- 1Department of Clinical and Experimental Medicine, University of Messina, Messina, Italy
- 2Department of Health Sciences, University Magna Graecia of Catanzaro, Catanzaro, Italy
- 3Department of Cognitive Science, Psychology, Education and Cultural Studies, University of Messina, Messina, Italy
- 4Department of Endocrinology and Metabolism, Rigshospitalet, Copenhagen, Denmark
- 5Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, Messina, Italy
- 6Institute for Biomedical Research and Innovation (IRIB), National Research Council of Italy (CNR), Messina, Italy
Background: Growing evidence reveals the important role of clinical psychological factors in chronic-immune diseases. The aim of this study was to investigate Health-Related Quality of Life (HR-QoL), depression, anxiety, and alexithymia in patients with severe hypersensitivity reactions such as Severe Allergic Asthma (SAA) and Hymenoptera Venom Anaphylaxis (HVA).
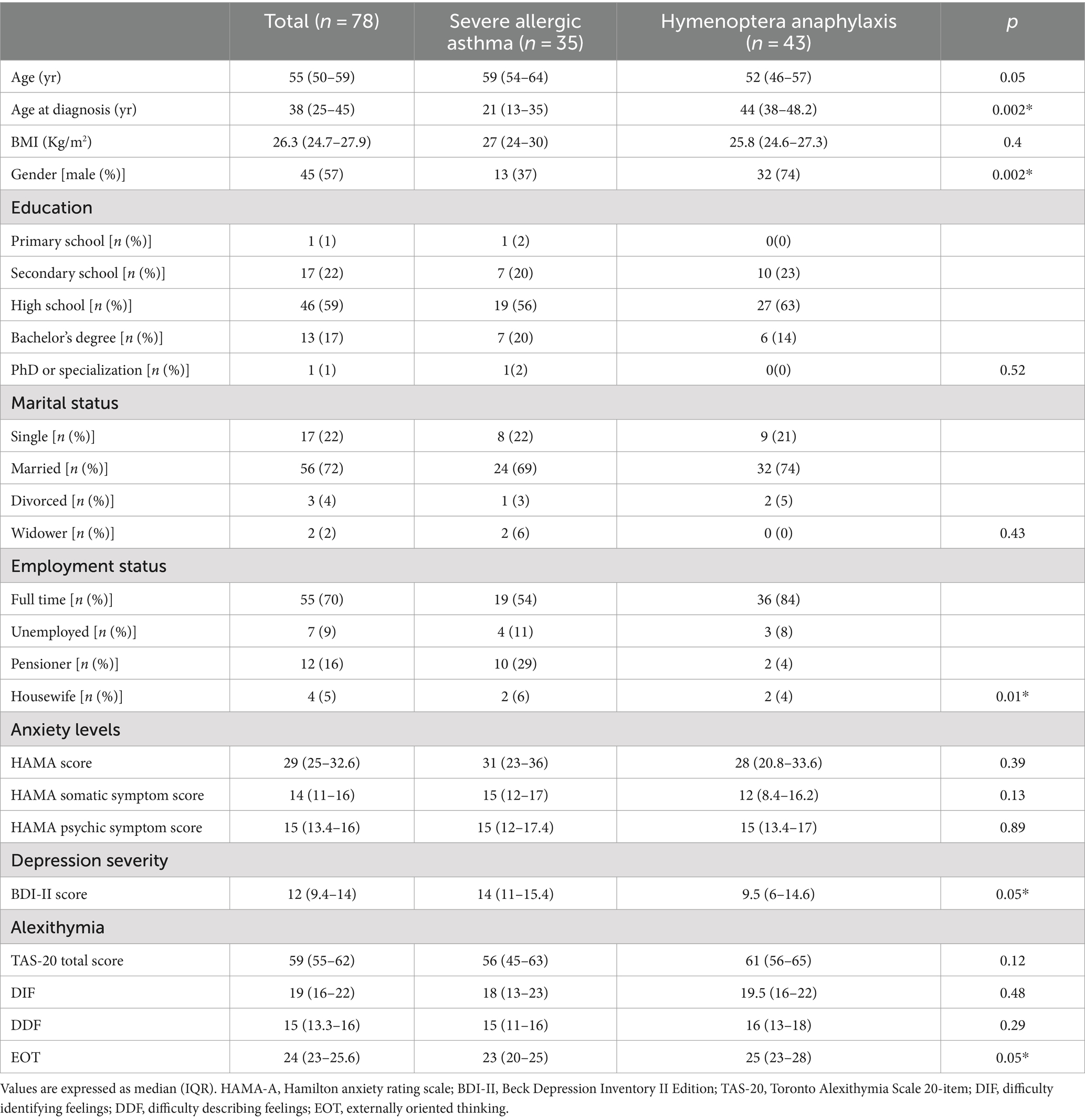
Methods: The Short-Form Health Survey-36 (SF-36), the Beck Depression Inventory Questionnaire (BDI-II), the Hamilton Anxiety Rating Scale (HAM-A) and the Toronto Alexithymia Scale (TAS-20) were used to assess HR-QoL and clinical psychological features of patients with SAA and HVA.
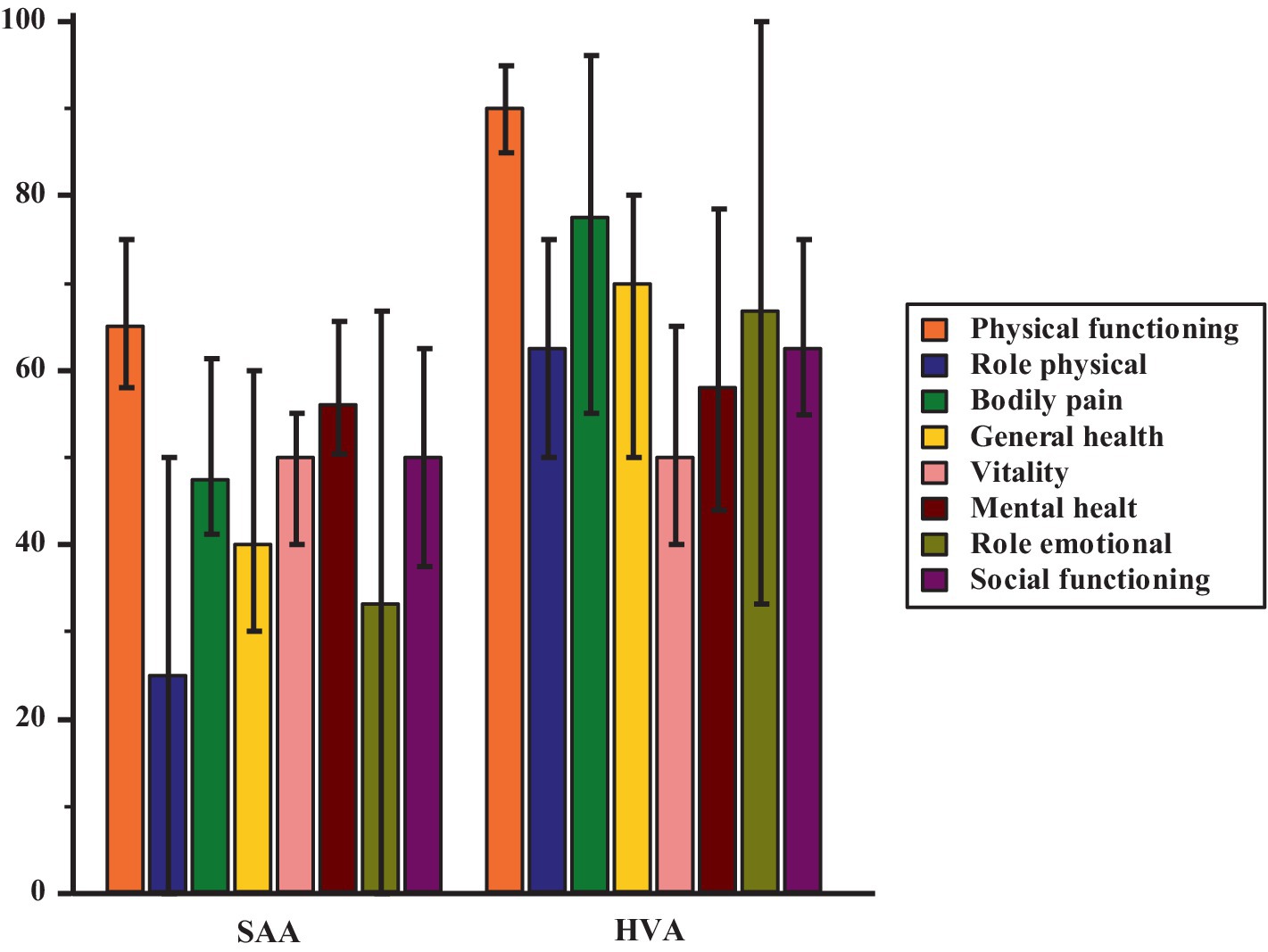
Results: Overall, 78 patients were recruited. Patients with SAA (n = 35) reported lower scores for physical functioning [65 (58–75) vs. 90 (85–95); p = <0.001], role limitations due to physical health [25 (0–50) vs. 62 (50–75); p = 0.004], bodily pain [47.5 (41.1–61.3) vs. 55.5 (55–96); p = 0.001], general health [40 (30–60) vs. 70 (50–80); p = 0.0003] and social functioning [50 (37.5–62.5) vs. 62.5 (54.9–75); p = 0.007] while higher scores for depressive symptoms [14 (11–15.4) vs. (9.5 (6–15.4); p = 0.05)] compared to HVA patients (n = 43). All the dimensions of SF-36 were negatively correlated with anxiety (r from −0.26 to −0.66; pall < 0.01) and depressive symptoms (r from −0.44 to −0.73; pall < 0.001). Alexithymia was negatively correlated with vitality (r = −0.28; p = 0.02) and mental health (r = −027; p = 0.03). Additionally, patients with alexithymia (38% of participants) showed higher levels of depressive symptoms [9.5 (10–19) vs. 14 (6–13.9); p = 0.005] and anxiety levels [31 (27.9–35) vs. 24 (16–33.9); p = 0.02]; they also showed less vitality [40 (39.9–50) vs. 55 (50–60) p = 0.01], social functioning [50 (37.5–62.5) vs. 62.5 (50 vs. 75); p = 0.01] and mental health [48 (44–60) vs. 68 (56–76); p = 0.004].
Conclusion: Clinical psychological features due to severe hypersensitive reactions may contribute to the patient’s perceived HR-QoL. Focused clinical psychological interventions should be promoted to improve the clinical management of such conditions.
1 Introduction
Empirical evidence suggests that chronic diseases may impact psychological well-being, increasing the risk of morbidity with incident psychopathologies, such as depression and anxiety (Di Giuseppe and Conversano, 2022; Isvoranu et al., 2021; Lin et al., 2022). Chronic illness represents a challenge for patients and requires continuous adjustment in the management of daily life (Merlo, 2019; Braido, 2013; van Houtum et al., 2015).
Asthma is a chronic respiratory disease characterized by persistent airway inflammation and airway stiffening, resulting in variable difficulty in breathing (World Health Organization, 2019). Asthma appears with heterogeneous and variable symptomatology, including airway secretion, shortness of breath, wheezing, chest pain, and coughing attacks (Braido, 2013; Louis et al., 2023). For these reasons the Global Initiative for Asthma (2023) classifies asthma based on the control of symptoms and distinguishes between well-controlled or uncontrolled asthma, the latter is characterized by the presence of frequent symptoms’ exacerbations, requiring timely use of oral corticosteroids (OCS) or hospitalization.
Severe Asthma (SA) is a subtype of difficult-to-treat asthma, characterized by poor symptoms control despite adherence to a correctly prescribed maximal inhaler with high-dose inhalant corticosteroids (ICS) and beta2 long-acting agents’ (LABA) treatment (Bagnasco et al., 2021; Ricciardi et al., 2023). Patients with SA represent about 5–10% of the asthma population (Chung et al., 2014). SA is characterized by low lung function, immune dysregulation, and frequent exacerbations, with life-threatening asthma attacks (Backman et al., 2019). For these reasons, asthma is one of the major public health issues worldwide and causes a significant social and economic burden (Mortimer et al., 2022; López-Tiro et al., 2022). Severe allergic asthma (SAA) patients have chronic allergic asthma due to immunoglobulin E (IgE)-mediated sensitization to inhalant allergens, prevalently Dust Mites or, in Southern Italy, to Parietaria Judaica pollens (Liotta et al., 2023).
In this context we would mention the not-negligible incidence of asthma in workers, as occupational asthma represents an important environmental workplace disease, especially in outdoor workers. Several organic, inorganic and xenobiotic substances may provoke immunoreactions with consequences on the respiratory system, even resulting in occupational asthma (Toletone et al., 2016; Ruëff et al., 2023). Previous literature has also highlighted how occupational asthma influences workers’ perceived quality of life of also concerning syndromes characterized by depression and anxiety (Suarthana et al., 2023; Del Roio et al., 2023).
Gruffydd-Jones et al. (2019) in a multinational survey, analyzing 1.598 patients with poor control of asthma symptoms despite long-term treatment, highlighted a significant reduction in work productivity with a negative impact on emotional well-being at work. Empirical evidence suggests that SA and occupational asthma are associated with low perceived Health-Related Quality of Life (HR-QoL) (Hossny et al., 2017; Bagnasco et al., 2021; Wang et al., 2020), psychological distress (Patella et al., 2022) and significant risk of psychiatric comorbidity, such as anxiety and depression (Roche et al., 2022). Additionally, recent research (Silvestro et al., 2023; Ricciardi et al., 2023) suggests that patients with SA and SAA may present a low awareness to identify and describe one’s feelings, experiencing a clinical condition known as alexithymia which negatively impacts the disease course (Nemiah et al., 1976).
Hymenoptera venom allergy is a typical IgE-mediated disease, provoked by bees or wasps, causing several symptoms including urticaria, angioedema, flushing, itching, hypotension, and anaphylaxis (Sturm et al., 2018): a systemic allergic reaction due to HVA may develop within minutes from a sting and in some cases, it can be potentially life-threatening leading to cardiorespiratory arrest (Schiener et al., 2017). Although there is a lack of epidemiological data, a European multicenter study estimated that about 48.2% of severe hypersensitivity reactions in adults (>18 years old) are caused by insect stings (Worm et al., 2014). Additionally, Pastorello et al. (2001) reported a death range per year due to HVA from 0.03 to 0.48% out of a population of 1,000,000 subjects.
Patients who have experienced anaphylaxis following Hymenoptera stinging have been found to present psychological distress (Schoeben et al., 2020; Ricciardi et al., 2018; Giorgianni et al., 2024). HVA may cause, fear of being stung again by an insect, anxiety, uncertainty, restrictions in social life and everyday activities, therefore leading to a lower HR-QoL (Höfer et al., 2023; Schaarschmidt et al., 2018).
Few study have investigated HVA related to the role of occupational exposure, but it would be appropriate to provide useful information to high risk outdoor workers to correctly manage environmental exposure to hymenoptera stings. Observational studies on populations of HVA subjects have documented that outdoor workers have greatest risk of occasional hymenoptera (Toletone et al., 2016). Since little evidence exists about the crucial role of clinical psychological factors in patients with severe hypersensitivity reactions, the present research study aims to: (1) investigate HR-QoL and clinical psychological characteristics in patients with a history of severe allergic diseases, including SAA and HVA; (2) analyze the clinical-psychological differences between SAA and HVA and (3) evaluate the associations of clinical-psychological features in these severe allergic diseases.
A greater understanding of the psychological complexity of patients suffering from SAA and HVA could promote a greater awareness of the integrated approach needed in such chronic diseases.
2 Methods
2.1 Participants
This cross-sectional study included 78 patients with a history of severe hypersensitivity reactions, 35 with SAA and 43 with HVA, who referred to the Outpatients Clinic for Allergy and Clinical Immunology at the Department of Clinical and Experimental Medicine of the University Hospital of Messina, Italy between January and May 2022. All SAA patients were treated with Omalizumab, an anti-IgE biologic treatment, in addition to high dose ICS + LABA, while HVA patients were under venom allergen immunotherapy (VAIT), 6 with bee venom extract and 37 with wasp venom extract (ALK, Alutard, Milan). Exclusion criteria were age under 18 years, cognitive decline, moderate to severe kidney or liver failure, heart failure with NYHA (New York Heart Association) class ≥2, cancer, malabsorption, endocrine disorders of thyroid, parathyroid or adrenal glands, and known psychopathological diseases and psychotropic drugs assumption.
2.2 Ethics statement
The research will be carried out following the Declaration of Helsinki (World Medical Association, 2013). Ethical approval was obtained from the Ethics Committee of the University Hospital of Messina University (Protocol number 16/19). All patients were informed about privacy and the use of anonymous data for research purposes and signed an informed consent according to the European General Data Protection Regulation 2016/679.
2.3 Clinical evaluation
A psychological assessment was conducted by a researcher in clinical psychology, performing a gold-standard clinical psychological interview and a psycho-diagnostics examination.
The Beck Depression Inventory, second edition (BDI-II), was administered to measure depressive symptoms (Beck et al., 1996; Ghisi et al., 2006). It consists of a self-report instrument, composed of 21 items scored on a four-point Likert scale. BDI-II detects both somatic-affective (e.g., agitation, sleep disorder, and loss of energy) and cognitive (e.g., pessimism, suicidal thoughts, self-criticalness) features of depression. In the present study, the Italian version of BDI-II was adopted, as it showed good proprieties and a bi-factorial structure with an α coefficient of 0.86 for cognitive/affective and 0.65 for somatic symptoms (Montano and Flebus, 2006).
The Hamilton Anxiety Rating Scale (HAM-A) was used to assess the severity of anxiety symptoms (Hamilton, 1959). It is a self-report questionnaire, consisting of 14 items scored on a five-point Likert scale. HAM-A presents a bi-factorial structure, detecting both somatic (e.g., respiratory, autonomic, gastrointestinal symptoms) and psychic components of anxiety (e.g., tension, fears and depressed mood). Previous research documented, good statistical proprieties, high reliability, and diagnostic accuracy for the Italian version of this scale (Martino et al., 2021; Scimeca et al., 2014).
The Italian version of the Short-Form Health Survey-36 (SF-36) was used to measure patients’ perceived HR-QoL. SF-36 is a self-administered questionnaire that detects eight dimensions of HR-QoL, comprising physical functioning, limitation due to physical role, bodily pain, general health, vitality, mental health, limitation due to emotional role and social functioning (Ware and Sherbourne, 1992). SF-36 presents a range score from 0 to 100; a lower score indicates a poorer HR-QoL. Previous studies confirmed the psychometric qualities of the scale on Italian clinical samples, with reliability (Cronbach’s α) for the eight factors ranging from 0.77 to 0.93 (Apolone and Mosconi, 1998).
The Toronto Alexithymia Scale-20 (TAS-20) was used to assess alexithymic traits (Taylor et al., 1997; Taylor, 2000; Bagby et al., 1994a). It consists of a self-report questionnaire, composed of 20 items scored on a five-point Likert scale. Three cut-off scores were identified to recognize alexithymic (≥61), borderline (51 to 60) and non-alexithymic (≤50) individuals (Bagby et al., 1994b). TAS-20 presents a three-factor structure that comprises the main features of alexithymia: difficulty identifying feelings (DIF), difficulty describing feelings (DDF) and externally oriented thinking (EOT). In the present study, the Italian version of TAS-20 was used; previous research highlighted a good propriety and reliability of the three factors structure (Cronbach’s α) considering a score of 0.86 for full scale and 0.83, 0.79, and 0.81 for DIF, DDF, EOT, respectively (Bressi et al., 1996).
2.4 Statistical analyses
Statistical analysis was performed using MedCalc software (version 10.2.0.0; Mariakerke, 173 Belgium). The Kolmogorov–Smirnov test was used to verify the normal distribution of values of studied variables. The entire sample was divided into groups according to the allergic disease and the presence (TAS-20 scores ≥61) or the absence of alexithymia and the Mann–Whitney test was used to observe any differences in the level of anxiety, depressive symptoms and QoL. The χ2 test was used to calculate differences in the proportion of categorical variables. Spearman correlation coefficient was applied to evaluate the degree of association between two variables. Finally, a multiple regression analysis was performed to explore the association between alexithymia, identified as the dependent variable, and the explanatory variables age, age at diagnosis, anxiety and depression. For all the tests used, the value of p < 0.05 was considered to indicate the statistical significance.
2.5 Results
The main socio-demographic and clinical characteristics of recruited patients are reported in Table 1. Overall, the median age of participants was 55 yrs., and the prevalent gender was male (57%). Participants showed moderate anxiety levels, mild depressive symptoms, conceivable alexithymia and low perceived HR-QoL. The age at diagnosis was significantly higher in patients with HVA in comparison with patients with SAA [44 (38–48.2) vs. 21 (13–35), p = 0.002, respectively]. Moreover, the HVA group presented a significant difference in the employment status in comparison with patients with SAA, particularly in the number of full-time workers (84% vs. 54%) respectively. Regarding clinical psychological features, both groups showed no significant differences in anxiety and alexithymia levels. However, the SAA group presented higher depressive symptoms levels in comparison with HVA patients [14 (11–15.4) vs. (9.5 (6–15.4); p = 0.05)]. On the other hand, patients in the HVA group showed higher levels of externally oriented thinking [25 (23–28) vs. 23 (20–25); p = 0.05]. Data on the SF-36 survey are reported in Figure 1; patients with SAA showed a lower score in physical functioning [65 (58–75) vs. 90 (85–95); p < 0.001], role limitations due to physical health [25 (0–50) vs. 62 (50–75); p = 0.004], bodily pain [47.5 (41.1–61.3) vs. 55.5 (55–96); p = 0.001], general health, [40 (30–60) vs. 70 (50–80); p = 0.0003] and social functioning [50 (37.5–62.5) vs. 62.5 (54.9–75); p = 0.007] in comparison to the HVA group. There were no statistically significant differences between the groups concerning vitality, role limitations due to emotional problems and mental health. Considering TAS-20 scores ≥61, it was observed that 29 (38%) participants exhibited clinically significant levels of alexithymia. Taking into account the presence (TAS-20 scores ≥61) or absence (TAS-20 <61) of alexithymia, it was highlighted that patients with alexithymia presented higher levels of depression [9.5 (10–19) vs. 14 (6–13.9); p = 0.005], anxiety, with particular regard to the psychic dimension [31 (27.9–35) vs. 24 (16–33.9); p = 0.02] and lower scores in vitality [40 (39.9–50) vs. 55 (50–60); p = 0.01], social functioning [50 (37.5–62.5) vs. 62.5 (50 vs. 75); p = 0.01] and mental health [48 (44–60) vs. 68 (56–76); p = 0.004] to the patients without alexithymia.
Overall, the number of explored clinical psychological morbidities was positively related to age (r = 0.48; p < 0.01), BMI (r = 0.34; p = 0.003) anxiety (r = 0.32; p = 0.01), depression (r = 025; p = 0.04); conversely, it was negatively associated with HR-QoL: physical functioning (r = −036; p = 0.004), limitations due to physical health (r = −0.37; p = 0.003), bodily pain (r = −0.35; p = 0.005) and general health (r = −0.38; p = 0.003). At correlation analysis, all the dimensions of SF-36 were negatively associated with age (r from −0.2 to −0.57; pall < 0.05), anxiety, both somatic and psychic (r from −0.26 to −0.66; pall < 0.01) and depressive symptoms (r from −0.44 to −0.73; pall < 0.001). Similar associations were observed when analyzing these variables in both groups separately. Moreover, considering the entire sample, TAS-20 was negatively correlated with vitality (r = −0.28; p = 0.02) and mental health (r = −027; p = 0.03), also DDF was negatively correlated with vitality (r = −028; p = 0.02) and mental health (r = −0.32; p = 0.01) and positively associated with depressive symptoms (r = 0.26; p = 0.04). Additionally, anxiety (somatic and psychic) was positively correlated with depressive symptoms (r = 0.61; p < 0.001). Only in the group of patients with SAA, the alexithymia total score was associated with anxiety (r = 0.36; p = 0.04), while DDF was correlated with depressive symptoms (r = 0.42; p = 0.01).
Finally, at multiple regression analysis which considered alexithymia as the dependent variable, and age, age at diagnosis, anxiety and depression as explanatory variables, only anxiety was significantly and independently associated with alexithymia in the SAA group (β = 0.4375; SE = 0.198; p = 0.03).
3 Discussion
This research highlights that patients with a history of severe allergic diseases, including SAA and HVA, show moderate anxiety levels, mild depressive symptoms, conceivable alexithymia and low perceived HR-QoL. The main results of this study indicate that the group of patients with SAA showed low HR-QoL in both physical and emotional dimensions. In line with this statement, empirical evidence underlined that the experience of living with SAA significantly impacts physical and emotional functioning, determining limitations in completing daily activities (McDonald et al., 2018), decrease in work performance (Hiles et al., 2018), and difficulty in managing leisure time and social activities (Dockrell et al., 2007).
Regarding differences between patients with SAA and with HVA, the first group reported lower results in all dimensions of the SF-36, except for vitality, limitations due to emotional role, and mental health. Both groups reported low-to-medium scores in these dimensions, highlighting the potential negative impact of these chronic conditions on patients’ psychological well-being. Concerning these results, we hypothesized that, if on the one hand the invalidating respiratory symptoms of SAA, most of all shortness of breath, may cause significant impairment in all dimensions of perceived HR-QoL, on the other hand, anaphylaxis experienced by patients with HVA can lead to uncertainty and fear of experiencing a new hypersensitivity reaction, with negative effects on psychological dimensions of HR-QoL in the long term. Tal et al. (2020), analyzing 44 patients with a history of anaphylaxis due to a Hymenoptera sting, highlighted a major susceptibility to symptoms of post-traumatic stress disorders in patients with local reactions, demonstrating that severe hypersensitivity reactions could compromise psychological health.
In the present study, no differences were found between the two disease groups for anxiety levels and alexithymia. However, patients with SAA presented more depressive symptoms than patients with HVA. Numerous evidence suggests comorbidity between asthma and depression (Zielinski et al., 2000; Gao et al., 2015; Lu et al., 2018). Meta-analysis of Jiang et al. (2014) highlighted that patients with depression are more likely to present in comorbidity asthma (3.17 times more) than healthy subjects. Similarly, patients with asthma are more likely to have depression as a comorbidity (1.52 times more). According to Medina-Rodriguez et al. (2018), patients with major depressive disorder present immune system alterations with significant changes in plasma cytokine levels. Therefore, the inflammatory response might represent a common pathway between allergic diseases such as asthma and mental disorders (Jiang et al., 2014; Lu et al., 2018).
Regarding the association between clinical psychological features and levels of HR-QoL, depression and anxiety, both somatic and psychic, were related to low HR-QoL, while higher levels of alexithymia were associated with reduced vitality and social function dimensions, in both groups. These findings confirmed the relevance of accurate psycho-diagnostic assessment to detect the presence of clinically significant features in both SAA and HVA patients (Conversano and Di Giuseppe, 2021; Adelmeyer et al., 2021; Esmaeel and Aly, 2019). A multidisciplinary clinical approach, both medical and psychological, could allow early detection of at-risk situations or identification of cases in which a mental disorder is already concluded, to ensure the most suitable patient-tailored treatment (Majellano et al., 2019; Cooley et al., 2022).
Furthermore, it would be appropriate to give indications on the correct risk management at work of subjects highly exposed to hymenoptera stings, both in the case of workers suffering from occupational asthma and for those with HVA. The risk of being affected by the exposure to environmental factors can be the cause of suffering among outdoor workers with the consequent development of depression and anxiety. In the coming researches it could be relevant to study further populations of outdoor workers in relation to what has emerged from our findings to provide guidelines on the management and prevention of such sufferings (Ruëff et al., 2023).
Depression, anxiety, and alexithymia have been associated with adverse health outcomes in several chronic conditions; regarding asthma, in the United States, Lin et al. (2022) highlighted that 14.16% of patients with asthma showed comorbidity with depression and the co-occurrence of asthma and depression was associated with major death risk than in asthmatic patients without depression. The presence of anxiety and/or depression in comorbidity with asthma was associated with poorer asthma control (Stubbs et al., 2022), higher corticosteroid dosage (McLoughlin and McDonald, 2021), greater frequency of exacerbation (Zhang et al., 2016) and greater healthcare use (Sastre et al., 2018). Regarding the correlation of HVA with depression and anxiety, Schaarschmidt et al. (2018), analysing 55 patients with HVA, found that 14.5% showed clinically significant levels of anxiety, while 5.5% had definite depressive disorder. Schoeben et al. (2020) suggested that female patients with HVA had higher anxiety symptoms than male patients. Despite such empirical evidence, there is a lack of knowledge regarding the risk of depression and anxiety in patients with HVA and the impact of these variables on HR-QoL. Therefore, future research should analyse, also through longitudinal designs, the association between psychological factors and HVA, with particular attention to patients who have experienced a severe anaphylactic reaction. The latter, due to the risk of death from anaphylaxis, could develop strong anxiety in outdoor environments, limit social activities and experience low perceived HR-QoL, with negative effects on global psychophysical well-being (Höfer et al., 2023; Nowak et al., 2015).
Regarding alexithymia, in the present study, 38% of participants showed a clinically significant score of TAS-20. Alexithymic patients showed greater depressive symptoms, anxiety, both psychic and somatic, and a lower perception of HR-QoL for the dimension vitality, social functioning, and mental health than non-alexithymic patients. From a qualitative perspective, these findings support the hypothesis that alexithymia is linked to precise medical domains (Tesio et al., 2018; Di Giuseppe and Conversano, 2022), as in the case of dermatological (Holmes et al., 2022; Namdar and Kurtoglu, 2021), gastrointestinal (Fuchs et al., 2023; Martino et al., 2020, 2023; Kano et al., 2018) and respiratory diseases (Silvestro et al., 2023; Ricciardi et al., 2023), as in the present study which considered also patients with a history HVA. Although in the present study, it was not possible to consider causal associations between alexithymia and the other variables, the results allow us to observe how the difficulty in identifying and recognizing feelings and the external event oriented-thinking style may negatively impact the course of chronic illnesses. Alexithymia could alter patients’ ability to distinguish kinaesthetic sensations related to emotional arousal from symptoms of severe hypersensitivity reactions, negatively affecting the ability to self-manage chronic conditions (Baiardini et al., 2011).
Finally, we acknowledge that the present study has some limitations, as the number of participants was low and moreover, that the group with HVA was mostly of men; these factors limit the possibility of generalizing our results to a broader context. The cross-sectional design does not allow us to establish a cause-effect association among clinical psychological features and dimensions of perceived HR-QoL, and because of the lack of studies, the psychological characteristics of patients with HVA should be further investigated. Nevertheless, our findings may contribute to a better understanding of the psychological complexity of patients with hypersensitivity reactions, allowing a greater awareness of how anxiety, depressive symptoms, and alexithymia can influence the clinical characteristics of severe allergic diseases.
4 Conclusion
The present study highlights that patients with SAA showed lower perceived HR-QoL and greater depressive symptoms than patients with HVA. Patients with HVA reported moderate-low levels of vitality, limitations due to emotional role, and mental health, as well as patients with SAA. Overall, clinically significant levels of alexithymia were associated with higher depressive symptoms and lower vitality and mental health. Therefore, clinicians and psychologists could apply a multidisciplinary approach, considering the body–mind complex, to early detect clinical psychological features such as depression, anxiety, and alexithymia, and to reach a timely diagnosis and accurate therapeutic support in clinical settings, targeting a higher perceived HR-QoL.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical Committee, “Gaetano Martino” University Hospital of Messina, Italy. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LR: Writing – original draft, Conceptualization. OS: Writing – original draft, Investigation. GM: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. AC: Writing – original draft, Software, Methodology, Investigation, Formal analysis. CV: Writing – original draft, Formal analysis, Data curation. TL-J: Writing – original draft, Supervision. PS: Writing – original draft, Supervision. DS: Writing – original draft, Supervision. SG: Writing – original draft, Project administration, Supervision. GP: Writing – original draft, Project administration. CG: Writing – review & editing, Writing – original draft, Supervision.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1394954/full#supplementary-material
References
Adelmeyer, J., Pickert, J., Pfützner, W., and Möbs, C. (2021). Long-term impact of hymenoptera venom immunotherapy on clinical course, immune parameters, and psychosocial aspects. Allergologie Select 5, 57–66. doi: 10.5414/ALX02175E
Apolone, G., and Mosconi, P. (1998). The Italian SF-36 health survey: translation, validation and norming. J. Clin. Epidemiol. 51, 1025–1036. doi: 10.1016/s0895-4356(98)00094-8
Backman, H., Jansson, S. A., Stridsman, C., Eriksson, B., Hedman, L., Eklund, B. M., et al. (2019). Severe asthma—a population study perspective. Clin. Experimental Allergy J. Br. Soc. Allergy Clin. Immunol. 49, 819–828. doi: 10.1111/cea.13378
Bagby, R. M., Parker, J. D., and Taylor, G. J. (1994a). The twenty-item Toronto alexithymia scale-I. Item selection and cross-validation of the factor structure. J. Psychosom. Res. 38, 23–32. doi: 10.1016/0022-3999(94)90005-1
Bagby, R. M., Taylor, G. J., and Parker, J. D. (1994b). The twenty-item Toronto alexithymia scale-II. Convergent, discriminant, and concurrent validity. J. Psychosom. Res. 38, 33–40. doi: 10.1016/0022-3999(94)90006-x
Bagnasco, D., Paggiaro, P., Latorre, M., Folli, C., Testino, E., Bassi, A., et al. (2021). Severe asthma: one disease and multiple definitions. World Allergy Organ. J. 14:100606. doi: 10.1016/j.waojou.2021.100606
Baiardini, I., Abbà, S., Ballauri, M., Vuillermoz, G., and Braido, F. (2011). Alexithymia and chronic diseases: the state of the art. G. Ital. Med. Lav. Ergon. 33, A47–A52
Beck, A. T., Steer, R. A., and Brown, G. (1996). Beck depression inventory-II (BDI-II) [database record]. APA PsycTests. 37:e742. doi: 10.1037/t00742-000
Braido, F. (2013). Failure in asthma control: reasons and consequences. Scientifica 2013, 1–15. doi: 10.1155/2013/549252
Bressi, C., Taylor, G., Parker, J., Bressi, S., Brambilla, V., Aguglia, E., et al. (1996). Cross validation of the factor structure of the 20-item Toronto alexithymia scale: an Italian multicenter study. J. Psychosom. Res. 41, 551–559. doi: 10.1016/s0022-3999(96)00228-0
Chung, K. F., Wenzel, S. E., Brozek, J. L., Bush, A., Castro, M., Sterk, P. J., et al. (2014). International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur. Respir. J. 43, 343–373. doi: 10.1183/09031936.00202013
Conversano, C., and Di Giuseppe, M. (2021). Psychological factors as determinants of chronic conditions: clinical and psychodynamic advances. Front. Psychol. 12:635708. doi: 10.3389/fpsyg.2021.635708
Cooley, C., Park, Y., Ajilore, O., Leow, A., and Nyenhuis, S. M. (2022). Impact of interventions targeting anxiety and depression in adults with asthma. J. Asthma Off. J. Assoc. Care Asthma 59, 273–287. doi: 10.1080/02770903.2020.1847927
Del Roio, L. C., Stelmach, R., Mizutani, R. F., Terra-Filho, M., and De Paula Santos, U. (2023). Work-related asthma consequences on socioeconomic, asthma control, quality of life, and psychological status compared with non-work-related asthma: a cross-sectional study in an upper-middle-income country. Am. J. Ind. Med. 66, 529–539. doi: 10.1002/ajim.23472
Di Giuseppe, M., and Conversano, C. (2022). Psychological components of chronic diseases: the link between defense mechanisms and alexithymia. Mediterranean. J. Clin. Psychol. 10:3602. doi: 10.13129/2282-1619/mjcp-3602
Dockrell, M., Partridge, M. R., and Valovirta, E. (2007). The limitations of severe asthma: the results of a European survey. Allergy 62, 134–141. doi: 10.1111/j.1398-9995.2006.01304.x
Esmaeel, H. M., and Aly, H. Y. (2019). Psychological assessment of patients with bronchial asthma: focus on some predictors of abnormalities. Egypt. J. Bronchol. 13, 35–42. doi: 10.4103/ejb.ejb_42_18
Fuchs, K. H., Musial, F., Retzbach, L., Hann, A., and Meining, A. (2023). Quality of life in benign colorectal disease—a review of the assessment with the gastrointestinal quality of life index (GIQLI). Int. J. Color. Dis. 38:172. doi: 10.1007/s00384-023-04473-y
Gao, Y. H., Zhao, H. S., Zhang, F. R., Gao, Y., Shen, P., Chen, R. C., et al. (2015). The relationship between depression and asthma: a meta-analysis of prospective studies. PLoS One 10:e0132424. doi: 10.1371/journal.pone.0132424
Ghisi, M., Flebus, G. B., Montano, A., Sanavio, E., and Sica, C. (2006). L’adattamento italiano del BDI-II [Italian adaptation of BDI-II], Beck depression inventory-II, Eds A. T. Beck, R. A. Steer, and G. K. Brown, Firenze: Organizzazioni Speciali
Giorgianni, C. M., Martino, G., Brunetto, S., Buta, F., Lund-Jacobsen, T., Tonacci, A., et al. (2024). Allergic Sensitization and psychosomatic involvement in outdoor and indoor workers: a preliminary and explorative survey of motorway toll collectors and office employees. Healthcare. 12:1429. doi: 10.3390/healthcare12141429
Global Initiative for Asthma . (2023). Global strategy for asthma management and prevention, 2023. Available at: https://www.ginasthma.org/
Gruffydd-Jones, K., Thomas, M., Roman-Rodríguez, M., Infantino, A., FitzGerald, J. M., Pavord, I., et al. (2019). Asthma impacts on workplace productivity in employed patients who are symptomatic despite background therapy: a multinational survey. J. Asthma Allergy 12, 183–194. doi: 10.2147/JAA.S204278
Hamilton, M. (1959). The assessment of anxiety states by rating. Br. J. Med. Psychol. 32, 50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x
Hiles, S. A., Harvey, E. S., McDonald, V. M., Peters, M., Bardin, P., Reynolds, P. N., et al. (2018). Working while unwell: workplace impairment in people with severe asthma. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 48, 650–662. doi: 10.1111/cea.13153
Höfer, V., Martini, M., Dölle-Bierke, S., Worm, M., and Bilò, M. B. (2023). Health-related quality of life in food and venom induced anaphylaxis and role of influencing factors. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 53, 295–306. doi: 10.1111/cea.14268
Holmes, A., Marella, P., Rodriguez, C., Glass Ii, D., and Goerlich, K. S. (2022). Alexithymia and cutaneous disease morbidity: a systematic review. Dermatology 238, 1120–1129. doi: 10.1159/000524736
Hossny, E., Caraballo, L., Casale, T., El-Gamal, Y., and Rosenwasser, L. (2017). Severe asthma and quality of life. World Allergy Organiz. J. 10:28. doi: 10.1186/s40413-017-0159-y
Isvoranu, A.-M., Abdin, E., Chong, S. A., Vaingankar, J., Borsboom, D., and Subramaniam, M. (2021). Extended network analysis: from psychopathology to chronic illness. BMC Psychiatry 21:119. doi: 10.1186/s12888-021-03128-y
Jiang, M., Qin, P., and Yang, X. (2014). Comorbidity between depression and asthma via immune-inflammatory pathways: a meta-analysis. J. Affect. Disord. 166, 22–29. doi: 10.1016/j.jad.2014.04.027
Kano, M., Endo, Y., and Fukudo, S. (2018). Association between alexithymia and functional gastrointestinal disorders. Front. Psychol. 9:599. doi: 10.3389/fpsyg.2018.00599
Lin, P., Li, X., Liang, Z., and Wang, T. (2022). Association between depression and mortality in persons with asthma: a population-based cohort study. Allergy, Asthma Clin. Immunol. 18, 29–27. doi: 10.1186/s13223-022-00672-4
Liotta, M., Liotta, M., Saitta, S., and Ricciardi, L. (2023). Severe allergic asthma: does alexithymia interfere with omalizumab treatment outcome? Asian Pac. J. Allergy Immunol. 41, 53–59. doi: 10.12932/AP-040121-1031
López-Tiro, J., Contreras-Contreras, A., Rodríguez-Arellano, M. E., and Costa-Urrutia, P. (2022). Economic burden of severe asthma treatment: a real-life study. World Allergy Organiz. J. 15:100662. doi: 10.1016/j.waojou.2022.100662
Louis, G., Schleich, F., Louis, R., Guillaume, M., Sousa-Pinto, B., Bousquet, J., et al. (2023). How respiratory symptoms impact asthma-related quality of life in mild asthmatics. Respir. Med. 207:107098. doi: 10.1016/j.rmed.2022.107098
Lu, Z., Chen, L., Xu, S., Bao, Q., Ma, Y., Guo, L., et al. (2018). Allergic disorders and risk of depression: a systematic review and meta-analysis of 51 large-scale studies. Ann. Allergy Asthma Immunol. 120, 310–317.e2. doi: 10.1016/j.anai.2017.12.011
Majellano, E. C., Clark, V. L., Winter, N. A., Gibson, P. G., and McDonald, V. M. (2019). Approaches to the assessment of severe asthma: barriers and strategies. J. Asthma Allergy 12, 235–251. doi: 10.2147/JAA.S178927
Martino, G., Caputo, A., Schwarz, P., Bellone, F., Fries, W., Quattropani, M. C., et al. (2020). Alexithymia and inflammatory bowel disease: a systematic review. Front. Psychol. 11:1763. doi: 10.3389/fpsyg.2020.01763
Martino, G., Caputo, A., Vicario, C. M., Feldt-Rasmussen, U., Watt, T., Quattropani, M. C., et al. (2021). Alexithymia, emotional distress, and perceived quality of life in patients with Hashimoto’s thyroiditis. Front. Psychol. 12:667237. doi: 10.3389/fpsyg.2021.667237
Martino, G., Viola, A., Vicario, C. M., Bellone, F., Silvestro, O., Squadrito, G., et al. (2023). Psychological impairment in inflammatory bowel diseases: the key role of coping and defense mechanisms. Res. Psychotherapy 26:731. doi: 10.4081/rippo.2023.731
McDonald, V. M., Hiles, S. A., Jones, K. A., Clark, V. L., and Yorke, J. (2018). Health-related quality of life burden in severe asthma. Med. J. Aust. 209, S28–S33. doi: 10.5694/mja18.00207
McLoughlin, R. F., and McDonald, V. M. (2021). The management of extrapulmonary comorbidities and treatable traits; obesity, physical inactivity, anxiety, and depression, in adults with asthma. Front. Allergy 2:735030. doi: 10.3389/falgy.2021.735030
Medina-Rodriguez, E. M., Lowell, J. A., Worthen, R. J., Syed, S. A., and Beurel, E. (2018). Involvement of innate and adaptive immune systems alterations in the pathophysiology and treatment of depression. Front. Neurosci. 12:547. doi: 10.3389/fnins.2018.00547
Merlo, E. M. (2019). Opinion article: the role of psychological features in chronic diseases, advancements and perspectives. Mediterranean. J. Clin. Psychol. 7:2341. doi: 10.6092/2282-1619/2019.7.2341
Montano, A., and Flebus, G. B. (2006). Presentazione del Beck depression inventory-Seconda edizione (BDI-II): Conferma della struttura bifattoriale in un campione di popolazione italiana [presentation of the Beck depression inventory-second edition (BDI-II): confirmation of the bifactorial structure in a champion of the Italian population]. Psicoterapia Cognitiva e Comportamentale 12, 67–82.
Mortimer, K., Lesosky, M., García-Marcos, L., Asher, M. I., Pearce, N., Ellwood, E., et al. (2022). The burden of asthma, hay fever and eczema in adults in 17 countries: GAN phase I study. Eur. Respir. J. 60:2102865. doi: 10.1183/13993003.02865-2021
Namdar, N. D., and Kurtoglu, Y. (2021). Alexithymia, anxiety, and depression in patients with vitiligo. Ann. Med. Res. 28:e581. doi: 10.5455/annalsmedres.2020.06.581
Nemiah, J., Freyberger, H., and Sifneos, P. E. (1976). Alexithymia: a view of the psychosomatic process. In, OW Hill (1976). Mod. Tends Psych. Med. 3, 430–439.
Nowak, N., Bazan-Socha, S., Pulka, G., Pełka, K., and Latra, P. (2015). Evaluation of the quality of life in subjects with a history of severe anaphylactic reaction to the Hymenoptera venom. Pneumonol. Alergol. Pol. 83, 352–358. doi: 10.5603/PiAP.2015.0057
Pastorello, E. A., Rivolta, F., Bianchi, M., Mauro, M., and Pravettoni, V. (2001). Incidence of anaphylaxis in the emergency department of a general hospital in Milan. J. Chromatogr. B Biomed. Sci. Appl. 756, 11–17. doi: 10.1016/s0378-4347(01)00067-6
Patella, V., Pelaia, C., Zunno, R., and Pelaia, G. (2022). Biologicals decrease psychological distress, anxiety and depression in severe asthma, despite Covid-19 pandemic. Respir. Med. 200:106916. doi: 10.1016/j.rmed.2022.106916
Ricciardi, L., Papia, F., Cataldo, G., Giorgianni, M., Spatari, G., and Gangemi, S. (2018). Hymenoptera sting reactions in southern Italy forestry workers: our experience compared to reported data. Clin. Mol. Allergy 16:8. doi: 10.1186/s12948-018-0087-6
Ricciardi, L., Spatari, G., Vicario, C. M., Liotta, M., Cazzato, V., Gangemi, S., et al. (2023). Clinical psychology and clinical immunology: is there a link between alexithymia and severe asthma? Mediterranean. J. Clin. Psychol. 11:3704. doi: 10.13129/2282-1619/mjcp-3704
Roche, N., Garcia, G., de Larrard, A., Cancalon, C., Bénard, S., Perez, V., et al. (2022). Real-life impact of uncontrolled severe asthma on mortality and healthcare use in adolescents and adults: findings from the retrospective, observational RESONANCE study in France. BMJ Open 12:e060160. doi: 10.1136/bmjopen-2021-060160
Ruëff, F., Bauer, A., Becker, S., Brehler, R., Brockow, K., Chaker, A., et al. (2023). Diagnosis and treatment of hymenoptera venom allergy. Allergol. Select 7, 154–190. doi: 10.5414/alx02430e
Sastre, J., Crespo, A., Fernandez-Sanchez, A., Rial, M., and Plaza, V.investigators of the CONCORD Study Group (2018). Anxiety, depression, and asthma control: changes after standardized treatment. J. Allergy Clin. Immunol. Pract. 6, 1953–1959. doi: 10.1016/j.jaip.2018.02.002
Schaarschmidt, M. L., Gutknecht, M., Schoeben, L., and Schmieder, A. (2018). Disease burden, psychological well-being and attitudes regarding the set of emergency medication in adults with insect venom allergy. Int. Arch. Allergy Immunol. 176, 150–156. doi: 10.1159/000488721
Schiener, M., Graessel, A., Ollert, M., Schmidt-Weber, C. B., and Blank, S. (2017). Allergen-specific immunotherapy of hymenoptera venom allergy—also a matter of diagnosis. Hum. Vaccin. Immunother. 13, 2467–2481. doi: 10.1080/21645515.2017.1334745
Schoeben, L. S., Bubak, C., Schaarschmidt, M. L., and Schmieder, A. (2020). Sex differences in adults with insect venom allergy regarding psychological distress, attitudes toward the emergency medication, and factual knowledge about the disease. Int. Arch. Allergy Immunol. 181, 529–535. doi: 10.1159/000507625
Scimeca, G., Bruno, A., Cava, L., Pandolfo, G., Muscatello, M. R., and Zoccali, R. (2014). The relationship between alexithymia, anxiety, depression, and internet addiction severity in a sample of Italian high school students. TheScientificWorldJOURNAL 2014:504376. doi: 10.1155/2014/504376
Silvestro, O., Ricciardi, L., Catalano, A., Vicario, C. M., Tomaiuolo, F., Pioggia, G., et al. (2023). Alexithymia and asthma: a systematic review. Front. Psychol. 14:1221648. doi: 10.3389/fpsyg.2023.1221648
Stubbs, M. A., Clark, V. L., Gibson, P. G., Yorke, J., and McDonald, V. M. (2022). Associations of symptoms of anxiety and depression with health-status, asthma control, dyspnoea, dysfunction breathing and obesity in people with severe asthma. Respir. Res. 23:341. doi: 10.1186/s12931-022-02266-5
Sturm, G. J., Varga, E. M., Roberts, G., Mosbech, H., Bilò, M. B., Akdis, C. A., et al. (2018). EAACI guidelines on allergen immunotherapy: hymenoptera venom allergy. Allergy 73, 744–764. doi: 10.1111/all.13262
Suarthana, E., Moual, N. L., Lemière, C., Bousquet, J., Pierre, S., Sousa-Pinto, B., et al. (2023). Work-related asthma and its impact on quality of life and work productivity. J. Allergy Clin. Immunol. Pract. 12, 372–382.e2. doi: 10.1016/j.jaip.2023.10.044
Tal, Y., Shany, G., Hershko, A. Y., Ribak, Y., Mizrahi, E., Shamriz, O., et al. (2020). The association between anaphylaxis and post-traumatic stress disorder in subjects with Hymenoptera venom allergy. J. Allergy Clin. Immunol. Pract. 8, 775–777. doi: 10.1016/j.jaip.2019.07.035
Taylor, G. J. (2000). Recent developments in alexithymia theory and research. Can. J. Psychiatry 45, 134–142. doi: 10.1177/070674370004500203
Taylor, G. J., Bagby, R. M., and Parker, J. D. A. (1997). Disorders of affect regulation: alexithymia in medical and psychiatric illness : Cambridge University Press.
Tesio, V., Di Tella, M., Ghiggia, A., Romeo, A., Colonna, F., Fusaro, E., et al. (2018). Alexithymia and depression affect quality of life in patients with chronic pain: a study on 205 patients with fibromyalgia. Front. Psychol. 9:442. doi: 10.3389/fpsyg.2018.00442
Toletone, A., Voltolini, S., Passalacqua, G., Dini, G., Bignardi, D., Minale, P., et al. (2016). Hymenoptera venom allergy in outdoor workers: occupational exposure, clinical features and effects of allergen immunotherapy. Hum. Vaccin. Immunother. 13, 477–483. doi: 10.1080/21645515.2017.1264748
van Houtum, L., Rijken, M., and Groenewegen, P. (2015). Do everyday problems of people with chronic illness interfere with their disease management? BMC Public Health 15:1000. doi: 10.1186/s12889-015-2303-3
Wang, E., Wechsler, M. E., Tran, T. N., Heaney, L. G., Jones, R. C., Menzies-Gow, A. N., et al. (2020). Characterization of severe asthma worldwide: data from the international severe asthma registry. Chest 157, 790–804. doi: 10.1016/j.chest.2019.10.053
Ware, J. E., and Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 30, 473–483. doi: 10.1097/00005650-199206000-00002
World Health Organization (2019). International statistical classification of diseases and related health problems. 11th Edn Available at: https://icd.who.int/.
World Medical Association (2013). World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310, 2191–2194. doi: 10.1001/jama.2013.281053
Worm, M., Moneret-Vautrin, A., Scherer, K., Lang, R., Fernandez-Rivas, M., Cardona, V., et al. (2014). First European data from the network of severe allergic reactions (NORA). Allergy 69, 1397–1404. doi: 10.1111/all.12475
Zhang, L., Zhang, X., Zheng, J., Wang, L., Zhang, H. P., Wang, L., et al. (2016). Co-morbid psychological dysfunction is associated with a higher risk of asthma exacerbations: a systematic review and meta-analysis. J. Thorac. Dis. 8, 1257–1268. doi: 10.21037/jtd.2016.04.68
Keywords: clinical psychology, immunology, alexithymia, severe allergic asthma, hymenoptera venom anaphylaxis, H-R quality of life, severe hypersensitivity reactions, outdoor workers
Citation: Ricciardi L, Silvestro O, Martino G, Catalano A, Vicario CM, Lund-Jacobsen T, Schwarz P, Sapienza D, Gangemi S, Pioggia G and Giorgianni CM (2024) Health-related quality of life in severe hypersensitivity reactions: focus on severe allergic asthma and hymenoptera venom anaphylaxis—a cross-sectional study. Front. Psychol. 15:1394954. doi: 10.3389/fpsyg.2024.1394954
Edited by:
Gianluca Castelnuovo, Catholic University of the Sacred Heart, ItalyReviewed by:
Alberto Sardella, University of Catania, ItalyAda Ghiggia, University of Trieste, Italy
Copyright © 2024 Ricciardi, Silvestro, Martino, Catalano, Vicario, Lund-Jacobsen, Schwarz, Sapienza, Gangemi, Pioggia and Giorgianni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antonino Catalano, Y2F0YWxhbm9hQHVuaW1lLml0
 Luisa Ricciardi
Luisa Ricciardi Orlando Silvestro
Orlando Silvestro Gabriella Martino
Gabriella Martino Antonino Catalano
Antonino Catalano Carmelo Mario Vicario
Carmelo Mario Vicario Trine Lund-Jacobsen
Trine Lund-Jacobsen Peter Schwarz
Peter Schwarz Daniela Sapienza
Daniela Sapienza Sebastiano Gangemi
Sebastiano Gangemi Giovanni Pioggia
Giovanni Pioggia Concetto Mario Giorgianni
Concetto Mario Giorgianni