- 1Department of Neurodegeneration, Hertie Institute for Clinical Brain Research, University of Tübingen, Tübingen, Germany
- 2German Center for Neurodegenerative Diseases (DZNE), Tübingen, Germany
- 3Department of Neurology, University Hospital Schleswig-Holstein, Campus Kiel and Kiel University, Kiel, Germany
- 4Department of Psychiatry and Psychotherapy, University Hospital Tübingen, Tübingen, Germany
- 5German Center for Mental Health (DZPG), Partner Site, Tübingen, Germany
Introduction: Unipolar depression is a frequent psychiatric disorder and associated with cognitive and motor deficits. It is also a prodromal or risk marker for various neurodegenerative diseases. Little research has been done on the extent to which motor and cognitive deficits persist in remitted depressive episode, and to what extent these deficits can be progressive.
Methods: A total of 401 healthy subjects of the Tübingen TREND study aged between 50 and 80 years were examined over 6 years at intervals of 2 years. Of those, 81 had a positive history of unipolar depression (Dep+) and 320 had not (Dep-). We ruled out currently depressive participants. Mini-Mental-State Examination (MMSE), Consortium to Establish a Registry for Alzheimer’s disease (CERAD), the motor part of the Movement disorder society-revised version of the Unified Parkinson disease rating scale (MDS-UPDRS III), gait speed, and dual tasking parameters were compared between groups.
Results: Dep+ had lower gait velocity than Dep-. No significant change in parameters was found over the observed time.
Discussion: Reduced gait speed in Dep+ may have potential as a diagnostic and prognostic marker for Dep- if confirmed in further studies. The lack of progression of all studied parameters over 6 years specifically in Dep+ argues against a relevant potential of this approach to define prodromal neurodegenerative cohorts by history of depression.
Introduction
With a lifetime prevalence of 16%–20%, unipolar depressive disorder is one of the most common psychiatric conditions worldwide (Kessler et al., 2003; Jacobi et al., 2014; Maske et al., 2016). In 85%–94% of the cases it is associated with changes in cognitive performance, such as reduction of attention, executive function, and memory. These symptoms may persist beyond remission (Rovner et al., 1991; Doumas et al., 2012; Metzger et al., 2016). Unipolar depression is also associated with a 2–4-fold increased risk of developing (neurodegenerative) dementias and/or may be a prodromal symptom thereof (Byers and Yaffe, 2011; Kessing, 2012; Bennett and Thomas, 2014a). In addition, unipolar depressive disorder is associated with changes in motor performance, especially with a reduction of gait speed (Sloman et al., 1982; Metzger et al., 2016; Serrano-Checa et al., 2020; Hobert et al., 2023), and a prodromal marker of neurodegenerative diseases associated with motor dysfunction, particularly Parkinson disease (PD) (Lerche et al., 2014; Schrag et al., 2015; Del Din et al., 2019; Bareeqa et al., 2022; Lempriere, 2022).
However, to the best of our knowledge, whether depressive episodes lead to prolonged reductions in motor, especially gait speed, or cognitive performance beyond the acute depressive episode, has not been well investigated. This is particularly interesting as reduced gait speed in older adults is associated, among others, with increased risk of dementia, reduced independence of daily living (den Ouden et al., 2011; Artaud et al., 2015; Sanders et al., 2017; Binotto et al., 2018; Kamiya et al., 2018), increased hospitalization rate and increased mortality (Dumurgier et al., 2009; den Ouden et al., 2011; Studenski et al., 2011; Artaud et al., 2015). The aim of this 6 years longitudinal observational study was therefore to investigate various motor and cognitive parameters between participants with (Dep+) and without depressive episodes in their history (Dep-) over multiple assessments.
Materials and methods
Longitudinal TREND study and definition of the dataset used for the actual analysis
This is a sub-analysis from the still ongoing prospective longitudinal observational TREND study (Tübinger Erhebung von Risikofaktoren zur Erkennung von Neurodegeneration), conducted in the South of Germany. Approval for the study was obtained from the Ethics Committee of the Medical Faculty of Tübingen in 2009 (protocol number 90/2009BO2). A total of 1201 participants aged between 50 and 80 years were recruited from 2009 onwards and are re-assessed every 2 years (the study is still ongoing). Inclusion criteria were either the presence of hyposmia, rapid eye movement behavior disorder, and/or history of depressive episodes. In addition, healthy volunteers without any of these symptoms were included (Berg et al., 2015; Skorvanek et al., 2017). Exclusion criteria were relevant (other) neurological and psychiatric diseases, cognitive deficits, immobility (all as judged by the investigator), and taking neuroleptics, anticonvulsants, and benzodiazepines. Details of the study assessment protocol are available in Hobert et al. (2011).
In this analysis, data from visits 1–4 of 401 healthy participants were included. To rule out the effect of currently present unipolar depression, subjects with > 17 points on the Beck Depression Inventory I (BDI-I) were excluded from the analysis (group 2 and 3, n = 126 subjects). Details are presented in Figure 1. Of those, 81 were Dep+ (positive history of depression) and 320 Dep- (negative history of depression). A person was included in the Dep+ cohort if they indicated in a self-reported questionnaire, according to the model of the Federal Health Survey (Jacobi et al., 2002), and approved in a personal interview, that they suffered from physician-confirmed unipolar depression over the life course. Fourth, due to the design of the research question and the study, the extent to which the criteria for manifest depression were present could not be verified. Dep- was defined as answering the question in the negative. We excluded datasets of TREND participants whose information regarding their unipolar depression history was ambiguous or if no medical examination had taken place (group 4, n = 178 subjects). Non-native speakers were also excluded to prevent comprehension problems due to language (n = 41).
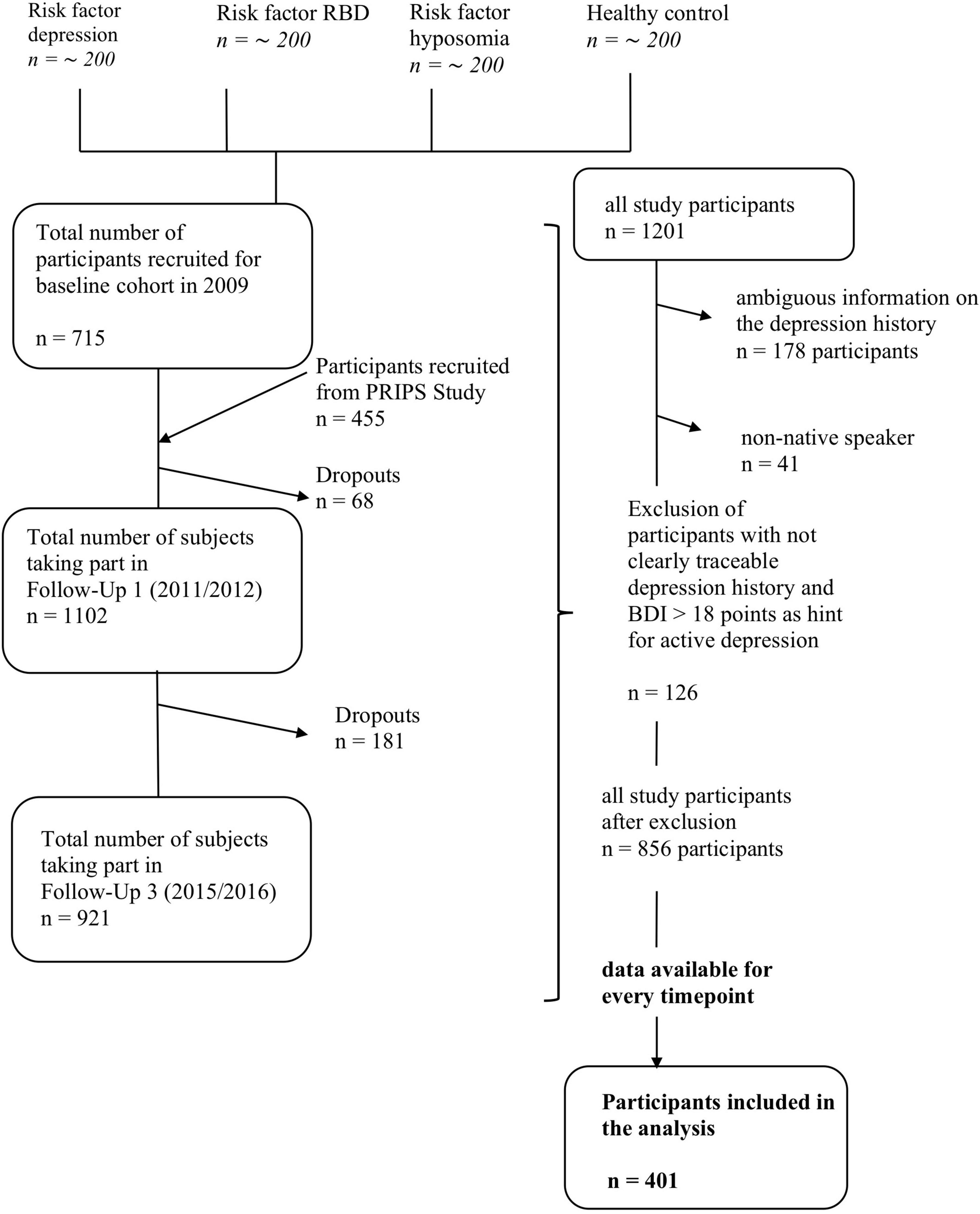
Figure 1. Flow chart for TREND participants included in this analysis. The left-hand side of the diagram shows the general process of the TREND study with corresponding fluctuations in the number of test subjects (drop-outs, further inclusions). The right-hand side shows the process of the analysis carried out with the exclusion of test subjects prior to the evaluation. RBD, Rapid Eye Movement Sleep behavior disorder; PRIPS Study, screening battery for subjects at risk for Parkinson’s disease.
Extracted parameters
The following parameters were extracted from the TREND database: BDI-I (Arnau et al., 2001) Mini-Mental-State Examination (MMSE) (Folstein et al., 1975; Morris et al., 1989), Consortium to Establish a Registry for Alzheimer’s disease (CERAD) test battery (Thalmann et al., 1997), motor part of the Movement disorder society-revised version of the Unified Parkinson disease rating scale (MDS-UPDRS III) (Goetz et al., 2008), fast gait speed and checking boxes speed from a single and dual tasking assessment, where participants walk 20 m on level ground in a corridor of at least 4 m width with the instruction to walk as fast as possible (Doumas et al., 2012; Metzger et al., 2016). Amount of sport activities was assessed with the German National Health Interview and Examination Survey 1999 (Mensink, 1999). Physical activity was defined by the type of sport and frequency (< 0.5 h/week, 0.5–1 h/week, > 1–2 h/week, > 2–4 h/week, and > 4 h/week). Details are provided in Table 1.
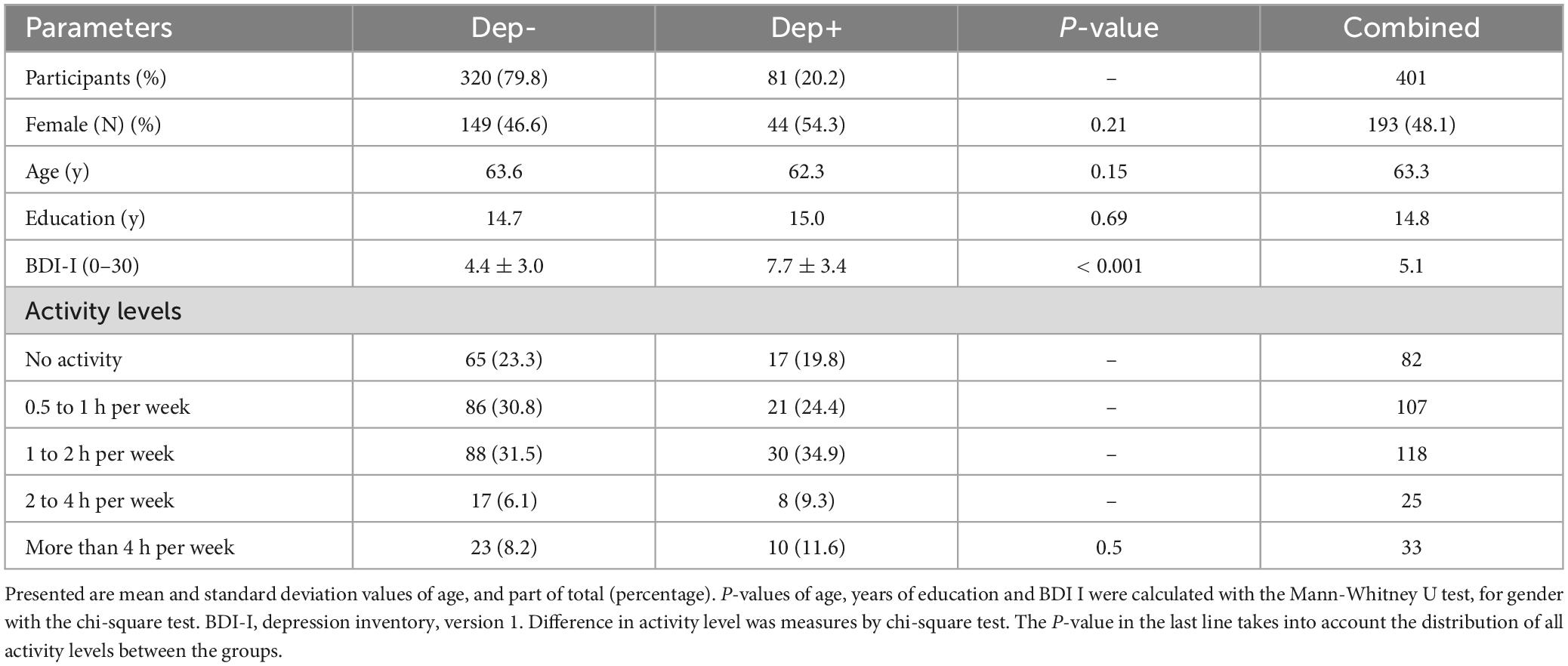
Table 1. Demographic data of participants with (Dep+) and without history of unipolar depression (Dep-).
Statistical analysis
SPSS Statistics Version 24.0.0.0 (IBM) was used for statistical analyses. Distributions of age and years of education were compared between groups using the Mann-Whitney-U test, and distribution of gender using the chi-square test. Longitudinal analyses were performed using analysis of variance with repeated measures (rmANOVA, Park et al., 2009), as covariates we defined the BDI-I. The mean change in performance over time was calculated with the within-subjects effect. It depicts the influence of time on the parameters independent of the group assignment. Differences in the parameters between the two groups Dep+ and Dep-, independent of time, were calculated with the between-subjects effect (Brambor et al., 2006). Univariate rmANOVAs were calculated for the following parameters: BDI-I, MMSE, CERAD, MDS-UPDRS III, gait speed, and dual task costs (DTC). DTC were calculated based on Hobert et al. (2011). Significance level was set at 0.05. Bonferroni correction was applied for variance analysis with repeated measures (six tests, corrected values indicated).
Results
Dep+ participants were not significantly different from Dep- participants in terms of age, gender and years of education, but Dep+ participants had higher BDI scores at baseline. Details are presented in Table 1. Gait speed was lower in Dep+ participants, compared to Dep- (mean for all time points 98 ± 11 m/min versus 101 ± 13 m/min, p = 0.048; Table 2). Over the observation period of 6 years, Dep+ and Dep- groups did not show a significant within-subjects effect in any of the rmANOVAs (MMSE, CERAD, MDS-UPDRS III, gait speed and DTC). Details, including p-values, F values and effect sizes are shown in Figure 2 and Table 2. Dep- did not show higher level of physical activity compared to Dep + (p = 0.5; Figure 1) based on the hours of exercise per week reported.
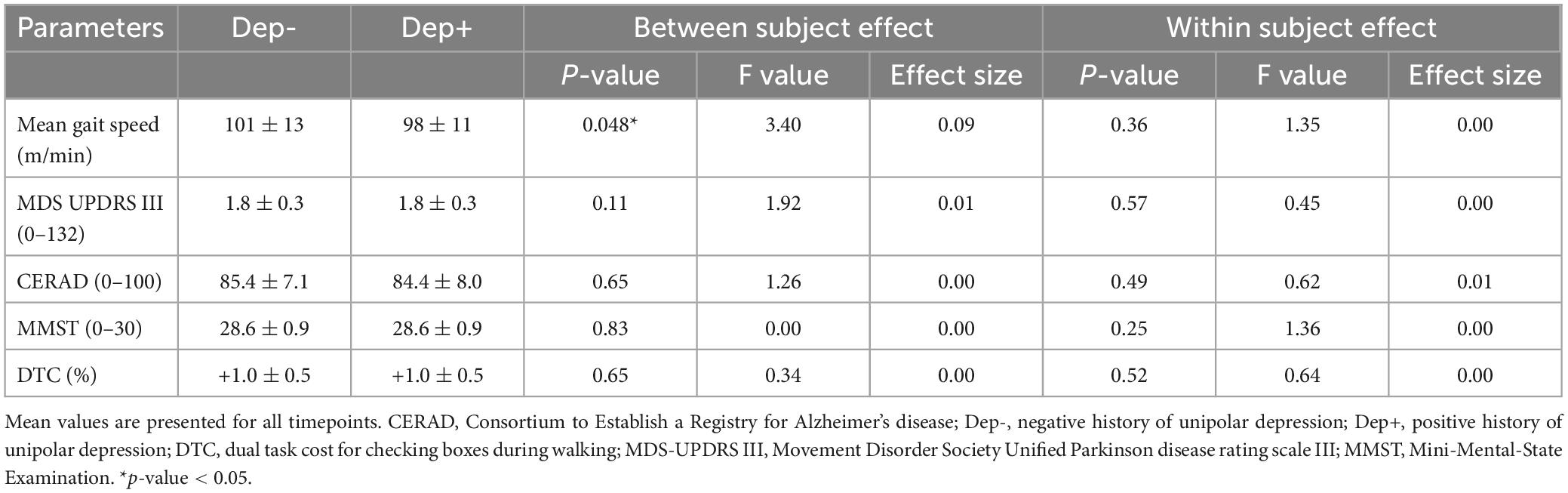
Table 2. Comparison of outcome parameters between participants with (Dep+) and without history of unipolar depression (Dep–).
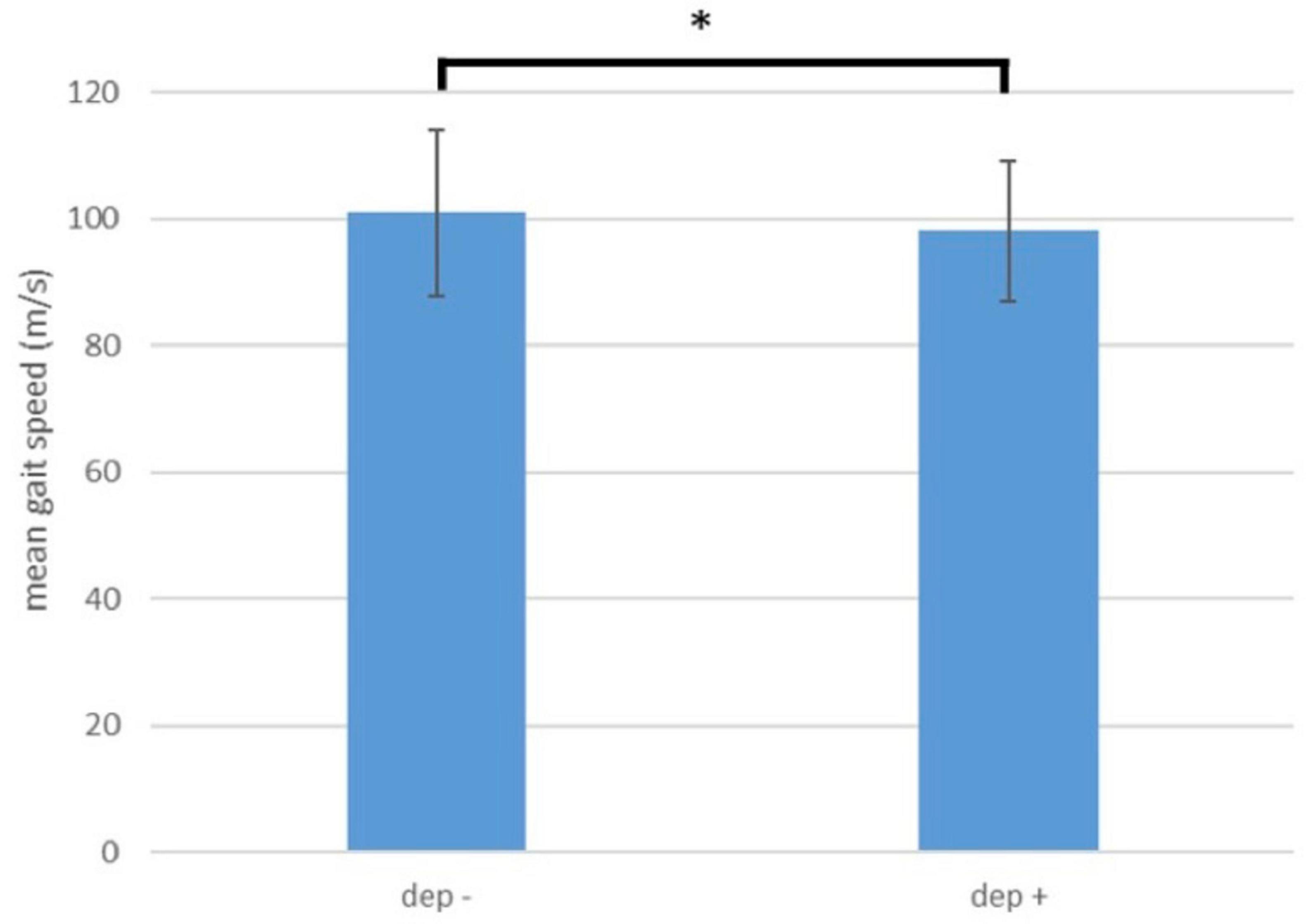
Figure 2. Comparison of gait speed between participants with (Dep+) and without history of depression.
Discussion
To the best of our knowledge, this is the first longitudinal observational case-control study that investigated motor and cognitive deficits after unipolar depressive episodes while considering relevant confounding factors. We found a significantly lower gait speed in participants with a positive history of unipolar depression over an observation period of 6 years. Our study adds relevant aspects to results of earlier studies showing a decrease in gait speed in individuals with unipolar depression (Everson-Rose et al., 2005; Michalak et al., 2009; Brandler et al., 2012). In more detail, our results indicate that the slowing of gait persists even after the persons affected recover from the depressive episode.
What could be the reasons for this phenomenon? One option is a persistent reduction of internal motivation and agility. This would be, at least indirectly, in line with a study showing that severity of unipolar depressive episode correlates negatively with gait speed (Brandler et al., 2012). However, as the BDI-I (which was indeed significantly higher in Dep+ than in Dep-) was considered as a covariate in our calculations, this explanation probably falls short, and it makes sense to look at other potential explanatory mechanisms. Another option could be a decrease of physical resources due to reduced activity in the context of, and after depression. Such an association has already been demonstrated (Penninx et al., 1999; Geerlings et al., 2001; Hybels et al., 2009), even in remission (Hiles et al., 2017; Schuch et al., 2017). However, as Dep+ and Dep- showed comparable physical activity levels, this option also does not seem to be a sound explanation for the observed differences. Eventually, it is also conceivable that people who have remitted from an unipolar depression walk more slowly due to a more relaxed or hesitant attitude to life, and thus slower gait speed in these people does not necessarily reflect a disease-associated deficit but rather a constitutional factor (Kermott et al., 2019; Laird et al., 2019). It could also be that people with slow gait speed are more prone to depressive episodes, which has to be investigated in future studies. Another noteworthy point is that we compared the fastest possible gait speed (capacity measure). It would be interesting to know whether Dep+ also have a slower gait speed in everyday life (performance measure). This aspect could be useful for the transfer to everyday functionality (Maetzler et al., 2021).
Interestingly, none of the motor and cognitive parameters investigated in this study deteriorated over the observation period of 6 years, particularly not in the Dep+ cohort. It has been suggested that subsyndromal depressive symptoms and slow gait are part of a geriatric syndrome that also includes impaired executive function (Albert, 2019; Patience et al., 2019). In addition, unipolar depression is associated with a 2–4-fold increased risk of dementia (Kessing, 2012; Bennett and Thomas, 2014b), which, in turn, is associated with reduced gait speed even in the prodromal phases (Metzger et al., 2016; Grande et al., 2019; Windham et al., 2022). Therefore, decline in gait speed in our cohort could have been interpreted as a “prodromal sign of cognitive impairment” although confirmation by clinical (dementia) diagnosis would have been helpful for validation with this respect. Moreover, unipolar depression is also associated with future development of PD (Schrag et al., 2015), and PD patients may have reduced gait speed over the last years before clinical diagnosis is possible (Del Din et al., 2019). As we did not find any evidence of a cognitive and motor deterioration over the observation period of 6 years in our groups, it remains unclear whether our groups were too small or the observation period too short to show significant changes over time. Another point is that the subject age may have been too low to reliably detect possible incipient neurodegenerative processes.
This study faces some limitations. First, although the TREND study overlooks a relatively large cohort of older adults, results may apply mainly for areas where the cohort was recruited (here in Central Europe). Second, two thirds of the original dataset could not be included in the analysis, due to the definition and completeness of the data available, so there remains some risk of bias due to the selection of datasets Third, we did not collect information about our participants before the depressive episode occurred that could potentially explain lower gait speed, and therefore cannot exclude the possibility that lowered gait speed in the Dep+ cohort is a constitutional factor. Moreover, it is also possible that the factors “slow gait speed” and “unipolar depressive episode” are only indirectly associated with each other. It therefore seems reasonable to confirm or reject the results we have presented here in another longitudinally observed cohorts.
In conclusion, we found in older adults that a history of unipolar depression in remitted persons is related to reduced gait speed. The extent to which constitutional and learned mechanisms play a role here cannot be determined in the end and needs to be determined in future studies. A steady decrease in function indicative of a neurodegenerative process could not be shown.
Data availability statement
The original contributions presented in this study are included in this article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Medical Faculty of Tübingen in 2009 (protocol number 90/2009BO2). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The animal study was approved by Ethics Committee of the Medical Faculty of Tübingen in 2009 (protocol number 90/2009BO2). The study was conducted in accordance with the local legislation and institutional requirements.
Authors contributions
SS: Conceptualization, Formal Analysis, Writing – original draft. MH: Conceptualization, Funding acquisition, Writing – review and editing. KE: Formal Analysis, Writing – review and editing. CH: Conceptualization, Writing – review and editing. ME: Conceptualization, Supervision, Writing – review and editing. US: Data curation, Supervision, Writing – review and editing. IW: Writing – review and editing. BR: Conceptualization, Resources, Writing – review and editing. MZ: Conceptualization, Resources, Writing – review and editing. AF: Conceptualization, Funding acquisition, Validation, Writing – review and editing. DB: Conceptualization, Funding acquisition, Writing – review and editing. WM: Formal Analysis, Funding acquisition, Project administration, Supervision, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The TREND study was being conducted at the University Hospital Tübingen and has been supported by the Hertie Institute for Clinical Brain Research, the DZNE, the Geriatric Center of Tübingen, the Center for Integrative Neuroscience, Teva Pharmaceutical Industries, Union Chimique Belge, Janssen Pharmaceuticals, the International Parkinson Foundation and the German Research Society. Specifically, the CORO-TREND project of the TREND study was funded by the German Research Society (DFG, grant number: AOBJ: 675915).
Acknowledgments
We thank the participants for their continued participation in the TREND study. We acknowledge the work of the numerous (doctoral) students and study nurses, who actively contributed to study organization, and data collection, entry, and monitoring. We used RedCap as database software. Study data are collected and managed using REDCap electronic data capture tools hosted at University of Tübingen (Harris et al., 2009).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Albert, S. (2019). Depressive symptoms, executive deficit, and slow gait: A geriatric syndrome? Am. J. Geriatr. Psychiatry 27, 1384–1385. doi: 10.1016/j.jagp.2019.08.001
Arnau, R., Meagher, M., Norris, M., and Bramson, R. (2001). Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychol. 20, 112–119. doi: 10.1037//0278-6133.20.2.112
Artaud, F., Singh-Manoux, A., Dugravot, A., Tzourio, C., and Elbaz, A. (2015). Decline in fast gait speed as a predictor of disability in older adults. J. Am. Geriatr. Soc. 63, 1129–1136. doi: 10.1111/jgs.13442
Bareeqa, S., Samar, S., Kamal, S., Masood, Y., Allahyar, Ahmed, S., et al. (2022). Prodromal depression and subsequent risk of developing Parkinson’s disease: A systematic review with meta-analysis. Neurodegener. Dis. Manag. 12, 155–164. doi: 10.2217/nmt-2022-0001
Bennett, S., and Thomas, A. (2014a). Depression and dementia: Cause, consequence or coincidence? Maturitas 79, 184–190. doi: 10.1016/j.maturitas.2014.05.009
Bennett, S., and Thomas, A. (2014b). Maturitas Depression and dementia: Cause, consequence or coincidence? Maturitas 79, 184–190. doi: 10.1016/j.maturitas.2014.05.009
Berg, D., Postuma, R., Adler, C., Bloem, B., Chan, P., Dubois, B., et al. (2015). MDS research criteria for prodromal Parkinson ’ s disease. Mov. Disord. 30, 1600–1609. doi: 10.1002/mds.26431
Binotto, M., Lenardt, M., and Rodríguez-Martínez, M. (2018). Physical frailty and gait speed in community elderly: A systematic review. Rev. Esc. Enferm. USP 52:e03392. doi: 10.1590/S1980-220X2017028703392
Brambor, T., Clark, W. R., and Golder, M. (2006). Understanding interaction models: Improving empirical analyses. Polit. Anal. 14, 63–82. doi: 10.1093/pan/mpi014
Brandler, T., Wang, C., Oh-Park, M., Holtzer, R., and Verghese, J. (2012). Depressive symptoms and gait dysfunction in the elderly. Am. J. Geriatr. Psychiatry 20, 425–432. doi: 10.1097/JGP.0b013e31821181c6
Byers, A., and Yaffe, K. (2011). Depression and risk of developing dementia. Nat. Rev. Neurol. 7, 323–331. doi: 10.1038/nrneurol.2011.60
Del Din, S., Elshehabi, M., Galna, B., Hobert, M., Warmerdam, E., Suenkel, U., et al. (2019). Gait analysis with wearables predicts conversion to parkinson disease. Ann. Neurol. 86, 357–367. doi: 10.1002/ana.25548
den Ouden, M., Schuurmans, M., Arts, I., and van der Schouw, Y. (2011). Physical performance characteristics related to disability in older persons: A systematic review. Maturitas 69, 208–219. doi: 10.1016/j.maturitas.2011.04.008
Doumas, M., Smolders, C., Brunfaut, E., Bouckaert, F., and Krampe, R. (2012). Dual task performance of working memory and postural control in major depressive disorder. Neuropsychology 26, 110–118. doi: 10.1037/a0026181
Dumurgier, J., Elbaz, A., Ducimetière, P., Tavernier, B., Alpérovitch, A., and Tzourio, C. (2009). Slow walking speed and cardiovascular death in well functioning older adults: Prospective cohort study. BMJ 339:b4460. doi: 10.1136/bmj.b4460
Everson-Rose, S., Skarupski, K., Bienias, J., Wilson, R., Evans, D., and Mendes de Leon, C. (2005). Do depressive symptoms predict declines in physical performance in an elderly, biracial population? Psychosom Med. 67, 609–615. doi: 10.1097/01.psy.0000170334.77508.35
Folstein, M., Folstein, S., and McHugh, P. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198. doi: 10.1016/0022-3956(75)90026-6
Geerlings, S., Beekman, A., Deeg, D., Twisk, J., and Van Tilburg, W. (2001). The longitudinal effect of depression on functional limitations and disability in older adults: An eight-wave prospective community-based study. Psychol. Med. 31, 1361–1371. doi: 10.1017/s0033291701004639
Goetz, C., Tilley, B., Shaftman, S., Stebbins, G., Fahn, S., Martinez-Martin, P., et al. (2008). Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Mov. Disord. 23, 2129–2170. doi: 10.1002/mds.22340
Grande, G., Triolo, F., Nuara, A., Welmer, A., Fratiglioni, L., and Vetrano, D. (2019). Measuring gait speed to better identify prodromal dementia. Exp. Gerontol. 124:110625. doi: 10.1016/j.exger.2019.05.014
Harris, P., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., and Conde, J. (2009). Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381. doi: 10.1016/j.jbi.2008.08.010
Hiles, S., Lamers, F., Milaneschi, Y., and Penninx, B. (2017). Sit, step, sweat: Longitudinal associations between physical activity patterns, anxiety and depression. Psychol. Med. 47, 1466–1477. doi: 10.1017/S0033291716003548
Hobert, M., Bruhn, D., Koch, J., and Studt, S. (2023). Depression as a major component of a gait disorder-Successful multimodal treatment including electroconvulsive therapy : A case report. Z. Gerontol. Geriatr. 56, 59–64. doi: 10.1007/s00391-022-02135-2
Hobert, M., Niebler, R., Meyer, S., Brockmann, K., Becker, C., Huber, H., et al. (2011). Poor trail making test performance is directly associated with altered dual task prioritization in the elderly–baseline results from the TREND study. PLoS One 6:e27831. doi: 10.1371/journal.pone.0027831
Hybels, C., Pieper, C., and Blazer, D. (2009). The complex relationship between depressive symptoms and functional limitations in community-dwelling older adults: The impact of subthreshold depression. Psychol. Med. 39, 1677–1688. doi: 10.1017/S0033291709005650
Jacobi, F., Höfler, M., Strehle, J., Mack, S., Gerschler, A., Scholl, L., et al. (2014). [Mental disorders in the general population : Study on the health of adults in Germany and the additional module mental health (DEGS1-MH)]. Nervenarzt 85, 77–87. doi: 10.1007/s00115-013-3961-y
Jacobi, F., Wittchen, H., Hölting, C., Sommer, S., Lieb, R., Höfler, M., et al. (2002). Estimating the prevalence of mental and somatic disorders in the community: Aims and methods of the German National Health Interview and Examination Survey. Int. J. Methods Psychiatr. Res. 11, 1–18. doi: 10.1002/mpr.118
Kamiya, K., Hamazaki, N., Matsue, Y., Mezzani, A., Corrà, U., Matsuzawa, R., et al. (2018). Gait speed has comparable prognostic capability to six-minute walk distance in older patients with cardiovascular disease. Eur. J. Prev. Cardiol. 25, 212–219. doi: 10.1177/2047487317735715
Kermott, C., Johnson, R., Sood, R., Jenkins, S., and Sood, A. (2019). Is higher resilience predictive of lower stress and better mental health among corporate executives? PLoS One 14:e0218092. doi: 10.1371/journal.pone.0218092
Kessing, L. V. (2012). Depression and the risk for dementia. Curr. Opin. Psychiatry 25, 457–461. doi: 10.1097/YCO.0b013e328356c368
Kessler, R., Berglund, P., Demler, O., Jin, R., Koretz, D., Merikangas, K., et al. (2003). The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA 289, 3095–3105. doi: 10.1001/jama.289.23.3095
Laird, K., Krause, B., Funes, C., and Lavretsky, H. (2019). Psychobiological factors of resilience and depression in late life. Transl. Psychiatry 9:88. doi: 10.1038/s41398-019-0424-7
Lempriere, S. (2022). Daily step count linked to dementia risk. Nat. Rev. Neurol. 18:637. doi: 10.1038/s41582-022-00730-w
Lerche, S., Seppi, K., Behnke, S., Liepelt-Scarfone, I., Godau, J., Mahlknecht, P., et al. (2014). Risk factors and prodromal markers and the development of Parkinson’s disease. J. Neurol. 261, 180–187. doi: 10.1007/s00415-013-7171-0
Maetzler, W., Rochester, L., Bhidayasiri, R., Espay, A., Sánchez-Ferro, A., and van Uem, J. (2021). Modernizing daily function assessment in parkinson’s disease using capacity, perception, and performance measures. Mov. Disord. 36, 76–82. doi: 10.1002/mds.28377
Maske, U., Buttery, A., Beesdo-Baum, K., Riedel-Heller, S., Hapke, U., and Busch, M. (2016). Prevalence and correlates of DSM-IV-TR major depressive disorder, self-reported diagnosed depression and current depressive symptoms among adults in Germany. J. Affect. Disord. 190, 167–177. doi: 10.1016/j.jad.2015.10.006
Mensink, G. B. (1999). [Physical activity]’, Gesundheitswesen (Bundesverband der Arzte des Offentlichen Gesundheitsdienstes (Germany)), 61 Spec No. Available online at: http://europepmc.org/abstract/MED/10726410 (accessed December 01, 1999).
Metzger, F., Hobert, M., Ehlis, A., Hasmann, S., Hahn, T., Eschweiler, G., et al. (2016). Dual tasking for the differentiation between depression and mild cognitive impairment. Front. Aging Neurosci. 8:235. doi: 10.3389/fnagi.2016.00235
Michalak, J., Troje, N., Fischer, J., Vollmar, P., Heidenreich, T., and Schulte, D. (2009). Embodiment of sadness and depression–gait patterns associated with dysphoric mood. Psychosom. Med. 71, 580–587. doi: 10.1097/PSY.0b013e3181a2515c
Morris, J., Heyman, A., Mohs, R., Hughes, J., van Belle, G., Fillenbaum, G., et al. (1989). The consortium to establish a registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 39, 1159–1165. doi: 10.1212/wnl.39.9.1159
Park, E., Cho, M., and Ki, C. (2009). Correct use of repeated measures analysis of variance. Korean J. Lab. Med. 29, 1–9. doi: 10.3343/kjlm.2009.29.1.1
Patience, J., Lai, K., Russell, E., Vasudev, A., Montero-Odasso, M., and Burhan, A. (2019). Relationship between mood, thinking, and walking: A systematic review examining depressive symptoms, executive function, and gait. Am. J. Geriatr. Psychiatry 27, 1375–1383. doi: 10.1016/j.jagp.2019.07.007
Penninx, B., Leveille, S., Ferrucci, L., van Eijk, J., and Guralnik, J. (1999). Exploring the effect of depression on physical disability: Longitudinal evidence from the established populations for epidemiologic studies of the elderly. Am. J. Public Health 89, 1346–1352. doi: 10.2105/ajph.89.9.1346
Rovner, B., German, P., Brant, L., Clark, R., Burton, L., and Folstein, M. (1991). Depression and mortality in nursing homes. JAMA 265, 993–996. doi: 10.1001/jama.265.8.993
Sanders, J., Bremmer, M., Comijs, H., van de Ven, P., Deeg, D., and Beekman, A. (2017). Gait speed and processing speed as clinical markers for geriatric health outcomes. Am. J. Geriatr. Psychiatry 25, 374–385. doi: 10.1016/j.jagp.2016.12.003
Schrag, A., Horsfall, L., Walters, K., Noyce, A., and Petersen, I. (2015). Prediagnostic presentations of Parkinson’s disease in primary care: A case-control study. Lancet Neurol. 14, 57–64. doi: 10.1016/S1474-4422(14)70287-X
Schuch, F., Vancampfort, D., Firth, J., Rosenbaum, S., Ward, P., Reichert, T., et al. (2017). Physical activity and sedentary behavior in people with major depressive disorder: A systematic review and meta-analysis. J. Affect. Disord. 210, 139–150. doi: 10.1016/j.jad.2016.10.050
Serrano-Checa, R., Hita-Contreras, F., Jiménez-García, J., Achalandabaso-Ochoa, A., Aibar-Almazán, A., and Martínez-Amat, A. (2020). Sleep quality, anxiety, and depression are associated with fall risk factors in older women. Int. J. Environ. Res. Public Health 17:4043. doi: 10.3390/ijerph17114043
Skorvanek, M., Ladomirjakova, Z., Han, V., Lesko, N., Feketeova, E., Jarcuskova, D., et al. (2017). Prevalence of prodromal Parkinson’s disease as defined by MDS research criteria among elderly patients undergoing colonoscopy. J. Parkinsons Dis. 7, 481–489. doi: 10.3233/JPD-161036
Sloman, L., Berridge, M., Homatidis, S., Hunter, D., and Duck, T. (1982). Gait patterns of depressed patients and normal subjects. Am. J. Psychiatry 139, 94–97. doi: 10.1176/ajp.139.1.94
Studenski, S., Perera, S., Patel, K., Rosano, C., Faulkner, K., Inzitari, M., et al. (2011). Gait speed and survival in older adults. JAMA 305, 50–58. doi: 10.1001/jama.2010.1923
Thalmann, B., Monsch, A. U., Bernasconi, F., Berres, M., Schneitter, M. Ermini-Fünfschilling, D., et al. (1997). Consortium to Establish a Registry for Alzheimer’s Disease Assessment Battery - deutsche Fassung. Basel: Universitäre Altersmedizin.
Keywords: unipolar depression, gait speed, neurodegenerative disorders, functional decline, cognition
Citation: Straub S, Hobert MA, Emmert K, Hansen C, Elshehabi M, Suenkel U, Wurster I, Roeben B, Zimmermann M, Fallgatter AJ, Berg D and Maetzler W (2025) Motor and cognitive function after unipolar depressive episodes: a 6 years longitudinal observational study. Front. Psychol. 16:1295848. doi: 10.3389/fpsyg.2025.1295848
Received: 17 September 2023; Accepted: 01 April 2025;
Published: 16 April 2025.
Edited by:
Sha Liu, First Hospital of Shanxi Medical University, ChinaReviewed by:
Cynthia Whissell, Laurentian University, CanadaBianca Crecan-Suciu, University of Medicine and Pharmacy Iuliu Hatieganu, Romania
Copyright © 2025 Straub, Hobert, Emmert, Hansen, Elshehabi, Suenkel, Wurster, Roeben, Zimmermann, Fallgatter, Berg and Maetzler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stephanie Straub, c3RlcGhhbmllLm1hZW5ubGluQG1lZC51bmktdHVlYmluZ2VuLmRl
 Stephanie Straub
Stephanie Straub Markus A. Hobert
Markus A. Hobert Kirsten Emmert3
Kirsten Emmert3 Clint Hansen
Clint Hansen Morad Elshehabi
Morad Elshehabi Ulrike Suenkel
Ulrike Suenkel Isabel Wurster
Isabel Wurster Benjamin Roeben
Benjamin Roeben Milan Zimmermann
Milan Zimmermann Andreas J. Fallgatter
Andreas J. Fallgatter Walter Maetzler
Walter Maetzler