Indigenous individuals or other options for skin color/ethnicity, and other options for sex/gender participants were excluded of the sample due to the low quantity (<0.1%). Fit indicators included R2, adjusted R2, delta R2 (Nagelkerke’s R2 for LogR) to identify individual contributions of the independent variables to the models (LinR and LogR). The Durbin-Watson test and tests for evaluating multicollinearity (VIF and Tolerance) were analyzed (LinR). A Pearson correlation test between PHQ-9 (skewness = 0.046 and Kurtosis = −1.090) and GAD-7 (skewness = 0.046 and Kurtosis = −0.081) was performed to examine evidences of convergent validity. The significance level for the analyses in this study was set at p < 0.05.
The CFA general model showed a unidimensional structure of the PHQ-9. The fit indices were considered satisfactory [TLI = 0.99; CFI = 0.99; RMSEA = 0.05 (CI 95% = 0.047–0.054); SRMR = 0.003] and the total explained variance (R2) by item varied from 0.271 (item 9) to 0.708 (item 2), with an average of 0.522. All items loaded above 0.500, ranging from 0.520 (item 9) to 0.841 (item 2) with a mean loading as high as 0.717 (Table 2). Models fit at all four different levels of invariance (configural, metric, scalar, and strict levels; ∆CFI and ∆RMSE criteria) in relation to year, gender, educational level, geographic region, skin color, and age group comparisons (Table 3).
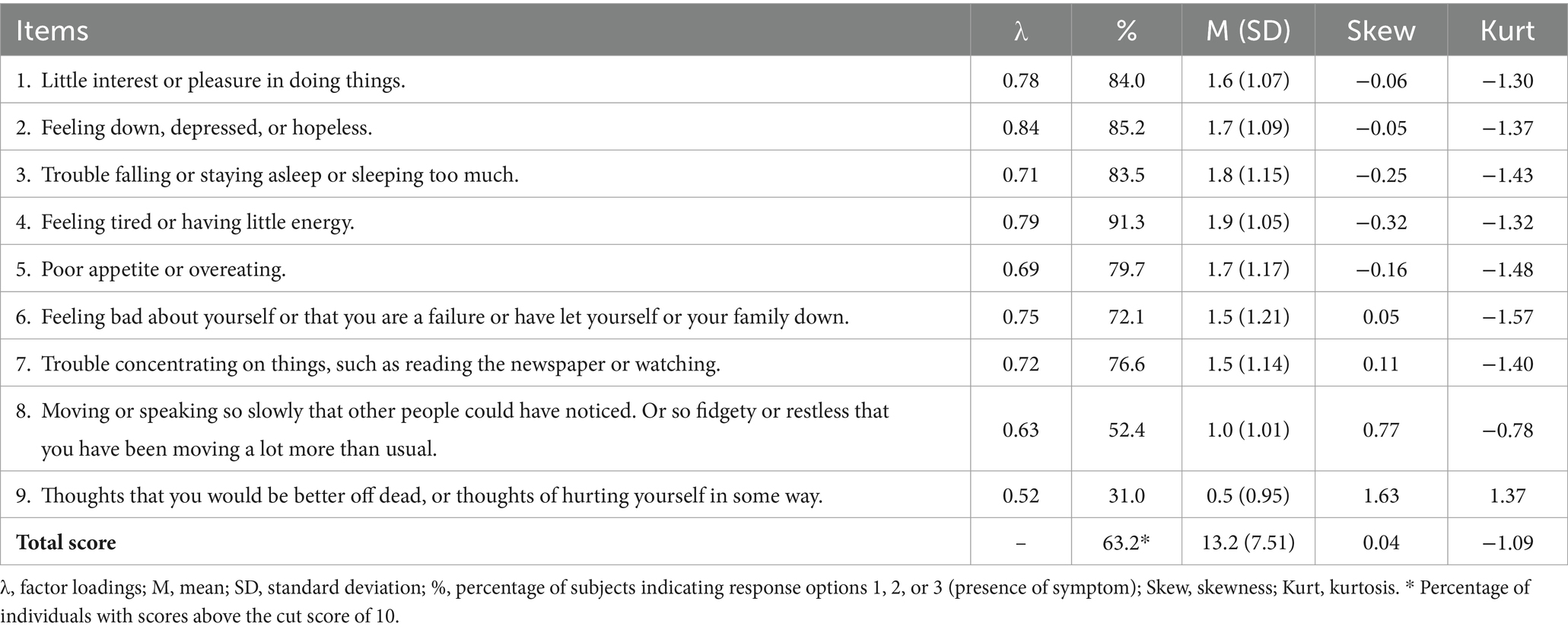
Table 2. Confirmatory factor analysis (factor loadings) and descriptive data of the Patient Health Questionnaire-9 items (PHQ-9), Brazil (2020–2023).
The descriptive data on the PHQ-9 items are displayed in Figure 1. Item 4 (Tiredness or lack of energy) showed the highest mean, followed by items 3 (had difficulty falling asleep or staying asleep without interruptions or slept too much), 2 (felt down, depressed, or hopeless), and 5 (had a poor or excessive appetite). The lowest were items 9 (thoughts that you would be better off dead, or of hurting yourself in some way) and 8 (Moved or spoke so slowly that other people could have noticed). The most frequent symptoms were item 4 (91.3%), item 2 (85.2%), and item 1 (had little interest or pleasure in doing things). The least common items were 9 (31.0%) and 8 (52.4%). The distribution of the item means from 2020 to 2023 is represented in Figure 1. A positive correlation between PHQ-9 and GAD-7 scores was found (Pearson = 0.756; p < 0.001), indicating the higher the depression score, the higher the anxiety score.
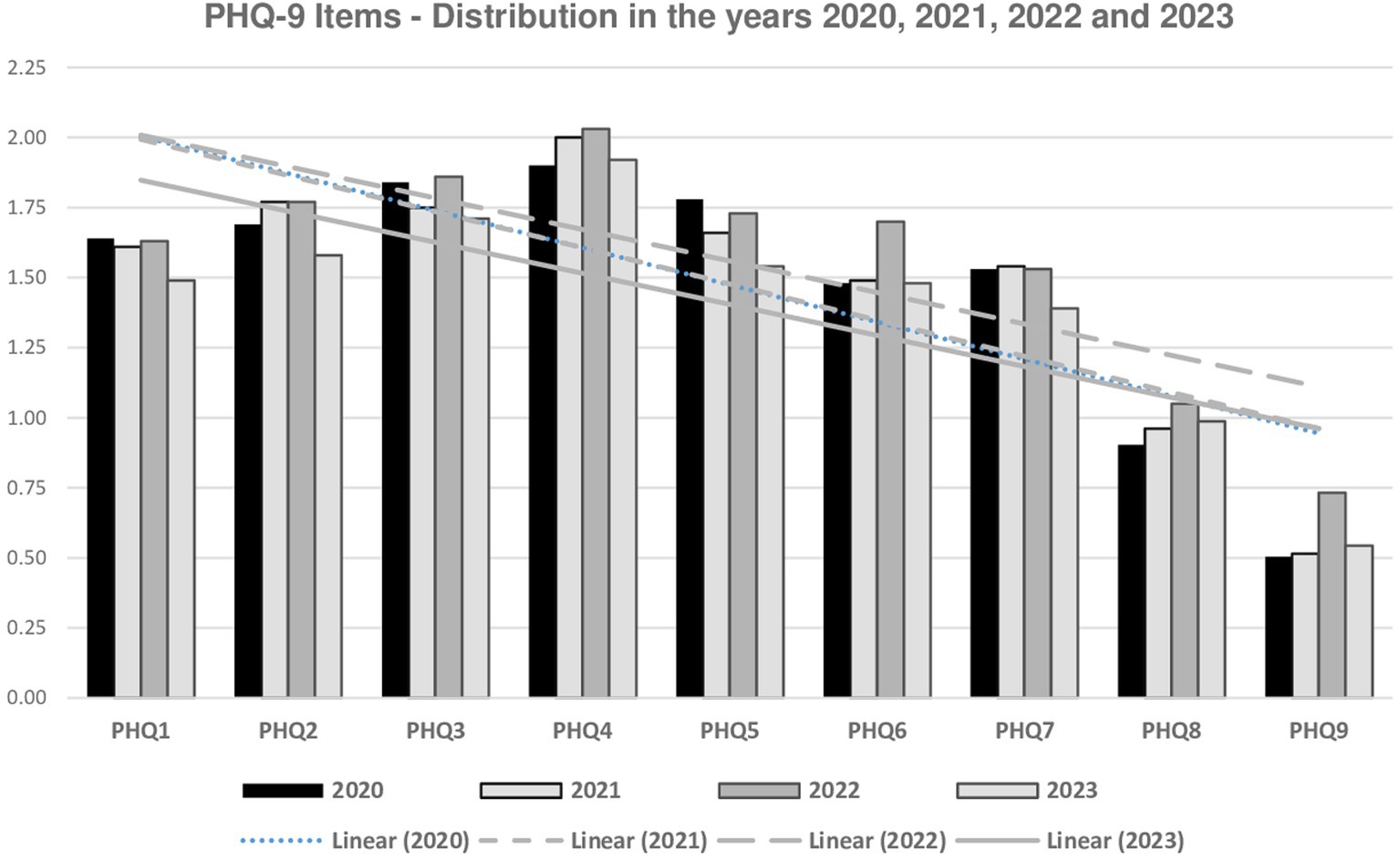
Figure 1. Distribution of PHQ-9 items, Brazil (2020–2023, n = 10,069). PHQ1, interest or pleasure; PHQ2, disinterest; PHQ3, sleep disturbances; PHQ4, fatigue; PHQ5, appetite changes; PHQ6, negative self-esteem; PHQ7, concentration difficulties; PHQ8, psychomotor changes; PHQ9, suicidal ideation.
Based on the CFA and CFAMG findings, Table 4 was created to propose parameters for estimating various scores based on the distribution in the total sample. Table 4 presents the T score for making comparisons on a standardized scale, the frequency of each score in the current population, and the cumulative frequency. Both the T Score and cumulative frequency provide support for hypothetical cut score indicating the severity of depressive symptoms in the general population. These suggestions are based on the social distribution of the PHQ-9 and can be a possible method for screening differences between samples or scenarios (e.g., different time-points after the COVID-19 pandemic). Therefore, the strata can be categorized as follows: very low (score 0 to 6, T = 40; F%cum ≈ 20%), low (score 7 to 13, T = 50; F%cum ≈ 50%), moderate (score 14 to 19, T = 58; F%cum ≈ 75%), high (score 20 to 23, T = 63; F%cum ≈ 90%), and very high (score > 24, T > 63; F%cum > 93.1%).
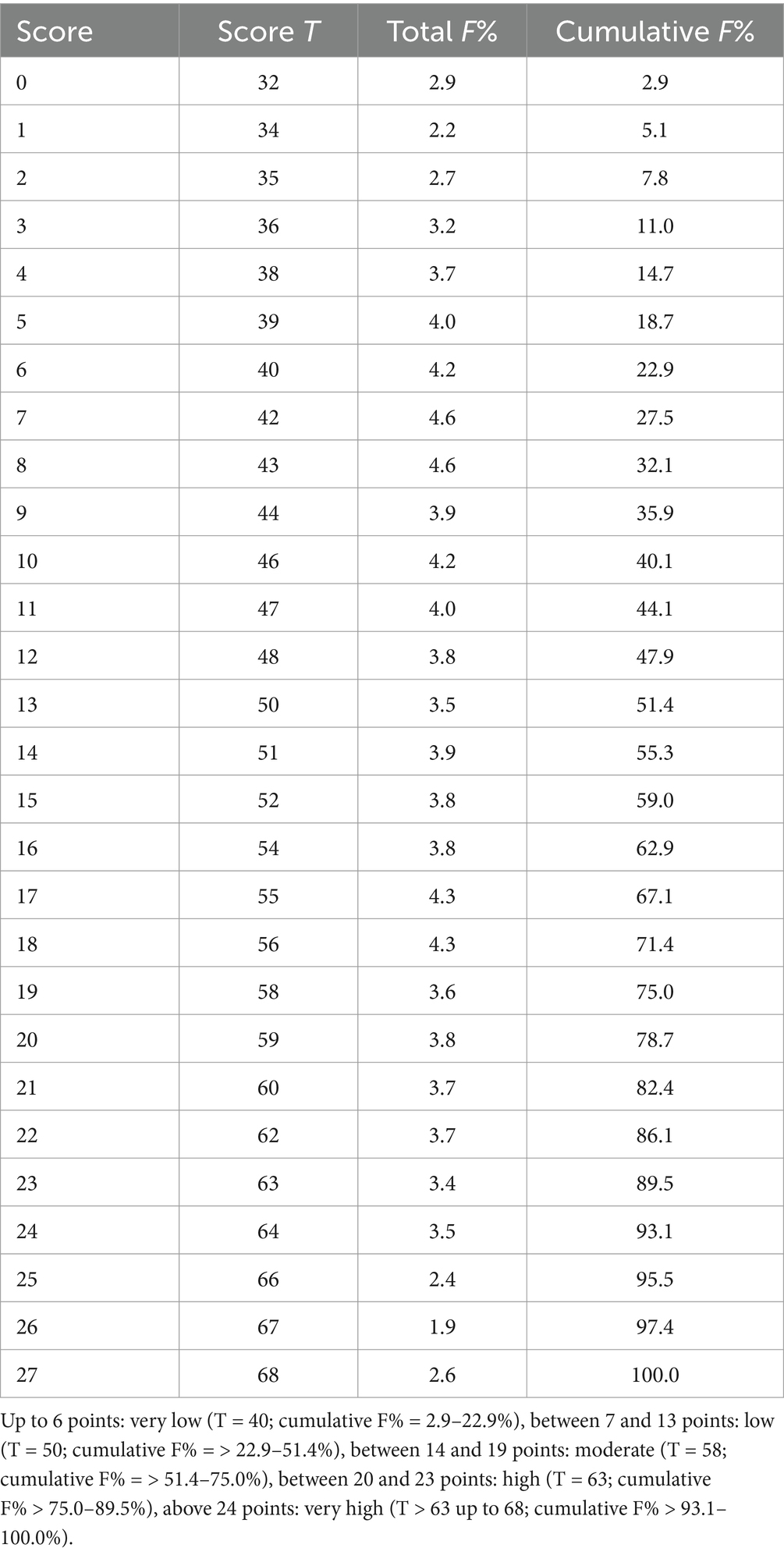
Table 4. Standardization of PHQ-9 scores during the COVID-19 pandemic, Brazil (cross-sectional data from 2020 to 2023, n = 10,069).
In the final adjusted linear regression model, all previous blocks showed statistical significance. In comparison to 2020, 2021 and 2022 exhibited a higher probability of being related to an increase in depressive symptomatology (β = 0.103 and 0.215, respectively; p < 0.001). There was no difference between 2020 and 2023 (p > 0.05). Females had greater depressive symptomatology compared to males (β = 0.345; p < 0.001). Participants identified as Pardos indicated more depressive symptoms than White individuals (β = 0.106; p < 0.001), but no difference was found when contrasting Black and White respondents (p > 0.05). Participants who self-reported having up to a high school education were more prone to show higher scores of depression symptoms (β = 0.132; p < 0.001). People living in the Northeast showed lower scores than those in the South (β = −0.342; p < 0.001); no other comparison by region was statistically significant (p > 0.05). Age indicated statistical significance overall with the younger age of the participant corresponding to a higher their score in depressive symptomatology (from β = 0.310 for 45–54; to 0.900 for 18–24 years old; age more than 55 as reference; p < 0.001) (Table 5).
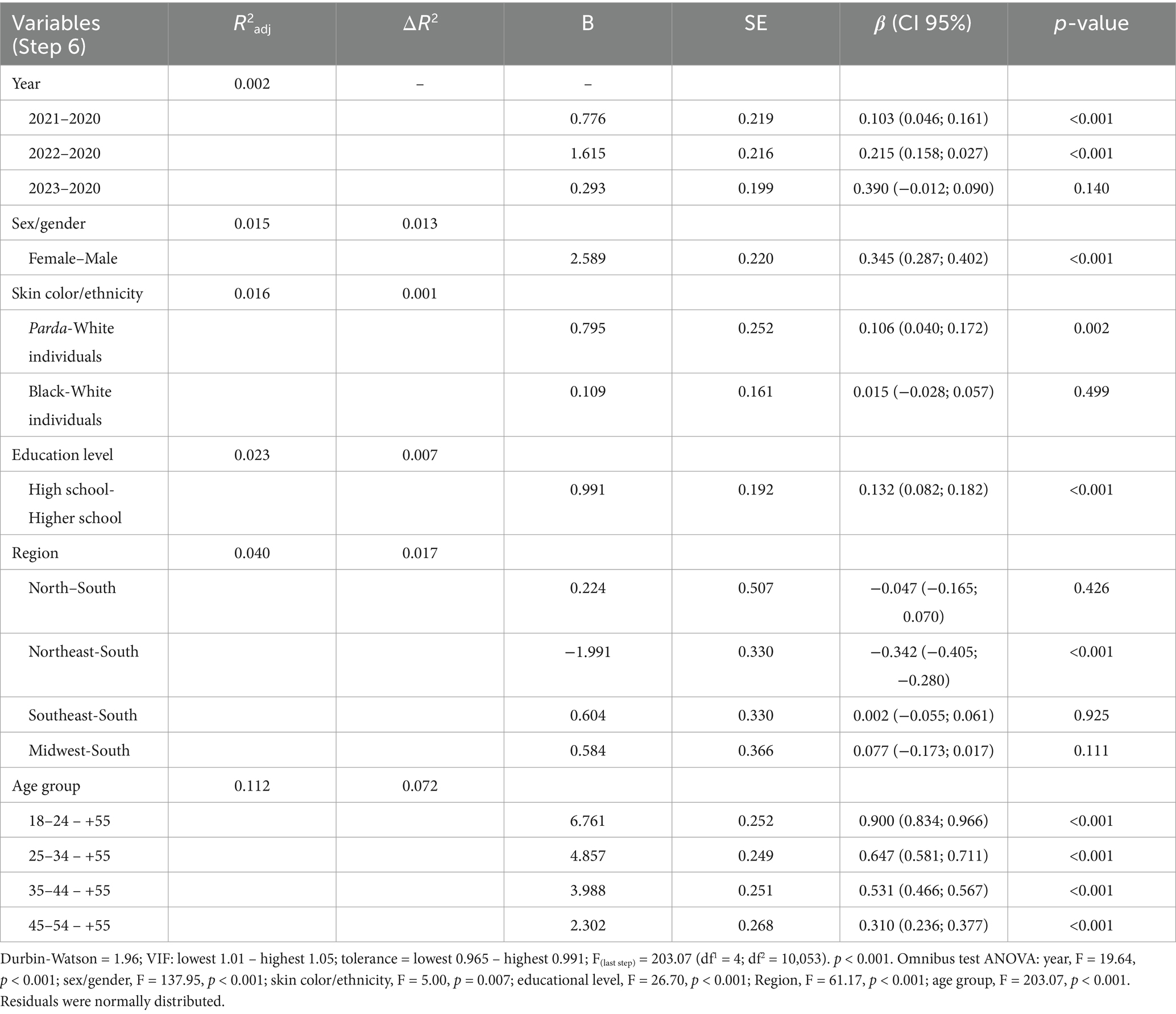
Table 5. Linear regression to the symptomatology of depression, PHQ-9, Brazil (cross-sectional data from 2020 to 2023, n = 10,069).
Considering the total explained variance of the final model (R2 converted to a percentage; 11.2%), the highest individual explained variance was related to age group, accounting for 7.2%. Skin color/ethnicity was the least powerful predictor (0.1%). In the middle were region (1.7%), education level (0.7%), sex/gender (1.3%), and year (0.2%) (Table 5).
The adjusted logistic regression was based on the binomial outcome of the PHQ-9 (score > 10 for the presence of significant depressive symptomatology at the screening level). The sixth block showed that all variables remained statistically significant (p < 0.001), with at least one categorical group showing statistical significance when contrasting has or not depression symptoms. The explained variance ranged from 0.012 (1.2%) in the first block to 0.127 (12.7%) in the last one. Within the variables, there were some exceptions: Black and White individuals (p = 0.599), and the regions North, Southeast, and Midwest versus South (p = 0.180, 0.580, and 0.138, respectively) did not show statistical significance (p > 0.05). All the other comparisons had a p-value less than 0.05. Table 6 displays the results, adjusted Odds Ratios (ORadj), and other indices of the logistic regression.
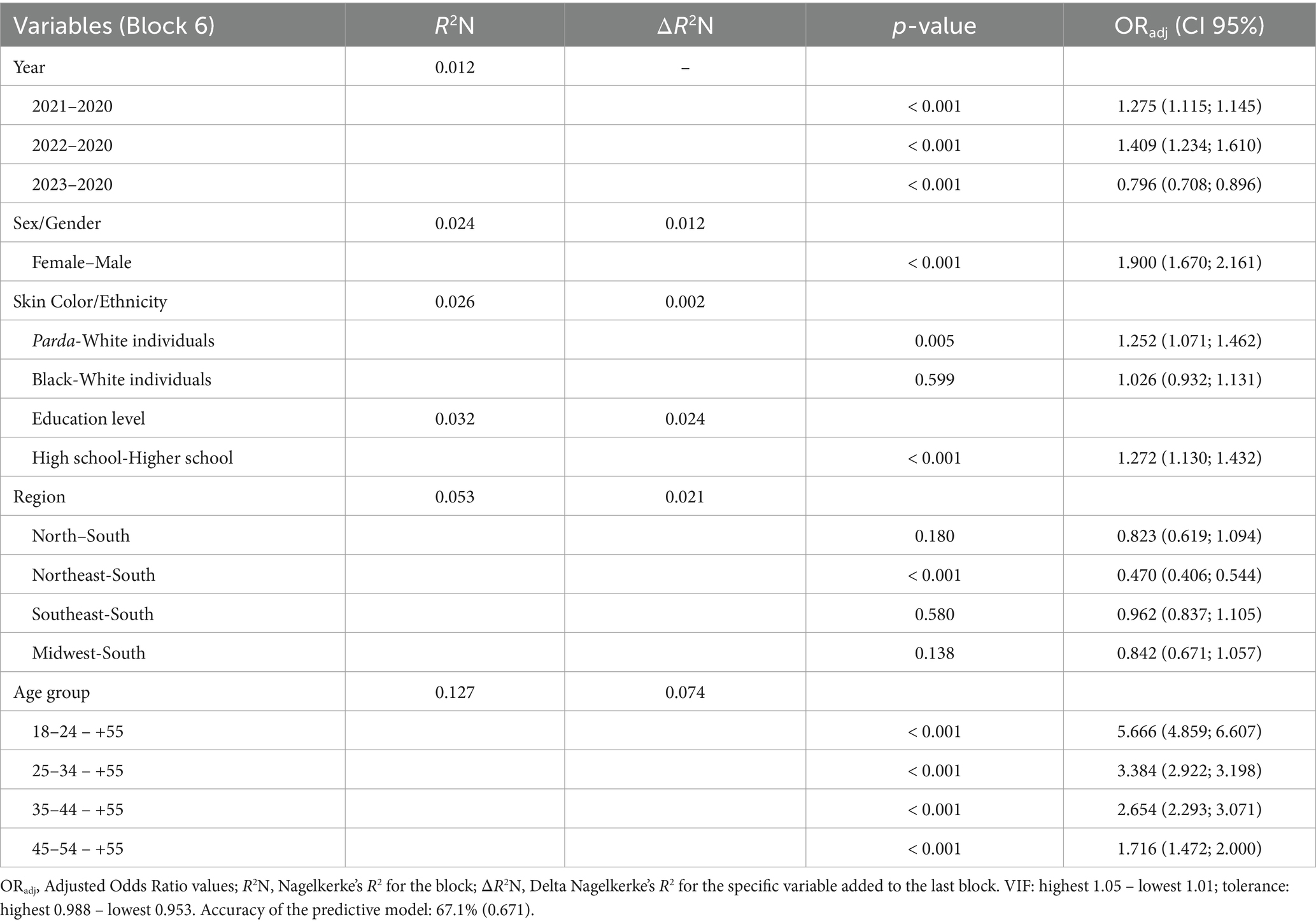
Table 6. Logistic regression to the symptomatology of depression, PHQ-9, Brazil (cross-sectional data from 2020 to 2023, n = 10,069).
2020 was the reference group, and all three other years presented significant differences as follows: 2021 and 2023 were more prone to have more cases of depressive symptomatology (ORadj = 1.275 [27.5%] and 1.409 [40.9%], respectively; p < 0.001). When comparing 2023 to 2020, there was a decrease in the prevalence of depressive symptomatology of around 20% (ORadj = 0.796; p = 0.140). Females were had almost two times greater prevalence of depressive symptomatology than males (ORadj = 1.900 [90.0%]; p < 0.001). Pardos individuals showed more likelihood of those with symptoms of depression (ORadj = 1.252 [25.2%]; p = 0.002) compared to White individuals. People who self-reported having only a high school education had a 27.2% (ORadj = 1.272; p < 0.001) higher chance of being part of the depression group. The only significant regional difference was between Northeast and South; the former had almost half the chance of the latter (ORadj = 0.470; p < 0.001). Age group had a progressive increase of top-down chances (from ORadj = 1.716 to 5.666; all contrasts at p < 0.001): the younger the strata, the higher the chances of being part of the group with depressive symptomatology (Table 6).
The Delta R2 of Nagelkerke indices arranged in descending order of importance with the percentage of individual explained variance by variable demonstrated age group as the most powerful (7.4%), followed by education level (2.4%), region (2.1%), sex/gender and Year (both 1.2%), and skin color/ethnicity (0.2%).
This study aimed to investigate different aspects related to the instrument, measure, and indicators of depression in the Brazilian population during the COVID-19 pandemic years of 2020, 2021, 2022, and 2023. We also assessed validity of the PHQ-9 by analyzing the internal structure of the measure (CFA and invariance analysis) and characterized the sample based on sociodemographic variables. This investigation sought to standardize PHQ-9 to establish cut score based on the obtained sample. Parameters of social distribution were then presented to estimate greater vulnerability to screening diagnoses.
Considering parameters suggested by Kroenke et al. (2001), over 60% of the sample had a positive screening diagnosis for depression, meaning that six out of every ten individuals exhibited depressive symptoms. The presence of depressive symptoms tends to be associated with functional impairment, reduced quality of life, and a higher risk of mortality (Ribeiro et al., 2020), in addition to an increased risk of suicide (Richie et al., 2021). This trend was found in studies on depression in Brazilian samples (Barros et al., 2020; Pereira-Ávila et al., 2021). Similar results were observed in studies from other countries as well (Choi et al., 2020; Clarke-Deelder et al., 2022; Fanaj and Mustafa, 2021). In comparison, a lower occurrence of depression was noted in research conducted before the pandemic (Martins-Monteverde et al., 2019; Nunes et al., 2022). Therefore, detecting that 60% of the participants in this study exhibited potential vulnerability to depression underscores indicating the need to monitor mental health outcomes in the post-pandemic period and to develop effective interventions to address current symptoms (Cataldo et al., 2023).
Similar to previous studies, we confirmed that the PHQ-9 exhibits a unidimensional structure (Fonseca-Pedrero et al., 2023; Mwangi et al., 2020; Pranckeviciene et al., 2022). This finding corroborates a previous investigation (Nunes and Faro, 2022) of the dynamics of the phenomenon throughout the pandemic. The aim was to expand the repertoire of statistical analyses to present greater robustness of the evidence for the validity of the instrument by standardizing the PHQ-9 scores and including other variables of interest in multi-group CFA (year, geographic region, skin color, and age). This investigation confirms the single-factor structure of the measure but includes a larger sample and temporal scope (different years of the pandemic). It is important to note that we did not aim to perform comparisons between CFA models (alternative factor structures) in the current study. We adopted the unidimensional structure, which has been used abroad (i.e., Bianchi et al., 2022; Boothroyd et al., 2019), including recent studies during the COVID-19 pandemic (i.e., Choi et al., 2020; Fukase et al., 2021; Kotabagi et al., 2020; Magalhaes et al., 2021; Palgi et al., 2020; Peretti-Watel et al., 2020; Sekimitsu et al., 2022; Stocker et al., 2021). However, it’s worth noting that there is no consensus on the ideal factor structure (e.g., two-factor structure, Lamela et al., 2020; four-factor structure, Tseng et al., 2024). We hope this decision can support direct comparisons between data from Brazil and other countries regarding the pandemic.
One of the innovations of this study was the standardization of PHQ-9 to establish cut scores to assess the severity levels of depressive symptoms. The suggested cut scores were established based on the social distribution of the PHQ-9; thus, it is not an analysis of criterion validity evidence. The establishment of cut scores and determination of the T score allow for the parameterization of the distribution of scores of this measure in other contexts as well as enabling the comparison of different research scenarios. For example, it would be possible to track the evolution of symptomatology over time at different points after the pandemic. The cut scores were established as follows: very low (score 0 to 6), low (score 7 to 13), moderate (score 14 to 19), high (score 20 to 23), and very high (score > 24). Consequently, it would be possible to map severity levels and identify associated vulnerabilities in different contexts. This approach enables comparisons with other regions or even other countries considering the diversity of coping responses adopted throughout the COVID-19 crisis.
An overview on the findings shows that the sex, skin color, age, education level, and year were predictors of depressive symptoms. Females, those who self-identified as Pardo, younger individuals, and those with education up to high school level had higher scores. The years 2021 and 2022 were more likely to be associated with an increase in depressive symptomatology.
Individual and social sex differences in depression occurrence are among the most robust and consistent findings in health Psychology research and represent a significant concern for healthcare professionals and researchers (Eid et al., 2019). As with other studies, we found no significant differences during the pandemic (Bucciarelli et al., 2022; Cha et al., 2022; Jeong et al., 2023). The findings of this investigation add valuable information and substantiate sex differences concerning concerns during COVID-19, prioritizing assessing females for depressive symptomatology (Ausín et al., 2021). Other research conducted during the pandemic indicated that women are among the most psychologically affected groups, demonstrating that the psychological impact during the COVID-19 outbreak was greater in this group, although men were also affected (Flentje et al., 2020). Since the early studies on the psychological effects of the pandemic, women have been found to be more affected with greater negative alterations in cognition or mood than men (Rania and Coppola, 2021). One possible explanation could be that women might be more susceptible to depression risk factors and more susceptible to the negative effects of social loneliness (Liu et al., 2020). Women might also perceive the pandemic period as more threatening and feel they lack sufficient resources to cope with the situation (Flentje et al., 2020). Regarding social factors, the pandemic context has reinforced structural gender inequality and differences in the roles played by men and women, which is a possible explanatory factor in understanding women’s greater vulnerability to depressive symptoms (Kolakowsky-Hayner et al., 2021). It is worth noting that men often omit their symptoms of depression due to the fear that it may affect their masculinity, resulting in a potential underestimation of the prevalence and underdiagnosis of depression in this group (Shi et al., 2021). Therefore, gender disparities reiterate a crucial public health concern, emphasizing the importance of prioritizing psychological support measures for more vulnerable groups.
Younger individuals were also more susceptible to depression during the pandemic, corroborating other findings in the literature (Robb et al., 2020; Varma et al., 2021). This finding aligns with previous studies on COVID-19-related effects on mental health across different age groups, where younger individuals seem to be at higher risk of increased depression compared to older adults (Haigh et al., 2018; Weinberger et al., 2018). Evidence indicated that depressive symptoms tend to be higher in younger adults, decreasing through mid-adulthood, and increasing again in older age (Hargrove et al., 2020). The trajectory of the disease became more prominent throughout life due to the severity of symptoms among young adults. In other words, the presence of higher levels of depression during this life stage was a contributing factor to the course of the disorder in other stages of development. Some explanations suggest that older adults are more resilient to adversities, worry less, and possess superior emotional regulation and coping strategies (Liu et al., 2022).
The years 2021 and 2022 had a higher likelihood of presenting elevated depression scores, consistent with other investigations (Hajek et al., 2022; Rudenstine et al., 2022). Despite advancements in dealing with COVID-19 and the increasing, albeit uneven, availability of vaccines, 2021 was the deadliest year of the pandemic worldwide. Approximately 3.9 million deaths occurred in 2021, accounting for nearly half of all COVID-19 deaths from 2020 to 2022. Brazil followed this global trend, with the year 2021 being the deadliest period of the pandemic in the country, which could help to explain the increase in mental health outcomes, including levels of depression. The years 2021 and 2023 were more likely to have more cases of depression. These results suggest a delayed effect of the psychological impacts of the pandemic. Given that it is a chronic stressor event, it is expected that different adaptive responses may be established later, considering the adaptive wear and tear experienced in the preceding pandemic years (Park et al., 2021).
Lower levels of education have been associated with depression occurrence within (Peng et al., 2020; Song et al., 2021) and before (Nunes et al., 2022; Lotfaliany et al., 2018) the pandemic period. Our findings corroborate these studies as participants with up to a high school education were more vulnerable to depressive symptomatology. One possible explanation is that individuals with higher education may perceive and cope with the pandemic’s impact more rationally, favoring adaptation compared to those with lower levels of education (Song et al., 2021). Furthermore, higher education level is likely to provide individuals with social and economic resources to cope with the pandemic whereas lower education levels eventually limit access to social and economic resources, which puts those at a higher risk (Abrams and Szefler, 2020). Individuals identifying as Pardo (mixed race) had greater depressive symptomatology. Another study conducted in Brazil found similar results where individuals identifying as Pardo had a 23% higher prevalence of symptoms than those who identified as White individuals (Santos et al., 2021). Literature suggests that non-White populations are more likely to suffer the impacts of the pandemic due to historical neglect resulting in greater social and psychological vulnerability (Dickinson et al., 2021). Our results indicate the same.
Individuals from the Northeast region were more vulnerable to depression compared to those from the South region. Although there is no direct explanation in the literature for this association (region x diagnosis), this finding appears to align with the relationship between depression and social and economic inequalities. A study on the effects of COVID-19 in the Northeast region suggested that despite the implementation of public health measures, the crisis exacerbated existing inequalities in the region leading to not only a significant number of cases and deaths, but also an increase in poverty and the growth of racial and ethnic disparities (Kerr et al., 2020). Thus, such scenario is a condition that influences the occurrence of depression (Proto and Quintana-Domeque, 2021).
Clinical implications of this investigation can be significant for public mental health services in Brazil and other similar countries, such as Low- and Middle-Income Countries (LMICs), particularly in the context of ongoing and future pandemic crises. Our findings confirm the suitability of the PHQ-9 as a reliable instrument, and its standardization for assessing depressive symptoms across diverse populations and time points during the COVID-19 pandemic revealed a relevant portrait. By identifying specific sociodemographic predictors, the study also helps to provide critical insights focused on the groups that showed higher vulnerability to significant depression symptoms. For instance, this information can guide the development of targeted interventions, such as mental health campaigns, policies, and support programs aimed at addressing these vulnerabilities (Arias de la Torre et al., 2023; Lund, 2023; Mughal et al., 2023; Terman et al., 2023). Furthermore, the establishment of normative cut scores for depressive symptom severity enables more accurate monitoring and comparison of mental health trends over time, facilitating early identification and treatment (GBD 2019 Mental Disorders Collaborators, 2022; Lattie et al., 2022; Shevlin et al., 2022; Witteveen et al., 2023). These insights highlight the need for integrating robust mental health strategies into broader public health responses to mitigate the psychological impact of health crises in the face of future global health challenges.
A question to consider is what factors may contribute to the maintenance of depressive symptoms within the context of the COVID-19 pandemic. Evidence from studies highlights the importance of dysfunctional coping strategies, such as perseveration, which includes repetitive behaviors like excessive checking, constant worrying, and monitoring driven by fear or perceived threats related to COVID-19 (Mansueto et al., 2022). Additionally, psychological inflexibility, which impairs individuals’ ability to adapt to challenging circumstances and regulate their emotional responses, has been linked to increased severity of depressive symptoms (Mansueto et al., 2024). Therefore, such behavioral, emotional, and cognitive patterns underscore how maladaptive responses to pandemic-related stressors can sustain or exacerbate depressive symptoms, emphasizing the need for targeted interventions.
Limitations of this study include a non-probabilistic and convenience-based sample design despite extensive geographical coverage. As such, it is not possible to generalize to the Brazilian population especially with the majority of sample being predominantly adult females with a higher level of education (completed or not) from the Northeast and Southeast regions of the country. The findings of this study provide no insights to other populations that are not adults, such as children, adolescents, or the elderly. Other limitations concern the fact that respondents were invited to participate in the research through social networks, which probably implies a reduced number of individuals over 60 years old in the sample, as the majority of the elderly population does not use social media platforms as younger generations. It should be also noted that the variable sex/gender was lastly used with only two groups (men and women). This may restrict the generalization of the results under a broader gender diversity, as the experiences and perspectives of individuals with non-binary, transgender, or other groups were not evaluated.
Future research should replicate this study with a more diversified and representative sample of the Brazilian population. Furthermore, another point require attention; for example, prior health issues such as mental health problems or pharmacological treatment, and other life events that could influence the presence of depressive symptoms were not explored. It is recommended that future studies address these gaps to map other aspects that assist in better understanding the occurrence of depression.
Finally, the use of PHQ-9 to measure depressive symptomatology in Brazil is recommended as it is a short instrument, easy to understand, apply, and score. The prevalence of depressive symptomatology was considered high overall and consistent with the varying impact of pandemic on the psychological adjustment in the general population by age, sex, and education level. Based on the assessment of PHQ-9 normative data, we believe is possible to monitor its social distribution and dynamic changes in the coming years. This study adds novel findings regarding the predictive ability to monitor these changes over time and prevent it from fading into partial, perhaps traumatic, resolution without new adaptive skills developed for future crises. It also has present implication considering the COVID-19 pandemic is still ongoing in 2023, albeit attenuated. Epidemiological projections predict new pandemics will come even if not on the same scale. Given the magnitude of these findings from a mental health perspective, future studies should ask: (a) What have we learned from dealing with the COVID-19 pandemic? and (b) Are we prepared for the next one or at least beginning to prepare?
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Brazilian Research Ethics Committee with Human Subjects (National Council of Ethics and Research [CONEP], no. 3.955.180). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
AF: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. DN: Writing – original draft, Writing – review & editing, Formal analysis, Investigation, Methodology, Validation. DF: Writing – original draft, Writing – review & editing, Formal analysis, Supervision, Validation, Visualization.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by Coordination of Superior Level Staff Improvement (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brazil (CAPES)) – Finance Code 001 and National Council for Scientific and Technological Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico – CNPq). The funding source was not involved in the study design, data collection, data analysis, or in any other aspect of this project.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abrams, E. M., and Szefler, S. J. (2020). COVID-19 and the impact of social determinants of health. Lancet Respir. Med. 8, 659–661. doi: 10.1016/S2213-2600(20)30234-4
Alhakami, A., Salem, V., Alateeq, D., Nikčević, A. V., Marci, T., Palmieri, S., et al. (2023). The Arab COVID-19 anxiety syndrome scale (C-19ASS): COVID-19 anxiety syndrome and psychological symptoms in the Saudi Arabian population. Clin. Psychol. Psychother. 30, 1083–1094. doi: 10.1002/cpp.2860
Arias de la Torre, J., Vilagut, G., Ronaldson, A., Bakolis, I., Dregan, A., Navarro-Mateu, F., et al. (2023). Reconsidering the use of population health surveys for monitoring of mental health. JMIR Public Health Surveill. 9:e48138. doi: 10.2196/48138
Ashby, J. S., Rice, K. G., Kira, I. A., and Davari, J. (2022). The relationship of COVID-19 traumatic stress, cumulative trauma, and race to posttraumatic stress disorder symptoms. J. Community Psychol. 50, 2597–2610. doi: 10.1002/jcop.22762
Aslan, J., Cova, F., Saldivia, S., Bustos, C., Inostroza, C., Rincón, P., et al. (2020). Psychometric properties of the patient health questionnaire-9 in elderly Chilean primary care users. Front. Psych. 11:555011. doi: 10.3389/fpsyt.2020.555011
Ausín, B., González-Sanguino, C., Castellanos, M. Á., and Muñoz, M. (2021). Gender-related differences in the psychological impact of confinement as a consequence of COVID-19 in Spain. J. Gend. Stud. 30, 29–38. doi: 10.1080/09589236.2020.1799768
Barros, M. B. D. A., Lima, M. G., Malta, D. C., Szwarcwald, C. L., Azevedo, R. C. S. D., Romero, D., et al. (2020). Report on sadness/depression, nervousness/anxiety and sleep problems in the Brazilian adult population during the COVID-19 pandemic. Epidemiologia e Serviços de Saúde 29, 1–12. doi: 10.1590/S1679-49742020000400018
Bianchi, R., Verkuilen, J., Toker, S., Schonfeld, I. S., Gerber, M., Brähler, E., et al. (2022). Is the PHQ-9 a unidimensional measure of depression? A 58,272-participant study. Psychol. Assess. 34, 595–603. doi: 10.1037/pas0001124
Boothroyd, L., Dagnan, D., and Muncer, S. (2019). PHQ-9: one factor or two? Psychiatry Res. 271, 532–534. doi: 10.1016/j.psychres.2018.12.048
Brailovskaia, J., Cosci, F., Mansueto, G., and Margraf, J. (2021). The relationship between social media use, stress symptoms and burden caused by coronavirus (COVID-19) in Germany and Italy: a cross-sectional and longitudinal investigation. J. Affect. Disord. Rep. 3:100067. doi: 10.1016/j.jadr.2020.100067
Breslau, J., Finucane, M. L., Locker, A. R., Baird, M. D., Roth, E. A., and Collins, R. L. (2021). A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev. Med. 143:106362. doi: 10.1016/j.ypmed.2020.106362
Bucciarelli, V., Nasi, M., Bianco, F., Seferovic, J., Ivkovic, V., Gallina, S., et al. (2022). Depression pandemic and cardiovascular risk in the COVID-19 era and long COVID syndrome: gender makes a difference. Trends Cardiovasc. Med. 32, 12–17. doi: 10.1016/j.tcm.2021.09.009
Cataldo, I., Novotny, D., Carollo, A., and Esposito, G. (2023). Mental health in the post-lockdown scenario: a scientometric investigation of the main thematic trends of research. Int. J. Environ. Res. Public Health 20:6310. doi: 10.3390/ijerph20136310
Cha, W. T., Joo, H. J., Park, Y. S., Park, E. C., and Kim, S. Y. (2022). Depression before and during-COVID-19 by gender in the Korean population. Int. J. Environ. Res. Public Health 19:3477. doi: 10.3390/ijerph19063477
Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. 14, 464–504. doi: 10.1080/10705510701301834
Cheung, G. W., and Rensvold, R. B. (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. 9, 233–255. doi: 10.1207/S15328007SEM0902_5
Choi, E. P. H., Hui, B. P. H., and Wan, E. Y. F. (2020). Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 17:3740. doi: 10.3390/ijerph17103740
Clarke-Deelder, E., Rokicki, S., McGovern, M. E., Birabwa, C., Cohen, J. L., Waiswa, P., et al. (2022). Levels of depression, anxiety, and psychological distress among Ugandan adults during the first wave of the COVID-19 pandemic: cross-sectional evidence from a mobile phone-based population survey. Glob. Ment. Health 9, 274–284. doi: 10.1017/gmh.2022.28
Costantini, L., Pasquarella, C., Odone, A., Colucci, M. E., Costanza, A., Serafini, G., et al. (2021). Screening for depression in primary care with patient health Questionnaire-9 (PHQ-9): a systematic review. J. Affect. Disord. 279, 473–483. doi: 10.1016/j.jad.2020.09.131
Demertzis, N., and Eyerman, R. (2020). COVID-19 as cultural trauma. Am. J. Cult. Sociol. 8, 428–450. doi: 10.1057/s41290-020-00112-z
Deng, J., Li, T., Wang, J., and Teng, L. (2021). Longitudinal influence of COVID-19-related stress on sexual compulsivity symptoms in Chinese undergraduates. BMC Psychiatry. 21:376. doi: 10.1186/s12888-021-03369-x
Dettmann, L. M., Adams, S., and Taylor, G. (2022). Investigating the prevalence of anxiety and depression during the first Covid-19 lockdown in the United Kingdom: systematic review and meta-analyses. Br. J. Clin. Psychol. 61, 757–780. doi: 10.1111/bjc.12360
Dickinson, K. L., Roberts, J. D., Banacos, N., Neuberger, L., Koebele, E., Blanch-Hartigan, D., et al. (2021). Structural racism and the COVID-19 experience in the United States. Health. Security 19:S-14. doi: 10.1089/hs.2021.0031
Eid, R. S., Gobinath, A. R., and Galea, L. A. (2019). Sex differences in depression: insights from clinical and preclinical studies. Prog. Neurobiol. 176, 86–102. doi: 10.1016/j.pneurobio.2019.01.006
Esterwood, E., and Saeed, S. A. (2020). Past epidemics, natural disasters, COVID19, and mental health: learning from history as we deal with the present and prepare for the future. Psychiatry Q. 91, 1121–1133. doi: 10.1007/s11126-020-09808-4
Ettman, C. K., Fan, A. Y., Subramanian, M., Adam, G. P., Goicoechea, E. B., Abdalla, S. M., et al. (2023). Prevalence of depressive symptoms in US adults during the COVID-19 pandemic: a systematic review. SSM Popul. Health 21:101348. doi: 10.1016/j.ssmph.2023.101348
Fanaj, N., and Mustafa, S. (2021). Depression measured by PHQ-9 in Kosovo during the COVID-19 outbreak: an online survey. Psychiatr. Danub. 33, 95–100. doi: 10.24869/psyd.2021.95
Flentje, A., Obedin-Maliver, J., Lubensky, M. E., Dastur, Z., Neilands, T., and Lunn, M. R. (2020). Depression and anxiety changes among sexual and gender minority people coinciding with onset of COVID-19 pandemic. J. Gen. Intern. Med. 35, 2788–2790. doi: 10.1007/s11606-020-05970-4
Fonseca-Pedrero, E., Díez-Gómez, A., Pérez-Albéniz, A., Al-Halabí, S., Lucas-Molina, B., and Debbané, M. (2023). Youth screening depression: validation of the patient health Questionnaire-9 (PHQ-9) in a representative sample of adolescents. Psychiatry Res. 328:115486. doi: 10.1016/j.psychres.2023.115486
Fukase, Y., Ichikura, K., Murase, H., and Tagaya, H. (2021). Depression, risk factors, and coping strategies in the context of social dislocations resulting from the second wave of COVID-19 in Japan. BMC Psychiatry 21, 33–39. doi: 10.1186/s12888-021-03047-y
Gao, X., and Liu, Z. (2024). Analyzing the psychometric properties of the PHQ-9 using item response theory in a Chinese adolescent population. Ann. General Psychiatry 23:7. doi: 10.1186/s12991-024-00492-3
GBD 2019 Mental Disorders Collaborators (2022). Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry 9, 137–150. doi: 10.1016/S2215-0366(21)00395-3
Gorenko, J. A., Moran, C., Flynn, M., Dobson, K., and Konnert, C. (2021). Social isolation and psychological distress among older adults related to COVID-19: a narrative review of remotely-delivered interventions and recommendations. J. Appl. Gerontol. 40, 3–13. doi: 10.1177/0733464820958550
Gradidge, S., Yap, W. M., Liem, A., and Dass, G. (2023). Taking on the “new normal”: emerging psychologist' reflections on the COVID-19 pandemic. J. Humanit. Appl. Soc. Sci. 5, 144–157. doi: 10.1108/JHASS-08-2022-0101
Grineski, S. E., Morales, D. X., Collins, T. W., Nadybal, S., and Trego, S. (2024). Anxiety and depression among US college students engaging in undergraduate research during the COVID-19 pandemic. J. Am. Coll. Health. 72, 20–30. doi: 10.1080/07448481.2021.2013237
Haigh, E. A., Bogucki, O. E., Sigmon, S. T., and Blazer, D. G. (2018). Depression among older adults: a 20-year update on five common myths and misconceptions. Am. J. Geriatr. Psychiatry 26, 107–122. doi: 10.1016/j.jagp.2017.06.011
Haight, B. L., Peddie, L., Crosswell, A. D., Hives, B. A., Almeida, D. M., and Puterman, E. (2023). Combined effects of cumulative stress and daily stressors on daily health. Health Psychol. 42, 325–334. doi: 10.1037/hea0001281
Hair, J., Black, W., Babin, B., Anderson, R., and Tatham, R. (2014). Multivariate data analysis. Upper Saddle River, NJ: Pearson New International Edition/Prentice Hall.
Hajek, A., Sabat, I., Neumann-Böhme, S., Schreyögg, J., Barros, P. P., Stargardt, T., et al. (2022). Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the European COvid survey (ECOS). J. Affect. Disord. 299, 517–524. doi: 10.1016/j.jad.2021.12.029
Hargrove, T. W., Halpern, C. T., Gaydosh, L., Hussey, J. M., Whitsel, E. A., Dole, N., et al. (2020). Race/ethnicity, gender, and trajectories of depressive symptoms across early-and mid-life among the add health cohort. J. Racial Ethn. Health Disparities 7, 619–629. doi: 10.1007/s40615-019-00692-8
Hernández, A., Hidalgo, M. D., Hambleton, R. K., and Gómez Benito, J. (2020). International test commission guidelines for test adaptation: a criterion checklist. Psicothema 32, 390–398. doi: 10.7334/psicothema2019.306
Hettich, N., Entringer, T. M., Kroeger, H., Schmidt, P., Tibubos, A. N., Braehler, E., et al. (2022). Impact of the COVID-19 pandemic on depression, anxiety, loneliness, and satisfaction in the German general population: a longitudinal analysis. Soc. Psychiatry Psychiatr. Epidemiol. 57, 2481–2490. doi: 10.1007/s00127-022-02311-0
Hiscott, J., Alexandridi, M., Muscolini, M., Tassone, E., Palermo, E., Soultsioti, M., et al. (2020). The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 53, 1–9. doi: 10.1016/j.cytogfr.2020.05.010
Jeong, Y. J., Wi, Y. M., Park, H., Lee, J. E., Kim, S. H., and Lee, K. S. (2023). Current and emerging knowledge in COVID-19. Radiology 306:e222462. doi: 10.1148/radiol.222462
Kazlauskas, E., and Quero, S. (2020). Adjustment and coronavirus: how to prepare for COVID-19 pandemic-related adjustment disorder worldwide? Psychol. Trauma Theory Res. Pract. Policy 12, S22–S24. doi: 10.1037/tra0000706
Kerr, L., Kendall, C., Silva, A. A. M. D., Aquino, E. M. L., Pescarini, J. M., Almeida, R. L. F. D., et al. (2020). COVID-19 in Northeast Brazil: achievements and limitations in the responses of the state governments. Ciênc. Saúde Colet. 25, 4099–4120. doi: 10.1590/1413-812320202510.2.28642020
Kira, I. A., Shuwiekh, H. A., Ashby, J. S., Elwakeel, S. A., Alhuwailah, A., Sous, M. S. F., et al. (2021). The impact of COVID-19 traumatic stressors on mental health: is COVID-19 a new trauma type. Int. J. Ment. Heal. Addict. 21, 51–70. doi: 10.1007/s11469-021-00577-0
Kolakowsky-Hayner, S. A., Goldin, Y., Kingsley, K., Alzueta, E., Arango-Lasprilla, J. C., Perrin, P. B., et al. (2021). Psychosocial impacts of the COVID-19 quarantine: a study of gender differences in 59 countries. Medicina 57:789. doi: 10.3390/medicina57080789
Kotabagi, P., Fortune, L., Essien, S., Nauta, M., and Yoong, W. (2020). Anxiety and depression levels among pregnant women with COVID-19. Acta Obstet. Gynecol. Scand. 99, 953–954. doi: 10.1111/aogs.13928
Kroenke, K., Spitzer, R. L., and Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Lakhan, R., Agrawal, A., and Sharma, M. (2020). Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J. Neurosci. Rural Pract. 11, 519–525. doi: 10.1055/s-0040-1716442
Lamela, D., Soreira, C., Matos, P., and Morais, A. (2020). Systematic review of the factor structure and measurement invariance of the patient health questionnaire-9 (PHQ-9) and validation of the Portuguese version in community settings. J. Affect. Disord. 276, 220–233. doi: 10.1016/j.jad.2020.06.066
Lattie, E. G., Stiles-Shields, C., and Graham, A. K. (2022). An overview of and recommendations for more accessible digital mental health services. Nat. Rev. Psychol. 1, 87–100. doi: 10.1038/s44159-021-00003-1
Layton, H., Owais, S., Savoy, C. D., and Van Lieshout, R. J. (2021). Depression, anxiety, and mother-infant bonding in women seeking treatment for postpartum depression before and during the COVID-19 pandemic. J. Clin. Psychiatry. 82:35146. doi: 10.4088/JCP.21m13874
Lee, J. O., Kapteyn, A., Clomax, A., and Jin, H. (2021). Estimating influences of unemployment and underemployment on mental health during the COVID-19 pandemic: who suffers the most? Public Health 201, 48–54. doi: 10.1016/j.puhe.2021.09.038
Limbu, Y. B., Gautam, R. K., and Pham, L. (2022). The health belief model applied to COVID-19 vaccine hesitancy: a systematic review. Vaccine 10:973. doi: 10.3390/vaccines10060973
Liu, W., Yu, F., Geldsetzer, P., Yang, J., Wang, Z., Golden, T., et al. (2022). Prevalence of depression in China during the early stage of the COVID-19 pandemic: a cross-sectional study in an online survey sample. BMJ Open 12:e056667. doi: 10.1136/bmjopen-2021-056667
Liu, H., Zhang, M., Yang, Q., and Yu, B. (2020). Gender differences in the influence of social isolation and loneliness on depressive symptoms in college students: a longitudinal study. Soc. Psychiatry Psychiatr. Epidemiol. 55, 251–257. doi: 10.1007/s00127-019-01726-6
Lotfaliany, M., Bowe, S. J., Kowal, P., Orellana, L., Berk, M., and Mohebbi, M. (2018). Depression and chronic diseases: co-occurrence and communality of risk factors. J. Affect. Disord. 241, 461–468. doi: 10.1016/j.jad.2018.08.011
Lua, I., Freitas, K. S., Teixeira, J. R. B., Reichenheim, M. E., Almeida, M. M. G. D., and Araújo, T. M. D. (2022). Measurement of depression in the Brazilian population: validation of the patient health questionnaire (PHQ-8). Cad. Saude Publica 38:e00176421. doi: 10.1590/0102-311XEN176421
Lund, C. (2023). Global mental health and its social determinants: how should we intervene? Behav. Res. Ther. 169:104402. doi: 10.1016/j.brat.2023.104402
Maciel, G. P., da Costa, B. G. G., Bezerra, I. N., Silva, K. S., Lopes, I. E., de Castro, V. H. S., et al. (2023). Factors related to depressive symptoms during the second year of COVID-19 pandemic in Brazil: A cross-sectional study with adolescents. J. Pediatr. Nurs. 73, e534–e540. doi: 10.1016/j.pedn.2023.10.027
Magalhaes, E., Stoner, A., Palmer, J., Schranze, R., Grandy, S., Amin, S., et al. (2021). An assessment of mental health outcomes during the COVID-19 pandemic. Community Ment. Health J. 57, 1267–1277. doi: 10.1007/s10597-021-00876-9
Mahmud, S., Mohsin, M., Dewan, M. N., and Muyeed, A. (2023). The global prevalence of depression, anxiety, stress, and insomnia among general population during COVID-19 pandemic: a systematic review and meta-analysis. Trends Psychol. 31, 143–170. doi: 10.1007/s43076-021-00116-9
Mansueto, G., Lopes, F. L., Grassi, L., and Cosci, F. (2021). Impact of COVID-19 outbreak on Italian healthcare workers versus general population: results from an online survey. Clin. Psychol. Psychother. 28, 1334–1345. doi: 10.1002/cpp.2644
Mansueto, G., Palmieri, S., Marino, C., Caselli, G., Sassaroli, S., Ruggiero, G. M., et al. (2022). The Italian COVID-19 anxiety syndrome scale: investigation of the COVID-19 anxiety syndrome and its association with psychological symptoms in an Italian population. Clin. Psychol. Psychother. 29, 1972–1990. doi: 10.1002/cpp.2767
Mansueto, G., Ruggiero, G. M., and Palmieri, S. (2024). The relationship between COVID-19 fear, affective symptoms and well-being: the mediating role of psychological flexibility. J. Ration. Emot. Cogn. Behav. Ther. 42, 945–963. doi: 10.1007/s10942-024-00556-z
Martins-Monteverde, C. M. S., Baes, C. V. W., Reisdorfer, E., Padovan, T., Tofoli, S. M. D. C., and Juruena, M. F. (2019). Relationship between depression and subtypes of early life stress in adult psychiatric patients. Front. Psych. 10, 1–8. doi: 10.3389/fpsyt.2019.00019
McPherson, K. E., McAloney-Kocaman, K., McGlinchey, E., Faeth, P., and Armour, C. (2021). Longitudinal analysis of the UK COVID-19 psychological wellbeing study: trajectories of anxiety, depression and COVID-19-related stress symptomology. Psychiatry Res. 304:114138. doi: 10.1016/j.psychres.2021.114138
Moura, E. C., Cortez-Escalante, J., Cavalcante, F. V., Barreto, I. C. D. H. C., Sanchez, M. N., and Santos, L. M. P. (2022). Covid-19: evolução temporal e imunização nas três ondas epidemiológicas, Brasil, 2020–2022. Rev. Saúde Pública. 56:105. doi: 10.11606/s1518-8787.2022056004907
Mughal, S., Salmon, A., Churchill, A., Tee, K., Jaouich, A., and Shah, J. (2023). Guiding principles for implementing stepped Care in Mental Health: alignment on the bigger picture. Community Ment. Health J. 59, 1035–1042. doi: 10.1007/s10597-023-01116-y
Mwangi, P., Nyongesa, M. K., Koot, H. M., Cuijpers, P., Newton, C. R., and Abubakar, A. (2020). Validation of a Swahili version of the 9-item patient health questionnaire (PHQ-9) among adults living with HIV compared to a community sample from Kilifi, Kenya. J. Affect. Disord. Rep. 1:100013. doi: 10.1016/j.jadr.2020.100013
Nielsen, L. M., Gregersen Østergaard, L., Maribo, T., Kirkegaard, H., and Petersen, K. S. (2019). Returning to everyday life after discharge from a short-stay unit at the emergency department—a qualitative study of elderly patients’ experiences. Int. J. Qual. Stud. Health Well Being 14:1563428. doi: 10.1080/17482631.2018.1563428
Nii-Trebi, N. I., Mughogho, T. S., Abdulai, A., Tetteh, F., Ofosu, P. M., Osei, M. M., et al. (2023). Dynamics of viral disease outbreaks: a hundred years (1918/19–2019/20) in retrospect-loses, lessons and emerging issues. Rev. Med. Virol. 33:e2475. doi: 10.1002/rmv.2475
Nunes, D., and Faro, A. (2021). The role of self-efficacy, self-esteem and self-concept in depression in adolescents. Ciencias Psicológicas 15, 1–14. doi: 10.22235/cp.v15i2.2164
Nunes, D., and Faro, A. (2022). Factor structure, invariance analysis and social distribution of the patient health Questionnaire-9 (PHQ-9). Revista Iberoamericana de Diagnóstico y Evaluación-e Avaliação Psicológica 62, 37–49. doi: 10.21865/RIDEP62.1.04
Nunes, D., Menezes, M. S., and Faro, A. (2022). Rastreamento domiciliar da sintomatologia depressiva em Aracaju (Sergipe, brasil). Rev. Psicol. 31, 1–13. doi: 10.5354/0719-0581.2022.57478
Odero, S. A., Mwangi, P., Odhiambo, R., Mumbua Nzioka, B., Shumba, C., Ndirangu-Mugo, E., et al. (2023). Psychometric evaluation of PHQ–9 and GAD–7 among community health volunteers and nurses/midwives in Kenya following a nation-wide telephonic survey. Front. Psych. 14:1123839. doi: 10.3389/fpsyt.2023.1123839
Palgi, Y., Shrira, A., Ring, L., Bodner, E., Avidor, S., Bergman, Y., et al. (2020). The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 275, 109–111. doi: 10.1016/j.jad.2020.06.036
Park, C. L., Finkelstein-Fox, L., Russell, B. S., Fendrich, M., Hutchison, M., and Becker, J. (2021). Psychological resilience early in the COVID-19 pandemic: stressors, resources, and coping strategies in a national sample of Americans. Am. Psychol. 76, 715–728. doi: 10.1037/amp0000813
Peng, M., Mo, B., Liu, Y., Xu, M., Song, X., Liu, L., et al. (2020). Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID-19 outbreak. J. Affect. Disord. 275, 119–124. doi: 10.1016/j.jad.2020.06.035
Pereira-Ávila, F. M. V., Lam, S. C., Góes, F. G. B., Pereira-Caldeira, N. M. V., and Gir, E. (2021). Factors associated with symptoms of depression among older adults during the covid-19 pandemic. Texto Contexto Enferm. 30:e20200380. doi: 10.1590/1980-265X-TCE-2020-0380
Peretti-Watel, P., Alleaume, C., Léger, D., Beck, F., and Verger, P.COCONEL Group (2020). Anxiety, depression and sleep problems: a second wave of COVID-19. Gen. Psychiatr. 33:e100299. doi: 10.1136/gpsych-2020-100299
Piret, J., and Boivin, G. (2021). Pandemics throughout history. Front. Microbiol. 11:631736. doi: 10.3389/fmicb.2020.631736
Pranckeviciene, A., Saudargiene, A., Gecaite-Stonciene, J., Liaugaudaite, V., Griskova-Bulanova, I., Simkute, D., et al. (2022). Validation of the patient health questionnaire-9 and the generalized anxiety disorder-7 in Lithuanian student sample. PLoS One 17:e0263027. doi: 10.1371/journal.pone.0263027
Proto, E., and Quintana-Domeque, C. (2021). COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLoS One 16:e0244419. doi: 10.1371/journal.pone.0244419
Qian, Y., and Fan, W. (2024). Stressful life events and depressive symptoms during COVID‐19: A gender comparison. Br. J. Sociol. 75, 38–47. doi: 10.1111/1468-4446.13067
Rahman, M. A., Dhira, T. A., Sarker, A. R., and Mehareen, J. (2022). Validity and reliability of the patient health questionnaire scale (PHQ-9) among university students of Bangladesh. PLoS One 17:e0269634. doi: 10.1371/journal.pone.0269634
Rania, N., and Coppola, I. (2021). Psychological impact of the lockdown in Italy due to the COVID-19 outbreak: are there gender differences? Front. Psychol. 12:567470. doi: 10.3389/fpsyg.2021.567470
Reich, H., Rief, W., Brähler, E., and Mewes, R. (2018). Cross-cultural validation of the German and Turkish versions of the PHQ-9: an IRT approach. BMC Psychol. 6, 26–13. doi: 10.1186/s40359-018-0238-z
Reitsma, L., Boelen, P. A., de Keijser, J., and Lenferink, L. I. M. (2021). Online treatment of persistent complex bereavement disorder, posttraumatic stress disorder, and depression symptoms in people who lost loved ones during the COVID-19 pandemic: study protocol for a randomized controlled trial and a controlled trial. Eur. J. Psychotraumatol. 12:1987687. doi: 10.1080/20008198.2021.1987687
Renaud-Charest, O., Lui, L. M., Eskander, S., Ceban, F., Ho, R., Di Vincenzo, J. D., et al. (2021). Onset and frequency of depression in post-COVID-19 syndrome: a systematic review. J. Psychiatr. Res. 144, 129–137. doi: 10.1016/j.jpsychires.2021.09.054
Ribeiro, O., Teixeira, L., Araújo, L., Rodríguez-Blázquez, C., Calderón-Larrañaga, A., and Forjaz, M. J. (2020). Anxiety, depression and quality of life in older adults: trajectories of influence across age. Int. J. Environ. Res. Public Health 17:9039. doi: 10.3390/ijerph17239039
Richie, F. J., Bonner, J., Wittenborn, A., Weinstock, L. M., Zlotnick, C., and Johnson, J. E. (2021). Social support and suicidal ideation among prisoners with major depressive disorder. Arch. Suicide Res. 25, 107–114. doi: 10.1080/13811118.2019.1649773
Robb, C. E., De Jager, C. A., Ahmadi-Abhari, S., Giannakopoulou, P., Udeh-Momoh, C., McKeand, J., et al. (2020). Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: a survey of older adults in London, UK. Front. Psychiatry 11:591120. doi: 10.3389/fpsyt.2020.591120
Rudenstine, S., Schulder, T., Bhatt, K. J., McNeal, K., Ettman, C. K., and Galea, S. (2022). Long-COVID and comorbid depression and anxiety two years into the COVID-19 pandemic. Psychiatry Res. 317:114924. doi: 10.1016/j.psychres.2022.114924
Rufino, J. V., Rodrigues, R., Birolim, M. M., Girotto, E., Mesas, A. E., Martínez-Vizcaíno, V., et al. (2024). Analysis of the dimensional structure of the patient health Questionnaire-9 (PHQ-9) in undergraduate students at a public university in Brazil. J. Affect. Disord. 349, 158–164. doi: 10.1016/j.jad.2024.01.051
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., et al. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health 16, 1–11. doi: 10.1186/s12992-020-00589-w
Santos, K. M. R. D., Galvão, M. H. R., Gomes, S. M., Souza, T. A. D., Medeiros, A. D. A., and Barbosa, I. R. (2021). Depressão e ansiedade em profissionais de enfermagem durante a pandemia da COVID-19. Esc. Anna Nery. 25:e20200370. doi: 10.1590/2177-9465-EAN-2020-0370
Sekimitsu, S., Shweikh, Y., and Zebardast, N. (2022). Effect of visual impairment on depression and anxiety during the COVID-19 pandemic in the United States. Can. J. Ophthalmol. 59, e331–e337. doi: 10.1016/j.jcjo.2022.11.019
Shader, R. I. (2020). COVID-19 and depression. Clin. Ther. 42, 962–963. doi: 10.1016/j.clinthera.2020.04.010
Shaff, J., Kahn, G., and Wilcox, H. C. (2024). An examination of the psychometric properties of the patient health Questionnaire-9 (PHQ-9) in a multiracial/ethnic population in the United States. Front. Psych. 14:1290736. doi: 10.3389/fpsyt.2023.1290736
Shen, C., Smith, R. B., Heller, J., Spiers, A. D., Thompson, R., Ward, H., et al. (2024). Depression and anxiety in adolescents during the COVID-19 pandemic in relation to the use of digital technologies: Longitudinal cohort study. J. Med. Internet Res. 26:e45114. doi: 10.2196/45114
Shevlin, M., Butter, S., McBride, O., Murphy, J., Gibson-Miller, J., Hartman, T. K., et al. (2022). Measurement invariance of the patient health questionnaire (PHQ-9) and generalized anxiety disorder scale (GAD-7) across four European countries during the COVID-19 pandemic. BMC Psychiatry 22:154. doi: 10.1186/s12888-022-03787-5
Shi, P., Yang, A., Zhao, Q., Chen, Z., Ren, X., and Dai, Q. (2021). A hypothesis of gender differences in self-reporting symptom of depression: implications to solve under-diagnosis and under-treatment of depression in males. Front. Psych. 12:589687. doi: 10.3389/fpsyt.2021.589687
Smail, E., Schneider, K. E., DeLong, S. M., Willis, K., Arrington-Sanders, R., Yang, C., et al. (2021). Health beliefs and preventive behaviors among adults during the early COVID-19 pandemic in the United States: a latent class analysis. Prev. Sci. 22, 1013–1022. doi: 10.1007/s11121-021-01273-0
Smallwood, M. (Ed.). (2023). “COVID-19 versus past pandemics: What can we learn?” in The future of long COVID: A threatcasting approach (Cham: Springer Nature Switzerland), 57–75.
Song, S., Yang, X., Yang, H., Zhou, P., Ma, H., Teng, C., et al. (2021). Psychological resilience as a protective factor for depression and anxiety among the public during the outbreak of COVID-19. Front. Psychol. 11:618509. doi: 10.3389/fpsyg.2020.618509
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Stocker, R., Tran, T., Hammarberg, K., Nguyen, H., Rowe, H., and Fisher, J. (2021). Patient health questionnaire 9 (PHQ-9) and general anxiety disorder 7 (GAD-7) data contributed by 13,829 respondents to a national survey about COVID-19 restrictions in Australia. Psychiatry Res. 298:113792. doi: 10.1016/j.psychres.2021.113792
Suess, C., Maddock, J. E., Dogru, T., Mody, M., and Lee, S. (2022). Using the health belief model to examine travelers’ willingness to vaccinate and support for vaccination requirements prior to travel. Tour. Manag. 88:104405. doi: 10.1016/j.tourman.2021.104405
Sun, Y., Fu, Z., Bo, Q., Mao, Z., Ma, X., and Wang, C. (2020). The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry 20, 474–477. doi: 10.1186/s12888-020-02885-6
Terman, J. M., Rohan, K. J., Cruz, R. C., and Greenberger, E. (2023). Ultra-brief cognitive-behavioral therapy for routine primary care visits: feasibility and acceptability of a brief provider training workshop. Fam. Syst. Health 42, 559–569. doi: 10.1037/fsh0000862
The jamovi project. (2022). jamovi. Available at: https://www.jamovi.org
Tseng, V. W. S., Tharp, J. A., Reiter, J. E., Ferrer, W., Hong, D. S., Doraiswamy, P. M., et al. (2024). Identifying a stable and generalizable factor structure of major depressive disorder across three large longitudinal cohorts. Psychiatry Res. 333:115702. doi: 10.1016/j.psychres.2023.115702
Turna, J., Zhang, J., Lamberti, N., Patterson, B., Simpson, W., Francisco, A. P., et al. (2021). Anxiety, depression and stress during the COVID-19 pandemic: results from a cross-sectional survey. J. Psychiatr. Res. 137, 96–103. doi: 10.1016/j.jpsychires.2021.02.059
Urtasun, M., Daray, F. M., Teti, G. L., Coppolillo, F., Herlax, G., Saba, G., et al. (2019). Validation and calibration of the patient health questionnaire (PHQ-9) in Argentina. BMC Psychiatry 19, 1–10. doi: 10.1186/s12888-019-2262-9
Varma, P., Junge, M., Meaklim, H., and Jackson, M. L. (2021). Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 109:110236. doi: 10.1016/j.pnpbp.2020.110236
Weinberger, A. H., Gbedemah, M., Martinez, A. M., Nash, D., Galea, S., and Goodwin, R. D. (2018). Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol. Med. 48, 1308–1315. doi: 10.1017/S0033291717002781
Wilson, J. M., Lee, J., Fitzgerald, H. N., Oosterhoff, B., Sevi, B., and Shook, N. J. (2020). Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J. Occup. Environ. Med. 62, 686–691. doi: 10.1097/JOM.0000000000001962
Wisting, L., Johnson, S. U., Bulik, C. M., Andreassen, O. A., Rø, Ø., and Bang, L. (2021). Psychometric properties of the Norwegian version of the patient health Questionnaire-9 (PHQ-9) in a large female sample of adults with and without eating disorders. BMC Psychiatry 21, 6–11. doi: 10.1186/s12888-020-03013-0
Witteveen, A. B., Young, S. Y., Cuijpers, P., Ayuso-Mateos, J. L., Barbui, C., Bertolini, F., et al. (2023). COVID-19 and common mental health symptoms in the early phase of the pandemic: an umbrella review of the evidence. PLoS Med. 20:e1004206. doi: 10.1371/journal.pmed.1004206
Wu, D., Yang, T., Hall, D. L., Jiao, G., Huang, L., and Jiao, C. (2021). COVID-19 uncertainty and sleep: the roles of perceived stress and intolerance of uncertainty during the early stage of the COVID-19 outbreak. BMC Psychiatry 21:306. doi: 10.1186/s12888-021-03310-2
Keywords: depression, PHQ-9, psychometric properties, normative score assessment, social distribution, COVID-19
Citation: Faro A, Nunes D and Falk D (2025) Depressive symptomatology in Brazil: perspectives of statistical and psychometrics analyses of the PHQ-9 at four time-points (2020–2023) in the COVID-19 pandemic. Front. Psychol. 16:1440054. doi: 10.3389/fpsyg.2025.1440054
Received: 28 May 2024; Accepted: 23 January 2025;
Published: 05 February 2025.
Edited by:
Stefania Mancone, University of Cassino, ItalyReviewed by:
Giovanni Mansueto, University of Florence, ItalyCopyright © 2025 Faro, Nunes and Falk. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence:Andre Faro, YW5kcmUuZmFyby51ZnNAZ21haWwuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.