- 1Department of Human Sciences, European University of Rome, Rome, Italy
- 2Rheumatology and Clinical Immunology, Department of Medicine, University of Rome "Campus Bio-Medico" School of Medicine, Rome, Italy
- 3Clinical and Research Section of Rheumatology and Clinical Immunology, Fondazione Policlinico Universitario Campus Bio-Medico, Rome, Italy
Pain is a central feature of inflammatory rheumatic diseases and is associated with psychological distress. Pain is widely recognized not as a mere physical sensation, but as a complex, multidimensional phenomenon with an affective component. A plethora of research has conceptualized adaptation to pain by focusing on minimizing the pain experience. However, pain in autoimmune inflammatory rheumatic diseases is often neither avoidable nor curable. This cross-sectional study aimed to investigate the processes explaining how pain intensity may be associated with low well-being and why some patients may live well despite pain. Drawing upon the psychological (in)flexibility model and the process model of emotion regulation, we propose that cognitive reappraisal moderates the association between pain and euthymia through experiential avoidance. Ninety-seven patients with rheumatoid arthritis, psoriatic arthritis, or axial spondyloarthritis were included for analyses (mean age = 53.4; mean time since diagnosis = 9.2 years). Most patients were women (75%), married/cohabitant (71%), and attended high school (47%). Results indicate that experiential avoidance may explain how severe pain is associated with lowered euthymia. This indirect negative effect of pain intensity on euthymia became non-significant at high levels of cognitive reappraisal, suggesting that cognitive reappraisal may serve as a protective factor for patients with autoimmune inflammatory rheumatic diseases. This study paves the way for future research in this promising context by providing an initial step towards integrating emotion regulation and psychological inflexibility in pain conditions.
1 Introduction
Research on chronic pain has mostly considered pain as a clinically relevant outcome (e.g., Martinez-Calderon et al., 2018a,b; Reiner et al., 2013). The identification of factors contributing to the experience of pain is crucial for developing targeted interventions and to identify vulnerable patients. However, research on characteristics that allow patients to live well despite pain is still limited (e.g., Flink et al., 2015; Peters et al., 2017). Studies addressing this issue are in line with the clinicians’ goal to improve patients’ quality of life, rather than merely striving to reduce chronic pain (Sullivan and Ballantyne, 2016). This is particularly relevant given that a significant number of patients suffering from autoimmune inflammatory rheumatic diseases—a family of autoimmune conditions primarily affecting the connective tissues and musculoskeletal organs—exhibit persistent residual pain despite the achievement of remission or low disease activity (Ishida et al., 2018; Liu et al., 2021). Some studies have demonstrated that advances in biological treatments for rheumatoid arthritis are still not enough to improve some relevant patient-reported outcomes. A recent meta-analysis investigated the temporal improvement of patient-reported outcomes over the last 30 years in light of new treatment strategies employed in early 2000s (Carpenter et al., 2020). It was found that adopting new therapy approaches [i.e., Treat-2-Target, and biologic Disease Modifying Anti-Rheumatic Drugs (DMARDs)] coincided with improvements in disease activity and physical function, but not in pain, functional disability, and mental well-being (Carpenter et al., 2020).
Pain is not merely a physical symptom (i.e., nociception); it also reflects unpleasant emotional states (i.e., affective-motivational dimension), and appraisals of meanings and consequences of pain (i.e., cognitive-evaluative dimension; Lumley et al., 2011; Melzack and Casey, 1968). The Dynamic Model of Effective Pain Adaptation emphasizes how persons adaptively respond to the pain experience, rather than focusing on pain itself (Sturgeon and Zautra, 2016). Dimensions of resilient pain adaptation include recovery, referring to the ways a person effectively returns to baseline levels of emotional and physical functioning (e.g., low pain intensity), and sustainability, reflecting the positive and meaningful engagement of a person despite the presence of pain (Sturgeon and Zautra, 2016). The latter may be operationalized as “the continuing experience of optimal emotional, psychological, and social well-being in the presence of pain” (Goubert and Trompetter, 2017, p. 3), that is flourishing (Keyes, 2002, 2005). In this context, the concept of euthymia might represent an important outcome for patients suffering from pain conditions. Euthymia includes affective and hedonic dimensions of subjective well-being (including restorative sleep), and psychological well-being, which entails an integration and balance of psychic forces (i.e., flexibility), a unifying outlook on life that guides behaviours and feelings to fashion the future consistently (i.e., consistency), resilience and tolerance to frustration and anxiety (i.e., resistance to stress; Carrozzino et al., 2021; Kusier and Folker, 2020; Fava and Bech, 2016; Fava and Guidi, 2020; Guidi and Fava, 2022).
A paucity of studies investigated well-being domains in patients with inflammatory rheumatic diseases, reflecting mainstream research focusing on negative functioning and likely glossing over the unique contributions of positive functioning (Wood and Tarrier, 2010). Nonetheless, there is evidence showing that over half of people with arthritis report high levels of emotional, psychological, and social well-being (Almweisheer et al., 2023) even those living with disabling chronic pain (Fuller-Thomson et al., 2023), and to a lesser extent (38%) in those with recurrent pain (Trompetter et al., 2019). To the best of our knowledge, euthymia has never been examined in people with inflammatory rheumatic disease, but research on other chronic health conditions suggests that lower levels of euthymia are associated with worse clinical conditions (Carrozzino et al., 2019; Cosci et al., 2021; Guidi et al., 2019; Zhang et al., 2022). Moreover, euthymia is positively associated with several dimensions of psychological well-being, suggesting only a partial overlap between the two constructs (Carrozzino et al., 2019).
A research tradition that emphasizes the processes by which people can live a fulfilling life despite pain is the one focusing on psychological flexibility (Goubert and Trompetter, 2017). Psychological flexibility allows individuals to accept inner experiences, including negative ones, while remaining sensitive to their direct experiences and engaging in values-based actions consistent with personal values (McCracken and Morley, 2014). Conversely, psychological inflexibility refers to a “rigid dominance of psychological reactions over chosen values and contingencies in guiding actions” (Bond et al., 2011, p. 678). Thus, it is strictly related to experiential avoidance, as individuals unwilling to stay in contact with unpleasant inner experiences are likely to take action to alter or avoid them (Bond et al., 2011; Hayes et al., 1996). The psychological (in)flexibility model posits that psychological inflexibility (e.g., experiential avoidance cognitive fusion, pain acceptance) is related to decreased engagement in values-based action, leading to reduced well-being (Hayes et al., 2012). In chronic pain patients, experiential avoidance predicted several outcomes, including depression and pain-related anxiety, over and beyond pain intensity, pain acceptance, and mindfulness (McCracken and Zhao-O’Brien, 2010). Although the psychological flexibility model has been successfully extended to chronic pain patients (McCracken and Vowles, 2014; Vowles et al., 2007, 2014), few studies investigated whether psychological (in)flexibility might explain associations between pain and psychological or physical outcomes. In chronic pain patients, the association between pain and psychological distress was mediated by cognitive fusion (Carvalho et al., 2019) and experiential avoidance (Goldbart et al., 2021). In patients with fibromyalgia and obesity, the pain severity-disability association was accounted for by pain acceptance (Varallo et al., 2022). The role of psychological inflexibility was also investigated in cancer patients, where cancer-related pain was positively related to psychological distress through cognitive fusion, experiential avoidance, and functional impairment (Brown et al., 2020). Overall, this initial evidence suggests that psychological flexibility model may successfully explain the relationship between pain and psychological distress.
Since pain is a complex phenomenon implying both physical and affective dimensions (Lumley et al., 2011), adaptive or dysfunctional responses to pain may rely on emotion regulation strategies used by people suffering from pain conditions. According to the process model, cognitive reappraisal and expressive suppression are the most used emotion regulation strategies (Gross, 2008, 2015). There is evidence showing that cognitive reappraisal and expressive suppression were not directly associated with pain, but expressive suppression was associated with higher anxiety and depression (Koechlin et al., 2018), and cognitive reappraisal predicted psychological distress (Karademas et al., 2020). Previous research suggested the importance of cognitive reappraisal in modulating the emotional component of episodic pain in rheumatoid arthritis (Hamilton et al., 2005, 2007). Specifically, emotion regulation and affective intensity moderated the prospective associations between pain and both positive and negative affect, suggesting that patients could recover from arthritic pain, except for those with difficulties in regulating strong unpleasant emotions (Hamilton et al., 2005). Thus, intense unpleasant emotions may not necessarily lead to emotion dysregulation in patients with good emotion regulation abilities (Hamilton et al., 2007). A transdiagnostic perspective on psychological inflexibility and emotion regulation has been recently proposed (Faustino, 2021). Faustino (2021) found that cognitive fusion was negatively associated with cognitive reappraisal both in the clinical and non-clinical sample, whereas it was positively associated with emotion suppression only in the non-clinical sample. Moreover, cognitive reappraisal predicted cognitive fusion in both samples, suggesting that individuals who lack cognitive reappraisal abilities are more likely to be fused with their inner experience (Faustino, 2021). Indeed, cognitive reappraisal reflects a shift from an evaluation to another one (i.e., reappraisal); to do that, “individuals must have the ability to distance themselves from the first evaluation. It is the ability to shift internal dispositions accordingly with context-dependent demands that underlies psychological flexibility” (Faustino, 2021, p. 10).
The overall objective of the present study was to investigate how pain intensity may be associated with well-being and why some patients, but not others, may live well despite arthritis-related pain. Particularly, we focused on pain related to three autoimmune inflammatory rheumatic diseases, namely rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis. These diseases share several characteristics, including pain, stiffness, fatigue, decreased physical function, and potential deformities and joint destruction (Mease et al., 2019). Previous research on the mediation role of psychological flexibility solely focused on outcomes related to negative functioning (Carvalho et al., 2019; Goldbart et al., 2021; Varallo et al., 2022). The current study sought to extend current knowledge by considering euthymia as a relevant outcome. Specifically, we hypothesized that the unwillingness to stay in contact with unpleasant inner experiences and the tendency to take action to alter or avoid them (i.e., experiential avoidance) may explain the association between pain intensity and euthymia. Drawing upon the transdiagnostic perspective of emotion regulation and previous research (Faustino, 2021; Hamilton et al., 2005, 2007), we further hypothesized that cognitive reappraisal might represent a protective factor by moderating the association between pain intensity and euthymia through experiential avoidance. Thus, the following statistical hypothesis was derived: pain intensity would be positively associated with experiential avoidance (path a), which in turn would be associated with lower levels of euthymia (path b). Cognitive reappraisal would moderate the indirect effect, such that at higher levels of cognitive reappraisal, the association between pain and experiential avoidance would be weaker, which in turn would be associated with higher euthymia.
2 Methods
2.1 Participants and procedure
This is a cross-sectional study with patients recruited consecutively at the Immuno-rheumatology Unit, Campus Bio-Medico University of Rome. Patients were asked to participate in the study if they met the following inclusion criteria: (a) diagnosis of either rheumatoid arthritis, psoriatic arthritis, or axial spondyloarthritis/ankylosing spondylitis confirmed through ACR-EULAR, CASPAR, and ASAS classification criteria, respectively; (b) ability to understand and speak Italian; (c) aged 18 or older; (d) reading and signing informed consent. Exclusion criteria included: (a) current or past diagnosis of psychiatric disorder; (b) current or recent (within 1 year) diagnosis of cancer; (c) current infective disease; (d) currently in psychotherapy; (e) past psychotherapy for at least 6 months within the last 6 years.
The participants were recruited during routine follow-up visits, which were conducted by rheumatologists twice a week, from May 2020 to November 2021. Before each follow-up visit, rheumatologists verified whether eligibility criteria were met by reviewing clinical records. For patients who met eligibility criteria, a research assistant presented the study and provided the informed consent after the follow-up visit. The points of the informed consent were verbally explained, including anonymity and the right to decline to participate or withdraw from the study. All invited patients agreed to participate. The study was approved by the ethics committee of Campus Bio-Medico University of Rome (n. 77/19 OSS), complied with the Declaration of Helsinki, and adhered to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies (Supplementary Table S1) (Vandenbroucke et al., 2007).
2.2 Measures
Clinical data (i.e., time since diagnosis, type of disease, number of comorbidities, presence/absence of fibromyalgia) were extracted from patients’ clinical records. Sociodemographic characteristics (i.e., age, gender, marital status, education level) and psychological measures were self-reported.
2.2.1 Euthymia
The Euthymia Scale (Carrozzino et al., 2019, 2021) is composed by 10 items, which are scored as a False/True response format. Sample items include “I am able to adjust to changing situations” and “I generally feel cheerful and in good spirits.” Higher scores indicate higher levels of euthymia.
2.2.2 Experiential avoidance
The Acceptance and Action Questionnaire-II (AAQ-II) is a 7-item self-report questionnaire designed to measure experiential avoidance (Bond et al., 2011; Pennato et al., 2013). Each item is rated on 7-point Likert scale (1 = never true; 7 = always true). Sample items include “I worry about not being able to control my worries and feelings” and “My painful experiences and memories make it difficult for me to live a life that I would value.” Higher scores indicate a greater level of experiential avoidance. Internal consistency in the original sample was good (Cronbach’s alpha = 0.88; Bond et al., 2011), while it was excellent in the present sample (Cronbach’s alpha = 0.93).
2.2.3 Cognitive reappraisal
The Emotion Regulation Questionnaire was designed to measure individual differences in the usual adoption of cognitive reappraisal and expressive suppression (Balzarotti et al., 2010; Gross and John, 2003). For the purpose of this study, only the cognitive reappraisal subscale was used. It is composed of 6 items measured on a 7-point likert scale (1 = strongly disagree; 7 = strongly agree). Sample items include “When I want to feel less negative emotion, I change the way I’m thinking about the situation” and “When I’m faced with a stressful situation, I make myself think about it in a way that helps me stay calm.” In the original validation samples, Cronbach’s alpha ranged from 0.75 to 0.82 (Gross and John, 2003). In the present study, Cronbach’s alpha was 0.83.
2.2.4 Pain intensity
Intensity of arthritic pain was measured with a Numeric Rating Scale (NRS) ranging from 0 (“no pain”) to 10 (“pain as bad as possible”). The patients were asked to rate their pain intensity in the last week. This instrument is commonly used to assess pain in arthritis (Hawker et al., 2011).
2.3 Data analysis
All statistical analyses were performed using IBM SPSS for Windows (version 22). Occasional missing values were imputed by computing the mean score of the respective sub-scale for each participant. Significant missing values were treated with listwise deletion (N = 26). Thus, analyses were conducted on 97 participants. A post-hoc power analysis (Cohen, 1988) with GPower 3.1.9.7 (Faul and Erdfelder, 1992) was conducted to check for adequacy of achieved power after excluding participants with significant missing values. Power was calculated as a function of population effect size (medium: f2 = 0.15), significance level (α = 0.05), sample size (N = 97), and number of tested predictors (i.e., experiential avoidance, cognitive reappraisal, pain intensity, type of disease) resulting in a statistical power of 0.83.
Univariate outliers were identified through z scores greater than 3.29 (p < 0.001; Tabachnick et al., 2007), whereas multivariate outliers through Mahalanobis distance (D2), Cook’s distance, and leverage values. Criteria for multivariate outliers were: (a) cases with a D2 value greater than 20.515 (i.e., D2 value at p < 0.001, 5 degrees of freedom; Tabachnick et al., 2007); (b) Cook’s distance larger than 1.00 (Tabachnick et al., 2007); (c) leverage values greater than 3(p + 1)/N = 0.1856 (p = number of predictors; N = sample size; Howell, 2012).
Independence of observations was checked through Durbin-Watson statistic. Linearity was verified through a scatterplot of studentized residuals and unstandardized predicted value for independent and dependent variables collectively. Homoscedasticity was checked through inspection of the latter scatterplot and through Breusch-Pagan test. Normality of residuals was assessed by inspecting histogram and P–P plot (Clement and Bradley-Garcia, 2022), and by following recommendations of Kim (2013) for medium-sized samples (i.e., 50 < n < 300); specifically, normality assumption was met if the absolute z-values of skewness and kurtosis were smaller than 3.29. No outliers were identified and all assumptions were met.
Descriptive statistics were performed for all variables (i.e., sociodemographic, clinical, and psychological) by calculating means and percentages for continuous and categorical variables, respectively. Pearson correlations were computed.
Moderated mediation analysis was carried out by means of PROCESS macro (Model 7; Hayes, 2013). According to the study hypothesis, pain intensity was regarded as the independent variable, euthymia as the dependent variable, experiential avoidance as the mediator, and cognitive reappraisal as the moderator. Type of disease was dummy coded (0 = rheumatoid arthritis; 1 = psoriatic arthritis; 2 = axial spondyloarthritis) and was included as a covariate to control for differences among participants, with rheumatoid arthritis serving as the reference group. Interaction variables were mean centered (Aiken and West, 1991) and simple slope analysis was used to estimate the conditional indirect effect of pain intensity on euthymia through experiential avoidance at low (−1 SD), moderate (mean), and high (+1 SD) values of the moderator. The index of moderated mediation was used to test the moderation of the indirect effect (Hayes, 2015). All models were performed with a 5,000 bootstrap sample as recommended by Hayes (2013).
3 Results
3.1 Participants characteristics
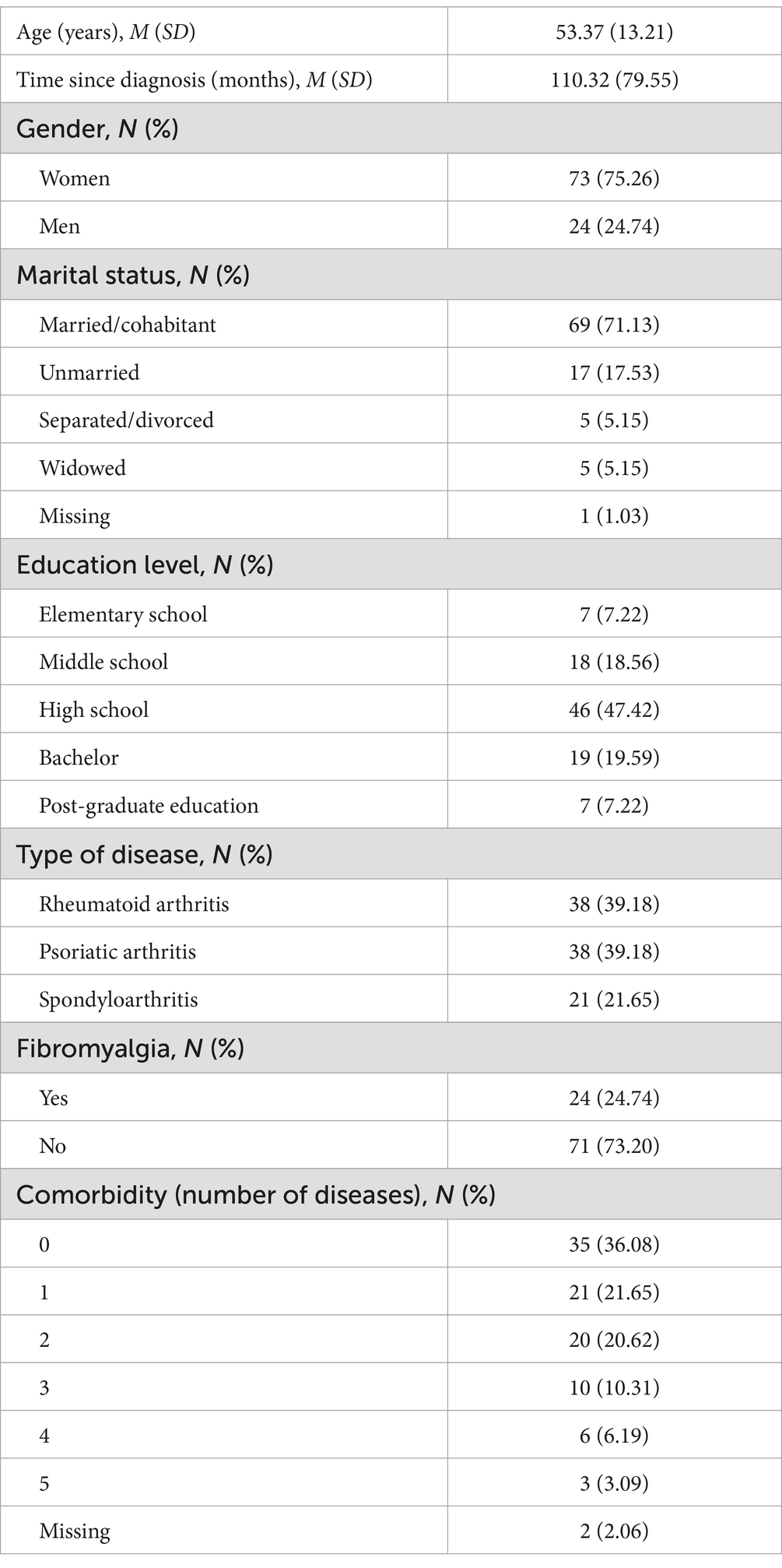
A total of 123 patients agreed to participate and completed the questionnaires. Since 26 participants were excluded due to significant missing values (listwise deletion), the final sample comprised 97 participants. Demographic and clinical characteristics of the sample are shown in Table 1. Patients had an average age of 53. The majority were women, married or cohabitant, and completed high school. With regards to clinical characteristics, patients were diagnosed since 9.19 years and most of them did not have secondary fibromyalgia, although 61.9% had at least one comorbid medical condition.
3.2 Correlation analyses
The correlation analyses showed that pain intensity was positively correlated with experiential avoidance (r = 0.39, p < 0.001) and negatively with euthymia (r = −0.35, p < 0.001). Experiential avoidance was negatively correlated with euthymia (r = −0.48, p < 0.001), whereas higher levels of cognitive reappraisal were significantly associated with higher levels of euthymia (r = 0.21, p < 0.05). The association of cognitive reappraisal with experiential avoidance was not significant. All correlations are detailed in Supplementary Table S2.
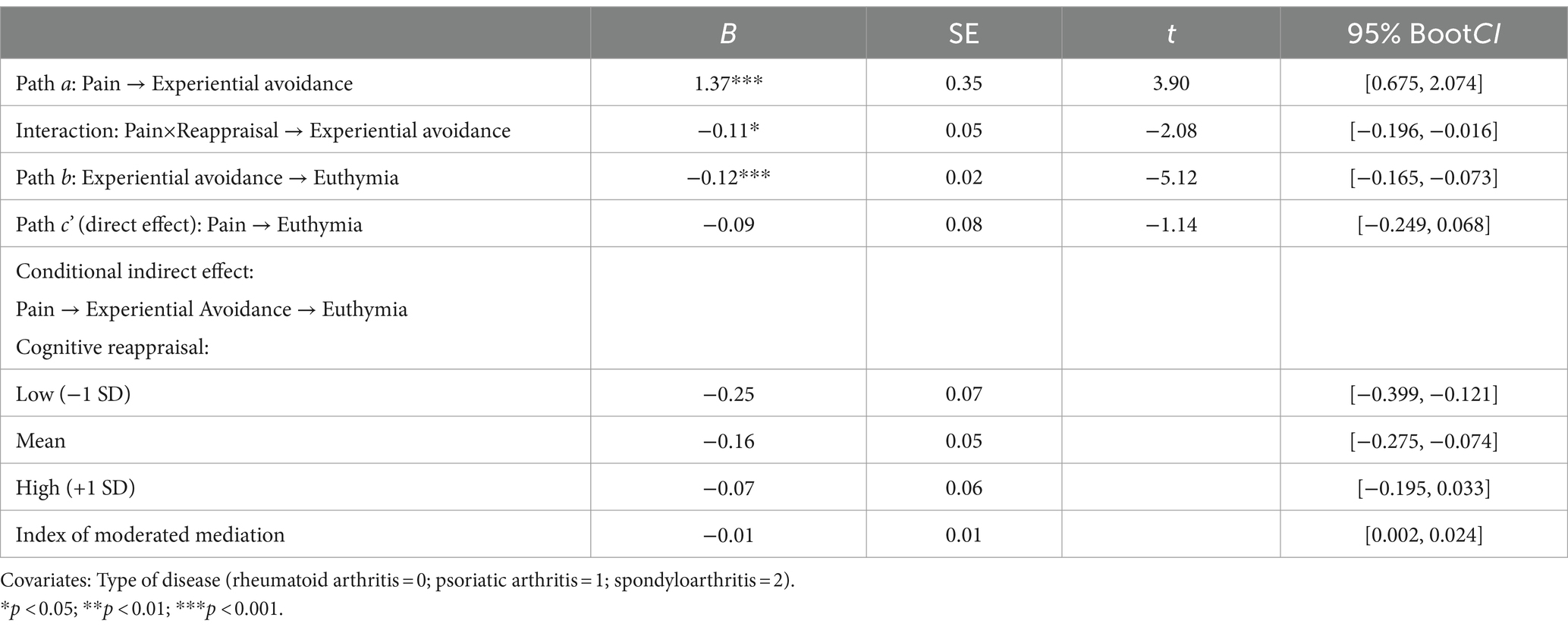
3.2.1 Moderated mediation analysis
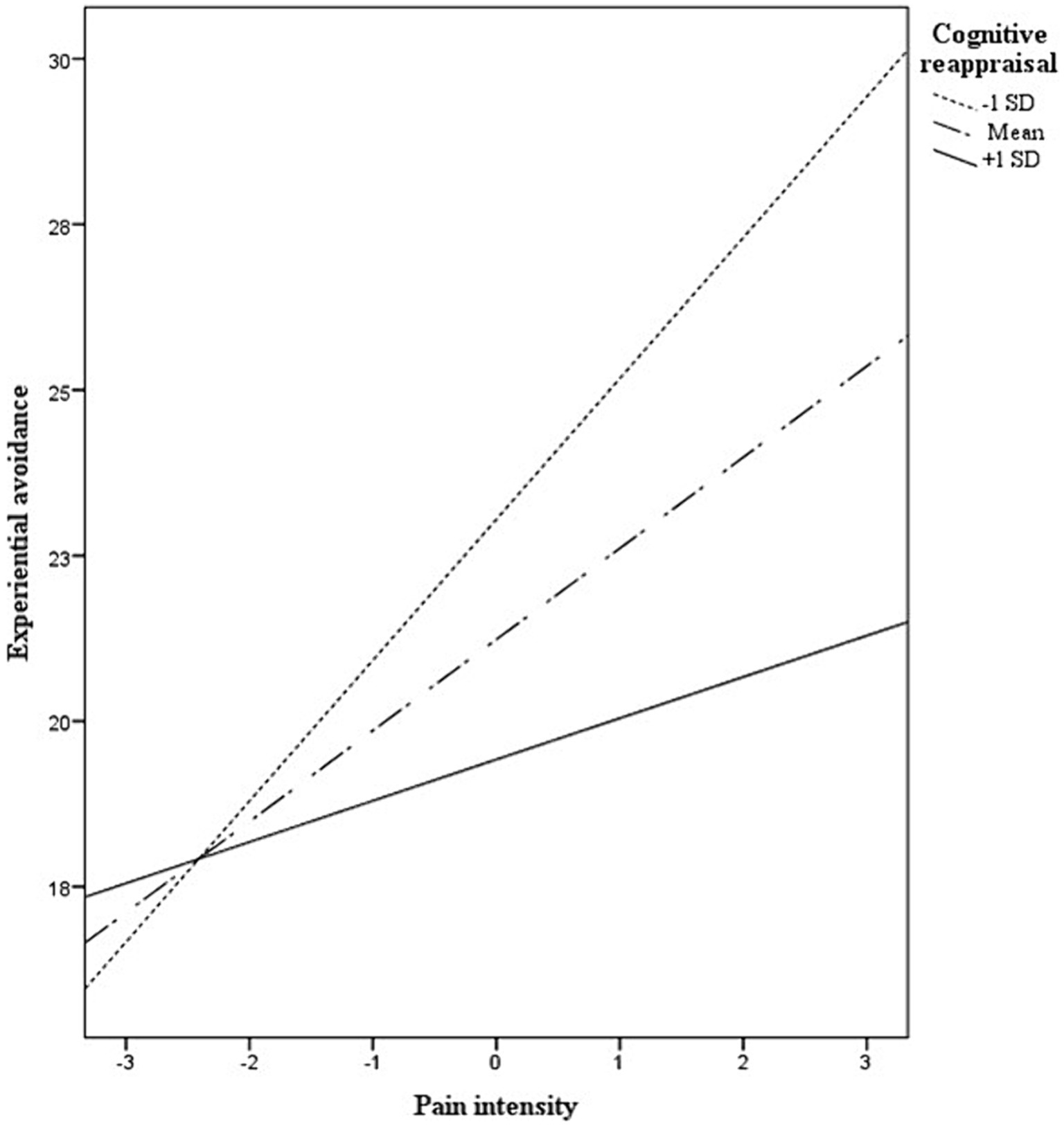
The moderated mediation analysis is shown in Table 2. The explained variance of the overall model was 35%, R2 = 0.35, F(4,92) = 13.98, p < 0.001. Specifically, the direct effect of pain intensity on euthymia (path c’) was not significant after controlling for experiential avoidance, cognitive reappraisal, its interaction with pain intensity, and type of disease (p = −0.09). The conditional indirect effect of pain intensity on euthymia by way of experiential avoidance was significant in patients with low (i.e., one SD below the mean = −7.10) and medium (i.e., mean = 0) levels of cognitive reappraisal. This effect was not significant in those with high levels (i.e., above the mean = 7.10) of cognitive reappraisal. The index of moderated mediation was significant (Table 2). Overall, the higher the cognitive reappraisal, the lower the effect of pain on euthymia through experiential avoidance. A graphical representation of the association between pain and experiential avoidance (path a) at different levels of cognitive reappraisal is provided in Figure 1. The coefficients of bootstrap results for regression model parameters are shown in Figure 2. We further explored whether the moderated mediation model was affected by covariates such as age and time since diagnosis. This analysis showed that the model did not substantially change after controlling for these covariates, R2 = 0.39, F(6,87) = 9.98, p < 0.001; index of moderated mediation = 0.01, CI95% = [0.001, 0.024].
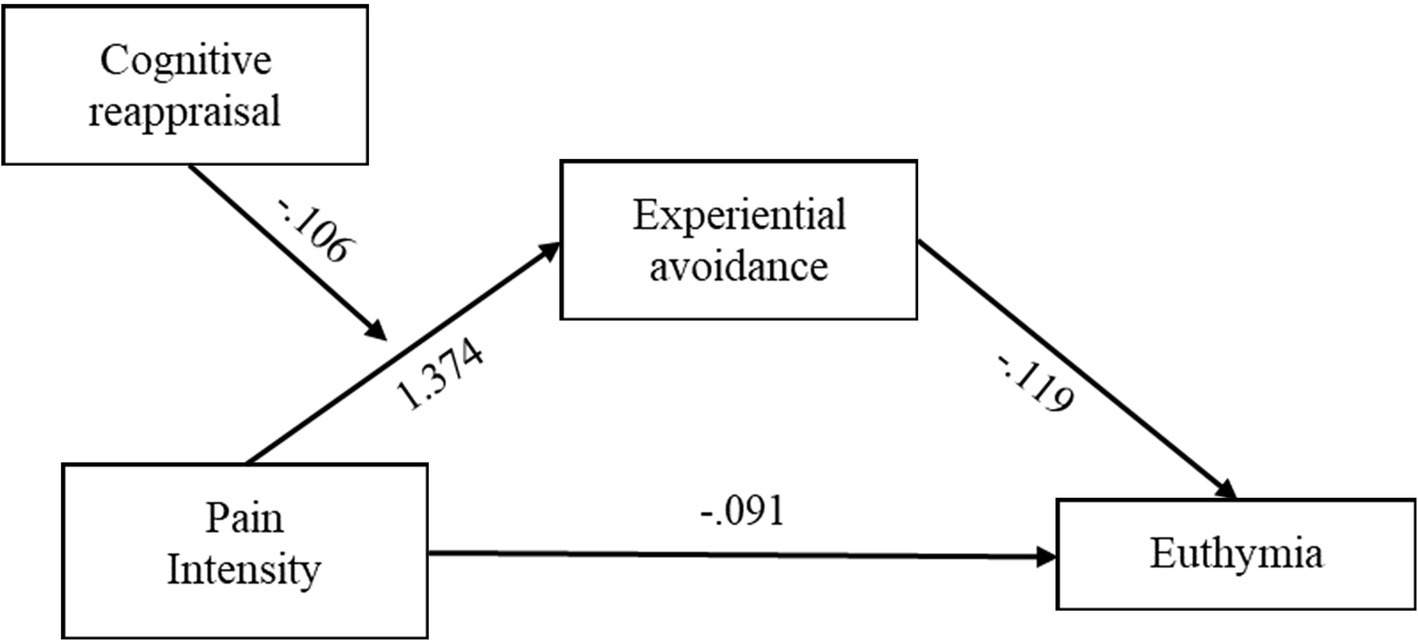
Figure 2. Conceptual moderated mediation model with coefficients of bootstrap results for regression model parameters.
4 Discussion
The main objective of this study was to investigate the link of pain intensity with well-being (i.e., euthymia) and to identify factors that contribute to better adaptation despite pain in patients with autoimmune inflammatory rheumatic diseases. Specifically, this study focused on the extent to which cognitive reappraisal, as an individual response of emotion regulation, moderates the association between pain and euthymia through experiential avoidance.
Previous research has identified psychological (in)flexibility-related constructs, such as cognitive fusion, experiential avoidance or pain acceptance, as mediators of the association between pain and disability in individuals with fibromyalgia (Varallo et al., 2022), as well as between pain and psychological distress in chronic pain (Carvalho et al., 2019; Goldbart et al., 2021) and cancer patients (Brown et al., 2020). The present study extends this knowledge beyond negative functioning by exploring how pain, cognitive reappraisal, and experiential avoidance contribute to positive outcomes, specifically euthymia, in patients with autoimmune inflammatory rheumatic diseases. Our findings indicate that patients with higher pain intensity reported increased experiential avoidance, which was associated with lower levels of euthymia. This suggests that an unwillingness to stay in contact with unpleasant inner experiences and taking action to alter or avoid them (Bond et al., 2011; Hayes et al., 1996) may explain the association between pain intensity and reduced euthymia. These results align with the psychological flexibility model (Hayes et al., 2012), which posits that psychological inflexibility is related to a lowered engagement in values-based action, thereby decreasing well-being (Hayes et al., 2012). Furthermore, the pain experience within this framework underscores how distressing cognitive content can dominate behaviour: “compelling cognitive content, such as this pain is terrible, my life is hopeless, or I am a complete failure, can have an overwhelming effect in experience where only behavior that follows or obeys what this content says can occur” (McCracken and Morley, 2014, p. 225).
Significantly, the negative effect of pain intensity on euthymia via experiential avoidance diminished as cognitive reappraisal increased. Thus, patients who effectively used cognitive reappraisal to regulate their emotions experienced improved well-being and a reduced negative impact of pain through decreased experiential avoidance. Notably, the indirect effect of pain intensity on euthymia became non-significant at high levels of cognitive reappraisal, suggesting that cognitive reappraisal may serve as a protective factor for patients with autoimmune inflammatory rheumatic diseases.
Cognitive reappraisal refers to a shift from an evaluation of an emotion-eliciting situation to another one, with a subsequent alteration of the emotional response (Faustino, 2021; Gross and John, 2003). Thus, it inherently reflects the ability of individuals in distancing from the first evaluation (Faustino, 2021). This process of distancing from initial evaluations and reappraising it in new ways may help patients manage painful stimuli and maintain higher levels of euthymia. Conversely, patients who do not engage in cognitive reappraisal may react to pain by avoiding unpleasant experiences, resulting in lower euthymia.
These findings have several clinical implications. Rather than solely targeting pain intensity, which often persists despite treatments (Carpenter et al., 2020; Sturgeon and Zautra, 2016; Sullivan and Ballantyne, 2016), improving euthymia may be achieved by addressing experiential avoidance and enhancing cognitive reappraisal. Acceptance and commitment therapy (ACT), which focuses on promoting behaviours congruent with one’s values despite internal unpleasant experiences (McCracken and Vowles, 2014), may be particularly effective. A recent systematic review showed that ACT was effective in improving emotional distress and physical functioning in patients with rheumatic diseases (Hegarty et al., 2020). However, the review included only patients with fibromyalgia and/or osteoarthritis, suggesting a lack of evidence for other rheumatic diseases. Future studies should consider extending these results in patients with rheumatoid arthritis, psoriatic arthritis, and axial spondylarthritis.
Cognitive reappraisal may be a valuable protective factor that may prevent an escalation from pain intensity to experiential avoidance, thus supporting higher euthymia. This is particularly significant considering that emotional dysregulation and past traumatic experiences typically co-occur in patients with chronic pain conditions (e.g., Nishimi et al., 2024), and are associated with increased somatic complaints (e.g., pain; Garnefski et al., 2017). Specific training fostering cognitive reappraisal may be helpful for patients with autoimmune inflammatory rheumatic diseases. Two tactics of reappraisal are distancing, involving a psychological distance from one’s construal of an emotional event, and reinterpretation, referring to the change of the meaning depicted in a stimulus (McRae et al., 2012). A longitudinal study found that both techniques reduced negative affect in healthy individuals, but only distancing showed a longitudinal reduction in perceived stress (Denny and Ochsner, 2014). Future studies may explore which cognitive reappraisal tactics may be most beneficial for patients with inflammatory rheumatic diseases to develop targeted interventions.
The results of this study should be interpreted in light of several limitations. First, the cross-sectional design of this study does not allow causal inferences. Future studies with a longitudinal design should investigate the directionality of associations between variables. Nonetheless, it is worth noting that proposed models are theoretically grounded. Second, this study relied solely on self-report measures and did not include other psychological or pain-related variables (e.g., nociceptive, neuropathic, nociplastic) that might be associated with euthymia. Third, the proposed models included only the type of autoimmune inflammatory rheumatic disease as a covariate; however, we also explored age and time since diagnosis as additional covariates. The analysis involving these additional covariates should be interpreted with caution due to limited statistical power. Future studies with a larger sample size should consider additional potential covariates to determine whether the proposed model remain significant. Fourth, a limitation is the reliance on a single measure of psychological inflexibility-related constructs. Future research could provide more comprehensive insights into the proposed associations by investigating multiple dimensions of psychological (in)flexibility (Landi et al., 2021). Furthermore, the study sample was consecutively recruited from a single clinical center, which may limit the generalizability of the findings. Finally, it should be emphasized that the study’s sample comprised patients with a variety of autoimmune inflammatory rheumatic diseases. Although the type of disease was included as a covariate in the statistical models, the associations between variables may still differ across specific diagnoses (i.e., rheumatoid arthritis, psoriatic arthritis, axial spondyloarthritis). Future research should further investigate these associations within more homogeneous subgroups to better understand how different inflammatory rheumatic disease might influence the associations among study variables. Despite these limitations, the study provides valuable and theoretically grounded insights into the role of cognitive reappraisal and experiential avoidance in managing pain in patients with autoimmune inflammatory rheumatic diseases. We found that higher pain intensity was associated with lower well-being (i.e., euthymia) through increased experiential avoidance. However, cognitive reappraisal moderated this effect, reducing the negative impact of pain. These findings highlight the potential of interventions that target experiential avoidance and enhance cognitive reappraisal to improve well-being. Future research should refine these approaches and examine their effectiveness across different rheumatic conditions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by ethics committee of Campus Bio-Medico University of Rome (n. 77/19 OSS). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FDV: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. LI: Conceptualization, Supervision, Writing – original draft. CA: Writing – original draft, Writing – review & editing. LN: Investigation, Resources, Writing – review & editing. DC: Conceptualization, Writing – review & editing. AM: Investigation, Writing – review & editing. AC: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1467555/full#supplementary-material
References
Aiken, L. S., and West, S. G. (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: SAGE Publications, Inc.
Almweisheer, S., Bernstein, C. N., Graff, L. A., Patten, S. B., Bolton, J., Fisk, J. D., et al. (2023). Well-being and flourishing mental health in adults with inflammatory bowel disease, multiple sclerosis and rheumatoid arthritis in Manitoba, Canada: a cross-sectional study. BMJ Open 13:e073782. doi: 10.1136/bmjopen-2023-073782
Balzarotti, S., John, O. P., and Gross, J. J. (2010). An Italian adaptation of the emotion regulation questionnaire. Eur. J. Psychol. Assess. 26, 61–67. doi: 10.1027/1015-5759/a000009
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., Orcutt, H. K., et al. (2011). Preliminary psychometric properties of the acceptance and action questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav. Ther. 42, 676–688. doi: 10.1016/j.beth.2011.03.007
Brown, S. L., Roush, J. F., Marshall, A. J., Jones, C., and Key, C. (2020). The intervening roles of psychological inflexibility and functional impairment in the relation between cancer-related pain and psychological distress. Int. J. Behav. Med. 27, 100–107. doi: 10.1007/s12529-019-09838-8
Carpenter, L., Barnett, R., Mahendran, P., Nikiphorou, E., Gwinnutt, J., Verstappen, S., et al. (2020). Secular changes in functional disability, pain, fatigue and mental well-being in early rheumatoid arthritis. A longitudinal meta-analysis. Semin. Arthritis Rheum. 50, 209–219. doi: 10.1016/j.semarthrit.2019.08.006
Carrozzino, D., Christensen, K. S., Mansueto, G., Brailovskaia, J., Margraf, J., and Cosci, F. (2021). A clinimetric analysis of the euthymia, resilience, and positive mental health scales. J. Affect. Disord. 294, 71–76. doi: 10.1016/j.jad.2021.07.001
Carrozzino, D., Svicher, A., Patierno, C., Berrocal, C., and Cosci, F. (2019). The euthymia scale: a clinimetric analysis. Psychother. Psychosom. 88, 119–121. doi: 10.1159/000496230
Carvalho, S. A., Pinto-Gouveia, J., Gillanders, D., and Castilho, P. (2019). Pain and depressive symptoms: exploring cognitive fusion and self-compassion in a moderated mediation model. J. Psychol. 153, 173–186. doi: 10.1080/00223980.2018.1507990
Clement, L. M., and Bradley-Garcia, M. (2022). A step-by-step tutorial for performing a moderated mediation analysis using PROCESS. Quant. Methods Psychol. 18, 258–271. doi: 10.20982/tqmp.18.3.p258
Cohen, J. (1988). Statistical power analysis for the behavioural sciences. 2nd Edn. New York, NY: Lawrence Erlbaum Associates.
Cosci, F., Svicher, A., Mansueto, G., Benemei, S., Chiarugi, A., De Cesaris, F., et al. (2021). Mental pain and pain-proneness in patients with migraine: results from the PAINMIG cohort-study. CNS Spectr. 26, 491–500. doi: 10.1017/S1092852920001480
Denny, B. T., and Ochsner, K. N. (2014). Behavioral effects of longitudinal training in cognitive reappraisal. Emotion (Washington, D.C.) 14, 425–433. doi: 10.1037/a0035276
Faul, F., and Erdfelder, E. (1992). GPOWER: A priori, post-hoc, and compromise power analyses for MS-DOS. Bonn, FRG: Bonn University.
Faustino, B. (2021). Transdiagnostic perspective on psychological inflexibility and emotional dysregulation. Behav. Cogn. Psychother. 49, 233–246. doi: 10.1017/S1352465820000600
Fava, G. A., and Bech, P. (2016). The concept of Euthymia. Psychother. Psychosom. 85, 1–5. doi: 10.1159/000441244
Fava, G. A., and Guidi, J. (2020). The pursuit of euthymia. World Psychiatry 19, 40–50. doi: 10.1002/wps.20698
Flink, I. K., Smeets, E., Bergboma, S., and Peters, M. L. (2015). Happy despite pain: pilot study of a positive psychology intervention for patients with chronic pain. Scand. J. Pain 7, 71–79. doi: 10.1016/j.sjpain.2015.01.005
Fuller-Thomson, E., Marshall, D. J., Moses, M., and Abudiab, S. (2023). Flourishing mental health despite disabling chronic pain: findings from a nationally representative sample of Canadians with arthritis. PLoS One 18:e0291722. doi: 10.1371/journal.pone.0291722
Garnefski, N., van Rood, Y., De Roos, C., and Kraaij, V. (2017). Relationships between traumatic life events, cognitive emotion regulation strategies, and somatic complaints. J. Clin. Psychol. Med. Settings 24, 144–151. doi: 10.1007/s10880-017-9494-y
Goldbart, A., Bodner, E., and Shrira, A. (2021). The role of emotion covariation and psychological flexibility in coping with chronic physical pain: an integrative model. Psychol. Health 36, 1299–1313. doi: 10.1080/08870446.2020.1841766
Goubert, L., and Trompetter, H. (2017). Towards a science and practice of resilience in the face of pain. Eur. J. Pain 21, 1301–1315. doi: 10.1002/ejp.1062
Gross, J. J. (2008). “Emotion regulation” in Handbook of emotions. 3rd ed. Eds. M. Lewis, J. M. Haviland-Jones, and L. F. Barrett (New York, NY: The Guilford Press).
Gross, J. J. (2015). Emotion regulation: current status and future prospects. Psychol. Inq. 26, 1–26. doi: 10.1080/1047840X.2014.940781
Gross, J. J., and John, O. P. (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 85, 348–362. doi: 10.1037/0022-3514.85.2.348
Guidi, J., and Fava, G. A. (2022). The clinical science of euthymia: a conceptual map. Psychother. Psychosom. 91, 156–167. doi: 10.1159/000524279
Guidi, J., Piolanti, A., Gostoli, S., Schamong, I., and Brakemeier, E. L. (2019). Mental pain and Euthymia as transdiagnostic Clinimetric indices in primary care. Psychother. Psychosom. 88, 252–253. doi: 10.1159/000501622
Hamilton, N. A., Zautra, A. J., and Reich, J. W. (2005). Affect and pain in rheumatoid arthritis: do individual differences in affective regulation and affective intensity predict emotional recovery from pain? Ann. Behav. Med. 29, 216–224. doi: 10.1207/s15324796abm2903_8
Hamilton, N. A., Zautra, A. J., and Reich, J. (2007). Individual differences in emotional processing and reactivity to pain among older women with rheumatoid arthritis. Clin. J. Pain 23, 165–172. doi: 10.1097/ajp.0b013e31802b4f58
Hawker, G. A., Mian, S., Kendzerska, T., and French, M. (2011). Measures of adult pain: visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res. 63, S240–S252. doi: 10.1002/acr.20543
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: The Guilford Press.
Hayes, A. F. (2015). An index and test of linear moderated mediation. Multivar. Behav. Res. 50, 1–22. doi: 10.1080/00273171.2014.962683
Hayes, S. C., Strosahl, K. D., and Wilson, K. G. (2012). Acceptance and commitment therapy. An experiential approach to behavior change. 2nd Edn. New York, NY: The Guildford Press.
Hayes, S. C., Wilson, K. G., Gifford, E. V., Follette, V. M., and Strosahl, K. (1996). Experimental avoidance and behavioral disorders: a functional dimensional approach to diagnosis and treatment. J. Consult. Clin. Psychol. 64, 1152–1168. doi: 10.1037//0022-006x.64.6.1152
Hegarty, R. S. M., Fletcher, B. D., Conner, T. S., Stebbings, S., and Treharne, G. J. (2020). Acceptance and commitment therapy for people with rheumatic disease: existing evidence and future directions. Musculoskeletal Care 18, 330–341. doi: 10.1002/msc.1464
Ishida, M., Kuroiwa, Y., Yoshida, E., Sato, M., Krupa, D., Henry, N., et al. (2018). Residual symptoms and disease burden among patients with rheumatoid arthritis in remission or low disease activity: a systematic literature review. Mod. Rheumatol. 28, 789–799. doi: 10.1080/14397595.2017.1416940
Karademas, E. C., Dimitraki, G., Papastefanakis, E., Ktistaki, G., Repa, A., Gergianaki, I., et al. (2020). Emotion regulation contributes to the well-being of patients with autoimmune diseases through illness-related emotions: a prospective study. J. Health Psychol. 25, 2096–2105. doi: 10.1177/135910531878
Keyes, C. L. M. (2002). The mental health continuum: from languishing to flourishing in life. J. Health Soc. Behav. 43, 207–222. doi: 10.2307/3090197
Keyes, C. L. M. (2005). Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consult. Clin. Psychol. 73, 539–548. doi: 10.1037/0022-006x.73.3.539
Kim, H. Y. (2013). Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor. Dent. Endod 38, 52–54. doi: 10.5395/rde.2013.38.1.52
Koechlin, H., Coakley, R., Schechter, N., Werner, C., and Kossowsky, J. (2018). The role of emotion regulation in chronic pain: a systematic literature review. J. Psychosom. Res. 107, 38–45. doi: 10.1016/j.jpsychores.2018.02.002
Kusier, A. O., and Folker, A. P. (2020). The well-being index WHO-5: hedonistic foundation and practical limitations. Med. Humanit. 46, 333–339. doi: 10.1136/medhum-2018-011636
Landi, G., Pakenham, K. I., Crocetti, E., Grandi, S., and Tossani, E. (2021). The multidimensional psychological flexibility inventory (MPFI): discriminant validity of psychological flexibility with distress. J. Contextual Behav. Sci. 21, 22–29. doi: 10.1016/j.jcbs.2021.05.004
Liu, V., Fong, W., Kwan, Y. H., and Leung, Y. Y. (2021). Residual disease burden in patients with axial spondyloarthritis and psoriatic arthritis despite low disease activity states in a multiethnic Asian population. J. Rheumatol. 48, 677–684. doi: 10.3899/jrheum.200934
Lumley, M. A., Cohen, J. L., Borszcz, G. S., Cano, A., Radcliffe, A. M., Porter, L. S., et al. (2011). Pain and emotion: a biopsychosocial review of recent research. J. Clin. Psychol. 67, 942–968. doi: 10.1002/jclp.20816
Martinez-Calderon, J., Meeus, M., Struyf, F., Miguel Morales-Asencio, J., Gijon-Nogueron, G., and Luque-Suarez, A. (2018a). The role of psychological factors in the perpetuation of pain intensity and disability in people with chronic shoulder pain: a systematic review. BMJ Open 8:e020703. doi: 10.1136/BMJOPEN-2017-020703
Martinez-Calderon, J., Struyf, F., Meeus, M., and Luque-Suarez, A. (2018b). The association between pain beliefs and pain intensity and/or disability in people with shoulder pain: a systematic review. Musculoskelet. Sci. Pract. 37, 29–57. doi: 10.1016/j.msksp.2018.06.010
McCracken, L. M., and Morley, S. (2014). The psychological flexibility model: a basis for integration and progress in psychological approaches to chronic pain management. J. Pain 15, 221–234. doi: 10.1016/j.jpain.2013.10.014
McCracken, L. M., and Vowles, K. E. (2014). Acceptance and commitment therapy and mindfulness for chronic pain: model, process, and progress. Am. Psychol. 69, 178–187. doi: 10.1037/a0035623
McCracken, L. M., and Zhao-O’Brien, J. (2010). General psychological acceptance and chronic pain: there is more to accept than the pain itself. Eur. J. Pain 14, 170–175. doi: 10.1016/j.ejpain.2009.03.004
McRae, K., Ciesielski, B., and Gross, J. J. (2012). Unpacking cognitive reappraisal: goals, tactics, and outcomes. Emotion (Washington, D.C.) 12, 250–255. doi: 10.1037/a0026351
Mease, P. J., Liu, M., Rebello, S., Kang, H., Yi, E., Park, Y., et al. (2019). Comparative disease burden in patients with rheumatoid arthritis, psoriatic arthritis, or axial Spondyloarthritis: data from two Corrona registries. Rheumatol. Ther. 6, 529–542. doi: 10.6084/m9.figshare.9725150
Melzack, R., and Casey, K. L. (1968). “Sensory, motivational and central control determinants of pain” in The skin senses. ed. D. R. Kenshalo (Springfield, IL: Thomas), 423–443.
Nishimi, K., Chen, R., Schmajuk, G., Neylan, T. C., and O’Donovan, A. (2024). Lifetime trauma exposure and arthritis in older adults. Psychosom. Med. doi: 10.1097/PSY.0000000000001331 [E-pub ahead of print].
Pennato, T., Berrocal, C., Bernini, O., and Rivas, T. (2013). Italian version of the acceptance and action questionnaire-II (AAQ-II): dimensionality, reliability, convergent and criterion validity. J. Psychopathol. Behav. Assess. 35, 552–563. doi: 10.1007/s10862-013-9355-4
Peters, M. L., Smeets, E., Feijge, M., van Breukelen, G., Andersson, G., Buhrman, M., et al. (2017). Happy despite pain. Clin. J. Pain 33, 962–975. doi: 10.1097/ajp.0000000000000494
Reiner, K., Tibi, L., and Lipsitz, J. D. (2013). Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Med. 14, 230–242. doi: 10.1111/pme.12006
Sturgeon, J. A., and Zautra, A. J. (2016). “Resilience to chronic arthritis pain is not about stopping pain that will not stop: development of a dynamic model of effective pain adaptation” in Psychosocial factors in arthritis. ed. P. Nicassio (Cham: Springer International Publishing), 133–149.
Sullivan, M. D., and Ballantyne, J. C. (2016). Must we reduce pain intensity to treat chronic pain? Pain 157, 65–69. doi: 10.1097/j.pain.0000000000000336
Tabachnick, B. G., Fidell, L. S., and Ullman, J. B. (2007). Using multivariate statistics. New York, NY: Pearson Education, Inc.
Trompetter, H. R., Mols, F., and Westerhof, G. J. (2019). Beyond adaptive mental functioning with pain as the absence of psychopathology: prevalence and correlates of flourishing in two chronic pain samples. Front. Psychol. 10:2443. doi: 10.3389/fpsyg.2019.02443
Vandenbroucke, J. P., von Elm, E., Altman, D. G., Gøtzsche, P. C., Mulrow, C. D., Pocock, S. J., et al. (2007). Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 4:e297. doi: 10.1371/journal.pmed.0040297
Varallo, G., Suso-Ribera, C., Ghiggia, A., Veneruso, M., Cattivelli, R., Guerrini Usubini, A., et al. (2022). Catastrophizing, kinesiophobia, and acceptance as mediators of the relationship between perceived pain severity, self-reported and performance-based physical function in women with fibromyalgia and obesity. J. Pain Res. 15, 3017–3029. doi: 10.2147/JPR.S370718
Vowles, K. E., McCracken, L. M., and Eccleston, C. (2007). Processes of behavior change in interdisciplinary treatment of chronic pain: contributions of pain intensity, catastrophizing, and acceptance. Eur. J. Pain 11, 779–787. doi: 10.1016/j.ejpain.2006.12.007
Vowles, K. E., McCracken, L. M., Sowden, G., and Ashworth, J. (2014). Psychological flexibility in coping with chronic pain: further examination of the brief pain coping inventory-2. Clin. J. Pain 30, 324–330. doi: 10.1097/ajp.0b013e31829ea187
Wood, A. M., and Tarrier, N. (2010). Positive clinical psychology: a new vision and strategy for integrated research and practice. Clin. Psychol. Rev. 30, 819–829. doi: 10.1016/j.cpr.2010.06.003
Keywords: euthymia, chronic pain, arthritis, psychological flexibility, experiential avoidance, cognitive reappraisal, emotion regulation, moderated mediation
Citation: De Vincenzo F, Iani L, Alessio C, Navarini L, Currado D, Marino A and Contardi A (2024) Euthymic despite pain: the role of cognitive reappraisal and experiential avoidance in autoimmune inflammatory rheumatic diseases—a cross-sectional study. Front. Psychol. 15:1467555. doi: 10.3389/fpsyg.2024.1467555
Edited by:
Juan Andrés Mercado, Pontifical University of the Holy Cross, ItalyReviewed by:
Ingrid Banovic, EA7475 Centre de Recherches sur les Fonctionnements et Dysfonctionnements Psychologiques (CRFDP), FranceAgata Benfante, University of Turin, Italy
Copyright © 2024 De Vincenzo, Iani, Alessio, Navarini, Currado, Marino and Contardi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Francesco De Vincenzo, ZnJhbmNlc2NvLmRldmluY2Vuem9AdW5pZXIuaXQ=
†Deceased
 Francesco De Vincenzo
Francesco De Vincenzo Luca Iani
Luca Iani Chiara Alessio
Chiara Alessio Luca Navarini
Luca Navarini Damiano Currado2,3
Damiano Currado2,3 Anna Contardi
Anna Contardi