- 1Department of Psychology, University of Konstanz, Konstanz, Germany
- 2Vivo International, Konstanz, Germany
- 3Department of Psychology, Saarland University, Saarbrücken, Germany
Background: High prevalence rates of mental disorders are reported in refugees due to experiencing substantial pre-, peri-, and post-migration stress. While long-term studies indicated that emotional distress of refugees either stagnates or ameliorates over time, long-term research on refugees’ integration and its’ interaction with emotional distress is limited. The examined long-term predictors for refugees’ emotional distress and integration in this study were, amongst others, severe physical abuse in childhood, residence status and length of stay.
Methods: The sample included 46 refugees, 91.3% male, mean age 20.8 years. Trained psychologists screened for emotional distress with the use of the Refugee Health Screener in a semi-structured interview. Integration progress was screened using the Integration Index with the subdimensions psychological, economic, political, social, linguistic and navigational integration. Longitudinal differences for emotional distress and integration sub-dimensions were evaluated by sign tests and t-tests. The longitudinal course of integration was evaluated with a Mixed ANOVA. Further, two hierarchical regression analyses were performed to analyze longitudinal predictors of emotional distress and integration.
Results: Overall, emotional distress decreased, and integration increased over time. In particular, the sub-dimensions of social, economic, and linguistic integration increased significantly over time. Two regression analyses determined significant predictors of (a) emotional distresst1 (adjusted R2 = 0.46): psychotherapy (ß = 0.35, p = 0.020), emotional distresst0 (ß = 0.34, p = 0.031), and integrationt0 (ß = −0.29, p = 0.043), and one significant predictor of (b) integrationt1 (adjusted R2 = 0.70): integrationt0 (ß = 0.89, p < 0.001).
Conclusion: This is the first study to longitudinally examine the Integration Index with all subdimensions. Over the course of 9 months refugees’ overall integration, and the sub-dimensions of social, economic, and linguistic integration increased. Whilst the emotional distress of initially highly distressed refugees ameliorated over the course of nine months, their symptom severity remained clinically significant. Results emphasize the importance of early integration for the long-term development of mental health and integration in refugees. Refugees’ emotional distress and integration are intertwined and need to be addressed promptly after refugees’ entry into the host country.
1 Introduction
In recent years, Germany has become one of the major host countries for refugees. In 2021, Germany hosted around 2.6 million refugees (United Nations High Commissioner for Refugees, 2021) and in 2023, Germany received the second highest number of new individual asylum applications, the world over (United Nations High Commissioner for Refugees, 2024). Refugees experience substantial pre-, peri-, and post-migration stress (Bogic et al., 2015). Numerous studies identified these stressful experiences as sources of emotional distress and cause of a high prevalence of mental disorders (Schick et al., 2016; Kartal et al., 2018). In addition, integration has been shown to be challenging for states, societies and health care systems (Schick et al., 2016; Kaltenbach, 2019; Silove et al., 2017) and existing approaches have often not been sufficient (German National Academy of Sciences Leopoldina, 2018; Walther et al., 2021). Further evidence of intensity and course of emotional distress in refugees, as well as the impact of emotional distress on refugees’ integration, could provide useful information for integration programs. Refugees’ access to health care service in Germany is limited and only few get the recommended treatment (German National Academy of Sciences Leopoldina, 2018; Dumke et al., 2024; Schneider et al., 2017). Structural barriers include that despite European guidelines and research recommendations a general mental health screening for all arriving refugees has not yet been implemented (German National Academy of Sciences Leopoldina, 2018; Commission E, 2018) and that during the first 18-months1, most asylum seekers in Germany did not have regular health insurance. Result is that only treatment for pain and acute illnesses, vaccinations, emergency and maternity care is covered (Bauhoff and Göpffarth, 2018; Baron and Flory, 2020). Additional services -such as psychotherapy- must be approved by municipalities on a case-by-case basis (Bauhoff and Göpffarth, 2018). The present study follows a cross-sectional assessment, conducted from 2020 to 2022, in Germany (Potter et al., 2022) that assessed adolescent refugees’ and asylum seekers’ emotional distress and integration. Subsequently, refugees2 in need of psychotherapy were referred to psychotherapist within the German health care system. Nine months after the initial assessment the intensity of emotional distress and integration was once again evaluated to assess changes and their reciprocal impact on each other. This research was conducted in a project facilitating adolescent refugees’ access to mental health services in Germany.
A recent meta-analysis emphasized the high prevalence of stress- and trauma-induced mental disorders in refugee populations (Hoell et al., 2021). Prevalence rates for newly arrived refugees in Germany were reported as high as 29.9% for post-traumatic stress disorder (PTSD), and 39.8% for depression. In adolescent refugees in Europe, Kien et al. (2019) found that up to 50% met the criteria for PTSD. Moreover, up to one-third of the sample presented with emotional or behavioral problems or met criteria for anxiety disorders or depression. Longitudinal studies examining emotional distress in refugees over varying time intervals documented stagnating as well as ameliorating emotional distress. For instance, Borho et al. (2020) reported relatively stable emotional distress levels over a course of one and a half years in a German sample. Similarly, Jakobsen et al. (2017) found refugees’ emotional distress levels to stay relatively unchanged over 26 months in a Norwegian sample. However, whilst Nikendei et al. (2019) reported that whilst posttraumatic stress and general anxiety in refugees in Germany did not significantly change over a three-month course, they observed that panic symptoms, depression, and quality of life scores improved. In accordance, a decline of psychiatric diagnoses - except PTSD - was found over a course of four to ten months in refugees in Germany (Richter et al., 2018). In refugees in Australia, psychological distress and PTSD symptoms improved over a 5 years period (Stuart and Nowosad, 2020).
Differences in the course of emotional distress may vary with social circumstances and living conditions (Richter et al., 2018) and research has proposed a dose–response relationship of post-migration stress (Ryan et al., 2008). Cross-sectional analyses elucidated the interplay of emotional distress and integration: Successful integration was found to be the best acculturation strategy for emotional well-being, followed by assimilation, marginalization, and separation (Behrens et al., 2015; Han et al., 2016). Research has repeatedly shown that refugees with mental disorders struggled to engage in integration activities, such as seeking employment or forming relationships with the host population (Phillimore, 2011). In interviews in Germany, refugees reported an interaction between their emotional distress and integration efforts across different areas of integration, e.g., how they felt overwhelmed by bureaucracy (Walther et al., 2021). Moreover, learning a new language was described to have taken a mental toll for some, e.g., for illiterate refugees, or when worries about the family that was left behind were too pressing (Walther et al., 2021). Further, they reported how mental health problems rooted in past traumata, with symptoms such as intrusions, sleeping or concentration problems, may hinder their abilities to visit an integration course or integrate into the German society (Walther et al., 2021). In this study, we follow the definition of (Harder et al., 2018), defining integration “as the degree to which immigrants have knowledge and capacity to build a successful, fulfilling life in the host society.” In this context, knowledge was defined as the skill to navigate the labor market of the host country whilst comprehending the host country’s national language, social institutions, and political system; further capacity was defined as the immigrants’ mental, social and economic assets, which might be useful to invest in their future development in the host country (Harder et al., 2018). In line with this definition integration was subdivided into six different dimensions: psychological, economic, political, navigational, social, as well as linguistic integration (Harder et al., 2018). Filling the lack of a common empirical measure of immigrant integration, the integration index allows comparisons across different immigrant groups (Harder et al., 2018). Evaluating the empirical performance of the integration index, Harder (Harder et al., 2018) completed four surveys with four different immigrant groups. They showed that the measure distinguished among these groups. In the United States a stratified sample of high-income immigrants showed an average standardized integration score of 0.8, a sample of low-income immigrants a score of 0.55, and in immigrants recently enrolled in English language classes the score was 0.46. Moreover, in a stratified sample of immigrants in Germany the score was 0.69.
Longitudinal studies examining an interplay between emotional distress and integration confirmed post-migration stressors such as loneliness, social integration stressors (Chen et al., 2019) and economic stressors (Wu et al., 2021) as relevant risk factors for refugees’ mental health. Similarly, Stuart and Nowosad (2020) found post-migration stressors such as cultural integration, financial stress and loneliness to affect refugees’ mental health more than pre-migration stressors over a course of 5 years. Moreover, Beiser (2006) showed that linguistic integration had more influence on refugees’ mental health in their later phase of resettlement than in their early phase of resettlement. However, in turn, increased psychological distress 3 years post-migration was shown to predict acculturative difficulties 20 years later (Tingvold et al., 2015). Lichtenstein and Puma (2019) examined different integration pathways in a sample of newly arrived refugees over a 4-year period in the USA and found that integration steadily increased. They further concluded that integration dimensions may evolve differently depending on the resettlement stage: While the pathways employment and economic sufficiency and language and cultural knowledge only increased in the first year of resettlement, the social bonding and social bridging pathways increased in the first and third year. Contrary to that, Schick et al. (2016) examined refugees seeking psychological treatment in outpatient clinics in Switzerland and concluded that they showed serious integration difficulties regardless of their duration of stay. Overall, longitudinal research on the detailed course of integration is still limited, and regarding subdimensions of integration almost non-existent.
Pre-migration stressors, particularly a high trauma load, were frequently associated with an elevated risk for stress related mental disorders (Kartal et al., 2018; Steel et al., 2009; Wilker et al., 2015). Especially interpersonal violence (Tinghög et al., 2017), physical abuse and other types of abuse during childhood (Margolin and Vickerman, 2011; Lindert et al., 2014) showed strong associations with mental health problems. A national cohort study accomplished by Webb et al. (2017) indicated that trauma-related hospital admissions, related to interpersonal violence or self-harm, increased the risks for later self-harm and violent criminal offending at ages 15–35 years. Hence, another factor adding to the dose–response relationship of trauma and emotional distress over time could be severe physical abuse in childhood, a pre-migration stressor with longitudinal prognostic value (Webb et al., 2017).
Regarding the impact of the residence status, studies in Australia (Silove et al., 2007), Ireland (Ryan et al., 2008), and Norway (Jakobsen et al., 2017) showed that the refusal of asylum was associated with higher levels of emotional distress over 11–26 months. Nevertheless, two reviews came to the conclusion that residence status was not a reliable predictive factor for unaccompanied refugee minors’ mental health (Höhne et al., 2020; Hornfeck et al., 2022). As another post-migration stressor, the COVID-19 pandemic has been shown to affect psychiatric disorders in refugees (Alpay et al., 2021). Moreover, several studies showed that the COVID-19 pandemic exacerbated PTSD symptoms in refugees (Kizilhan and Noll-Hussong, 2020). On top of other pre- and post-migration stressors, negative consequences of the pandemic added more strongly to the emotional distress of refugees compared to the general population (Kizilhan and Noll-Hussong, 2020; Aragona et al., 2020; Gibson et al., 2021).
Taken together, accumulating evidence indicated that emotional distress and integration within the first post-migration years are relevant predictors for the long-term integration and adaption of refugees to their new lives. A more thoroughly understanding of their interplay could help to prevent a vicious cycle between poor mental health caused from pre- and peri-migration traumata aggravated by post-migration stressors (Walther et al., 2021). Yet, integration has so far mainly been assessed in relation to social, cultural, economic, and linguistic integration. Evidence on emotional distress and its interplay with the integration status is limited, particularly of adolescent refugees. During the first cross-sectional assessment, we identified the time living under the restrictions of the pandemic and severe physical abuse in childhood as crucial predictors for emotional distress (Potter et al., 2022). Moreover, the length of stay in Germany as well as emotional distress were identified as most important predictors of integration. Aiming to assess the longitudinal impact of these factors on mental health and successful integration in refugees, the present study focused on the interplay of emotional distress and integration over the course of 9 months.
2 Methods
2.1 Sample
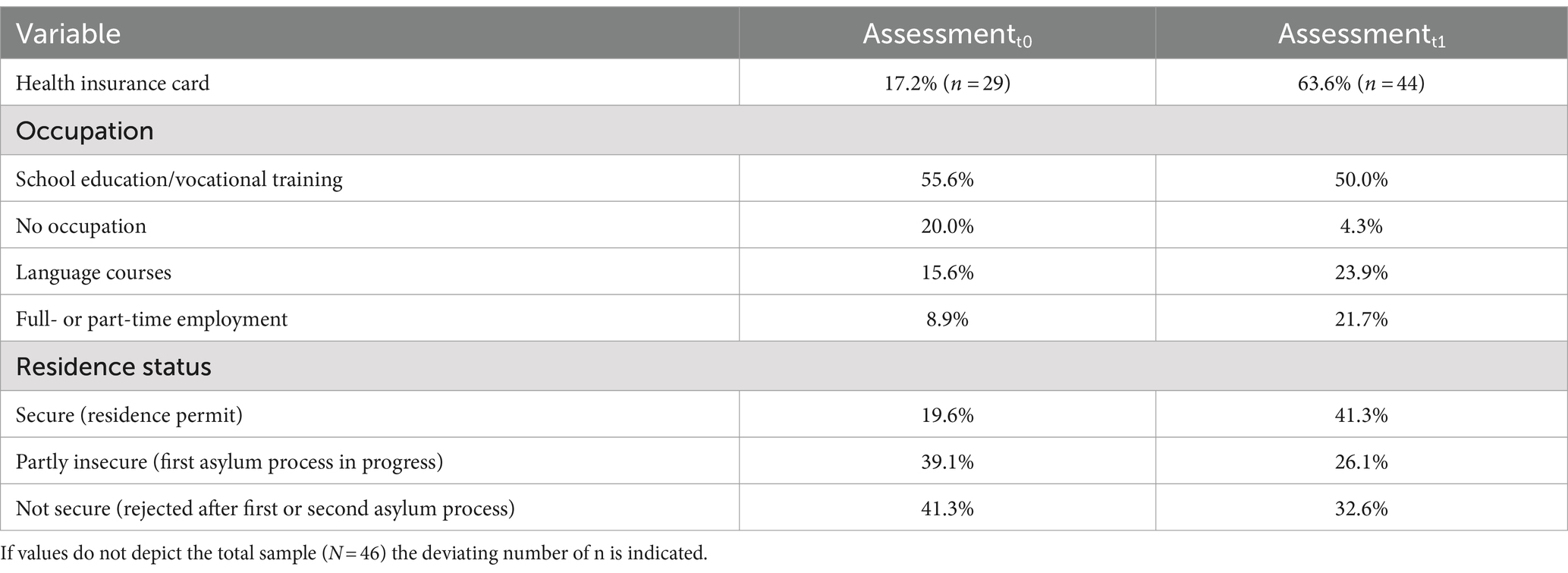
Participants were invited to partake in the initial assessment (assessmentt0) if they met the inclusion criteria of refugee status and presented sufficient understanding of study procedures and questions. The assessmentt0 of 104 refugees took place from March 2020 to June 2022. Follow-up assessments (assessmentt1) were scheduled 9 months after the assessmentt0. We tried to contact all participants of the assessmentt0 and 53 refugees took part in the assessmentt1 from April 2021 to March 2023. The most common reason for dropouts was that participants could not be reached because they had moved, had been deported or their contact details were missing. Other refugees were contacted but refused to participate for reasons of time or motivation. Thus, the final dropout rate was 44.9%. In addition, data of one refugee aged 41 years was excluded due to the research’s focus on refugee adolescents. From the sample of assessmentt1 completers, data of n = 6 participants had to be excluded due to missing data on one of the key variables emotional distress or integration. This resulted in an assessmentt1 total sample of N = 46, which included 42 male (91.3%) and 4 female (8.7%) participants. Age at assessmentt1 ranged from 15 to 23 years, with a mean age of 20.8 (SD = 2.2) years. In case of missing socio-demographic data, missing values are indicated by the deviating n in the results section. Assessmentt1 participants and dropouts were comparable in most aspects of the assessmentt0 (see Supplementary material 1), yet dropouts reported possessing health insurance cards more often.
2.2 Design and procedure
The research was conducted in a model project called “Fearless,” implemented by the Center of Excellence for Psychotraumatology of the University of Konstanz, the Bodensee-Institut für Psychotherapie, and the NGO “vivo international.” The overall aim of the project is facilitating adolescent refugees’ access to mental health services in Germany. Translators and peer counsellors were trained in translation in psychosocial contexts, mediating between cultures and navigating the German health care system. Therapists received 4 days of training in the diagnosis and treatment of post-traumatic disorders using Narrative Exposure Therapy (NET) and Forensic Offender Rehabilitation NET (FORNET), an adaptation of NET for offenders with a low aggression threshold (Hecker et al., 2015). Thereafter, therapists were supervised by psychotherapist supervisors in the German health care system who received project supervision in NET and FORNET if needed. Psychologically distressed refugees were offered psychotherapy – not limited to trauma-focused treatments - within the project or were referred to other services. For more information on the treatment see Potter et al. (2023). For the assessmentt0, government authorities working with refugees in the German state of Baden-Württemberg, mostly near the city of Konstanz, were informed of the upcoming research project. Social workers employed at the refugees’ accommodation informed potential participants about the project. Targeted participants were between 14 and 22 years of age. Appointments for the assessmentt1 were mostly scheduled via the social worker, in some cases the assessmentt1 was scheduled via the therapist or directly with the participants themselves.
Most of the assessments took place in the refugees’ accommodation in a separate office, some took place in the office of the Center of Excellence for Psychotraumatology at the University of Konstanz. During both assessments, questionnaires were administered in a semi-structured interview. In the assessmentt0 trained interpreters were present in 50% and in the assessmentt1 in 35% of all cases. The remaining assessments were conducted in English or German. Prior to both assessments, participants were informed about the study and signed a written informed consent form. For minors, a legal guardian gave additional written consent. In both assessments we explained that the participation was voluntary, that it would not influence the asylum procedure and that all data would be handled confidentially. In the assessmentt0 no monetary compensation was offered while for assessmentt1 participants received 15€ for participating. The assessmentt0 lasted about 45 min and the assessmentt1 about 40 min. After completion of the assessmentt0, the refugees’ symptoms and potential treatment offers were discussed, which included psychotherapy within the project or transfer to other institutions. After assessmentt1 all emotionally distressed participants who had not yet received therapy were offered assistance to get access to treatment. They were informed that they would not have to pay for any treatment and that it was voluntary. The project and current study were approved by the Ethics Committee of the University of Konstanz.
2.3 Assessment
The assessmentt0 included sociodemographic information about age, country of origin, years of education, residence status, health insurance, arrival date in Germany, whether the participants had arrived accompanied by family members and whether they had family living in Germany. Moreover, they were asked if they had been involved in physical fighting since entering the country. In addition to sociodemographic information, length of stay was calculated according to the arrival date in Germany and pandemic months was calculated according to the months passed since March 2020. Severe physical abuse in childhood was assessed with the question: “Have you been hit so badly before the age of 15 that you had to go to hospital or needed medical attention?” Participants responded with a yes/no answer. This question refers to the findings of Webb (Webb et al., 2017), who analyzed hospital admissions in a national cohort study, and showed that having experienced interpersonal violence causing hospitalization prior to the age of 15 years considerably increased the risk of harming one-self and/or being convicted because of a violent crime between the age of 15–35 years.
In the assessmentt1, participants were asked about their present residence status, health insurance, vocational training and German language skills. Moreover, they were asked if they had been involved in physical fighting or had started psychotherapeutic treatment since the assessmentt0. Participants who had started therapy were asked when it had started, how many outpatient sessions had been held, and if they had further remarks regarding therapy. The following questionnaires were administered in both assessments:
The Refugee Health Screener (RHS) was used to assess refugees’ emotional distress (Hollifield et al., 2013). The questionnaire shows good reliability and concurrent and predictive validity for anxiety, depression, and PTSD and has been used in diverse settings with refugees (Hollifield et al., 2013; Kaltenbach et al., 2017; Hollifield et al., 2016). The present study used the RHS-13 with 13 items (Hollifield et al., 2016), which proved to be efficient without compromising specificity or sensitivity while having acceptable psychometric properties (Hollifield et al., 2016). Participants rated the degree to which they were troubled by a symptom in the last month, e.g., “feeling down, sad, or blue most of the time.” The items were rated from 0 (not at all) to 4 (extremely) on a 5-point Likert scale and the cumulative score ranges between 0 and 52. Participants (n = 3) that did not rate > 10% of the RHS-13 items were excluded from the analyses (Hollifield et al., 2016). If participants’ missing items accounted for ≤10% of the RHS-13 (Kaltenbach et al., 2017), the respective items were set to zero. We used a dichotomous cut-off score. Psychotherapy was offered to participants with a total score ≥ 11, indicating high emotional distress (Hollifield et al., 2016). In the present study, Cronbach’s alpha for the instrument resulted in αt0 = 0.91 (n = 44) and αt1 = 0.87 (n = 44).
The Integration Index, developed by the Immigration Policy Lab (IPL), was used as a measure of the refugee’s status in his/her integration process. The IPL questionnaire assesses psychological, economic, political, social, linguistic and navigational dimensions of integration (Harder et al., 2018). The IPL has proven valid across immigrant groups and countries and correlates with length of stay and residence status and differentiates among groups with diverse integration levels (Harder et al., 2018). The present study used the IPL-12 scale, which covers each dimension with two items (Harder et al., 2018). Responses to each item are scored between 1 and 5 points, so that a cumulative score on each sub-dimension ranges between 2 and 10 and the overall integration score ranges between 12 and 60. As recommended by Harder et al. (2018), the cumulative scores were then rescaled to provide a standardized IPL Integration Index between 0 and 1. Participants were assigned to two groups of integration whether their overall score was lower or higher than 0.5. Participants (n = 4) that did not rate > 10% of the items on the IPL-12 were excluded from the analyses. Further, if participants’ missing items accounted for ≤10% of the IPL-12, the respective items were set to one (lowest value). In the present study, Cronbach’s alpha for the instrument resulted in αt0 = 0.82 (n = 44) and αt1 = 0.77 (n = 46).
2.4 Data analysis
Version 28 of the Statistical Package for Social Sciences (SPSS; IBM Deutschland GmbH, Ehningen, Germany) was used for all data preparation and statistical analyses. All sum scores and parameters were generated according to the guidelines of the questionnaires and as specified above. All analyses were tested two-sided and with a level of significance of 0.05. As there was no homogeneity of the error variances of emotional distress, longitudinal differences for emotional distress were evaluated by sign tests and t-tests. Although RHS difference scores of the total sample (N = 46) and cumulative (sub-dimension) integration scores were not normally distributed, t-tests were used, as they are robust with sample sizes >30 (Salkind, 2010), and after non-parametric tests provided the same results. The reported p-values for the changes in integration sub-dimensions were Bonferroni corrected. Integration status change over time was examined with a Mixed ANOVA, as homogeneity of the error variances of integration was given. As the Mixed ANOVA was shown to be robust to moderate departures from normality (Salkind, 2010), the Mixed ANOVA for integration was conducted even though one of the four factor groups (integrationt0: high vs. low and time: assessmentt0 vs. assessmentt1) was not normally distributed. The Reliable Change Index (RCI) was calculated to investigate the amount of change of emotional distress and integration in each refugee (Blampied, 2022). Kendall’s tau correlations and multiple hierarchical regression analyses served to delineate the contribution of various post-migration stressors on emotional distress and integration. The categorial variable ‘residence status’ was dummy coded to be included in the regressions and the reference category was secure. The first multiple hierarchical regression analysis targeted emotional distresst1 and included in the first block emotional distresst0 as the control variable and in the second block integrationt0, severe physical abuse in childhood, psychotherapy, and residence statust1. The second multiple hierarchical regression analysis predicted integrationt1 with integrationt0 and length of stay in Germany first entered as control variables. Emotional distresst0 and residence statutst1 were entered in a second block. The model fit of the regressions was examined by assessing in which model the Akaike Information Criterion (AIC) was lowest (Akaike, 1987).
3 Results
3.1 Participants’ current living situation
The time interval between the assessmentt0 und the assessmentt1 varied around M = 9.3 (SD = 0.7) months. Length of stayt1 was M = 38.0 (SD = 22.3, RoV = 10–82) months and M = 19.6 (SD = 6.0, RoV = 14–36) pandemic monthst1 (months since the beginning of the COVID-19 pandemic in March of 2020) had passed. Of the total sample (N = 46; mean aget1 = 20.8; SD = 2.2 years), n = 10 had entered Germany as accompanied minors and n = 14 had entered Germany as unaccompanied minors. At the assessmentt0 61.0% of participants did not have parents or siblings living in Germany. Years of educationt0 ranged from 0 to 15 years and participants had visited on average 8.5 (SD = 3.4) years of education. Most of the participants were from Afghanistan (32.6%), Syria (17.4%), and Gambia (15.2%). Since their arrival in Germany six participants of 46 in total, and since the assessmentt0 three of 46 in total reported having been involved in physical fights. Seventeen reported having experienced severe physical abuse in childhood.
Nine participants had started therapy in the Fearless project after the assessmentt0. At the assessmentt1, six of these were still in therapy, two had ended therapy prematurely after more than six sessions, and one had ended therapy before the sixth session. To control for possible effects of psychotherapy in the following examinations, we categorized these participants in two groups. Research in Germany proposes to classify psychotherapy as “started” when patients have completed at least six sessions (Hiller et al., 2011; Cinkaya et al., 2011). This classification is based on the German health care system where patients first complete up to six probationary sessions before starting a psychotherapy. In these probationary sessions therapists further clarify diagnoses and plan the therapy (Hiller et al., 2011). In accordance, we classified those having completed more than six sessions (n = 8) as “having started psychotherapy.” Those that had completed at least six sessions had completed M = 33.4 (SD = 13.0, RoV = 17–54, n = 7) therapy sessions at assessmentt1. Table 1 provides an overview of further details regarding the sociodemographic information of the sample.
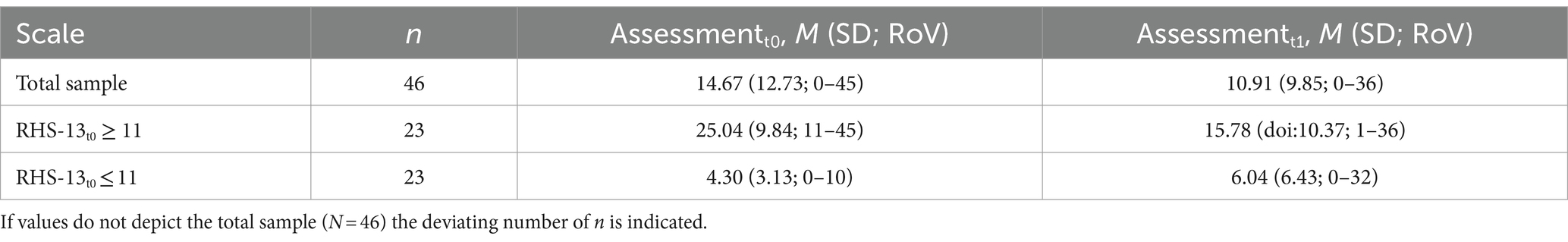
3.2 Longitudinal course of emotional distress
Overall, emotional distress decreased over time. Paired t-tests of RHS-scores of the total sample [t(45) = −2.45, p = 0.018, d = 0.36] and of the n = 23 participants with RHSt0 ≥ 11 [t(22) = −4.04, p < 0.001, d = 0.84] revealed significantly lower RHS-scores at the assessmentt1 than at the assessmentt0. This decrease was primarily seen in participants with high distress at assessmentt0, as the sign test did not confirm significantly different RHS-scores at assessmentt1 for participants with RHSt0 ≤ 11: p = 0.115, n = 23. The RCI (rounded to +10 or − 10), indicated a significant decrease with a RHS score difference of t1-t0 ≤ −10 and a significant increase with a difference of t1-t0 ≥ 10. Of the 12 participants (25.5%) showing a reliable change from assessmentt0 to assessmentt1, the RHS score increased in one and decreased in 11. Table 2 lists mean RHS-scores at assessmentt0 and at the assessmentt1 for the total sample (N = 46) and subgroups with high vs. low emotional distress at assessmentt0.
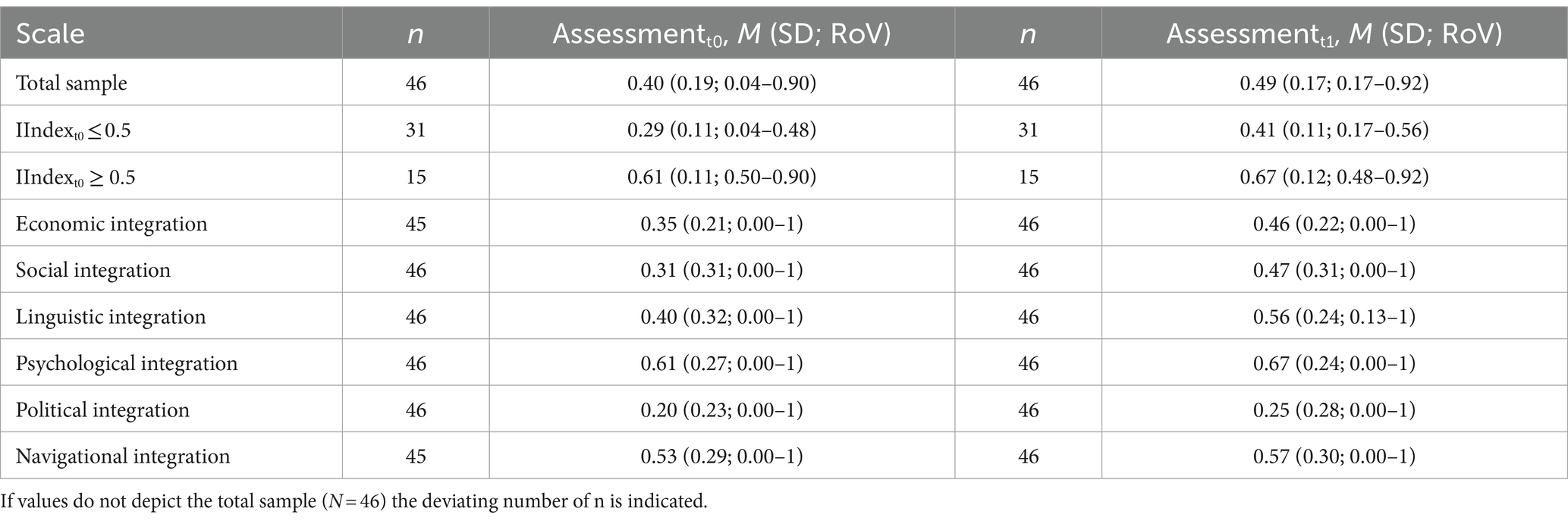
3.3 Longitudinal course of integration
Overall, the Integration Index increased over time in both groups: While the Mixed ANOVA did not confirm significant interaction of time (assessmentt0 vs. assessmentt1) and group (high vs. low integrationt0), assumed sphericity F(1,44) = 2.669, p = 0.109, partial η2 = 0.057, simple main effects were significant for time [assumed sphericity F(1,44) = 31.72, p < 0.001, partial η2 = 0.419] and group [F(1,44) = 86.16, p < 0.001, partial η2 = 0.662]. The RCI (rounded 0.30 or −0.30) indicated a significant increase in the Integration Index with a difference of t1-t0 ≤ 0.30 in two refugees (4.3%).
Changes per sub-dimension were probed by t-tests and reported p values for the sub-dimensions are Bonferroni corrected. Scores for economic [t(45) = 2.93 p = 0.030, d = 0.44], social [t(45) = 4.13, p = 0.006, d = 0.60] and linguistic integration [t(45) = 4.62, p = 0.006, d = 0.68] were significantly higher at the assessmentt1. Scores for the sub-dimensions psychological [t(45) = 1.73, p = 0.55, d = 0.26], political [t(45) = 1.48, p = 0.88, d = 0.22] and navigational integration [t(44) = 1.14, p > 0.999, d = 0.17] were not significantly different at the assessmentt1. Table 3 shows an overview of the mean Integration Index at assessmentt0 and at assessmentt1, divided by low vs. high integration at assessmentt0and of the mean Integration Indexes of the sub-dimensions at assessmentt0 and assessmentt1.
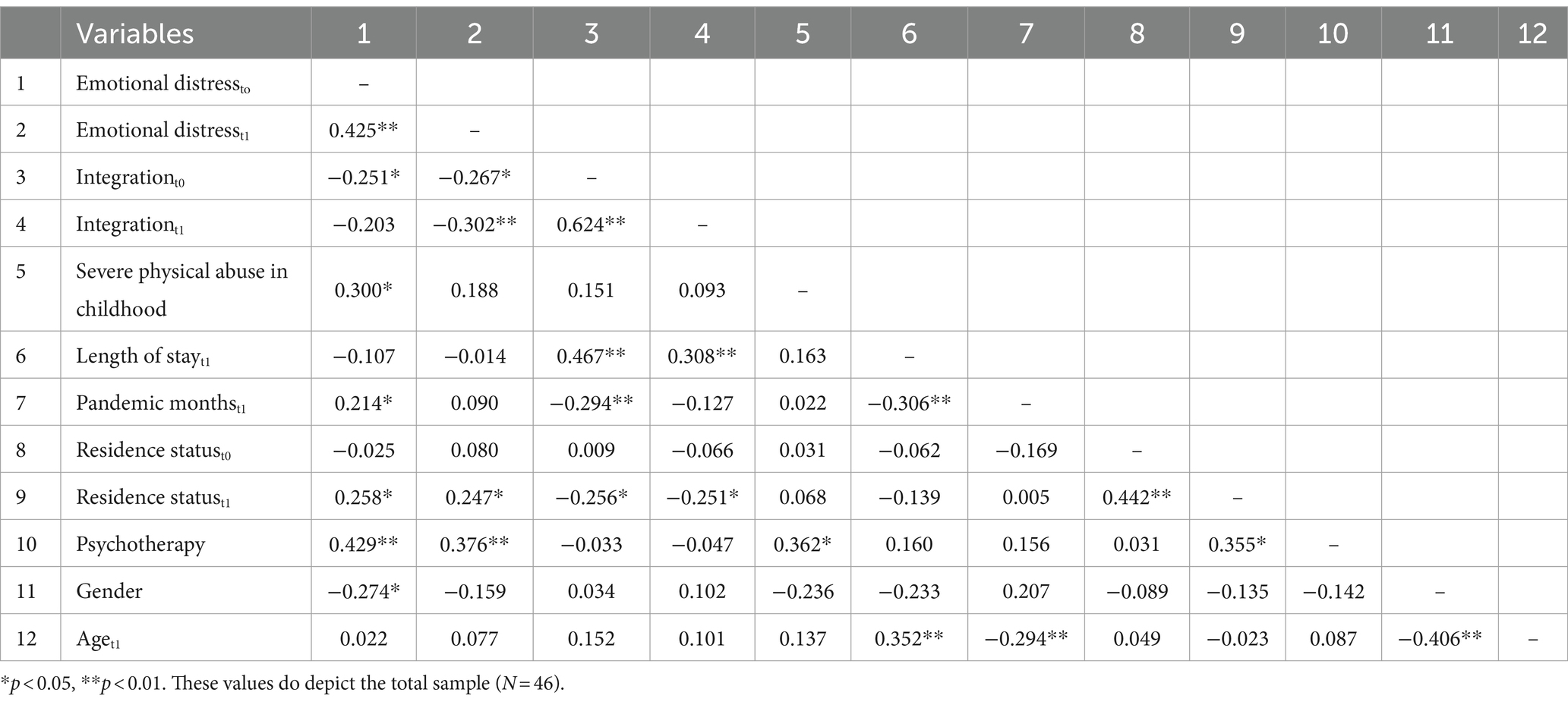
3.4 Associations of longitudinal outcome of psychological distress and integration
Correlational analyses substantiated the preceding results (see Table 4): Emotional distresst1 correlated positively with emotional distresst0 (r = 0.43, p < 0.001) and negatively with integrationt0 (r = −0.27, p = 0.011) and integrationt1 (r = −0.30, p = 0.004). In addition, correlation coefficients signaled an association of emotional distresst1 with living conditions such as residence statust1 (r = 0.25, p = 0.037) and psychotherapy (r = 0.38, p = 0.003). Integrationt1 correlated positively with integrationt0 (r = 0.62, p < 0.001), length of stay (r = 0.31, p = 0.003) and negatively with residence statust1 (r = −0.25, p = 0.034).
3.5 Regression analyses
Over and above the course of emotional distress and integration over time, the present analyses aimed at evaluating longitudinal predictors of emotional distress and integration. A hierarchical regression analysis confirmed that emotional distresst1 was best predicted by psychotherapy (ß = 0.35, p = 0.020), emotional distresst0 (ß = 0.34, p = 0.031) and integrationt0 (ß = −0.29, p = 0.043), neither residence status t1 nor severe physical violence during childhood reached significance. As illustrated in Table 5, the latter model [F(6,39) = 7.255, p < 0.001] showed the lowest AIC, explained most variance (adjusted R2 = 0.46) and the change in F(2.770) was significant p = 0.031. Integrationt1 was best predicted by integrationt0 (ß = 0.89, p < 0.001). As illustrated in Table 6, the first model [F(2,43) = 52.849, p < 0.001] explained most variance (adjusted R2 = 0.70) and the change in F (0.865) was not significant p = 0.467. However, the second model showed the lowest AIC and apart from integrationt0, no other predictor was significant.
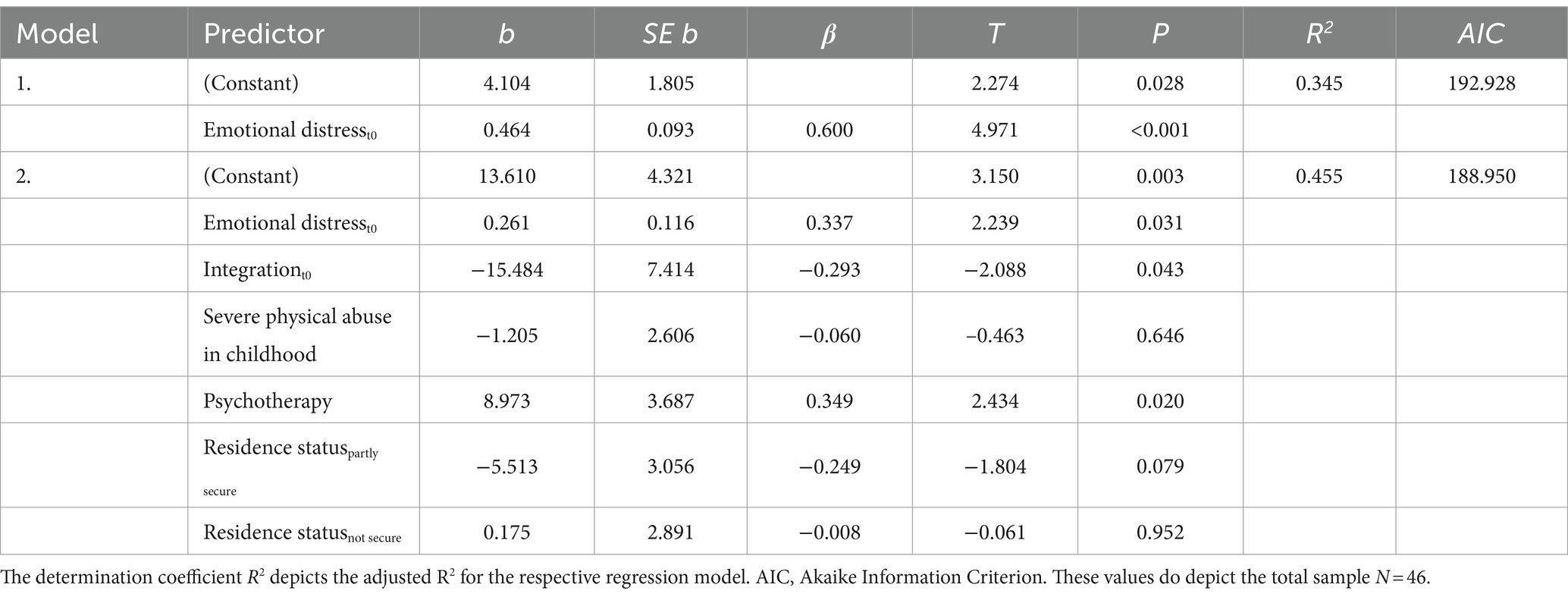
Table 5. Regression models of emotional distresst1 on emotional distresst0, integrationt0, severe physical abuse in childhood, psychotherapy and residence statust1.
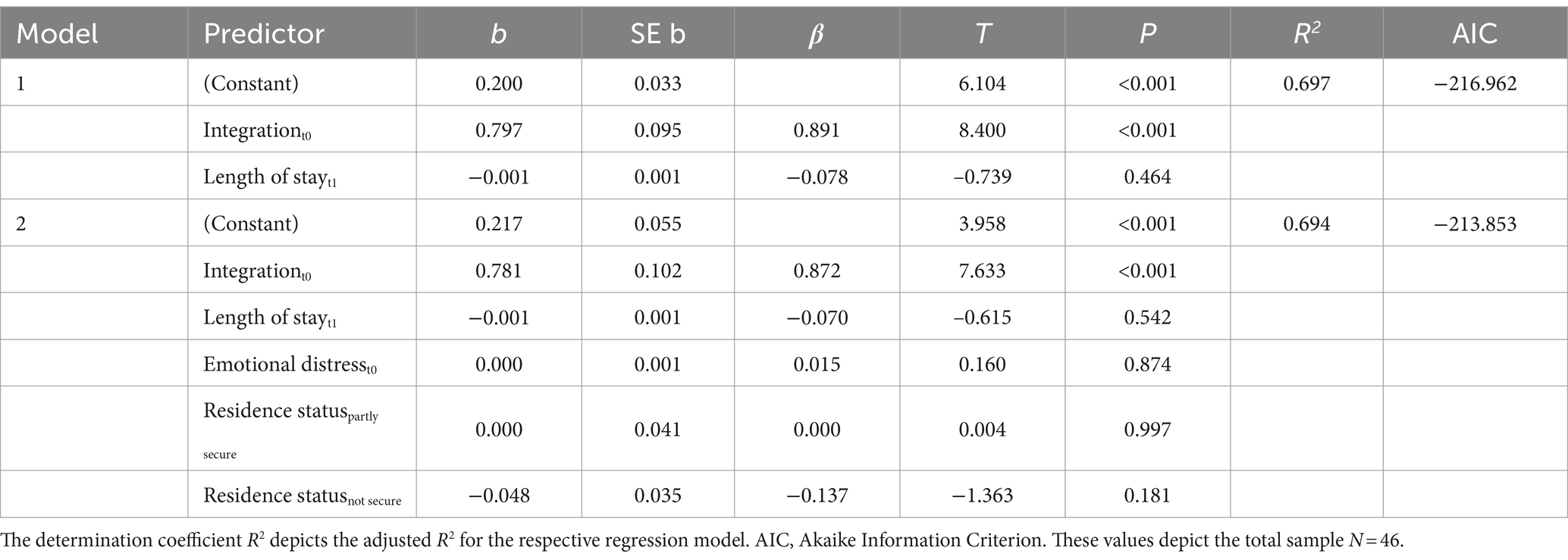
Table 6. Regression models of integrationt1 on integrationt0, emotional distresst0, length of stayt1 and residence statust1.
4 Discussion
Emotional distress and integration were assessed in a sample of refugees over 9 months to identify determinants of the longitudinal course of emotional distress and integration. Emotional distress of initially emotionally distressed refugees decreased over time but remained mostly clinically elevated, while emotional distress of refugees with low emotional distress at assessmentt0 did not significantly change. The most relevant longitudinal predictors of emotional distress were their emotional distress and integration at assessmentt0, as well as whether they started psychotherapy. Integration improved over time, yet contrary to our expectation, successful integration over time only depended on integration at assessmentt0. Further, only the sub-dimensions of social, economic, and linguistic integration changed significantly from assessmentt0 to assessmentt1.
The amelioration of emotional distress over time in initially highly distressed refugees is in line with other research in Germany examining refugees over a course of 3 (Nikendei et al., 2019), and 4–10 months (Richter et al., 2018). However, similar to results of previous research, whilst the emotional distress of severely affected refugees improved, it still remained in a clinical range (Nikendei et al., 2019). Examining the course of emotional distress of the sample separated into high vs. low emotional distress at assessmentt0 underlines the importance of examining mean changes of total samples in more detail. Separated according to their distress level at assessmentt0, the emotional distress of refugees ameliorated only in those who were initially highly distressed. The most important predictor for refugees’ follow-up emotional distress was their emotional distress at the assessmentt0. This result is in accordance with research examining refugees in Vietnam over a course of more than 20 years, which found that especially trauma-related mental disorders at arrival, and symptom improvement during the first 3 years of resettlement, were important for positive long-term mental health prognosis after 23 years (Vaage et al., 2010).
Highlighting integration as the best acculturation strategy for emotional well-being (Behrens et al., 2015; Han et al., 2016), refugees’ integration at assessmentt0 was a significant predictor for their emotional distress at follow-up: refugees with higher integration at assessmentt0 showed less emotional distress at assessmentt1. These results demonstrate the intertwinement of refugees’ mental health and their integration. Brea Larios et al. (2023) examined Afghan refugees in Norway with a modified version (without the political integration sub-dimension) of the Integration Index. They showed that only psychological integration (sense of belonging) had a significant effect on their emotional distress. Due to our limited sample size, we could not further explore the potentially varying impact of different integration sub-dimensions on refugees’ mental health.
The only significant predictor for refugees’ integration at the assessmentt1, over and above their emotional distresst0, or length of their stay, was their integration at assessmentt0. Our results emphasize that length of stay may rather act as a marker for other explanatory variables, such as language comprehension. No participant showed a reliable decrease of integration, whilst integration in total and on all sub-dimensions improved. This result gives hope that the right support could enhance integration as well as aid the progress of integration quicker. An increase of integration could be supported with integration courses, as already established in Germany. These courses include a German language course as well as information on the legal system, history and culture of Germany (Bundesregierung, 2019). Participation in these courses is offered to/required of refugees with a good chance of staying in Germany (Bundesregierung, 2019), which applied only to a small proportion of our sample. Apart from selective and often delayed access to these courses, only about 50% of the participating refugees successfully pass the exams at the end of the integration courses (Klinger et al., 2019). The high dropout rates from language and integration courses highlight the interplay of refugees’ emotional distress and their integration (German National Academy of Sciences Leopoldina, 2018; Walther et al., 2021). A direct and early support of emotionally distressed refugees even before starting an integration course is needed to enable their participation in integration activities (German National Academy of Sciences Leopoldina, 2018; Walther et al., 2021). Moreover, the courses have been criticized for showing high regional differences regarding the quality of and access to them (Etzel, 2022). Hence, there is a high demand for reforming them, especially since all refugees should have equal access (Klinger et al., 2019; Etzel, 2022).
To our knowledge, our study is the first to examine the longitudinal course of all sub-dimensions of the Integration Index. The sub-dimensions of social, economic, and linguistic integration changed significantly from assessmentt0 to assessmentt1. Psychological and navigational integration may not have significantly changed because both sub-dimensions were already more elevated at the assessmentt0 than the social, economic, and linguistic integration sub-dimensions at the assessmentt1. The only sub-dimension with low scores at assessmentt0 and assessmentt1 was political integration. Political integration may only be achieved later in the integration process, which would not be surprising regarding refugees’ restricted possibilities to participate in German politics, e.g., not being allowed to vote (Bundesministerium des Inneren und für Heimat, 2023). In Germany, refugees can mostly engage in political life through non-formal political participation and interviews with refugees highlighted that on top of structural barriers especially an insecure legal status and negative stereotyping composed barriers to refugees’ political participation (Ragab, 2018). Lastly, we want to emphasize that Governmental policies shape and are shaped by public opinions and attitudes, which influence refugees’ opportunities for inclusion and participation (Hynie, 2018). Hence, successful integration of refugees is a two-way street requiring a social context enhancing inclusion and participation (Etzel, 2022).
While severe physical abuse in childhood was a cross-sectional predictor for refugees’ emotional distress (Potter et al., 2022), it was not a longitudinal predictor. Similarly, Van Wyk et al. (2012) examined refugees’ PTSD, anxiety, depression and somatization symptoms over the course of 7 months and showed that traumatic events were associated with all mental health symptoms at baseline. However, at follow-up the number of traumatic events did not predict mental health outcomes anymore. Hence, symptoms themselves (Van Wyk et al., 2012) and post-migration stressors (Stuart and Nowosad, 2020) seem to be more relevant for the maintenance of pathology. Aligning with this result, Behrendt et al. (2022) showed that material and social stressors and not stressful life events further exacerbated anxiety and depression symptoms in the long term. Further, physical abuse in childhood, amongst other traumatic experiences, is most likely represented by a basic trauma burden, significantly contributing to emotional distress. If this basic trauma burden is taken into consideration, e.g., by controlling for baseline symptoms as in our study, their incremental predictive power may be reduced.
Psychotherapy was included as a control variable in our regression. Refugees with higher levels of emotional distress were more likely to be in psychotherapy in-between both assessments, as psychotherapy was only offered to refugees with high emotional distress at assessmentt0. In our study, 41.7% of all emotionally distressed participants accepted a treatment offer after assessmentt0. Other studies reported that 0% (Nikendei et al., 2019) to 75% (Hollifield et al., 2013) of emotionally distressed refugees accepted treatment offers. Most likely, higher emotional distress at the assessmentt1 resulted from the initially more emotionally distressed refugees participating in psychotherapy. Carlsson et al. (2005) examined refugees after 9 months while they were still in treatment and found no significant changes of mental health symptoms. They concluded that the time frame of 9 months to measure an amelioration caused by treatment was most likely too short, especially because therapies had not yet regularly ended. In accordance with this conclusion, systematic research examining long-term effects of NET found that effects were strongest long-term, e.g., at least 6 months after treatment (Siehl et al., 2020). Of all psychotherapies classified as started, 22.2% ended prematurely, which aligns with a weighted average dropout rate of 19.1% in a meta-analysis on refugees (Semmlinger et al., 2021).
One often researched post-migration stressor is refugees’ residence status. While in this research some refugees gained asylum acceptance over the course of 9 months (19.6–41.3%), refugees’ residence status was not a significant predictor for their emotional distress or integration. Schick (Schick et al., 2016) also found that residence status was not predictive of refugees’ emotional distress or integration difficulties over a course of 10 years. Refugees’ residence status may rather act as a marker for other post-migration stressors, such as a different access to health care services, language problems or living arrangements (Bauhoff and Göpffarth, 2018; Toar et al., 2009; Gleeson et al., 2020). Furthermore, whilst residence status might be associated with fears of deportation in the first years after arriving in Germany, over time other factors might become more important for long-term psychological well-being. On average, this sample included refugees who arrived in Germany 2 years prior to our assessmentt0. At assessmentt1, 9 months later, the risk of sudden deportation was even lower. Some of those, whose stay in Germany was refused, were already deported. Hence, in our study residence status might have lost its’ predictive value.
Systematic reviews examining the effects of the COVID-19 pandemic during 2020 on refugees showed a negative effect on refugees’ (Sevim et al., 2023) and refugee youths’ mental health (Nearchou et al., 2020). However, a first meta-analysis of longitudinal research on the psychological impact of COVID-19 first lockdowns concluded the impact to be rather small in magnitude and very heterogeneous (Prati and Mancini, 2021). Moreover, research examining a longer time-frame in Danish residents concluded that the COVID-19 pandemic may only have had small long-term effects on mental health (Thygesen et al., 2023). In our research, the predictor pandemic months had an impact at the assessmentt0 (Potter et al., 2022), but was not significant in the longitudinal analysis. Possibly, the negative impact of COVID-19 and associated isolation is waning over time, now that social interactions have returned to a pre-COVID level.
Some limitations need to be taken into consideration when interpreting the results of our study. A general limitation is that we relied on self-report questionnaires, which provide subjective and not verifiable answers. Further, our sample showed great heterogeneity regarding the participants originating from 13 different countries, their different living situations in Germany, differing lengths of stay, residence statuses as well as current activities. This diversity may limit general conclusions and the representativity of the sample, even though refugee samples are well-known for their heterogeneity (Stenmark et al., 2013; Hecker et al., 2018). Moreover, we had no control group without an offer of psychotherapy. The RHS was translated into many different languages while taking into consideration cultural aspects (Hollifield et al., 2016), nevertheless language- and culture-validated questionnaires were not available for everyone. While statistics on asylum seekers in Germany generally report a high amount of male refugees in the age group 16 to 25 years, as much as 73.1–75.9% (Bundesamt für Migration und Flüchtlinge, 2022), the even higher percentage of male participants in our sample might further limit the generalizability of the results. Due to our limited sample size and cross-sectional results, we did not control for gender or age in the regression analyses because there were no significant cross-sectional predictors (Potter et al., 2022). Moreover, Harder et al. (2018) did not find significant differences in Integration Index scores based on age or gender. Since there is a two-way causality between integration and emotional distress (especially at assessmentt0), our longitudinal design is limited in regard to causal conclusions on the relationship between emotional distress and integration. Another specificity of refugee samples is a high dropout rate at the assessmentt1. Our drop-out rate of 44.9% is another limitation even though the rate was in line with drop-out rates ranging from 40.7–71.1% in refugee samples (Borho et al., 2020; Nikendei et al., 2019; Ryan et al., 2008; Kindermann et al., 2020).
Refugees’ emotional distress and their integration are intertwined and hence need to be addressed promptly after refugees’ entry in the host society. As a first step we recommend implementing a mental health screening for all refugees on arrival. Schmidt et al. (2023) have just recently demonstrated the feasibility of such a mental health screening directly at a reception center by combining it with the mandatory physical examination. Further adjustments in the German health care system would include reinforcing education on the treatment of refugee clients in the curricula of psychotherapy training. In addition, therapists providing therapy to refugee clients should be supported by nationwide structural support systems, including financing professional translators, peer counsellors, a referral system for refugee clients, and ensuring adequate supervision. Moreover, access to integration courses needs to be improved, so that all refugees profit from an early access.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the University of Konstanz. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
FP: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. KD: Conceptualization, Data curation, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – review & editing. BR: Conceptualization, Supervision, Writing – review & editing. AC: Conceptualization, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The research costs were covered by the Baden-Württemberg foundation.
Acknowledgments
We would like to thank all refugees who participated in our study and all cooperation partners that made their participation possible. We would like to thank Maggie Schauer and Thomas Elbert for their support with the funding applications. Moreover, we want to thank Claudia Dang-Thai, Hendrikje Rost, Johanna Sill, Marlene Zehb and Veronika Müller-Bamouh for supporting with the data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1459934/full#supplementary-material
Footnotes
1. ^In 2024, this regulation was increased to the first 36-months.
2. ^Being aware that refugees and asylum seekers refer to populations with different characteristics, to simplify the terminology we refer to both as refugees.
References
Akaike, H. (1987). Factor analysis and AIC. Selected papers of hirotugu Akaike. New York, NY: Springer, 371–386.
Alpay, E. H., Kira, I. A., Shuwiekh, H. A., Ashby, J. S., Turkeli, A., and Alhuwailah, A. (2021). The effects of COVID-19 continuous traumatic stress on mental health: the case of Syrian refugees in Turkey. Traumatol 27, 375–387. doi: 10.1037/trm0000347
Aragona, M., Barbato, A., Cavani, A., Costanzo, G., and Mirisola, C. (2020). Negative impacts of COVID-19 lockdown on mental health service access and follow-up adherence for immigrants and individuals in socio-economic difficulties. Public Health 186, 52–56. doi: 10.1016/j.puhe.2020.06.055
Baron, J., and Flory, L. V. (2020). Zur psychosozialen Versorgung von Flüchtlingen und Folteropfern in Deutschland [on the psychosocial care of refugees and torture victims in Germany]. Berlin, Germany: Bundesweite Arbeitsgemeinschaft der Psychosozialen Zentren für Flüchtlinge und Folteropfer – BAfF e. V.
Bauhoff, S., and Göpffarth, D. (2018). Asylum-seekers in Germany differ from regularly insured in their morbidity, utilizations and costs of care. PLoS One 13:e0197881. doi: 10.1371/journal.pone.0197881
Behrendt, M., Pfeiffer, E., Devlieger, I., Adeyinka, S., Rota, M., Uzureau, O., et al. (2022). The impact of daily stressors on unaccompanied young refugees’ mental health: a longitudinal study. Am. J. Orthopsychiatry 92, 681–691. doi: 10.1037/ort0000644
Behrens, K., del Pozo, M. A., Großhennig, A., Sieberer, M., and Graef-Calliess, I. T. (2015). How much orientation towards the host culture is healthy? Acculturation style as risk enhancement for depressive symptoms in immigrants. Int. J. Soc. Psychiatry 61, 498–505. doi: 10.1177/0020764014560356
Beiser, M. (2006). Longitudinal research to promote effective refugee resettlement. Transcult. Psychiatry 43, 56–71. doi: 10.1177/1363461506061757
Blampied, N. M. (2022). Reliable change and the reliable change index: still useful after all these years? Cogn Behav Therap. 15:e50. doi: 10.1017/S1754470X22000484
Bogic, M., Njoku, A., and Priebe, S. (2015). Long-term mental health of war-refugees: a systematic literature review. BMC Int. Health Hum. Rights 15:29. doi: 10.1186/s12914-015-0064-9
Borho, A., Viazminsky, A., Morawa, E., Schmitt, G. M., Georgiadou, E., and Erim, Y. (2020). The prevalence and risk factors for mental distress among Syrian refugees in Germany: a register-based follow-up study. BMC Psychiatry 20, 362–313. doi: 10.1186/s12888-020-02746-2
Brea Larios, D., Sam, D. L., and Sandal, G. M. (2023). Psychological distress among afghan refugees in Norway as a function of their integration. Front. Psychol. 14:1143681. doi: 10.3389/fpsyg.2023.1143681
Bundesamt für Migration und Flüchtlinge . Aktuelle Zahlen 03/2022 [Current numbers 03/2022] (2022). Available at: https://www.bamf.de/SharedDocs/Anlagen/DE/Statistik/AsylinZahlen/aktuelle-zahlen-maerz-2022.pdf?__blob=publicationFile&v=4. (Accessed January 23, 2023)
Bundesministerium des Inneren und für Heimat . Ausländerwahlrecht [Voting rights for foreigners] (2023). Available at: https://www.bmi.bund.de/DE/themen/verfassung/wahlrecht/auslaenderwahlrecht/auslaenderwahlrecht-node.html. (Accessed January 30, 2023).
Bundesregierung, (2019). Darstellung der Maßnahmen der Bundesregierung zur Sprachförderung und integration [presentation of the federal government's measures for language promotion and integration]. Frankfurt: Bundesministerium des Innern, für Bau und Heimat.
Carlsson, J. M., Mortensen, E. L., and Kastrup, M. (2005). A follow-up study of mental health and health-related quality of life in tortured refugees in multidisciplinary treatment. J. Nerv. Ment. Dis. 193, 651–657. doi: 10.1097/01.nmd.0000180739.79884.10
Chen, W., Wu, S., Ling, L., and Renzaho, A. M. (2019). Impacts of social integration and loneliness on mental health of humanitarian migrants in Australia: evidence from a longitudinal study. Aust. N. Z. J. Public Health 43, 46–55. doi: 10.1111/1753-6405.12856
Cinkaya, F., Schindler, A., and Hiller, W. (2011). Wenn Therapien vorzeitig scheitern: Merkmale und Risikofaktoren von Abbrüchen in der ambulanten Psychotherapie [when therapies fail prematurely: characteristics and risk factors of discontinuations in outpatient psychotherapy]. Z. Klin. Psychol. Psychother. 40, 224–234. doi: 10.1026/1616-3443/a000121
Commission E (2018). Communication from the commission to the European parliament, the European council, the council, the european economic and social committee and the committee of the regions: Action plan on integration and inclusion 2021–2027. Brussels, Belgium: European Commission.
Dumke, L., Schmidt, T., Wittmann, J., Neldner, S., Weitkämper, A., Catani, C., et al. (2024). Low access and inadequate treatment in mental health care for asylum seekers and refugees in Germany—a prospective follow-up study over 12 months and a nationwide cross-sectional study. Appl. Psychol. Health Well Being 16, 1141–1158. doi: 10.1111/aphw.12523
Etzel, M. (2022). New models of the “good refugee”–bureaucratic expectations of Syrian refugees in Germany. Ethn. Racial Stud. 45, 1115–1134. doi: 10.1080/01419870.2021.1954679
German National Academy of Sciences Leopoldina (2018). Traumatised refugees – immediate response required. Halle. Deutsche Akademie der Naturforscher Leopoldina e. V.
Gibson, B., Schneider, J., Talamonti, D., and Forshaw, M. (2021). The impact of inequality on mental health outcomes during the COVID-19 pandemic: a systematic review. Can. Psychol. 62, 101–126. doi: 10.1037/cap0000272
Gleeson, C., Frost, R., Sherwood, L., Shevlin, M., Hyland, P., Halpin, R., et al. (2020). Post-migration factors and mental health outcomes in asylum-seeking and refugee populations: a systematic review. Eur. J. Psychotraumatol. 11:1793567. doi: 10.1080/20008198.2020.1793567
Han, L., Berry, J. W., and Zheng, Y. (2016). The relationship of acculturation strategies to resilience: the moderating impact of social support among Qiang ethnicity following the 2008 Chinese earthquake. PLoS One 11:e0164484. doi: 10.1371/journal.pone.0164484
Harder, N., Figueroa, L., Gillum, R. M., Hangartner, D., Laitin, D. D., and Hainmueller, J. (2018). Multidimensional measure of immigrant integration. Proc. Natl. Acad. Sci. 115, 11483–11488. doi: 10.1073/pnas.1808793115
Hecker, T., Hermenau, K., Crombach, A., and Elbert, T. (2015). Treating traumatized offenders and veterans by means of narrative exposure therapy. Front. Psych. 6:80. doi: 10.3389/fpsyt.2015.00080
Hecker, T., Huber, S., Maier, T., and Maercker, A. (2018). Differential associations among PTSD and complex PTSD symptoms and traumatic experiences and postmigration difficulties in a culturally diverse refugee sample. J. Trauma. Stress. 31, 795–804. doi: 10.1002/jts.22342
Hiller, W., Schindler, A., Andor, T., and Rist, F. (2011). Vorschläge zur evaluation regulärer Psychotherapien an Hochschulambulanzen im Sinne der phase-IV-Therapieforschung [proposals for the evaluation of regular psychotherapies at university outpatient clinics in terms of phase IV therapy research]. Z. Klin. Psychol. Psychother. 40, 22–32. doi: 10.1026/1616-3443/a000063
Hoell, A., Kourmpeli, E., Salize, H. J., Heinz, A., Padberg, F., Habel, U., et al. (2021). Prevalence of depressive symptoms and symptoms of post-traumatic stress disorder among newly arrived refugees and asylum seekers in Germany: systematic review and meta-analysis. BJPsych open. 7:12. doi: 10.1192/bjo.2021.54
Höhne, E., van der Meer, A. S., Kamp-Becker, I., and Christiansen, H. (2020). A systematic review of risk and protective factors of mental health in unaccompanied minor refugees. Eur. Child Adolesc. Psychiatry 31, 1–15. doi: 10.1007/s00787-020-01678-2
Hollifield, M., Toolson, E. C., Verbillis-Kolp, S., Farmer, B., Yamazaki, J., Woldehaimanot, T., et al. (2016). Effective screening for emotional distress in refugees: the refugee health screener. J. Nerv. Ment. Dis. 204, 247–253. doi: 10.1097/NMD.0000000000000469
Hollifield, M., Verbillis-Kolp, S., Farmer, B., Toolson, E. C., Woldehaimanot, T., Yamazaki, J., et al. (2013). The refugee health Screener-15 (RHS-15): development and validation of an instrument for anxiety, depression, and PTSD in refugees. Gen. Hosp. Psychiatry 35, 202–209. doi: 10.1016/j.genhosppsych.2012.12.002
Hornfeck, F., Sowade, C., and Bovenschen, I. (2022). Effects of the asylum process on the mental health of unaccompanied young refugees–a scoping review. Child Youth Serv. Rev. 137:106490. doi: 10.1016/j.childyouth.2022.106490
Hynie, M. (2018). Refugee integration: research and policy. Peace Conflict 24, 265–276. doi: 10.1037/pac0000326
Jakobsen, M., DeMott, M. A. M., Wentzel-Larsen, T., and Heir, T. (2017). The impact of the asylum process on mental health: a longitudinal study of unaccompanied refugee minors in Norway. BMJ Open 7:e015157. doi: 10.1136/bmjopen-2016-015157
Kaltenbach, E. (2019). Mental health of refugees: Addressing and overcoming challenges in the identification and treatment of mental health problems [doctoral thesis]. Konstanz, Germany: Konstanzer Online-Publikations-System (KOPS), Universität Konstanz.
Kaltenbach, E., Härdtner, E., Hermenau, K., Schauer, M., and Elbert, T. (2017). Efficient identification of mental health problems in refugees in Germany: the refugee health screener. Eur. J. Psychotraumatol. 8:1389205. doi: 10.1080/20008198.2017.1389205
Kartal, D., Alkemade, N., Eisenbruch, M., and Kissane, D. (2018). Traumatic exposure, acculturative stress and cultural orientation: the influence on PTSD, depressive and anxiety symptoms among refugees. Soc. Psychiatry Psychiatr. Epidemiol. 53, 931–941. doi: 10.1007/s00127-018-1532-z
Kien, C., Sommer, I., Faustmann, A., Gibson, L., Schneider, M., Krczal, E., et al. (2019). Prevalence of mental disorders in young refugees and asylum seekers in European countries: a systematic review. Eur. Child Adolesc. Psychiatry 28, 1295–1310. doi: 10.1007/s00787-018-1215-z
Kindermann, D., Zeyher, V., Nagy, E., Friederich, H.-C., Bozorgmehr, K., and Nikendei, C. (2020). Predictors of asylum seekers’ health care utilization in the early phase of resettlement. Front. Psych. 11:475. doi: 10.3389/fpsyt.2020.00475
Kizilhan, J. I., and Noll-Hussong, M. (2020). Psychological impact of COVID-19 in a refugee camp in Iraq. PCN. 74, 659–660. doi: 10.1111/pcn.13142
Klinger, A., Mikschl, J., and Simoleit, B. (2019). In integration investieren [investing in integration]. Für eine Reform der Deutschsprachförderung des Bundes. Available at: https://library.fes.de/pdf-files/wiso/15668.pdf#:~:text=Integration%20von%20Einwanderern%20und%20Einwanderin%E2%80%91%20nen%20ist%20ein20qualitativ%20hochwertiges (Accessed January 23, 2023).
Lichtenstein, G., and Puma, J. E. (2019). The refugee integration survey and evaluation (RISE): results from a four-year longitudinal study. J. Refug. Stud. 32, 397–416. doi: 10.1093/jrs/fey034
Lindert, J., von Ehrenstein, O. S., Grashow, R., Gal, G., Braehler, E., and Weisskopf, M. G. (2014). Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int. J. Public Health 59, 359–372. doi: 10.1007/s00038-013-0519-5
Margolin, G., and Vickerman, K. A. (2011). Posttraumatic stress in children and adolescents exposed to family violence: I. Overview and issues. Prof Psychol Res Pr. 1, 63–73. doi: 10.1037/2160-4096.1.S.63
Nearchou, F., Flinn, C., Niland, R., Subramaniam, S. S., and Hennessy, E. (2020). Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int. J. Environ. Res. Public Health 17:8479. doi: 10.3390/ijerph17228479
Nikendei, C., Kindermann, D., Brandenburg-Ceynowa, H., Derreza-Greeven, C., Zeyher, V., Junne, F., et al. (2019). Asylum seekers’ mental health and treatment utilization in a three months follow-up study after transfer from a state registration-and reception-center in Germany. Health Policy 123, 864–872. doi: 10.1016/j.healthpol.2019.07.008
Phillimore, J. (2011). Refugees, acculturation strategies, stress and integration. J. Soc. Policy 40, 575–593. doi: 10.1017/S0047279410000929
Potter, F., Dohrmann, K., Rockstroh, B., Schauer, M., and Crombach, A. (2022). The impact of experiencing severe physical abuse in childhood on adolescent refugees’ emotional distress and integration during the COVID-19 pandemic. Front. Psychol. 13:1023252. doi: 10.3389/fpsyg.2022.1023252
Potter, F., Zehb, M., Dohrmann, K., Müller-Bamouh, V., Rockstroh, B., and Crombach, A. (2023). “It is worth hanging in there”–psychotherapeutic experiences shaping future motivation for outpatient psychotherapy with refugee clients in Germany. BMC Psychiatry 23, 1–11. doi: 10.1186/s12888-023-05004-3
Prati, G., and Mancini, A. D. (2021). The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 51, 201–211. doi: 10.1017/S0033291721000015
Ragab, N. J. (2018). Political participation of refugees. The case of afghan and Syrian refugees in Germany. Stockholm, Sweden: International Institute for Democracy and Electoral Assistance.
Richter, K., Peter, L., Lehfeld, H., Zäske, H., Brar-Reissinger, S., and Niklewski, G. (2018). Prevalence of psychiatric diagnoses in asylum seekers with follow-up. BMC Psychiatry 18, 206–207. doi: 10.1186/s12888-018-1783-y
Ryan, D. A., Benson, C. A., and Dooley, B. A. (2008). Psychological distress and the asylum process: a longitudinal study of forced migrants in Ireland. J. Nerv. Ment. Dis. 196, 37–45. doi: 10.1097/NMD.0b013e31815fa51c
Schick, M., Zumwald, A., Knöpfli, B., Nickerson, A., Bryant, R. A., Schnyder, U., et al. (2016). Challenging future, challenging past: the relationship of social integration and psychological impairment in traumatized refugees. Eur. J. Psychotraumatol. 7:28057. doi: 10.3402/ejpt.v7.28057
Schmidt, T. L., Catani, C., Dumke, L., Groß, M., Neldner, S., Scharpf, F., et al. (2023). Welcome, how are you doing?–towards a systematic mental health screening and crisis management for newly arriving refugees. Eur. J. Psychotraumatol. 14:2202053. doi: 10.1080/20008066.2023.2202053
Schneider, F., Bajbouj, M., and Heinz, A. (2017). Psychische Versorgung von Flüchtlingen in Deutschland [mental health care of refugees in Germany]. Nervenarzt 88, 10–17. doi: 10.1007/s00115-016-0243-5
Semmlinger, V., Takano, K., Schumm, H., and Ehring, T. (2021). Dropout from psychological interventions for refugees and asylum seekers: a meta-analysis. J. Consult. Clin. Psychol. 89, 717–730. doi: 10.1037/ccp0000681
Sevim, F., Kiran, S., Yesildag, A., and Yilmaz, G. (2023). Impact of COVID-19 pandemic on mental health of refugees, immigrants, and asylum-seekers: a systematic review. Psychiatry Behav. Sci. :13. doi: 10.5455/PBS.20230320110036
Siehl, S., Robjant, K., and Crombach, A. (2020). Systematic review and meta-analyses of the long-term efficacy of narrative exposure therapy for adults, children and perpetrators. Psychother. Res. 31, 695–710. doi: 10.1080/10503307.2020.1847345
Silove, D., Steel, Z., Susljik, I., Frommer, N., Loneragan, C., Chey, T., et al. (2007). The impact of the refugee decision on the trajectory of PTSD, anxiety, and depressive symptoms among asylum seekers: a longitudinal study. Am. J. Disaster Med. 2, 321–329. doi: 10.5055/ajdm.2007.0041
Silove, D., Ventevogel, P., and Rees, S. (2017). The contemporary refugee crisis: an overview of mental health challenges. World Psychiatry 16, 130–139. doi: 10.1002/wps.20438
Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., and Van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA 302, 537–549. doi: 10.1001/jama.2009.1132
Stenmark, H., Catani, C., Neuner, F., Elbert, T., and Holen, A. (2013). Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behav. Res. Ther. 51, 641–647. doi: 10.1016/j.brat.2013.07.002
Stuart, J., and Nowosad, J. (2020). The influence of Premigration trauma exposure and early Postmigration stressors on changes in mental health over time among refugees in Australia. J. Trauma. Stress. 33, 917–927. doi: 10.1002/jts.22586
Thygesen, L. C., Rosenkilde, S., Møller, S. P., Ersbøll, A. K., Santini, Z. I., Nielsen, M. B. D., et al. (2023). Changes in mental well-being during the COVID-19 pandemic: a longitudinal study among Danes from 2019 to 2021. J. Psychiatr. Res. 161, 310–315. doi: 10.1016/j.jpsychires.2023.03.024
Tinghög, P., Malm, A., Arwidson, C., Sigvardsdotter, E., Lundin, A., and Saboonchi, F. (2017). Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: a population-based survey. BMJ Open 7:e018899. doi: 10.1136/bmjopen-2017-018899
Tingvold, L., Vaage, A. B., Allen, J., Wentzel-Larsen, T., Van Ta, T., and Hauff, E. (2015). Predictors of acculturative hassles among Vietnamese refugees in Norway: results from a long-term longitudinal study. Transcult. Psychiatry 52, 700–714. doi: 10.1177/1363461515572208
Toar, M., O'Brien, K. K., and Fahey, T. (2009). Comparison of self-reported health & healthcare utilisation between asylum seekers and refugees: an observational study. BMC Public Health 9, 1–10. doi: 10.1186/1471-2458-9-214
United Nations High Commissioner for Refugees (2024). Global trends forced displacement in 2023. Copenhagen, Denmark: UNHCR.
Vaage, A. B., Thomsen, P. H., Silove, D., Wentzel-Larsen, T., Van Ta, T., and Hauff, E. (2010). Long-term mental health of Vietnamese refugees in the aftermath of trauma. Br. J. Psychiatry 196, 122–125. doi: 10.1192/bjp.bp.108.059139
Van Wyk, S., Schweitzer, R., Brough, M., Vromans, L., and Murray, K. (2012). A longitudinal study of mental health in refugees from Burma: the impact of therapeutic interventions. Aust. N. Z. J. Psychiatry 46, 995–1003. doi: 10.1177/0004867412443059
Walther, L., Rayes, D., Amann, J., Flick, U., Ta, T. M. T., Hahn, E., et al. (2021). Mental health and integration: a qualitative study on the struggles of recently arrived refugees in Germany. Front. Public Health 9:576481. doi: 10.3389/fpubh.2021.576481
Webb, R. T., Antonsen, S., Carr, M. J., Appleby, L., Pedersen, C. B., and Mok, P. L. (2017). Self-harm and violent criminality among young people who experienced trauma-related hospital admission during childhood: a Danish national cohort study. Lancet Public Health 2, e314–e322. doi: 10.1016/S2468-2667(17)30094-4
Wilker, S., Pfeiffer, A., Kolassa, S., Koslowski, D., Elbert, T., and Kolassa, I.-T. (2015). How to quantify exposure to traumatic stress? Reliability and predictive validity of measures for cumulative trauma exposure in a post-conflict population. Eur. J. Psychotraumatol. 6:28306. doi: 10.3402/ejpt.v6.28306
Keywords: refugees, mental health, integration, emotional distress, longitudinal research, follow-up study, Germany
Citation: Potter F, Dohrmann K, Rockstroh B and Crombach A (2024) Refugees’ integration and emotional distress over the course of 9 months. Front. Psychol. 15:1459934. doi: 10.3389/fpsyg.2024.1459934
Edited by:
Eleni Petkari, University of Malaga, SpainCopyright © 2024 Potter, Dohrmann, Rockstroh and Crombach. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Flurina Potter, Zmx1cmluYS5wb3R0ZXJAdW5pLWtvbnN0YW56LmRl
 Flurina Potter
Flurina Potter Katalin Dohrmann1,2
Katalin Dohrmann1,2 Brigitte Rockstroh
Brigitte Rockstroh Anselm Crombach
Anselm Crombach