- 1Social Determinants of Health Research Center, Saveh University of Medical Sciences, Saveh, Iran
- 2School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Research Center for Biochemistry and Nutrition in Metabolic Diseases, Institute for Basic Sciences, Kashan University of Medical Sciences, Kashan, Iran
Background: Fatigue is a prevalent issue among cancer patients. Cognitive behavioral therapy (CBT) is an individualized intervention that empowers patients and caregivers to actively participate in the treatment process. A recent systematic review and meta-analysis examined the impact of CBT on fatigue in cancer patients.
Methods: Articles published up to April 2023 were systematically searched in Scopus, PubMed, and the Web of Science using relevant keywords. All randomized clinical trials (RCTs) investigating the effects of CBT on fatigue in cancer patients were included. Statistical analyses were conducted using Stata version 14, with a significance level set at a p-value of <0.05.
Results: The current systematic review and meta-analysis encompasses 10 RCTs. CBT demonstrated a significant reduction in fatigue scores among cancer patients [standardized mean difference (WMD): −2.50; 95%CI: −3.43, −1.56; I2 = 95.8%, p < 0.001]. This effect was consistent across all subgroup analyses.
Conclusion: This study underscores the significant impact of CBT on fatigue in cancer patients. Further randomized clinical trials focusing on various cancer types are warranted to validate and build upon these findings.
1 Background
Cancer poses a significant public health challenge worldwide (Sun et al., 2023; Milajerdi et al., 2018). Global cancer statistics project that the number of cancer cases will soar to 27 million individuals by 2040 (Sung et al., 2021). The World Health Organization (WHO) reports that cancer contributes to the highest burden of diseases globally, accounting for a total of 244.6 million disability-adjusted life years (DALYs) worldwide (Mattiuzzi and Lippi, 2019). While advanced treatment modalities such as chemotherapy and radiotherapy have led to improved survival rates among cancer patients in recent years (Choi et al., 2022; Darooghegi Mofrad et al., 2020), the adverse effects of these treatments remain a major concern for public health systems (Sung et al., 2021). Cancer-related fatigue (CRF) is a prevalent issue among cancer patients, often persisting even after conventional cancer treatments (Liu et al., 2022). Patients endure a distressing and enduring sensation of physical, cognitive, and emotional fatigue linked to cancer or its treatment, disrupting their daily functioning (Kröz et al., 2023).
Given the increased longevity of cancer patients, enhancing their quality of life and survival outcomes while mitigating physical, psychological, and psychosocial challenges is paramount (Zhang et al., 2022). Psychosocial interventions such as cognitive behavioral therapy (CBT) have demonstrated effectiveness in alleviating various physical and mental complications associated with cancer (Moorey and Greer, 2011). CBT interventions encompass a range of psychotherapeutic techniques aimed at addressing maladaptive behaviors and psychological distress through cognitive and behavioral modifications (Kaplan et al., 1995). By imparting essential skills to modify dysfunctional thoughts and behaviors, CBT empowers patients to take control of their condition, thereby boosting their self-assurance in battling the disease (Grégoire et al., 2017; Dobson and Dozois, 2021). A systematic review and meta-analysis focusing on breast cancer patients revealed that CBT significantly enhanced the quality of life among this patient population (Getu et al., 2021; Yennurajalingam et al., 2023). Furthermore, a systematic review evaluating the efficacy of CBT in managing cancer-related fatigue (CRF) in advanced cancer patients demonstrated a significant reduction in CRF scores compared to standard care (Poort et al., 2020). Another meta-analysis involving patients undergoing or post-cancer treatment indicated that combined CBT effectively reduced CRF levels (Hilfiker et al., 2018). Consistent findings were also observed in a comprehensive analysis of 6 randomized controlled trials (RCTs) involving 472 breast cancer patients (Zhang et al., 2019).
Despite these insights, to the best of our knowledge, there exists no comprehensive systematic review and meta-analysis specifically investigating the effects of CBT as a standalone intervention on CRF in cancer patients. Therefore, our objective is to conduct a current systematic review and meta-analysis to explore the impact of CBT on fatigue in individuals with cancer.
2 Methods
This systematic review and meta-analysis was performed according to PRISMA guidelines (Page et al., 2021). Scopus, PubMed, and Web of Science were searched using MESH and non-MESH terms up to April 2023: ((“cognitive therapy”[tiab] OR “cognitive-behavioral therapy”[tiab] OR “Cognitive Behavioral Intervention”[tiab] OR “cognitive behavioral therapy”[tiab] OR CBT[tiab]) AND (“cancer”[tiab] OR “tumour”[tiab] OR “tumor” [tiab]) AND (trial[tiab])). No time or language restrictions were applied during the search.
2.1 Eligibility criteria
The following criteria were considered for including studies: (A) original randomized controlled clinical trials, (B) studies conducted among cancer patients, (C) studies investigating the effects of cognitive-behavioral therapy alone, and (D) reported changes in fatigue score or baseline and final scores of fatigue in the intervention and control groups.
The exclusion criteria were: (1) systematic reviews and meta-analyses, (2) studies involving healthy subjects or patients with other diseases than cancer, (3) studies without a control group, and (4) studies examining multiple interventions along with CBT. In addition, grey literature, including theses and conference abstracts, was not included.
2.2 Data extraction
The following data were collected from each study by two independent researchers: first author’s name, year of publication, study location, study design, mean age and standard deviation, gender distribution in the intervention and control groups, number of participants in each group, intervention and control groups, mean and standard deviation of fatigue score before and after the intervention in each group, and any adjustments made for confounding factors. To ensure the reliability and accuracy of the data, two researchers independently collected them. Any disagreements between the researchers were resolved by a third researcher (AM).
2.3 Statistical analysis
Mean differences and confidence intervals were calculated using mean and standard deviation (SD) changes in the fatigue score between the intervention and control groups. In cases where variation was reported in other variables than SD, we calculated SD using the appropriate formula. Between-study heterogeneity was assessed using the Cochrane Q test and I2 statistics, which quantify the degree of variability across studies included in the analysis. In cases of significant between-studies heterogeneity, random-effect analysis was used for the analysis. Subgroup analyses were performed using the fixed-effect model. Stata version 14 (Stata Corp., College Station, TX) was used in the current meta-analysis. A p-value of <0.05 was considered statistically significant.
3 Results
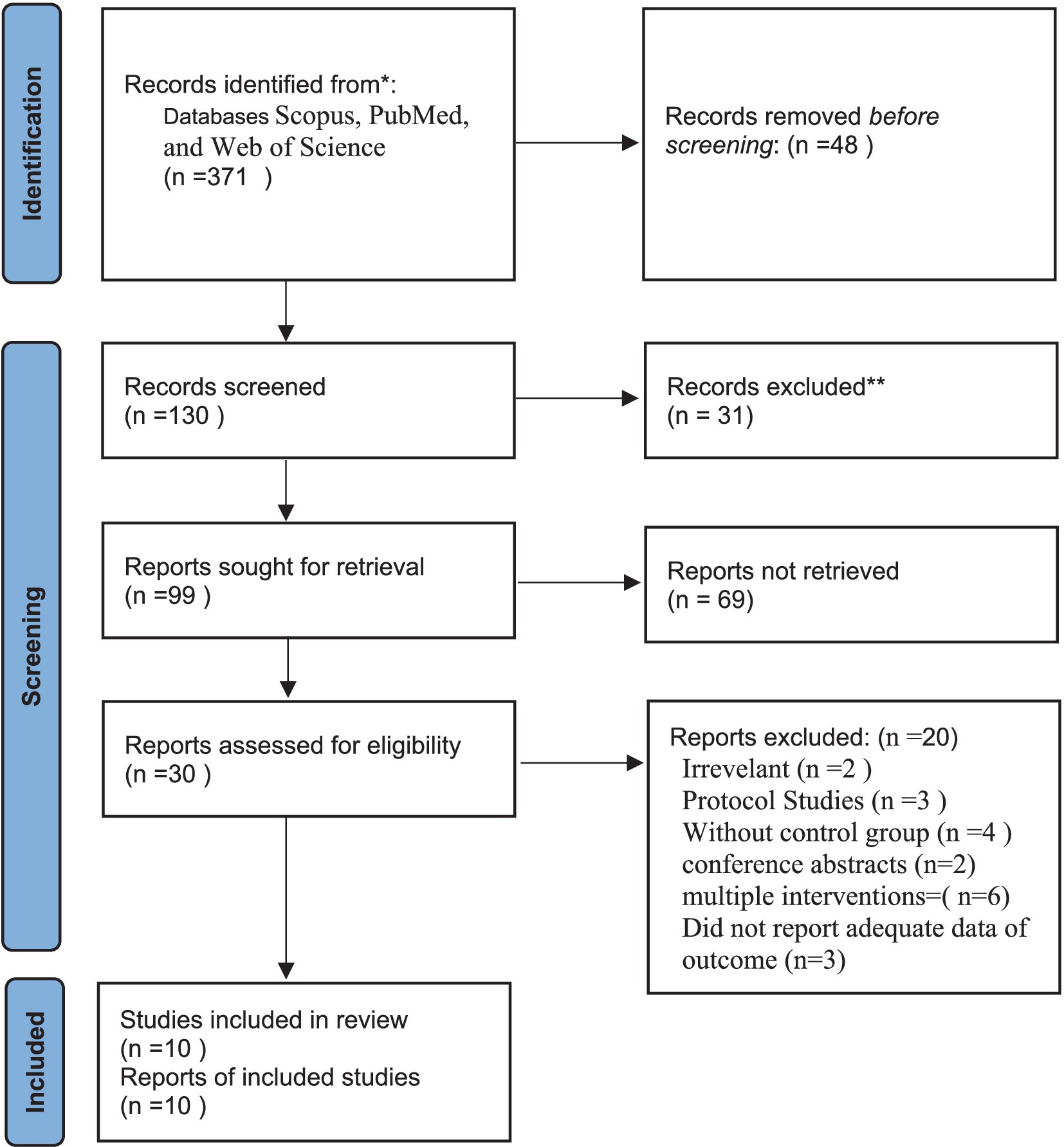
Overall, 371 papers were found in our initial search. After initial screening by title and abstract, 56 articles remained for the second stage of screening. Some of these articles were excluded after screening by the full text. In total, 10 RCTs were included in the current systematic review and meta-analysis (Grégoire et al., 2017; Abrahams et al., 2017; Bean et al., 2021; Goedendorp et al., 2014; Goedendorp et al., 2010; Hyland et al., 2022; Jim et al., 2020; Sheikhzadeh et al., 2021; van Weert et al., 2010; Wells-Di Gregorio et al., 2019). The flow diagram of study selection is shown in Figure 1.
3.1 Characteristics of included studies
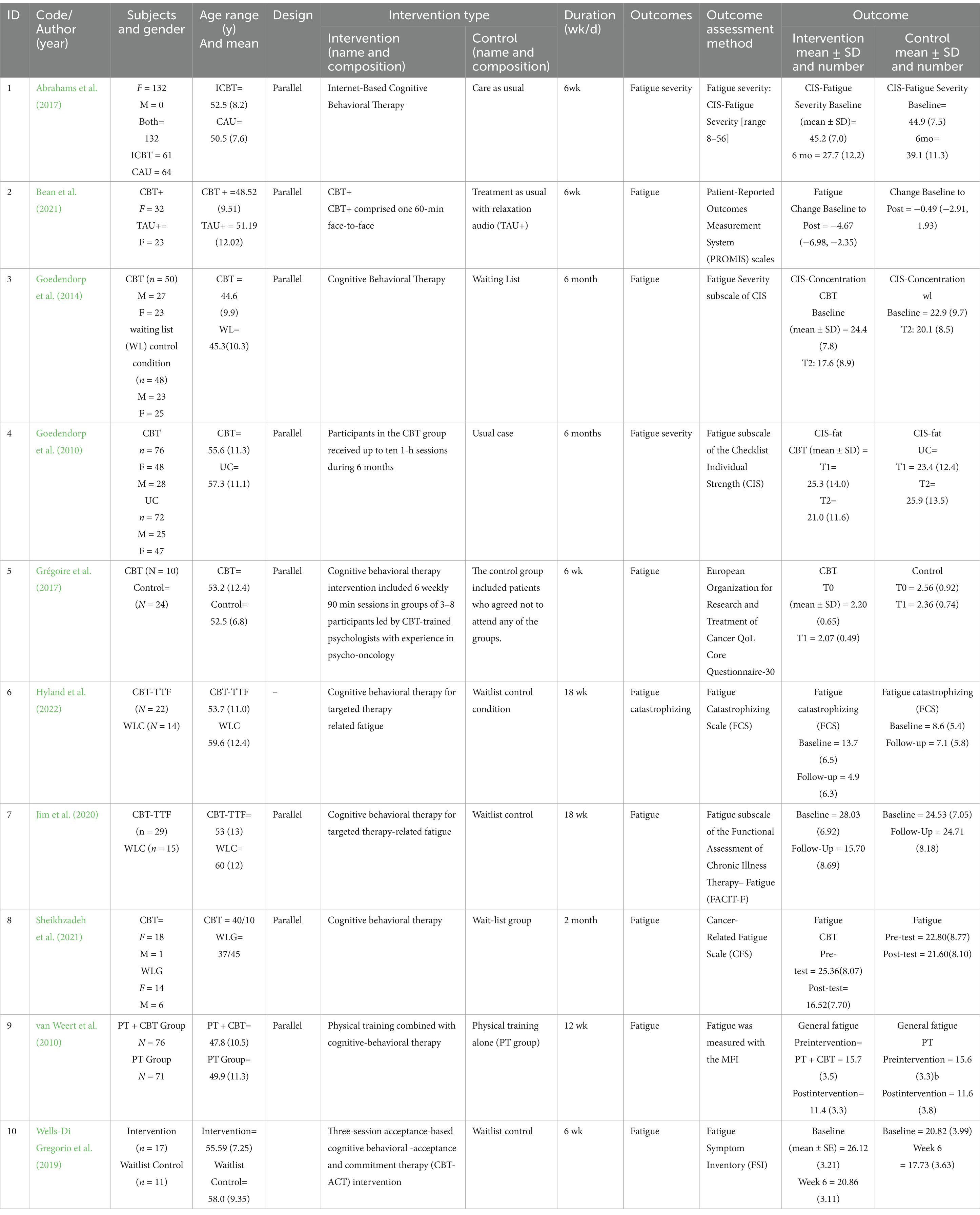
The general characteristics of included studies are summarized in Table 1. The studies were published between 2010 and 2022. Overall, 754 cancer cases participated in those studies. Four studies were performed exclusively on women (Grégoire et al., 2017; Abrahams et al., 2017; Bean et al., 2021; Jim et al., 2020), while the others included both genders. Cognitive behavioral therapy (Grégoire et al., 2017; Abrahams et al., 2017; Bean et al., 2021; Goedendorp et al., 2014; Jim et al., 2020; Sheikhzadeh et al., 2021; Wells-Di Gregorio et al., 2019) and physical training combined with cognitive-behavioral therapy (Goedendorp et al., 2010; Hyland et al., 2022; van Weert et al., 2010) were their interventions. Usual care (Abrahams et al., 2017; Goedendorp et al., 2010), physical training alone (van Weert et al., 2010), and being put on the waiting list (Goedendorp et al., 2010; Hyland et al., 2022; Jim et al., 2020; Sheikhzadeh et al., 2021; Wells-Di Gregorio et al., 2019) were the control groups. The study duration ranged between 6 weeks and 6 months.
3.2 Findings from the meta-analysis
CBT resulted in a significant reduction in fatigue score in cancer patients [standardized mean difference (WMD): −2.50; 95%CI: −3.43, −1.56, I2 = 95.8%, p = <0.001] (Figure 2). This finding remained unchanged after subgroup analysis by study duration (<1 month, ≥1 month), study sample size (<100, ≥100), and the study publication year (<2020, ≥2020) (Figures 3A–C).
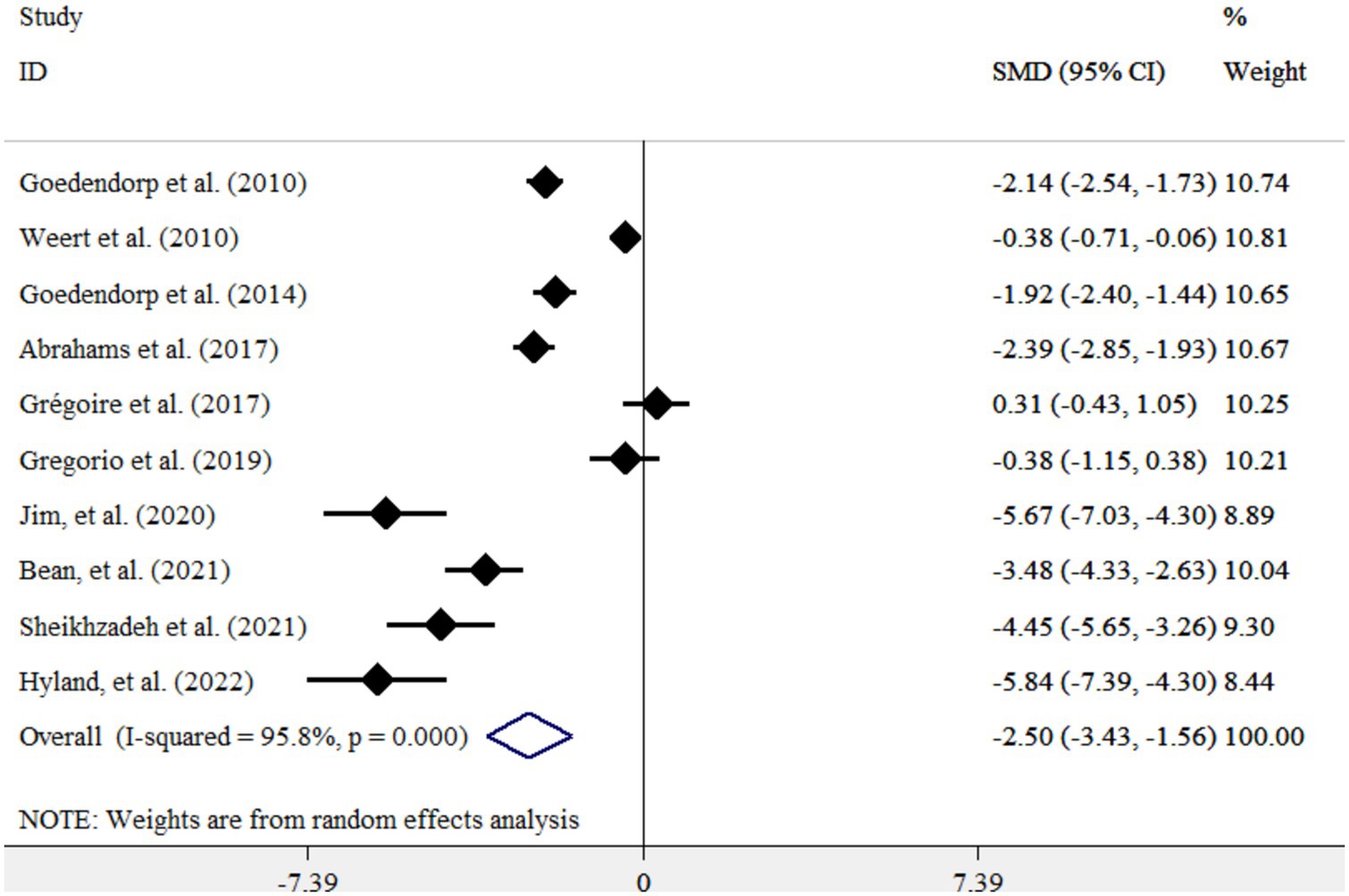
Figure 2. Forest plot for the effects of CBT on fatigue scores in cancer patients. Diamonds represent pooled estimates from random-effects analysis. Horizontal lines represent 95% CIs.
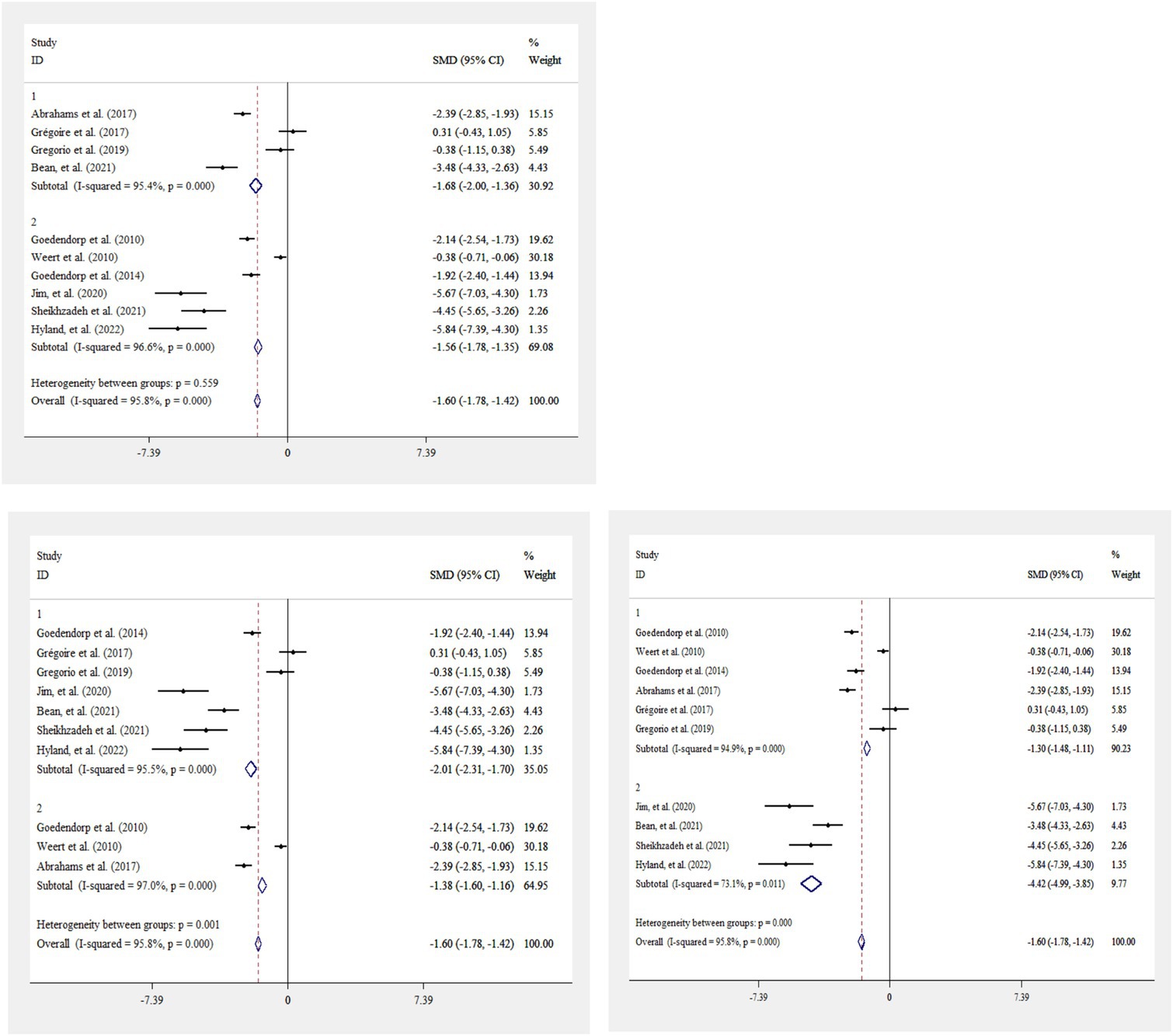
Figure 3. Forest plot for the effects of CBT on fatigue score in cancer patients, stratified by study duration (<1 month, ≥1 month) (A), study sample size (<100, ≥100) (B), and study publication year (<2020, ≥2020) (C). Diamonds represent pooled estimates from random-effects analysis. Horizontal lines represent 95% CIs.
4 Discussion
The current study demonstrated a significant impact of cognitive behavioral therapy (CBT) on fatigue scores in cancer patients, even conducting a subgroup analysis. To the best of our knowledge, this represents the inaugural systematic review and meta-analysis delving into the effects of CBT as a standalone intervention on fatigue in individuals with cancer.
In alignment with our meta-analysis, a recent systematic review and meta-analysis also underscored the notable effect of CBT on fatigue (Xu et al., 2023). This study highlighted the efficacy of CBT-based interventions in reducing sick leave duration and facilitating employees’ return to work. Conversely, a separate meta-analysis focusing on patients with knee osteoarthritis failed to observe a significant enhancement in fatigue levels (Lin et al., 2023). While several systematic reviews have explored the impact of CBT in conjunction with other psychological interventions on fatigue and other mental or physical variables in cancer patients (Maunick et al., 2023; Belloni et al., 2022; Blumenstein et al., 2022), the heterogeneous nature of the included studies has precluded definitive conclusions regarding the effects of CBT on fatigue in this population.
CBT is a personalized intervention that empowers patients and caregivers to actively engage in the treatment process (Sensky et al., 2000). The low dropout rates associated with CBT underscore its acceptability among patients. This approach enables individuals to gain insights into their symptoms, develop more adaptive attributions, and cultivate coping strategies for various manifestations, such as auditory hallucinations and paranoid beliefs. Moreover, CBT has been shown to enhance attitudes toward treatment, promote medication adherence, reduce relapse rates, and lower re-hospitalization rates (Rathod et al., 2005; Gumley et al., 2003). Importantly, CBT is considered a safe therapeutic modality, with no documented elevations in suicidal ideation, agitation, or violent behaviors (Turkington et al., 2003).
This study marks the first meta-analysis specifically focusing on fatigue in cancer patients within the context of CBT as a standalone intervention. The analysis encompassed studies where CBT interventions were administered independently, and fatigue was assessed using validated methodologies. However, certain limitations should be acknowledged. The meta-analysis included diverse cancer types, suggesting the need for further randomized controlled trials tailored to each specific cancer type. Additionally, variations in the measurement of fatigue using different questionnaires, lack of adjustment for confounding variables in the majority of studies, and limited reporting on distinct types of fatigue hindered the ability to conduct subgroup analyses. Finally, discrepancies in the duration of interventions served as a potential source of bias in the current meta-analysis.
5 Conclusion
In conclusion, our systematic review and meta-analysis demonstrated a significant effect of CBT on fatigue in patients with cancer. Further randomized clinical trials focusing on various types of cancer are necessary to provide additional insights into this matter.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
PH: Data curation, Writing – original draft. MK: Data curation, Formal analysis, Writing – original draft. MG: Conceptualization, Data curation, Methodology, Writing – original draft. AM: Project administration, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abrahams, H. J., Gielissen, M. F., Donders, R. R., Goedendorp, M. M., van der Wouw, A. J., Verhagen, C. A., et al. (2017). The efficacy of internet-based cognitive behavioral therapy for severely fatigued survivors of breast cancer compared with care as usual: a randomized controlled trial. Cancer 123, 3825–3834. doi: 10.1002/cncr.30815
Bean, H. R., Diggens, J., Ftanou, M., Alexander, M., Stafford, L., Bei, B., et al. (2021). Light enhanced cognitive behavioral therapy (CBT+) for insomnia and fatigue during chemotherapy for breast Cancer: a randomized controlled trial. medRxiv. doi: 10.1093/sleep/zsab246
Belloni, S., Arrigoni, C., Arcidiacono, M. A., Baroni, I., Conte, G., Dellafiore, F., et al. (2022). A systematic review of systematic reviews and pooled Meta-analysis on psychosocial interventions for improving Cancer-related fatigue. Semin. Oncol. Nurs. 39:151354. doi: 10.1016/j.soncn.2022.151354
Blumenstein, K. G., Brose, A., Kemp, C., Meister, D., Walling, E., DuVall, A. S., et al. (2022). Effectiveness of cognitive behavioral therapy in improving functional health in cancer survivors: a systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 175:103709. doi: 10.1016/j.critrevonc.2022.103709
Choi, T.-Y., Ang, L., Jun, J. H., Alraek, T., Birch, S., Lu, W., et al. (2022). Acupuncture for managing cancer-related fatigue in breast cancer patients: a systematic review and meta-analysis. Cancers 14:4419. doi: 10.3390/cancers14184419
Darooghegi Mofrad, M., Milajerdi, A., Sheikhi, A., and Azadbakht, L. (2020). Potato consumption and risk of all cause, cancer and cardiovascular mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Crit. Rev. Food Sci. Nutr. 60, 1063–1076. doi: 10.1080/10408398.2018.1557102
Dobson, K. S., and Dozois, D. J. (2021). Handbook of cognitive-behavioral therapies. New York, NY: Guilford Publications.
Getu, M. A., Chen, C., Panpan, W., Mboineki, J. F., Dhakal, K., and Du, R. (2021). The effect of cognitive behavioral therapy on the quality of life of breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Qual. Life Res. 30, 367–384. doi: 10.1007/s11136-020-02665-5
Goedendorp, M. M., Knoop, H., Gielissen, M. F., Verhagen, C. A., and Bleijenberg, G. (2014). The effects of cognitive behavioral therapy for postcancer fatigue on perceived cognitive disabilities and neuropsychological test performance. J. Pain Symptom Manag. 47, 35–44. doi: 10.1016/j.jpainsymman.2013.02.014
Goedendorp, M. M., Peters, M. E., Gielissen, M. F., Witjes, J. A., Leer, J. W., Verhagen, C. A., et al. (2010). Is increasing physical activity necessary to diminish fatigue during cancer treatment? Comparing cognitive behavior therapy and a brief nursing intervention with usual care in a multicenter randomized controlled trial. Oncologist 15, 1122–1132. doi: 10.1634/theoncologist.2010-0092
Grégoire, C., Bragard, I., Jerusalem, G., Etienne, A.-M., Coucke, P., Dupuis, G., et al. (2017). Group interventions to reduce emotional distress and fatigue in breast cancer patients: a 9-month follow-up pragmatic trial. Br. J. Cancer 117, 1442–1449. doi: 10.1038/bjc.2017.326
Gumley, A., Ogrady, M., Mcnay, L., Reilly, J., Power, K., and Norrie, J. (2003). Early intervention for relapse in schizophrenia: results of a 12-month randomized controlled trial of cognitive behavioural therapy. Psychol. Med. 33, 419–431. doi: 10.1017/S0033291703007323
Hilfiker, R., Meichtry, A., Eicher, M., Balfe, L. N., Knols, R. H., Verra, M. L., et al. (2018). Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. Br. J. Sports Med. 52, 651–658. doi: 10.1136/bjsports-2016-096422
Hyland, K. A., Nelson, A. M., Eisel, S. L., Hoogland, A. I., Ibarz-Pinilla, J., Sweet, K., et al. (2022). Fatigue perpetuating factors as mediators of change in a cognitive behavioral intervention for targeted therapy-related fatigue in chronic myeloid leukemia: a pilot study. Ann. Behav. Med. 56, 137–145. doi: 10.1093/abm/kaab035
Jim, H. S., Hyland, K. A., Nelson, A. M., Pinilla-Ibarz, J., Sweet, K., Gielissen, M., et al. (2020). Internet-assisted cognitive behavioral intervention for targeted therapy–related fatigue in chronic myeloid leukemia: results from a pilot randomized trial. Cancer 126, 174–180. doi: 10.1002/cncr.32521
Kaplan, C. A., Thompson, A. E., and Searson, S. M. (1995). Cognitive behaviour therapy in children and adolescents. Arch. Dis. Child. 73, 472–475. doi: 10.1136/adc.73.5.472
Kröz, M., Quittel, F., Reif, M., Zerm, R., Pranga, D., Bartsch, C., et al. (2023). Four-year follow-up on fatigue and sleep quality of a three-armed partly randomized controlled study in breast cancer survivors with cancer-related fatigue. Sci. Rep. 13:2705. doi: 10.1038/s41598-022-25322-y
Lin, H.-M., Hsieh, P.-S., Chen, N.-C., Tsai, C.-H., Kuo, W.-F., Lee, Y.-L., et al. (2023). Impact of cognitive behavior therapy on osteoarthritis-associated pain, insomnia, depression, fatigue, and physical function in patients with knee/hip osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Front. Med. 9:1083095. doi: 10.3389/fmed.2022.1083095
Liu, Y.-C., Hung, T.-T., Konara Mudiyanselage, S. P., Wang, C.-J., and Lin, M.-F. (2022). Beneficial exercises for Cancer-related fatigue among women with breast Cancer: a systematic review and network meta-analysis. Cancers 15:151. doi: 10.3390/cancers15010151
Mattiuzzi, C., and Lippi, G. (2019). Current cancer epidemiology. J. Epidemiol. Glob. Health 9, 217–222. doi: 10.2991/jegh.k.191008.001
Maunick, B., Skvarc, D., Olive, L., and Mikocka-Walus, A. (2023). Effects of acceptance and commitment therapy on fatigue for patients with cancer and other chronic health conditions: a systematic review and meta-analysis. J. Psychosom. Res. 171:111366. doi: 10.1016/j.jpsychores.2023.111366
Milajerdi, A., Namazi, N., Larijani, B., and Azadbakht, L. (2018). The association of dietary quality indices and cancer mortality: a systematic review and meta-analysis of cohort studies. Nutr. Cancer 70, 1091–1105. doi: 10.1080/01635581.2018.1502331
Moorey, S., and Greer, S. (2011). Oxford guide to CBT for people with cancer. United States: OUP Oxford.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 88:105906. doi: 10.1016/j.ijsu.2021.105906
Poort, H., Peters, M., Van Der Graaf, W., Nieuwkerk, P., Van de Wouw, A., Nijhuis-van Der Sanden, M., et al. (2020). Cognitive behavioral therapy or graded exercise therapy compared with usual care for severe fatigue in patients with advanced cancer during treatment: a randomized controlled trial. Ann. Oncol. 31, 115–122. doi: 10.1016/j.annonc.2019.09.002
Rathod, S., Kingdon, D., Smith, P., and Turkington, D. (2005). Insight into schizophrenia: the effects of cognitive behavioural therapy on the components of insight and association with sociodemographics—data on a previously published randomised controlled trial. Schizophr. Res. 74, 211–219. doi: 10.1016/j.schres.2004.07.003
Sensky, T., Turkington, D., Kingdon, D., Scott, J. L., Scott, J., Siddle, R., et al. (2000). A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Arch. Gen. Psychiatry 57, 165–172. doi: 10.1001/archpsyc.57.2.165
Sheikhzadeh, M., Zanjani, Z., and Baari, A. (2021). Efficacy of mindfulness-based cognitive therapy and cognitive behavioral therapy for anxiety, depression, and fatigue in cancer patients: a randomized clinical trial. Iran. J. Psychiatry 16:271. doi: 10.18502/ijps.v16i3.6252
Sun, J., Jiang, J., Wang, Y., Zhang, M., Dong, L., Li, K., et al. (2023). The efficacy of reminiscence therapy in Cancer-related symptom management: a systematic review and Meta-analysis. Integr. Cancer Ther. 22:15347354221147499. doi: 10.1177/15347354221147499
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. doi: 10.3322/caac.21660
Turkington, D., Kingdon, D., and Chadwick, P. (2003). Cognitive-behavioural therapy for schizophrenia: filling the therapeutic vacuum. Br. J. Psychiatry 183, 98–99. doi: 10.1192/bjp.183.2.98
van Weert, E., May, A. M., Korstjens, I., Post, W. J., van der Schans, C. P., van den Borne, B., et al. (2010). Cancer-related fatigue and rehabilitation: a randomized controlled multicenter trial comparing physical training combined with cognitive-behavioral therapy with physical training only and with no intervention. Phys. Ther. 90, 1413–1425. doi: 10.2522/ptj.20090212
Wells-Di Gregorio, S. M., Marks, D. R., DeCola, J., Peng, J., Probst, D., Zaleta, A., et al. (2019). Pilot randomized controlled trial of a symptom cluster intervention in advanced cancer. Psycho-Oncology 28, 76–84. doi: 10.1002/pon.4912
Xu, H., Cai, J., Sawhney, R., Jiang, S., Buys, N., and Sun, J. (2023). The effectiveness of cognitive-behavioral therapy in helping people on sick leave to return to work: a systematic review and Meta-analysis. J. Occup. Rehabil. 34, 4–36. doi: 10.1007/s10926-023-10116-4
Yennurajalingam, S., Konopleva, M., Carmack, C. L., Dinardo, C. D., Gaffney, M., Michener, H. K., et al. (2023). Treatment of Cancer-related-fatigue in acute hematological malignancies: results of a feasibility study of using cognitive behavioral therapy. J. Pain Symptom Manag. 65, e189–e197. doi: 10.1016/j.jpainsymman.2022.11.003
Zhang, L., Liu, X., Tong, F., Zou, R., Peng, W., Yang, H., et al. (2022). Cognitive behavioral therapy for anxiety and depression in cancer survivors: a meta-analysis. Sci. Rep. 12:21466. doi: 10.1038/s41598-022-25068-7
Keywords: cancer, CBT, cancer-related fatigue, cognitive behavioral therapy, CRF, fatigue
Citation: Hosseini Koukamari P, Karimy M, Ghaffari M and Milajerdi A (2025) Effect of cognitive-behavioral therapy on fatigue in cancer patients: a systematic review and meta-analysis. Front. Psychol. 15:1435110. doi: 10.3389/fpsyg.2024.1435110
Edited by:
Francesco Monaco, Azienda Sanitaria Locale Salerno, ItalyReviewed by:
Stefania Landi, ASL Salerno, ItalyStefania Palermo, Azienda Sanitaria Locale Salerno, Italy
Copyright © 2025 Hosseini Koukamari, Karimy, Ghaffari and Milajerdi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alireza Milajerdi, YW1raHZAeWFob28uY29t
 Parisa Hosseini Koukamari
Parisa Hosseini Koukamari Mahmood Karimy1
Mahmood Karimy1