- Addictive Behaviors and Quantitative Research Lab, Department of Psychology, Center for Alcohol Substance Use and Addiction, University of New Mexico, Albuquerque, NM, United States
Introduction: Mindfulness-based interventions show unique promise in treating substance use disorders among marginalized populations who face heightened stigma. The Mindful Resiliency in Recovery Model is introduced as a novel theoretical framework articulating how mindfulness training can mitigate the adverse effects of stigma, enhance psychological resilience, and facilitate sustained recovery from addiction.
Methods: The current manuscript synthesizes various models of mindfulness processes, stigma, and substance use disorder recovery to propose an integrated theoretical framework on the promise of mindfulness-based interventions in supporting recovery. Further, the current manuscript draws upon empirical literature to establish preliminary support for the premises and hypotheses of the Mindful Resiliency in Recovery Model concerning the mechanisms influencing the efficacy of mindfulness-based interventions among marginalized individuals.
Results: Preliminary evidence supports the premises of the proposed model. There is evidence to suggest that specific processes like increased present-moment awareness, acceptance, decentering, reappraisal, and savoring may be especially salient in mitigating internalized stigma and fostering resiliency in recovery. There is a need for additional research on these processes, and contextual factors that may moderate their efficacy.
Discussion: The Mindful Resiliency in Recovery Model has significant implications for optimizing mindfulness-based interventions to empower marginalized individuals to transcend stigma and actualize their capacity for wellbeing in substance use disorder recovery. It provides a roadmap for future research on the mechanisms and contextual factors affecting the efficacy of mindfulness-based interventions for marginalized and stigmatized communities. It further offers guidance to clinicians utilizing mindfulness-based interventions to support individuals experiencing stigma.
Introduction
Substance use disorder (SUD) poses a significant public health challenge, resulting in significant suffering for individuals, families, and communities (Delphin-Rittmon, 2022; Substance Abuse and Mental Health Services Administration, 2019; Lozano et al., 2012). This burden disproportionately affects individuals from marginalized backgrounds, including racial/ethnic minorities and those from lower socioeconomic status backgrounds, who often face additional barriers to treatment and recovery due to systemic inequities and discrimination (Chartier, 2010; Swan et al., 2021; Vaeth et al., 2017). Over the years, numerous empirically validated pharmacological, psychosocial, and behavioral treatments exist for SUD (Delphin-Rittmon, 2022; Marsch and Dallery, 2012). One such class of intervention approaches, mindfulness-based interventions (MBIs), have emerged as one of the most utilized third-wave behavioral treatments for SUD and other co-occurring pathologies (Korecki et al., 2020; Schwebel et al., 2020). Rooted in contemplative practices found within Eastern wisdom traditions like Buddhism, MBIs leverage non-judgmental present-moment awareness to support individuals with SUD in achieving wellbeing and recovery (Bowen et al., 2021; Kabat-Zinn, 2003). Over the last two decades, a plethora of MBIs, such as mindfulness-based relapse prevention, mindfulness-oriented recovery enhancement, and mindfulness-based cognitive therapy, have been developed and disseminated into clinical settings to support recovery from SUD (Korecki et al., 2020; Bowen et al., 2021; Garland, 2013). Importantly, despite variations in treatment design, each MBI is relatively equivalent in its efficacy (Korecki et al., 2020; Schwebel et al., 2020; Chiesa and Serretti, 2014; Li et al., 2017)—a phenomenon not unique to MBIs but found across varied psychological and behavioral treatments for SUD and other psychopathologies (Budd and Hughes, 2009; Magill et al., 2015).
Given the emergence of different MBI treatment packages targeting SUD, and their relative equivalency, there has been a growing movement to shift the focus of MBI research from merely assessing the efficacy of any given MBI to assessing the processes that make MBIs effective (Hayes et al., 2024; Lindsay and Creswell, 2019). Many theoretical frameworks have been proposed that attempt to articulate the most integral processes underlying the efficacy of MBIs—such as the Monitor and Acceptance Theory (Lindsay and Creswell, 2017) and Mindfulness-to-Meaning Theory (Garland et al., 2015). However, none of these theories have been extended to identify for whom and in what contexts specific mindfulness processes are most salient.
Mindfulness-based interventions among diverse, marginalized, and underserved groups
In this light, recent findings suggest that there may be unique benefits of MBIs for SUD among marginalized individuals specifically, particularly when compared to other empirically-supported SUD treatments like cognitive-behavioral therapy (Dela Cruz et al., 2022; Garland et al., 2016; Greenfield et al., 2018; Spears, 2019; Spears et al., 2017; Sun et al., 2022; Witkiewitz et al., 2013). A study by Witkiewitz et al. (2013) found that mindfulness-based relapse prevention was more efficacious than cognitive-behavioral relapse prevention for women with racial and ethnic minority identities involved in the criminal legal system, with those in mindfulness-based relapse prevention reporting significantly fewer drug use days and lower addiction severity at follow-up. In another study that examined individual race/ethnicity and racial group composition as moderators of mindfulness-based relapse prevention outcomes, it was demonstrated that mindfulness-based relapse prevention resulted in fewer drug use days for racial/ethnic minorities compared to non-Hispanic white individuals (Greenfield et al., 2018). Additionally, participants in groups comprising more than half racial/ethnic minority individuals had better substance use outcomes when in mindfulness-based relapse prevention versus cognitive-behavioral relapse prevention (Greenfield et al., 2018). These findings were substantiated by a recent systematic review of third-wave interventions (which include MBIs) for SUD among people of color and collectivist cultures. This review found that in the vast majority of studies, those who received a third-wave treatment showed greater improvements in at least one substance use outcome relative to controls (Dela Cruz et al., 2022). Importantly, however, few of these studies controlled for extenuating demographic factors such as socioeconomic status and other potential confounding variables often associated with racial/ethnic minority status (e.g., access to healthcare). This suggests that the observed benefits may be influenced by these unaccounted-for factors but nonetheless suggest highlight the potential effectiveness of MBIs among marginalized groups.
The unique promise of MBIs in treating SUD among stigmatized, diverse, and underserved populations is particularly compelling given the disproportionate burden of SUD on marginalized populations (Vaeth et al., 2017; Kilian et al., 2023; Lê Cook and Alegría, 2011; Zemore et al., 2018). Individuals from low-socioeconomic and racial/ethnic minority groups experience greater harm at equivalent levels of substance use (Chartier, 2010; Swan et al., 2021; Roche et al., 2015), and are also less likely to have access to, complete, and benefit from high-quality SUD treatment (Alegria et al., 2011; Lee et al., 2024; Rosales et al., 2022). Furthermore, there is a significant lack of representation in studies seeking to validate empirically-supported interventions for SUD more broadly (Chartier, 2010; Boness et al., 2023; Burlew et al., 2021), with this being especially true of trials evaluating the efficacy of MBIs (Korecki et al., 2020; Spears, 2019).
Together, the disproportionate harms of substance use among marginalized groups, the potential heightened efficacy of MBIs among marginalized populations, and the lack of representation in trials evaluating MBIs underscore a necessity for future research that not only includes more diverse samples but also delineates the factors that may explain their potentially unique efficacy for these populations. Failing to account for demographic factors like race, ethnicity, and socioeconomic in studies evaluating the efficacy of MBIs can confound research findings generally and thus effect the clinical implementation and effectiveness of MBIs. Given that marginalized individuals may experience unique stressors, such as discrimination and economic hardship, which can contribute to the development and maintenance of symptoms of SUD, it is essential to empirically examine in research settings how MBIs specifically may foster innate resilience among marginalized individuals. Thus, as the field shifts its emphasis away from focusing primarily on the outcomes of MBIs, to the processes underlying them, it will be crucial to account for whom any given empirically validated process is most salient (Boness and Witkiewitz, 2023). One potential transdiagnostic process tapped by MBIs that may be particularly relevant for underserved groups is that of stigma and its associated emotional hindrances, such as shame (Greene, 2023; Gull et al., 2023; Luoma et al., 2019).
Stigma, substance use disorder, and mindfulness-based interventions
Stigma is a complex social phenomenon characterized by stereotypes, prejudice, and discrimination toward individuals and groups based on perceived undesirable attributes and accompanying status in social hierarchies (Corrigan and Watson, 2002; Link and Phelan, 2001). Numerous models propose discrete forms of stigma across levels of context (Stangl et al., 2019; Bos et al., 2013). Public stigma refers to the negative beliefs, assumptions, and/or attitudes held by a society or cultural group, whereas self-stigma (also referred to as internalized stigma) refers to the process by which individuals become aware of, agree with, and apply these negative beliefs, assumptions, and attitudes to oneself (Stangl et al., 2019; Corrigan et al., 2011; Crocker and Major, 1989). When internalized, stigma can lead to numerous harms, such as reduced self-esteem, self-efficacy, quality of life, and interpersonal relationships, as well as increased psychological distress and avoidance of help-seeking behavior (Corrigan et al., 2011; Livingston and Boyd, 2010; Luoma et al., 2007; Schomerus et al., 2011). Shame, the central emotional experience associated with internalized stigma, can lead to social withdrawal, pathological rumination, and exacerbation of existing psychological difficulties (Luoma et al., 2019; Corrigan and Watson, 2002; Hatzenbuehler et al., 2013).
While early models of stigma tended to define and differentiate its impacts across two primary levels—public stigma vs. self-stigma (Link and Phelan, 2001; Link et al., 1989)—more recent frameworks offer nuanced depictions of how stigma manifests at varied levels of context, specifically at the levels of the individual, interpersonal, organizational, community, and public policy (Stangl et al., 2019; Bos et al., 2013; Burke et al., 2009). Further, advances in this literature have led to the identification of varied types of stigma existing at each level of context (Bos et al., 2013). For example, internalized and anticipated stigma represents stigma experiences manifesting at the level of the individual; secondary and enacted stigma represents expressions of stigma at interpersonal levels; structural stigma represents systematic biases and discriminatory practices at the level of organizations, communities, and public policies (Stangl et al., 2019; Bos et al., 2013; Sheehan et al., 2017). Additionally, while it was once assumed that individuals with stigmatized identities would inevitably experience internalized stigma (Link et al., 1989; Goffman, 2009), research has demonstrated this is not always so—with many individuals from stigmatized groups exhibiting resiliency despite existing in social systems that perpetuate stigmatizing narratives (Corrigan et al., 2011; Crocker and Major, 1989; Livingston and Boyd, 2010; Gu et al., 2023). The nuance provided by these updated frameworks allows for an improved capacity to understand not only how stigma manifests across each level, but also how these levels and types of stigma interact to compound harms (Stangl et al., 2019). These updated frameworks further highlight where opportunities for intervention and prevention may exist (Stangl et al., 2019; Gronholm et al., 2017).
These nuanced models are especially important for understanding the multi-level effects of stigma on SUD (Witkiewitz and Tucker, 2024). Globally, SUD is one of the most stigmatized psychological diagnoses (Schomerus et al., 2011; Barry et al., 2014) often falsely perpetuating notions of individuals with SUD as being unpredictable, lesser than, and personally at fault for their condition (Corrigan and Shapiro, 2010; Crisp et al., 2000). As a result, many individuals experiencing substance-related concerns face harms specific to SUD stigma, such as social rejection and discrimination in key life domains like housing, employment, and healthcare (Hatzenbuehler et al., 2013; Room, 2005; Van Boekel et al., 2013; Van Boekel et al., 2015). Importantly, individuals with SUD from marginalized communities, such as racial/ethnic minorities and individuals from low socioeconomic backgrounds, may experience even greater harm as a result of holding multiple stigmatized identities (Greene, 2023; Douglass et al., 2023). Structural inequities and social determinants of health can further exacerbate the harms of stigma, leading to greater barriers to accessing and benefiting from SUD treatment (Lê Cook and Alegría, 2011; Lee et al., 2024; Barry et al., 2014; Room, 2005). The so-called “war on drugs,” arguably better referred to as the “war on people who use drugs,” has only intensified these issues in nations like the United States by criminalizing substance use and disproportionately targeting marginalized populations, thereby perpetuating stigmatizing narratives and further increasing barriers to treatment and recovery (Earp et al., 2020; Mauer and King, 2007).
Considering the significant role of stigma experiences in exacerbating SUD symptoms and hindering recovery, particularly among marginalized populations, it is essential to identify interventions that can effectively target these processes specifically. Notably, MBIs and related third-wave interventions have shown promise in reducing self-stigma and shame across psychological disorders, including among individuals with SUD (Luoma et al., 2019; Livingston et al., 2012; Luoma et al., 2008; Mehel Tutuk and Budak, 2023; Moore et al., 2022; Stynes et al., 2022). Theory suggests that core processes such as the cultivation of non-judgmental awareness, self-compassion, and psychological flexibility in MBIs may help individuals develop a more balanced and accepting relationship with their experiences (Lindsay and Creswell, 2017; Garland et al., 2015). This, in turn, can buffer against the harms of stigma and promote resiliency (Luoma et al., 2008; Somohano and Bowen, 2022; Wong et al., 2019). However, sparse research to date has elucidated the specific mechanisms through which MBIs address stigma and shame, nor has any research sought to identify for whom these mechanisms are most salient.
Aims of the current paper
To this end, the current manuscript introduces the Mindful Resiliency in Recovery Model (MRRM), a novel framework that seeks to explain why MBIs may be particularly effective for marginalized individuals and those experiencing stigma, discrimination, and shame in the context of SUD. The MRRM builds upon current frameworks of stigma and recovery from SUD and extends these frameworks to individuals with stigmatized identities. It aims to describe a model that highlights the unique effectiveness of MBIs for stigmatized and marginalized individuals by fostering resilience to stigmatizing narratives. The MRRM represents a novel integration of existing theories, specifically tailored to address the unique challenges faced by marginalized and stigmatized individuals with SUD. Leveraging these established theories, the MRRM presents several significant advancements that surpass these individual theories when considered in isolation. As will be described in the following sections, the synthesis of these otherwise discrete theories guides the clinical application of MBIs for marginalized individuals while simultaneously identifying research opportunities that advance and clarify our understanding of the unique effectiveness of MBIs for marginalized and stigmatized groups.
It is important to note that terms like MBIs, third-wave treatments, and mindfulness and acceptance-based treatments are often conflated and, at times, differentiated from one another (Dimidjian et al., 2016; Hayes, 2004). For the purposes of the MRRM, the focus is not on the specific form of any given treatment manual, but rather on the functional processes which define it. In contrast to treatments like cognitive-behavioral therapy, the MRRM centers on treatments that emphasize changing one’s relationship to present moment experience, rather than changing the content of present moment experience. This distinction is best articulated by Crane et al. (2017) who highlight the essential components of MBIs in treating psychological disorders. As such, their definition of the core components comprising MBIs will be adopted here.
The following sections will explore the MRRM in detail, discussing its theoretical foundations, key premises, and implications for clinical practice and research. The MRRM aims to provide a comprehensive framework for understanding how MBIs can promote resiliency and recovery among individuals with SUD, especially those facing heightened stigma and marginalization. In doing so, it aims to contribute to the growing body of literature on MBIs for SUD to support the development of more effective, equitable, and contextually sensitive interventions for all communities.
The mindful resiliency in recovery model (MRRM)
Theoretical foundations
The MRRM integrates theories of mindfulness, stigma, and the role of contextual factors to explain how MBIs can support marginalized individuals in achieving recovery from SUD. As a novel integrated framework, it elucidates how mindfulness training can mitigate the adverse effects of stigma, enhance psychological resilience, and facilitate sustained recovery among those relegated to the margins of any given society or culture.
Two key theories of mindfulness, the Mindfulness-to-Meaning Theory (Garland et al., 2015) and the Monitor and Acceptance Theory (Lindsay and Creswell, 2017), provide insight into the core processes through which MBIs may promote recovery and resilience. The Mindfulness-to-Meaning Theory posits that mindfulness facilitates the generation of eudemonic meaning (i.e., meaning conducive to happiness/wellbeing), particularly in the face of adversity, through the mechanisms of decentering, reappraisal, and savoring (Garland et al., 2015). Decentering—akin to “self-as-context” in acceptance and commitment therapy (Hayes et al., 2013)—is the metacognitive state by which one disidentifies with sensory, cognitive, or emotional phenomena to achieve a reflexive distance in relation to internal experiences (Garland et al., 2015). In other words, it allows individuals to view thoughts as just thoughts, emotions just as emotions, and bodily sensations as bodily sensations without necessarily applying inherent meaning or veracity to them. Following decentering, the accompanying process of reappraisal allows for an adaptive reframing of one’s experience via an intentional shift in perspective (Garland et al., 2015). This reappraisal can further support a process of savoring whereby one’s ability to attend to and appreciate nourishing present-moment experiences is enhanced (Garland et al., 2015; Garland and Fredrickson, 2019).
Parallel to this, the Monitor and Acceptance Theory highlights the core processes of attention monitoring and acceptance as central to the efficacy of MBIs generally (Lindsay and Creswell, 2019; Lindsay and Creswell, 2017). The Monitor and Acceptance Theory proposes that attention monitoring heightens awareness of present-moment experiences whereas acceptance supports an adaptive modification to one’s relationship to the present moment (Lindsay and Creswell, 2017). While studies seeking to deliberately test both the Monitor and Acceptance Theory and Mindfulness-to-Meaning Theory are ongoing, presently, there exists a promising amount of literature supporting their utility in explaining the essential processes underlying MBIs (Sgherza et al., 2022; Simione and Saldarini, 2023; Wang et al., 2023). Yet, both theories tend to be examined in isolation from one another, without attempts to integrate the two explicitly. The MRRM is novel in that it proposes a framework by which both the Mindfulness-to-Meaning Theory and Monitor and Acceptance Theory are indeed synthesized to further explain the processes underlying the efficacy of MBIs. Specifically, the MRRM highlights how each set of processes—decentering, reappraisal, and savoring from the Mindfulness-to-Meaning Theory, and attention monitoring and acceptance from the Monitor and Acceptance Theory—work in concert to support individuals in disengaging from negative self-referential thoughts, reinterpreting their experiences more adaptively, and cultivating a non-reactive, present-focused awareness that enhances their capacity to cope with, recover from, and thrive in the face of the stigmatizing narratives. An additional unique contribution of the MRRM lies in its contextualization of mindfulness processes within the lived experiences of marginalized individuals. It proposes that the salience and efficacy of specific mindfulness processes may vary based on individual and contextual factors (see Figure 1), a consideration not fully explored in existing theoretical models.
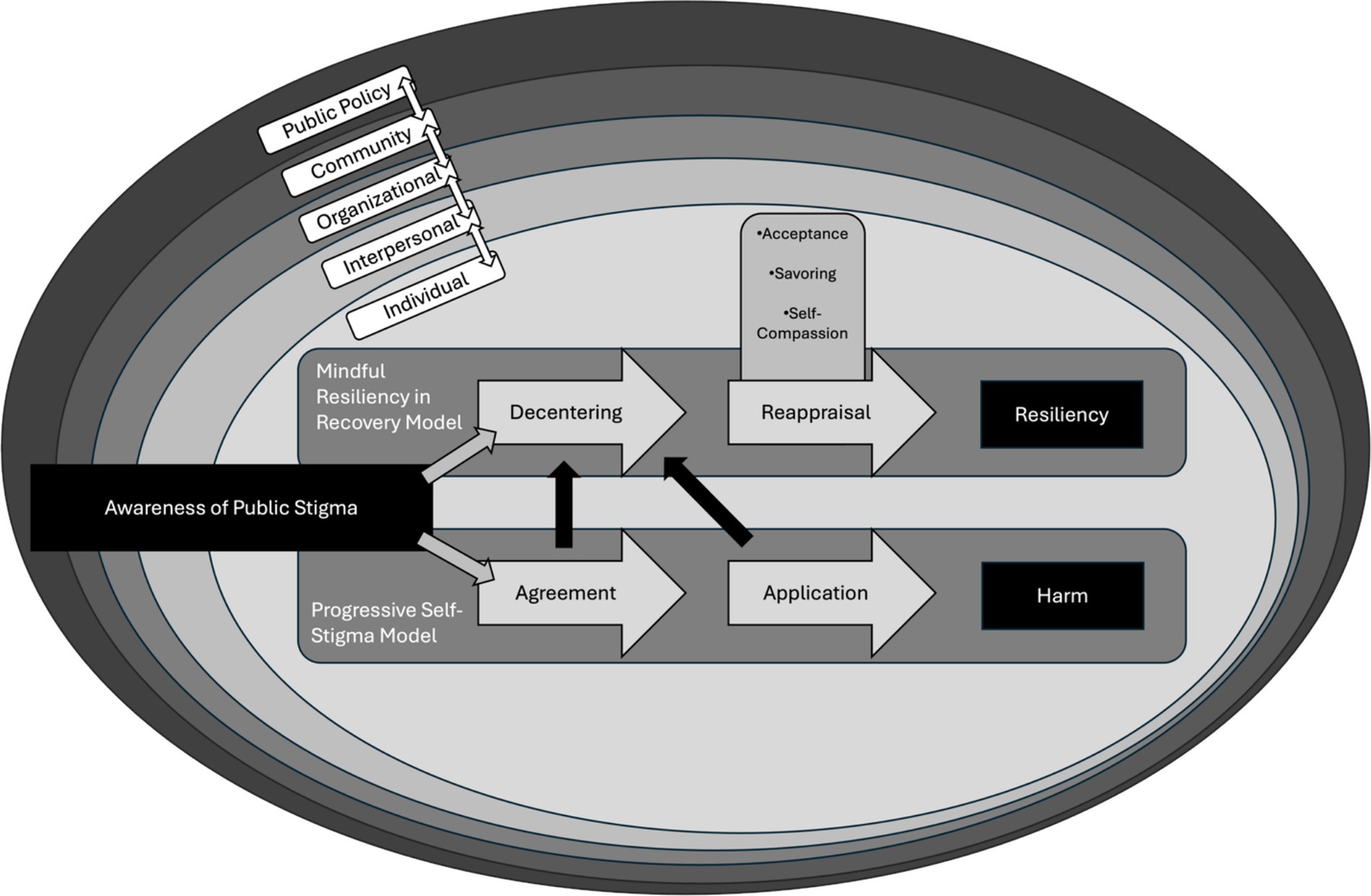
Figure 1. Visual representation of the mindful resiliency in recovery model (MRRM). At the center of the circle are two progressive paths: (1) the MRRM (path 1); (2) the Progressive Self-Stigma model (path 2). Each path represents the progression from awareness of public stigma to either (1) resiliency via the MRRM or (2) harm via the internalization of public stigma as described in the Progressive Self-Stigma model. Above the reappraisal process are additional mindfulness processes that support resiliency following decentering from stigmatizing public narratives. Note that the opportunity to decenter from the internalization of self-stigma is possible at any stage of the progressive self-stigma model as represented by the black arrows leading from path 1 to path 2. Further note how path paths 1 and 2 occur at the level of the individual, as represented by the inner-most oval (“Individual”). This inner-most oval is further surrounded by concentric ovals representing additional interdependent levels of context.
Alongside both the Monitor and Acceptance Theory and Mindfulness-to-Meaning Theory, the MRRM further integrates existing models of internalized stigma, namely the Modified Labeling Theory (Link et al., 1989) and Progressive Self-Stigma Model (Corrigan et al., 2011), to articulate the role of MBIs in fostering resilience in the face of stigmatizing social narratives. The Modified Labeling Theory proposes that individuals internalize societal beliefs (i.e., public stigma) of psychological disorders like SUD. It further articulates how the internalization of public stigma leads to detrimental self-preservation strategies like withdrawal, isolation, and self-denigration (Link et al., 1989). Extant research on the Modified Labeling Theory has demonstrated how public stigma can indeed lead to the internalization of stigma (Bos et al., 2013; Fox and Earnshaw, 2023; Glass et al., 2013). The Progressive Self-Stigma model builds upon this by delineating four distinct and progressive steps whereby public stigma results in individual harm via its internalization: (1) awareness of a stigmatizing narrative in the culture or society; (2) agreement with this narrative; (3) application of this narrative to oneself; (4) and harm as a product of applying the narrative to oneself (e.g., shame, self-contempt, isolation, etc.) (Corrigan et al., 2011). Leveraging these two frameworks, the MRRM highlights how MBIs punctuate and disrupt the progressive internalization of stigma via the mechanisms identified in the Mindfulness-to-Meaning and Monitor and Acceptance Theories. By fostering processes that enhance awareness without judgment and identification, and encourage adaptive reappraisal (e.g., self-compassion), MBIs are uniquely positioned to interrupt the internalization of public stigma. Further, even when stigma has been internalized, the MRRM highlights how these same processes found within MBIs can allow for the conscious abandonment of internalized stigma (i.e., decentering) in favor of more adaptive narratives (i.e., reappraisal; see Figure 1).
As a framework, the MRRM recognizes that the internalization of public stigma occurs within dynamic, multi-level contexts that influence recovery. Indeed, every human behavior is contextually bound, with contextual factors facilitating or hindering the reinforcement of behavior often outside the direct awareness of the individual (Burke et al., 2009; Bandura, 2006; Bouton, 2014; Witherington, 2017). Thus, when considering the core mechanisms underlying the efficacy of MBIs, and their effects on the progression and consequences of internalized stigma, it is essential to account for the ever-present nature of contextual factors that shape individual SUD recovery trajectories (Acuff et al., 2023; Tucker and Witkiewitz, 2021; Vuchinich et al., 2023). The MRRM draws upon the Dynamic Behavioral Ecological Model of Recovery (Witkiewitz and Tucker, 2024) and the Health Stigma and Discrimination Framework (Stangl et al., 2019) to articulate how MBIs support resiliency both at the individual level and at various levels of broader social-ecological contexts. Given the non-linear and dynamic nature of recovery and stigma internalization, as illuminated by the synthesis of these two frameworks, the MRRM seeks to clinically leverage and further compel research to study the flexible processes unique to MBIs that promote personalized adaptive responses to stigma-laden contexts (Moniz-Lewis et al., 2024). The MRRM further accounts for the interconnectedness between individual behavior and environmental factors (e.g., interpersonal, community, and policy factors) in the progression of internalized stigma. Including these contextual theoretical frameworks in the foundation of the MRRM alongside those previously discussed (i.e., theories of MBIs and stigma) enables the MRRM to remain theoretically coherent when accounting for the variability found across individuals and social-ecological contexts. Specifically, the MRRM accounts for this inter- and intra-contextual variability by postulating that the salience of MBI processes in promoting resilience to stigma can vary widely among individuals due to these contextual factors.
By synthesizing these theories, the MRRM offers a comprehensive framework for understanding how MBIs uniquely support individuals with SUD facing heightened stigma. Mindfulness processes like decentering, reappraisal, savoring, attention monitoring, and acceptance can buffer against the detrimental effects of self-stigma. While models like the Modified Labeling Theory focus primarily on individual level interventions, the inclusion of broader contextual frameworks within the MRRM allows for a nuanced understanding of the development of stigma-related harms for marginalized and stigmatized individuals with SUD. Thus, this framework better articulates the complex interplay between individual experiences and the social-ecological contexts shaping recovery (Witkiewitz et al., 2020).
The MRRM’s unique contribution lies in its contextualization of established mindfulness processes among marginalized individuals. It proposes that the salience and effectiveness of specific mindfulness processes may vary based on individual and contextual factors—a consideration not fully appreciated in existing models. Furthermore, the MRRM recognizes the fluidity of any individual’s social-ecological context and the dynamism inherent within it. As described in the core premises below, this model offers a theoretical expansion on existing mindfulness and stigma theories well-suited for future empirical investigation. Concurrently, it provides a practical framework for clinicians seeking to implement MBIs in a personalized and contextually sensitive manner that aligns with the complex realities of those we serve and would otherwise be less clear were these theories kept independent.
Core premises of the MRRM
Building upon this theoretical foundation, the MRRM proposes three core premises that articulate how MBIs may promote resilience and recovery among marginalized and stigmatized individuals with SUD. These premises focus on the role of mindfulness training in reducing shame and enhancing resilience, the mediating effects of specific mindfulness processes on recovery, and the impact of mindfulness training on individuals’ relationships with their evolving social-ecological contexts. Each premise contains specific hypotheses that outline the expected relationships among these factors, the mechanisms therein, and their association with one’s social-ecological context. Through these premises, the MRRM holds the two-fold aim of both (a) providing a catalyst for future research that seeks to clarify and leverage the unique potential of MBIs to support the recovery among marginalized individuals with SUD who experience stigma, and (b) highlighting discrete mechanisms and treatment kernels to be targeted by clinicians utilizing MBIs among these populations.
Each premise, along with its accompanying hypotheses, is presented below. Importantly, while these premises seek to provide added theoretical guidance for MBI clinicians, the premises and hypotheses of the MRRM are preliminary and thus warrant further empirical investigation. Nevertheless, they are presented here to inform and inspire future research, thereby advancing our understanding of the potential of MBIs in supporting recovery among marginalized individuals with SUD.
Premise 1. Mindfulness training reduces the harmful psychological and emotional impacts of stigma on individual wellbeing by enhancing resilience and promoting recovery
Hypothesis 1a. Individuals who are marginalized and/or experience stigma will show greater improvements in wellbeing and recovery-related outcomes following mindfulness training, potentially exceeding those achieved with non-third wave treatments.
Hypothesis 1b. The unique benefit of MBIs among stigmatized individuals is in part due to the effects of mindfulness training on buffering against the harms of stigma, such that reductions in internalized stigma and shame will mediate the association between mindfulness training and improved recovery outcomes.
Evidence for premise 1
While preliminary, there is indeed evidence supporting Premise 1 of the MRRM. For example, a recent study by Joseph et al. (2023) conducted secondary analysis of a randomized controlled trial comparing mindfulness-based relapse prevention to standard cognitive-behavioral relapse prevention among legal-system-involved women with SUD. They found evidence for significant reductions in internalized shame (a construct closely related to internalized stigma) across treatment conditions, with those assigned to mindfulness-based relapse prevention reporting the greatest reductions. However, it is important to note that while these findings suggest potential advantages of MBIs, the differences were not statistically significant when compared to the non-third-wave comparison group. These results are mirrored by a more recent study that found support for a mindfulness-based psychoeducation program in reducing internalized stigma among adults with SUD (Mehel Tutuk and Budak, 2023). In this study, it was shown that mindfulness-based psychoeducation resulted in a significant reduction in internalized stigma and substance use proclivity among individuals with SUD. Specifically, the study found significant improvements in the subfacets of a measure of internalized stigma, including alienation, stereotype endorsement, discrimination experience, and social withdrawal (Mehel Tutuk and Budak, 2023). However, this study did not specific an active control group. Nonetheless, the results affirm that MBIs may reduce the psychological effects of stigma and improve the overall wellbeing of stigmatized individuals. This provides initial support for Hypotheses 1a and 1b and adds to the evidence showing the beneficial effects of mindfulness in aiding recovery from SUD by reducing stigma.
Additionally, research on MBIs with marginalized youth populations provides further support for Premise 1. Murray et al. (2018) conducted a literature review examining MBIs for youth involved in the criminal legal system—a highly marginalized and stigmatized group. The review synthesized findings from 10 studies and found that participation in MBIs was associated with significant reductions in perceived stress and improvements in emotional self-regulation and anger management. While these studies did not specifically measure internalized stigma or shame, the improvements in stress reduction and self-regulation suggest that mindfulness training reduces harmful psychological impacts of stigma and promotes wellbeing among marginalized youth, aligning with Hypotheses 1a and 1b.
Another study by Gul and Aqeel (2021) examined the efficacy of an acceptance and commitment therapy intervention targeting shame and stigma among individuals with SUD. They found that relative to those in a treatment as usual condition, those who received mindfulness training via acceptance and commitment therapy demonstrated significant decreases in stigma from pre- to post-course, as well as significant decreases in shame from pre- to post-course, and at follow-up. Further, those who received mindfulness training demonstrated improvements in general mental health, quality of life, psychological flexibility, and social support. Similarly, Ghaleh Emamghaisi and Atashpour (2020) examined the efficacy of acceptance and commitment therapy in reducing shame among males who use methamphetamine. Again, it was demonstrated that those who received mindfulness training via acceptance and commitment therapy experienced significant reductions in shame compared to a control condition.
These findings are further supported by Luoma et al. (2012) who found that those who received mindfulness training via an acceptance and commitment therapy-based intervention reported smaller immediate gains in shame initially before reporting larger reductions at follow-up. Those in the intervention group also reported fewer days of substance use and greater treatment attendance at follow-up with the effects of the intervention on treatment attendance being mediated by post-treatment levels of shame. These results highlight that shame may be an important mediator in the association of mindfulness-based treatment with SUD outcomes like treatment attendance. Further, it demonstrates that approaches targeting shame that leverage mindfulness processes appear to not only reduce levels of shame but further lead to improved treatment attendance and reduced substance use among those with SUD. These findings are further bolstered by research that has demonstrated an inverse correlation between levels of mindfulness and shame-oriented cognitions, both generally (Proeve et al., 2018; Woods and Proeve, 2014) and among individuals with SUD more specifically (Luoma et al., 2019; Brem et al., 2017). Taken together, this body of research demonstrates moderate preliminary support for Premise 1 of the MRRM, highlighting how MBIs have the potential to alleviate the internalization of stigma and shame that frequently hinder SUD treatment engagement.
Premise 2. Mechanisms specific to mindfulness training found within MBIs buffer against the harms of stigma and promote resiliency in recovery
Hypothesis 2a. Mechanisms of change identified in leading theories of MBIs—specifically decentering, reappraisal (e.g., self-compassion), savoring, present moment awareness, and acceptance will mediate the relationship between MBIs and reductions in internalized stigma and shame.
Hypothesis 2b. Contextual factors will moderate this mediation effect, such that these specific mechanisms will vary based on an individual’s social-ecological context. For example, the mediating effects of reappraisal may be more moderated by one’s current recovery capital.
Evidence for premise 2
While nascent literature has examined mechanisms leading to the efficacy of MBIs in targeting shame and self-stigma, there is nonetheless preliminary evidence supporting Premise 2 of the MRRM (Luoma et al., 2008; Stynes et al., 2022; Somohano and Bowen, 2022; Luoma et al., 2012; Harris, 2015; Masuda et al., 2009; Vowles et al., 2014). Indeed, the notion that specific mechanisms inherent to MBIs mediate the association between mindfulness training and reductions in internalized stigma and shame among individuals with SUD seems highly plausible based on this literature.
For example, a recent systematic review that explored the effectiveness of MBIs in addressing self-stigma and shame evidenced numerous potential mechanisms identified in this literature (Stynes et al., 2022). Notably, most of the studies in the review were not specific to SUD but nonetheless identified transdiagnostic processes theoretically shared across MBIs and psychological disorders with similar etiological mechanisms (e.g., eating disorders) (Dimidjian et al., 2016; Hayes, 2004; Kotov et al., 2021; Michelini et al., 2021). For example, enhancing psychological flexibility, emotion regulation, and acceptance were identified as salient mechanisms of change that mediate the association of treatment and reductions in self-stigma and shame (Stynes et al., 2022; Luoma et al., 2012; Lillis et al., 2009; Neacsiu et al., 2018). Further research evidences additional mechanisms such as increased awareness, decentering, and self-compassion as core mechanisms underlying the efficacy of MBIs in reducing shame and self-stigma (Somohano and Bowen, 2022; Harris, 2015; Ellerbroek et al., 2023; Heath et al., 2018; Moore et al., 2020; Price et al., 2020; Price and Smith-DiJulio, 2016). In a pilot study of a novel MBI for women with co-occurring SUD and post-traumatic stress disorder, mixed-methods analyses demonstrated support for numerous mechanisms that mitigate the harms of stigma (Somohano and Bowen, 2022). In this study, many women reported gains in present-moment awareness, non-judgmental acceptance, and self-compassion that facilitated an increased ability to adaptively respond to negative affective states like shame (Somohano and Bowen, 2022). Similarly, in another study examining mindfulness-based relapse prevention for SUD, qualitative analysis of participant experiences demonstrated that for many individuals bringing awareness and acceptance to negative affective states, such as shame resulting from stigma, was an essential process underlying its feasibility, acceptability, and efficacy (Harris, 2015). Further, Luoma et al. (2008) evidenced support for decreased experiential avoidance (i.e., acceptance) as a process underlying the efficacy of acceptance and commitment therapy for adults with SUD. Similar findings were demonstrated in a recent study of a mindfulness and self-compassion-based intervention for adults with opioid use disorder (Moore et al., 2022). The study found that participants who underwent the MBI program demonstrated significant improvements in self-compassion from baseline to 24 weeks. Qualitative interviews revealed that participants attributed these improvements to increased present-moment awareness, self-kindness, and a greater sense of common humanity (Moore et al., 2022). Moreover, the review by Murray et al. (2018) identified improved self-regulation, stress reduction, and anger management as key outcomes of MBIs for legal system-involved youth. These mechanisms align with Hypothesis 2a, suggesting that mindfulness processes such as emotion regulation and present-moment awareness mediate the relationship between mindfulness training and reductions in psychological distress among marginalized youth. While preliminary, these findings align with Hypothesis 2a as they illustrate how mechanisms of MBIs, like self-compassion, present-moment awareness, and acceptance underly its effect in reducing internalized stigma and shame, thereby promoting recovery and resilience in individuals with SUD.
While the available evidence lends preliminary support to Hypothesis 2a, to date there is limited direct evidence for Hypothesis 2b, which posits that contextual factors moderate these mechanisms. However, the lack of evidence is not due to a lack of findings on the moderation of contextual factors but rather a lack of investigation into and appreciation for context altogether (Moniz-Lewis et al., 2024). As discussed elsewhere, the field of substance use research has largely overlooked the role of contextual factors in the recovery process, with few existing studies examining how factors such as socioeconomic status, cultural background, recovery capital, and social support might influence the effectiveness of MBIs through these mechanisms (Witkiewitz and Tucker, 2024; Tucker and Witkiewitz, 2021; Moniz-Lewis et al., 2024; Moniz-Lewis, 2024). For example, in a recent systematic review on mechanisms of change in MBIs for SUD, only 3 out of 22 studies that met the criteria for the review attended to contextual factors in any way, with no studies looking at the moderation effects of contextual factors impacting these mechanisms (Moniz-Lewis, 2024). Arguably, this lack of investigation is not merely an oversight but rather a side-effect of a predominant worldview and philosophy of science that discounts the complexities, contexts, and lived experiences of individuals from marginalized backgrounds (Burlew et al., 2021; Buchanan et al., 2021).
While there is a dire need to both investigate and appreciate the role of context in MBI research more broadly, there is nonetheless strong evidence to suggest the potential moderating roles of contextual factors in SUD recovery (Spears, 2019; Moniz-Lewis et al., 2024). For example, it has been shown that proximity to substance use outlets, financial stability, access to recovery capital (e.g., supportive social networks), and regional income equality are predictive of maintenance of recovery over time (Swan et al., 2021; Joshi et al., 2022; Pouille et al., 2021; Slutske et al., 2019). Given these findings, it is reasonable to hypothesize that contextual factors may moderate not only access to MBIs but also the efficacy of specific mindfulness mechanisms in promoting recovery from SUD—hence a moderated mediation model of contextual factors influencing mindfulness processes.
The MRRM hypothesizes that the effectiveness of mindfulness processes (e.g., reappraisal, decentering, etc.) in reducing internalized stigma and shame may vary depending on an individual’s social-ecological context. For instance, individuals in environments characterized by less stigma and greater support for recovery (e.g., non-discriminatory drug policies, access to substance-free activities, and high recovery capital) may experience enhanced benefits from mindfulness processes like reappraisal as adaptive reappraisal is reinforced by external supports. Conversely, in highly stigmatizing environments (e.g., discriminatory drug policies, legal-system involvement, incarceration, etc.), mechanisms like self-compassion may prove more crucial as individuals must rely more on internal resources to find resiliency through adversity.
This proposition aligns with ecological models of health behavior which recognize the dynamic interplay between individual health behaviors and environmental contingencies (Stangl et al., 2019). However, it is important to note that these propositions remain speculative and require empirical further investigation. Hypothesis 2b thus emphasizes the need to move beyond a context-insensitive approach to understanding mindfulness processes in SUD recovery by calling for research that explicitly examines how varied social-ecological factors may moderate the mediating effects of specific mindfulness mechanisms. Such work is critical to validate, refute, or refine Hypothesis 2b and to identify for whom and in what context a given mechanism is effective in buffering against stigma.
Premise 3. Mindfulness training bolsters individuals’ engagement with their evolving social-ecological environment, contributing to sustained improvements in recovery over time
Hypothesis 3. Those who receive mindfulness training will be more likely to experience improvements in their social-ecological contexts (e.g., social support, recovery capital, interpersonal relationships, etc.) which in turn will predict improved long-term recovery outcomes.
Evidence for premise 3
The importance of social factors in recovery is well documented through recent research on social recovery capital, defined as the extent to which an individual’s social networks support SUD recovery (Gu et al., 2023; Cano et al., 2017; Cloud and Granfield, 2008). A growing body of research supports the notion that mindfulness training can positively impact individuals’ social-ecological contexts, including social recovery capital, which in turn contributes to improved recovery outcomes for those with SUD (Gu et al., 2023; Gannon et al., 2022; LaBelle et al., 2023; Skoranski et al., 2019; Smith et al., 2020; Thiermann and Sheate, 2022). This premise is grounded in the understanding that recovery occurs within a dynamic social-ecological context, where various factors at different levels of context (e.g., individual, interpersonal, community, and public policy) interact to influence recovery processes (Stangl et al., 2019; Witkiewitz and Tucker, 2024). Indeed, research demonstrates that the benefits of mindfulness training extend beyond the individual to encompass broader contextual factors (LaBelle et al., 2023; Adair et al., 2018; Lindsay et al., 2019). Further, research on discriminatory contexts consistently demonstrates how experiences like racism, stigmatization, and discrimination can lead to isolation, withdrawal, and decreased wellbeing generally (Amaro et al., 2021; Brondolo et al., 2012). As such, an important factor explaining the efficacy of MBIs in buffering against stigma may be found in how mindfulness training changes one’s relationship with their social-ecological context.
Preliminary research suggests that social support and interpersonal functioning are key factors influenced by mindfulness training and impact one’s broader SUD recovery context. Birtel et al. (2017) found that perceived social support improved mental health outcomes among individuals with SUD and was mediated by reductions in internalized stigma and shame. Though not directly examining an MBI, when discussing their findings, the authors note that “targeting the stigma of substance [use] may not only reduce the negative psychological impact of stigma on people’s appraisals of their emotions, cognitions, and behaviors, but may also help people to utilize their social support in order to enhance their coping strategies to deal with both their primary illness as well as the stigma attached to it” (Birtel et al., 2017). Qualitative evidence from a previously discussed study (Moore et al., 2022) further supports this proposition for MBIs specifically. As mentioned, participants with opioid use disorder who engaged in mindfulness and self-compassion training reported enhanced awareness and prosocial behavior in their daily lives as a product of the training. Importantly, participants reported experiencing enhanced positive social support and engagement in their relationships following the training, which bolstered their recovery. Participants reported on the processes of enhanced mindfulness and self-compassion as being core to this shift in their relationship with their social-ecological context. A more recent study by LaBelle et al. (2023) provides additional support for the uptake of mindfulness skills leading to enhanced recovery capital. Specifically, among members of a Buddhist-based peer support program for addiction recovery, the study found that levels of mindfulness, frequency of mindfulness practice, and perceived support from peers significantly predicted recovery capital. Notably, the frequency of meditation practice was a better predictor of recovery capital than the duration of meditation practice (LaBelle et al., 2023). This suggests that consistent, regular engagement with mindfulness practices may be particularly beneficial for building and maintaining the underlying processes (e.g., acceptance, self-compassion, etc.) that lead to improved prosocial engagement with one’s recovery context. Findings such as these underscore the potential of mindfulness training to not only improve individual-level factors but also to subsequently enhance the quality of interpersonal relationships and social support networks as a result of the enhancement in these individual-level factors.
While these studies lend preliminary support for the role of mindfulness processes in enhancing social support and building recovery capital, it is important to note that research directly examining the impact of mindfulness training on broader social-ecological contexts in SUD recovery remains nascent. Therefore, there is a need for research that more explicitly tests Premise 3 to better glean how MBIs influence individuals’ relationships with their recovery context despite stigmatizing narratives.
Implications for stigmatized, marginalized, and underserved populations
Marginalized and underserved communities, who often face multiple, intersecting forms of stigma and discrimination, experience disproportionate harms from SUD relative to more dominant groups (Alegria et al., 2011; Greene, 2023; Room, 2005; Birtel et al., 2017). The compounded effects of societal marginalization and SUD-related stigma can exacerbate health disparities, impede access to quality care, and undermine recovery efforts (Lê Cook and Alegría, 2011; Van Boekel et al., 2013; Douglass et al., 2023; Morris and Schomerus, 2023). Addressing these disparities requires a multi-level approach beyond just individual-level efforts (Stangl et al., 2019; Gronholm et al., 2017). There is a dire need to change the political and social policies, practices, and narratives that perpetuate stigma and health disparities (Grisamore and DeMatteo, 2024; Koehm et al., 2024; Rehman et al., 2024). Alongside these concerted efforts to bring about greater social justice and compassion, there is a need to develop and implement contextually responsive, affirming, and efficacious interventions that attend to the unique needs and experiences of the individuals experiencing stigmatization and marginalization (Stangl et al., 2019; Mincin, 2018; Sibley et al., 2024). In other words, while social efforts are needed to address the root causes of stigma and marginalization at a social and political level, there is nonetheless a necessity to acknowledge and uplift the innate capacities of marginalized individuals and communities to remain resilient in the face of these social injustices. To that end, the MRRM offers a promising framework for identifying how MBIs may be particularly well-suited to this task by targeting key mechanisms of change that can help buffer against the harms of stigma and promote resilient recovery among marginalized individuals with SUDs.
Figure 1 provides a visual representation of the MRRM, illustrating how mindfulness processes promote resilience in the face of stigma. The diagram demonstrates the model’s unique integration of individual-level mindfulness processes within broader social-ecological contexts. At its center, two pathways diverge from the awareness of public stigma: one leading to resiliency through mindfulness processes, and the other to harm via internalized stigma. The concentric circles surrounding these two pathways represent the multiple interrelated levels of context - from individual to public policy—that remain largely beyond the scope of any given MBI yet nonetheless influence one’s recovery process. The figure further illustrates the possibility of decentering from stigmatizing narratives at any point in the processes of internalizing public stigma (i.e., the progressive-self stigma model). Further, as individuals engaged in the reappraisal process as outlined by the MRRM, additional complimentary mindfulness processes, namely acceptance, savoring, and self-compassion, can support the cultivation of innate resilience via reappraisal. This visual framework not only synthesizes the theoretical foundations of the MRRM but outlines a testable model seeking to explain how specific mindfulness processes may buffer against stigma when accounting for contextual factors. For instance, it suggests the reappraisal processes may contain differential effects depending on an individual’s position within these broader contexts, a proposition outlined by Hypothesis 2b which warrants further empirical investigation.
At the core of the MRRM lies the foundational assumption that all individuals, regardless of their race, gender, socioeconomic status, lived experiences, etc. have the innate capacity to define, discover, and lead lives of greater purpose, meaning, and wellbeing. Rooted in this assumption, the MRRM highlights key mechanisms that can be leveraged in the clinical practice of MBIs to support marginalized individuals in decentering from stigmatizing narratives and developing adaptive reappraisals of their life circumstances. Drawing upon the Mindfulness-to-Meaning Theory (Garland et al., 2015) and the Monitor and Acceptance Theory (Lindsay and Creswell, 2017), the MRRM posits that mindfulness enables individuals to become aware of and step back from the maladaptive appraisals by which public stigma becomes internalized. By instead entering a state of metacognitive awareness, the process of decentering allows for a broadening of attention and the adaptive reappraisal of one’s present moment experience—one that more accurately represents the innate capacities for wellbeing existent in all individuals.
For individuals with SUDs who come from diverse groups, these decentering and reappraisal processes could entail the acknowledgment of the innate strengths within oneself, one’s community, or one’s cultural practices, such that one’s potential for recovery is not defined by societal prejudices or negative stereotypes about addiction. Instead, one can begin to see oneself as a whole person with inherent dignity, capable of change, and connected to something greater than a limited, socially defined sense of self. This shift in perspective can be particularly empowering for marginalized individuals who may have internalized stigmatizing messages about their substance use and its implications for their identity, worth, and future opportunities. To maximize these benefits, MBIs can be adapted to explicitly integrate core mindfulness principles relevant to marginalized populations with contextual supports (Moniz-Lewis et al., 2024). For example, integrating cultural traditions, community values, and collective healing practices into mindfulness exercises can help individuals connect more deeply with their sources of innate resilience. Such adaptations not only provide a clear mediating link to specific populations but also align with the MRRM’s emphasis on contextualizing mindfulness processes within the lived experiences of marginalized individuals.
Again leveraging the Mindfulness-to-Meaning Theory, the MRRM emphasizes the role of savoring in enhancing the benefits of adaptive reappraisals (Garland et al., 2015). By mindfully attending to the positive aspects of their lives and communities, marginalized individuals in SUD recovery can tap into sources of meaning, connection, and strength that transcend their stigmatized status (Garland and Fredrickson, 2019; Garland, 2021). For example, one may savor moments of genuine connection with supportive others, experiences of personal accomplishment in their recovery journey, or the beauty and resilience they witness in their communities and culture. This savoring process can motivate values-driven behavior and the pursuit of a purposeful life, even in the face of adversity (Garland, 2021). It can help individuals build an adaptive recovery identity and cultivate hope for the future, countering the socially perpetuated stigma and shame associated with SUD (Luoma et al., 2019; Moore et al., 2020). MBIs may further support stigmatized individuals in extending kindness and understanding toward themselves, both decreasing the likelihood that public stigma becomes internalized or countering the harms of stigma if already internalized (Wong et al., 2019). By learning how to relate to oneself with compassion, even in the face of SUD-related challenges and setbacks, individuals can develop a more stable and affirming sense of self, reducing the likelihood of a return to undesired substance use in response to stigma-induced distress (Somohano and Bowen, 2022; Witkiewitz et al., 2020).
The MRRM also recognizes the importance of contextual factors, such as social support, interpersonal relationships, and access to recovery-supportive environments in buffering the impact of SUD-related stigma for marginalized individuals. No group or community is homogeneous, and as such, it is essential to acknowledge not only the moderating effects of context on individual behavior, but also the heterogeneous and varied pathways to recovery that exist for individuals from marginalized communities (Witkiewitz et al., 2020). To this end, the MRRM seeks to embrace contextual sensitivity to account for how contextual factors may impact the processes underlying the efficacy of MBIs for SUD. For example, mindfulness training, especially when conducted in group settings, may enhance marginalized individuals’ sense of belonging and social support (Greenfield et al., 2018; Spears, 2019; Witkiewitz et al., 2013; Foale et al., 2024). Participating in an MBI group with others who share similar experiences can help normalize individual struggles and reduce isolation (LaBelle et al., 2023; Russo, 2019). Furthermore, by fostering reappraisal processes such as self-compassion and forgiveness, MBIs may facilitate more adaptive responses to stigma-related interpersonal transgressions (Wong et al., 2019; Luberto et al., 2018; Miyagawa and Taniguchi, 2022; Neff, 2023). For instance, individuals may learn to accept the fears and misconceptions that underlie others’ stigmatizing beliefs, allowing for greater empathy and less personalization of negative interactions.
The premises offered by the MRRM have additional implications for clinical practice with stigmatized and marginalized populations seeking SUD treatment beyond those mentioned above. When adapting MBIs for these groups, it may be particularly beneficial to emphasize practices that cultivate self-compassion, reappraisal skills, and savoring (Moniz-Lewis et al., 2024). For example, loving-kindness meditations and self-compassion exercises can be incorporated to help individuals develop a more caring and forgiving stance toward themselves and build greater self-efficacy in being able to achieve self-defined recovery (Witkiewitz and Tucker, 2024; Chen, 2021; Hofmann et al., 2011; Moniz-Lewis et al., 2022). Cognitive reappraisal strategies can be explicitly taught and practiced, with a focus on identifying and challenging SUD-related stigmatizing beliefs (Luoma et al., 2008; Mehel Tutuk and Budak, 2023). Savoring practices found in MBIs like mindfulness-oriented recovery enhancement can be leveraged to support marginalized individuals in attending to the nourishing aspects of their lives and counteract the predominance of stigma-related self-perceptions (Garland, 2013; Bryan et al., 2022). Fostering greater awareness of stigma and its impact on SUD recovery can support increased self-acceptance and foster a sense of common humanity (Garland and Fredrickson, 2019; Chen, 2021; Shreffler et al., 2022). Further, to enhance the effectiveness of MBIs for marginalized communities, it may be beneficial to adapt these interventions by explicitly linking core mindfulness mechanisms and concepts to contextually relevant experiences. For example, this could involve tailoring reappraisal practices directly to culturally specific strengths and including collaborative discussions of how mindfulness practices can be used when experiencing discrimination or stigma generally (Moniz-Lewis et al., 2024). By doing so, the MRRM outlines direct avenues by which MBIs can be tailored to strengthen the underlying mechanisms that allow marginalized individuals to benefit from their innate resiliency when experiencing stigma. Indeed, cultural adaptions of existing MBI programs exist (Castellanos et al., 2020), and while arguably not widely yet implemented these programs offer clear examples of how MBIs can be improved to better serve those from marginalized groups.
Ultimately, the MRRM postulates that MBIs have the potential to empower marginalized and stigmatized individuals with SUDs to transcend limiting narratives and actualize their innate capacity for wellbeing. By developing decentered present-moment awareness, adaptive reappraisal (e.g., self-compassion, savoring, etc.), and a non-reactive values-driven behavior, individuals can prevent or overcome the internalization of stigma. The MRRM provides a framework for understanding and optimizing the mechanisms through which MBIs confer these benefits. Further, it offers guidance on the application of more efficacious interventions to be implemented alongside efforts to uproot systematic causes perpetuating the stigmatization of individuals with SUD.
Discussion
The current manuscript introduces the MRRM, a novel framework that seeks to explain why MBIs may be particularly effective for marginalized individuals with SUD who experience stigma and discrimination. The MRRM draws upon existing theories of mindfulness, stigma, and contextual factors in recovery to propose an integrated theoretical framework elucidating how mindfulness training can mitigate the adverse effects of stigma, enhance psychological resilience, and facilitate sustained recovery among those unjustly relegated to the margins of society.
At its foundation the MRRM synthesizes core theoretical models: the Mindfulness-to-Meaning Theory (Garland et al., 2015), the Monitor and Acceptance Theory (Lindsay and Creswell, 2017), the Modified Labeling Theory (Link et al., 1989), the Progressive Self-Stigma Model (Corrigan et al., 2011), the Dynamic Behavioral Ecological Model of Recovery (Witkiewitz and Tucker, 2024), and the Health Stigma and Discrimination Framework (Stangl et al., 2019). Through integrating these theories and frameworks, the MRRM articulates how core mindfulness processes found within MBIs buffer against the detrimental effects of self-stigma and promote resilience in the face of stigmatizing narratives. Further, it seeks to extend current work on the processes underlying the efficacy of MBIs to account for whom and in what contexts these processes are salient. In doing so, it offers a theoretical model that accounts for recent evidence suggesting a unique efficacy of third-wave treatments for individuals from marginalized groups (Dela Cruz et al., 2022; Greenfield et al., 2018; Spears, 2019; Sun et al., 2022; Witkiewitz et al., 2013), while further accounting for the role of contextual factors in moderating recovery outcomes (Witkiewitz and Tucker, 2024; Tucker and Witkiewitz, 2021).
The MRRM has significant clinical and research implications for those serving stigmatized, marginalized, and underserved populations with SUD. Clinically, the MRRM highlights the opportunity for MBIs to support marginalized individuals in decentering from stigmatizing narratives and developing adaptive reappraisals of their life circumstances, tapping into innate resources and strengths, both within the individual and their surrounding context, that transcend stigmatizing social narratives. The MRRM offers guidance when adapting MBIs for these populations, highlighting practices that target core change processes which may be especially salient in the recovery process (Moniz-Lewis et al., 2024; Venner et al., 2008).
From a research perspective, the MRRM offers a testable framework for investigating the mechanisms and contextual factors that contribute to the efficacy of MBIs among marginalized populations with SUDs. By proposing specific hypotheses related to the role of mindfulness processes in reducing internalized stigma, promoting resilience, and enhancing engagement with supportive social-ecological contexts, the MRRM provides a roadmap for future empirical work. Furthermore, the MRRM highlights the need for research on MBI adaptations tailored to the unique needs and experiences of marginalized communities, ensuring that these interventions are not only effective but also contextually sensitive. By guiding research efforts toward a more nuanced understanding of how MBIs work for whom and under what conditions, the MRRM can inform the development of more targeted and impactful interventions for marginalized individuals with SUDs.
Limitations and future research
The MRRM is not without limitations that dually serve as opportunities for future research. Importantly, the MRRM proposes three core premises that outline how MBIs may uniquely support marginalized individuals with SUDs. Alongside these premises, the MRRM presents testable hypotheses that will advance our understanding of the efficacy of MBIs for marginalized communities, the role of MBIs in mitigating the harms of stigma and promoting resiliency, and the mechanisms therein. An important current limitation of this model is that the evidence supporting each premise and its accompanying hypotheses is preliminary. As such, the MRRM is presented as a theoretical model to be updated, refined, or refuted altogether as research on the efficacy of MBIs for marginalized populations advances. Thus, future research that tests each premise of the MRRM, and its hypotheses, is essential to advancing our understanding of how MBIs can support recovery among marginalized populations who experience stigma.
An important limitation of the MRRM is the lack of clear empirical evidence directly supporting some of its sub-hypotheses, particularly those related to the moderating effects of contextual factors on mindfulness mechanisms (e.g., Hypotheses 2b and 3). While the theoretical rationale is strong and preliminary studies offer preliminary support, the absence of substantial empirical studies testing these specific hypotheses limits the current applicability of the model. This lack of direct evidence is noteworthy and highlights the need for future research to empirically validate these propositions. Without such evidence, the model remains speculative in these areas, and its practical implications should be interpreted with caution.
It is crucial to note that the vast majority of research informing the MRRM was conducted in Western cultures, primarily in a United States American context. As such, the extent to which this model accounts for the potential efficacy of MBIs in non-Western contexts is unclear. Thus, there is an additional need for future research that examines the applicability and explanatory power of the MRRM in non-Western contexts. Consequently, there is a dire need for future research on MBIs that prioritizes the inclusion of participants from various cultural, ethnic, and socioeconomic backgrounds to better understand the efficacy and processes within MBIs for these groups (Spears, 2019; Wilson et al., 2017).
Future research should further prioritize the empirical validation of the MRRM in diverse samples and settings via methods rooted in a plurality of world views (Hayes et al., 1988). Thus, methods that leverage both qualitative and quantitative investigations of the hypothesized mechanisms of MBIs’ effects on stigma-related outcomes, as well as methods that allow for the merging of nomothetic and idiographic findings are essential next steps in this literature as a whole (Hayes et al., 2024; Molenaar, 2004; Piccirillo and Rodebaugh, 2019). Research on the efficacy and acceptability of MBI adaptations tailored to specific underserved communities will be essential in translating empirical findings to direct clinical practice such that it results in a tangible positive impact on the communities these treatments seek to serve (Spears, 2019; Moniz-Lewis et al., 2024; Wilson et al., 2017). Further, given the scarcity of studies that directly examine the efficacy of MBIs in targeting stigma when compared to non-third-wave treatments (e.g., cognitive-behavioral therapy), it will be important to examine the efficacy of MBIs compared to active control groups.
Conclusion
In conclusion, the MRRM provides a novel integrated framework for better understanding and optimizing the mechanisms through which MBIs confer benefits to marginalized individuals with SUDs, specifically seeking to explain the role of stigma in the recovery processes. While the literature supporting the MRRM is preliminary, it nonetheless offers promise in empowering marginalized individuals to transcend limiting and stigmatizing social narratives and to instead actualize their innate resiliency and capacity for wellbeing. To this end, MBIs can play a vital role in uplifting marginalized individuals and mitigating the harms resulting from the disparities and social injustices that perpetuate SUD-related stigma. Through this work, we can advance the promise of MBIs as a means of promoting individual and collective wellbeing in the face of the pervasive and pernicious stigma surrounding SUDs. By empowering marginalized individuals to reclaim their narratives, actualize their innate resilience, and pursue lives of greater meaning, purpose, and wellbeing, MBIs can play a vital role in ameliorating the suffering resulting from stigma. Ultimately, this work is not only about alleviating individual suffering, but empowering all individuals, especially those that have been historically marginalized, stigmatized, and underappreciated, such that we all can collectively create a more compassionate and equitable world for all.
Data availability statement
The original contributions presented in the study are included in the article further inquiries can be directed to the corresponding author.
Author contributions
DM-L: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author declares that financial support was received for the research, authorship, and/or publication of this article. DML is supported via the National Institute on Alcohol Abuse and Alcoholism T32 Predoctoral Fellowship (5T32AA018108) and the National Institute on Drug Abuse POSITIVE Research Study (UG3/UH3DA051441).
Acknowledgments
The primary author would like to thank Katie Witkiewitz, Frank Schwebel, Megan Kirouac, and Sarah Bowen for their ongoing mentorship and for the many conversations that lead to the ideas underlying this manuscript. The primary author would further like to acknowledge that generative artificial intelligence technology was used in the editing of the manuscript. Specifically, Claude 3 Opus and Grammarly AI Writing Assistant were used to edit the manuscript to correct for grammatical and spelling mistakes. At times, Claude 3 Opus was used to provide suggested edits to the author’s original writing for improved clarity. All writing presented here is original and derives solely from the primary author.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Acuff, S. F., MacKillop, J., and Murphy, J. G. (2023). A contextualized reinforcer pathology approach to addiction. Nat Rev Psychol. 2, 309–323. doi: 10.1038/s44159-023-00167-y
Adair, K. C., Fredrickson, B. L., Castro-Schilo, L., Kim, S., and Sidberry, S. (2018). Present with you: does cultivated mindfulness predict greater social connection through gains in decentering and reductions in negative emotions? Mindfulness 9, 737–749. doi: 10.1007/s12671-017-0811-1
Alegria, M., Carson, N. J., Goncalves, M., and Keefe, K. (2011). Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. J. Am. Acad. Child Adolesc. Psychiatry 50, 22–31. doi: 10.1016/j.jaac.2010.10.005
Amaro, H., Sanchez, M., Bautista, T., and Cox, R. (2021). Social vulnerabilities for substance use: stressors, socially toxic environments, and discrimination and racism. Neuropharmacology 188:108518. doi: 10.1016/j.neuropharm.2021.108518
Bandura, A. (2006). Toward a psychology of human agency. Perspect. Psychol. Sci. 1, 164–180. doi: 10.1111/j.1745-6916.2006.00011.x
Barry, C. L., McGinty, E. E., Pescosolido, B. A., and Goldman, H. H. (2014). Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness. Psychiatr. Serv. 65, 1269–1272. doi: 10.1176/appi.ps.201400140
Birtel, M. D., Wood, L., and Kempa, N. J. (2017). Stigma and social support in substance abuse: implications for mental health and well-being. Psychiatry Res. 252, 1–8. doi: 10.1016/j.psychres.2017.01.097
Boness, C. L., Votaw, V. R., Schwebel, F. J., Moniz-Lewis, D. I. K., McHugh, R. K., and Witkiewitz, K. (2023). An evaluation of cognitive behavioral therapy for substance use disorders: a systematic review and application of the society of clinical psychology criteria for empirically supported treatments. Clin. Psychol. Sci. Pract. 30, 129–142. doi: 10.1037/cps0000131
Boness, C. L., and Witkiewitz, K. (2023). Precision medicine in alcohol use disorder: mapping etiologic and maintenance mechanisms to mechanisms of behavior change to improve patient outcomes. Exp. Clin. Psychopharmacol. 31, 769–779. doi: 10.1037/pha0000613
Bos, A. E. R., Pryor, J. B., Reeder, G. D., and Stutterheim, S. E. (2013). Stigma: advances in theory and research. Basic Appl. Soc. Psychol. 35, 1–9. doi: 10.1080/01973533.2012.746147
Bouton, M. E. (2014). Why behavior change is difficult to sustain. Prev. Med. 68, 29–36. doi: 10.1016/j.ypmed.2014.06.010
Bowen, S., Chawla, N., and Grow, J. (2021). Mindfulness-based relapse prevention for addictive behaviors: A Clinician’s guide. 2nd Edn. New York, NY: Guilford Press.
Bowen, S., Dingle, T., Laue, C., Mallik, D., and Somohano, V. C. (2021). Overlaying Buddhist and behaviorist lenses to better understand and address human suffering. Spirituality Clin Prac 8, 281–289. doi: 10.1037/scp0000275
Brem, M. J., Shorey, R. C., Anderson, S., and Stuart, G. L. (2017). Dispositional mindfulness, shame, and compulsive sexual behaviors among men in residential treatment for substance use disorders. Mindfulness 8, 1552–1558. doi: 10.1007/s12671-017-0723-0
Brondolo, E., Libretti, M., Rivera, L., and Walsemann, K. M. (2012). Racism and social capital: the implications for social and physical well-being. J. Soc. Issues 68, 358–384. doi: 10.1111/j.1540-4560.2012.01752.x
Bryan, M. A., Mallik, D., Cochran, G., and Lundahl, B. (2022). Mindfulness and savoring: a commentary on savoring strategies and their implications for addiction treatment. Subst. Use Misuse 57, 822–826. doi: 10.1080/10826084.2022.2046090
Buchanan, N. T., Perez, M., Prinstein, M. J., and Thurston, I. B. (2021). Upending racism in psychological science: strategies to change how science is conducted, reported, reviewed, and disseminated. Am. Psychol. 76, 1097–1112. doi: 10.1037/amp0000905
Budd, R., and Hughes, I. (2009). The dodo bird verdict-controversial, inevitable and important: a commentary on 30 years of meta-analyses: the dodo bird verdict: a commentary. Clin. Psychol. Psychother. 16, 510–522. doi: 10.1002/cpp.648
Burke, N. J., Joseph, G., Pasick, R. J., and Barker, J. C. (2009). Theorizing social context: rethinking behavioral theory. Health Educ. Behav. 36, 55S–70S. doi: 10.1177/1090198109335338
Burlew, K., McCuistian, C., and Szapocznik, J. (2021). Racial/ethnic equity in substance use treatment research: the way forward. Addict. Sci. Clin. Pract. 16:50. doi: 10.1186/s13722-021-00256-4
Cano, I., Best, D., Edwards, M., and Lehman, J. (2017). Recovery capital pathways: modelling the components of recovery wellbeing. Drug Alcohol Depend. 181, 11–19. doi: 10.1016/j.drugalcdep.2017.09.002
Castellanos, R., Yildiz Spinel, M., Phan, V., Orengo-Aguayo, R., Humphreys, K. L., and Flory, K. (2020). A systematic review and meta-analysis of cultural adaptations of mindfulness-based interventions for hispanic populations. Mindfulness 11, 317–332. doi: 10.1007/s12671-019-01210-x
Chartier, K. (2010). Ethnicity and health disparities in alcohol research. Alcohol Res. Health 33, 152–160.
Chen, G. (2021). The role of acceptance and change in recovery from substance use disorders. J. Psychoactive Drugs 54, 340–347. doi: 10.1080/02791072.2021.1979700
Chiesa, A., and Serretti, A. (2014). Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Subst. Use Misuse 49, 492–512. doi: 10.3109/10826084.2013.770027
Cloud, W., and Granfield, R. (2008). Conceptualizing recovery capital: expansion of a theoretical construct. Subst. Use Misuse 43, 1971–1986. doi: 10.1080/10826080802289762
Corrigan, P. W., Rafacz, J., and Rüsch, N. (2011). Examining a progressive model of self-stigma and its impact on people with serious mental illness. Psychiatry Res. 189, 339–343. doi: 10.1016/j.psychres.2011.05.024
Corrigan, P. W., and Shapiro, J. R. (2010). Measuring the impact of programs that challenge the public stigma of mental illness. Clin. Psychol. Rev. 30, 907–922. doi: 10.1016/j.cpr.2010.06.004
Corrigan, P. W., and Watson, A. C. (2002). Understanding the impact of stigma on people with mental illness. World Psychiatr. 1, 16–20.
Crane, R. S., Brewer, J., Feldman, C., Kabat-Zinn, J., Santorelli, S., Williams, J. M. G., et al. (2017). What defines mindfulness-based programs? The warp and the weft. Psychol. Med. 47, 990–999. doi: 10.1017/S0033291716003317
Crisp, A. H., Gelder, M. G., Rix, S., Meltzer, H. I., and Rowlands, O. J. (2000). Stigmatisation of people with mental illnesses. Br. J. Psychiatry 177, 4–7. doi: 10.1192/bjp.177.1.4
Crocker, J., and Major, B. (1989). Social stigma and self-esteem: the self-protective properties of stigma. Psychol. Rev. 96, 608–630. doi: 10.1037/0033-295X.96.4.608
Dela Cruz, G. A., Johnstone, S., Kim, H. S., and Castle, D. J. (2022). Review of third-wave therapies for substance use disorders in people of color and collectivist cultures: current evidence and future directions. Psychol. Addict. Behav. 37, 681–694. doi: 10.1037/adb0000883
Delphin-Rittmon, M. E. (2022). The National Survey on drug use and health 2020. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Dimidjian, S., Arch, J. J., Schneider, R. L., Desormeau, P., Felder, J. N., and Segal, Z. V. (2016). Considering meta-analysis, meaning, and metaphor: a systematic review and critical examination of “third wave” cognitive and behavioral therapies. Behav Ther 47, 886–905. doi: 10.1016/j.beth.2016.07.002
Douglass, C. H., Win, T. M., Goutzamanis, S., Lim, M. S. C., Block, K., Onsando, G., et al. (2023). Stigma associated with alcohol and other drug use among people from migrant and ethnic minority groups: results from a systematic review of qualitative studies. J Immigrant Minority Health 25, 1402–1425. doi: 10.1007/s10903-023-01468-3
Earp, B. D., Lewis, J., and Hart, C. L. (2020). Racial justice requires ending the war on drugs. Am. J. Bioeth. 21, 4–19. doi: 10.1080/15265161.2020.1861364
Ellerbroek, H., Hanssen, I., Lathouwers, K., Cillessen, L., Dekkers, S., Veldman, S. E., et al. (2023). Mindfulness-based cognitive therapy for chronic noncancer pain and prescription opioid use disorder: a qualitative pilot study of its feasibility and the perceived process of change. Brain Behav. 13:e3005. doi: 10.1002/brb3.3005
Foale, S., Botma, Y., and Heyns, T. (2024). Mindfulness-based interventions to support wellbeing of adults in low socio-economic settings: a realist review. BMC Compl Med Ther 24:52. doi: 10.1186/s12906-023-04263-7
Fox, A. B., and Earnshaw, V. A. (2023). The relationship between mental illness stigma and self-labeling. Psychiatr. Rehabil. J. 46, 127–136. doi: 10.1037/prj0000552
Gannon, M., Mackenzie, M., Short, V., Reid, L., Hand, D., and Abatemarco, D. (2022). “You can’t stop the waves, but you can learn how to surf”: realized mindfulness in practice for parenting women in recovery. Complement. Ther. Clin. Pract. 47:101549. doi: 10.1016/j.ctcp.2022.101549
Garland, E. L. (2013). Mindfulness-oriented recovery enhancement for addiction, stress, and pain. 1st Edn. Washington, DC: NASW Press.
Garland, E. L. (2021). Mindful positive emotion regulation as a treatment for addiction: from hedonic pleasure to self-transcendent meaning. Curr. Opin. Behav. Sci. 39, 168–177. doi: 10.1016/j.cobeha.2021.03.019
Garland, E. L., Farb, N. A., Goldin, P. R., and Fredrickson, B. L. (2015). The mindfulness-to-meaning theory: extensions, applications, and challenges at the attention–appraisal–emotion interface. Psychol. Inq. 26, 377–387. doi: 10.1080/1047840X.2015.1092493
Garland, E. L., and Fredrickson, B. L. (2019). Positive psychological states in the arc from mindfulness to self-transcendence: extensions of the mindfulness-to-meaning theory and applications to addiction and chronic pain treatment. Curr. Opin. Psychol. 28, 184–191. doi: 10.1016/j.copsyc.2019.01.004
Garland, E. L., Roberts-Lewis, A., Tronnier, C. D., Graves, R., and Kelley, K. (2016). Mindfulness-oriented recovery enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: proximal outcomes from a pragmatic randomized trial. Behav. Res. Ther. 77, 7–16. doi: 10.1016/j.brat.2015.11.012
Ghaleh Emamghaisi, Z., and Atashpour, S. H. (2020). Effectiveness of acceptance and commitment therapy on self-criticism and feeling of shame in methamphetamine users. J. Subst. Abus. 25, 372–376. doi: 10.1080/14659891.2019.1704082
Glass, J. E., Mowbray, O. P., Link, B. G., Kristjansson, S. D., and Bucholz, K. K. (2013). Alcohol stigma and persistence of alcohol and other psychiatric disorders: a modified labeling theory approach. Drug Alcohol Depend. 133, 685–692. doi: 10.1016/j.drugalcdep.2013.08.016
Goffman, E. (2009). Stigma: Notes on the management of spoiled identity. New York, NY: Simon and Schuster.
Greene, M. C. (2023). Commentary on Salehet al: the triple burden of stigma experienced by forcibly displaced people with substance use disorder ‐ considerations for research and practice. Addiction 118, 254–255. doi: 10.1111/add.16094
Greenfield, B. L., Roos, C., Hagler, K. J., Stein, E., Bowen, S., and Witkiewitz, K. A. (2018). Race/ethnicity and racial group composition moderate the effectiveness of mindfulness-based relapse prevention for substance use disorder. Addict. Behav. 81, 96–103. doi: 10.1016/j.addbeh.2018.02.010
Grisamore, S. P., and DeMatteo, D. (2024). Overcoming stigma: community support for overdose prevention sites. Int. J. Drug Policy 127:104415. doi: 10.1016/j.drugpo.2024.104415
Gronholm, P. C., Henderson, C., Deb, T., and Thornicroft, G. (2017). Interventions to reduce discrimination and stigma: the state of the art. Soc. Psychiatry Psychiatr. Epidemiol. 52, 249–258. doi: 10.1007/s00127-017-1341-9
Gu, W., Yang, X., Liu, X., and Xu, W. (2023). Mindfulness and negative emotions among females who inject drugs: the mediating role of social support and resilience. Int J Ment Health Addiction 21, 3627–3640. doi: 10.1007/s11469-022-00812-2
Gul, M., and Aqeel, M. (2021). Acceptance and commitment therapy for treatment of stigma and shame in substance use disorders: a double-blind, parallel-group, randomized controlled trial. J. Subst. Abus. 26, 413–419. doi: 10.1080/14659891.2020.1846803
Gull, M., Javaid, Z. K., Khan, K., and Chaudhry, H. A. (2023). Improving healthcare for substance users: the moderating role of psychological flexibility on stigma, mental health, and quality of life. Int J Hum Rights Healthcare 4, 1–12. doi: 10.1108/IJHRH-08-2023-0072
Harris, A. H. (2015). A qualitative study on the introduction of mindfulness based relapse prevention (MBRP) into a therapeutic community for substance abusers. Therap Commun Int J Ther Commun 36, 111–123. doi: 10.1108/TC-04-2014-0015
Hatzenbuehler, M. L., Phelan, J. C., and Link, B. G. (2013). Stigma as a fundamental cause of population health inequalities. Am. J. Public Health 103, 813–821. doi: 10.2105/AJPH.2012.301069
Hayes, S. C. (2004). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behav. Ther. 35, 639–665. doi: 10.1016/S0005-7894(04)80013-3
Hayes, S. C., Hayes, L. J., and Reese, H. W. (1988). Finding the philosophical core: a review of Stephen C. Pepper’s world hypotheses: a study in evidence. J. Exp. Anal. Behav. 50, 97–111. doi: 10.1901/jeab.1988.50-97
Hayes, S. C., Levin, M. E., Plumb-Vilardaga, J., Villatte, J. L., and Pistorello, J. (2013). Acceptance and commitment therapy and contextual behavioral science: examining the progress of a distinctive model of behavioral and cognitive therapy. Behav. Ther. 44, 180–198. doi: 10.1016/j.beth.2009.08.002
Hayes, S. C., Sahdra, B. K., Ciarrochi, J., Hofmann, S. G., and Sanford, B. (2024) How a process-based Idionomic approach changes our understanding of mindfulness as a method and process.
Heath, P. J., Brenner, R. E., Lannin, D. G., and Vogel, D. L. (2018). Self-compassion moderates the relationship of perceived public and anticipated self-stigma of seeking help. Stigma Health 3, 65–68. doi: 10.1037/sah0000072
Hofmann, S. G., Grossman, P., and Hinton, D. E. (2011). Loving-kindness and compassion meditation: potential for psychological interventions. Clin. Psychol. Rev. 31, 1126–1132. doi: 10.1016/j.cpr.2011.07.003
Joseph, V. W., Moniz-Lewis, D. I. K., Richards, D. K., Pearson, M. R., Luoma, J. B., and Witkiewitz, K. (2023). Internalized shame among justice-involved women in substance use disorder treatment: measurement invariance and changes during treatment. Stigma Health 9, 303–310. doi: 10.1037/sah0000427
Joshi, S., Schmidt, N. M., Thyden, N. H., Glymour, M. M., Nelson, T. F., Haynes, D. 2nd, et al. (2022). Do alcohol outlets mediate the effects of the moving to opportunity experiment on adolescent excessive drinking? A secondary analysis of a randomized controlled trial. Subst. Use Misuse 57, 1788–1796. doi: 10.1080/10826084.2022.2115847
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: past, present, and future. Clin. Psychol. Sci. Pract. 10, 144–156. doi: 10.1093/clipsy.bpg016
Kilian, C., Lemp, J. M., and Probst, C. (2023). Who benefits from alcohol screening and brief intervention? A mini-review on socioeconomic inequalities with a focus on evidence from the United States. Addict. Behav. 145:107765. doi: 10.1016/j.addbeh.2023.107765
Koehm, K., Rosen, J. G., Yedinak Gray, J. L., Tardif, J., Thompson, E., and Park, J. N. (2024). “Politics versus policy”: qualitative insights on stigma and overdose prevention center policymaking in the United States. Subst Use Addict J 28:29767342241253663. doi: 10.1177/29767342241253663
Korecki, J. R., Schwebel, F. J., Votaw, V. R., and Witkiewitz, K. (2020). Mindfulness-based programs for substance use disorders: a systematic review of manualized treatments. Subst. Abuse Treat. Prev. Policy 15, 1–18. doi: 10.1186/s13011-020-00293-3
Kotov, R., Krueger, R. F., Watson, D., Cicero, D. C., Conway, C. C., DeYoung, C. G., et al. (2021). The hierarchical taxonomy of psychopathology (HiTOP): a quantitative nosology based on consensus of evidence. Annu. Rev. Clin. Psychol. 17, 83–108. doi: 10.1146/annurev-clinpsy-081219-093304
LaBelle, O., Hastings, M., Vest, N., Meeks, M., and Lucier, K. (2023). The role of mindfulness, meditation, and peer support in recovery capital among recovery dharma members. J Subst Use Addict Treat 145:208939. doi: 10.1016/j.josat.2022.208939
Lê Cook, B., and Alegría, M. (2011). Racial-ethnic disparities in substance abuse treatment: the role of criminal history and socioeconomic status. PS 62, 1273–1281. doi: 10.1176/ps.62.11.pss6211_1273
Lee, C. A., Bonar, E. E., and Ilgen, M. A. (2024). Impact of social determinants of health and individual characteristics on substance use disorder treatment utilization among emerging adults aged 18–25. Addict. Res. Theor. 12, 1–7. doi: 10.1080/16066359.2024.2314049
Li, W., Howard, M. O., Garland, E. L., McGovern, P., and Lazar, M. (2017). Mindfulness treatment for substance misuse: a systematic review and meta-analysis. J. Subst. Abus. Treat. 75, 62–96. doi: 10.1016/j.jsat.2017.01.008
Lillis, J., Hayes, S. C., Bunting, K., and Masuda, A. (2009). Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann. Behav. Med. 37, 58–69. doi: 10.1007/s12160-009-9083-x
Lindsay, E. K., and Creswell, J. D. (2017). Mechanisms of mindfulness training: monitor and acceptance theory (MAT). Clin. Psychol. Rev. 51, 48–59. doi: 10.1016/j.cpr.2016.10.011
Lindsay, E. K., and Creswell, J. D. (2019). Mindfulness, acceptance, and emotion regulation: perspectives from monitor and acceptance theory (MAT). Curr. Opin. Psychol. 28, 120–125. doi: 10.1016/j.copsyc.2018.12.004
Lindsay, E. K., Young, S., Brown, K. W., Smyth, J. M., and Creswell, J. D. (2019). Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proc. Natl. Acad. Sci. USA 116, 3488–3493. doi: 10.1073/pnas.1813588116
Link, B. G., Cullen, F. T., Struening, E., Shrout, P. E., and Dohrenwend, B. P. (1989). A modified labeling theory approach to mental disorders: an empirical assessment. Am. Sociol. Rev. 54:400. doi: 10.2307/2095613
Link, B. G., and Phelan, J. C. (2001). Conceptualizing Stigma. Annu. Rev. Sociol. 27, 363–385. doi: 10.1146/annurev.soc.27.1.363
Livingston, J. D., and Boyd, J. E. (2010). Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc. Sci. Med. 71, 2150–2161. doi: 10.1016/j.socscimed.2010.09.030
Livingston, J. D., Milne, T., Fang, M. L., and Amari, E. (2012). The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review: reducing substance use-related stigma. Addiction 107, 39–50. doi: 10.1111/j.1360-0443.2011.03601.x
Lozano, R., Naghavi, M., Foreman, K., Lim, S., Shibuya, K., Aboyans, V., et al. (2012). Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. The Lancet 380, 2095–2128. doi: 10.1016/S0140-6736(12)61728-0
Luberto, C. M., Shinday, N., Song, R., Philpotts, L. L., Park, E. R., Fricchione, G. L., et al. (2018). A systematic review and meta-analysis of the effects of meditation on empathy, compassion, and prosocial behaviors. Mindfulness 9, 708–724. doi: 10.1007/s12671-017-0841-8
Luoma, J. B., Chwyl, C., and Kaplan, J. (2019). Substance use and shame: a systematic and meta-analytic review. Clin Psychol Rev. 70, 1–12. doi: 10.1016/j.cpr.2019.03.002
Luoma, J. B., Kohlenberg, B. S., Hayes, S. C., Bunting, K., and Rye, A. K. (2008). Reducing self-stigma in substance abuse through acceptance and commitment therapy: model, manual development, and pilot outcomes. Addict. Res. Theory 16, 149–165. doi: 10.1080/16066350701850295
Luoma, J. B., Kohlenberg, B. S., Hayes, S. C., and Fletcher, L. (2012). Slow and steady wins the race: a randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. J. Consult. Clin. Psychol. 80, 43–53. doi: 10.1037/a0026070
Luoma, J. B., Twohig, M. P., Waltz, T., Hayes, S. C., Roget, N., Padilla, M., et al. (2007). An investigation of stigma in individuals receiving treatment for substance abuse. Addict. Behav. 32, 1331–1346. doi: 10.1016/j.addbeh.2006.09.008
Magill, M., Kiluk, B. D., Mccrady, B. S., Tonigan, J. S., and Longabaugh, R. (2015). Active ingredients of treatment and client mechanisms of change in behavioral treatments for alcohol use disorders: Progress 10 years later. Alcohol. Clin. Exp. Res. 39, 1852–1862. doi: 10.1111/acer.12848
Marsch, L. A., and Dallery, J. (2012). Advances in the psychosocial treatment of addiction. Psychiatr. Clin. N. Am. 35, 481–493. doi: 10.1016/j.psc.2012.03.009
Masuda, A., Hayes, S. C., Lillis, J., Bunting, K., Herbst, S. A., and Fletcher, L. B. (2009). The relation between psychological flexibility and mental health stigma in acceptance and commitment therapy: a preliminary process investigation. Behav Soc Iss 18, 25–40. doi: 10.5210/bsi.v18i1.2525
Mauer, M., and King, R. S. (2007). A 25-year quagmire: the war on drugs and its impact on American society.
Mehel Tutuk, S. P., and Budak, F. (2023). The effect of mindfulness-based psychoeducation on internalized stigma and substance abuse proclivity in individuals with substance use disorder. J. Subst. Abus. 29, 1–9. doi: 10.1080/14659891.2023.2199847
Michelini, G., Palumbo, I. M., DeYoung, C. G., Latzman, R. D., and Kotov, R. (2021). Linking RDoC and HiTOP: a new interface for advancing psychiatric nosology and neuroscience. Clin. Psychol. Rev. 86:102025. doi: 10.1016/j.cpr.2021.102025
Mincin, J. (2018). Addiction and stigmas: overcoming labels, empowering people. New Directions Treatment Educ. Outreach Mental Health Addict. 2018, 125–131. doi: 10.1007/978-3-319-72778-3_9
Miyagawa, Y., and Taniguchi, J. (2022). Self-compassion helps people forgive transgressors: cognitive pathways of interpersonal transgressions. Self Identity 21, 244–256. doi: 10.1080/15298868.2020.1862904
Molenaar, P. C. M. (2004). A manifesto on psychology as idiographic science: bringing the person back into scientific psychology, this time forever. Measur Interdis Res Persp 2, 201–218. doi: 10.1207/s15366359mea0204_1
Moniz-Lewis, D. I. K. (2024). Processes and mechanisms of change in mindfulness-based interventions for substance use disorders: A comprehensive and contextually-sensitive systematic review. Cham: Springer.
Moniz-Lewis, D. I. K., Carlon, H. A., Hebden, H. H., Tuchman, F. R., and Witkiewitz, K. (2024). Beyond the individual: Considering contextual factors in addiction psychology. London: The SAGE Handbook of Addiction Psychology.
Moniz-Lewis, D. I. K., Stein, E. R., Bowen, S., and Witkiewitz, K. (2022). Self-efficacy as a potential mechanism of behavior change in mindfulness-based relapse prevention. Mindfulness 13, 2175–2185. doi: 10.1007/s12671-022-01946-z
Moniz-Lewis, D. I. K., Votaw, V. R., and Witkiewitz, K. (2024). Adapting mindfulness-based interventions for substance use and comorbid conditions among diverse populations. J. Health Serv. Psychol. 50, 17–26. doi: 10.1007/s42843-024-00100-8
Moore, S. K., Okst, K., Smith, L., Fatkin, T., Creedon, T., Fredericksen, A. K., et al. (2022). “Today I can look in the Mirror and like myself”: effects of a trauma-informed mindful recovery program on self-compassion. Front. Psychol. 13:780383. doi: 10.3389/fpsyg.2022.780383
Moore, K. E., Stein, M. D., Kurth, M. E., Stevens, L., Hailemariam, M., Schonbrun, Y. C., et al. (2020). Risk factors for self-stigma among incarcerated women with alcohol use disorder. Stigma Health 5, 158–167. doi: 10.1037/sah0000182
Morris, J., and Schomerus, G. (2023). Why stigma matters in addressing alcohol harm. Drug Alcohol Rev. 42, 1264–1268. doi: 10.1111/dar.13660
Murray, R., Amann, R., and Thom, K. (2018). Mindfulness-based interventions for youth in the criminal justice system: a review of the research-based literature. Psychiatry Psychol. Law 25, 829–838. doi: 10.1080/13218719.2018.1478338
Neacsiu, A. D., Rompogren, J., Eberle, J. W., and McMahon, K. (2018). Changes in problematic anger, shame, and disgust in anxious and depressed adults undergoing treatment for emotion dysregulation. Behav. Ther. 49, 344–359. doi: 10.1016/j.beth.2017.10.004
Neff, K. D. (2023). Self-compassion: theory, method, research, and intervention. Annu. Rev. Psychol. 74, 193–218. doi: 10.1146/annurev-psych-032420-031047
Piccirillo, M. L., and Rodebaugh, T. L. (2019). Foundations of idiographic methods in psychology and applications for psychotherapy. Clin. Psychol. Rev. 71, 90–100. doi: 10.1016/j.cpr.2019.01.002
Pouille, A., Bellaert, L., Vander Laenen, F., and Vanderplasschen, W. (2021). Recovery capital among migrants and ethnic minorities in recovery from problem substance use: an analysis of lived experiences. Int. J. Environ. Res. Public Health 18:13025. doi: 10.3390/ijerph182413025
Price, C. J., Merrill, J. O., McCarty, R. L., Pike, K. C., and Tsui, J. I. (2020). A pilot study of mindful body awareness training as an adjunct to office-based medication treatment of opioid use disorder. J. Subst. Abus. Treat. 108, 123–128. doi: 10.1016/j.jsat.2019.05.013
Price, C., and Smith-DiJulio, K. (2016). Interoceptive awareness is important for relapse prevention: perceptions of women who received mindful body awareness in substance use disorder treatment. J. Addict. Nurs. 27, 32–38. doi: 10.1097/JAN.0000000000000109
Proeve, M., Anton, R., and Kenny, M. (2018). Effects of mindfulness-based cognitive therapy on shame, self-compassion and psychological distress in anxious and depressed patients: a pilot study. Psychol. Psychother. Theory Res. Pract. 91, 434–449. doi: 10.1111/papt.12170
Rehman, M., Chapman, L., Liu, L., Calvert, S., and Sukhera, J. (2024). Structural stigma within inpatient care for people who inject drugs: implications for harm reduction. Harm Reduct. J. 21:53. doi: 10.1186/s12954-024-00971-6
Roche, A., Kostadinov, V., Fischer, J., Nicholas, R., O’Rourke, K., Pidd, K., et al. (2015). Addressing inequities in alcohol consumption and related harms. Health Promot. Int. 30, ii20–ii35. doi: 10.1093/heapro/dav030
Room, R. (2005). Stigma, social inequality and alcohol and drug use. Drug Alcohol Rev. 24, 143–155. doi: 10.1080/09595230500102434
Rosales, R., Janssen, T., Yermash, J., Yap, K. R., Ball, E. L., Hartzler, B., et al. (2022). Persons from racial and ethnic minority groups receiving medication for opioid use disorder experienced increased difficulty accessing harm reduction services during COVID-19. J. Subst. Abus. Treat. 132:108648. doi: 10.1016/j.jsat.2021.108648
Russo, C. (2019). The group benefits of mindfulness meditation in education and mental health care. Hum. Arenas 2, 509–515. doi: 10.1007/s42087-019-00060-2
Schomerus, G., Corrigan, P. W., Klauer, T., Kuwert, P., Freyberger, H. J., and Lucht, M. (2011). Self-stigma in alcohol dependence: consequences for drinking-refusal self-efficacy. Drug Alcohol Depend. 114, 12–17. doi: 10.1016/j.drugalcdep.2010.08.013
Schwebel, F. J., Korecki, J. R., and Witkiewitz, K. (2020). Addictive behavior change and mindfulness-based interventions: current research and future directions. Curr. Addict. Rep. 7, 117–124. doi: 10.1007/s40429-020-00302-2
Sgherza, T. R., DeMarree, K. G., and Naragon-Gainey, K. (2022). Testing the mindfulness-to-meaning theory in daily life. Mindfulness 13, 2324–2336. doi: 10.1007/s12671-022-01961-0
Sheehan, L., Nieweglowski, K., and Corrigan, P. W. (2017). “Structures and types of stigma”. in The stigma of mental illness — end of the story? Eds. W. Gaebel, W. Rössler, and N. Sartorius (Springer International Publishing/Springer Nature), 43–82.
Shreffler, J., Thomas, J. J., McGee, S., Ferguson, B., Kelley, J., Cales, R., et al. (2022). Self-compassion in individuals with substance use disorder: the association with personal growth and well-being. J. Addict. Dis. 40, 366–372. doi: 10.1080/10550887.2021.2005382
Sibley, A. L., Colston, D. C., and Go, V. F. (2024). Interventions to reduce self-stigma in people who use drugs: a systematic review. J Subst Use Addict Treatment 159:209284. doi: 10.1016/j.josat.2023.209284
Simione, L., and Saldarini, F. (2023). A critical review of the monitor and acceptance theory of mindfulness. Mindfulness 14, 1317–1328. doi: 10.1007/s12671-023-02129-0
Skoranski, A., Coatsworth, J. D., and Lunkenheimer, E. (2019). A dynamic systems approach to understanding mindfulness in interpersonal relationships. J. Child Fam. Stud. 28, 2659–2672. doi: 10.1007/s10826-019-01500-x
Slutske, W. S., Deutsch, A. R., and Piasecki, T. M. (2019). Neighborhood density of alcohol outlets moderates genetic and environmental influences on alcohol problems. Addiction 114, 815–822. doi: 10.1111/add.14534
Smith, J. M., Bright, K. S., Mader, J., Smith, J., Afzal, A. R., Patterson, C., et al. (2020). A pilot of a mindfulness based stress reduction intervention for female caregivers of youth who are experiencing substance use disorders. Addict. Behav. 103:106223. doi: 10.1016/j.addbeh.2019.106223
Somohano, V. C., and Bowen, S. (2022). Trauma-integrated mindfulness-based relapse prevention for women with comorbid post-traumatic stress disorder and substance use disorder: a cluster randomized controlled feasibility and acceptability trial. J Integ Compl Med 28, 729–738. doi: 10.1089/jicm.2021.0306
Spears, C. A. (2019). Mindfulness-based interventions for addictions among diverse and underserved populations. Curr. Opin. Psychol. 30, 11–16. doi: 10.1016/j.copsyc.2018.12.012
Spears, C. A., Houchins, S. C., Bamatter, W. P., Barrueco, S., Hoover, D. S., and Perskaudas, R. (2017). Perceptions of mindfulness in a low-income, primarily African American treatment-seeking sample. Mindfulness 8, 1532–1543. doi: 10.1007/s12671-017-0720-3
Stangl, A. L., Earnshaw, V. A., Logie, C. H., van Brakel, W., Simbayi, L., Barré, I., et al. (2019). The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 17:31. doi: 10.1186/s12916-019-1271-3
Stynes, G., Leão, C. S., and McHugh, L. (2022). Exploring the effectiveness of mindfulness-based and third wave interventions in addressing self-stigma, shame and their impacts on psychosocial functioning: a systematic review. J. Contextual Behav. Sci. 23, 174–189. doi: 10.1016/j.jcbs.2022.01.006
Substance Abuse and Mental Health Services Administration . (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19‑5068, NSDUH Series H‑54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration.
Sun, S., Goldberg, S. B., Loucks, E. B., and Brewer, J. A. (2022) Mindfulness-based interventions among people of color: a systematic review and meta-analysis. J. Society Psychotherapy Res. 32, 277–290. doi: 10.1080/10503307.2021.1937369
Swan, J. E., Aldridge, A., Joseph, V., Tucker, J. A., and Witkiewitz, K. (2021). Individual and community social determinants of health and recovery from alcohol use disorder three years following treatment. J. Psychoactive Drugs 53, 394–403. doi: 10.1080/02791072.2021.1986243
Thiermann, U. B., and Sheate, W. R. (2022). How does mindfulness affect pro-environmental behaviors? A qualitative analysis of the mechanisms of change in a sample of active practitioners. Mindfulness 13, 2997–3016. doi: 10.1007/s12671-022-02004-4
Tucker, J. A., and Witkiewitz, K. (2021). Dynamic pathways to recovery from alcohol use disorder: Meaning and methods. 1st Edn. Cambridge: Cambridge University Press.
Vaeth, P. A. C., Wang-Schweig, M., and Caetano, R. (2017). Drinking, alcohol use disorder, and treatment access and utilization among U.S. racial/ethnic groups. Alcohol. Clin. Exp. Res. 41, 6–19. doi: 10.1111/acer.13285
Van Boekel, L. C., Brouwers, E. P. M., Van Weeghel, J., and Garretsen, H. F. L. (2013). Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 131, 23–35. doi: 10.1016/j.drugalcdep.2013.02.018
Van Boekel, L. C., Brouwers, E. P., Van Weeghel, J., and Garretsen, H. F. (2015). Comparing stigmatising attitudes towards people with substance use disorders between the general public, GPs, mental health and addiction specialists and clients. Int. J. Soc. Psychiatry 61, 539–549. doi: 10.1177/0020764014562051
Venner, K. L., Feldstein, S. W., and Tafoya, N. (2008). Helping clients feel welcome: principles of adapting treatment cross-culturally. Alcohol. Treat. Q. 25, 11–30. doi: 10.1300/J020v25n04_02
Vowles, K. E., Witkiewitz, K., Sowden, G., and Ashworth, J. (2014). Acceptance and commitment therapy for chronic pain: evidence of mediation and clinically significant change following an abbreviated interdisciplinary program of rehabilitation. J. Pain 15, 101–113. doi: 10.1016/j.jpain.2013.10.002
Vuchinich, R. E., Tucker, J. A., Acuff, S. F., Reed, D. D., Buscemi, J., and Murphy, J. G. (2023). Matching, behavioral economics, and teleological behaviorism: final cause analysis of substance use and health behavior. J Exper Analysis Behav 119, 240–258. doi: 10.1002/jeab.815
Wang, Y., Garland, E. L., and Farb, N. A. S. (2023). An experimental test of the mindfulness-to-meaning theory: casual pathways between decentering, reappraisal, and well-being. Emotion 23, 2243–2258. doi: 10.1037/emo0001252
Wilson, A. D., Roos, C. R., Robinson, C. S., Stein, E. R., Manuel, J. A., Enkema, M. C., et al. (2017). Mindfulness-based interventions for addictive behaviors: implementation issues on the road ahead. Psychol. Addict. Behav. 31, 888–896. doi: 10.1037/adb0000319
Witherington, D. (2017). “Dynamic systems theory” in Advancing Developmental Science. eds. A. S. Dick and U. Mueller (London: Routledge), 41–52.
Witkiewitz, K., Greenfield, B. L., and Bowen, S. (2013). Mindfulness-based relapse prevention with racial and ethnic minority women. Addict. Behav. 38, 2821–2824. doi: 10.1016/j.addbeh.2013.08.018
Witkiewitz, K., Montes, K. S., Schwebel, F. J., and Tucker, J. A. (2020). What is recovery? Alcohol Res. 40, 1–12. doi: 10.35946/arcr.v40.3.01
Witkiewitz, K., and Tucker, J. A. (2024). Whole person recovery from substance use disorder: a call for research examining a dynamic behavioral ecological model of contexts supportive of recovery. Addict. Res. Theor. 12, 1–12. doi: 10.1080/16066359.2024.2329580
Wong, C. C. Y., Knee, C. R., Neighbors, C., and Zvolensky, M. J. (2019). Hacking stigma by loving yourself: a mediated-moderation model of self-compassion and stigma. Mindfulness 10, 415–433. doi: 10.1007/s12671-018-0984-2
Woods, H., and Proeve, M. (2014). Relationships of mindfulness, self-compassion, and meditation experience with shame-proneness. J. Cogn. Psychother. 28, 20–33. doi: 10.1891/0889-8391.28.1.20
Keywords: mindfulness, substance use disorder, stigma, addiction, marginalized populations, resilience, mechanisms of change, context
Citation: Moniz-Lewis DIK (2024) The mindful resiliency in recovery model: empowering the transcendence of stigma. Front. Psychol. 15:1460329. doi: 10.3389/fpsyg.2024.1460329
Edited by:
Vanessa Caridad Somohano, United States Department of Veterans Affairs, United StatesReviewed by:
Keith Burt, University of Vermont, United StatesAmanda Chiapa, Oregon Health and Science University, United States
Copyright © 2024 Moniz-Lewis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David I. K. Moniz-Lewis, bW9uaXpsZXdpc0B1bm0uZWR1
 David I. K. Moniz-Lewis
David I. K. Moniz-Lewis