- 1Sylvester Comprehensive Cancer Center, Miller School of Medicine, University of Miami, Miami, FL, United States
- 2Division of Medical Oncology, Department of Medicine, Miller School of Medicine, University of Miami, Miami, FL, United States
- 3Department of Psychiatry and Behavioral Sciences, Miller School of Medicine, University of Miami, Miami, FL, United States
- 4University of Minnesota Medical School, Duluth, MN, United States
- 5Department of Palliative, Rehabilitation and Integrative Medicine, The University of Texas M. D. Anderson Cancer Center, Houston, TX, United States
- 6Department of Neurosurgery, The University of Texas M. D. Anderson Cancer Center, Houston, TX, United States
- 7Department of Pediatrics Hematology-Oncology, Baylor College of Medicine, Houston, TX, United States
- 8Westat, Rockville, MD, United States
- 9Huntsman Cancer Institute, University of Utah, Salt Lake City, UT, United States
- 10Department of Population Health Sciences, University of Utah, Salt Lake City, UT, United States
- 11Department of Psychology, University of Miami, Miami, FL, United States
- 12Department of Medicine, Miller School of Medicine, University of Miami, Miami, FL, United States
Introduction: Cancer survivors experienced poorer health-related quality of life (HRQoL) and greater psychological distress during the COVID-19 pandemic than those without cancer. However, the underlying mechanisms that may explain how negative experiences during the pandemic are associated with distress and HRQoL remain unknown. We examined whether psychosocial risk factors (i.e., healthcare disruption, disruption to daily activities and social interaction [DDASI], and financial hardship) mediated the relationship between negative COVID-19-related experiences and cancer survivors’ HRQoL and psychological distress (i.e., depressive symptoms, and anxiety) and whether the mediating effects were moderated by psychosocial protective factors (i.e., stress management ability and social support).
Methods: A total of 9,651 cancer survivors completed a questionnaire assessing negative COVID-19-related experiences, psychosocial and practical experiences, and HRQoL. Conditional process analysis was used to evaluate the proposed moderated mediation models.
Results: Participants had a mean age of 63.8 years (SD = 12.3) and were mostly non-Hispanic White (82.3%). DDASI and financial hardship mediated the relationship between negative COVID-19-related experiences and cancer survivor’s HRQoL and psychological distress. Stress management ability buffered the indirect effect of DDASI on cancer survivors’ HRQoL and psychological distress. Social support buffered the indirect effect of financial hardship on HRQoL and depressive symptoms.
Conclusion: Financial resources and social interactions may buffer negative effects of major disruptions such as the COVID-19 pandemic. Future studies should assess the longitudinal impact of these associations.
1 Introduction
The COVID-19 pandemic was one of the most challenging and disruptive global events experienced in several generations. While the federal COVID-19 Public Health Emergency declaration ended on May 11, 2023, the COVID-19 pandemic presented a chronic and challenging public health threat that continues to impact all communities (Nelson and Kaminsky, 2020). Cancer survivors are considered particularly vulnerable due to their increased propensity to infections and poor immunological responses to COVID-19 vaccines and boosters, as well as ongoing cancer-related stressors (Becerril-Gaitan et al., 2022; Ligumsky et al., 2022; Naranbhai et al., 2022). One of the challenges among cancer survivors regarding the COVID-19 pandemic is the trade-off between increased risk of contracting COVID-19 while receiving treatment/follow-up care vs. reduced risk of COVID-19 infection by postponing treatment/follow-up (Burki, 2020). As cancer survivors are already coping with multiple, and often chronic, challenges associated with a cancer diagnosis and treatment, these were exacerbated by the COVID-19 pandemic (Ayubi et al., 2021; Momenimovahed et al., 2021; Muls et al., 2022). These challenges include, but are not limited to, emotional and social concerns regarding disease activity, treatment response, interpersonal disruptions, healthcare disruptions, and financial burden (Steel et al., 2022; Williams et al., 2022). Collectively, these chronic stressors can significantly further impact health-related quality of life (HRQoL) and psychological distress, such as symptoms of anxiety and depression. However, the characterization of potential processes by which pandemics may impact psychological distress and HRQoL in cancer survivors remains relatively unknown.
A robust psychosocial literature has documented the role of multiple psychosocial factors on HRQoL and psychological distress outcomes in cancer populations. These include concerns about unmet needs specific to health care delivery, daily activities, social interaction, and finances (Brose et al., 2023; Ghazal et al., 2023; Lu et al., 2023; Tan et al., 2023). Furthermore, the impact of these factors on adverse outcomes can vary according to socio-economic status (SES) and other social determinants of health (Bambra et al., 2020; Chu et al., 2022). Multiple studies have reported worse HRQoL and greater emotional distress among cancer survivors during the COVID-19 pandemic; however, limited research has examined the underlying mechanisms that may explain how negative experiences during the COVID-19 pandemic may impact psychological distress and HRQoL outcomes (Ayubi et al., 2021; Muls et al., 2022). Conversely, resilience factors such as social support, perceived benefits in the face of challenges, and stress management skills have been shown to favorably impact HRQoL and other patient-reported outcomes (Velasco-Durantez et al., 2022; Guidry et al., 2023). Identifying factors associated with psychological distress and HRQoL is the first step in mitigating the deleterious effects of added stressors on cancer survivors by intervening on the modifiable risk and protective factors.
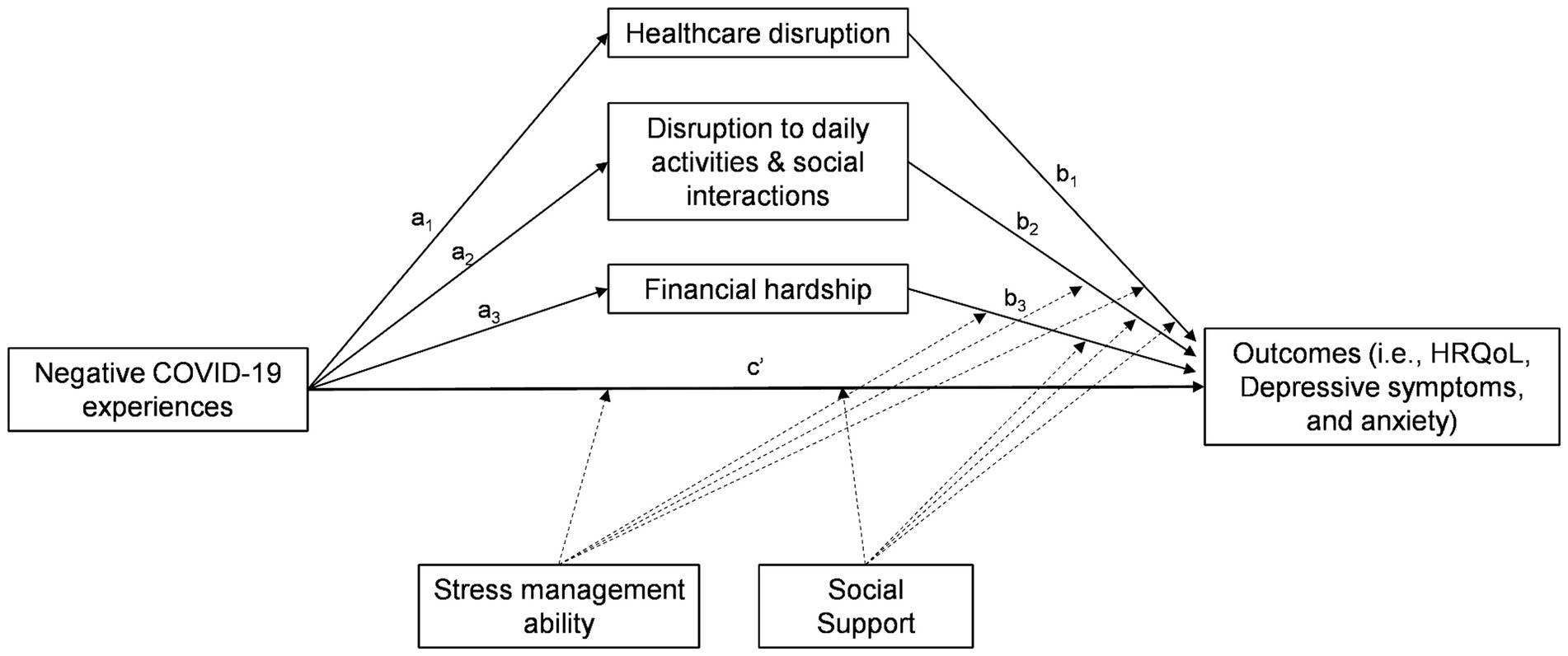
This study aimed to:(1) assess whether psychosocial risk factors [i.e., healthcare disruption, disruption to daily activities and social interaction (DDASI), and financial hardship] mediated the relationship between negative COVID-19-related experiences and cancer survivors’ HRQoL and psychological distress (i.e., anxiety and depressive symptoms), and (2) assess whether psychosocial protective factors (i.e., stress management ability and social support) moderated any mediating effect of psychosocial risk factors in the relationship between negative COVID-19-related experiences and cancer survivors’ HRQoL and psychological distress. We thus examined the following hypotheses: (1) greater negative COVID-19-related experiences would be associated with poorer HRQoL and greater psychological distress and psychosocial risk factors; (2) the relationship between negative COVID-19-related experiences and cancer survivors’ HRQoL and psychological distress would be mediated by psychosocial risk factors, and (3) psychosocial protective factors would moderate the relationship between negative COVID-19-related experiences and cancer survivors’ HRQoL and psychological distress such that at higher levels of psychosocial protective factors the direct effect of negative COVID-19-related experiences as well as the indirect effects of psychosocial risk factors become weaker (Figure 1).
2 Materials and methods
2.1 Participants
This study involved an online survey conducted between May 2020 and January 2021 to investigate the impact of the COVID-19 pandemic on cancer survivors. An individual is considered a cancer survivor from the time of diagnosis through the balance of life (National Cancer Institute, 2024). Participants were recruited from the University of Texas MD Anderson Cancer Center (MDACC; IRB #2020-0508) and the University of Miami Sylvester Comprehensive Cancer Center (SCCC; IRB #202000450). Inclusion criteria were: ≥18 years old; English- or Spanish-speaking; MDACC or SCCC patient; attended a clinical visit within the past 5 years; ICD-10 confirmed cancer diagnosis; and contactable via email or electronic patient portal. Patients received either an email or patient portal message with the link to the online REDCap survey (Harris et al., 2009; Harris et al., 2019). All participants signed an electronic informed consent prior to data collection.
2.2 Measures
2.2.1 Negative COVID-19-related experiences
Survey participants were asked whether or not they underwent adverse COVID-19 experiences. This questionnaire included 21 questions and were answered as Yes = 1 or No = 0. Sample items include: “If you tested positive for COVID-19, were you hospitalized?,” “Did a family member or a member of your household die of COVID-19?,” “Did you lose your job or primary source of income due to COVID-19?” The summation of the responses represented the total number of negative COVID-19-related experiences (Perry et al., 2023).
2.2.2 COVID-19-related psychosocial and practical experiences questionnaire
The COVID-PPE is a validated questionnaire that assesses COVID-19-related psychological distress (i.e., anxiety and depressive symptoms) and psychosocial risk and protective factors (Saez-Clarke et al., 2023). This 5-point Likert scale instrument, ranging from 0 (strongly disagree) to 4 (strongly agree), includes 43 items and yields nine subscales (i.e., COVID-19 specific anxiety and depressive symptoms, healthcare disruption, satisfaction with provider response, disruption to daily activities and social interaction, financial hardship, perceived benefit, social support, and perceived stress management ability). A subscale score was estimated by averaging the corresponding items (range 0–4), with a higher score indicating a higher level of the construct being assessed (Cronbach’s alphas [α’s] = 0.61–0.89). The correlations across the psychosocial risk factors range from 0.29 to 0.56. The correlation between the psychosocial protective factors was 0.37. See Saez-Clarke et al. (2023) for additional details on the development and psychometric evaluation of the COVID-PPE questionnaire.
2.2.3 Health-related quality of life
HRQoL was measured using the Functional Assessment of Cancer Therapy-General-7 Item Version (FACT-G7), a well-validated measure of HRQoL in oncology (Pearman et al., 2014). Four item scores were reverse-coded. The total score ranges from 0 to 28, with a higher total score indicating better HRQoL (α = 0.80).
2.2.4 Sociodemographic and clinical characteristics
Age, sex, self-reported race and ethnicity, insurance type (i.e., managed care, Medicaid, Medicare, other/self-pay), cancer diagnosis and stage (metastatic vs. non-metastatic disease), and ZIP code of residence were extracted from electronic health records. SES was assessed with the area deprivation index (ADI), which is a validated multidimensional measure of neighborhood socioeconomic disadvantages based on 17 census indicators assessing education, income, household characteristics, and housing (Kind and Buckingham, 2018). ADI ranges from 1, least deprived, to 100, the most deprived neighborhood.
2.3 Data analysis
The survey responses were inspected for data quality check. Descriptive analysis was computed for all variables to ensure values were within expected ranges and errors were eliminated. Then, descriptive statistics (i.e., mean, standard deviation, counts, and percentages) were calculated using SAS version 9.4 (SAS Institute, Cary, NC). Moderated mediation analysis was conducted with the PROCESS macro for SAS version 4.3.1 (Copyright 2017–2023 by Andrew F. Hayes), a regression-based modeling tool for mediation, moderation, and conditional process analysis (Hayes and Rockwood, 2020; Hayes, 2022). First, we estimated separate parallel multiple mediation models to assess the impact of negative COVID-19-related experiences (X) on each outcome (i.e., HRQoL, anxiety symptoms, and depressive symptoms). The involved mediators of the models were: healthcare disruption (M1), disruption to daily activities and social interaction (M2), and financial hardship (M3). To examine whether stress management ability (W1) and social support (W2) moderated the direct effect of negative COVID-19-related experiences as well as the specific indirect effect of each mediator, eight interaction terms were included in the moderated mediation models (e.g., X*W1, X*W2, M1*W1, M1*W2). “High” and “low” levels of both moderators were determined at one standard deviation above and below the mean of each scale. Bias-corrected bootstrapping methods with 5,000 bootstrap samples were used to examine the significance of the effects, which were considered significant if the resulting confidence interval did not contain 0. Continuous variables were grand mean centered and categorial covariates were dummy coded. To account for potential confounding by sociodemographic and medical variables, all models were adjusted for study site, age, sex, race/ethnicity, ADI score, insurance type, cancer type (hematologic vs. solid tumor), and whether patients had metastatic disease. We computed the variance inflation factor (VIF) of each variable to assess the degree of multicollinearity. All VIFs were below two suggesting that the model estimations did not have a multicollinearity bias (Noora, 2020). The effects of the covariates were expressed in terms of standardized regression coefficients (betas).
3 Results
A total of 11,325 patients responded to the questionnaire. Of these, 9,651 cancer survivors had valid mailing addresses and were included in this study. Overall, participants had a mean age of 63.8 years (SD = 12.3). The majority were female (57.3%), non-Hispanic White (82.3%), and had managed care (50.3%) or Medicare (45.8%). Participants had a mean ADI score of 39.6 (SD = 24.5). The majority were diagnosed with a solid tumor (84.5%) and had non-metastatic disease (77.3%). Regarding psychosocial characteristics, out of the 21 possible negative COVID-19-related experiences, participants reported a mean of 7.3 negative experiences (SD = 1.9). From the COVID-PPE subscale scores (range 0–4), mean depressive symptoms score was 1.75 (SD = 0.98); anxiety symptoms score was 2.33 (SD = 0.92); healthcare disruption was 1.76 (SD = 1.13); disruption to daily activities and social interaction was 2.24 (SD = 0.86); financial hardship was 1.09 (SD = 0.85); perceived stress management skills was 2.67 (SD = 0.60); and social support was 2.60 (SD = 0.63). They also had a mean FACT-G7 score of 19.0 (SD = 5.3; Supplementary Table S1).
3.1 Sociodemographic and clinical characteristics and study outcomes
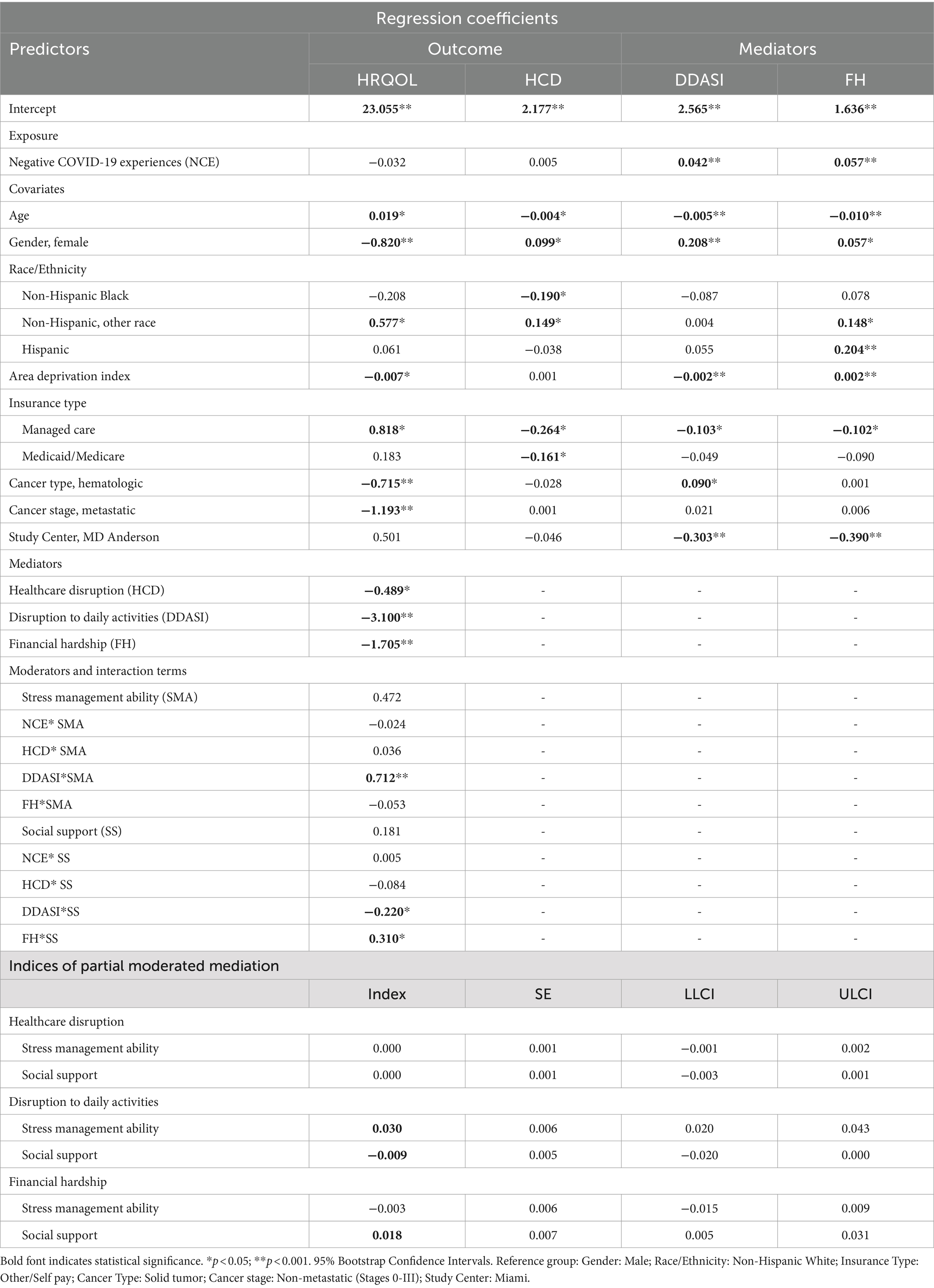
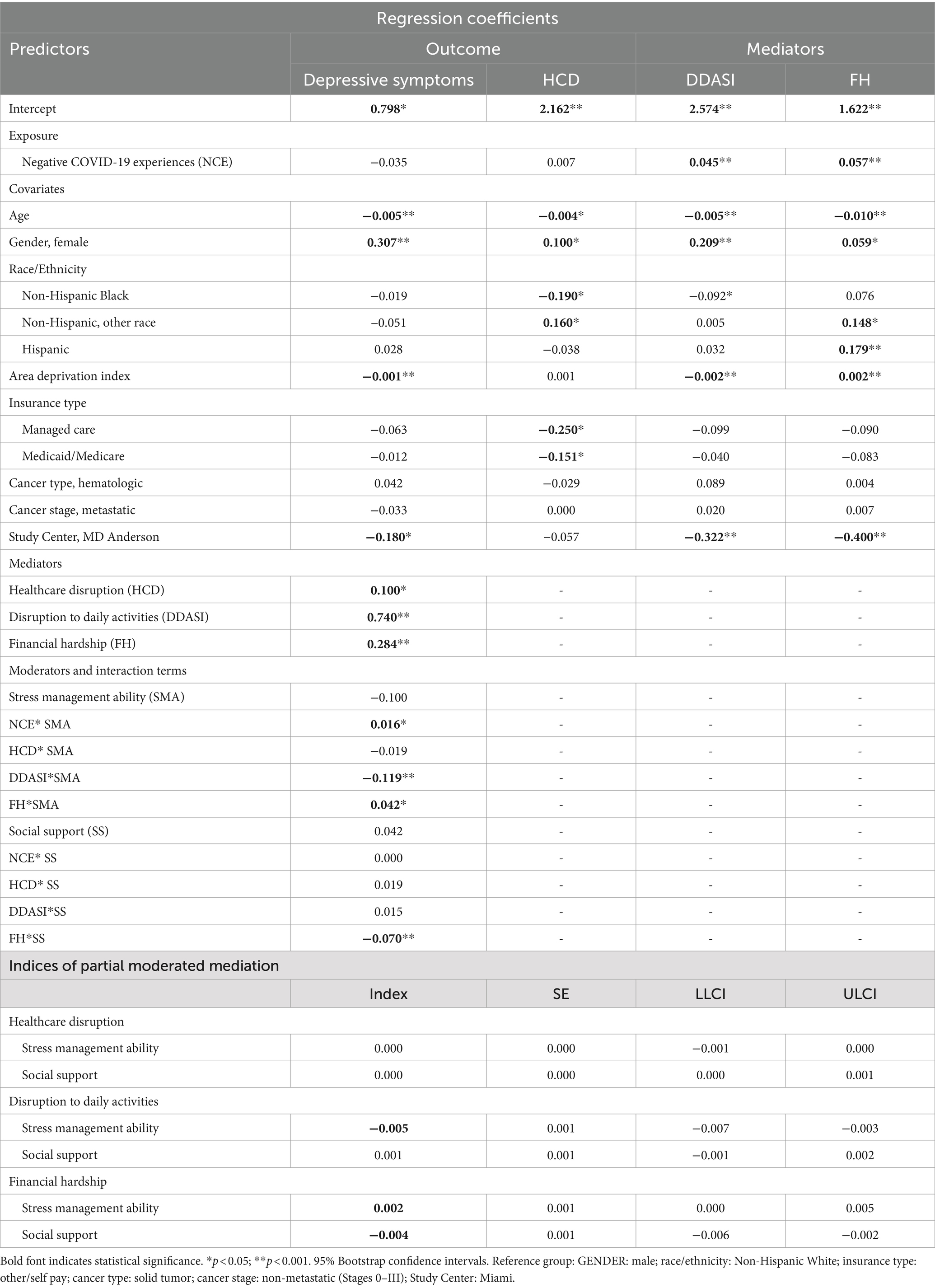
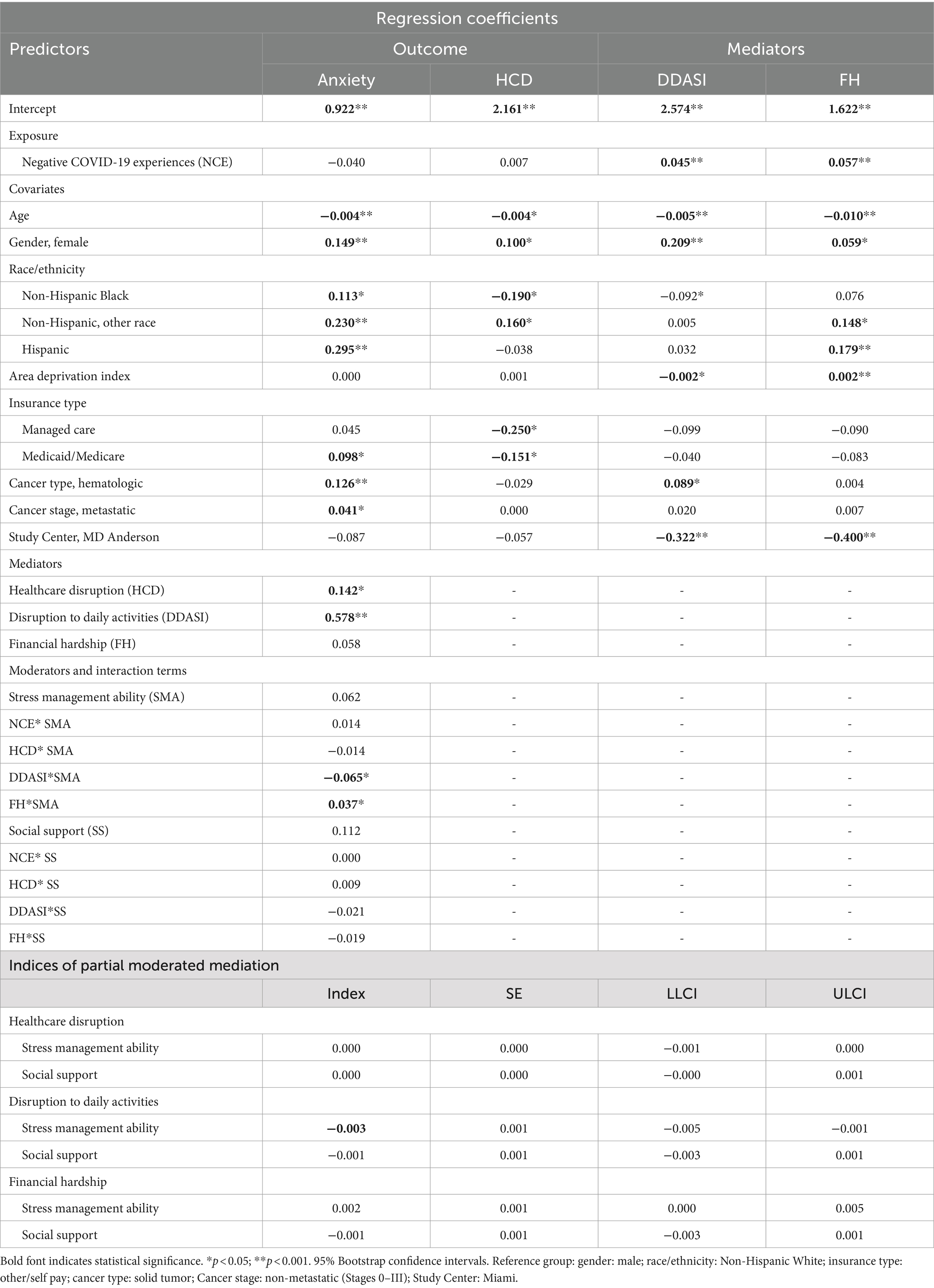
Tables 1–3 present the effects of the covariates on both study outcomes and mediators. Older age was associated with greater HRQoL, and less depressive and anxiety symptoms, and psychosocial risk factors (i.e., healthcare disruption, DDASI, financial hardship). Compared to men, women reported worse HRQoL, and more depressive and anxiety symptoms, and psychosocial risk factors. Compared to non-Hispanic Whites, non-Hispanic Black survivors had reported less healthcare disruption, but more anxiety symptoms. Hispanic cancer survivors reported more anxiety symptoms and financial hardship than non-Hispanic Whites. Cancer survivors with a higher ADI (more socioeconomically disadvantaged) had worse HRQoL, fewer depressive symptoms, less disruption to daily activities and social interaction, and more financial hardship. Compared to survivors with solid tumors, those with hematologic cancers reported worse HRQoL and more anxiety symptoms and disruption to daily activities and social interaction. Survivors with metastatic disease had worse HRQoL and more anxiety symptoms compared to those with stage 0-III disease.
3.2 Health-related quality of life
The parallel mediation model shows that the direct effect (DE) of negative COVID-19-related experiences on HRQoL was statistically significant (β = −0.083 95% Bootstrap Confidence Intervals [BCI]: −0.139, −0.028; Supplementary Table S2). The total indirect effect of the set of proposed mediators was statistically significant (β = −0.149; 95%BCI: −0.180, −0.116). Specifically, disruption to daily activities and social interaction (Indirect effect [IE] = −0.077, 95%BCI: −0.097, −0.057) and financial hardship (IE = −0.068, 95%BCI: −0.083, −0.054) mediated the relationship between negative COVID-19-related experiences and HRQoL.
The moderated mediation model shows that the DE of negative COVID-19-related experiences on HRQoL was not moderated by the proposed moderators (Table 1). Stress management ability moderated the IE of disruption to daily activities and social interaction. The interaction term was significant (β = 0.712, SE = 0.100, p < 0.001), and confirmed by a formal test using the index of moderated mediation [IMM] (0.030; 95%BCI: 0.020, 0.043), indicating that stress management ability buffered the IE of disruption to daily activities and social interaction on HRQoL (Supplementary Table S3; Supplementary Figure S1a). Social support moderated the IEs of disruption to daily activities and social interaction and financial hardship. The interaction terms were statistically significant (DDASI: β = −0.220, SE = 0.098, p = 0.023; FH: β = 0.310, SE = 0.098, p = 0.002), and confirmed by the IMM (DDASI: −0.009; 95%BCI: −0.020, −0.0004; FH: 0.018; 95%BCI: 0.005, 0.031). Social support enhanced the IE of disruption to daily activities and social interaction but buffered the IE of financial hardship on HRQoL (Supplementary Figure S1).
3.3 Depressive symptoms
The parallel mediation model shows that the total IE of the set of proposed mediators was statistically significant (β = 0.035; 95%BCI: 0.028, 0.042; Supplementary Table S4). Disruption to daily activities and social interaction (IE = 0.021, 95%BCI: 0.016, 0.026) and financial hardship (IE = 0.013, 95%BCI: 0.011, 0.016) mediated the relationship between negative COVID-19-related experiences and depressive symptoms.
The moderated mediation model shows that stress management ability moderated the IE of disruption to daily activities and social interaction and financial hardship (Table 2). The interaction terms were statistically significant (DDASI: β = −0.119, SE = 0.018, p < 0.0001; FH: β = 0.042, SE = 0.017, p = 0.012), and confirmed by the IMM (DDASI: −0.005; 95%BCI: −0.007, −0.003; FH: 0.002; 95%BCI: 0.0001, 0.005). Stress management ability buffered the IE of disruption to daily activities and social interaction but enhanced the IE of financial hardship on depressive symptoms (Supplementary Table S5; Supplementary Figure S2a). Social support moderated the IE of financial hardship on depressive symptoms. The interaction term was statistically significant (β = −0.070, SE = 0.017, p < 0.0001; IMM = −0.004; 95%BCI: −0.006, −0.002), indicating that social support buffered the IE of financial hardship on depressive symptoms.
3.4 Anxiety symptoms
The parallel mediation model shows that the total IE of the set of proposed mediators was statistically significant (β = 0.023; 95%BCI: 0.018, 0.028; Supplementary Table S6). Disruption to daily activities and social interaction (IE = 0.016, 95%BCI: 0.012, 0.020) and financial hardship (IE = 0.006, 95%BCI: 0.004, 0.008) mediated the relationship between negative COVID-19-related experiences and anxiety symptoms.
The moderated mediation model shows that stress management ability moderated the IE of disruption to daily activities and social interaction (Table 3). The interaction term was statistically significant (β = −0.065, SE = 0.018, p = 0.0003; IMM = -0.003; 95%BCI: −0.005, −0.001). Stress management ability buffered the IE of disruption to daily activities and social interaction on anxiety symptoms (Supplementary Table S7; Supplementary Figure S2a). Social support did not moderate any indirect effect.
4 Discussion
In early 2020, governments started to implement different public health measures ranging from physical distancing to full lockdowns to mitigate the spread of SARS-CoV-2. While the containment measures helped reduce COVID-19 spread, these events might also have had unintended adverse secondary effects negatively impacting on physical and mental health, causing financial hardship, and disrupting social interaction, employment, and medical care. In this study, we found that disruption to daily activities and social interaction, as well as financial hardship, mediated the relationship between negative COVID-19-related experiences and cancer survivors’ HRQoL and psychological distress. The results are consistent with prior research that reported negative impacts of the COVID-19 pandemic on psychosocial well-being and HRQoL in cancer survivors. For instance, a meta-analysis of studies examining mental health conditions among survivors during the pandemic revealed elevated levels of anxiety and depression (Ayubi et al., 2021). Furthermore, several studies showed the association between high financial burden and worse HRQoL among cancer survivors during the pandemic (Ayubi et al., 2021; Chen et al., 2021; Momenimovahed et al., 2021; Staehler et al., 2021; Muls et al., 2022). The current study contributes to our understanding of how major disruptive events, such as the COVID-19 pandemic, impact psychological distress and HRQoL in cancer survivors, by identifying potential intervention targets that may buffer the adverse effects of these acute and chronic global stressors.
Social support buffered the negative effect of financial hardship on HRQoL and depressive symptoms, while perceived stress management skills buffered the effect of disruption to daily activities on HRQoL, depressive and anxiety symptoms. Our findings align with previous research demonstrating a positive association between social support and HRQoL of cancer survivors (Gudina et al., 2021). Participants in our study may have benefitted from tangible or material support from friends and family during the COVID-19 pandemic, which likely provided some relief from financial difficulties. In addition, our results support research indicating that stress management interventions can improve cancer survivors’ psychological and physiological adaptation as well as clinical health outcomes (Antoni et al., 2023). Stress management skills may equip cancer survivors with coping mechanisms to handle disruptions (e.g., relaxation exercises, mindfulness), while also building resilience, fostering a positive outlook, and helping them focus on what can be controlled. Our findings underscore the importance of fostering strong social support networks and stress management skills to enhance the well-being of cancer survivors, particularly during times of crisis. Contrary to expectations, we also found that perceived stress management enhanced the negative effect of financial hardship on depression and social support enhanced the negative effect of disruption to daily activities and social interaction on HRQoL. Stress management skills may amplify the negative effects of financial hardship on depression by increasing awareness of financial difficulties, and promoting unrealistic expectations that these skills could mitigate completely the impact of financial strain. The latter finding, while seemingly contradictory, may indicate that cancer survivors who rely heavily on social support had greater sensitivity to disruptions in daily life and social interactions because they are accustomed to a certain level of assistance and stability. Future research should explore the nuanced roles of social support and stress management skills in different contexts to better understand their complex interactions and impacts on cancer survivors’ well-being.
Our findings showed that older cancer survivors reported less disruption to daily activities, less depressive and anxiety symptoms, and greater HRQoL. This finding is consistent with prior studies examining the impact of the COVID-19 pandemic on cancer survivors’ distress (Jeppesen et al., 2021; Koinig et al., 2021). Older survivors may have already become accustomed to restrictions in their daily life, and thus, they might be able to cope better with the additional restrictions imposed by the COVID-19 pandemic. Similar to previous studies, we also found that female cancer survivors reported worse HRQoL, greater psychosocial risk, and more depressive and anxiety symptoms (Jeppesen et al., 2021; Koinig et al., 2021). Compared to non-Hispanic Whites, Hispanics and non-Hispanic Blacks reported more anxiety symptoms, which is not surprising given racial-ethnic disparities in psychological distress prior to and during the COVID-19 pandemic (Wen et al., 2023).
Some work has documented that prevalence and mortality of COVID-19 infection were higher in traditionally vulnerable communities (Bambra et al., 2020; Maroko et al., 2020; Dioun et al., 2023). Although cancer survivors in high ADI (more disadvantaged area) reported statistically worse HRQoL, more depressive symptoms and financial hardship, and less disruption to daily life and social interaction, it should be noted that the magnitude of these differences were relatively small compared to other predictors. There is established evidence indicating that neighborhood disadvantage contributes to inequity in health outcomes through access to resources, environmental exposures, health behaviors, material deprivation, and psychological mechanisms among cancer patients (Chu et al., 2022). However, specific to subjective measures such as financial toxicity, several studies reported no difference in financial toxicities among cancer patients by SES (Esselen et al., 2023; Kieran et al., 2023). Although economic hardships resulting from the COVID-19 pandemic are well documented (Baddour et al., 2020), significant government funding and assistance, such as federal stimulus checks directed towards lower- and middle-income families, may have alleviated financial impacts of the pandemic (Garner et al., 2020; Kochhar and Sechopoulos, 2020).
This study has several limitations. First, although our sample was large, the survey participants were cancer patients recruited from two NCI-designated cancer centers. Also, the sample was somewhat homogenous regarding race and ethnicity. These sampling biases limit generalizability to more diverse cancer survivors cared for in other settings. Second, the study used ADI, secondary geospatial data, to assess SES and, therefore, may not have fully captured the actual socioeconomic adversity of survivors. Furthermore, information on the cancer treatment status of participants was not collected. These factors may influence the results and lead to more nuanced findings. Third, although the COVID-PPE questionnaire was developed by experts in psycho-oncology and psychometrically evaluated with over 10,000 cancer survivors, its concurrent validity has yet to be demonstrated. Last, the survey was conducted during the initial phases of the COVID-19 pandemic, potentially limiting generalizability to the later phases of the pandemic. Future work should evaluate long-term impacts of the COVID-19 pandemic across multiple psychosocial risks. Notwithstanding these limitations, our study suggests that negative COVID-19-related experiences put cancer survivors at greater risk for financial burden and disruption to daily activities and social interaction, which can have downstream effects on HRQoL and psychological distress. These negative effects were buffered by stress management skills and social support. Financial navigation, such as financial and legal counseling, and other types of psychological and social work interventions, including positive reappraisal or reframing and recommendation to maintain social contacts through social media or video calls, may be useful to mitigate financial burden and disruption to social interaction due to the pandemic.
4.1 Conclusion
In conclusion, greater negative COVID-19-related experiences were associated with higher depression and poor HRQoL. Financial hardship, disruption to daily activities and social interaction mediated the association between negative COVID-19-related experiences and anxiety, depression, and HRQoL, and perceived stress management skills and social support buffered these relationships. Augmentation of cancer support and financial counseling services may help cancer patients mitigate the adverse effects of major disruptive events and protect their well-being.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee (Institutional Review Board) of the University of Texas MD Anderson Cancer Center (IRB #2020-0508) and University of Miami Sylvester Comprehensive Cancer Center (IRB #202000450). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BN: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft. AN: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft. MA: Writing – review & editing. AO: Writing – review & editing. SP: Writing – review & editing. RW: Writing – review & editing. TG: Writing – review & editing. CH: Writing – review & editing. CU: Writing – review & editing. AP: Writing – review & editing. LC: Funding acquisition, Investigation, Project administration, Resources, Writing – review & editing. FP: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported in part by the National Institutes of Health (NIH) through University of Miami Sylvester Comprehensive Cancer Center’s Cancer Center Support Grant P30CA240139 and MD Anderson’s Cancer Center Support Grant P30CA016672, the Duncan Family Institute for Cancer Prevention and Risk Assessment, and the Richard E. Haynes Distinguished Professorship for Clinical Cancer Prevention at The University of Texas MD Anderson Cancer Center (L. Cohen). Blanca Noriega Esquives was supported by grant T32CA251064 (Penedo F. J. and Kobetz, E. MPIs). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Conflict of interest
Antoni and Penedo are paid consultants for Blue Note Therapeutics. Antoni is a paid consultant for Atlantis Healthcare.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1423106/full#supplementary-material
Abbreviations
ADI, Area deprivation index; DDASI, Disruption to daily activities and social interaction; FH, Financial hardship; HCD, Healthcare disruption; HRQoL, Health-related quality of life; NCE, Negative COVID-19 experiences; SMA, Stress management ability; SS, Social support.
References
Antoni, M. H., Moreno, P. I., and Penedo, F. J. (2023). Stress management interventions to facilitate psychological and physiological adaptation and optimal health outcomes in Cancer patients and survivors. Annu. Rev. Psychol. 74, 423–455. doi: 10.1146/annurev-psych-030122-124119
Ayubi, E., Bashirian, S., and Khazaei, S. (2021). Depression and anxiety among patients with Cancer during COVID-19 pandemic: a systematic review and Meta-analysis. J. Gastrointest. Cancer 52, 499–507. doi: 10.1007/s12029-021-00643-9
Baddour, K., Kudrick, L. D., Neopaney, A., Sabik, L. M., Peddada, S. D., Nilsen, M. L., et al. (2020). Potential impact of the COVID-19 pandemic on financial toxicity in cancer survivors. Head Neck 42, 1332–1338. doi: 10.1002/hed.26187
Bambra, C., Riordan, R., Ford, J., and Matthews, F. (2020). The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 74, 964–968. doi: 10.1136/jech-2020-214401
Becerril-Gaitan, A., Vaca-Cartagena, B. F., Ferrigno, A. S., Mesa-Chavez, F., Barrientos-Gutiérrez, T., Tagliamento, M., et al. (2022). Immunogenicity and risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection after coronavirus disease 2019 (COVID-19) vaccination in patients with cancer: a systematic review and meta-analysis. Eur. J. Cancer 160, 243–260. doi: 10.1016/j.ejca.2021.10.014
Brose, J. M., Willis, E., and Morgan, D. D. (2023). The intentional pursuit of everyday life while dying: a longitudinal qualitative study of working-aged adults living with advanced cancer. Palliat. Med. 37, 1210–1221. doi: 10.1177/02692163231180911
Burki, T. K. (2020). Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. 21, 629–630. doi: 10.1016/S1470-2045(20)30217-5
Chen, Y. S., Zhou, Z. N., Glynn, S. M., Frey, M. K., Balogun, O. D., Kanis, M., et al. (2021). Financial toxicity, mental health, and gynecologic cancer treatment: the effect of the COVID-19 pandemic among low-income women in new York City. Cancer 127, 2399–2408. doi: 10.1002/cncr.33537
Chu, J. N., Canchola, A. J., Keegan, T. H. M., Nickell, A., Oakley-Girvan, I., Hamilton, A. S., et al. (2022). Evaluating the impact of social and built environments on health-related quality of life among Cancer survivors. Cancer Epidemiol. Biomarkers Prev. 31, 161–174. doi: 10.1158/1055-9965.EPI-21-0129
Dioun, S., Chen, L., Hillyer, G., Tatonetti, N. P., May, B. L., Melamed, A., et al. (2023). Association between neighborhood socioeconomic status, built environment and SARS-CoV-2 infection among cancer patients treated at a Tertiary Cancer Center in New York City. Cancer Rep. (Hoboken) 6:e1714. doi: 10.1002/cnr2.1714
Esselen, K. M., Baig, R. A., Gompers, A., Stack-Dunnbier, H., Hacker, M. R., and Jang, J. W. (2023). Factors associated with increased financial toxicity after the completion of radiation treatment for gynecologic cancer. Support Care Cancer 31:388. doi: 10.1007/s00520-023-07849-6
Garner, T.I., Safir, A., and Schild, J. (2020). Receipt and use of stimulus payments in the time of the Covid-19 pandemic.
Ghazal, L. V., Abrahamse, P., Ward, K. C., Morris, A. M., Hawley, S. T., and Veenstra, C. M. (2023). Financial toxicity and its association with health-related quality of life among Partners of Colorectal Cancer Survivors. JAMA Netw. Open 6:e235897. doi: 10.1001/jamanetworkopen.2023.5897
Gudina, A. T., Cheruvu, V. K., Gilmore, N. J., Kleckner, A. S., Arana-Chicas, E., Kehoe, L. A., et al. (2021). Health related quality of life in adult cancer survivors: importance of social and emotional support. Cancer Epidemiol. 74:101996. doi: 10.1016/j.canep.2021.101996
Guidry, J. P. D., Miller, C. A., Perrin, P. B., Carlyle, K. E., Savage, M. W., Sheppard, V. B., et al. (2023). Pandemic coping and COVID-19 preventive behaviors among cancer survivors. Patient Educ. Couns. 112:107716. doi: 10.1016/j.pec.2023.107716
Harris, P. A., Taylor, R., Minor, B. L., Elliott, V., Fernandez, M., O'Neal, L., et al. (2019). The REDCap consortium: building an international community of software platform partners. J. Biomed. Inform. 95:103208. doi: 10.1016/j.jbi.2019.103208
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., and Conde, J. G. (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381. doi: 10.1016/j.jbi.2008.08.010
Hayes, A. F. (2022). Introduction to mediation, moderation, and conditional process analysis. A regression-based approach. New York, NY: Guilford Press.
Hayes, A. F., and Rockwood, N. J. (2020). Conditional process analysis: concepts, computation, and advances in the modeling of the contingencies of mechanisms. Am. Behav. Sci. 64, 19–54. doi: 10.1177/0002764219859633
Jeppesen, S. S., Bentsen, K. K., Jørgensen, T. L., Holm, H. S., Holst-Christensen, L., Tarpgaard, L. S., et al. (2021). Quality of life in patients with cancer during the COVID-19 pandemic - a Danish cross-sectional study (COPICADS). Acta Oncol. 60, 4–12. doi: 10.1080/0284186X.2020.1830169
Kieran, R., Moloney, C., Alken, S., Corrigan, L., Gallagher, D., Grant, C., et al. (2023). Patient knowledge, personal experience, and impact of the first wave of the COVD-19 pandemic in an Irish oncology cohort. Ir. J. Med. Sci. 192, 533–540. doi: 10.1007/s11845-022-02999-8
Kind, A. J. H., and Buckingham, W. R. (2018). Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N. Engl. J. Med. 378, 2456–2458. doi: 10.1056/NEJMp1802313
Kochhar, R., and Sechopoulos, R. (2020). COVID-19 pandemic pinches finances of America's lower- and middle- income families [online]. Pew Research Center. Available at: https://www.pewresearch.org/social-trends/2022/04/20/covid-19-pandemic-pinches-finances-of-americas-lower-and-middle-income-families/ (Accessed August 9, 2023).
Koinig, K. A., Arnold, C., Lehmann, J., Giesinger, J., Köck, S., Willenbacher, W., et al. (2021). The cancer patient's perspective of COVID-19-induced distress-a cross-sectional study and a longitudinal comparison of HRQOL assessed before and during the pandemic. Cancer Med. 10, 3928–3937. doi: 10.1002/cam4.3950
Ligumsky, H., Dor, H., Etan, T., Golomb, I., Nikolaevski-Berlin, A., Greenberg, I., et al. (2022). Immunogenicity and safety of BNT162b2 mRNA vaccine booster in actively treated patients with cancer. Lancet Oncol. 23, 193–195. doi: 10.1016/S1470-2045(21)00715-4
Lu, S. C., Porter, I., Valderas, J. M., Harrison, C. J., and Sidey-Gibbons, C. (2023). Effectiveness of routine provision of feedback from patient-reported outcome measurements for cancer care improvement: a systematic review and meta-analysis. J. Patient Rep. Outcomes 7:54. doi: 10.1186/s41687-023-00578-8
Maroko, A. R., Nash, D., and Pavilonis, B. T. (2020). COVID-19 and inequity: a comparative spatial analysis of new York City and Chicago hot spots. J. Urban Health 97, 461–470. doi: 10.1007/s11524-020-00468-0
Momenimovahed, Z., Salehiniya, H., Hadavandsiri, F., Allahqoli, L., Günther, V., and Alkatout, I. (2021). Psychological distress among Cancer patients during COVID-19 pandemic in the world: a systematic review. Front. Psychol. 12:682154. doi: 10.3389/fpsyg.2021.682154
Muls, A., Georgopoulou, S., Hainsworth, E., Hartley, B., O'Gara, G., Stapleton, S., et al. (2022). The psychosocial and emotional experiences of cancer patients during the COVID-19 pandemic: a systematic review. Semin. Oncol. 49, 371–382. doi: 10.1053/j.seminoncol.2022.08.001
Naranbhai, V., Pernat, C. A., Gavralidis, A., St Denis, K. J., Lam, E. C., Spring, L. M., et al. (2022). Immunogenicity and Reactogenicity of SARS-CoV-2 vaccines in patients with Cancer: the CANVAX cohort study. J. Clin. Oncol. 40, 12–23. doi: 10.1200/JCO.21.01891
National Cancer Institute (2024). NCI dictionary of Cancer terms [online]. Available at: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/survivor (Accessed August 12, 2024).
Nelson, B., and Kaminsky, D. B. (2020). COVID-19's multipronged attack on mental health: months of uncertainty and threats to health, social, and financial security have contributed to intense anxiety, depression, posttraumatic stress disorder, and even suicide. Here, in part 2 of a 2-part series, we investigate the pandemic's growing mental health toll on the general public and efforts to address it. Cancer Cytopathol. 128, 679–680. doi: 10.1002/cncy.22364
Noora, S. (2020). Detecting multicollinearity in regression analysis. Am. J. Appl. Math. Stat. 8, 39–42. doi: 10.12691/ajams-8-2-1
Pearman, T., Yanez, B., Peipert, J., Wortman, K., Beaumont, J., and Cella, D. (2014). Ambulatory cancer and US general population reference values and cutoff scores for the functional assessment of cancer therapy. Cancer 120, 2902–2909. doi: 10.1002/cncr.28758
Perry, L. M., Peipert, J. D., Kircher, S. M., Cantoral, J., Penedo, F. J., and Garcia, S. F. (2023). Adverse COVID-19 experiences and health-related quality of life in cancer survivors: indirect effects of COVID-19-related depression and financial burden. J. Patient Rep. Outcomes 7:71. doi: 10.1186/s41687-023-00601-y
Saez-Clarke, E., Otto, A. K., Prinsloo, S., Natori, A., Wagner, R. W., Gomez, T. I., et al. (2023). Development and initial psychometric evaluation of a COVID-related psychosocial experiences questionnaire for cancer survivors. Qual. Life Res. 32, 3475–3494. doi: 10.1007/s11136-023-03456-4
Staehler, M. D., Battle, D. J., Bergerot, C. D., Pal, S. K., and Penson, D. F. (2021). COVID-19 and financial toxicity in patients with renal cell carcinoma. World. J. Urol. 39, 2559–2565. doi: 10.1007/s00345-020-03476-6
Steel, J. L., Amin, A., Peyser, T., Olejniczak, D., Antoni, M., Carney, M., et al. (2022). The benefits and consequences of the COVID-19 pandemic for patients diagnosed with cancer and their family caregivers. Psychooncology 31, 1003–1012. doi: 10.1002/pon.5891
Tan, Y., Qin, M., Liao, B., Wang, L., Chang, G., Wei, F., et al. (2023). Effectiveness of peer support on quality of life and anxiety in breast cancer patients: a systematic review and meta-analysis. Breast Care (Basel) 18, 49–59. doi: 10.1159/000527849
Velasco-Durantez, V., Jimenez-Fonseca, P., Martín Abreu, C. M., Ghanem, I., González Moya, M., Asensio, E., et al. (2022). Resilience, social support, and anxious preoccupation in patients with advanced cancer during COVID-19 pandemic. Cancer Investig. 40, 475–482. doi: 10.1080/07357907.2022.2067864
Wen, M., Shi, L., Zhang, D., Li, Y., Chen, Z., Chen, B., et al. (2023). Racial-ethnic disparities in psychological distress during the COVID-19 pandemic in the United States: the role of experienced discrimination and perceived racial bias. BMC Public Health 23:957. doi: 10.1186/s12889-023-15912-4
Keywords: cancer survivors, COVID-19 pandemic, financial hardship, health-related quality of life, moderated mediation analysis, psychological distress
Citation: Noriega Esquives BS, Natori A, Antoni MH, Otto AK, Prinsloo S, Wagner RW, Gomez TI, Hathaway CA, Ulrich CM, Peoples AR, Cohen L and Penedo FJ (2024) The impact of negative COVID-19 experiences on cancer survivors’ health-related quality of life and psychological distress: a moderated mediation model. Front. Psychol. 15:1423106. doi: 10.3389/fpsyg.2024.1423106
Edited by:
Julia Roick, Technical University of Munich, GermanyReviewed by:
Miriam Grapp, Heidelberg University, GermanyKwabena Amo-Antwi, Kwame Nkrumah University of Science and Technology, Ghana
Copyright © 2024 Noriega Esquives, Natori, Antoni, Otto, Prinsloo, Wagner, Gomez, Hathaway, Ulrich, Peoples, Cohen and Penedo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Frank J. Penedo, ZnBlbmVkb0BtaWFtaS5lZHU=
†These authors have contributed equally to this work and share first authorship
‡These authors share senior authorship
 Blanca S. Noriega Esquives
Blanca S. Noriega Esquives Akina Natori
Akina Natori Michael H. Antoni
Michael H. Antoni Amy K. Otto
Amy K. Otto Sarah Prinsloo
Sarah Prinsloo Richard W. Wagner5
Richard W. Wagner5 Anita R. Peoples
Anita R. Peoples Frank J. Penedo
Frank J. Penedo