- 1Institute of Medical Sociology, Interdisciplinary Center of Health Sciences, Medical Faculty, Martin-Luther-University Halle-Wittenberg, Halle (Saale), Germany
- 2Faculty of Applied Social Sciences, University of Applied Sciences Erfurt, Erfurt, Germany
- 3Institute for Social Medicine, Rehabilitation Sciences and Health Services Research, Nordhausen University of Applied Science, Nordhausen, Germany
- 4Department of Psychiatry, Psychotherapy, and Psychosomatics, University Hospital Halle, Halle (Saale), Germany
Sexual problems relevant to psychotherapy, such as compulsive sexual behavior (CSB) and sexual functioning problems (SFP), have been related to harmful substance use in several studies. Substance use is prevalent among medical students (MS) and is often considered a maladaptive coping strategy for stress, as well as a risk factor for mental health issues. Sexual problems and substance use share trauma exposure and post-traumatic symptoms as risk factors for their development. This study aimed to explore the interaction effects between problematic sexual behaviors, substance use, and trauma among German MS. A cross-sectional study (n = 359; 69% women, 29% men) was conducted using an online questionnaire. MS at a German university were recruited via email. CSB (CSBD-19), SFP (SBQ), harmful alcohol (AUDIT) and drug use (DAST), childhood trauma exposure (CTQ), and current post-traumatic symptoms (IES-R) were assessed. Multivariate linear and ordinal regressions, as well as path analyses, were conducted to investigate associations between the study variables. CSB was identified in 3% of all MS. The most commonly reported SFPs were decreased sexual desire and difficulties achieving orgasms among women and premature ejaculation among men. Higher CSBD scores were predicted by male sex, elevated AUDIT scores, and increased frequencies of hyperarousal (IES-R). Path analyses revealed associations between the severity of emotional/sexual abuse, the intensity of post-traumatic symptoms, and both CSBD and AUDIT scores. Among female MS, less severe emotional abuse and more severe physical abuse in childhood predicted higher frequencies of orgasmic difficulties. The frequency of SFPs was correlated with the use of benzodiazepines among female MS, with cannabis and MDMA/ecstasy among male MS, and with cocaine/crack, speed, and AUDIT among both sexes. No interaction effects were found between SFPs, substance use, or trauma-related factors in the path analyses. To some extent, there appears to be a relationship between substance use, childhood trauma exposure, and currently persisting post-traumatic symptoms with problematic sexual behaviors among MS. However, further research is required to explore these relationships in greater depth and to identify the underlying pathways. Mental health support measures should incorporate the factors of sexuality, substance use, and trauma while also exploring their relationships with workload, career-related anxieties, and other curriculum-related factors.
1 Introduction
1.1 Background
This study aimed to explore the trilateral relationships between problematic sexual behaviors, namely compulsive sexual behavior (CSB) and sexual functioning problems (SFP), substance use, and trauma-related factors among medical students (MS) in Germany. While regular substance use can lead to the development of sexual problems due to its effect on the body, depending on the type of substance consumed, substance use may also serve as a coping mechanism to deal with CSB and SFP and related consequences (Jepsen et al., 2023). Although all these factors have been individually investigated among German MS in previous studies, to the best of our knowledge, no study has examined them simultaneously.
Sexuality plays a significant role in many individuals’ lives, making it unsurprising that problematic sexual behaviors can contribute to persistent mental health challenges. “Emerging adulthood” defines the life stage between youth and adulthood (Arnett, 2014; Wood et al., 2018). In this phase of life, a variety of career opportunities and identities are explored while young adults gain more independence and experience less social control. Emerging adulthood is also a crucial life stage in terms of the exploration of individual sexuality (Vasilenko, 2021). Those who decide to go to university usually leave their parental home and start a campus life where they can explore the new environment on their own (Wood et al., 2018). During this transitional period, most emerging adults engage in sexual activities, typically in their late 30s or early 30s (Vasilenko, 2021). However, greater independence and less control have the potential to encourage hazardous health behaviors (Stone et al., 2012). This article focuses on two hazardous health behaviors among MS, who are a vulnerable group prone to persistent mental stress: problematic sexual behaviors and substance use. As we will learn later in this article, these two factors are strongly related to each other and can have a negative impact on wellbeing in general but also on MS.
1.1.1 Problematic sexual behaviors
To further explore the link between problematic sexual behaviors and substance use, it is crucial to define when sexual behavior is considered problematic from a psychotherapeutic perspective. According to the current state of research, two dimensions of problematic sexual behaviors—compulsive sexual behavior (CSB) and sexual functioning problems (SFP)—seem to be relevant in research addressing harmful substance use behaviors.
CSB is defined by an extraordinarily high level of sexual activity and arousal, paired with the loss of control of sexual behaviors, resulting in psychological strain and functioning problems in important areas of life. It is characterized by behaviors such as excessive pornography consumption, masturbation, or sex dating (Grubbs et al., 2020). Conversely, SFP is defined as impaired or absent sexual desire, arousal, and activity, leading to clinically significant distress (World Health Organisation (WHO), 2024). There are various forms of SFP, including hypoactive sexual desire and impaired sexual arousal, solely to women’s problems with achieving orgasm and pain during sexual activity and solely to men’s erectile dysfunction and premature and delayed ejaculation (Briken et al., 2020; Jepsen et al., 2023). It is important to emphasize that fluctuations in the intensity of sexual arousal and frequency of sexual activity are normal. However, CSB and SFP are patterns that develop over time, with distress and loss of control being core characteristics that render them problematic from a psychotherapeutic standpoint.
Research on problematic sexual behaviors, such as CSB or SFP, among MS or physicians is scarce. Previous studies found SFP among 40–60% of female MS (Wallwiener et al., 2017; Shindel et al., 2008). In a study by Shindel et al. (2008), approximately 30% of male MS report erectile dysfunction and problems controlling ejaculation. No additional studies were found that focused on the SFP, and no study at all was identified that investigated CSB among MS.
1.1.2 Substance use and sexual behavior
1.1.2.1 General relationships between problematic sexual behaviors and substance use
Regular consumption of alcohol and illegal drugs is often associated with negative health outcomes, and sexual problems have received close attention in recent years (Jepsen et al., 2023). Substances such as alcohol, cannabis, and amphetamines can increase sexual arousal and activity in the short term, while more frequent or long-term use of psychotropic substances is associated with the development of SFPs (Jepsen et al., 2023; Krüger, 2020). In particular, the risky use of substances such as alcohol, cannabis, and cocaine has been associated with CSB (Ballester-Arnal et al., 2020; Jepsen et al., 2024). Harmful alcohol consumption is associated especially with vaginal pain during penetration and the absence of vaginal lubrication among women (Grover et al., 2014) and erectile dysfunction, premature ejaculation, and reduced sexual desire among men (Grover et al., 2014; Prabhakaran et al., 2018; Rohilla et al., 2020). Also, the regular use of other psychotropic substances, such as opioids, cocaine, cannabis, and methamphetamines, seems to be related to similar SFP (Grover et al., 2014; Diehl et al., 2016; Yee et al., 2016; Dolatshahi et al., 2016). In summary, risky or harmful substance use can have both excitatory effects, such as CSB, and inhibitory effects, such as SFP, on sexual behavior (Krüger, 2020). In this context, substances can be used to cope with problematic sexual behaviors that lead to impairments in important areas of life. Inversely, CSB can also arise as a coping mechanism for dealing with the consequences of problematic substance use in important areas of life. A third possibility is the development of SFP due to the physiological effects of regular or problematic substance use, which vary depending on the substance consumed (Hallinan, 2021; Jepsen et al., 2023; Palha and Esteves, 2008).
1.1.2.2 Substance use among medical students and its relation to problematic sexual behaviors
Previous research has thoroughly examined the substance use behavior of MS and its associations with psychosocial risk factors. Most MS report alcohol consumption in the past year, while information about the prevalence of risky or harmful alcohol use varies between 9 and 34% (Bryl et al., 2020; Wang et al., 2023; Ayala et al., 2017; Voigt et al., 2009). Studies on licit and illicit substance use among German MS are rare and inconsistent in terms of investigated drugs and measurement approaches. Hoff et al. (2023) investigated inter alia the use of cannabis and alcohol among students in Germany across various fields of study. Approximately 40% of all students reported risky alcohol consumption, while MS showed a similar proportion compared to students in other fields. Cannabis was consumed by 11% of the total sample of students, whereas MS showed the lowest consumption proportion (8.3%). A sex effect was observed for cannabis consumption (and not for alcohol), with female students reporting lower consumption rates.
Various studies have revealed that alcohol, tobacco, and cannabis are the most commonly consumed substances among MS (Ayala et al., 2017; Roncero et al., 2015; Candido et al., 2018; Gupta et al., 2022). Substance use is more prevalent among male MS than among females, especially concerning alcohol and cannabis (Ayala et al., 2017; Voigt et al., 2009; Hoff et al., 2023; Roncero et al., 2015; Wilson et al., 2022). Further studies have identified a relationship between MS substance use and negative psychosocial and health-related outcomes. Hence, tranquilizer use appears to be linked to suicidal ideation (Keuch et al., 2023) and depressive symptoms (Pukas et al., 2022) among MS. Moreover, several studies suggest that physicians are a vulnerable group to developing substance use disorders (Beschoner et al., 2019), while it can be assumed that they use alcohol and drug abuse as maladaptive coping strategies to deal with occupational distress (Medisauskaite and Kamau, 2019; Vijendren et al., 2015). At the same time, the psychological distress level of MS is consistently higher than that of the general population (Dyrbye et al., 2006), which suggests a higher risk of implementing problematic substance use patterns as coping mechanisms.
In a study by Wallwiener et al. (2017), an association was found between alcohol consumption and the intensity of female sexual dysfunction in a sample of MS. No other study has examined the relationship between SFP and substance use among MS. To the best of our knowledge, no research investigated the relationship between CSB and substance use among MS. However, MS and physicians comprise vulnerable groups for developing harmful substance use patterns and their resulting psychosocial consequences (Dyrbye et al., 2006). Thus, it seems beneficial to explore associations with problematic sexual behavior as potential risk factors for developing and maintaining harmful substance use patterns.
1.1.3 Trauma exposure and post-traumatic stress are common risk factors
Traumatic experiences comprise an often-identified risk factor for CSB (von Franqué and Briken, 2018), SFP (Lalchandani et al., 2020; Sack and Büttner, 2014), and substance abuse and disorders (Moustafa et al., 2021; Pace et al., 2022). It is essential to consider these factors while exploring the relationship between problematic sexual behaviors and substance use. Childhood maltreatment by primary attachment figures, including emotional, physical, and sexual abuse, as well as emotional and physical neglect, can lead to various psychosocial and health-related consequences (Gilbert et al., 2009), including post-traumatic symptoms. According to ICD-11 PTSD is characterized by three primary symptoms: intrusions (e.g., flashbacks or nightmares), avoidance (e.g., steering clear of activities or situations that trigger traumatic memories), and hyperarousal (a persistent sense of threat, leading to hypervigilance and related symptoms) (World Health Organisation (WHO), 2024).
The few studies that have examined childhood trauma exposure (CTE) among MS vary regarding identified prevalence and measures used. According to a systematic review by King et al. (2017), the prevalence of physical abuse is 5 to 65%. Emotional trauma is approximately 4%, sexual abuse is 3 to 13%, and general trauma is 13% among MS. In a study by Ignatova et al. (2022), most reported general trauma exposures of MS were witnessing violence, family mental illness, serious personal injuries, or illness of a parent or friend, while at least one type of general trauma was reported by around 80%. In the same study, correlations between CTE among MS and depression, anxiety, and compulsive symptoms were found, as well as with alexithymia and subjective lower quality of life (Ignatova et al., 2022). Furthermore, a higher risk of burnout is considered a suspected negative health outcome related to trauma exposure among MS (Sciolla et al., 2019). Because of the psychosocial consequences that CTE can have on individuals in general, as well as MS specifically, it is important to consider CTE in investigating the relationships between problematic sexual behaviors and substance use.
1.2 Objectives
Considering the current state of research, data on problematic sexual behaviors such as CSB and SFP, as well as related factors concerning mental health among MS, are scarce. Notably, several studies investigated substance use among MS, few explored SFP and CTE, and none focused on CSB among MS in Germany or in general. Further, to the best of our knowledge, no study has addressed trilateral associations between problematic sexual behavior, substance use, and CTE. This study aims to fill these research gaps by focusing on the following objectives:
1. Providing a first overview of frequencies of CSB and SFP among MS.
2. Identifying predictors of CSB and SFP among MS related to substance use and trauma.
3. Investigating the interaction effects between CSB, SFP, substance use, and trauma-related factors.
2 Materials and methods
2.1 Study design and procedure
Data were collected online through a cross-sectional explorative study between May and December 2023. The questionnaire was developed using the software RedCap (Research Electronic Data Caption). The survey was conducted among MS at a mid-sized university in Germany. Students were invited to participate voluntarily by their lecturers during courses and through email, with all data collected anonymously. The study was conducted in accordance with the Declaration of Helsinki (World Medical Association (WMA), 2022).
2.2 Measures
2.2.1 Compulsive sexual behavior and sexual functioning problems
CSB was measured via the German version of the Compulsive Sexual Behavior Scale (CSBD-19) (Bőthe et al., 2020), which includes 19 five-pointed ordinal-scaled items (answer options between 1 = not agree at all and 4 = totally agree) based on the ICD-11 diagnosis of compulsive sexual behavior disorder (CSBD). The scale consists of five subscales (control, salience, relapse, dissatisfaction, and negative consequences). The cut-off value of the sum score is ≥50, indicating a prevalent CSBD (Bőthe et al., 2020). The internal consistency was excellent (Cronbach’s α = 0.926).
Indications for SFP were measured using the German version of the Sexual Behavior Questionnaire (SBQ-G) (Müller, 2016), originally invented by Macdonald et al. (2003). The scale includes four-pointed ordinal-scaled items addressing the frequency of occurring problems concerning desire for sex, capability for sexual arousal, capability for sexual enjoyment, satisfaction with sexual life, and orgasm within the last 3 months. It measures several facets of SFP via six items concerning sexual behavior applied to all sexes and five or six additional items regarding sex-specific behaviors. For women, items addressed orgasmic dysfunction and pain during penetration, and for men, erectile dysfunction, premature, and delayed ejaculation. Values of 0 and 1 on the respective ordinal-scaled items indicate SFP (Müller, 2016).
2.2.2 Substance use
The German version of the Alcohol Use Disorder Identification Test (AUDIT) was used to measure alcohol consumption habits via three subscales (alcohol consumption, dependence, and alcohol-related consequences), consisting of 3- to 5-pointed Likert-scaled items. Depending on the calculated sum score, alcohol use habits can be classified as abstinence/low-risk use (values from 0 to 7), risky use (values from 8 to 15), harmful use (values from 16 to 19), and chronic alcoholism (values from 20 to 40) (Babor and Robaina, 2016). The internal consistency was good (Cronbach’s α = 0.803).
Moreover, the participants were asked which illegal drugs they use/have used and how regularly. The Drug Abuse Screening Test (DAST-10), consisting of ten dichotomous items (answer options 0 = no and 1 = yes), was used to identify problematic consumption of illegal drugs within the past 12 months. Based on the determined sum scores, drug use can be classified as low/moderate (values from 1 to 5), substantial (values from 6 to 8), and severe level (values from 9 to 10) (National Institute on Drug Abuse, 2014; Yudko et al., 2007). The scale was translated into German via forward-backward translation (Acquadro et al., 2008) since no German version of the DAST currently exists. The internal consistency of the DAST was good (Cronbach’s α = 0.883).
The consumption frequencies of illicit drugs—including cannabis; amphetamines (MDMA/ecstasy, mephedrone, crystal meth, and Ritalin); hallucinogens (LSD, ketamine, other hallucinogens such as mushrooms/mescaline); cocaine/crack; opiates/opioids (heroin, fentanyl, and methadone), tranquilizers (barbiturates, benzodiazepines, and z-substances); and other illicit substances—were measured using eight-point ordinal scale items, with response options ranging from 1 (never) to 8 (every day).
2.2.3 Trauma exposure and post-traumatic stress
The German version (Klinitzke et al., 2012) of the Childhood Trauma Questionnaire (CTQ) by Bernstein et al. (1994) was utilized to measure trauma exposure during childhood and adolescence. The inventory consists of 28 five-pointed ordinal-scaled items, divided into five subscales, measuring the severity of emotional abuse (Cronbach’s α = 0.846), physical abuse (Cronbach’s α = 0.774), sexual abuse (Cronbach’s α = 0.911), emotional neglect (Cronbach’s α = 0.893), and physical neglect (Cronbach’s α = 0.465) using sum scores, respectively.
To assess currently occurring symptoms related to post-traumatic stress, the Impact of Event Scale (revised; IES-R) by Weiss and Marmar (1996) was used. It consists of 22 four-pointed ordinal items and three subscales, measuring the frequencies of currently occurring post-traumatic symptoms: intrusions (Cronbach’s α = 0.930), avoidance (Cronbach’s α = 0.923), and hyperarousal (Cronbach’s α = 0.892) with sum scores, respectively. In addition, the total IES-R score (Cronbach’s α = 0.962) was used for the data analyses.
2.2.4 Control variables
Participants were asked which semester they were currently studying. Sociodemographic information was collected, including age, sex, gender identity, size of current place of residence, marital status, religious affiliation, highest educational degree, and occupational status. Data on somatic and psychiatric conditions, medications, and relevant medical histories of family members and other important persons of participants were collected, as compulsive sexual behavior or sexual functioning problems may be related to other health-related factors beyond substance use.
2.2.5 Data analyses
Data analysis was conducted using SPSS version 28 and R. Mean value comparisons by sex were calculated using t-tests for independent samples (for the metric scales: AUDIT, DAST, CSBD, CTQ subscales, and IES-R subscales) and U-tests (for all SBQ items), which were ordinal-scaled.
T-tests were conducted if the variables’ kurtosis and skewness levels fell within the acceptable ranges of −/+ 7 for kurtosis and −/+2 for skewness, indicating normal distribution (Hair et al., 2010). Kurtosis and skewness for all subscales can be found in Supplementary Table S1. Levene’s test was used to prove the homogeneity of variances.
In the first step, correlations and Cramer’s V (CV) were calculated for all relevant variables. Stepwise multiple regression was conducted, with the CSBD score as a dependent variable and all other (control) variables that showed significant correlations with the CSBD score. AUDIT, DAST, substance consumption frequency, CTQ-, and IES-R subscales were included in the first block of the stepwise regression, and control variables were added in the second block. Normal distribution of the residuals was tested using the Breusch-Pagan test to see if the residuals were normally distributed. If this was not the case, the White test was applied accordingly. Variance inflation factors (VIF) were used to check for multicollinearity, which was assumed for values of >10 (Marcoulides and Raykov, 2019). Ordinal regression models were calculated with every investigated occurrence frequency of SFP (SBQ) as the respective dependent variable and the same potential predictors.
To better interpret the results of correlation and regression analyses, a path analysis with maximum-likelihood estimation was conducted using R Studio, incorporating CTQ subscales (Z1), IES-R subscales (Z2), substance use (Z 3 ), and CSBD scores/frequencies of SFPs (Z4 Model fit was evaluated using chi-square), root mean square error of approximation (RMSEA), and comparative fit index (Backhaus et al., 2016; Kenny et al., 2015). Given that sample size and degrees of freedom can influence the performance of RMSEA, we examined its 90% confidence interval according to the recommendations of Kenny et al. (2015). For RMSEA, values below 0.08 are deemed acceptable (Browne and Cudeck, 1993; Kenny et al., 2015; MacCallum et al., 1996), while CFI values above 0.90 indicate a good fit (Backhaus et al., 2016).
3 Results
3.1 Descriptive results
3.1.1 Sociodemographic information and health status
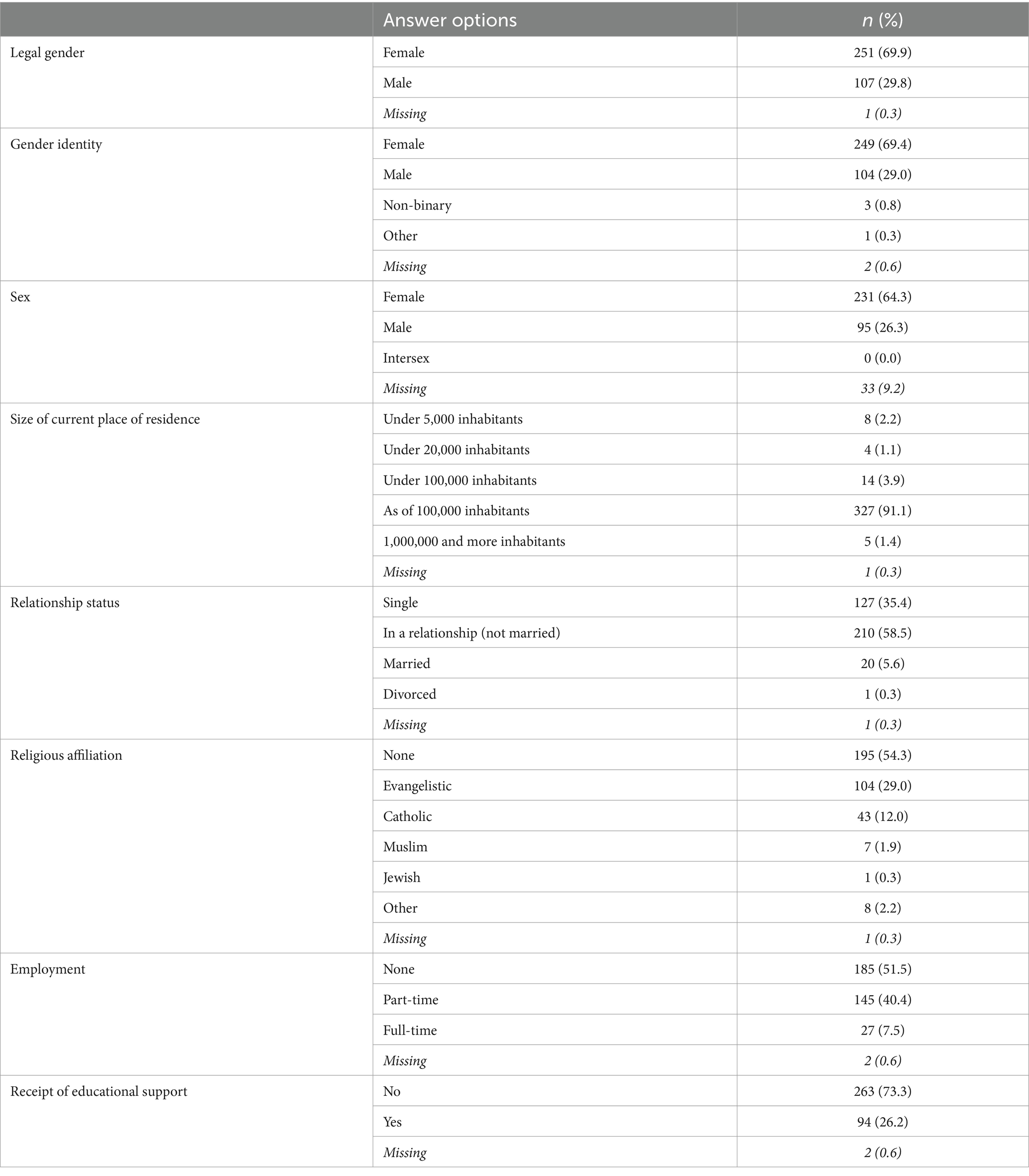
The survey was started by n = 445 MS, but after data cleaning and removing all cases of people who did not answer the items about problematic sexual behaviors, the final sample size was reduced to n = 359. Most participants were in their third semester (32.0%, n = 115), followed by the ninth (23.1%, n = 83) and fifth semester (21.2%, n = 76). The average age was M = 23.6 (SD = 3.4). Female gender identity was reported by 69.4% (n = 249), male gender identity by 29.0% (n = 104), non-binary by 0.8% (n = 3), and another not specified gender identity by 0.3% (n = 1). However, 64.3% (n = 231) stated female sex and 26.5% (n = 95) male sex. The gender distribution of the sample is roughly consistent with the current national comparison in Germany (64.4% female and 35.6% male) (Statistisches Bundesamt, 2024). Approximately one-fifth of the sample (21.7%, n = 78) reported somatic diseases (especially respiratory and dermatological diseases), and 18.4% (n = 66) stated a psychiatric disorder, with depression being the most frequently mentioned (n = 41). See Table 1 for the frequencies of all the measured socio-demographic information.
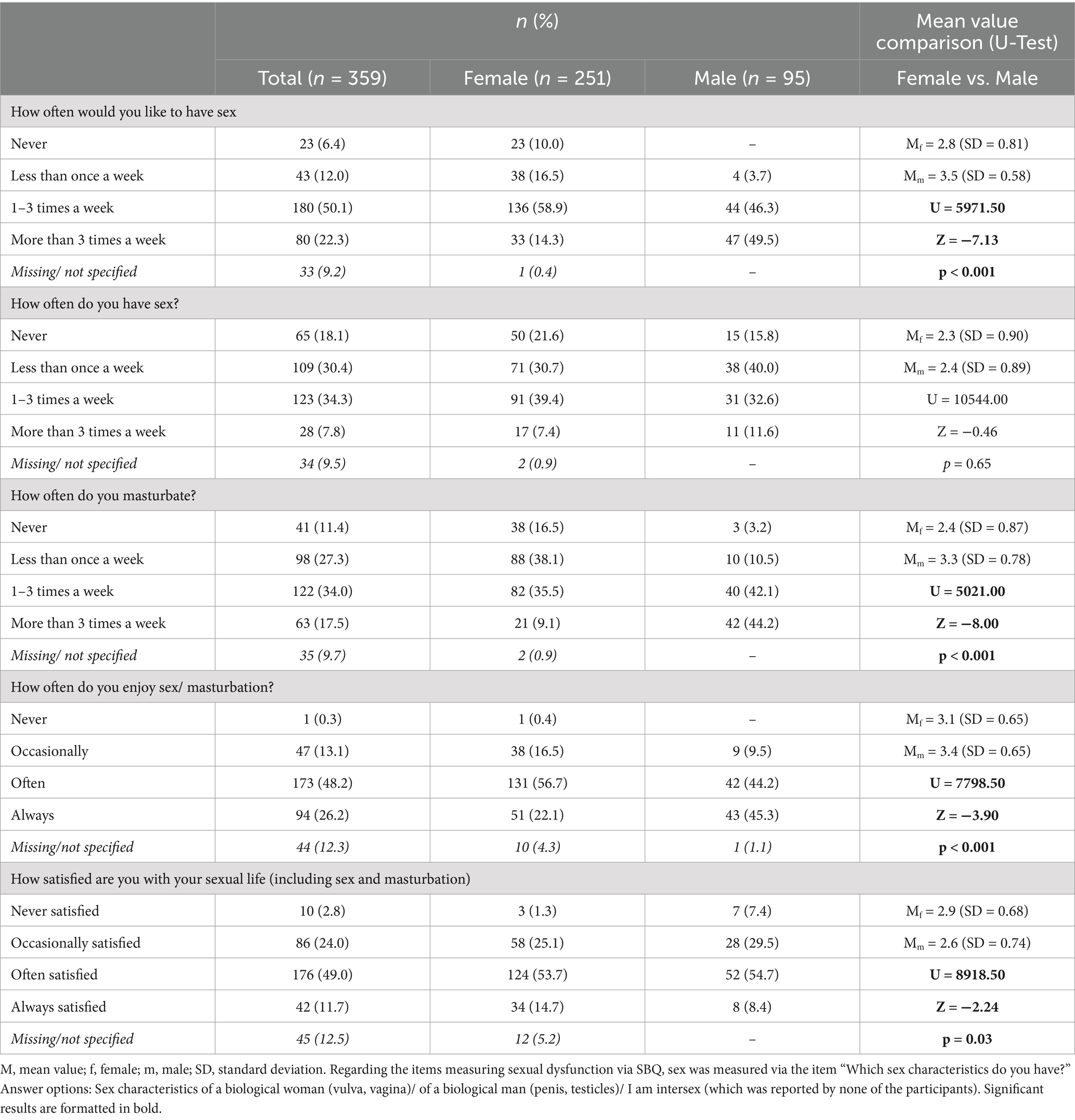
3.1.2 (Problematic) sexual behavior
The CSBD cut-off value of ≥50 was reached by 3.1% (n = 11, nfemale = 6, nmale = 5). The mean CSBD score was 25.6 (SD = 9.1). No significant mean value difference among CSBD scores by sex was found. As presented in Table 2, according to the U-test results, female participants reported slightly, yet significantly, lower frequencies of sexual desire, masturbation, and enjoyment of sex/masturbation than male participants. However, they also reported to be slightly more satisfied with their overall sex life. The most common SFP reported by men was premature ejaculation, affecting 22.2%. Conversely, the most frequent SFPs among female MS were sexual arousal and orgasmic problems, reported by 30.7 and 33.4%, respectively. The frequencies of all the investigated sexual functioning problems are shown in Figures 1, 2.
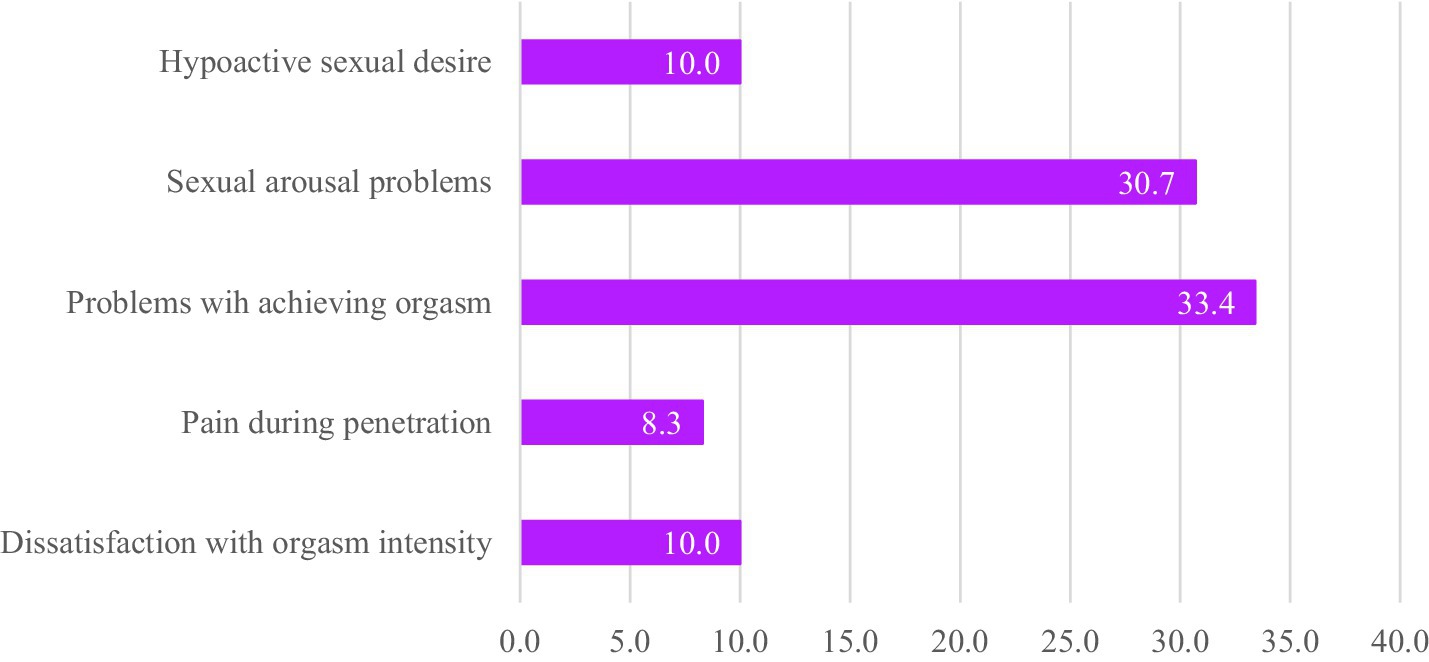
Figure 1. Frequency of sexual functioning problems among female medical students (%). Hypoactive desire was indicated if the answer option “I have no desire for sex” was chosen. Sexual arousal problems were indicated if the answer options “I never get aroused” or “I laboriously get aroused” were chosen. Problems with achieving orgasm were indicated if the answer options “I never have an orgasm” or “I occasionally have an orgasm” were chosen. Pain during penetration was indicated if the answer options “I always have pain” and “I often have pain” were chosen. Dissatisfaction with orgasm intensity was indicated if the answer options “I am not satisfied at all” or “I am somewhat satisfied” were chosen.
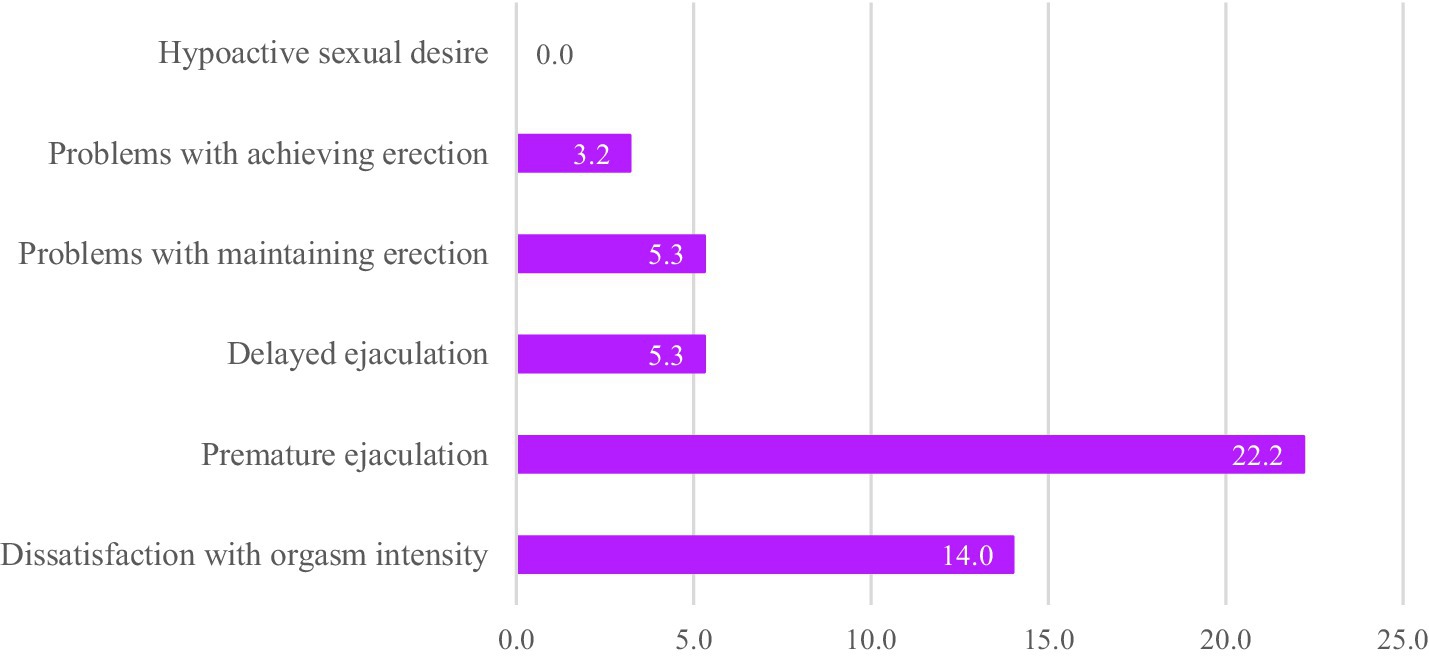
Figure 2. Frequency of sexual functioning problems among male medical students. Hypoactive desire was indicated if the answer option “I have no desire for sex” was chosen. Sexual arousal problems were indicated if the answer options “I never get aroused” or “I laboriously get aroused” were chosen. Problems with achieving erection were indicated if the answer options “I never get an erection” or “I occasionally get an erection” were chosen. Problems with maintaining erection were indicated if the answer options “I am never able to maintain an erection” I am occasionally able to maintain an erection” were chosen. Delayed ejaculation was indicated if the answer options “My ejaculation is always delayed” and “My ejaculation is often delayed” were chosen. Premature ejaculation was indicated if the answer options I always cum too early” and “I often cum too early” were chosen. Dissatisfaction with orgasm was indicated if the answer options “I am not satisfied at all” or “I am somewhat satisfied” were chosen.
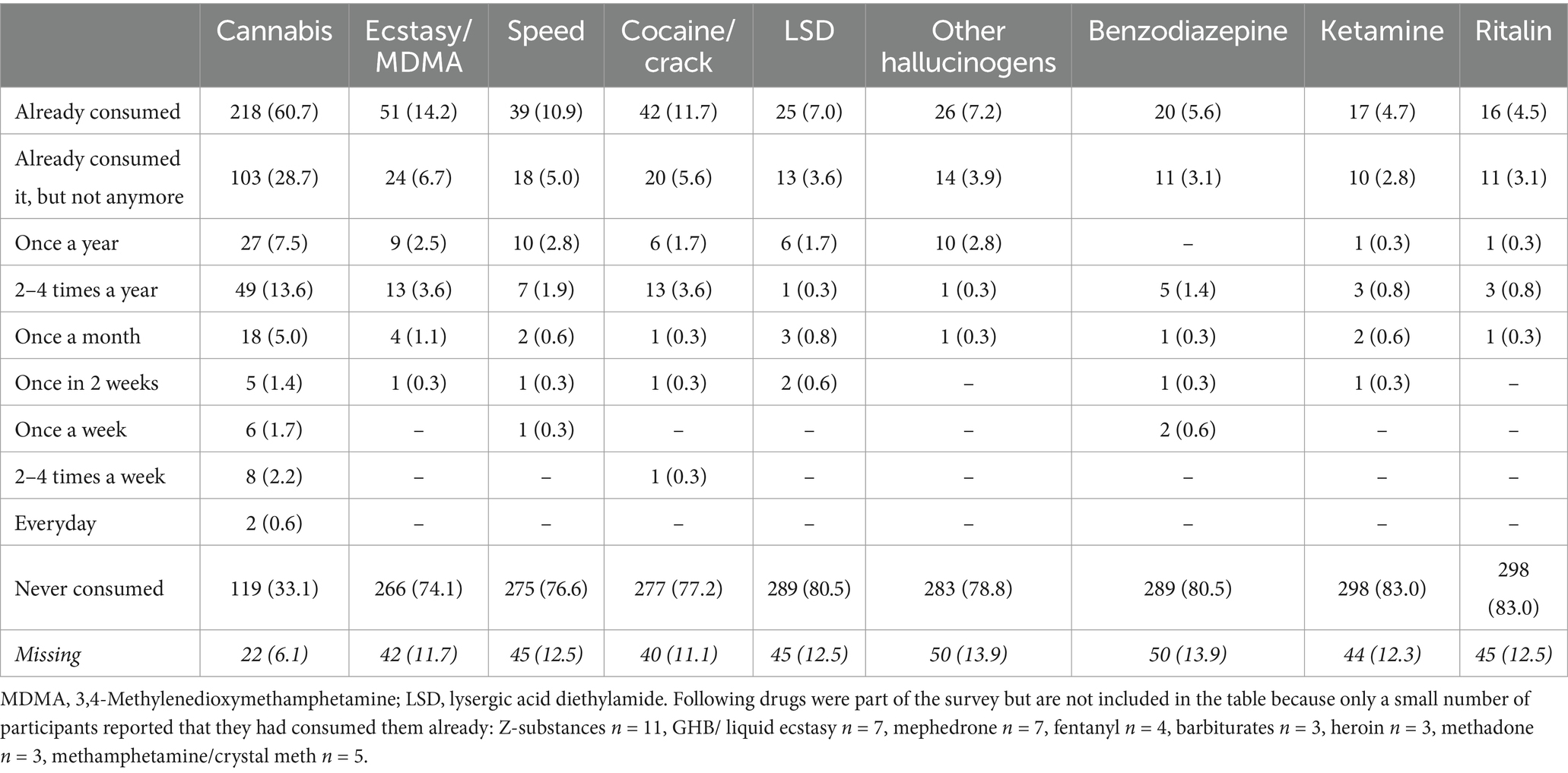
3.1.3 Substance use
According to the AUDIT score, alcohol consumption was classified as unproblematic by most of the participants (66.0%, n = 237, nfemale = 185, nmale = 52). An indication of a harmful consumption pattern was identified in 30.4% (n = 109, nfemale = 55, nmale = 54), while 6.4% (n = 23, nfemale = 12, nmale = 11) reached a critical value, indicating a requirement for professional consultation with great probability. A significantly higher AUDIT Score was identified among male MS (M = 7.9, SD = 4.8) compared to female MS (M = 5.5, SD = 4.3), t(344) = −4.72, p < 0.001, d = 0.53 (equal variances assumed, Levene’s test p = 0.06).
Regarding DAST score, an indication for harmful drug consumption was identified in 4.2% (n = 15, nfemale = 10, nmale = 5) of the sample, whereas among 53.8% (n = 193, nfemale = 119, nmale = 74), drug use could be determined as unproblematic (included were all participants who stated they used drugs at least once in their lifetime). The mean value comparison of the DAST score by gender identity showed insignificant results, t(206) = −0.55, p = 0.58. The consumption frequencies of all the investigated substances are presented in Table 3. Cannabis was the most consumed illicit drug within the sample, followed by ecstasy/MDMA, speed, and cocaine/crack. Male MS used cannabis (CV = 0.31, p = 0.01) more often than female MS, and no other sex differences were found concerning the frequency of illegal drug consumption. A significant relationship was found between indications of harmful alcohol consumption and drug use (CV = 0.25, p < 0.001).
3.1.4 Childhood trauma exposure and post-traumatic symptoms
The frequencies of traumatic exposure in the sample stratified by sex are presented in Figure 3. The severity of emotional abuse was significantly higher for female MS (t(316) = 2.10, p = 0.04, d = 0.26) than for male MS, with a small effect size (equal variances assumed, Levene’s test p = 0.13). No other significant mean value comparisons were observed. No sex differences were found in the severity of currently occurring post-traumatic symptoms.
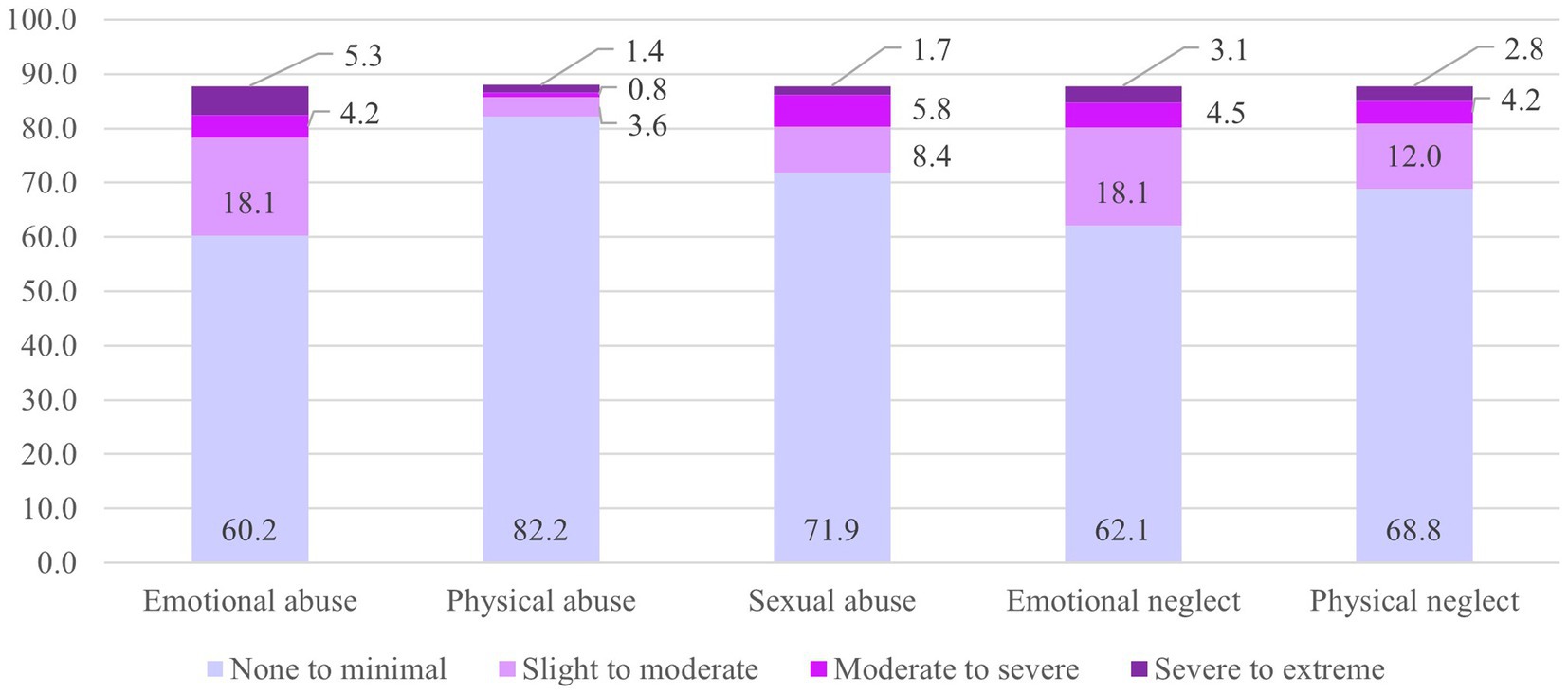
Figure 3. Severity of childhood trauma exposure (%). CTQ, Childhood trauma questionnaire; f, female; m, male. SD, standard deviation. Regarding the items measuring sexual dysfunction via SBQ, sex was measured via the item “Which sex characteristics do you have?” Answer options: Sex characteristics of a biological woman (vulva, vagina)/ of a biological man (penis, testicles)/ I am intersex (which was reported by none of the participants).
3.2 Correlative results with problematic sexual behaviors as dependent variables
Tables 4, 5 show the correlations of CSBD score/SBQ subscale scores and variables measuring facets of substance use, trauma exposition, and current post-traumatic stress symptoms.
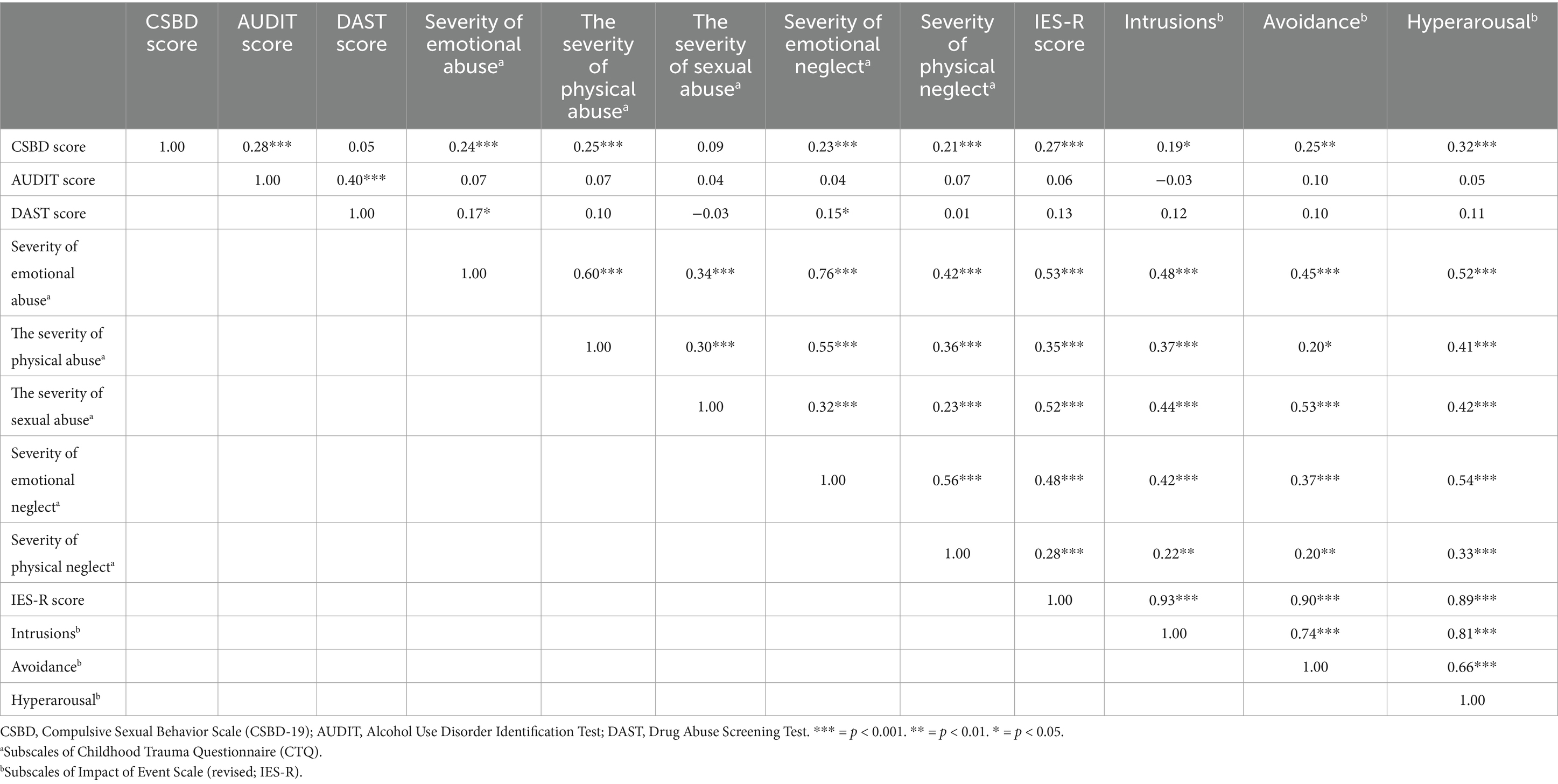
Table 4. Correlationships between compulsive sexual behavior score and independent variables (Pearson’s product–moment coefficient, r).
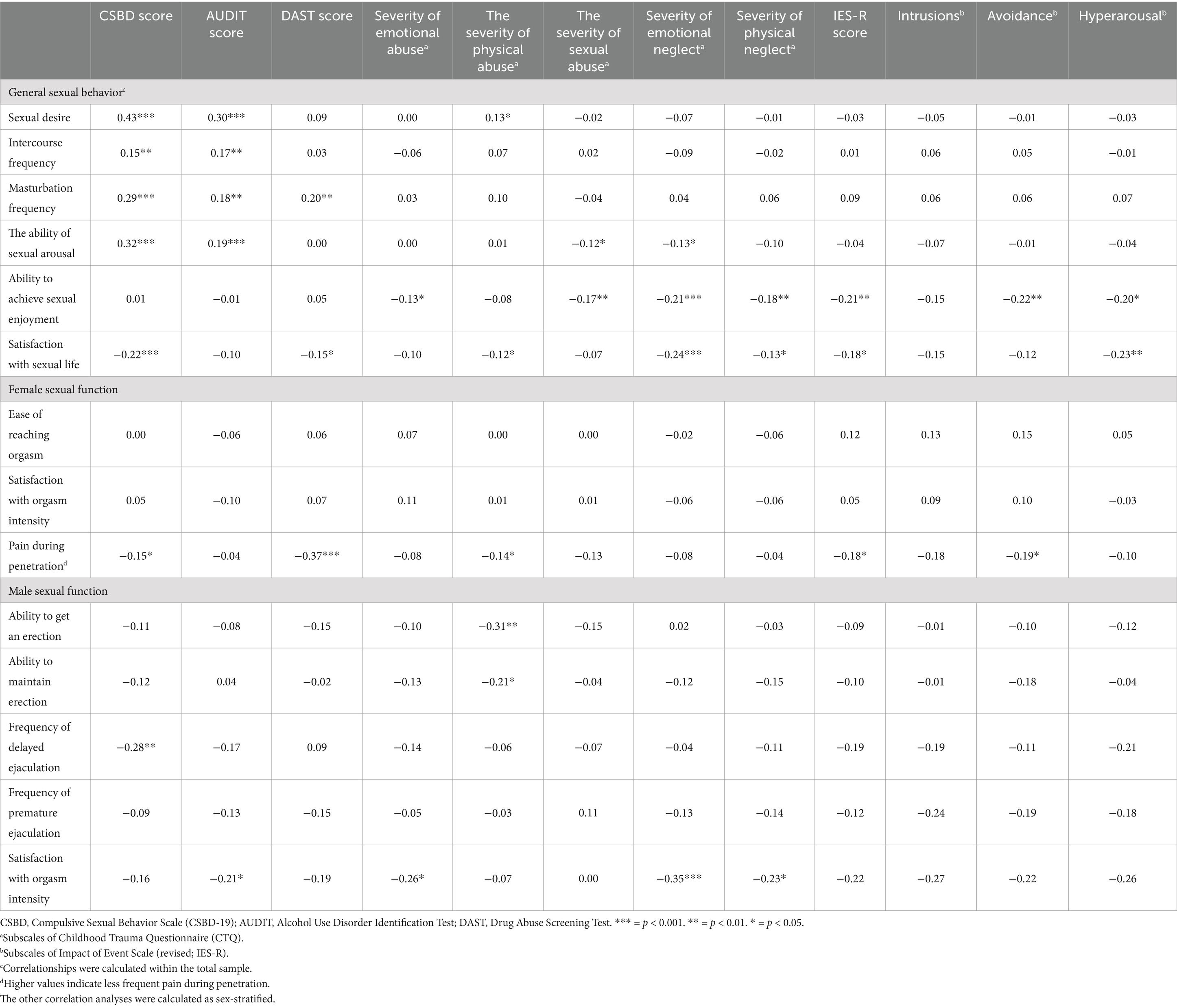
Table 5. Correlationships between sexual behavior/dysfunction and independent variables (Spearman’s rank correlation coefficient, r).
3.2.1 Correlations between problematic sexual behaviors and substance use frequency
No significant correlations were found between the CSBD score and the consumption frequencies of alcohol and illicit drugs.
Among female MS, the frequency of sexual desire correlated with alcohol consumption frequency (r = 0.22, p < 0.001). The frequency of sexual activity was related to the frequency of consumption of hallucinogenic substances (except LSD; r = 0.72, p = 0.01). Masturbation frequency was negatively correlated with ketamine (r = −0.76, p = 0.05), and speed (r = −0.50, p = 0.04) consumption frequency. The frequencies of benzodiazepine use (r = −0.88, p < 0.001) and cocaine/crack use (r = −0.50, p = 0.03) were associated with a decreased ability to enjoy orgasm. Additionally, a higher frequency of speed consumption was associated with decreased ability to become sexually aroused (r = −0.60, p = 0.01) and reach orgasm (r = −0.49, p = 0.05), as well as decreased satisfaction with the intensity of orgasm (r = −0.58, p = 0.02). The frequency of pain during sexual activity was related to a higher frequency of crack use (r = 0.65, p < 0.001).
Among male MS, significant correlations were found between substance use and sexual functioning problems. No associations were identified between sexual function problems and the frequency of alcohol consumption or DAST. A decreased ability to experience sexual arousal was related to the frequency of cannabis consumption (r = −0.25, p = 0.03). Cocaine/crack use frequency correlated with masturbation frequency (r = 0.46, p = 0.05). LSD use frequency was found to be negatively correlated with the ability to achieve erection (r = −0.69, p = 0.01), while cannabis use frequency was found to be negatively correlated with the ability to maintain erection (r = −0.33, p = 0.01).
Regarding trauma-related factors, associations were identified between the severity of emotional neglect and decreased satisfaction with sexual life (r = −0.22, p < 0.001). The frequency of pain during sexual activity was associated with the frequency of currently occurring intrusions (r = 0.24, p = 0.01) and avoidance (r = 0.21, p = 0.02). The frequency of currently occurring hyperarousal and decreased satisfaction with sexual life (r = −0.25, p < 0.001) and ability to enjoy sexual activity (r = −0.25, p < 0.01).
A decreased ability to enjoy sexual activity was correlated with the severity of emotional abuse (r = −0.23, p = 0.03) and neglect (r = −0.26, p = 0.01). Additionally, the severity of emotional neglect was further associated with decreased satisfaction with sexual life (r = −0.28, p = 0.01), ability to maintain erections (r = −0.23, p = 0.03), and decreased satisfaction with orgasm intensity (r = −0.36, p < 0.001). Another correlation was identified between the severity of physical neglect and a decrease in satisfaction with orgasm intensity (r = −0.24, p = 0.02). A decreased satisfaction with sexual life was related to the frequency of occurring intrusions (r = −0.35, p = 0.02) and hyperarousal (r = −0.37, p = 0.01). Furthermore, a decreased ability to enjoy sexual activity was related to the frequency of occurring avoidance (r = −0.36, p = 0.02).
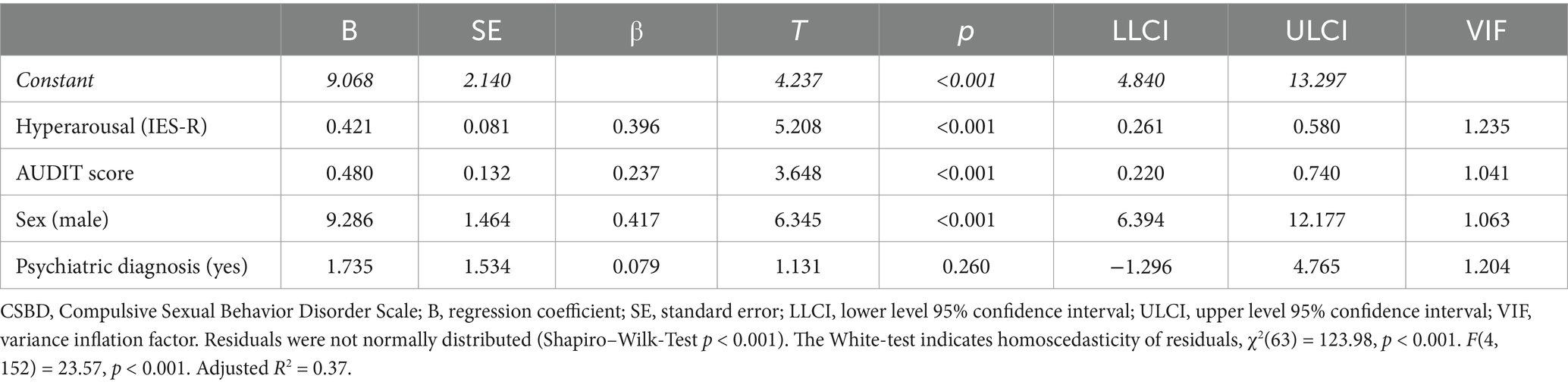
3.3 Prediction of compulsive sexual behavior
3.3.1 Results of stepwise linear regression
The results of stepwise linear regression are presented in Table 6. Male sex, higher AUDIT scores, and frequency of currently occurring hyperarousal were significant predictors of higher CSBD scores. No significant moderation effects were found, indicating a potential interaction effect of the IES-R subscales on the relationship between AUDIT-/DAST- and CSBD scores.
3.3.2 Results of path analysis
The results of the confirmatory path analysis can be found in the Supplementary Table S2. Since DAST was not correlated or identified as a significant predictor of CSBD score, path analyses were only conducted, including the AUDIT score. In the first step of the model specification, the insignificant paths were excluded. The final path model with standardized path coefficients (?) is illustrated in Figure 4. Indices indicate a good model fit, χ2(4) = 1.34, p = 0.86. RMSEA = 0.00, 90% CI [0.00; 0.04]. CFI = 1.00.

Figure 4. The final model of path analysis compulsive sexual behavior and alcohol use (N = 358). CSBD, Compulsive Sexual Behavior Scale; AUDIT, Alcohol Use Disorder Identification Test; e, residual. *** = p < 0.001. ** = p < 0.01. * = p < 0.05. Model fit: χ2(4) = 1.34, p = 0.86. RMSEA = 0.00, 90% CI [0.00; 0.04]. CFI = 1.00.
3.4 Prediction of sexual functioning problems
The results of all ordinal regression models with types of sexual functioning problems as dependent variables can be found in the Supplementary material.
3.4.1 Prediction of sexual functioning problems among female medical students
Among female MS, the following significant predictors of higher frequencies in SFP were identified via ordinal regression models: lower values in the severity of emotional abuse as a predictor of higher frequencies in problems with achieving orgasm (B = −0.21, p = 0.03, R2 = 0.23) and orgasm intensity (B = −0.36, p = 0.00, R2 = 0.29). Childhood physical abuse severity predicted a higher frequency of problems with orgasm intensity (B = 0.37, p = 0.04, R2 = 0.29). As the Nagelkerke’s R2 value was not within an acceptable range, the ordinal regression models of pain during sex (R2 = 0.19) among female MS could not be considered. See the results of all the calculated models with female sexual functioning problems as dependent variables in the Supplementary material. As AUDIT and DAST were not identified as significant predictors of SFP, no path analyses were calculated.
3.4.2 Prediction of sexual functioning problems among male MS
None of the ordinal regression models examining the sexual functioning problems of male MS as a dependent variable were significant (see the results in the Supplementary material). Since no maximum likelihood estimation could be calculated for the models with the frequency of problems with getting and maintaining an erection as a dependent variable, the goodness-of-fit measure is not sufficiently reliable. Harmful alcohol/drug use was not found to be a predicting variable for any of the investigated SFPs. Thus, no path analyses were conducted to examine these relations.
4 Discussion
4.1 Summary of results
The objectives of this study were to (1) provide a first overview of the frequencies of CSB and SFP among MS, (2) identify predictors of CSB and SFP among MS related to substance use and trauma-related factors, and (3) investigate the interaction effects between CSB/SFP, substance use, and trauma-related factors.
One-third of female MS reported a decreased sexual desire and problems with achieving orgasm. A higher frequency of premature ejaculation was reported by around a fifth of male MS. Other sexual functioning problems, as well as CSB, were rarely reported in the sample. More intense CSB was predicted by the harmfulness of alcohol use, the frequency of post-traumatic hyperarousal, and the male sex. Path analyses revealed significant effects of emotional and sexual abuse as well as emotional neglect on the intensity of currently occurring post-traumatic hyperarousal, which in turn affected the intensity of CSB, which conclusively covariates with the harmfulness of alcohol use. The model should not be rejected (considering the χ2-test and 90% CI of RMSEA, which suggests a good model fit), but however, considering RMSEA and CFI, it seems that with this data basis, the model is not able to evaluate the effects demonstrably. Possible reasons for that are the small effect sizes and sample size.
Among female MS, sexual function was negatively related to the frequency of cannabis, cocaine/crack, and speed use (however, the use frequencies of these substances were reported to be low in general), but also to the severity of emotional neglect and the intensity of currently occurring post-traumatic stress symptoms. Whereas lower levels of emotional abuse severity and higher levels of physical abuse severity predicted problems related to orgasm experience among female MS, no predictors of sexual functioning problems were identified among male MS. Thus, regression and correlation analyses could not provide a basis for conducting path analyses investigating the relationships between SFP, substance use, and trauma-related factors.
4.2 Implications
The cut-off value for compulsive sexual behavior, which indicates a high risk of having CSBD, was exceeded by 3.1% of MS, which is slightly lower than the general CSBD prevalence estimates for Germany (Briken et al., 2022) and worldwide (Bőthe et al., 2023). More intense CSB is predicted by the male sex (which is consistent with most studies on CSB among varying samples (Grubbs et al., 2020), harmful alcohol use, and current persisting hyperarousal as a post-traumatic stress reaction). The results of the path analyses suggest that the relationship between the intensity of currently occurring post-traumatic hyperarousal (significantly associated with the severity of emotional and sexual abuse) and the intensity of CSB is mediated by the harmfulness of alcohol use. Therefore, in combination with the results of regression calculations, MS who experienced more severe emotional trauma are at a higher risk of developing CSB as well as more harmful alcohol consumption. More research is essential to explore the interrelation between post-traumatic stress symptoms—especially hyperarousal—and CSB, while previous research indicates that CSB could be a strategy to cope with the occurring post-traumatic symptoms. Even though harmful alcohol use was associated with CSB in this study (and also consistent with Ballester-Arnal et al., 2020; Jepsen et al., 2024), no relation was found between the harmfulness of alcohol use and trauma-related factors. Thus, on the basis of this data, CSB appears to be predicted by post-traumatic stress independently from the harmfulness of alcohol use among MS.
The identified frequencies of SFPs among the male MS in this sample are roughly consistent with the results of current prevalence measurements of the same age group (age 18–25) (Briken et al., 2020). However, female MS in this study showed significantly higher frequencies of sexual arousal problems (30.7% vs. 16.8% in the comparative study) and lower frequencies of pain during sexual activity (8.3% vs. 16.2% in the comparative study) (Briken et al., 2020). Moreover, the frequencies of SFPs and childhood trauma exposure among MS in this study were significantly lower than those reported by Ignatova et al. (2022) and Shindel et al. (2008). The frequency of sexual (functioning) problems correlated with the consumption frequency of benzodiazepines among female MS, with cannabis and MDMA/ecstasy among male MS, and with cocaine/crack, speed, and AUDIT among both sexes.
Among female MS, less severe exposure to emotional abuse during childhood predicted higher frequencies of problems with achieving orgasm and orgasm intensity. These findings may seem surprising at first glance, as they contradict those of previous studies (Lutfey et al., 2008; Weiss et al., 2023). However, it should be considered that potential protection and resilience factors, such as, e.g., family cohesion, social support, high self-esteem, and low rumination (Fritz et al., 2018), were not examined. Thus, it remains unclear whether these associations are mediated or moderated by these factors. Moreover, there are diverse potential reasons for the impairment of the orgasmic experience. Our results indicate a difference in the frequency of experienced orgasm between male and female MS, which corresponds to the gender orgasm gap. This phenomenon describes a gap in orgasm frequency and quality between men and women (Döring and Mohseni, 2022). From a psychosocial perspective, power relationships dominate heterosexual intercourse, with penetrative sex and coitus at the center of heterosexual activities (Döring and Mohseni, 2022; Wade, 2016; Frith, 2013). According to Wade et al. (2005), “It [the gender orgasm gap] is […] strongly impacted by social forces that privilege men’s pleasure over women’s, an ignorance about the clitoris, a prioritization of men’s pleasure, the gendered sexy/sexual binary, and a coital imperative.” This gap also extends to the operationalization of measuring female orgasms. When examining the items of the Sexual Behavior Questionnaire (SBQ), it is difficult to believe that it adequately represents the embodied experience of female orgasm (Frith, 2013; Jannini et al., 2012). There is a need to incorporate the results and further research of qualitative feminist scholars (Frith, 2013) into a methodological-mixed research design to develop an improved method of measurement. This also implies the need for female-led science in these topics to provide an appropriate representation.
The most frequently consumed substances among MS were alcohol, cannabis, and amphetamines (ecstasy/MDMA, speed). As in most cases, the consumption pattern of illegal drugs seems unremarkable from a therapeutic perspective. Approximately one-third of our sample showed indications of harmful alcohol use, which is consistent with the findings of most previous research (Hoff et al., 2023; Jackson et al., 2016; Gajda et al., 2021; Gignon et al., 2015). While interpreting the significant associations found between AUDIT and CSBD in this sample, it is important to consider that these relationships may be moderated or mediated by various mental health issues. Previous studies have shown that academic stress (Sheehama et al., 2022), exhaustion, and financial concerns (Jackson et al., 2016; Dahlin et al., 2011) are associated with higher AUDIT scores among MS. Respective effects may be expected concerning further individual factors such as age, gender, specialty, and career stage (Wilson et al., 2022). However, it is widely recognized that MS are at high risk of experiencing increased levels of stress, depression, and anxiety symptoms (Dyrbye et al., 2006). These symptoms are also commonly associated with CSB (Schultz et al., 2014; Ciocca et al., 2022; Walton et al., 2017; Reid et al., 2014) and SFP (Gonçalves et al., 2023; Hamilton and Julian, 2014; Velurajah et al., 2022). Previous research suggests that the presence of sexuality-related problems can be a risk factor for developing and maintaining harmful substance use, which is especially important to emphasize in this connection, as physicians are a vulnerable group for developing problematic substance use patterns and substance dependencies (Dyrbye et al., 2006). As consumption patterns manifest in substance use disorders over time, affected physicians report various barriers to seeking help for substance use disorders, such as fear of stigma, denial of the disease, psychiatric comorbidities, as well as expected negative familial, social, professional, and economic consequences (Vayr et al., 2019; Rogoža et al., 2021). Stigma towards mental health problems and their treatment remains a serious problem within the profession. Especially younger physicians report more barriers to seeking help for mental health problems than older physicians do, such as confidentiality or an anticipated negative impact on career progression (Wijeratne et al., 2021).
The most frequently reported forms of childhood trauma exposure were emotional neglect and abuse, while female MS showed significantly higher levels of emotional abuse severity compared to male MS. Additionally, a significantly higher prevalence of emotional abuse (27.6%) was identified in MS compared to the general German population (10.2 to 18.5%) (Glaesmer, 2016; Witt et al., 2017). However, the prevalence of all other investigated traumatic childhood experiences in this sample is highly similar compared to estimates in the general German population (Glaesmer, 2016; Witt et al., 2017).
This study suggests that substance use, childhood trauma exposure, and currently persistent post-traumatic symptoms may be associated with problematic sexual behaviors among MS to some extent. Notably, harmful alcohol use, emotional abuse during childhood, and, among female MS, sexual arousal problems and orgasmic dysfunction seem to occur frequently. Therefore, these factors should be considered in mental health support measures targeting medical students.
In this context, it is necessary to (1) identify the primary mental health issue that may trigger other mental health problems, (2) develop a tailored, individually adapted case plan for psychosocial care, and (3) connect and refer cases to relevant institutions for counseling and support concerning substance use, sexuality-related problems, and trauma.
Addressing mental health challenges among MS generally requires psychological support, as highlighted by various studies on this population (Gupta et al., 2022; Vayr et al., 2019). However, nearly half of MS experiencing mental health problems report unmet related needs for support (Gupta et al., 2022). Therefore, it is crucial to create accessible, low-threshold, and anonymous mental health support tailored to the needs of MS, as these are currently lacking in most universities and affiliated institutions.
The provision of psychosocial support measures is important, but it is not the only factor that needs to be implemented to improve the mental health of MS. Moreover, it is crucial to start programs that primarily focus on the reduction of career-related stigma and anxiety already during medical studies, as these factors are well-known to be important causes of mental health problems among MS and physicians (Vayr et al., 2019; Wijeratne et al., 2021). Furthermore, several studies have found that changes to the MS-adapted curriculum and workload are necessary to decrease mental stress among MS (Slavin et al., 2014; Jestin et al., 2023; Del Carmen et al., 2019), which would be beneficial in preventing the development of maladaptive coping strategies (such as substance abuse) and resulting mental health consequences (such as problematic sexual behaviors).
4.3 Limitations
When interpreting the results of this study, it is important to consider that the data were collected from a single institution using a cross-sectional design. Therefore, the main findings cannot be directly generalized to all MS. It is also worth noting that in Germany, cannabis was classified as an illegal drug only until April 2024.
All relevant constructs were measured using well-validated questionnaires (AUDIT, DAST, CSBD-19, CTQ, and IES-R). However, no validated questionnaire currently exists that measures clinically significant sexual functioning problems according to DSM or ICD diagnoses.
It is necessary to investigate additional factors to further explore the relationships between problematic sexual behaviors, substance use, and trauma exposure, as well as their respective developmental pathways. Further studies should consider factors such as workload, elements of the medical curriculum, additional sexuality-related aspects (e.g., sexual experiences with current sexual partner(s)), and burdens in the participants’ individual life situations. Despite these limitations, the results of this study provide an initial overview of problematic sexual behaviors among MS and their associations with substance use and trauma exposure.
5 Conclusion
CSB and most measured SFPs were relatively infrequent within this sample of MS. However, the study found that harmful alcohol use, emotional abuse during childhood, and, specifically, among female MS, sexual arousal problems, or orgasmic dysfunction were found quite frequently. Alcohol use and the intensity of current persistent post-traumatic hyperarousal appear to predict CSB among MS, while SFP appears mainly related to the use frequency of illicit drugs.
In particular, among women, dissatisfaction with orgasmic intensity was predicted by less severe emotional abuse but more severe physical abuse during childhood. However, further research is needed to explore in greater depth the pathways and interactions between problematic sexual behaviors, substance use, and trauma.
It is essential to incorporate factors such as sexuality, substance use, and trauma into mental health support measures while also exploring their relationships with workload, career-related stigma, anxieties, and other curriculum-related factors. MS with trauma exposure should be considered a vulnerable group at higher risk for problematic sexual behaviors and harmful alcohol consumption.
Data availability statement
The datasets presented in this article are not readily available because the participants were ensured that the collected information would be processed solely within the scope of the research project and not shared with third parties. Requests to access the datasets should be directed to ZGVubmlzLmplcHNlbkBtZWRpemluLnVuaS1oYWxsZS5kZQ==.
Ethics statement
The studies involving humans were approved by the Ethical committee of the medical faculty of Martin-Luther-University Halle-Wittenberg, Germany. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
DJ: Writing – review & editing, Writing – original draft, Visualization, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. TL: Writing – review & editing, Supervision, Conceptualization. CH: Writing – original draft. JN: Writing – original draft. KW: Writing – original draft. SW: Writing – review & editing, Supervision, Project administration, Conceptualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Open Access Publication Fund of the Martin Luther University Halle-Wittenberg.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1423690/full#supplementary-material
Abbreviations
AUDIT, Alcohol Use Disorder Identification Test; CSB, Compulsive sexual behavior; CSBD, Compulsive sexual behavior disorder; CTE, Childhood trauma exposure; CTQ, Childhood Trauma Questionnaire; DAST, Drug Abuse Screening Test; IES-R, Impact of Event Scale (revised); MS, Medical students; SBQ, Sexual Behavior Questionnaire; SFP, Sexual functioning problems.
References
Acquadro, C., Conway, K., Hareendran, A., and Aaronson, N. (2008). Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Health 11, 509–521. doi: 10.1111/J.1524-4733.2007.00292.X
Ayala, E. E., Roseman, D., Winseman, J. S., and Mason, H. R. C. (2017). Prevalence, perceptions, and consequences of substance use in medical students. Med. Educ. Online 22:1392824. doi: 10.1080/10872981.2017.1392824
Babor, T. F., and Robaina, K. (2016). The alcohol use disorders identification test (AUDIT): a review of graded severity algorithms and national adaptations. Int. J. Alcohol Drug Res. 5, 17–24. doi: 10.7895/Ijadr.V5i2.222
Backhaus, K., Erichson, B., Plinke, W., and Weiber, R. (2016). Multivariate Analysemethoden [methods of multivariate analysis]. Berlin, Heidelberg: Springer.
Ballester-Arnal, R., Castro-Calvo, J., Giménez-García, C., Gil-Juliá, B., and Gil-Llario, M. D. (2020). Psychiatric comorbidity in compulsive sexual behavior disorder (CSBD). Addict. Behav. 107:106384. doi: 10.1016/j.addbeh.2020.106384
Bernstein, D. P., Fink, L., Handelsman, L., and Foote, J. (1994). Childhood trauma questionnaire (CTQ) [database record]. Washington, DC: APA PsycTests.
Beschoner, P., Limbrecht-Ecklundt, K., and Jerg-Bretzke, L. (2019). Burnout, depression, anxiety and substance abuse in the occupational context. Nervenarzt 90, 961–974. doi: 10.1007/s00115-019-0739-x
Bőthe, B., Koós, M., Nagy, L., Kraus, S. W., Demetrovics, Z., Potenza, M. N., et al. (2023). Compulsive sexual behavior disorder in 42 countries: insights from the international sex survey and introduction of standardized assessment tools. J. Behav. Addict. 12, 393–407. doi: 10.1556/2006.2023.00028
Bőthe, B., Potenza, M. N., Griffiths, M. D., Kraus, S. W., Klein, V., Fuss, J., et al. (2020). The development of the compulsive sexual behavior disorder scale (CSBD-19): an ICD-11 based screening measure across three languages. J. Behav. Addict. 9, 247–258. doi: 10.1556/2006.2020.00034
Briken, P., Matthiesen, S., Pietras, L., Wiessner, C., Klein, V., Reed, G. M., et al. (2020). Estimating the prevalence of sexual dysfunction using the new ICD-11 guidelines. Dtsch. Arztebl. Int. 117, 653–658. doi: 10.3238/arztebl.2020.0653
Briken, P., Wiessner, C., Štulhofer, A., Klein, V., Fuß, J., Reed, G. M., et al. (2022). Corrigendum to: who feels affected by "out of control" sexual behavior? Prevalence and correlates of indicators for ICD-11 compulsive sexual behavior disorder in the German health and sexuality survey (GeSiD). J. Behav. Addict. 11, 1093–1095. doi: 10.1556/2006.2022.20000
Browne, M. W., and & Cudeck, R. (1993). “Alternative ways of assessing model fit,” in Testing structural equation models, ed. K. A. Bollen and J. S. Long (CA: Sage), 136–162.
Bryl, N., Czarnecka-Iwańczuk, M., Romanowska, M., Stanisić, M. G., Michalak, M., and Posadzy-Małaczyńska, A. (2020). Picie alkoholu jako sposób radzenia sobie ze stresem u studentów kierunków medycznych [drinking alcohol as a way of coping with stress in students of medical faculties]. Psychiatr. Pol. 54, 265–277. doi: 10.12740/PP/99029
Candido, F. J., Souza, R., Stumpf, M. A., Fernandes, L. G., Veiga, R., Santin, M., et al. (2018). The use of drugs and medical students: a literature review. Rev. Assoc. Med. Bras. 64, 462–468. doi: 10.1590/1806-9282.64.05.462
Ciocca, G., Fontanesi, L., Robilotta, A., Limoncin, E., Nimbi, F. M., Mollaioli, D., et al. (2022). Hypersexual behavior and depression symptoms among dating app users. Theol. Sex. 3, 298–307. doi: 10.3390/sexes3020023
Dahlin, M., Nilsson, C., Stotzer, E., and Runeson, B. (2011). Mental distress, alcohol use and help-seeking among medical and business students: a cross-sectional comparative study. BMC Med. Educ. 11:92. doi: 10.1186/1472-6920-11-92
Del Carmen, M. G., Herman, J., Rao, S., Hidrue, M. K., Ting, D., Lehrhoff, S. R., et al. (2019). Trends and factors associated with physician burnout at a multi-specialty academic faculty practice organization. JAMA Netw. Open 2:e190554. doi: 10.1001/jamanetworkopen.2019.0554
Diehl, A., Pillon, S. C., Dos Santos, M. A., Rassool, G. H., and Laranjeira, R. (2016). Sexual dysfunction and sexual behaviors in a sample of Brazilian male substance misusers. Am. J. Mens Health 10, 418–427. doi: 10.1177/1557988315569298
Dolatshahi, B., Farhoudian, A., Falahatdoost, M., Tavakoli, M., and Rezaie Dogahe, E. (2016). A qualitative study of the relationship between methamphetamine abuse and sexual dysfunction in male substance abusers. Int. J. High Risk Behav. Addict. 5:e29640. doi: 10.5812/ijhrba.29640
Döring, N., and Mohseni, M. R. (2022). Der gender orgasm gap [the gender orgasm gap]. Zeitschrift für Sexualforschung 35, 73–87. doi: 10.1055/a-1832-4771
Dyrbye, L. N., Thomas, M. R., and Shanafelt, T. D. (2006). Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad. Med. 81, 354–373. doi: 10.1097/00001888-200604000-00009
Frith, H. (2013). Labouring on orgasms: embodiment, efficiency, entitlement and obligations in heterosex. Cult. Health Sex. 15, 494–510. doi: 10.1080/13691058.2013.767940
Fritz, J., De Graaff, A. M., Caisley, H., van Harmelen, A.-L., and Wilkinson, P. O. (2018). A systematic review of amenable resilience factors that moderate and/or mediate the relationship between childhood adversity and mental health in young people. Front. Psych. 9:230. doi: 10.3389/fpsyt.2018.00230
Gajda, M., Sedlaczek, K., Szemik, S., and Kowalska, M. (2021). Determinants of alcohol consumption among medical students: results from POLLEK cohort study. Int. J. Environ. Res. Public Health 18:5872. doi: 10.3390/ijerph18115872
Gignon, M., Havet, E., Ammirati, C., Traullé, S., Manaouil, C., Balcaen, T., et al. (2015). Alcohol, cigarette, and illegal substance consumption among medical students: a cross-sectional survey. Workplace Health Saf. 63, 54–63. doi: 10.1177/2165079915570917
Gilbert, R., Widom, C. S., Browne, K., Fergusson, D., Webb, E., and Janson, S. (2009). Burden and consequences of child maltreatment in high-income countries. Lancet 373, 68–81. doi: 10.1016/S0140-6736(08)61706-7
Glaesmer, H. (2016). Assessing childhood maltreatment on the population level in Germany: findings and methodological challenges. Child Adolesc. Psychiatry Ment. Health 10:15. doi: 10.1186/s13034-016-0104-9
Gonçalves, W. S., Gherman, B. R., Abdo, C. H. N., Coutinho, E. S. F., Nardi, A. E., and Appolinario, J. C. (2023). Prevalence of sexual dysfunction in depressive and persistent depressive disorders: a systematic review and meta-analysis. Int. J. Impot. Res. 35, 340–349. doi: 10.1038/s41443-022-00539-7
Grover, S., Mattoo, S. K., Pendharkar, S., and Kandappan, V. (2014). Sexual dysfunction in patients with alcohol and opioid dependence. Indian J. Psychol. Med. 36, 355–365. doi: 10.4103/0253-7176.140699
Grubbs, J. B., Hoagland, K. C., Lee, B. N., Grant, J. T., Davison, P., Reid, R. C., et al. (2020). Sexual addiction 25 years on: a systematic and methodological review of empirical literature and an agenda for future research. Clin. Psychol. Rev. 82:101925. doi: 10.1016/j.cpr.2020.101925
Gupta, H., Gupta, S., and Rozatkar, A. R. (2022). Magnitude of substance use and its associated factors among the medical students in India and implications for medical education: a narrative review. Indian J. Psychol. Med. 44, 218–226. doi: 10.1177/02537176211032366
Hair, J., Black, W. C., Babin, B. J., and Anderson, R. E. (2010). Multivariate data analysis. 7th Edn. Upper Saddle River, New Jersey: Pearson Educational International.
Hallinan, R. (2021). “Sexual function and alcohol and other drug use” in Textbook of addiction treatment. eds. N. El-Guebaly, G. Carrà, M. Galanter, and A. M. Baldacchino (Cham: Springer International Publishing), 1225–1239.
Hamilton, L. D., and Julian, A. M. (2014). The relationship between daily hassles and sexual function in men and women. J. Sex Marital Ther. 40, 379–395. doi: 10.1080/0092623X.2013.864364
Hoff, T. A., Heller, S., Reichel, J. L., Werner, A. M., Schäfer, M., Tibubos, A. N., et al. (2023). Cigarette smoking, risky alcohol consumption, and marijuana smoking among university students in Germany: identification of potential sociodemographic and study-related risk groups and predictors of consumption. Healthcare 11:3182. doi: 10.3390/healthcare11243182
Ignatova, D., Joseph, S., Priebe, L., Kamenova, I., and Vladimirova, R. (2022). Prevalence and correlationships between childhood trauma and negative mental health outcomes in medical students. Bulgarian J. Psychiatry 7, 21–32.
Jackson, E. R., Shanafelt, T. D., Hasan, O., Satele, D. V., and Dyrbye, L. N. (2016). Burnout and alcohol abuse/dependence among U.S. medical students. Acad. Med. 91, 1251–1256. doi: 10.1097/ACM.0000000000001138
Jannini, E. A., Rubio-Casillas, A., Whipple, B., Buisson, O., Komisaruk, B. R., and Brody, S. (2012). Female orgasm(s): one, two, several. J. Sex. Med. 9, 956–965. doi: 10.1111/j.1743-6109.2012.02694.x
Jepsen, D., Healy, K. V., Bernard, M., Markert, J., and Brzank, P. J. (2024). Patterns of sexual risk behaviors and sexuality-related risk factors among young adults in Germany: implications for prevention and therapy. Arch. Sex. Behav. 53, 2671–2688. doi: 10.1007/s10508-024-02877-7
Jepsen, D., Luck, T., Bernard, M., Moor, I., and Watzke, S. (2023). Study protocol: hypersexual and hyposexual behavior among adults diagnosed with alcohol- and substance use disorders – associations between traumatic experiences and problematic sexual behavior. Front. Psych. 14:1088747. doi: 10.3389/fpsyt.2023.1088747
Jestin, M., Sharma, S., Jhaveri, D., Mitchell, B., Micciche, D., Venkataraman, V., et al. (2023). Mental health differences in medical students based on curriculum and gender. BMC Med. Educ. 23:971. doi: 10.1186/s12909-023-04946-2
Kenny, D. A., Kaniskan, B., and McCoach, D. B. (2015). The performance of RMSEA in models with small degrees of freedom. Sociol. Methods Res. 44, 486–507. doi: 10.1177/0049124114543236
Keuch, L., Pukas, L., Rabkow, N., Ehring, E., Kindt, T., Rehnisch, C., et al. (2023). Beck’s depression inventory II suicidal ideation in medical students – prevalence and associated factors. Int. J. Med. Stud. 11, 38–44. doi: 10.5195/ijms.2023.1434
King, E., Steenson, C., Shannon, C., and Mulholland, C. (2017). Prevalence rates of childhood trauma in medical students: a systematic review. BMC Med. Educ. 17:159. doi: 10.1186/s12909-017-0992-2
Klinitzke, G., Romppel, M., Häuser, W., Brähler, E., and Glaesmer, H. (2012). Die deutsche version des childhood trauma questionnaire (CTQ) – psychometrische Eigenschaften in einer bevölkerungsrepräsentativen Stichprobe [the German version of the childhood trauma questionnaire (CTQ): psychometric characteristics in a representative sample of the general population]. Psychother. Psychosom. Med. Psychol. 62, 47–51. doi: 10.1055/S-0031-1295495
Krüger, T. H. C. (2020). “Der Einfluss von psychiatrischen und neurologischen Erkrankungen auf die Sexualität [the influence of psychiatric and neurological disorders on sexuality]” in Sexualmedizin Für die praxis – Sexualberatung und Krisenintervention Bei Sexuellen Störungen [sexual medicine for practice–sexual counselling and crisis intervention]. eds. U. Hartmann, T. Krüger, V. Kürbitz, and C. Neuhof (Berlin: Springer), 44–59.
Lalchandani, P., Lisha, N., Gibson, C., and Huang, A. J. (2020). Early life sexual trauma and later life genitourinary dysfunction and functional disability in women. J. Gen. Intern. Med. 35, 3210–3217. doi: 10.1007/S11606-020-06118-0
Lutfey, K. E., Link, C. L., Litman, H. J., Rosen, R. C., and McKinlay, J. B. (2008). An examination of the association of abuse (physical, sexual, or emotional) and female sexual dysfunction: results from the Boston area community health survey. Fertil. Steril. 90, 957–964. doi: 10.1016/j.fertnstert.2007.07.1352
MacCallum, R. C., Browne, M. W., and Sugawara, H. M. (1996). Power analysis and determination of sample size for covariance structure modeling. Psychol. Methods 1, 130–149. doi: 10.1037/1082-989X.1.2.130
Macdonald, S., Halliday, J., MacEwan, T., Sharkey, V., Farrington, S., Wall, S., et al. (2003). Nithsdale schizophrenia surveys 24: sexual dysfunction. Case-control study. Br. J. Psychiatry 182, 50–56. doi: 10.1192/bjp.182.1.50
Marcoulides, K. M., and Raykov, T. (2019). Evaluation of variance inflation factors in regression models using latent variable modeling methods. Educ. Psychol. Meas. 79, 874–882. doi: 10.1177/0013164418817803
Medisauskaite, A., and Kamau, C. (2019). Does occupational distress raise the risk of alcohol use, binge-eating, ill health and sleep problems among medical doctors? A UK cross-sectional study. BMJ Open 9:e027362. doi: 10.1136/bmjopen-2018-027362
Moustafa, A. A., Parkes, D., Fitzgerald, L., Underhill, D., Garami, J., Levy-Gigi, E., et al. (2021). The relationship between childhood trauma, early-life stress, and alcohol and drug use, abuse, and addiction: an integrative review. Curr. Psychol. 40, 579–584. doi: 10.1007/S12144-018-9973-9
Müller, M. J. (2016). SBQ-G – Sexual Behaviour Questionnaire – deutsche Version : Trier: Leibniz Institut für Psychologische Information und Dokumentation (ZPID) – Testarchiv.
National Institute on Drug Abuse (2014). DAST-10. Available at: https://cde.nida.nih.gov/sites/nida_cde/files/DrugAbuseScreeningTest_2014Mar24.pdf (Accessed October 16, 2024).
Pace, C. S., Muzi, S., Rogier, G., Meinero, L. L., and Marcenaro, S. (2022). The adverse childhood experiences – international questionnaire (ACE-IQ) in community samples around the world: a systematic review (part I). Child Abuse Negl. 129:105640. doi: 10.1016/j.chiabu.2022.105640
Palha, A. P., and Esteves, M. (2008). Drugs of abuse and sexual functioning. Adv. Psychosom. Med. 29, 131–149. doi: 10.1159/000126628
Prabhakaran, D. K., Nisha, A., and Varghese, P. J. (2018). Prevalence and correlates of sexual dysfunction in male patients with alcohol dependence syndrome: a cross-sectional study. Indian J. Psychiatry 60, 71–77. doi: 10.4103/psychiatry.IndianJPsychiatry_42_17
Pukas, L., Rabkow, N., Keuch, L., Ehring, E., Fuchs, S., Stoevesandt, D., et al. (2022). Prevalence and predictive factors for depressive symptoms among medical students in Germany – a cross-sectional study. GMS J. Med. Educ. 39:Doc13. doi: 10.3205/zma001534
Reid, R. C., Bramen, J. E., Anderson, A., and Cohen, M. S. (2014). Mindfulness, emotional dysregulation, impulsivity, and stress proneness among hypersexual patients. J. Clin. Psychol. 70, 313–321. doi: 10.1002/jclp.22027
Rogoža, D., Strumila, R., Klivickaitė, E., Diržius, E., and Čėnaitė, N. (2021). Depressive symptoms, help-seeking, and barriers to mental healthcare among healthcare professionals in Lithuania. Acta Med. Litu. 28, 59–76. doi: 10.15388/Amed.2020.28.1.3
Rohilla, J., Dhanda, G., Meena, P. S., Jilowa, C. S., Tak, P., and Jain, M. (2020). Sexual dysfunction in alcohol-dependent men and its correlation with marital satisfaction in spouses: a hospital-based cross-sectional study. Ind. Psychiatry J. 29, 82–87. doi: 10.4103/Ipj.Ipj_5_20
Roncero, C., Egido, A., Rodríguez-Cintas, L., Pérez-Pazos, J., Collazos, F., and Casas, M. (2015). Substance use among medical students: a literature review 1988–2013. Actas Esp. Psiquiatr. 43, 109–121.
Sack, M., and Büttner, M. (2014). Sexuelle Störungen als Folge sexueller Traumatisierungen [sexual disorders as a consequence of sexual trauma]. Psychotherapie im Dialog 15, 28–31. doi: 10.1055/S-0034-1370807
Schultz, K., Hook, J. N., Davis, D. E., Penberthy, J. K., and Reid, R. C. (2014). Nonparaphilic hypersexual behavior and depressive symptoms: a meta-analytic review of the literature. J. Sex Marital Ther. 40, 477–487. doi: 10.1080/0092623X.2013.772551
Sciolla, A. F., Wilkes, M. S., and Griffin, E. J. (2019). Adverse childhood experiences in medical students: implications for wellness. Acad. Psychiatry 43, 369–374. doi: 10.1007/s40596-019-01047-5
Sheehama, J. H., Mbangula, H. J., and Lukolo, L. N. (2022). Alcohol drinking patterns and contributing factors among medical students, a systematic review. Clin. Med. Rev. Rep. 4, 01–03. doi: 10.31579/2690-8794/094
Shindel, A. W., Ferguson, G. G., Nelson, C. J., and Brandes, S. B. (2008). The sexual lives of medical students: a single institution survey. J. Sex. Med. 5, 796–803. doi: 10.1111/j.1743-6109.2007.00744.x
Slavin, S. J., Schindler, D. L., and Chibnall, J. T. (2014). Medical student mental health 3.0: improving student wellness through curricular changes. Acad. Med. 89, 573–577. doi: 10.1097/ACM.0000000000000166
Statistisches Bundesamt (2024). “Studierende insgesamt und Studierende Deutsche im Studienfach Medizin (Allgemein-Medizin) nach Geschlecht [Total amount of students/ German students studying medicine by sex].” Available at: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bildung-Forschung-Kultur/Hochschulen/Tabellen/lrbil05.html#242500 (Accessed October 16, 2024).
Stone, A. L., Becker, L. G., Huber, A. M., and Catalano, R. F. (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict. Behav. 37, 747–775. doi: 10.1016/j.addbeh.2012.02.014
Vasilenko, S. A. (2021). “Emerging adult sexual behavior” in Sexuality in emerging adulthood. eds. E. Morgan and M. H. M. van Dulmen (New York: Oxford University Press), 43–64.
Vayr, F., Herin, F., Jullian, B., Soulat, J. M., and Franchitto, N. (2019). Barriers to seeking help for physicians with substance use disorder: a review. Drug Alcohol Depend. 199, 116–121. doi: 10.1016/j.drugalcdep.2019.04.004
Velurajah, R., Brunckhorst, O., Waqar, M., McMullen, I., and Ahmed, K. (2022). Erectile dysfunction in patients with anxiety disorders: a systematic review. Int. J. Impot. Res. 34, 177–186. doi: 10.1038/s41443-020-00405-4
Vijendren, A., Yung, M., and Sanchez, J. (2015). Occupational health issues amongst UK doctors: a literature review. Occup. Med. 65, 519–528. doi: 10.1093/occmed/kqv088
Voigt, K., Twork, S., Mittag, D., Göbel, A., Voigt, R., Klewer, J., et al. (2009). Consumption of alcohol, cigarettes and illegal substances among physicians and medical students in Brandenburg and Saxony (Germany). BMC Health Serv. Res. 9:219. doi: 10.1186/1472-6963-9-219
von Franqué, F., and Briken, P. (2018). “Hypersexuelle Störung bei sexuellen Missbrauchserfahrungen [hypersexual disorder and experiences of sexual abuse]” in Sexualität und trauma – Grundlagen und Therapie Traumassoziierter Sexueller Störungen [sexuality and trauma– Fundamentals and therapy of trauma-associated sexual disorders]. ed. M. Büttner (Stuttgart: Schattauer), 116–122.
Wade, L. (2016). “Are women bad at orgasms? Understanding the gender gap” in Gender, sex, and politics: In the streets and between the sheets in the 21st century. ed. S. Tarrant (New York: Routledge), 227–237.
Wade, L., Kremer, E. C., and Brown, J. (2005). The incidental orgasm: the presence of clitoral knowledge and the absence of orgasm for women. Women Health 42, 117–138. doi: 10.1300/J013v42n01_07
Wallwiener, C. W., Wallwiener, L.-M., Seeger, H., Schönfisch, B., Mueck, A. O., Bitzer, J., et al. (2017). Sexual function, contraception, relationship, and lifestyle in female medical students. J. Women's Health 26, 169–177. doi: 10.1089/jwh.2015.5731
Walton, M. T., Cantor, J. M., and Lykins, A. D. (2017). An online assessment of personality, psychological, and sexuality trait variables associated with self-reported hypersexual behavior. Arch. Sex. Behav. 46, 721–733. doi: 10.1007/s10508-015-0606-1
Wang, J., Fitzke, R. E., Tran, D. D., Grell, J., and Pedersen, E. R. (2023). Mental health treatment-seeking behaviors in medical students: a mixed-methods approach. J. Med. Access 7:27550834221147787. doi: 10.1177/27550834221147787
Weiss, D. S., and Marmar, C. R. (1996). “The impact of event scale – revised” in Assessing psychological trauma and PTSD. eds. J. P. Wilson and T. M. Keane (New York: Guilford), 399–411.
Weiss, J., Steil, R., Priebe, K., Lindauer, P., Kleindienst, N., Fydrich, T., et al. (2023). Sexual dysfunctions in women with post-traumatic stress disorder following childhood sexual abuse: prevalence rates according to DSM-5 and clinical correlates. Arch. Sex. Behav. 52, 3365–3378. doi: 10.1007/s10508-023-02652-0
Wijeratne, C., Johnco, C., Draper, B., and Earl, J. (2021). Doctors' reporting of mental health stigma and barriers to help-seeking. Occup. Med. 71, 366–374. doi: 10.1093/occmed/kqab119
Wilson, J., Tanuseputro, P., Myran, D. T., Dhaliwal, S., Hussain, J., Tang, P., et al. (2022). Characterization of problematic alcohol use among physicians: a systematic review. JAMA Netw. Open 5:e2244679. doi: 10.1001/jamanetworkopen.2022.44679
Witt, A., Brown, R. C., Plener, P. L., Brähler, E., and Fegert, J. M. (2017). Child maltreatment in Germany: prevalence rates in the general population. Child Adolesc. Psychiatry Ment. Health 11:47. doi: 10.1186/s13034-017-0185-0
Wood, D., Crapnell, T., Lau, L., Bennett, A., Lotstein, D., Ferris, M., et al. (2018). “Emerging adulthood as a critical stage in the life course” in Handbook of life course health development. eds. N. Halfon, C. B. Forrest, R. M. Lerner, and E. M. Faustman (Cham: Springer).
World Health Organisation (WHO) (2024). “ICD-11 for Mortality and Morbidity Statistics (ICD-11 MMS).” Available at: https://icd.who.int/browse11/l-m/en. (Accessed October 16, 2024).
World Medical Association (WMA) (2022). “WMA Decleration of Helsinki – Ethical principals for medical research invovlving human subjects.” Available at: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (Accessed October 16, 2024).
Yee, A., Danaee, M., Loh, H. S., Sulaiman, A. H., and Ng, C. G. (2016). Sexual dysfunction in heroin dependents: a comparison between methadone and buprenorphine maintenance treatment. PLoS One 11:e0147852. doi: 10.1371/journal.pone.0147852
Keywords: adverse childhood experiences, addiction, childhood trauma, hypersexual behavior, hyposexual behavior, sexual dysfunction, post-traumatic stress
Citation: Jepsen D, Luck T, Heckel C, Niemann J, Winter K and Watzke S (2024) Compulsive sexual behavior, sexual functioning problems, and their linkages to substance use among German medical students: exploring the role of sex and trauma exposure. Front. Psychol. 15:1423690. doi: 10.3389/fpsyg.2024.1423690
Edited by:
Carlos Emanuel Rodriguez-Diaz, Boston University, United StatesReviewed by:
Jürgen Fuchshuber, Medical University of Vienna, AustriaStefania Muzi, University of Genoa, Italy
Copyright © 2024 Jepsen, Luck, Heckel, Niemann, Winter and Watzke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dennis Jepsen, ZGVubmlzLmplcHNlbkBtZWRpemluLnVuaS1oYWxsZS5kZQ==
 Dennis Jepsen
Dennis Jepsen Tobias Luck
Tobias Luck Christian Heckel
Christian Heckel Jana Niemann
Jana Niemann Kristina Winter
Kristina Winter Stefan Watzke
Stefan Watzke