- School of Nursing, Guangzhou Medical University, Guangzhou, Guangdong, China
Background: The majority of elderly individuals prefer to spend their final days in the Intensive Care Unit (ICU). ICU nurses are key providers in hospice care, and their attitudes toward death influence the quality of end-of-life nursing. Positive psychology emphasizes promoting positive attitudes toward death. A sense of meaning in life and resilience are critical aspects of positive psychology, which are essential for shaping ICU nurses’ attitudes toward death.
Objective: This study aims to investigate whether a sense of meaning in life indirectly affects attitudes toward death through the mediation of resilience.
Method: A total of 212 ICU nurses from four tertiary general hospitals in Guangdong and Fujian provinces, China, participated in this study. They completed an online questionnaire, including the Death Attitude Profile-Revised, the Connor-Davidson Resilience Scale, and the China Meaning in Life Questionnaire for ICU nurses.
Results: ICU nurses scored highest in natural acceptance (3.26 ± 0.53), followed by escaping acceptance (2.54 ± 0.59), and fear of death (2.53 ± 0.78). The proposed model fit the data well. Both the presence of meaning and the search for meaning were positive predictors of resilience (β = 0.313, p < 0.05; β = 0.256, p < 0.05). Resilience, the presence of meaning, and the search for meaning positively predicted natural acceptance (β = 0.299, p < 0.05; β = 0.294, p < 0.05; β = 0.177, p < 0.05). Conversely, these factors negatively predicted fear of death (β = −0.179, p < 0.05; β = −0.251, p < 0.05; β = −0.192, p < 0.05) and escaping acceptance (β = −0.208, p < 0.05; β = −0.208, p < 0.05; β = −0.219, p < 0.05). Mediation analysis indicated that resilience had a partial mediating role.
Conclusion: The presence of meaning and the search for meaning influence attitudes toward death, with resilience serving as a partial mediator. It is recommended that nursing administrators consider ICU nurses’ attitudes toward death and emphasize the importance of meaning in life and resilience in death education. This approach can help protect the psychological well-being of ICU nurses, promote a deeper understanding of life’s meaning, and develop a scientific perspective on death. Such measures are crucial for providing better humanistic care and psychological comfort to terminally ill patients and their families, thereby improving the quality of end-of-life care.
1 Introduction
With advancements in medical technology, increased average life expectancy, and improved living standards, hospice care focusing on the “quality of dying” has gained attention. In 2020, 18.7% of China’s population will be elderly, and many with chronic illnesses and malignant tumors may qualify for hospice care. Hospice care services in China face significant challenges (Zhihong and Yan, 2023). Studies indicate that an increasing number of elderly people are spending their final month in the intensive care unit (ICU) (Cook and Rocker, 2014; Khandelwal and Curtis, 2014). ICU patients often have severe conditions and a higher mortality risk. Data shows that ICU patient mortality rates abroad range from 6.4 to 40.0% (Sakr et al., 2012; Brinkman et al., 2013; Mezzaroba et al., 2022), while in China, the rates vary between 12.8 and 45.6% (Pengcheng and Tian, 2023). Consequently, ICU nurses bear significant responsibility in providing end-of-life care. Beyond improving their advanced life support skills, they must also develop a proper perspective on life and death. Due to traditional Chinese culture, discussing death is often avoided. Nurses, too, may feel anxious and struggle to confront and accept death (Cardoso et al., 2021; He and Li, 2022). In 2015, the Economist Intelligence Unit (EIU) reported that the quality of life for terminally ill patients in mainland China was relatively low (He et al., 2023). Nurses, as primary hospice care providers, play a crucial role in the quality of life of these patients. Their attitudes toward death can influence their approach to hospice care and affect their nursing behavior toward terminally ill patients (Costello, 2006; Meng et al., 2019; Mastroianni et al., 2015; Zhang et al., 2019). Nurses with objective and impartial views on death and the value of life naturally understand the significance of hospice care, allowing them to meet the nursing needs of terminally ill patients and their families with a positive hospice care attitude, providing humanistic care and psychological comfort, which helps improve the quality of end-of-life care services (Meng et al., 2019). Additionally, evidence suggests that a scientific attitude toward death is essential for ICU nurses to provide effective hospice care (Cho and Kang, 2017; Liu, 2023). Therefore, strengthening the development of ICU nurses’ attitudes toward death is vital.
Attitude toward death refers to an individual’s consistent and evaluative psychological disposition toward death, encompassing five components: fear of death, death avoidance, natural acceptance, approach acceptance, and escape acceptance (Dezutter et al., 2009). Recently, nursing management has increasingly focused on nurses’ attitudes toward death due to its relation to their work competency, coping strategies regarding death, physical and mental health, and professional conduct. Research indicates that nurses who naturally accept death are more likely to demonstrate positive caring behaviors (Braun et al., 2010; Meng et al., 2019; Zhang et al., 2019). In contrast, those who avoid or fear death often face conflicts between their personal and professional roles, leading to a reduced ability to provide spiritual and psychological support to patients and their families (Peters et al., 2013; Kudubes et al., 2021). This suggests that a negative attitude toward death can adversely affect the quality of care. Furthermore, positive attitudes toward death correlate with higher levels of personal achievement and self-worth among nurses, which in turn leads to greater job satisfaction and improved care quality (Jing et al., 2012). Studies have shown that ICU nurses are frequently exposed to near-death or death events, which can lead to anxiety, loss, fear, and even post-traumatic stress disorder (PTSD). This exposure can increase the likelihood of quitting, complicating the provision of end-of-life care (Cho and Kang, 2017; Liu, 2023; Lian et al., 2022; Arli, 2023). Additionally, Braun et al. (2010) suggested that an individual’s attitude toward death is often influenced by their understanding of death. Ay and Öz (2019) found that the more nurses comprehend concepts related to death, such as hospice care, death, and euthanasia, the more positive their attitude toward death becomes. Consequently, death education has become a crucial method for promoting a correct attitude toward death (Testoni et al., 2018). With an aging population, China urgently needs to implement death education for ICU nurses and improve their training in perspectives on life and death to meet end-of-life care demands. However, death education in China began late, has an overly complex curriculum system, and lacks sufficient research on ICU nurses’ attitudes toward death and related factors. Therefore, it is necessary to explore further the influencing mechanisms of factors related to ICU nurses’ attitudes toward death to establish effective and targeted death education programs for ICU nurses.
Life ultimately culminates in death, which highlights the finite nature of existence. People increasingly recognize this and actively contemplate its purpose and significance (Testoni et al., 2018). The sense of meaning in life involves individuals’ subjective assessment of life’s goals and meaning, as well as their sense of achievement and satisfaction. This concept is divided into two parts: the presence of meaning and the search for meaning (Steger et al., 2006). Durlak (1972) suggested that life’s meaning is a vital component of mental health. Individuals with a strong sense of meaning in life can increase resilience, reduce the fear of dying, and approach it with a positive attitude. Studies have shown a significant positive relationship between meaning in life and the natural acceptance of death among nurses (Cardoso et al., 2021). The stronger it is, the more likely individuals are to view and face death rationally (Ran et al., 2018). Chinese researchers have found that frequent interactions with dying patients and their families provide oncology nurses with opportunities for self-reflection and contemplation of life’s meaning, which shifts their perspectives and attitudes toward death (Wang, 2022). Conversely, a strong sense of meaning in life negatively predicts fear of death and avoidance acceptance among nurses (Ran et al., 2018; Xiaomin et al., 2021). For nurses who may experience emotional distress, applying the meaning of life when caring for terminal patients is particularly important (Zheng et al., 2015). The evidence suggests a significant correlation between the meaning of life and attitudes toward death. Therefore, many nursing managers view the sense of meaning in life as essential for shaping attitudes toward death. However, no research has yet examined the relationship between ICU nurses’ sense of meaning in life and their attitudes toward death. Hence, the hypothesis is proposed that there is a correlation between ICU nurses’ sense of meaning in life and their attitudes toward death.
Resilience refers to an individual’s ability to adapt when facing stress and adversity (White et al., 2008). Nurse resilience is characterized as a complex, dynamic process that helps nurses actively adjust to workplace stressors, prevent psychological harm, and maintain high-quality patient care (Cooper et al., 2020). Schreiber et al. (2019) found that resilience can protect nurses caring for infected patients from various psychological and mental health issues. Edo-Gual et al. (2015) emphasized that resilience is a crucial emotional skill for coping with death. Jiao et al. (2023) reported that medical students’ resilience predicts their attitudes toward death, with those having higher resilience more likely to view death positively and face various challenges and stresses courageously. Wang (2022) showed that oncology nurses with strong resilience could maintain a healthy psychological state when dealing with dying patients and their families. These studies suggest that resilience positively influences attitudes toward death. Compared to nurses in general departments, ICU nurses experience greater pressure from end-of-life care and psychological stress throughout their careers and thus need higher resilience to develop a proper attitude toward death. Therefore, we predict that ICU nurses’ resilience will be a predictor of their attitude toward death in this study.
The sense of meaning in life and psychological resilience are key elements of positive psychology, acting as protective factors for mental health. A strong sense of meaning in life can promote psychological resilience by reducing uncertainty and related distress (Du et al., 2017; Yela et al., 2020; Ostafin and Proulx, 2020). According to the dynamic model of psychological resilience, resilience helps individuals adapt well by utilizing all protective resources (Connor and Davidson, 2003). Folkman (1997) suggested that resilience can influence the relationship between the sense of meaning in life and mental health. For example, Huayu and Guangming (2019) found that college students who actively seek meaning in life are more likely to use their psychological resilience to overcome boredom, thereby adapting better to their academic lives. Ya'nan and Xiaoyu, 2023 reported that final-year medical students who struggle to find meaning in life may remain resilient yet pessimistic, leading to anxiety and impeding their future professional growth. Han et al. (2023) demonstrated that nurses’ psychological resilience improved their post-traumatic growth (PTG) through a sense of meaning in life during the COVID-19 pandemic. This evidence indicates that the sense of meaning in life can promote positive psychological states and mitigate negative psychological disturbances through psychological resilience. Therefore, we anticipate that resilience will mediate the relationship between the sense of meaning in life and the attitude toward death among ICU nurses.
Based on the literature review, this study aims to examine the relationships between meaning in life, resilience, and attitudes toward death, and to determine if resilience mediates the relationship between meaning in life and attitudes toward death. Understanding these relationships is crucial for developing strategies in death education to improve ICU nurses’ attitudes toward death.
2 Materials and methods
2.1 Study design and participants
ICU nurses were selected through convenience sampling from four tertiary grade A hospitals in Fujian and Guangdong provinces, China. The inclusion criteria were: (1) ICU nurses holding a qualification certificate from the People’s Republic of China, and (2) having worked in the intensive care unit for more than 1 year and agreeing to participate. Nurses in training and those on leave were excluded. According to the Kendall sample size estimation method, the sample size is generally 5 ~ 10 times the number of items. With 20 items in this study and a 10% attrition rate, the sample size range was 110 ~ 220. Additionally, considering that structural equation modeling requires a sample size of more than 200, a total of 216 questionnaires were collected, with 212 valid responses (effective response rate: 98.15%).
2.2 Data collection
The study was conducted in Fujian and Guangdong Provinces, China, from July to August 2022. Prior to data collection, nursing managers from the four tertiary hospitals were contacted and briefed on the study’s objectives, requesting their assistance with the survey. An online questionnaire platform1 was used for data collection. The link to the online questionnaire was distributed to the WeChat group of ICU nurses working at the four hospitals. Researchers explained the study’s objectives to the participants, assured them of confidentiality, and informed them about the time required to complete the questionnaire (approximately 10 ~ 15 min). Upon agreeing to participate, informed consent was obtained, and participants completed the Meaning in Life Questionnaire, the Resilience Scale, and the Death Attitude Profile-Revised.
2.2.1 General characteristics questionnaire
The general information questionnaire was designed by the researchers and included details such as gender, age, marital status, fertility, academic status, years of work, title, religious belief, whether participants had received education on death and life sensitivity, and whether the hospital intended to provide education on death and vitality.
2.2.2 Meaning in life questionnaire
The Meaning in Life Questionnaire (MLQ) was created by Steger et al. (2006). This scale consists of 10 items divided into two subscales: the presence of meaning (e.g., “I understand the meaning of my life”) and the search for meaning (e.g., “I am looking for a purpose or mission in my life”), each containing 5 items. This study used the Chinese version of the MLQ revised by Mengcheng and Xiaoyang (2008). Items are rated on a Likert 7 scale, ranging from 1 (completely unsatisfactory) to 7 (completely satisfactory), with the second item reverse scored. The total score ranges from 10 to 70, with higher scores indicating a greater sense of meaning in life. In this study, the Cronbach’s α coefficients for the two subscales were 0.92 and 0.887, respectively.
2.2.3 Resilience scale
The Resilience Scale, developed by Connor and Davidson (2003), includes three dimensions: tenacity (13 items), strength (8 items), and optimism (4 items). Participants rate items on a 5-point Likert scale (from 0 = “never” to 4 = “always”). The total score ranges from 0 to 100 points, with higher scores indicating greater resilience. The Chinese version of the Resilience Scale has demonstrated good reliability and has been validated by multiple studies (Meng et al., 2019; Cheng et al., 2020). In this study, the scale showed strong reliability, with a Cronbach’s α of 0.942.
2.2.4 Death attitude profile-revised
The Death Attitude Profile-Revised was developed by Wong et al. (1994). This study utilized the Chinese version of the Death Attitude Profile-Revised (Zhu and Shi, 2011) to assess ICU nurses’ attitudes toward death. The scale comprises 25 items across 5 subscales: fear of death, death avoidance, escape acceptance, neutral acceptance, and approach acceptance. A Likert 4-point scale is used (from 1 = “strongly disagree” to 4 = “strongly agree”). Scores for each dimension are averaged by the number of items, and the scale does not calculate a total score but rather interprets attitudes based on individual dimension scores. Higher scores indicate a stronger tendency towards the attitude represented by each dimension. In this study, Cronbach’s α for the five subscales ranged from 0.765 to 0.885.
2.3 Statistical analysis
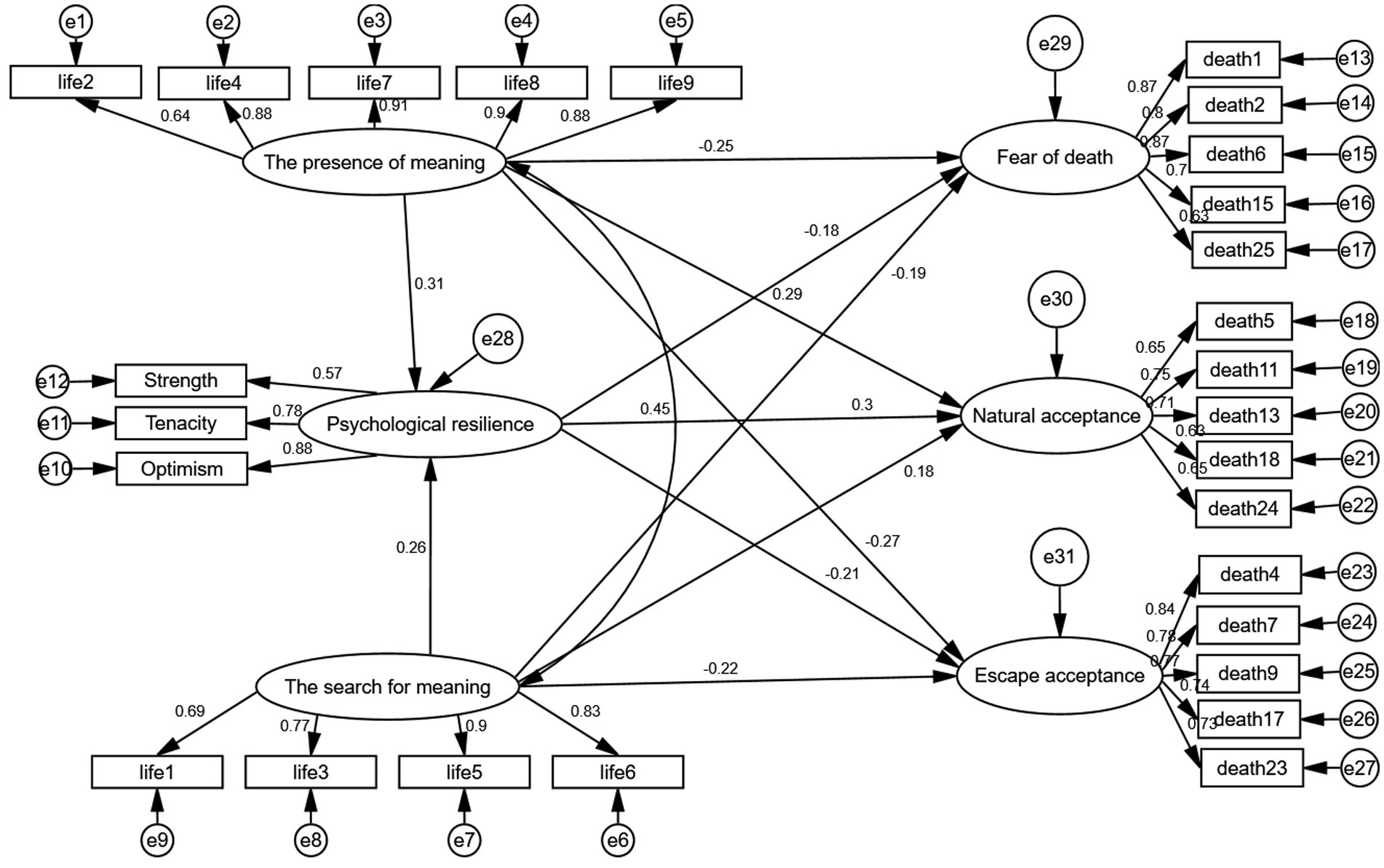
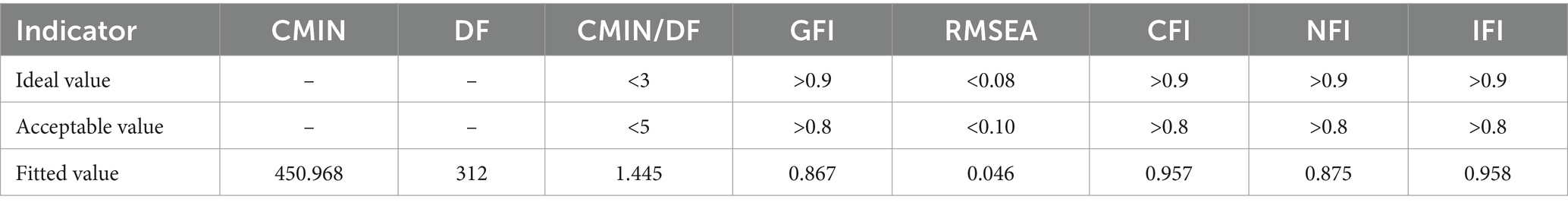
Statistical analysis was conducted using SPSS 25.0. The mean ± standard deviation was used to describe the levels of each variable, and Pearson’s correlation was employed to examine the relationships between variables. AMOS 26.0 was utilized to establish the structural equation model to explore the internal relationships and pathways between the sense of meaning in life, resilience, and attitude toward death. Differences were considered statistically significant at p < 0.05. The conceptual model is illustrated in Figure 1. The model’s fitness was evaluated using several indices: Chi-Square Minimum (CMIN), Degrees of Freedom (DF), the ratio of Chi-Square Minimum to Degrees of Freedom (CMIN/DF), Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), Incremental Fit Index (IFI), Goodness of Fit Index (GFI), and Normed Fit Index (NFI). The significance of the mediation effect was tested using Bootstrap, with a 95% confidence interval (CI) for the mediation effect calculated by sampling 2,000 times from the original data through repeated random sampling.
3 Results
3.1 General characteristics of the participants
In the final valid sample, women constituted 90.1%, while men made up 9.9%. Regarding age distribution, the sample primarily consisted of ICU nurses over 25 years old. In this study, 66% of the ICU nurses had a bachelor’s or graduate degree, 73.5% were married, 64.6% had children, 37.2% held positions as supervisor nurses or higher, and 43.9% had more than 10 years of work experience. Additionally, 21.2% of ICU nurses reported having religious beliefs. While 81.1% of ICU nurses expressed a desire for hospitals to offer education on death and the meaning of life, only 31.1% had actually received such education (Table 1).
3.2 Descriptive statistics and correlation analysis
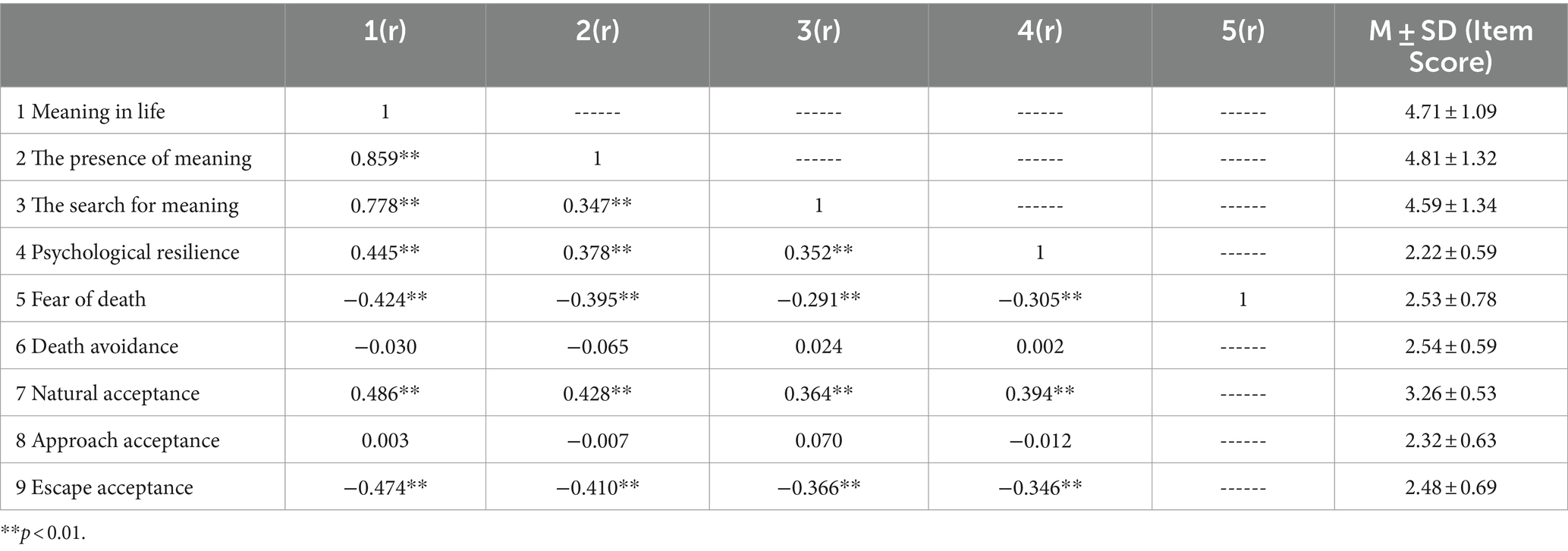
Table 2 presents the averages, standard deviations, and correlation coefficients for each variable in this study. Comparing the scores of the DAP-R five dimensions revealed that ICU nurses’ attitudes toward death were most aligned with natural acceptance (3.26 ± 0.53), followed by avoidance acceptance (2.54 ± 0.59), and fear of death (2.53 ± 0.78). Correlation analysis results indicated that the meaning of life (both presence of meaning and search for meaning) and psychological resilience were positively correlated with natural acceptance. Conversely, the meaning of life (presence of meaning and search for meaning) and psychological resilience were negatively correlated with fear of death and escape acceptance.
3.3 Mediating effect analysis
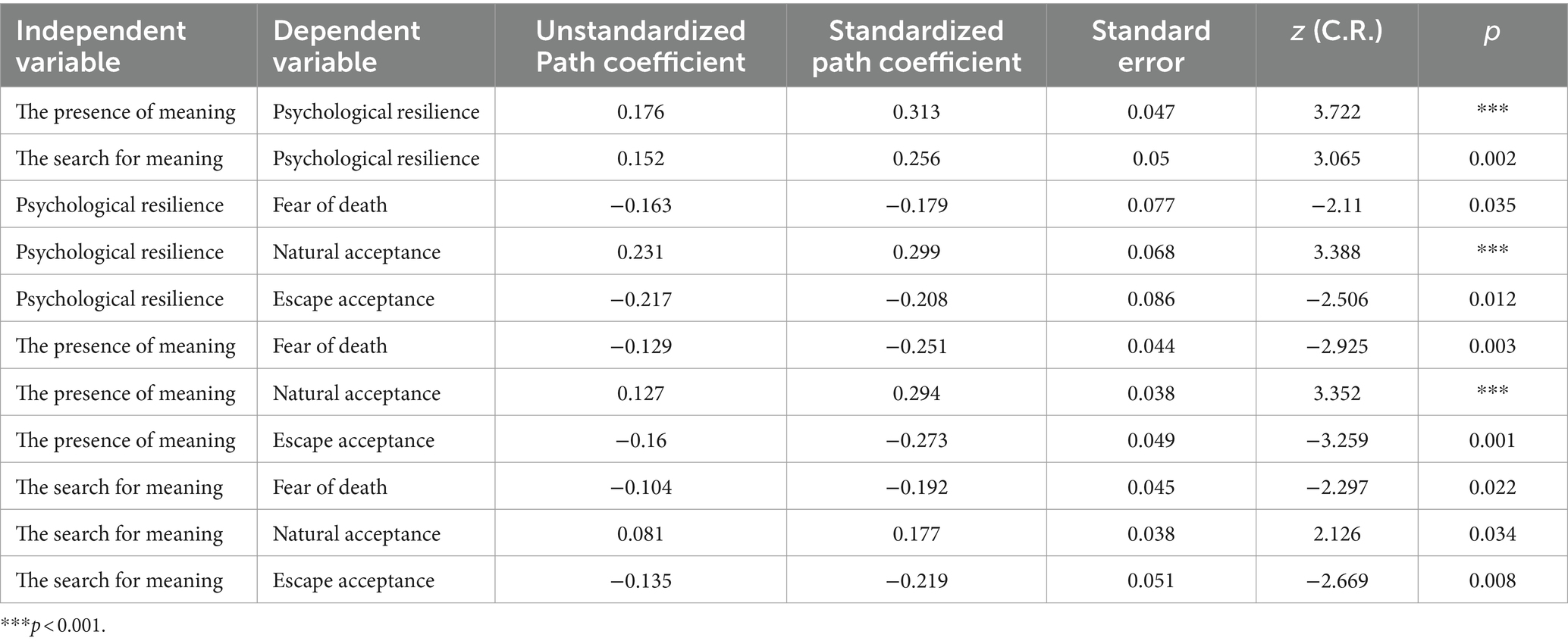
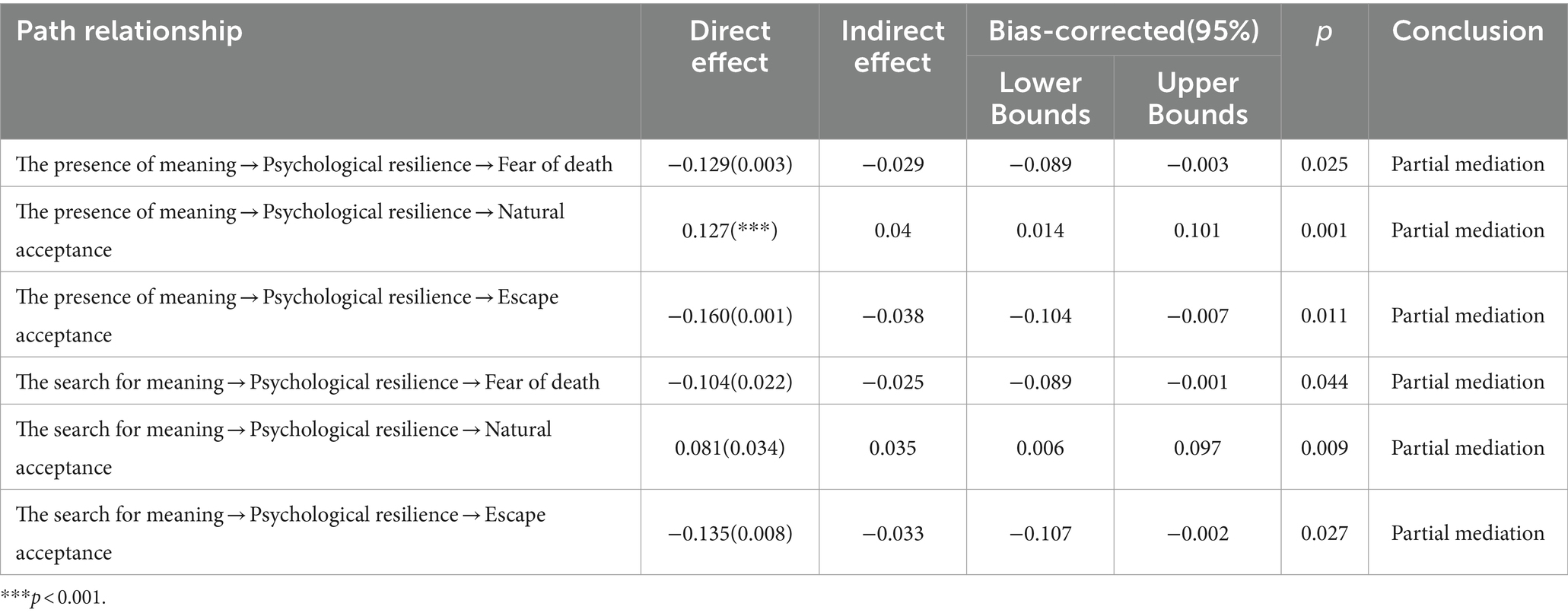
A structural equation model was constructed based on literature reviews and correlation analysis to examine the mediating role of psychological resilience in the relationship between the meaning of life (both presence of meaning and search for meaning) and attitudes toward death (natural acceptance, fear of death, and escape acceptance). The model results (Figure 1) indicate that psychological resilience did not significantly mediate the relationship between the meaning of life, death avoidance, and approach acceptance; only results for natural acceptance, fear of death, and escape acceptance were reported. The model showed a good fit with the data (CMIN/DF = 1.445, GFI = 0.867, RMSEA = 0.046, CFI = 0.957, NFI = 0.875, and IFI = 0.958), indicating a satisfactory fit (Table 3). The model revealed positive predictive relationships between meaning in life (presence of meaning and search for meaning) and psychological resilience (β = 0.313, p < 0.01; β = 0.256, p < 0.05); between meaning in life (presence of meaning and search for meaning) and psychological resilience and natural acceptance (β = 0.299, p < 0.05; β = 0.294, p < 0.05; β = 0.177, p < 0.05); and negative predictive relationships between meaning in life (presence of meaning and search for meaning) and psychological resilience and death avoidance (β = −0.179, p < 0.05; β = −0.251, p < 0.05; β = −0.192, p < 0.05) and approach acceptance (β = −0.208, p < 0.05; β = −0.208, p < 0.05; β = −0.219, p < 0.05) (Table 4).
The Bootstrap method was used to estimate confidence intervals. By repeating 2,000 samples and calculating 95% confidence intervals, the results showed that the six paths’ 95% confidence intervals did not include 0, indicating statistical significance. This confirmed that resilience partially mediated the relationship between the meaning of life (presence of meaning and search for meaning) and attitudes toward death (natural acceptance, fear of death, and escape acceptance). Detailed test results are presented in Table 5.
4 Discussion
This study investigated the impact of the presence of meaning and the search for meaning on natural acceptance, escape acceptance, and fear of death, respectively, while examining the partial mediating role of resilience. The findings are valuable for nursing managers to improve and expand the death education curriculum, aiding ICU nurses in better understanding and dealing with death.
The study compared the average scores across the five dimensions of death attitude and found that ICU nurses mainly displayed natural acceptance (3.26 ± 0.53), escape acceptance (2.54 ± 0.59), and fear of death (2.53 ± 0.78). ICU nurses tend to exhibit natural acceptance, viewing death as an inevitable part of life without fearing or welcoming it. This perspective may stem from their medical background and frequent encounters with death, allowing for a more logical view of life and death (Cardoso et al., 2021). Additionally, ICU nurses scored relatively high on escape acceptance. Zhu and Shi (2010) indicated that physical health often prompts deep reflections on death and life’s value. When experiencing extreme pain without a cure, individuals might see death as the final escape from suffering (Jinling et al., 2020). Therefore, it is speculated that ICU nurses’ tendency to escape acceptance of death might relate to the critical condition and poor prognosis of ICU patients. Furthermore, ICU nurses also experience a certain level of fear of death. According to Terror Management Theory, fear of death is a fundamental human fear that directly influences attitudes toward death (Lieberman, 2004; Yu et al., 2022). Thus, the fear of death among ICU nurses may be an instinctive response to facing death. Overall, ICU nurses’ attitudes toward death are characterized by natural acceptance, escape acceptance, and fear of death, reflecting various cognitive and emotional responses to death. Research indicates a significant correlation between nurses’ attitudes toward death and their perspectives on hospice care (Zhaoxia et al., 2014; Mastroianni et al., 2015; Huiying and Liqin, 2018). During the pandemic, Cardoso et al. (2021) found that varying levels of knowledge and skills among nurses can lead to differing attitudes toward death and different approaches to handling death-related events. Samson and Shvartzman (2018) reported that a positive attitude towards death can improve the care of dying patients. A positive death attitude, particularly one based on natural acceptance, is crucial in the hospice care process and is a key objective for nursing managers through death education (Cardoso et al., 2021; He et al., 2023). However, due to the relatively late development of China’s death education system and the influence of traditional culture, death education in China is still evolving. It currently features limited content and monotonous implementation methods, which somewhat hinder the advancement of death education. Additionally, death education is essential for providing hospice care. Healthcare providers, especially nurses, must first undergo death education to understand the nature of death and acquire coping skills. This education enables them to effectively assist and guide terminal patients and their families in facing death with courage, provide psychological counseling, ensure patients pass away peacefully with minimal suffering and no regrets, and offer support and understanding to their families. Therefore, it is recommended that nursing administrators improve the content and delivery methods of death education for ICU nurses. This will help nurses fully grasp the meaning of life, accept death as an inevitable part of life, confront and address death with bravery, and ultimately deliver high-quality hospice care services.
Consistent with a previous study by Ran et al. (2018) and Cardoso et al. (2021), this study found that the presence of meaning and the search for meaning were positively correlated with natural acceptance and negatively correlated with fear of death and escape acceptance. Barnett et al. (2019) observed that nurses with a higher sense of meaning may develop greater self-esteem, which helps them resist the negative effects of death. Humans are inherently driven to create and seek meaning, and pursuing meaning in life is one of the best ways to alleviate the fear of death (Zhang et al., 2019). Death challenges the possibility of achieving fundamental life goals and beliefs in life’s meaning (Barnett et al., 2018). After traumatic events involving the threat of death, individuals often re-evaluate the events and construct new meanings (Park and George, 2013). Some studies suggest that a lack of meaning in life can lead to feelings of boredom, depression, despair, and a loss of the will to live, making death seem like a form of liberation, and thus resulting in escaping acceptance (Pinquart, 2002; Xiaomin et al., 2021). Therefore, enhancing the sense of meaning in life is crucial for cultivating a scientific view of life and death. Amenta (1984) stated that the sense of meaning in life is an important and effective indicator of death education. A Chinese Taiwanese scholar noted that the essence of death education lies in exploring the nature of death, encouraging individuals to deeply consider their relationships with others, society, nature, and various topics related to dying and mourning. This process helps people understand the true meaning and value of existence, thereby overcoming fear and anxiety about death (Zhang et al., 2019). Nursing administrators should emphasize the sense of meaning in life as a critical component of death education for ICU nurses. This approach can help ICU nurses gain a deeper understanding of life’s meaning, actively contemplate and pursue the significance and value of existence, and eliminate negative psychological attitudes like fear and avoidance of death. By promoting an objective, calm, and accepting mindset towards death, ICU nurses can provide comfort, care, and patience to patients and their families, creating a comfortable medical environment, offering warm emotional support, and providing necessary psychological comfort.
The key finding of this study is that ICU nurses’ resilience is positively correlated with natural acceptance and negatively correlated with fear of death and escape acceptance. This suggests that ICU nurses with resilience experience fewer negative psychological processes when dealing with death and are more likely to naturally accept death and life’s finite nature. Wang (2022) found that oncology nurses with strong psychological resilience can maintain a positive mindset when facing death and have confidence in providing end-of-life care. Similarly, numerous studies have shown that psychological resilience can buffer the negative psychological impacts of stressful events, such as adversity, tragedy, and trauma experienced by nurses in clinical work, effectively maintaining their physical and mental balance and promoting a positive state of development and adaptation (Luthar et al., 2000; Kalisch et al., 2017; Cooper et al., 2020). Therefore, it is essential to recognize the role of resilience in ICU nurses’ psychological state when confronting near-death or death situations.
Another important finding is that ICU nurses’ resilience partially mediated the relationship between the sense of meaning in life (presence of meaning and the search for meaning) and attitudes toward death (natural acceptance, escape acceptance, and fear of death).This indicates that ICU nurses’ attitudes toward death can be predicted through their resilience. Kalisch et al. (2017) suggest that a sense of meaning in life can enhance resilience and improve psychological adaptation, fulfilling the psychosocial needs arising from stressful events. During the COVID-19 pandemic, some scholars showed that searching for meaning and value in life can provide people with positive psychological qualities and goal-oriented motivation when coping with stressors, rather than avoiding them (Ostafin and Proulx, 2020; Yildirim et al., 2021). Therefore, it is suggested that ICU nurses with a strong sense of meaning in life can empower themselves with positive energy and support, thus exhibiting high resilience when facing death events. Resilience is regarded as a dynamic process that can mediate between a sense of meaning in life and mental health (Folkman, 1997; Ya'nan and Xiaoyu, 2023). The findings of this study align with previous research. For example, psychological resilience was found to mediate the relationship between a sense of meaning in life and academic boredom among Chinese college students (Huayu and Guangming, 2019). Additionally, resilience was shown to mediate the relationship between a sense of meaning in life and anxiety or depressive emotions among fourth-year medical students (Ya'nan and Xiaoyu, 2023). Korean researchers discovered that resilience can improve the relationship between nurses’ sense of meaning in life and post-traumatic growth (Han et al., 2023). Thus, it is essential to enhance ICU nurses’ resilience. Southwick et al. (2014) suggested that psychological resilience is not an innate trait but can be learned or developed through various coping strategies tailored to individual conditions. For instance, Foureur et al. (2013) utilized mindfulness-based stress reduction therapy to help nursing staff better manage work-related stress and improve physical and mental health. Increased resilience levels were also observed through mindfulness-based meditation training. Mealer et al. (2014) conducted a 12-week multimodal resilience training program for 27 ICU nurses, which not only boosted individual resilience levels but also reduced anxiety, depression, and burnout among the nurses. Chesak et al. (2015) implemented the Stress Management and Resilience Training (SMART) curriculum with newly employed nurses, resulting in higher resilience levels in the experimental group post-training. These methods involved consciously guiding nurses to adjust their cognitive responses, adapt to stress, and increase their adaptability to internal and external environments, supporting constructive problem-solving and promoting effective outcomes. Therefore, it is recommended to develop multimodal resilience training programs within ICU nurses’ death education.
Our findings provide a theoretical foundation for death education among ICU nurses. Nursing administrators can use these results to develop advanced courses in death education and establish clearer educational objectives to scientifically improve ICU nurses’ attitudes toward death. Additionally, the effectiveness of death education can be assessed through measures of meaning in life and psychological resilience. It is essential to create specific death education courses and fully utilize internal hospital resources for ICU nurses, helping them develop psychological resilience and a sense of meaning in life. This approach encourages nurses to view death as a natural part of life without fear or anxiety, allowing them to face and accept it calmly, maintain hope, and employ reasonable strategies to manage the consequences of death.
5 Limitations
This cross-sectional survey, which explores mediating effects using structural equation modeling, has some limitations. ICU nurses were recruited through convenience sampling from four tertiary hospitals in Fujian and Guangdong provinces, China. These samples may not represent all ICU nurses in mainland China, limiting the generalizability of the results. Future research should expand the sample size or divide it into different groups, and conduct multi-center surveys and longitudinal studies. Additionally, the use of an online self-assessment scale to collect data may introduce reporting bias.
6 Conclusion
This study examined the structural relationships among ICU nurses’ sense of meaning in life, resilience, and attitudes toward death. The results confirmed the correlations among these variables and the partial mediating role of resilience. We suggest that ICU nurses’ attitudes toward death should receive greater attention as an important professional quality. By establishing multi-level death education courses, we can improve the sense of meaning in life and resilience, enabling ICU nurses to naturally accept death and provide high-quality care for dying patients. Future research should focus on the mechanisms and pathways influencing attitudes toward death, providing a theoretical basis and empirical evidence for developing more scientific death education strategies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Guangzhou Medical University (202403031). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LW: Writing – review & editing, Methodology, Conceptualization. SL: Writing – review & editing, Writing – original draft, Data curation. XL: Writing – review & editing, Investigation, Data curation. RoL: Writing – review & editing. RaL: Writing – review & editing, Investigation.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We thank all the participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Amenta, M. M. (1984). Death anxiety, purpose in life and duration of service in hospice volunteers. Psychol. Rep. 54, 979–984. doi: 10.2466/pr0.1984.54.3.979
Arli, S. K. (2023). An investigation of the relationship between attitudes towards caring for dying patients and compassion. Omega 86, 1167–1175. doi: 10.1177/00302228211004805
Ay, M. A., and Öz, F. (2019). Nurses attitudes towards death, dying patients and euthanasia: a descriptive study. Nurs. Ethics 26, 1442–1457. doi: 10.1177/0969733017748481
Barnett, M. D., Anderson, E. A., and Marsden, A. D. (2018). Is death anxiety more closely linked with optimism or pessimism among older adults? Arch. Gerontol. Geriatr. 77, 169–173. doi: 10.1016/j.archger.2018.05.003
Barnett, M. D., Moore, J. M., and Garza, C. J. (2019). Meaning in life and self-esteem help hospice nurses withstand prolonged exposure to death. J. Nurs. Manag. 27, 775–780. doi: 10.1111/jonm.12737
Braun, M., Gordon, D., and Uziely, B. (2010). Associations between oncology nurses' attitudes toward death and caring for dying patients. Oncol. Nurs. Forum 37, E43–E49. doi: 10.1188/10.ONF.E43-E49
Brinkman, S., Bakhshi-Raiez, F., Abu-Hanna, A., de Jonge, E., and de Keizer, N. F. (2013). Determinants of mortality after hospital discharge in ICU patients: literature review and Dutch cohort study. Crit. Care Med. 41, 1237–1251. doi: 10.1097/CCM.0b013e31827ca4f9
Cardoso, M. F. P. T., Martins, M. M. F. P. D. S., Trindade, L. L., Ribeiro, O. M. P. L., and Fonseca, E. F. (2021). The COVID-19 pandemic and nurses' attitudes toward death. Rev. Lat. Am. Enfermagem 29:e3448. doi: 10.1590/1518.8345.4769.3448
Cheng, C., Dong, D., He, J., Zhong, X., and Yao, S. (2020). Psychometric properties of the 10-item Connor-Davidson resilience scale (CD-RISC-10) in Chinese undergraduates and depressive patients. J. Affect. Disord. 261, 211–220. doi: 10.1016/j.jad.2019.10.018
Chesak, S. S., Bhagra, A., Schroeder, D. R., Foy, D. A., Cutshall, S. M., and Sood, A. (2015). Enhancing resilience among new nurses: feasibility and efficacy of a pilot intervention. Ochsner J. 15, 38–44
Cho, G. J., and Kang, J. (2017). Type D personality and post-traumatic stress disorder symptoms among intensive care unit nurses: the mediating effect of resilience. PLoS One 12:e0175067. doi: 10.1371/journal.pone.0175067
Connor, K. M., and Davidson, J. R. (2003). Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress. Anxiety 18, 76–82. doi: 10.1002/da.10113
Cook, D., and Rocker, G. (2014). Dying with dignity in the intensive care unit. N. Engl. J. Med. 370, 2506–2514. doi: 10.1056/NEJMra1208795
Cooper, A. L., Brown, J. A., Rees, C. S., and Leslie, G. D. (2020). Nurse resilience: a concept analysis. Int. J. Ment. Health Nurs. 29, 553–575. doi: 10.1111/inm.12721
Costello, J. (2006). Dying well: nurses' experiences of 'good and bad' deaths in hospital. J. Adv. Nurs. 54, 594–601. doi: 10.1111/j.1365-2648.2006.03867.x
Dezutter, J., Luyckx, K., and Hutsebaut, D. (2009). Are you afraid to die? Religion and death attitudes in an adolescent sample. J. Psychol. Theol. 37, 163–173. doi: 10.1177/009164710903700302
Du, H., Li, X., Chi, P., Zhao, J., and Zhao, G. (2017). Meaning in life, resilience, and psychological well-being among children affected by parental HIV. AIDS Care 29, 1410–1416. doi: 10.1080/09540121.2017.1307923
Durlak, J. A. (1972). Relationship between individual attitudes toward life and death. J. Consult. Clin. Psychol. 38:463. doi: 10.1037/h0032854
Edo-Gual, M., Monforte-Royo, C., Aradilla-Herrero, A., and Tomás-Sábado, J. (2015). Death attitudes and positive coping in Spanish nursing undergraduates: a cross-sectional and correlational study. J. Clin. Nurs. 24, 2429–2438. doi: 10.1111/jocn.12813
Folkman, S. (1997). Positive psychological states and coping with severe stress. Soc. Sci. Med. 45, 1207–1221. doi: 10.1016/s0277-9536(97)00040-3
Foureur, M., Besley, K., Burton, G., Yu, N., and Crisp, J. (2013). Enhancing the resilience of nurses and midwives: pilot of a mindfulness-based program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemp. Nurse 45, 114–125. doi: 10.5172/conu.2013.45.1.114
Han, S. J., Yeun, Y. R., and Roh, H. (2023). The impact of resilience on post-traumatic growth among nurses in COVID-19-designated hospitals: the mediating effect of meaning in life. Healthcare 11:2895. doi: 10.3390/healthcare11212895
He, Y., and Li, T. (2022). Death attitudes and death anxiety among medical interns after the 2020 outbreak of the novel coronavirus. Front. Psychol. 13:698546. doi: 10.3389/fpsyg.2022.698546
He, S., Zhao, H., Wang, H., Chen, F., Lv, T., Li, L., et al. (2023). The mediating effects of attitude toward death and meaning of life on the relationship between perception of death and coping with death competence among Chinese nurses: a cross-sectional study. BMC Nurs. 22:87. doi: 10.1186/s12912-023-01245-5
Huayu, T., and Guangming, L. (2019). The relationship between college Students' sense of life meaning and boredom: the mediating effect of psychological elasticity. Educ. Res. Monthly 2, 92–97. doi: 10.16477/j.cnki.issn1674-2311.2019.02.011
Huiying, Z., and Liqin, W. (2018). Influence of death attitude on hospice care attitude of clinical nurses in Xinjiang. Chin. Gen. Pract. Nurs. 11, 1291–1294. doi: 10.3969/j.issn.1674-4748.2018.11.004
Jiao, Y. A. N. G., Rongzhuma, L. U., Ruojia, W. U., Qiuyan, H. E., and Xiumei, Y. A. N. G. (2023). Analysis on current status and correlation of mental toughness, illness notification preference and death attitude among medical students. Med. Pharm. Yunnan 1, 100–103.
Jing, C., Hailin, Z., Baoxin, S., and Linlin, Z. (2012). Study on correlation between attitude to death and subjective well-being of contract nurses in military hospital. Chin. Nurs. Res. 10, 891–893. doi: 10.3969/j.issn.1009-6493.2012.10.014
Jinling, L., Xiao, C., Qianyi, Y., Zhenjiang, C., Lichang, T., Qiguang, L., et al. (2020). Analysis of death attitude levels among 331 ICU nurses. J. Nurs. 9, 42–47. doi: 10.16460/j.issn1008-9969.2020.09.042
Kalisch, R., Baker, D. G., Basten, U., Boks, M. P., Bonanno, G. A., Brummelman, E., et al. (2017). The resilience framework as a strategy to combat stress-related disorders. Nat. Hum. Behav. 1, 784–790. doi: 10.1038/s41562-017-0200-8
Khandelwal, N., and Curtis, J. R. (2014). Clinical and economic implications of timing of limitations in life support. Crit. Care Med. 42, 455–456. doi: 10.1097/CCM.0b013e3182a522de
Kudubes, A. A., Akıl, Z. K., Bektas, M., and Bektas, İ. (2021). Nurses' attitudes towards death and their effects on spirituality and spiritual care. J. Relig. Health 60, 153–161. doi: 10.1007/s10943-019-00927-2
Lian, Z. E. N. G., Li Changying, Z. E. N. G., Chengyao, L. S., Yonghong, W. A. N. G., and Hongmei, L. (2022). The situation and correlation between death attitudes and job burnout among medical staff in Neijiang. Modern Nurse 2, 122–127. doi: 10.19792/j.cnki.1006-6411.2022.05.038
Lieberman, E. J. (2004). Terror management theory. Am. J. Psychiatry 161, 1508–1509. doi: 10.1176/appi.ajp.161.8.1508
Liu, Cai. (2023). Status and influencing factors of ICU nurses’ attitude toward death. MA thesis. doi: 10.27652/d.cnki.gzyku.2022.001341
Luthar, S. S., Cicchetti, D., and Becker, B. (2000). The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 71, 543–562. doi: 10.1111/1467-8624.00164
Mastroianni, C., Piredda, M., Taboga, C., Mirabella, F., Marfoli, E., Casale, G., et al. (2015). Frommelt attitudes toward Care of the Dying Scale Form B: psychometric testing of the Italian version for students. Omega 70, 227–250. doi: 10.1177/0030222815568944
Mealer, M., Conrad, D., Evans, J., Jooste, K., Solyntjes, J., Rothbaum, B., et al. (2014). Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am. J. Crit. Care 23, e97–e105. doi: 10.4037/ajcc2014747
Mengcheng, W. A. N. G., and Xiaoyang, D. A. I. (2008). Clinical and economic implications of timing of limitations in life support. Chin. J. Clin. Psychol. 16:3.
Meng, M., He, J., Guan, Y., Zhao, H., Yi, J., Yao, S., et al. (2019). Factorial invariance of the 10-item Connor-Davidson resilience scale across gender among Chinese elders. Front. Psychol. 10:1237. doi: 10.3389/fpsyg.2019.01237
Mezzaroba, A. L., Larangeira, A. S., Morakami, F. K., Junior, J. J., Vieira, A. A., Costa, M. M., et al. (2022). Evaluation of time to death after admission to an intensive care unit and factors associated with mortality: a retrospective longitudinal study. Int. J. Crit. Illn. Inj. Sci. 12, 121–126. doi: 10.4103/ijciis.ijciis_98_21
Ostafin, B. D., and Proulx, T. (2020). Meaning in life and resilience to stressors. Anxiety Stress Coping 33, 603–622. doi: 10.1080/10615806.2020.1800655
Park, C. L., and George, L. S. (2013). Assessing meaning and meaning making in the context of stressful life events: measurement tools and approaches. J. Posit.Psychol. 8, 483–504. doi: 10.1080/17439760.2013.830762
Pengcheng, S. H. E. N., and Tian, Z. H. U. (2023). Predictive value of mortality and OASIS score in elderly and young ICU patients. China J. Emerg. Resuscit. Disaster Med. 2, 232–235. doi: 10.3969/j.issn.1673-6966.2023.02.024
Peters, L., Cant, R., Payne, S., O'Connor, M., McDermott, F., Hood, K., et al. (2013). Emergency and palliative care nurses' levels of anxiety about death and coping with death: a questionnaire survey. Austral. Emerg. Nursing J. 16, 152–159. doi: 10.1016/j.aenj.2013.08.001
Pinquart, M. (2002). Creating and maintaining purpose in life in old age: a meta-analysis. Ageing Int. 27, 90–114. doi: 10.1007/s12126-002-1004-2
Ran, G. A. O., Yingjie, C. A. I., Yanjiao, L. I., Chunli, S. O. N. G., and Tieying, S. H. I. (2018). The relationship between the meaning in life and attitude death of nurses. Chin. Nurs. Manag. 4, 461–465. doi: 10.3969/j.issn.1672-1756.2018.04.008
Sakr, Y., Lobo, S. M., Moreno, R. P., Gerlach, H., Ranieri, V. M., Michalopoulos, A., et al. (2012). Patterns and early evolution of organ failure in the intensive care unit and their relation to outcome. Crit. Care 16:R222. doi: 10.1186/cc11868
Samson, T., and Shvartzman, P. (2018). Association between level of exposure to death and dying and professional quality of life among palliative care workers. Palliat. Support. Care 16, 442–451. doi: 10.1017/S1478951517000487
Schreiber, M., Cates, D. S., Formanski, S., and King, M. (2019). Maximizing the resilience of healthcare workers in multi-hazard events: lessons from the 2014-2015 Ebola response in Africa. Mil. Med. 184, 114–120. doi: 10.1093/milmed/usy400
Southwick, S. M., Bonanno, G. A., Masten, A. S., Panter-Brick, C., and Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. Eur. J. Psychotraumatol. 5. doi: 10.3402/ejpt.v5.25338
Steger, M. F., Frazier, P., Oishi, S., and Kaler, M. (2006). The meaning in life questionnaire: assessing the presence of and search for meaning in life. J. Couns. Psychol. 53, 80–93. doi: 10.1037/0022-0167.53.1.80
Testoni, I., Ronconi, L., Palazzo, L., Galgani, M., Stizzi, A., and Kirk, K. (2018). Psychodrama and moviemaking in a death education course to work through a case of suicide among high school students in Italy. Front. Psychol. 9:441. doi: 10.3389/fpsyg.2018.00441
Wang, Lihua. (2022). The investigation and analysis of influencing factors on Nurses' coping ability to death in oncology department of 3 hospitals in Nanchang. MA thesis
White, B., Driver, S., and Warren, A. M. (2008). Considering resilience in the rehabilitation of people with traumatic disabilities. Rehabil. Psychol. 53, 9–17. doi: 10.1037/0090-5550.53.1.9
Wong, P. T. P., Reker, G. T., and Gesser, G. (1994). “Death attitude profile— revised: a multidimensional measure of attitudes toward death” in Death anxiety handbook: Research, instrumentation, and application. ed. R. A. Neimeye, vol. 6 (Abingdon: Taylor & Francis), 121–148. doi: 10.1037/t17237-000
Xiaomin, X. U., Bingying, Z. H. U., and Kai, R. E. N. (2021). Study on the correlation between the purpose in life and attitude towards death of medica students in higher vocational colleges. Chin. Evid Based Nurs. 6, 783–786. doi: 10.12102/j.issn.2095-8668.2021.06.014
Ya'nan, Zheng, & Xiaoyu, Li. (2023). Investigation and analysis of the relationship between mental health, mental resilience and sense of life meaning of senior medical students. Health Vocat. Educ., (16), 153–156. doi: 10.20037/j.issn.1671-1246.2023.16.44
Yela, J. R., Crego, A., Gómez-Martínez, M. Á., and Jiménez, L. (2020). Self-compassion, meaning in life, and experiential avoidance explain the relationship between meditation and positive mental health outcomes. J. Clin. Psychol. 76, 1631–1652. doi: 10.1002/jclp.22932
Yildirim, M., Arslan, G., and Wong, P. T. P. (2021). Meaningful living, resilience,affective balance, and psychological health problems among Turkish young adults during coronavirus pandemic. Curr. Psychol. 76, 1–12. doi: 10.1007/s12144-020-01244-8
Yinglan, L., Yue, Z., Yanfang, L., Lingyun, T., Boya, L., Ningning, H., et al. (2024). Death education for clinical nurses in China: a scoping review. Chin. Nurs. Manag. 24, 186–191. doi: 10.3969/j.issn.1672-1756.2024.02.006
Yu, H., Sun, C., Xie, L., Wang, L., Song, J., Zhu, Y., et al. (2022). Using a mediating model of death attitude and meaning in life to understand nursing students attitude about hospice care. Nurse Educ. Today 116:105448. doi: 10.1016/j.nedt.2022.105448
Zhang, J., Peng, J., Gao, P., Huang, H., Cao, Y., Zheng, L., et al. (2019). Relationship between meaning in life and death anxiety in the elderly: self-esteem as a mediator. BMC Geriatr. 19:308. doi: 10.1186/s12877-019-1316-7
Zhaoxia, M., LiYanlin, Z. C., and Liangliang, G. (2014). Correlation between nurses' attitudes to terminal patients and their personal attitudes toward death. J. Nurs. Sci. 2, 51–53. doi: 10.3870/hlxzz.2014.02.051
Zheng, R. S., Guo, Q. H., Dong, F. Q., and Owens, R. G. (2015). Chinese oncology nurses' experience on caring for dying patients who are on their final days: a qualitative study. Int. J. Nurs. Stud. 52, 288–296. doi: 10.1016/j.ijnurstu.2014.09.009
Zhihong, D., and Yan, W. (2023). The change of financial support of Chinese older adults from 2010 to 2020: an comparative analysis of census data in 2010 and 2020. Sci. Res. Aging 11, 1–18. doi: 10.3969/j.issn.2095-5898.2023.04.002
Zhu, H. L., and Shi, B. X. (2010). Research progress on influencing factors of death attitudes. Chin. J. Nurs. 6, 569–571. doi: 10.3761/j.issn.0254-1769.2010.06.034
Keywords: intensive care unit nurses, attitude toward death, meaning in life, resilience, structural equation modeling
Citation: Wang L, Li S, Liu X, Li R and Li R (2024) The mediating role of resilience in the relationship between meaning in life and attitude toward death among ICU nurses: a cross-sectional study. Front. Psychol. 15:1414989. doi: 10.3389/fpsyg.2024.1414989
Edited by:
Ahmed A. Karim, University Hospital Tübingen, GermanyReviewed by:
Yuke Tien Fong, Singapore General Hospital, SingaporeJasmin Abdel Karim, University Hospital Tübingen, Germany
Copyright © 2024 Wang, Li, Liu, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lifang Wang, d2xpZmFuZzAwMUAxNjMuY29t
†These authors share first authorship
 Lifang Wang
Lifang Wang Sisi Li
Sisi Li Xiaorong Liu†
Xiaorong Liu† Rong Li
Rong Li Ran Li
Ran Li