- 1International Nursing School, Hainan Medical University, Haikou, China
- 2Department of Nursing Management, Hainan General Hospital, Haikou, China
Background: Depression seriously affects the quality of life of breast cancer patients and even hinders treatment and recovery after diagnosis. Subthreshold depression should be worthy of attention, and the risk of subthreshold depression developing into depression increases if timely intervention is not available. However, there is limited research on interventions for subthreshold depression, especially for newly diagnosed breast cancer patients.
Objective: Exploring the efficacy of a PERMA-based positive psychological intervention programme in newly diagnosed breast cancer patients with subthreshold depression.
Methods: Using PERMA as a framework, we constructed the intervention programme through a literature review and expert discussion approach, and revised the programme using the Delphi method. Then we selected 84 newly diagnosed breast cancer patients for a randomised controlled trial. The control group received conventional care (primary care, specialist care, psychological care, etc.), and the observation group received a PERMA-based positive psychological intervention programme. Patient data were collected before and after the intervention, and the dataset consisted of patient responses to general information, the Depression Screening Scale (CES-D), the Hamilton Depression Inventory (HAMD-17), and the Questionnaire on Psychosocial Adjustment in Breast Cancer Patients.
Results: A total of 79 patients completed the study (38 patients in the observation group and 41 patients in the control group), and before the intervention, there were no statistical differences in the comparison of general information, subthreshold depression scores, and psychosocial adaptation scores between the two groups (p > 0.05). After the intervention, the subthreshold depression (CES-D and HAMD-17 scores) scores of the observation group were lower than those of the control group (p < 0.01), and the psychosocial adaptation scores were significantly higher than those of the control group (p < 0.01).
Conclusion: A positive psychological intervention programme using PERMA as a framework was more effective in reducing subthreshold depression levels and promoting levels of psychosocial adjustment in newly diagnosed breast cancer patients.
Implications for practice: Interventions for subthreshold depression are not limited to the traditional aftercare model, but rather from a positive psychology perspective. Especially for patients newly diagnosed with breast cancer, this is a new endeavour that has important implications for them. Because, instead of focusing on their negative emotions, we help them gradually adapt to their new identity and treatment process from a positive aspect during their most difficult period, thus reducing their subthreshold depression level and preventing it from developing into a more severe depression.
Introduction
Major Depressive Disorder (MDD) is a common mental disorder and one of the major contributors to the global burden of disease, which is characterised by persistent low mood, loss of interest, and can even lead to suicide (Peveler et al., 2002; Wu et al., 2020). Subthreshold Depression (SD) is a psychological sub-health state between health and MDD for which there is no gold standard for diagnosis (Sadek and Bona, 2000; Zhang, 1998; Yuan et al., 2020). Newly diagnosed breast cancer patients face tremendous stress on their psychological and social functioning during the diagnosis and treatment process, which can impede their subsequent treatment and recovery and seriously affect their quality of life (Hamer et al., 2017). The prevalence of SD in patients with newly diagnosed of breast cancer is 48.6% or 60.56% (Lv et al., 2017; Chen et al., 2019), and such people are 5 times more likely to develop MDD than healthy people after 1 year (Liu et al., 2015). Failure to intervene in time for SD will increase the risk of MDD (Zhang et al., 2020; Ullah et al., 2022). In clinical, between diagnosis and completion of surgery, patients go through neoadjuvant chemotherapy, endocrine therapy, targeted therapy and other treatments (Zheng and Liu, 2024), which is a long and painful process. The longitudinal survey reported (Luo et al., 2024; Charles et al., 2022; Kanani et al., 2016), during this period, patients’ subthreshold depressive symptoms or clinical depressive symptoms were associated with poorer survival, and early screening was important, and then interventions were necessary for patients with HADS-D scores >11 by screening (HAMD subthreshold depression scores range 7–17). Therefore, healthcare providers need to be more attentive to SD in this population and use proactive preventive measures in a timely manner, which is important to prevent SD from evolving into more severe MDD (Zhang, 1998). In recent years, traditional psychology has turn to positive psychology and researchers are gradually discovering its value, positive psychology not only criticises the current model of post hoc “treatment” advocated by negative psychology, but also promotes the idea of positive “prevention” (Li et al., 2023; Liu et al., 2016; Fang et al., 2023). In 2011 Seligman (Seligman et al., 2005) proposed the positive psychology intervention model PERMA, which summarizes the five main elements that influence well-being as Positive emotions (P), Engagement (E), Relationships (R), Meaning (M) and Achievement (A). The model uses the five elements as an implementation framework for different interventions. It aims to uncover positive emotions and create positive outcomes (Miao et al., 2013). This approach has been demonstrated in various populations to be effective in reducing patients’ anxiety and depression and promoting their psychosocial resilience (Li et al., 2024; Chen et al., 2024; Liu et al., 2024). By reviewing the literature we found that there are fewer interventions on SD in newly diagnosed breast cancer patients. One study (Wu et al., 2024) reported that they performed an intervention on patients with SD after breast cancer surgery and reduced the level of depression in the patients, but they have only focused on postoperative SD in breast cancer patients, In addition, positive psychology has rarely been studied in SD patients with newly diagnosed breast cancer. Therefore, our study aims to explore the effectiveness of a intervention programmes constructed on the basis of PERMA and to evaluate the application of this programmes in SD patients with newly diagnosed breast cancer, which is a novel attempt.
Method
Study design
Before the study began, a research team was assembled. (i) One graduate nursing student was primarily responsible for the design and implementation of the study and the preparation of the data analysis article; (ii) One head nurse of the breast surgery department provided assistance in the implementation of the intervention; (iii) Two psychologists were responsible for the revision and improvement of the intervention programme was modified and implemented by the specialised clinical nurses who participated in the study. The distribution and collection of the questionnaires was undertaken by one graduate and one undergraduate nursing student. Overall quality control of the study was the responsibility of the graduate student supervisors.
The study was comprised of two distinct parts. (i) The first part involved the construction of a prevention programme based on the PERMA model. (ii) The programme was conducted as a randomised controlled study. Firstly, the intervention strategy was developed and the initial draft of the protocol was formulated using PERMA theory as a framework. This was followed by two rounds of Delphi expert communication, after which the intervention protocol was revised based on expert opinions and internal discussions within the research team. Subsequently, patients were selected through a rigorous recruitment process and the intervention was implemented as a randomised controlled trial. During the study, data was collected from patients before and after the intervention. This dataset included general information about the patients as well as responses to the CES-D, HAMD-17 and Psychosocial Adaptation questionnaires (Chinese version).
Operational definition
In study, we defined SD using the methodology of other researchers (Yuan et al., 2020; Ullah et al., 2022; Chen et al., 2024). There were two steps, firstly, the patients were assessed by using the CES-D. Secondly, these patients with CES-D scores more than16 were assessed again using the HAMD-17, and patients with scores between 7 and 17 were defined as SD (CES-D: >16, HAMD-17: 7 to 17).
Participants and setting
1. Participants included both the experts who developed the programme and the patients who received the intervention.
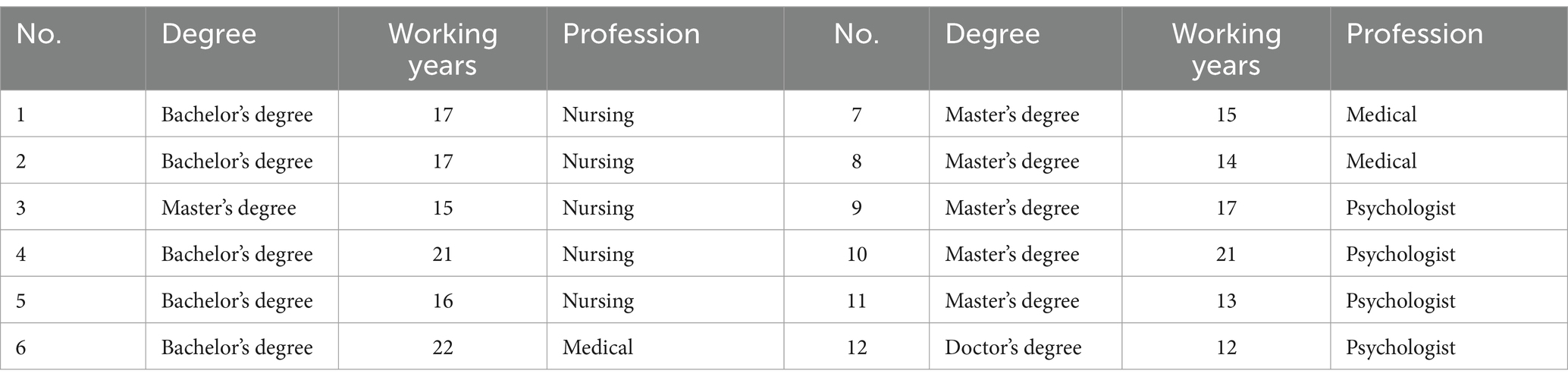
2. We selected experts from various professional backgrounds, including psycho-educational professors, clinicians, and clinical nursing specialists, based on the following criteria: (I) They were engaged in clinical medical care and psychology education; (II) They were familiar with positive psychology; (III) They had more than 10 years of experience in their respective professional fields, held an intermediate professional title or above, and possessed a bachelor’s degree or higher (Table 1).
3. From April to December 2022, patients in the breast surgery department of a hospital in Hainan Province, China, who had been newly diagnosed with breast cancer and exhibited SD, were chosen as the subjects of this study.
Inclusion criteria: (1) The first pathological diagnosis of breast cancer; (2) Depression Screening Scale (CES-D) score ≥ 16 points, and Hamilton Depression Scale (HAMD-17) score 7–17 points (Yuan et al., 2020; Ullah et al., 2022); (3) Patients receiving neoadjuvant chemotherapy and 6 cycles of chemotherapy; (4) Age 18–65 years old; (5) The expected survival time is more than 6 months (Wu et al., 2024).
Exclusion criteria: (1) have serious heart, brain, kidney organ dysfunction; (2) people with communication and visual impairment; (3) have participated in other researchers within the last 3 months; (4) do not know the disease.
Shedding criteria: (1) patients with serious life-threatening conditions; (2) those who quit midway due to irresistible factors; (3) participants participated in the intervention less than 3 times.
Samples size
We referred to a similar study, and used the sample size calculation formula for the comparison of the means of two independent samples: = =[( + ) 2 2]/ 2 (Chen, 2019), took the two-sided test, and the test level was set at α = 0.05 and β = 0.10, which was substituted into the formula to calculate a sample size of 72 cases for the two groups, and finally determined to be 84 cases considering the 15% sample shedding rate.
Recruitment, randomisation, and allocation
The study was double blinded and the study statisticians were randomly assigned to a group of 42 (1:1). Study allocation was based on a computer-generated random number table. Blind allocation was carried out using opaque sealed envelopes containing the allocation information from the computerised random number tables. To determine the experimental group, the envelopes were opened by the researcher with the consent of the subjects. In order to avoid any possible response bias or contamination, the researchers conducted the final tests by personnel who had no prior contact with the subjects. In addition, the two groups of patients were placed in two different wards (Ward A and Ward C) to avoid communication between the two groups.
Ethical considerations
The study was approved by the Medical Ethics Committee (HYLL-2024-163) before the start of the study, and the principles of benefit, respect, fairness and altruism were strictly observed in the implementation process, and patients voluntarily signed informed consent.
Quality control
The quality control of this study was carried out throughout the whole process of intervention implementation. We use PERMA as a guiding framework, reviewed the international literature to understand the psychological characteristics of patients with first diagnosis of breast cancer, solicited the opinions of clinical staff and psychologists, controlled the quality and feasibility of the programme by experts meeting, and ensured the reliability of the programme by the Delphi method. Before the intervention, staff were uniformly trained to ensure consistency of the intervention. During data collection, without any prompting or guidance, two researchers entered the data together and a statistician analyzed the results to ensure the accuracy of the study data. In order to avoid intergroup contamination, we placed the beds of the two groups of patients in partitioned areas, with the observation group in area A and the control group in area C, to reduce the communication between the two groups of patients on the content of the intervention. In addition, a psychologist supervised the quality of the intervention throughout its implementation.
Intervention
Observation group
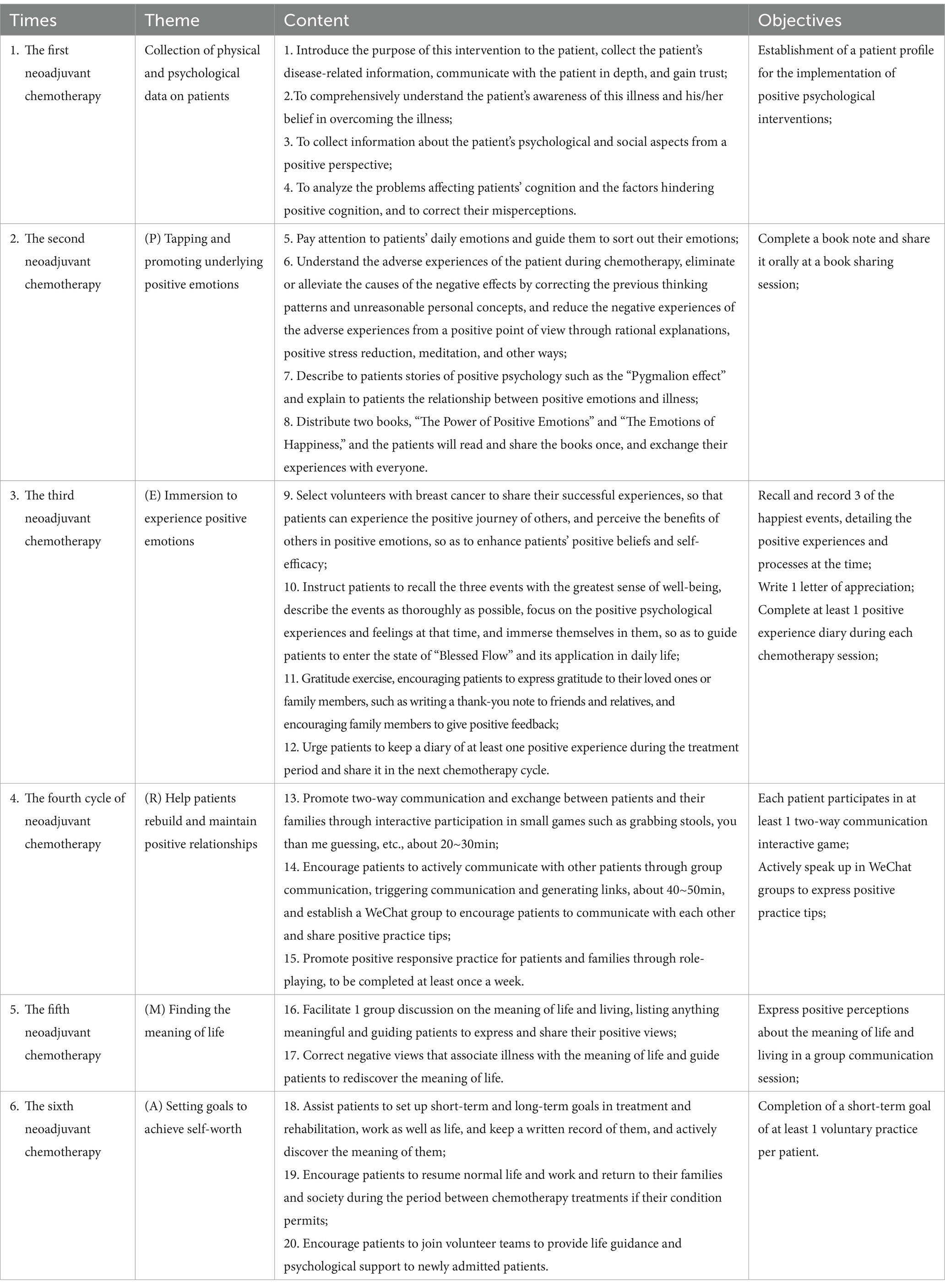
We adopted a positive psychological intervention programme based on PERMA, the implementation of which consisted of five components: tapping and enhancing patients’ positive emotions (positive emotions, P) and enabling patients to immerse themselves in a state of engagement (engagement, E); rebuilding and maintaining interpersonal relationships (relationships, R); discovering the meaning of life (meaning, M); and realizing the self (achievement, A). The intervention was conducted in the afternoon of the first day of each chemotherapy cycle in the patient’s health education room, with 4–6 participants in each group, for 30–50 min each time, and two psychotherapists were involved in guiding the whole implementation process, as shown in Table 2.
Control group
Provide patients with basic care, specialist care and psychological care, and timely psychological care based on SD screening results. Health education was carried out, and health education manuals were distributed to explain the precautions related to chemotherapy as well as the treatment and prevention of adverse reactions, and dietary guidance was given. At the end of each chemotherapy session, we learned about the patients’ psychological status, provided psychological counselling when necessary, helped patients adapt to the chemotherapy process, and explained the precautions to be taken for discharge and the next chemotherapy session. Weekly follow-up visits were made to answer patients’ questions and provide psychological counselling.
Research tools
1. General information questionnaire Including the patient’s age, education level, monthly family income, employment status, marital status, menstrual status, and chemotherapy regimen.
2. The Centre for Epidemiological Studies Depression Scale (CES-D) It is a commonly used international screening scale for MDD, and the Chinese version was cross-culturally validated by Zhang et al. (2010), which contains 20 items on a 0–3 point scale, with scores greater than 16 indicating different degrees of depression, and the higher the score, the higher the degree of depression, with a Cronbach’s α coefficient of 0.90.
3. Hamilton Rating Scale for Depression 17-item version (HAMD-17) It is a commonly used international depression scale, the Chinese version (Zheng et al., 1988) uses a 0–4 scale, which is routinely assessed through conversation and observation, with higher scores indicating more severe depression, and the criteria for depression assessment are that a total score of <7 is normal, 7–17 is probably depressed, 17–24 is definitely depressed, and > 24 is severely depressed, and its Cronbach’s α coefficient is 0.90.
4. Psychosocial Adaptation Questionnaire for Breast Cancer Patients The questionnaire was developed by Cheng (2010) and consisted of 63 items with five dimensions: anxiety/depression dimension, self-esteem and self-acceptance dimension, attitude dimension, self-control and self-efficacy dimension, and belongingness dimension. A 5-point Likert scale was used, with negative items reverse scored, and the higher the score, the higher the degree of psychosocial adjustment, as follows: <132 is low adjustment, 132–175 is moderate adjustment, and ≥ 176 is high adjustment, with a Cronbach’s α coefficient of 0.902 and a CVI >0.75.
Data analysis
The data of this study were recorded in Excel (version 2019) by two researchers and statistically analysed using SPSS 25.0. First, descriptive statistics were calculated per skewness, histograms, Q-Q plots, and box plots to test the distribution normality and possible continuous variable outliers. Before the intervention, the basic data of the two groups of patients were analyzed, age belongs to the measurement data and conforms to the normal distribution, the two-sample mean t-test was used for comparison; marital status, employment, menstruation, chemotherapy regimen data belongs to the counting data, the chi-square test was used for comparison; literacy, personal income belongs to the grade of the seniority data was used for comparison using the Kruskal-Wallis H test. Before and after the intervention, the CES-D, HAMD-17, total psychosocial adjustment scores and the scores of each dimension between the two groups conformed to the normal distribution, and the two samples t-test was used. Before and after the intervention, the CES-D and HAMD-17 scores within the two patient groups conformed to a normal distribution, using a paired-sample t-test before and after itself. The threshold of significance was set at 0.05.
Results
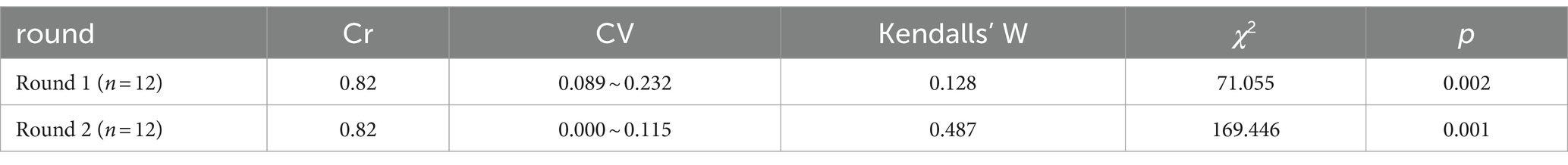
Programme validity
The intervention programme constructed on the basis of PERMA had good expert consistency and content validity (Table 3).
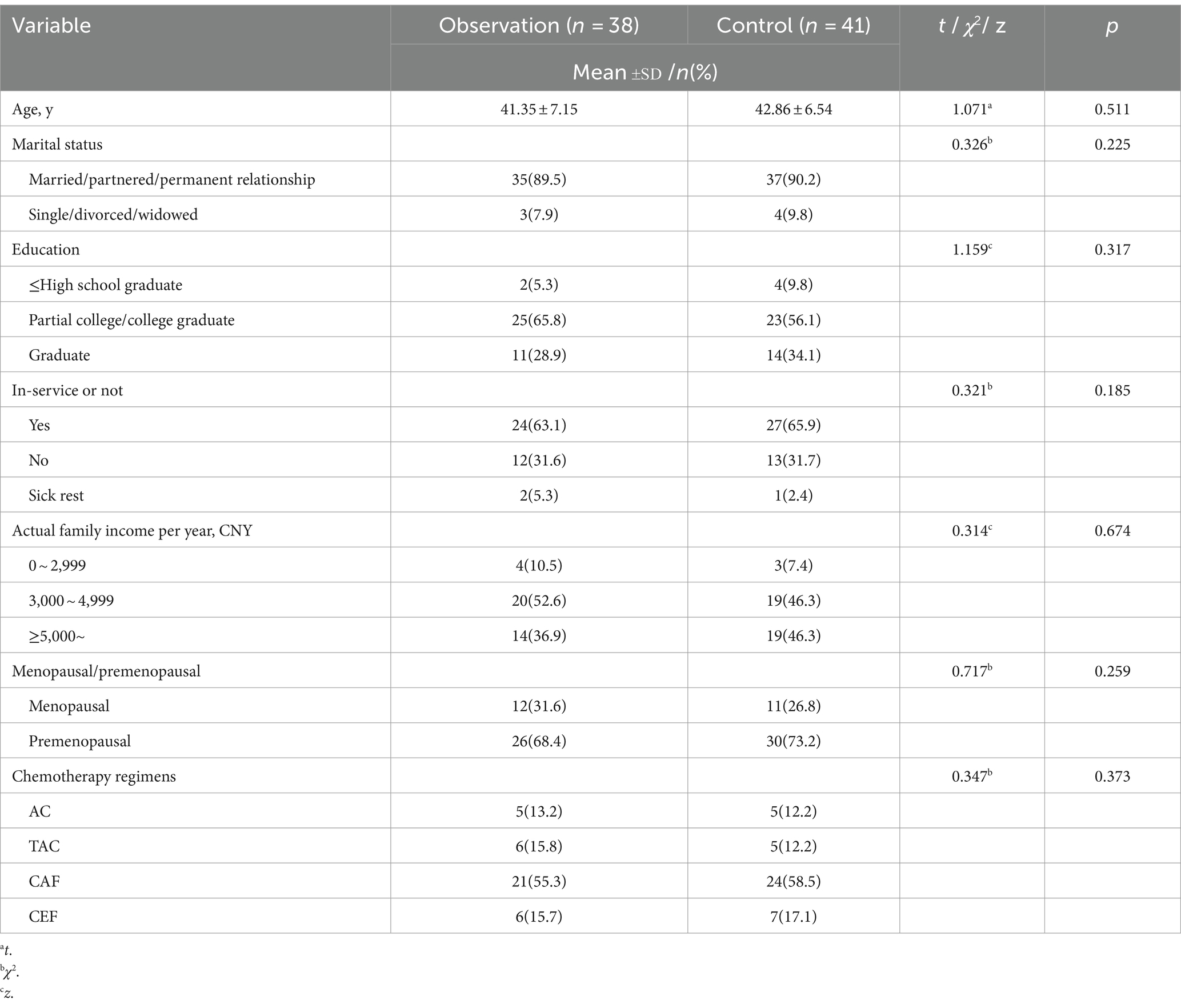
Sociodemographic characteristics
During the implementation of the intervention in this study, a total of 5 cases were missed: 1 case was missed in the observation group (the patient was referred to treatment for major depression), and a total of 4 cases were missed in the control group (2 cases were automatically withdrawn, 1 case was withdrawn in the second cycle of chemotherapy after a serious adverse reaction, and 1 case was terminated). Eventually, 38 patients in the experimental group and 41 in the control group, totaling 79 patients, completed the intervention. The baseline difference between the two groups was not statistically significant (p > 0.05) (Table 4).
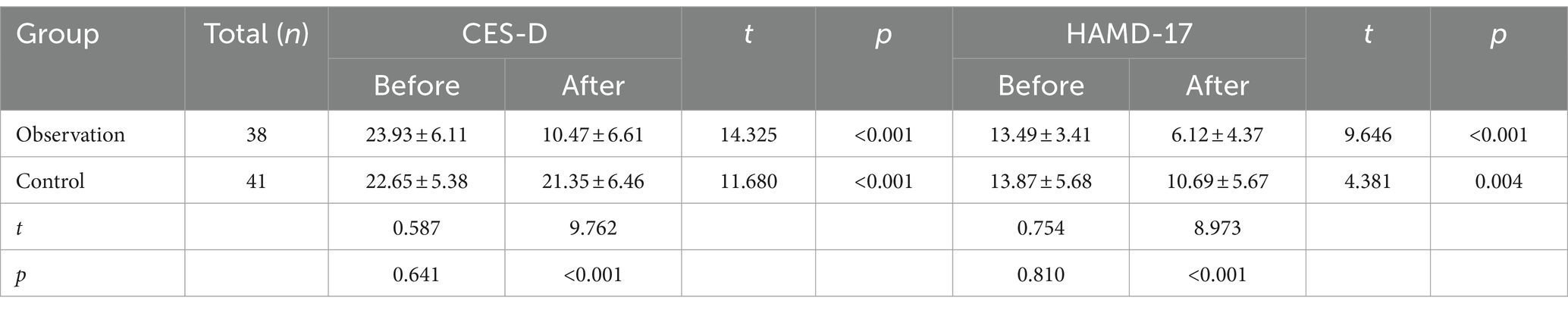
Comparison of subthreshold depression scores before and after intervention
The scores of CES-D and HAMD-17 showed no statistically significant difference between the two groups before intervention (p > 0.05), while the scores of the observation group were significantly lower than those of the control group after intervention (p < 0.001), as shown in Table 5.
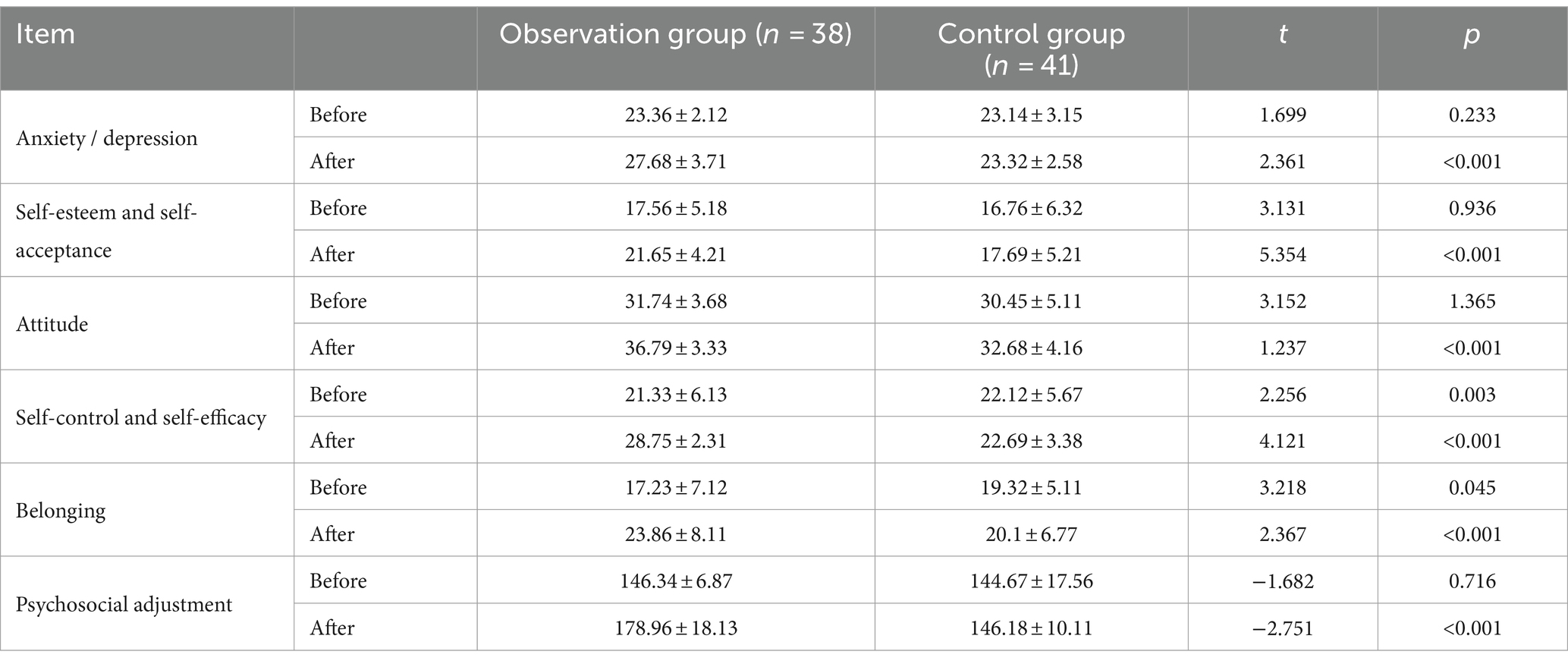
Comparison of psychosocial adaptation scores before and after intervention
Before intervention, there was no statistically significant difference in psychosocial adjustment scores between the two groups (p > 0.05). After intervention, the observation group was significantly higher than the control group, and the difference between the two groups was statistically significant (p < 0.001) (see Table 6).
Discussion
Validity of PERMA-based positive psychology intervention programmes
A study reported that the positive psychological intervention programme constructed around the five elements of positive emotions, participation, relationship, meaning and achievement, using PERMA as a framework, has a certain degree of scientific and normative validity (Cheng, 2010). When constructing the programme, we selected physicians, nurses, and psychoeducational experts with intermediate or higher titles, all of whom are experienced experts in the field, and discussed all the elements of the programme cautiously and agreed on the opinions. In Delphi studies, the validity of the findings depends on the authority of the expert (Cr) and the consistency of the expert’s opinion. It is generally accepted that an expert authority coefficient Cr ≥ 0.7 implies that the results of the study are reliable. The degree of expert coordination depends on the size of the coefficient of variation (Cv) and Kendall’s coefficient of concordance (Kendall’s W), the value of Kendall’s W ranges from 0 to 1, and the larger the value is, the better the degree of expert coordination is. A Cv value of less than 0.25 means that the more consistent the expert opinion is (p < 0.05). The results of the study showed that, the Cr value of the two rounds of consultation is 0.82, which indicates that the degree of expert authority is high, the Kendall’s W of the two rounds of correspondence is 0.128 and 0.487, and the Cv value is 0.089 ~ 0.232 and 0.00 ~ 0.15, which indicates that the expert opinions converge, and we terminate the expert consultation. Therefore, the scheme we constructed has good validity. In addition, in the process of intervention implementation, the two psychoeducational experts participated in the whole process of intervention guidance and quality control, and solved the problems of the patients on time. The retention rate in the intervention group was 90.5%, with patients completing all components of each intervention and meeting the intervention goals that were settled out in the program, making the intervention program feasible.
PERMA-based positive psychological intervention reduces SD levels in newly diagnosed breast cancer patients
Impaired body image and dysfunction experienced by breast cancer patients during treatment can exacerbate the patient’s increased psychological burden, with depression being the most common and worrisome issue, but less attention has been paid to SD (Liu et al., 2015). One study found that patients with SD were five times more likely to be depressed 1 year later than healthy individuals (Chen, 2019). Patients with first diagnosed breast cancer are in the early stages of disease treatment, and acceptance of the disease still requires a certain process of psychological adjustment, and SD should receive more attention (Zheng and Liu, 2024; Wu et al., 2024).
In this study, we used a 6-phase continuous intervention based on the PERMA positive psychology intervention programme. Firstly, we collected information on patients’ perceptions related to the disease and looked for their positive perceptions as much as possible. Secondly, by tapping into their underlying positive psychological factors and amplifying these positive emotions through guidance, such as reading two positive psychology books and sharing and exchanging them in groups in the form of book clubs. Third, patients participate in immersive experiential activities and enhance positive states. Through volunteers sharing their successful experiences (the volunteers are patients with positive emotions in the process of breast cancer recovery), patients perceive the benefits of others in positive emotions and enhance their positive experiences. For example, each patient shared three things that made them happy. Encourage patients to engage in gratitude exercises to express appreciation to family members. Record at least one positive experience during treatment and share it at the next stage. Fourth, help patients rebuild and maintain positive relationships. For example, the patient participated in some interactive games with others. Fifth, we held positive discussions to assist the patient in discovering the meaning of life. Sixth, we help patients to set long-term or short-term goals and promote their self-actualisation through the achievement of these goals. From the perspective of positive psychology, through understanding the patients’ self-perception of the disease, correcting incorrect perceptions, adopting different ways of explanation, dissection and excavation, and encouraging the patients to carry out positive guiding activities in the form of gratitude practice, writing expression, sharing and communication, the patients were gradually returned to a positive state of mind, experiencing the “input” and “blessing” of the patients. It gradually makes patients return to a positive psychological state, experience “input” and “blessing flow,” and then improves and relieves patients’ depression. The results of the study showed that the CES-D and HAMD-17 scores of patients in the observation group were significantly lower than those of the control group after the intervention, Significant differences were found within and between the two groups (p<0.001), indicating the effectiveness of positive psychological intervention based on PERMA in the subthreshold depressed population of first-diagnosed breast cancer, and the effect is significantly better than that of the conventional care group, which in turn proves that the effect of the positive psychology intervention model is superior to that of the traditional psychology intervention model. In China, Liu et al. (2024) and others adopted PERMA positive intervention for diabetic foot patients with similar results, through the guidance of the patients to re-establish goals and confidence, actively search for the meaning of life, and realize the self-worth of the patients with positive significance. Cheavens et al. (2006) and others implemented goal reconstruction and hope reconstruction of psychological interventions for cancer patients, similarly proved that goal adjustment has a positive effect on cancer patients.
In summary, in this study, we did not directly intervene or treat the patients’ adverse experiences and negative emotions, but rather, under the PERMA perspective, through a series of positive psychological interventions, we gradually guided the patients to discover their own positive emotions and good experiences, taught the patients to master the methods of obtaining positive emotions, actively guided the patients, prompted the patients to be more focused and fulfilled, assisted the patients in re-establishing interpersonal relationships, re-establishing life goals, and promoting self-realisation, etc., thus effectively alleviating SD in patients with first-diagnosed breast cancer.
PERMA-based positive psychological interventions improved levels of psychosocial adaptation in newly diagnosed breast cancer patients
“Psychosocial adaptation of breast cancer patients” refers to the emotional reactions, cognitive attitudes and self-evaluation of breast cancer patients when they encounter psychological stress, as well as the degree to which their own behaviors are compatible with various types of groups, such as the family, the collective, and the society, as well as coordinated with social customs and norms, which can be evaluated from the aspects of anxiety and depression, self-esteem and self-acceptance, attitudes, self-control and self-efficacy, and sense of belonging in five dimensions (Liu et al., 2021). Therefore, the subthreshold depression status of patients is also one of the important factors affecting the level of psychosocial adjustment of patients.
Li (2023) and others found that the level of psychosocial adaptation of patients with first diagnosis of breast cancer was at a low level, while the level of psychosocial adaptation of breast cancer patients could be improved by positive cognitive intervention (Zhao, 2023). In this study, we found that the positive psychological intervention simultaneously improved the patients’ psychosocial adaptation, and the difference was statistically significant (p<0.001). Some studies have pointed out that suffering from cancer seriously affects patients’ life goals and pursuit of self-worth, and reasonable adjustments should be made to the original life goals for different target groups, which can help to promote patients’ psychosocial adaptability, alleviate psychological burden, and improve prognostic outcomes (Ran et al., 2024). The goal of positive psychology is to develop personal strengths and enhance positive emotions, which in turn promotes positive changes in patients (Chen et al., 2024). Therefore, rather than working to urge patients to develop positive emotions from bad experiences and experiences, this intervention approach taps into the positive qualities and underlying strengths of patients and responds positively through a series of measures (Sin and Lyubomirsky, 2009). This study utilized positive-responsive exercises, role-playing, and two-way communication with family members to help patients engage in their roles and pass through the period of adjustment to the illness, and then assisted them in re-establishing their goals and pursuits and returning to normal life and work. In addition, by encouraging patients to act as volunteers to help other patients, it helps them to realize their self-worth and gain a sense of achievement, and therefore improves the psychosocial adaptive capacity of first-diagnosed breast cancer patients, which is similar to the findings of Niu et al. (2023) and others. Therefore, the subthreshold depression intervention program constructed on the basis of the positive psychology perspective of PERMA is similarly conducive to promoting the level of psychosocial adaptation of patients.
Limitations
This intervention study yielded relatively satisfactory preliminary results, but the limitations of this study are that the sample was selected from only one hospital, which may be under-representative, and the low baseline age of the intervention population, which leaves self-destructive and psychosocial resilience in the older population to be further investigated in the future. The absence of intentional analyses of the decontextualised sample is also a shortcoming as our study is still ongoing at this stage, which will be added in subsequent studies.
Despite the rigorous baseline treatment of the two groups in this study, the actual effect of demographic factors on depression cannot be ruled out, which is an issue that deserves ongoing attention to facilitate the provision of individualised interventions. In addition, the intervention period in this study was long, and we did not repeat the measurement of patients’ depression levels, so it is not possible to determine the impact of time effects on the results of the study, as problems with these measurement tools could lead to Barnum effects in psychological testing, which in turn could affect the results of the intervention.
Conclusion
In conclusion, SD in newly diagnosed breast cancer patients is a clinical problem that should not be ignored, and we should actively intervene as early as possible to prevent it from developing into more serious depression, which is very necessary for patients. The positive psychology intervention programme developed in this study based on PERMA is scientific, standardised, effective and operable, which can improve the SD condition of newly diagnosed breast cancer patients and promote their psychosocial adaptability. This shows that this intervention approach from a positive psychology perspective is recommendable, and further studies will be conducted to explore its long-term effects.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Hainan Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
DW: Data curation, Writing – original draft, Writing – review & editing, Investigation, Project administration, Software. BL: Project administration, Writing – original draft, Writing – review & editing. HX: Writing – original draft, Writing – review & editing, Investigation, Methodology. XW: Writing – original draft, Writing – review & editing, Validation. JX: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Key Research and Development Project in Hainan Province (ZDYF2022SHFZ102), Provincial Natural Science Foundation Project of Hainan Provincial Department of Science and Technology in 2023 (823RC495), and 2024 Joint Project of Health Science and Technology Innovation of Hainan Province (WSJK2024MS215).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Charles, C., Bardet, A., Larive, A., Gorwood, P., Ramoz, N., Thomas, E., et al. (2022). Characterization of depressive symptoms trajectories after breast Cancer diagnosis in women in France. JAMA Netw. Open 5:e225118. doi: 10.1001/jamanetworkopen.2022.5118
Cheavens, J. S., Feldman, D. B., Gum, A., Michael, S. T., and Snyder, C. R. (2006). Hope therapy in a community sample: a pilot investigation. Soc. Indic. Res. 77, 61–78. doi: 10.1007/s11205-005-5553-0
Chen, J. J. (2019) Research on the effect of group psychological intervention on the quality of life of subthreshold depressed patients with first diagnosis of breast cancer [D]. Changjiang University.
Chen, Y. F., Feng, Y. Y., and Zhai, W. J. (2024). Effects of psychological intervention under the PERMA model on fear of disease progression and perceived disease stress in patients with thrombosis after lower limb fracture [J]. Chinese Journal of Health Psychology 32, 719–723. doi: 10.13342/j.cnki.cjhp.2024.05.015
Chen, J. J., Wang, H., Zhang, H., and Ding, J. (2019). Relationship between subthreshold depressive status and quality of social relationships in patients with first diagnosis of breast cancer [J]. China Med. Herald 16, 37–40.
Cheng, R. (2010) Development of a psychosocial adaptation questionnaire for breast cancer patients and the correlation between psychosocial adaptation and quality of life [D]. China Medical University
Fang, H., Zeng, Y., Liu, Y., and Zhu, C. (2023). The effect of the PERMA model-based positive psychological intervention on the quality of life of patients with breast cancer. Heliyon 9:e17251. doi: 10.1016/j.heliyon.2023.e17251
Hamer, J., McDonald, R., Zhang, L., Verma, S., Leahey, A., Ecclestone, C., et al. (2017). Quality of life (QOL) and symptom burden (SB) in patients with breast cancer. Support Care Cancer 25, 409–419. doi: 10.1007/s00520-016-3417-6
Kanani, R., Davies, E. A., Hanchett, N., and Jack, R. H. (2016). The association of mood disorders with breast cancer survival: an investigation of linked cancer registration and hospital admission data for south East England. Psychooncology 25, 19–27. doi: 10.1002/pon.4037
Li, Q. (2023) Research on the trajectory of psychosocial adaptation of breast cancer patients and its relationship with body imagery [D]. Jiangsu University
Li, L. L., Li, X. Y., and Zeng, L. (2023). Progress of the PERMA model in cancer patients [J]. J. Nurse Adv. 38, 799–803. doi: 10.16821/j.cnki.hsjx.2023.09.006
Li, S. W., Wang, T., and Lei, C. L. (2024). The effects of stage-specific psychological interventions under the guidance of the PERMA model on the psychological status and subjective well-being of primiparous women [J]. Chin. J. Health Psychol. 32, 814–818. doi: 10.13342/j.cnki.cjhp.2024.06.003
Liu, L. J., An, J. H., Zhang, Y., and Zhang, J. X. (2024). Effect of positive psychological intervention based on PERMA model to improve psychosomatic symptoms in diabetic foot patients [J]. Nurs. Res. 38, 714–718. doi: 10.12102/j.issn.1009-6493.2024.04.029
Liu, X. F., Kang, F. Y., Li, Z. S., Guo, M. M., and Yang, Y. (2021). Progress in the study of psychosocial adaptation of breast cancer patients [J]. Gen. Pract. Nurs. 19, 4085–4088. doi: 10.12104/j.issn.1674-4748.2021.29.013
Liu, X. H., Ma, C. Q., and Song, C. X. (2016). Implications of new advances in positive psychological interventions for clinical nursing in China [J]. Nurs. Res. 30, 912–914. doi: 10.3969/j.issn.1009-6493.2016.08.006
Liu, Y., Tan, X., Zhang, J., Qiao, Y., Chen, L. X., Yu, L. L., et al. (2015). Current status and prospect of subthreshold depression identification [J]. World Chin. Med. 10, 798–800. doi: 10.3969/j.issn.1673-7202.2015.05.041
Luo, Y., Deng, Y. C., Zhou, Q. M., Zhou, F. M., and Zhang, H. (2024). A longitudinal study of cognitive level and negative emotions during neoadjuvant chemotherapy in breast cancer patients [J]. Anhui Med. 45, 630–635. doi: 10.3969/j.issn.1000-0399.2024.05.020
Lv, L. M., Zhang, X. H., Wang, X. X., and Zhang, J. L. (2017). A study of subthreshold depression and social participation status in young and middle-aged postoperative breast cancer patients [J]. J. Nurs. 32, 84–87. doi: 10.3870/j.issn.1001-4152.2017.06.084
Miao, Y. J., Li, M. J., and Zhu, X. H. (2013). Review of the research on "heart sheng" – a model of mental health based on positive psychology [J]. Shanghai Educ. Res. 1, 26–29. doi: 10.3969/j.issn.1007-2020.2013.01.008
Niu, M. R., Dong, S. W., Wang, H. C., Chen, X., Yin, Z., and Lv, M. (2023). Evaluation of the effectiveness of a group positive psychological intervention for parents of children with leukemia [J]. J. Nurs. 38, 15–18. doi: 10.3870/j.issn.1001-4152.2023.01.015
Peveler, R., Carson, A., and Rodin, G. (2002). ABC of psychological medicine: depression in medical patients. BMJ 325, 149–152. doi: 10.1136/bmj.325.7356.149
Ran, J. R., Sun, R. X., Jia, J. Y., Che, Z. Y., Li, R. X., and He, Y. (2024). Research progress on cancer patients’ ability to adjust life goals and its impact on physical and mental health [J]. Chin. Family Med., 1–8. doi: 10.12114/j.issn.1007-9572.2023.0613
Sadek, N., and Bona, J. (2000). Subsyndromal symptomatic depression: a new concept. Depress. Anxiety 12, 30–39. doi: 10.1002/1520-6394(2000)12:1<30::AID-DA4>3.0.CO;2-P
Seligman, M. E., Steen, T. A., Park, N., and Peterson, C. (2005). Positive psychology progress: empirical validation of interventions. Am. Psychol. 60, 410–421. doi: 10.1037/0003-066X.60.5.410
Sin, N. L., and Lyubomirsky, S. (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J. Clin. Psychol. 65, 467–487. doi: 10.1002/jclp.20593
Ullah, H., di Minno, A., Esposito, C., el-Seedi, H. R., Khalifa, S. A. M., Baldi, A., et al. (2022). Efficacy of a food supplement based on S-adenosyl methionine and probiotic strains in subjects with subthreshold depression and mild-to-moderate depression: a monocentric, randomized, cross-over, double-blind, placebo-controlled clinical trial. Biomed. Pharmacother. 156:113930. doi: 10.1016/j.biopha.2022.113930
Wu, C. S., Kuo, C. J., Su, C. H., Wang, S. H., and Dai, H. J. (2020). Using text mining to extract depressive symptoms and to validate the diagnosis of major depressive disorder from electronic health records. J. Affect. Disord. 260, 617–623. doi: 10.1016/j.jad.2019.09.044
Wu, G. F., Li, X. R., Zhong, M. F., Yang, L., Cheng, S. J., Chen, Y., et al. (2024). A study of the effect of cloud-based extended care on subthreshold depression in breast cancer patients [J]. Chin. J. Nurs. 59, 142–148. doi: 10.3761/j.issn.0254-1769.2024.02.002
Yuan, S. L., Zhu, C. Y., and Zhang, K. Y. (2020). Effects of nursing intervention guided by positive psychology theory on rehabilitation and social functioning of schizophrenic patients [J]. Hospital Manage. Forum 37, 40–43. doi: 10.3969/j.issn.1671-9069.2020.08.012
Zhang, M. Y. (1998). Handbook of psychiatric rating scales [M]. 2nd Edn. Changsha: Hunan Science and Technology Press.
Zhang, J., Wu, Z. Y., Fang, F., Li, J., Han, B. X., and Chen, Z. Y. (2010). Establishment of a national urban norm for the flow center depression scale [J]. Chin. J. Mental Health 24, 139–143. doi: 10.3969/J.issn.1000.6729.2010.02.015
Zhang, T., Zhao, B., Shi, C., Nie, B., Liu, H., Yang, X., et al. (2020). Subthreshold depression may exist on a spectrum with major depressive disorder: evidence from gray matter volume and morphological brain network. J. Affect. Disord. 266, 243–251. doi: 10.1016/j.jad.2020.01.135
Zhao, L. M. (2023) Study on the intervention effect of positive thinking cognitive therapy on psychosocial adaptation of breast cancer chemotherapy patients [D]. Jiangnan University.
Zheng, W., and Liu, Q. (2024). Year-end inventory of clinical research progress in breast cancer in 2023 [J]. Chin. J. Gen. Surg. 33, 669–682. doi: 10.7659/j.issn.1005-6947.2024.05.001
Keywords: breast cancer, PERMA, psychology, prevention, subthreshold depression
Citation: Wang D, Li B, Xin H, Wu X and Xia J (2024) A study of a PERMA-based positive psychological intervention programme in subthreshold depressed patients with newly diagnosed breast cancer: formulation and application. Front. Psychol. 15:1437025. doi: 10.3389/fpsyg.2024.1437025
Edited by:
Fei Fei Huang, Fujian Medical University, ChinaReviewed by:
Siaw Leng Chan, Universiti Putra Malaysia Bintulu Sarawak Campus, MalaysiaUmashankar Krishnappa, Manipal Academy of Higher Education, India
Copyright © 2024 Wang, Li, Xin, Wu and Xia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bin Li, bGJsYmxiMTk5OUAxNjMuY29t; Jieqiong Xia, NTQwNzAyMTQ0QHFxLmNvbQ==; Hongmei Xin, OTM5ODM4MjRAcXEuY29t
†These authors have contributed equally to this work
 Deju Wang
Deju Wang Bin Li2*†
Bin Li2*†