- Department of Rehabilitation Medicine, Zibo Central Hospital, Zibo, China
Objective: Reminiscence therapy is increasingly being utilized for cancer patients to address psychological pressure and enhance their quality of life. This meta-analysis aimed to comprehensively evaluate the effect of a reminiscence therapy-involved program (RTIP) on anxiety, depression, and quality of life in cancer patients.
Methods: A systematic literature search was conducted in the Web of Science, PubMed, Embase, and Cochrane Library databases until December 2023 to screen randomized control trials (RCTs) comparing the effect of RTIP and control care.
Results: A total of 16 RCTs published from 2013 to 2023 were included, with 1,963 cancer patients undergoing RTIP with or without control care (RTIP group, N = 984) or control care (control group, N = 979). The results showed the the anxiety score [standardized mean differences (SMD) = −0.539; 95% confidence interval (CI) = −0.700, −0.378; P < 0.001], anxiety rate [relative risk (RR) = 0.736; 95% CI: 0.627, 0.865; P < 0.001], depression score (SMD = −0.664; 95% CI: −0.967, −0.361; P < 0.001), and depression rate (RR = 0.632; 95% CI = 0.532, 0.750; P < 0.001) were significantly reduced in the RTIP group compared to the control group. Furthermore, overall quality of life was increased in the RTIP group than in the control group (SMD = 0.501; 95% CI: 0.314, 0.689; P < 0.001). In digestive system cancer patients, anxiety/depression scores and rates were reduced, and the overall quality of life was elevated in the RTIP group in comparison with the control group (all P < 0.050). The quality of evidence was generally high, with a low risk of bias in most studies and no publication bias in any outcomes (all P > 0.050).
Conclusion: RTIP attenuates anxiety and depression and improves the quality of life in cancer patients, benefitting their overall health condition.
Systematic Review Registration: This meta-analysis was registered at PROSPERO with registration number CRD42024563266.
1 Introduction
Cancer is one of the leading obstacles to increasing life expectancy, with ~19.9 million new cases and 9.7 million deaths worldwide in 2022 (Sung et al., 2021; Bray et al., 2024). Conceivably, the psychological burden of cancer patients is heavy, caused not only by confronting major life stressors or threats but also by many other factors, including the physical dimension, treatment dimension, as well as economic and interpersonal communication aspects (Emery et al., 2022). For the physical dimension, it is estimated that 32%−90% of patients experience cancer-related fatigue, and 35%−96% of patients suffer from cancer-related neuropathy or bone pain, which enhances psychological pressure (Henson et al., 2020; Renna et al., 2022; Wu et al., 2022). Concerning the treatment dimension, postoperative complications and medication/radiotherapy-induced side effects lead to increased perceived pressure and a sense of loss in cancer patients (Wagland et al., 2015; Henson et al., 2020). Moreover, financial burdens and social isolation aggravate the psychological pressure of cancer patients (Abrams et al., 2021; Liang et al., 2022). More importantly, the heavy psychological burden, commonly manifested by anxiety and depression, is linked with treatment discontinuation, disease recurrence, and death of cancer patients (Morrison et al., 2017; Wang et al., 2020). In addition, an unpleasant quality of life frequently occurs in cancer patients, which is adversely affected by the aforementioned influencing factors and psychological pressure as well (van Montfort et al., 2020; Carbajal-Lopez et al., 2022; Jiang et al., 2023; Licu et al., 2023). Studies have reported that poor quality of life and anxiety and depression are prevalent in patients with cancers (Zheng et al., 2020; Li Y. et al., 2022; Fu et al., 2023). Consequently, developing oncology care plans and providing proper intervention to help cancer patients cope with psychological pressure as well as improve their quality of life is quite necessary (Mullen et al., 2023).
Reminiscence therapy, developed by Robert Butler in 1963 and initially applied in the elderly population with cognitive impairment, is a life-reviewing caring approach that encourages subjects to recall autobiographical events (Cuevas et al., 2020; Yan et al., 2023). This intervention has been widely used in patients with cognitive impairment, such as Alzheimer's disease, post-stroke cognitive impairment, and dementia (Smallfield et al., 2024). During the intervention procedure, it was surprisingly noticed that reminiscence therapy can relieve psychological pressure and enhance the self-confidence of participants (Tam et al., 2021). Gradually, reminiscence therapy has been introduced in cancer patients to alleviate anxiety/depression and improve quality of life, which has served as optional management to improve the lives of patients with cancers (Xiao et al., 2013; Vuksanovic et al., 2017; Kleijn et al., 2018; Dong et al., 2019; Liu and Li, 2021; Zhang et al., 2021; Zhao, 2021; Zhou and Sun, 2021; Chen et al., 2022; Guo et al., 2022; Huang et al., 2022; Li T. et al., 2022; Liu et al., 2022; Zheng et al., 2022; Babaei et al., 2023; Wu and Zhang, 2023). For instance, one study discloses reduced anxiety score, anxiety rate, and depression score, as well as elevated quality of life in colorectal cancer patients who receive reminiscence therapy compared to those treated with control care, while the depression rate is similar between them (Zhou and Sun, 2021). Another study shows that reminiscence therapy decreases anxiety score and anxiety rate, but it does not affect depression score or depression rate in surgical gastric cancer patients (Zhang et al., 2021). Differently, one previous study indicates that no difference is observed in anxiety score, depression score, or quality of life between cancer patients undergoing reminiscence therapy and usual care (Kleijn et al., 2018).
To date, only one previous meta-analysis has indicated that reminiscence therapy ameliorates anxiety and depression and improves the quality of life in cancer patients (Sun et al., 2023). However, the aforementioned meta-analysis includes articles from 2010 to 2021 (Sun et al., 2023), and a number of relevant studies (n = 8) published after 2021 have not yet been included in a pooled analysis (Chen et al., 2022; Guo et al., 2022; Huang et al., 2022; Li Y. et al., 2022; Liu et al., 2022; Zheng et al., 2022; Babaei et al., 2023; Wu and Zhang, 2023).
In this study, this meta-analysis summarized the existing randomized control trials (RCTs), intending to comprehensively evaluate the effect of a reminiscence therapy-involved program (RTIP) on anxiety, depression, and the quality of life in cancer patients.
2 Methods
2.1 Database searching
This meta-analysis has been registered at PROSPERO with registration number CRD42024563266. Two investigators systematically and independently searched English databases, including Web of Science, PubMed, Embase, and Cochrane Library. The study's search time span was from the establishment to December 2023. The search terms contained “reminiscence therapy,” “life review therapy,” “cancer,” “tumor,” and “malignant neoplasm.”
2.2 Study selection
The inclusion criteria for this meta-analysis were as follows: (1) studies reported comparisons between RTIP and control intervention in cancer patients; (2) studies reported patients age were more than 18 years old; (3) studies reported data about physiological pressure (anxiety or depression) or quality of life; (4) studies were RCTs; and (5) studies were published in English. The exclusion criteria were as follows: (1) duplicative studies; (2) studies did not contain relevant data that could be extracted or relevant data could not be used; (3) reviews, meta-analyses, or case reports; and (4) studies reported data in cancer patients' caregivers. Two investigators completed this part of the study, and in case of disagreement, they discussed the decision with a third researcher.
2.3 Definition and grouping
The control intervention contained blank, health education, exercise guidance, routine care, usual care, control care, and so on. The “control” group was defined as cancer patients who received control intervention. The RTIP was defined as life review therapy or reminiscence therapy, through shared memories or past experiences, aimed at improving the patient's physiological pressure and overall quality of life. The “RTIP” group was defined as cancer patients who underwent the RTIP with or without control intervention.
2.4 Quality assessment
After determining the included studies, two investigators read the studies independently. The quality of the studies was assessed via the Cochrane Collaboration Risk of Bias Assessment Instrument (Zeng et al., 2015). If the study met the criteria, it indicated that the occurrence of various biases was minimal (low). If the quality criteria were partially satisfied, it suggested that the possibility of bias occurrence was moderate or unclear (unclear). However, if the study did not meet the criteria, it implied a high risk of bias (high). For the overall assessment, if all items were low, the overall result was low; if one or more items were assessed as high, the overall result was high, and the remaining cases were considered unclear.
2.5 Data extraction
The first author's name, publish year, sample size, cancer type, age, sex, intervention-related information, and ending index were extracted by two investigators. The extracted ending indexes included anxiety score [measured by Patients Dignity Inventory (PDI), hospital anxiety or depression scale (HADS) for anxiety, or Self-Rating Anxiety Scale (SAS)], anxiety rate, depression score [measured by PDI, HDAS for depression, Self-Rating Depression Scale (SDS), or Beck's Depression Inventory], depression rate, and overall quality of life [measured by overall quality of life, European Organization for Research and Treatment of Cancer Quality-of-Life Questionnaire PAL 15 (EORTC QLQ-C15-PAL), or EORTC QLQ-Core 30]. For the studies with only relevant figure results, we first tried to contact the corresponding authors to seek the original data. If this was not successful, a gadget called “GetData” was used to extract values from the figures.
2.6 Data analysis
RStudio software based on R version 4.3.1 was used to analyze data. The standardized mean differences (SMD) with a 95% confidence interval (CI) were used to analyze the continuous variable and eliminate the differences between scales (Schwarzer et al., 2015). The relative risk (RR) with a 95% CI was adopted for dichotomous outcomes. Heterogeneity across studies was determined via the I2 test and Q test. The random effects model was used when the heterogeneity existed. Publication bias was assessed using Egger's test. Besides, studies reported that patients with digestive system cancer accounted for a large proportion of the population, so those studies with the above particular populations were extracted separately for meta-analysis. A P value < 0.05 indicated significance.
3 Results
3.1 The procedure of study selection
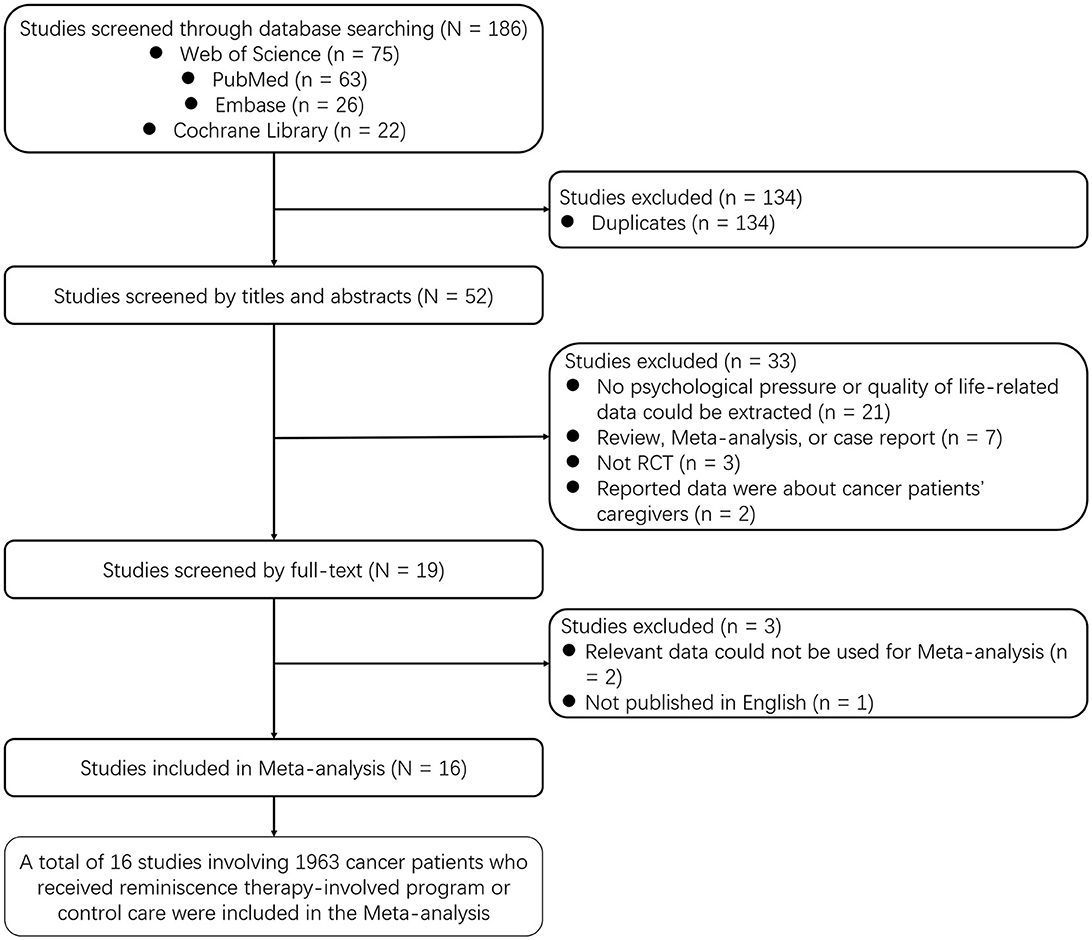
A total of 186 studies were screened in the Web of Science (n = 75), PubMed (n = 63), Embase (n = 26), and Cochrane Library (n = 22) databases. Among them, 134 duplicated studies were excluded. Then, the remaining 52 studies were screened by titles and abstracts. During this process, 33 studies were excluded, including 21 studies with no psychological pressure or quality of life-related data, seven review/meta-analysis/case reports, three non-RCTs, and two studies focusing on cancer patients' caregivers. Subsequently, 19 studies were screened in full-text, and three of them were excluded for relevant data inapplicable for meta-analysis (n = 2) and not published in English (n = 1). Finally, 16 studies involving 1,963 cancer patients who underwent RTIP or control care were included in this meta-analysis (Figure 1).
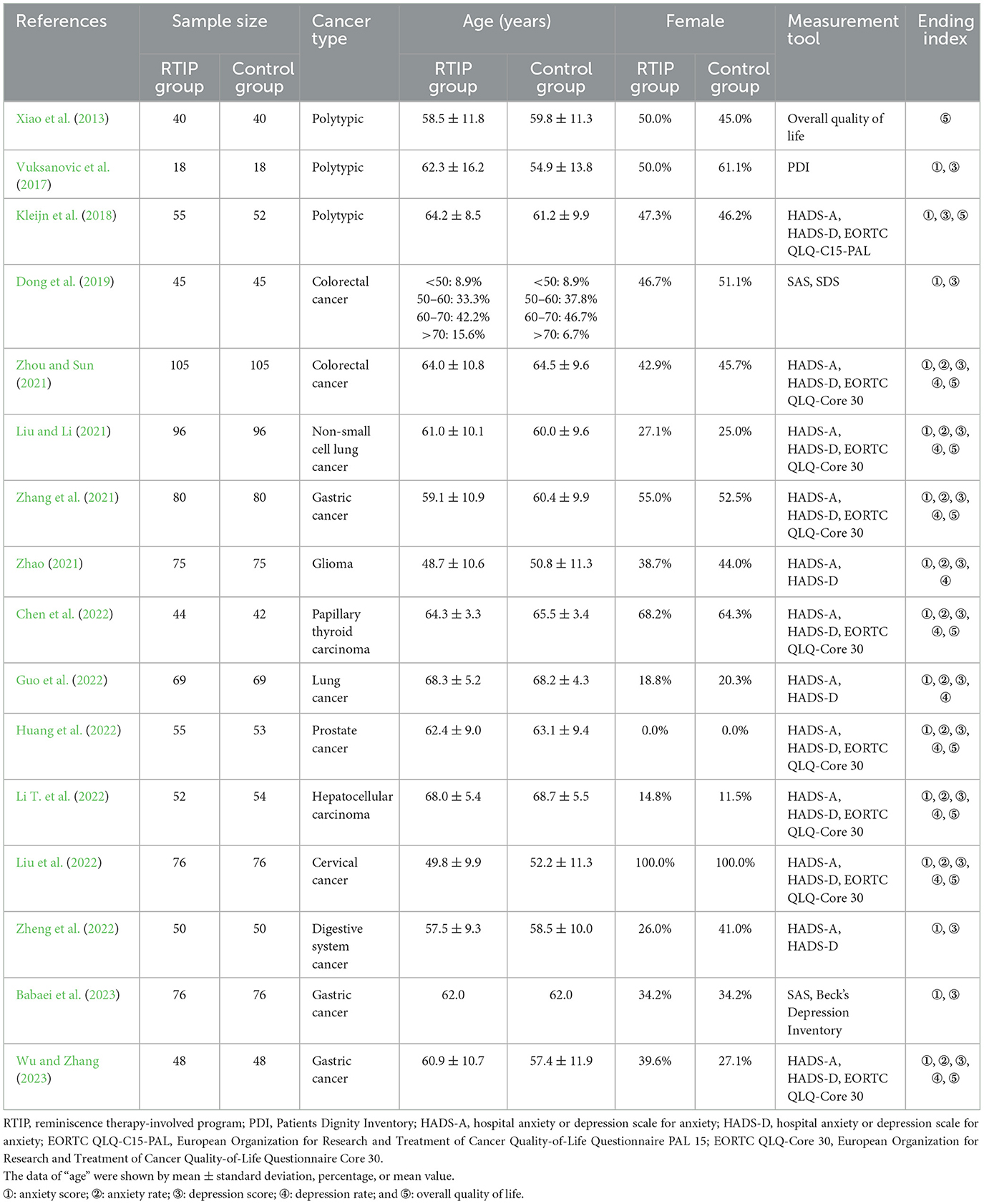
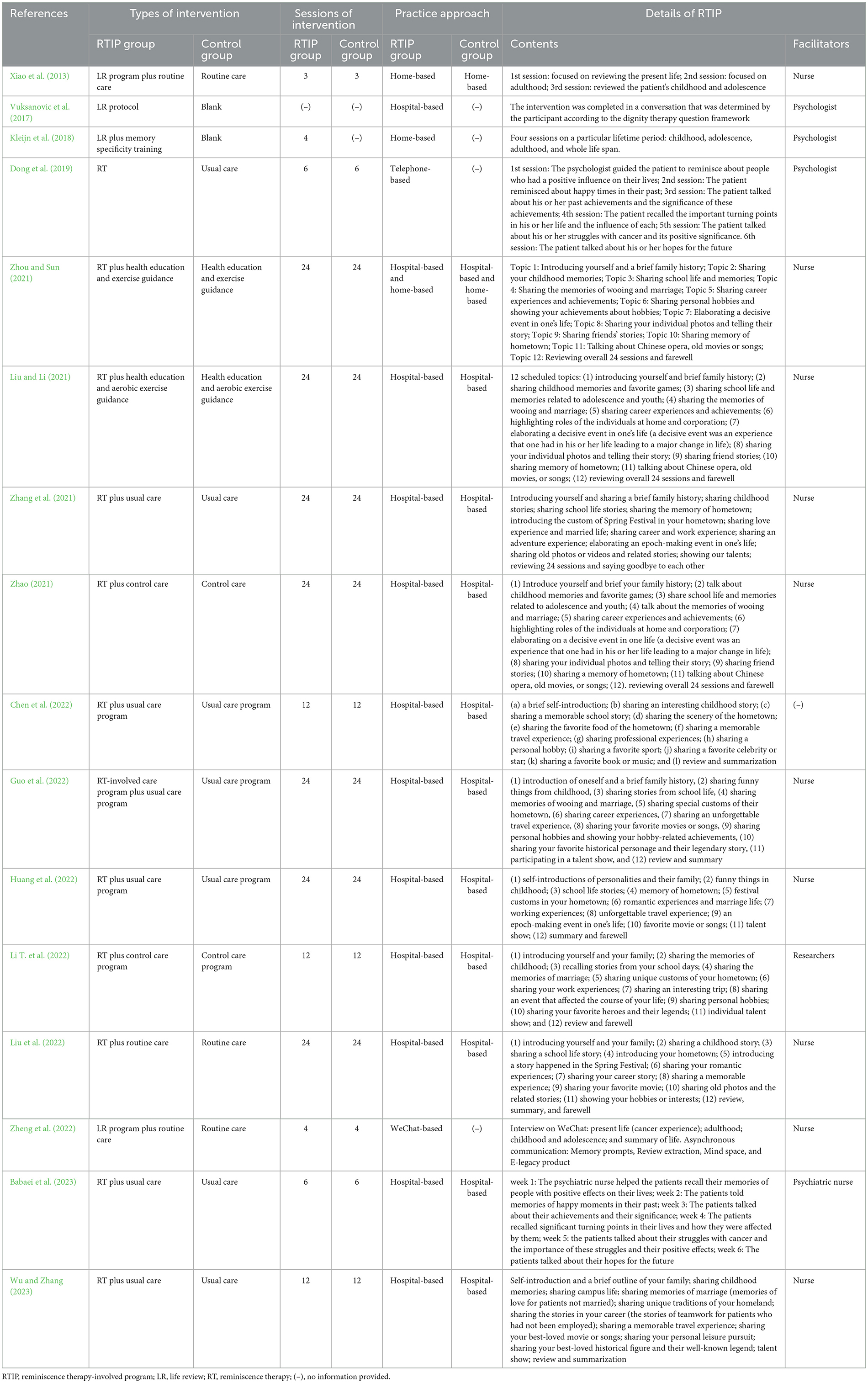
3.2 Information on the enrolled studies and treatment
The included 16 RCTs were published from 2013 to 2023, containing 1,963 cancer patients who underwent RTIP with or without control care (N = 984) or control care (N = 979) (Xiao et al., 2013; Vuksanovic et al., 2017; Kleijn et al., 2018; Dong et al., 2019; Liu and Li, 2021; Zhang et al., 2021; Zhao, 2021; Zhou and Sun, 2021; Chen et al., 2022; Guo et al., 2022; Huang et al., 2022; Li Y. et al., 2022; Liu et al., 2022; Zheng et al., 2022; Babaei et al., 2023; Wu and Zhang, 2023). The involved cancer types included colorectal cancer, lung cancer, gastric cancer, glioma, papillary thyroid carcinoma, prostate cancer, hepatocellular carcinoma, and cervical cancer. The details of the included studies are exhibited in Table 1. In addition, the intervention-related information, including types of intervention, sessions of intervention, and practice approach, is listed in Table 2.
3.3 Risk of bias and publication bias
Overall, most articles were conducted with rigorous randomization (16/16), allocation concealment (12/16), complete outcome data (16/16), and low risk of selective reporting (16/16), while the performance bias (13/16) and detection bias (10/16) were unclear in most studies. Besides, a high risk of bias arose in four articles, containing one study at high risk of performance bias (Xiao et al., 2013), one study at high risk of selection bias, performance bias, and other bias (Kleijn et al., 2018), one study at high risk of other bias (Zhao, 2021), and one study at high risk of performance bias (Zheng et al., 2022) (Figures 2A, B). The Rob 2.0 tool was also applied to assess the quality of the studies (Supplementary Table 1). The results showed that all studies were considered low risk regarding bias arising from the randomization process, bias due to missing outcome data, and bias in selecting the reported result. Moreover, 13 studies were assessed as low risk regarding bias due to deviations from intended interventions, while the other three studies had some concerns; six studies were considered low risk regarding bias in measuring the outcome, while the other 10 had some concerns.
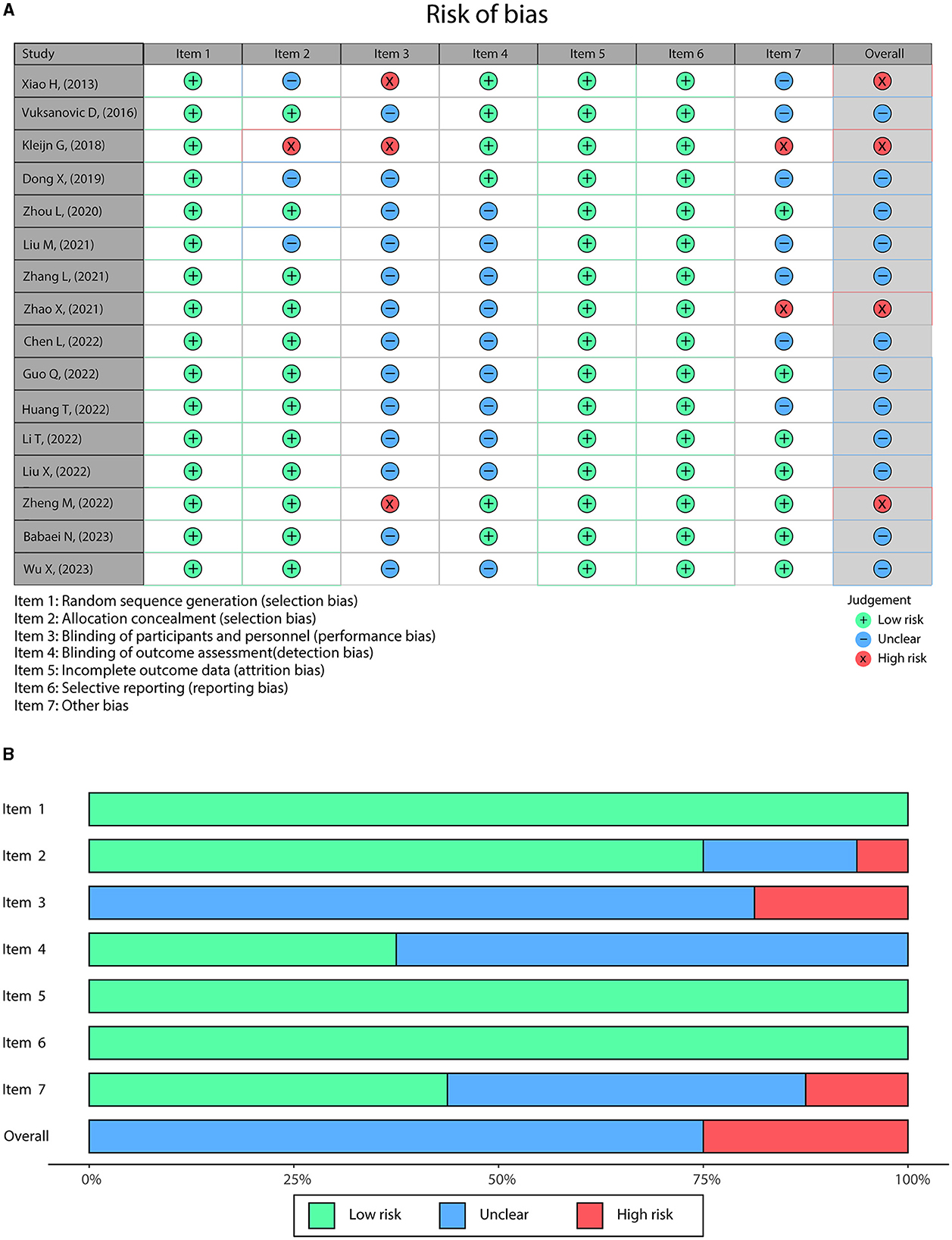
Figure 2. The risk of bias was evaluated using standard Cochrane criteria. Detailed (A) and overall (B) risk of bias in the included studies.
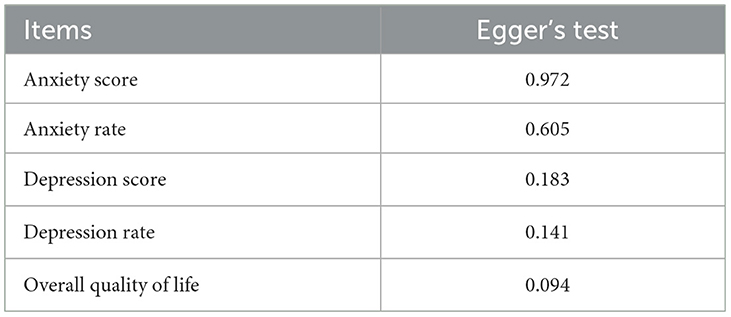
Egger's test disclosed that no publication bias existed in each outcome, including anxiety score, anxiety rate, depression score, depression rate, and overall quality of life (all P > 0.050; Table 3).
3.4 Effect of RTIP on anxiety
Fifteen studies compared anxiety scores between the RTIP and control groups with heterogeneity (I2 = 65.5%, P < 0.001). The random effects model showed that anxiety score was reduced in the RTIP group compared to the control group [SMD (95% CI): −0.539 (−0.700, −0.378), P < 0.001; Figure 3A]. Besides, 10 studies compared anxiety rates between the RTIP and control groups, and there was no heterogeneity (I2 = 0.0%, P = 0.946). Pooled analysis revealed that the anxiety rate declined in the RTIP group compared to the control group [RR (95% CI): 0.736 (0.627, 0.865), P < 0.001; Figure 3B].
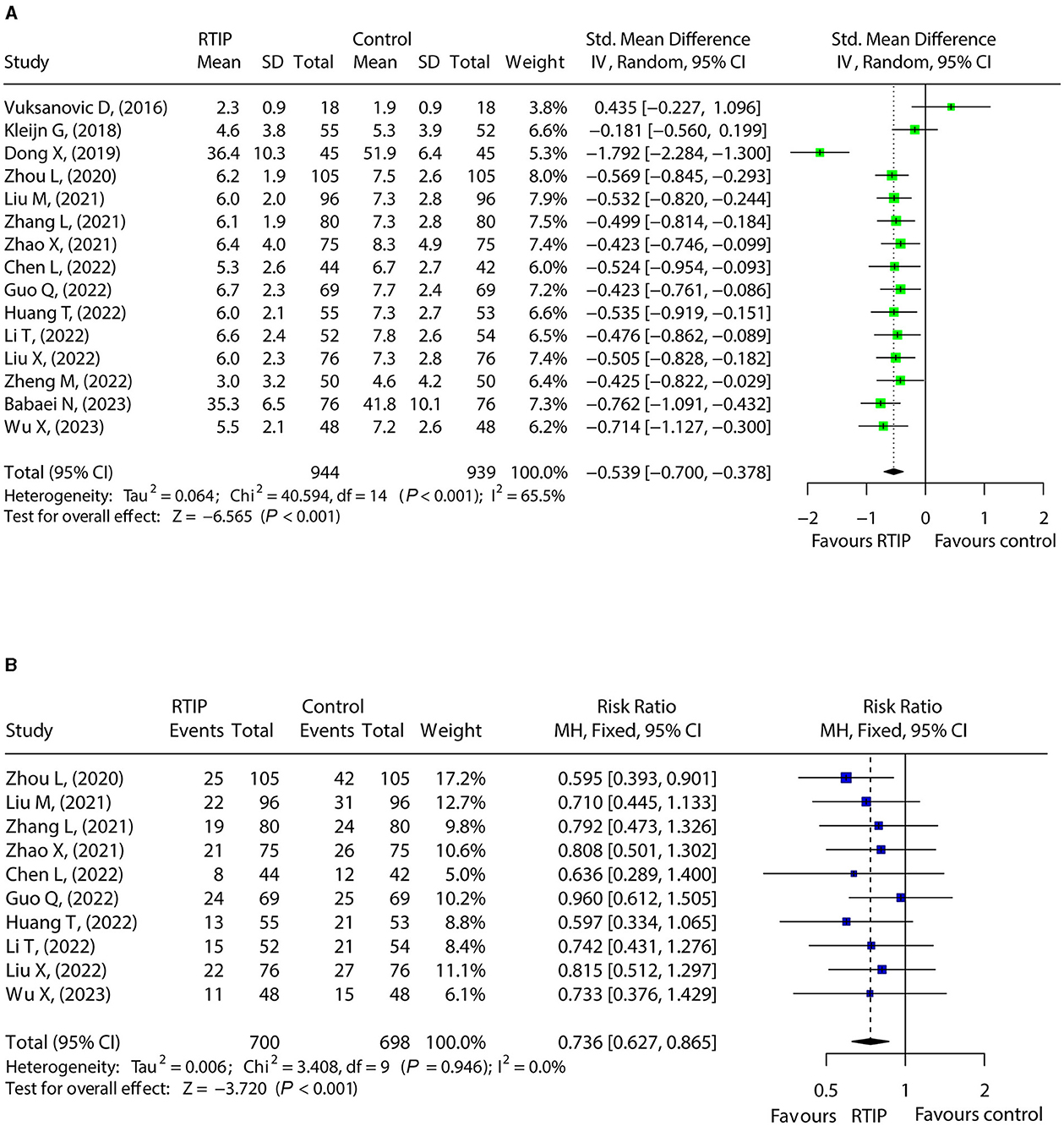
Figure 3. RTIP with or without control care reduced anxiety in cancer patients. Forest plot for the effect of RTIP on anxiety score (A) and anxiety rate (B) in cancer patients.
3.5 Effect of RTIP on depression
A total of 15 studies compared depression scores between the RTIP group and the control group. Data were heterogeneous (I2 = 90.1%, P < 0.001). The depression score declined in the RTIP group compared with the control group [SMD (95% CI): −0.664 (−0.967, −0.361), P < 0.001; Figure 4A]. A total of studies reported depression rates in the RTIP group and control group without heterogeneity (I2 = 0.0%, P = 0.975). After pooled analysis, it was found that the depression rate was lower in the RTIP group compared to the control group [RR (95% CI): 0.632 (0.532, 0.750), P < 0.001; Figure 4B].
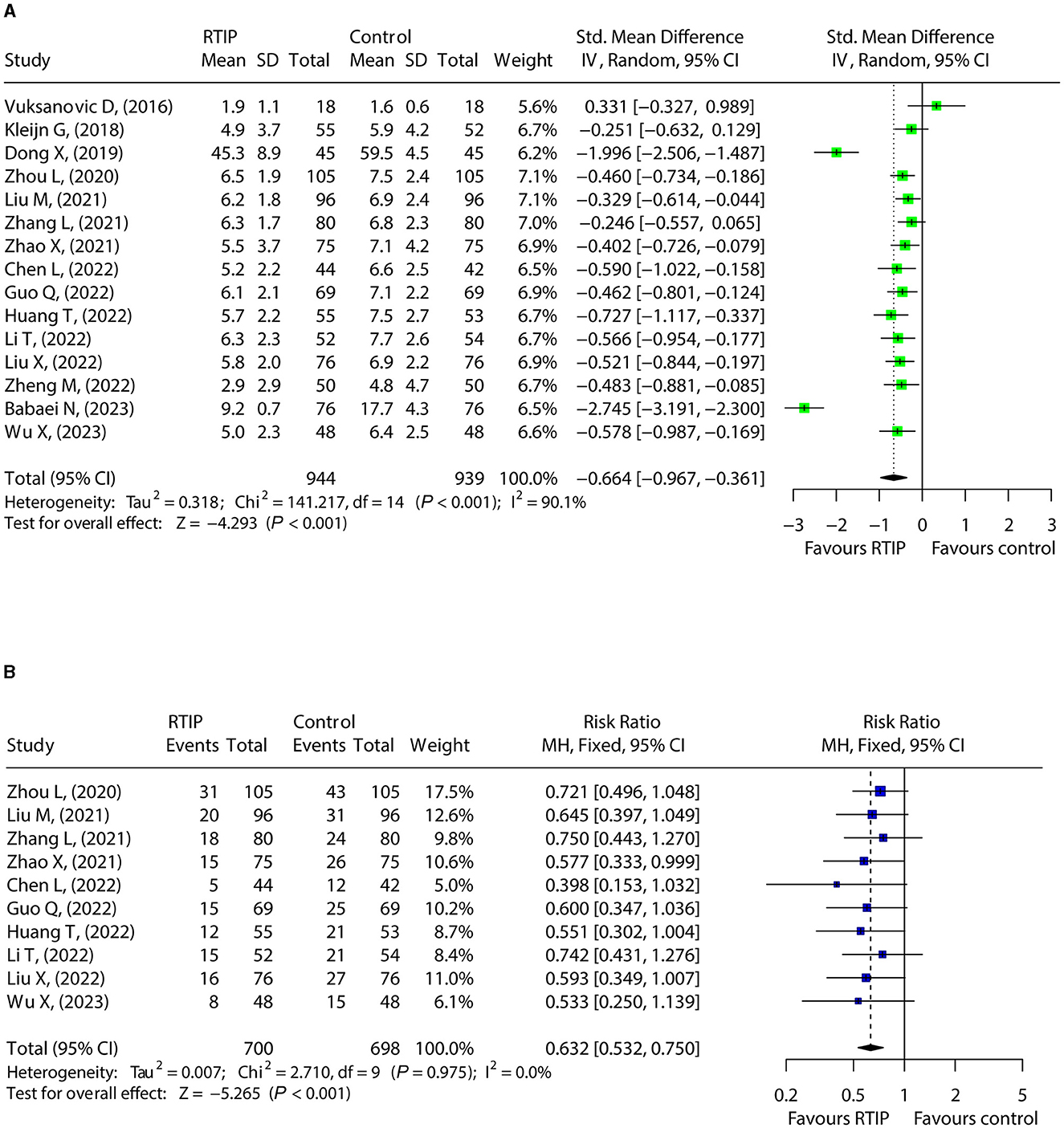
Figure 4. RTIP with or without control care reduced depression in cancer patients. Forest plot for the effect of RTIP on depression score (A) and depression rate (B) in cancer patients.
3.6 Effect of RTIP on overall quality of life
A total of 10 studies compared the overall quality of life between the RTIP and control groups, where heterogeneity existed (I2 = 63.7%, P = 0.003). The random effects model disclosed elevated overall quality of life in the RTIP group compared to the control group [SMD (95% CI): 0.501 (0.314, 0.689), P < 0.001; Figure 5].
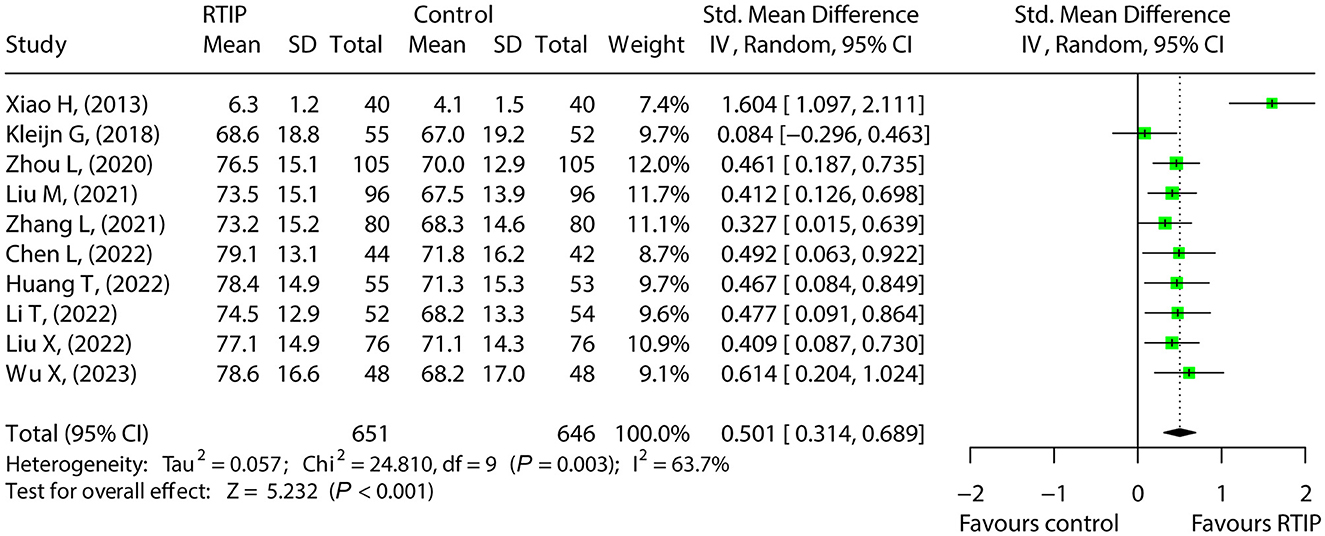
Figure 5. RTIP, with or without control care, elevates the overall quality of life of cancer patients.
3.7 Further analysis
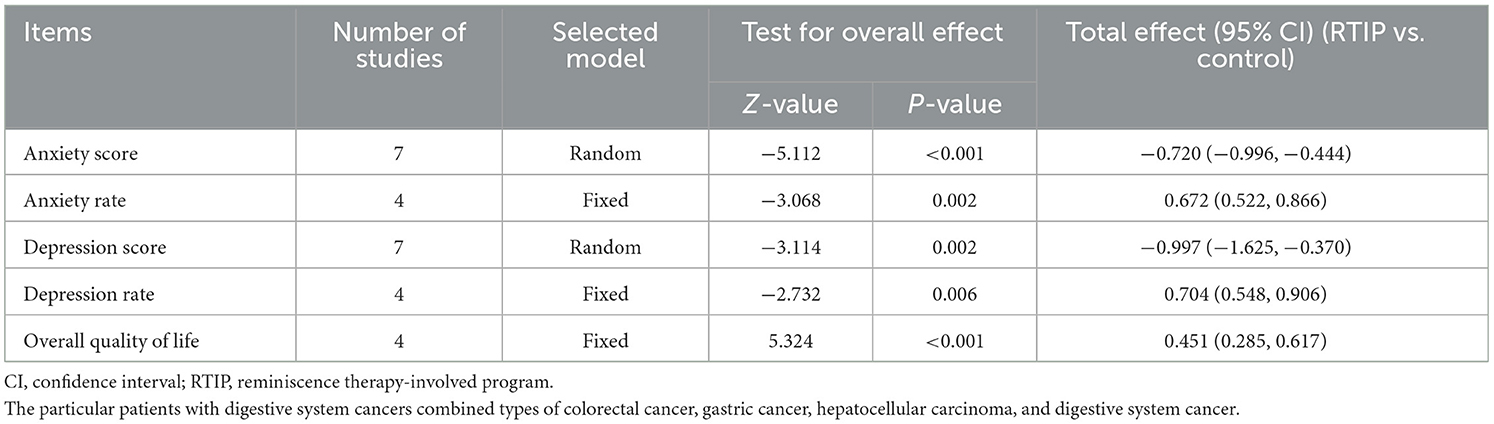
Respectively, 7, 4, 7, 4, and 4 studies compared anxiety score, anxiety rate, depression score, depression rate, and overall quality of life of digestive system cancer patients between the RTIP group and the control group. It was observed that in digestive system cancer patients, anxiety score [SMD (95% CI): −0.720 (−0.996, −0.444), P < 0.001], anxiety rate [RR (95% CI): 0.672 (0.522, 0.866), P = 0.002], depression score [SMD (95% CI): −0.997 (−1.625, −0.370), P = 0.002], and depression rate [RR (95% CI): 0.704 (0.548, 0.906), P = 0.006] was declined, and overall quality of life [SMD (95% CI): 0.451 (0.285, 0.617), P < 0.001] was increased in the RTIP group compared to the control group (Table 4).
We have also conducted moderator analysis based on sessions of intervention and practice approach (Supplementary Table 2). The data showed that the RTIP group had lower anxiety scores, depression scores, and depression rates, as well as higher overall quality of life compared with the control group in studies with sessions of intervention ≤12 or >12. However, the anxiety rate was only lower in the RTIP group compared with the control group in studies with sessions of intervention >12. Regarding practice approach, both studies with hospital-based practice approach or others illustrated a lower anxiety score and higher overall quality of life in the RTIP group compared with the control group, while the depression score was only reduced in the RTIP group compared with the control group in studies with the hospital-based practice approach.
4 Discussion
Reminiscence therapy is a process in which individuals reflect on their lives and past experiences with the aid of music, photographs, videos, and other props. This therapy traces the core theory of “life review,” which can help promote a sense of integrity and adjustment (Zhong et al., 2023). As a non-pharmacological intervention, reminiscence therapy typically targets older adults with mental health difficulties.
However, its application in cancer patients has attracted increasing attention (Guo et al., 2022; Zheng et al., 2022; Wu and Zhang, 2023; Yan et al., 2023). For example, one study demonstrated that reminiscence therapy decreases both anxiety and depression scores in the first month and sixth months after intervention compared to routine care in patients with digestive system cancer (Zheng et al., 2022). Another study discloses reduced anxiety and depression in elderly lung cancer patients treated with reminiscence therapy compared with those receiving usual care (Guo et al., 2022). This meta-analysis found that RTIP with or without control care reduced the score and rate of anxiety and depression compared to control care in cancer patients. The probable explanations were as follows: (i) The procedure of RTIP involved the recall and sharing of selected personal memories and stories, which facilitated a more positive view of life (Kleijn et al., 2018). (ii) In addition, RTIP also drew past, present, and future together, which contributed to ego integrity and assisted patients in adapting to disease-related losses. (iii) During the process of RTIP, cancer patients perceived caring and support from the medical workers, which reduced their feelings of isolation (Laidlaw et al., 2023). Combining these aspects, RTIP with or without control care attenuated the score and rate of anxiety and depression compared to control care in cancer patients.
Impaired quality of life is another common concern in cancer patients (Suarez-Almazor et al., 2021). One previous study identifies that reminiscence therapy elevates the QLQ-C30 global health status score compared with usual control in recurrent gastric cancer patients (Wu and Zhang, 2023). Another clinical study noted that the overall quality of life does not vary between reminiscence therapy and usual care in cancer patients (Kleijn et al., 2018). The meta-analysis elucidated that RTIP with or without control care elevated the overall quality of life compared to control care in cancer patients. The possible reasons might be that symptoms of anxiety and depression adversely affect the overall quality of life (Polanski et al., 2018; van Montfort et al., 2020; Carbajal-Lopez et al., 2022). However, as described above, RTIP effectively alleviated anxiety and depression in cancer patients, which led to improved psychological wellbeing. Subsequently, the overall quality of life was improved in cancer patients who underwent RTIP.
Besides, it is worth discussing that RTIP can be conducted individually, one-on-one with a therapeutic listener, or in a group form, and the choice of modality is controversial. Some clinicians think that the treatment effect may be compromised in a group setting, as patients may not be willing to share their privacy and personal feelings with others (Ando et al., 2007). Conversely, other medical workers argue that RTIP in a group setting is beneficial for both patients and implementers. Patients can encourage each other and build closer social relationships, while the group setting allows for more efficient use of resources for the implementers compared to one-on-one sessions (Rubin et al., 2019).
Therefore, further research is needed to address these differing perspectives. Another important consideration is that implementing RTIP requires additional medical resources. Therefore, relevant studies are warranted to explore whether the clinical benefits of patients outweigh the medical costs of such interventions.
The current meta-analysis also conducted moderator analysis based on the sessions of intervention sessions (≤ 12 or >12) and the practice approach (hospital-based or others). The data suggested that the effect of RTIP on the anxiety score and overall quality of life was not affected by the number of intervention sessions or the practice approach. However, RTIP showed no effect on anxiety rate in studies with intervention sessions ≤12 and on depression scores in studies using non-hospital-based approaches. These findings indicate that RTIP might be more effective with intervention sessions >12 and a hospital-based approach. Therefore, clinicians might consider encouraging patients to undergo hospital-based RTIP with longer intervention sessions to maximize the effectiveness of this treatment.
A previous meta-analysis of RCTs revealed that reminiscence therapy reduced anxiety and depression scores while promoting overall quality of life in patients with cancers; however, this previous meta-analysis only included studies published before 2021 (Sun et al., 2023). Therefore, we conducted an updated meta-analysis and found similar findings: RTIP decreased anxiety and depression and improved the overall quality of life in cancer patients. Based on these meta-analyses, the application of RTIP could be recommended in cancer patients to improve psychological health and overall quality of life, especially using a hospital-based approach with longer intervention sessions. Despite the overall good quality of evidence and the absence of no publication bias in each outcome, some limitations should be mentioned. First, blinding was difficult to implement, resulting in a high risk or unclear risk of performance bias in the included studies. Second, the sample size of most included studies was relatively small.
Consequently, larger-scale studies should be conducted to verify these findings. Third, due to the limited amount of evidence, the influence of some particular intervention details, such as RTIP session compositions, length, and frequency, on treatment efficacy could not be evaluated in this meta-analysis. Fourth, due to the limited number of studies, subgroup analysis in patients with cancers other than the digestive system could not be performed. Future studies should investigate the effects of RTIP in patients with other types of cancers. Fifth, articles published in other languages might have been excluded. Further studies could consider using artificial intelligence to bridge the language gap. Finally, since the data based on age, sample size, and different reminiscence content could not be combined, a moderator analysis based on these variables could not be performed.
In summary, RTIP efficiently improves the psychological health and overall quality of life in cancer patients. This therapy can be included in oncology care plans to meet multidimensional care needs and enhance the general health condition of cancer patients. Future studies should consider investigating whether different materials used in the intervention, different facilitators, and the frequency of intervention could affect the outcomes of RTIP in cancer patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XS: Data curation, Investigation, Methodology, Writing – original draft. WS: Data curation, Formal analysis, Methodology, Visualization, Writing – original draft. MY: Data curation, Formal analysis, Methodology, Resources, Writing – original draft. LX: Conceptualization, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1408941/full#supplementary-material
References
Abrams, H. R., Durbin, S., Huang, C. X., Johnson, S. F., Nayak, R. K., Zahner, G. J., et al. (2021). Financial toxicity in cancer care: origins, impact, and solutions. Transl. Behav. Med. 11, 2043–2054. doi: 10.1093/tbm/ibab091
Ando, M., Tsuda, A., and Morita, T. (2007). Life review interviews on the spiritual well-being of terminally ill cancer patients. Support Care Cancer 15, 225–231. doi: 10.1007/s00520-006-0121-y
Babaei, N., Zamanzadeh, V., Pourabbasi, M., Avazeh, M., and Shokoufamanesh, A. (2023). The effect of virtual reminiscence therapy on depression and anxiety in patients with gastric cancer undergoing chemotherapy. Support Care Cancer 32:64. doi: 10.1007/s00520-023-08268-3
Bray, F., Laversanne, M., Sung, H., Ferlay, J., Siegel, R. L., Soerjomataram, I., et al. (2024). Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74, 229–263. doi: 10.3322/caac.21834
Carbajal-Lopez, E. B., Juarez-Garcia, D. M., Sanchez-Jauregui, T. J., Espinoza-Velazco, A., Calderillo-Ruiz, G., Salas-Benavides, R., et al. (2022). Psychological distress, fatigue and quality of life in patients with gastrointestinal stromal tumors. Psychol. Russ. 15, 3–13. doi: 10.11621/pir.2022.0201
Chen, L., Yang, X., Ren, X., and Lin, Y. (2022). Reminiscence therapy care program as a potential nursing intervention to relieve anxiety, depression, and quality of life in older papillary thyroid carcinoma patients: a randomized, controlled study. Front. Psychol. 13:1064439. doi: 10.3389/fpsyg.2022.1064439
Cuevas, P. E. G., Davidson, P. M., Mejilla, J. L., and Rodney, T. W. (2020). Reminiscence therapy for older adults with Alzheimer's disease: a literature review. Int. J. Ment. Health Nurs. 29, 364–371. doi: 10.1111/inm.12692
Dong, X., Sun, G., Zhan, J., Liu, F., Ma, S., Li, P., et al. (2019). Telephone-based reminiscence therapy for colorectal cancer patients undergoing postoperative chemotherapy complicated with depression: a three-arm randomised controlled trial. Support. Care Cancer 27, 2761–2769. doi: 10.1007/s00520-018-4566-6
Emery, J., Butow, P., Lai-Kwon, J., Nekhlyudov, L., Rynderman, M., Jefford, M., et al. (2022). Management of common clinical problems experienced by survivors of cancer. Lancet 399, 1537–1550. doi: 10.1016/S0140-6736(22)00242-2
Fu, Y., Shi, W., Zhao, J., Cao, X., Cao, Y., Lei, M., et al. (2023). Prediction of postoperative health-related quality of life among patients with metastatic spinal cord compression secondary to lung cancer. Front. Endocrinol. 14:1206840. doi: 10.3389/fendo.2023.1206840
Guo, Q., Li, T., Cao, T., and Ma, C. (2022). Reminiscence therapy involved care programs as an option to improve psychological disorders and patient satisfaction in elderly lung cancer patients: a randomized, controlled study. J. Cancer Res. Ther. 18, 1937–1944. doi: 10.4103/jcrt.jcrt_425_22
Henson, L. A., Maddocks, M., Evans, C., Davidson, M., Hicks, S., Higginson, I. J., et al. (2020). Palliative care and the management of common distressing symptoms in advanced cancer: pain, breathlessness, nausea and vomiting, and fatigue. J. Clin. Oncol. 38, 905–914. doi: 10.1200/JCO.19.00470
Huang, T., Su, H., Zhang, S., and Huang, Y. (2022). Reminiscence therapy-based care program serves as an optional nursing modality in alleviating anxiety and depression, improving quality of life in surgical prostate cancer patients. Int. Urol. Nephrol. 54, 2467–2476. doi: 10.1007/s11255-022-03282-6
Jiang, H., Lyu, J., Mou, W., Jiang, Q., and Du, J. (2023). Association between financial toxicity and health-related quality of life in cancer survivors: a systematic review. Asia Pac. J. Clin. Oncol. 19, 439–457. doi: 10.1111/ajco.13901
Kleijn, G., Lissenberg-Witte, B. I., Bohlmeijer, E. T., Steunenberg, B., Knipscheer-Kuijpers, K., Willemsen, V., et al. (2018). The efficacy of life review therapy combined with memory specificity training (LRT-MST) targeting cancer patients in palliative care: a randomized controlled trial. PLoS ONE 13:e0197277. doi: 10.1371/journal.pone.0197277
Laidlaw, R. J., McGrath, R., Adams, C., Kumar, S., and Murray, C. M. (2023). Improved mental health, social connections and sense of self: a mixed methods systematic review exploring the impact and experience of community reminiscence programs. J. Multidiscip. Healthc. 16, 4111–4132. doi: 10.2147/JMDH.S438730
Li, T., Li, B., Tan, L., and Lv, B. (2022). Reminiscence therapy as a potential method to improve psychological health and quality of life in elderly hepatocellular carcinoma patients: a randomized, controlled trial. Front. Surg. 9:873843. doi: 10.3389/fsurg.2022.873843
Li, Y., Long, Z., Wang, X., Lei, M., Liu, C., Shi, X., et al. (2022). A novel nomogram to stratify quality of life among advanced cancer patients with spinal metastatic disease after examining demographics, dietary habits, therapeutic interventions, and mental health status. BMC Cancer 22:1205. doi: 10.1186/s12885-022-10294-z
Liang, Y., Hao, G., Wu, M., and Hou, L. (2022). Social isolation in adults with cancer: an evolutionary concept analysis. Front. Psychol. 13:973640. doi: 10.3389/fpsyg.2022.973640
Licu, M., Ionescu, C. G., and Paun, S. (2023). Quality of life in cancer patients: the modern psycho-oncologic approach for romania-a review. Curr. Oncol. 30, 6964–6975. doi: 10.3390/curroncol30070504
Liu, M., and Li, Y. (2021). Reminiscence therapy-based care program relieves anxiety, depression, and improves quality of life in post-operational non-small cell lung cancer patients. Clin. Respir. J. 15, 472–481. doi: 10.1111/crj.13323
Liu, X., Yuan, K., Ye, X., and Liu, R. (2022). Proposing a novel care program: reminiscence therapy involved care for anxiety, depression, and quality of life in postoperative cervical cancer patients. Ir. J. Med. Sci. 191, 2019–2027. doi: 10.1007/s11845-021-02728-7
Morrison, E. J., Novotny, P. J., Sloan, J. A., Yang, P., Patten, C. A., Ruddy, K. J., et al. (2017). Emotional problems, quality of life, and symptom burden in patients with lung cancer. Clin. Lung Cancer 18, 497–503. doi: 10.1016/j.cllc.2017.02.008
Mullen, L., Signorelli, C., Nekhlyudov, L., Jacobsen, P. B., Gitonga, I., Estape, T., et al. (2023). Psychosocial care for cancer survivors: a global review of national cancer control plans. Psychooncology 32, 1684–1693. doi: 10.1002/pon.6218
Polanski, J., Chabowski, M., Chudiak, A., Uchmanowicz, B., Janczak, D., Rosinczuk, J., et al. (2018). Intensity of anxiety and depression in patients with lung cancer in relation to quality of life. Adv. Exp. Med. Biol. 1023, 29–36. doi: 10.1007/5584_2017_50
Renna, M. E., Shrout, M. R., Madison, A. A., Alfano, C. M., Povoski, S. P., Lipari, A. M., et al. (2022). Depression and anxiety in colorectal cancer patients: ties to pain, fatigue, and inflammation. Psychooncology 31, 1536–1544. doi: 10.1002/pon.5986
Rubin, A., Parrish, D. E., and Miyawaki, C. E. (2019). Benchmarks for evaluating life review and reminiscence therapy in alleviating depression among older adults. Soc. Work 64, 61–72. doi: 10.1093/sw/swy054
Schwarzer, G., Carpenter, J., and Rücker, G. (2015). Meta-Analysis With R [M]. Springer International Publishing. doi: 10.1007/978-3-319-21416-0
Smallfield, S., Metzger, L., Green, M., Henley, L., and Rhodus, E. K. (2024). Occupational therapy practice guidelines for adults living with Alzheimer's disease and related neurocognitive disorders. Am. J. Occup. Ther. 78:7801397010. doi: 10.5014/ajot.2024.078101
Suarez-Almazor, M., Pinnix, C., Bhoo-Pathy, N., Lu, Q., Sedhom, R., Parikh, R. B., et al. (2021). Quality of life in cancer care. Med. 2, 885–888. doi: 10.1016/j.medj.2021.07.005
Sun, J., Jiang, J., Wang, Y., Zhang, M., Dong, L., Li, K., et al. (2023). The efficacy of reminiscence therapy in cancer-related symptom management: a systematic review and meta-analysis. Integr. Cancer Ther. 22:15347354221147499. doi: 10.1177/15347354221147499
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., et al. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. doi: 10.3322/caac.21660
Tam, W., Poon, S. N., Mahendran, R., Kua, E. H., and Wu, X. V. (2021). The effectiveness of reminiscence-based intervention on improving psychological well-being in cognitively intact older adults: a systematic review and meta-analysis. Int. J. Nurs. Stud. 114:103847. doi: 10.1016/j.ijnurstu.2020.103847
van Montfort, E., de Vries, J., Arts, R., Aerts, J. G., Kloover, J. S., Traa, M. J., et al. (2020). The relation between psychological profiles and quality of life in patients with lung cancer. Support. Care Cancer 28, 1359–1367. doi: 10.1007/s00520-019-04923-w
Vuksanovic, D., Green, H. J., Dyck, M., and Morrissey, S. A. (2017). Dignity therapy and life review for palliative care patients: a randomized controlled trial. J. Pain Symptom Manage. 53, 162–170. e1. doi: 10.1016/j.jpainsymman.2016.09.005
Wagland, R., Richardson, A., Armes, J., Hankins, M., Lennan, E., Griffiths, P., et al. (2015). Treatment-related problems experienced by cancer patients undergoing chemotherapy: a scoping review. Eur. J. Cancer Care 24, 605–617. doi: 10.1111/ecc.12246
Wang, X., Wang, N., Zhong, L., Wang, S., Zheng, Y., Yang, B., et al. (2020). Prognostic value of depression and anxiety on breast cancer recurrence and mortality: a systematic review and meta-analysis of 282,203 patients. Mol. Psychiatry 25, 3186–3197. doi: 10.1038/s41380-020-00865-6
Wu, I. H. C., Balachandran, D. D., Faiz, S. A., Bashoura, L., Escalante, C. P., Manzullo, E. F., et al. (2022). Characteristics of cancer-related fatigue and concomitant sleep disturbance in cancer patients. J. Pain Symptom Manage. 63, e1–e8. doi: 10.1016/j.jpainsymman.2021.07.025
Wu, X., and Zhang, W. (2023). Reminiscence therapy-based care program alleviates anxiety and depression, as well as improves the quality of life in recurrent gastric cancer patients. Front. Psychol. 14:1133470. doi: 10.3389/fpsyg.2023.1133470
Xiao, H., Kwong, E., Pang, S., and Mok, E. (2013). Effect of a life review program for Chinese patients with advanced cancer: a randomized controlled trial. Cancer Nurs. 36, 274–283. doi: 10.1097/NCC.0b013e318268f7ba
Yan, Z., Dong, M., Lin, L., and Wu, D. (2023). Effectiveness of reminiscence therapy interventions for older people: evidence mapping and qualitative evaluation. J. Psychiatr. Ment. Health Nurs. 30, 375–388. doi: 10.1111/jpm.12883
Zeng, X., Zhang, Y., Kwong, J. S., Zhang, C., Li, S., Sun, F., et al. (2015). The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J. Evid. Based Med. 8, 2–10. doi: 10.1111/jebm.12141
Zhang, L., Li, Y., Kou, W., Xia, Y., Yu, X., Du, X., et al. (2021). Reminiscence therapy exhibits alleviation of anxiety and improvement of life quality in postoperative gastric cancer patients: a randomized, controlled study. Medicine 100:e26821. doi: 10.1097/MD.0000000000026821
Zhao, X. (2021). Reminiscence therapy-based care program for reducing anxiety and depression in glioma survivors: a randomized controlled trial. Medicine 100:e23056. doi: 10.1097/MD.0000000000023056
Zheng, M., Zhang, X., and Xiao, H. (2022). Effects of a WeChat-based life review program for patients with digestive system cancer: 3-arm parallel randomized controlled trial. J. Med. Internet Res. 24:e36000. doi: 10.2196/36000
Zheng, W., Lei, M., Liu, Y., Lu, X., Yu, D., Zhang, X., et al. (2020). An algorithm to stratify the risk of postoperative emotional distress in cancer patients with advanced metastatic spinal disease. Psychol. Res. Behav. Manag. 13, 721–731. doi: 10.2147/PRBM.S261613
Zhong, Q., Chen, C., and Chen, S. (2023). Effectiveness on quality of life and life satisfaction for older adults: a systematic review and meta-analysis of life review and reminiscence therapy across Settings. Behav. Sci. 13:830. doi: 10.3390/bs13100830
Keywords: reminiscence therapy-involved program, cancer patients, anxiety and depression, quality of life, meta-analysis
Citation: Sun X, Su W, Yin M and Xia L (2024) Effects of a reminiscence therapy-involved program on anxiety, depression, and the quality of life in cancer patients: a meta-analysis of randomized controlled trials. Front. Psychol. 15:1408941. doi: 10.3389/fpsyg.2024.1408941
Received: 29 March 2024; Accepted: 25 July 2024;
Published: 17 September 2024.
Edited by:
Srinivasa Murthy, National Institute of Mental Health and Neurosciences (NIMHANS), IndiaReviewed by:
Yaosheng Liu, Chinese PLA General Hospital, ChinaJazmin Hernandez, National Autonomous University of Mexico, Mexico
Hsin-Yen Yen, Taipei Medical University, Taiwan
Copyright © 2024 Sun, Su, Yin and Xia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Xia, bGluZ3hpYXpiQDE2My5jb20=
 Xingliang Sun
Xingliang Sun Ling Xia
Ling Xia