- 1Applied Research Division for Cognitive and Psychological Science, European Institute of Oncology IEO, IRCCS, Milan, Italy
- 2Department of Oncology and Hemato-Oncology, University of Milan, Milan, Italy
- 3Department of Psychology, Università Cattolica del Sacro Cuore, Milan, Italy
Breast cancer impairs physical and psychological well-being, even some years after treatments. Oncological treatments can strongly affect the body due to scars and breast(s) removal, for example, increasing symptoms of anxiety and depression. Psychological studies are effective in improving breast cancer survivors’ emotions and behaviors through several approaches to interventions. Over years, the Mindfulness-Based Stress Reduction (MBSR) has been evaluated as an effective intervention to promote well-being in breast cancer survivors. The present study protocol aims to evaluate the effectiveness of a MBSR intervention in regulating interoceptive sensations, as the ability to be aware of inner sensations. Second, it seeks to identify changes in interoceptive feelings, mood, and body perception following the intervention. These changes will be evaluated across three data collection times to assess differences about emotions and body perception over time, focusing on their relevance for breast cancer survivors’ well-being. Finally, the present study protocol aims to detect improvements in anxiety, depression, and body awareness, considering the potential positive impact of the MBSR approach on emotional well-being. Direction for future psychological intervention are given.
Introduction
Most women with breast cancer have to deal with diagnosis and its related oncological treatments as a very difficult experience to accept, starting with the consequences on their Quality of Life (Schell et al., 2019). Oncological treatments (e.g., chemotherapy, radiotherapy, immunotherapy) can damage the body due to the presence of scars, hair loss, and breast(s) removal, for example (Fioretti et al., 2017). Therefore, patients generally report high levels of distress, anxiety, depression, physical symptoms of pain, fatigue and sleep–wake rhythm dysfunction, even several years after finishing treatments (Abrahams et al., 2018). Concerning emotional issues, it is mandatory to address the bodily self, defined as an expression of implicit knowledge about physical actions and movements (Sebri et al., 2021). Addressing bodily self is particularly relevant for breast cancer survivors, who concern changes in body image perception due to altered weight, possible hair loss, and the sudden onset of menopausal symptoms (Pintado and Andrade, 2017; Sebri et al., 2022). Additionally, body perception and body image are strictly tied to social and intimate relationships. Following the Discrepancy Theory by Higgins (1987), when there is a significant gap between one’s current and the desired body, it can lead to feelings of dissatisfaction and emotional distress. This discrepancy can severely impact women’s sense of femininity and sexuality (Male et al., 2016). Moreover, one’s own body after diagnosis and oncological treatments can be experienced as ill and damaged, even perceiving them as a source of danger for the fear of cancer recurrence. This can increase the risk of being labeled as “patients” rather than “persons,” reinforcing this type of self-definition and representation (McGannon et al., 2016). To improve levels of psycho-emotional well-being, the literature highlights the effectiveness of multimodal interventions aimed at improving both self-image perception and psycho-social aspects (Lengacher et al., 2009). Current studies demonstrated the efficacy of complementary and alternative interventions in groups of breast cancer survivors to improve positive social support (Durosini et al., 2021; Sebri et al., 2023; Sebri and Pravettoni, 2023). More specifically, numerous studies show the effectiveness of integrating standardized techniques and complementary medicine therapies, with a view to a multidisciplinary approach. Among them, one method effectively applied in the oncology field, and specifically in breast cancer patients (Carlson et al., 2004; Henderson et al., 2013), is the application of the Mindfulness-Based Stress Reduction (MBSR) protocol developed by Kabat-Zinn (1979).
Mindfulness is defined as paying attention to the unfolding of experience moment by moment, with intention and in a non-judgmental manner (Segal et al., 2014), cultivating a stable and non-reactive awareness even in stressful situations, such as that induced by a course of illness (Guu et al., 2023). Mindfulness allows one to pause ruminating thoughts, and access a greater awareness of one’s mental habits and related bodily sensations (Mehling et al., 2009; Pintado and Andrade, 2017). In this regard, the perception and awareness of what is happening within the body (e.g., concerning a general feeling of pleasantness/unpleasantness) is referred to as interoception (Barrett, 2017). Most Mindfulness-based protocols permit to cultivate interoceptive awareness, which plays a crucial role in the effectiveness of mindfulness-based interventions (Fischer et al., 2017), allowing the practitioners to shift attention from thinking about one’s bodily sensations to immediately feeling them (Farb et al., 2015; Mehling et al., 2017). Indeed, mindfulness can improve the relationship with interoceptive signals, encouraging more adaptive behaviors toward bodily sensations and reducing experiential avoidance (Weng et al., 2021). Accordingly, individuals who have practiced mindfulness report changes in their interoceptive awareness, having learned to redirect attention to their body, manage stress, regulate emotions and facilitate cognitive insight into their body/emotional state (de Jong et al., 2016; Fissler et al., 2016). Furthermore, enhanced interoception is also linked to improved mental health outcomes, making it a relevant and valuable capacity targeted in MBSR interventions for breast cancer patients.
Increased emotional awareness is indeed associated with a decrease in somatic symptoms (such as nausea, pain and fatigability) and distress, as well as a subsequent reduction in mortality in breast cancer patients (Czamanski-Cohen et al., 2019). Specifically, previous studies noted increased vitality, decreased physical pain, improvements in both mood (e.g., anxiety and depression) and social functioning (Reibel et al., 2001). The MBSR program also facilitates other ways of taking care of oneself (e.g., more rest and physical activity), paying attention without evaluation or judgment (Glynn et al., 2020). Accordingly, it provides greater benefits compared to usual care across all diagnoses, except for cognitive-behavioral therapy that is considered more efficacy in some specific cases (e.g., pain management) (Pardos-Gascón et al., 2021). Comparisons between mindfulness interventions are scarce, with MBSR being the most studied. In central sensitization syndromes, variables associated with pain tend to improve with treatment (Pardos-Gascón et al., 2021). Finally, regarding body perception, some studies report greater acceptance of oneself and one’s body after MBSR interventions (Luiggi-Hernandez et al., 2018; Penlington, 2019; Tate et al., 2018; Visser et al., 2015). Indeed, the effectiveness of MBSR programs about changes in body image perception is noted, highlighting how increased awareness can positively impact self-image. In this regard, a study by Pérez-Peña et al. (2022) highlighted the impact of mindfulness on proprioception within the body image perception. Proprioception is defined as the perception of body movement and position. It depends on both psychological (e.g., memory and learning) and physiological processes (e.g., mechanosensory neurons throughout the body known as proprioceptors) (Tuthill and Azim, 2018). Similar to interoception, proprioception is largely unconscious, although some proprioceptive information can be brought into conscious awareness (Pérez-Peña et al., 2022).
Even though the cancer experience causes quite a few issues related to the perception of self and one’s internal states, few programs specifically aimed at improving body image have been developed so far (Pintado and Andrade, 2017; Pidgeon and Appleby, 2014). To date, few studies have analyzed the effectiveness of MBSR programs in treating body image in breast cancer patients. In a recent randomized trial (Pintado and Andrade, 2017), patients who followed an MBSR protocol reported a decrease in negative thoughts and emotions related to self-image perception, an increase in positive thoughts, and increased body awareness. However, the scientific literature has so far not focused on measuring the effectiveness of MBSR protocols on interoceptive awareness in breast cancer patients. The overall aim of the present study is to evaluate the effectiveness of a MBSR intervention in regulating interoceptive feelings in women with breast cancer experience. This study will highlight possible changes in emotions and body perception in breast cancer survivors. Specifically, we aim to identify predictive aspects of the intervention on interoceptive feelings, mood, and body perception according to the three data collection times. In addition, we expect to be able to detect an improvement in mood (anxiety and depression) and body awareness (medium-term benefit).
Methods
The present protocol was obtained from a licensing committee from a University that approved the study. Additionally, all participants signed the informed consent form. Lastly, this study follows the Declaration of Helsinki and method design will be carried out in accordance with relevant guidelines and regulations. Participants who belong to breast cancer associations will be contacted and invited to take part in this project by email. If they will accept, an informed consent before starting the first meeting will be sent.
The inclusion criteria for participation in the study are as follows:
1. Age between 30 and 50 to guarantee the sample homogeneity;
2. Patients with the first diagnosis of stage I, II, and III breast cancer;
3. Patients who have experience of previous surgery as an oncological intervention to remove cancer.
4. Patients who have received chemotherapy and completed treatment. Only chemotherapy can be accepted as the oncological treatments, not immunotherapy or radiotherapy. This criterion is chosen to ensure the homogeneity of the sample and to focus on patients who are not in an advanced stage of therapy but have completed their treatments.
5. Fluently understand and speak the Italian language.
Exclusion criteria are related to:
1. Metastatic disease, meaning the need to treat other types of cancer in addition to breast cancer;
2. Patients with a previous cancer diagnosis who have developed other types of cancer, different from breast cancer;
3. Patients who are undergoing psychological treatment, whether individually or in groups. It is relevant to ask them if they are currently participating in a psychological intervention, especially if it involves processing of cancer-related issues;
4. Presence of neurological deficits and/or psychiatric disorders that could impair rationale participation to the study;
5. Lack of knowledge of the Italian language, which could affect the full and accurate understanding of both the mindfulness practice and the questionnaires’ contents.
This study will last approximately 6 months and will use a quantitative research methodology, with a between-subjects design. Forty participants meeting the inclusion and exclusion criteria set out above will be enrolled and randomly distributed through Excel software (RAND function) into the following two groups:
Experimental group: participants who will be immediately included in the MBSR protocol;
Waitlist control group: participants who will be included in the MBSR protocol after 12 weeks from the start of the protocol.
The intervention proposed to the experimental group will be conducted by a psychologist expert in the MBSR protocol. The MBSR intervention will be structured as follows: it envisages eight weekly group meetings lasting about 2/2.5 h each, plus an intensive meeting (generally proposed between the sixth and seventh meetings or between the seventh and eighth meetings), which lasts about 5 h. Moreover, a follow-up meeting about a month after the conclusion of the course will be proposed. Participation in the course is preceded by an acquaintance and information meeting with the trainer who will be the course leader (40 min). The program will be experiential; participants do not passively receive guidance on how to manage stress but become active participants through systematic training in mindfulness practice. Specifically, based on the definition of mindfulness, the MBSR protocol invites people to cultivate awareness through meditation and teach how to enter into a different relationship with suffering, regardless of the specific causes, whether medical or psychological. It is possible to hypothesize that insights gained during meditative practice could serve as a basis for developing effective strategies for managing chronic pain conditions (Giommi, 2006).
The study will take place in a brightly lit and spacious room. This room will be specifically dedicated to accommodate group sessions, mindfulness exercises and group practices, with ample space for participants to either sit on the floor or use chairs, ensuring comfort and flexibility. All sessions will consistently be conducted in this same room, providing a stable and familiar environment for participants throughout the study.
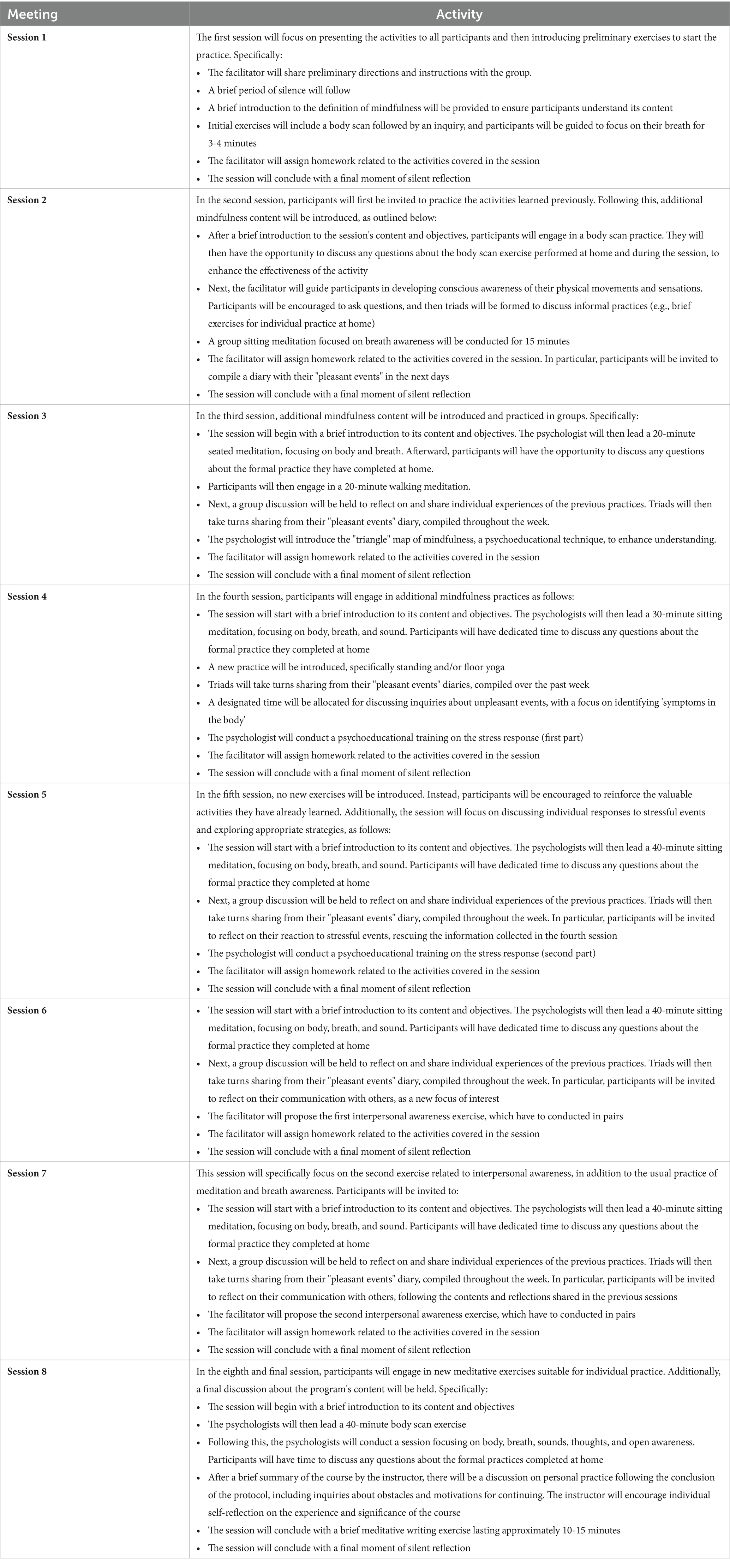
On a practical level, the MBSR protocol will include (see Table 1 for a detailed schedule of meetings):
1. Moments of formal practice (sitting meditation with a focus on breath, body, sound, and mind content; body scan; mindful movement; walking meditation. These points will be discussed in detail below);
2. Free sharing of experiences and inquiry;
3. Formal practice to be performed daily at home with the support of audio tracks;
4. Informal practice (bringing awareness into everyday actions that we generally repeat daily according to automatic patterns);
5. Printed material to support formal and informal practice.
6. The formal and informal practice that the participant will be invited to perform daily takes approximately 40 min per day.
Formal practice
MBSR intervention will be based of some formal practices, as follows:
• Sitting meditation consists of sitting while maintaining a composed, upright, yet not rigid posture, with head, neck and back aligned along a vertical axis, shoulders relaxed and hands in a comfortable position. This posture allows one to practice an attitude of dignity, patience, and calmness, bringing attention to the sensations emerging in the present moment without trying to fill time. For these reasons, it is necessary to dedicate time and space to the practice. The sitting meditation practice proposed in the first meetings of the MBSR pathway consists of directing attention with intention to the breath, remaining present to the sensations that accompany each inhale and exhale, without changing it. During meditation, the mind can become distracted and drift away from the object of attention; participants are asked To pay attention firmly and gently to one’s own breath, training the mind to be less reactive and more stable. This approach allows us to embrace each moment, cultivating concentrated calm, managing the mind’s resistance, and developing acceptance, patience, absence of judgment, and inner strength. It represents a training that teaches to deliberately let go of one’s thoughts, disidentifying from their content. In the course of the MBSR program, the practice of sitting meditation gradually broadens the field of attention to other objects besides the breath: sensations in various parts of the body and the body as a whole, sounds, and the process of thoughts. Recognizing thoughts as such allows us, as Kabat-Zinn (1979, 1997, 2016), to free ourselves from the distorted reality they can create, enabling us to manage our lives with greater fluidity. Similarly, dedicating time to practice daily allows us to strengthen our awareness, recognizing and accepting ourselves as we are and not as we would like to be;
• The body scan is a meditative practice that allows us to reconnect with the body, exploring it through a meticulous examination aimed at developing concentration and flexibility of attention. It is performed by lying on one’s back and systematically directing attention to various parts of the body. During the practice, participants are invited to inhabit each area of the body with full awareness, the sensations they are experiencing as well as their absence, attuning oneself as best as one can with the experience of the part of the body, which is the object of attention. The goal is to feel each part of the body and cultivate a non-judgmental, a moment-to-moment condition of awareness. Kabat-Zinn (1997) stated that the practice of body scan allows many practitioners to perceive their bodies positively; in particular, directing attention, kindness, and acceptance toward the own body becomes a valuable experience for what he describes as self-healing.
• The practice related to conscious movement through yoga consists of slowly performing and maintaining for a time a series of stretches of muscles and joints, while also continuously bringing attention to the breath and the current sensations. Kabat-Zinn (1997) describes this formal practice as an effective method to know ourselves more deeply, whatever our health conditions. During the conscious practice of yoga, there are no efforts or goals to achieve. On the contrary, this practice allows to grasp and get closer to physical and psychological limits, without having to cross or overcome them, but practicing patience with ourselves and observing the habitual way we deal with them;
• The walking meditation practice, in which attention is directed to the experience of walking in the moment and slow motion. More precisely, one chooses the place where to carry out the practice (indoors or outdoors); one defines the straight path to be followed (beginning and end); one stands still at the starting point of the path, for a few seconds, with feet parallel and apart, knees slightly flexed, arms stretched out along the sides or hands intertwined at belly level, the gaze unfocused in front of one. The invitation is to bring attention to the soles of the feet, to the physical sensations of contact with the floor, to the distribution of body weight during the steps taken, to the movement of the legs and the entire walking body, aiming at being present with each step, aimlessly, letting go of all thoughts. Being a moving practice, participants experience how the body keeps us anchored in the here-and-now through the grounding of the feet, while our mind tends to shift between the past and future. Participants are invited to practice walking meditation daily.
Intensive meeting
The intensive meeting will include several formal meditation practices conducted and supervised continuously by the trainer. It is usually conducted between the sixth and seventh meetings or between the seventh and eighth meetings of the study. At this time, participants have been exposed to all the formal mindfulness practices; this way, they will be able to experience them in a similar way as during silent meditation retreat days. The intensive meeting will also become a time to break the rhythm of the usual routine by paying attention to the present moment. In other words, it will be an opportunity to empower the practice of mindfulness as an invitation to turn toward one’s suffering and observe more clearly the possible mental patterns that can exacerbate it. Specifically, a sequence of practices adapted to the group of participants is usually proposed, such as: sitting meditation practices focusing on breath, body, sounds, thoughts, or non-selective meditation practices; slow conscious movements to allow space for listening to one’s body and present sensations; body scan; walking meditation. Furthermore, informal meditation practices such as mindful eating will also be offered. The trainer will invite each participant to observe his or her own experience of food during lunch (which is done more slowly than usual, devoting more time to curiously observing the sensations present during the stages of tasting, chewing, swallowing).
Evaluation tools
A battery of standardized and self-administered questionnaires will be administered through Qualtrics platform at the beginning and end of the MBSR intervention. The questionnaires will be administered to both groups in three stages: pre-intervention (T0), after 8 weeks (T1) and after 12 weeks (T2) from the beginning of the study. After the reading of the information sheet and the signing of the informed consent, participants will be asked to answer some socio-demographic and disease status questions, and then they will be asked to answer standardized and validated questionnaires designed to investigate interoceptive sensations, metacognitive and dissociative skills, sleep quality, state anxiety and depression, general well-being, and body perception. The duration of the questionnaire administration will be approximately 30–40 min.
Specifically, the questionnaires administered will be:
The multidimensional assessment of interoceptive awareness (MAIA)
MAIA is a self-report questionnaire that assesses eight dimensions related to interoceptive aspects of body awareness (Mehling et al., 2012). The scale includes a total of 32 items on a 6-point Likert scale, ranging from 0 (never) to 5 (always) and covers eight “distinct but related” dimensions of interoception: awareness of bodily sensations (e.g.: “I can tell where I feel good in my body”), the tendency to ignore uncomfortable bodily sensations (e.g., “I distract myself when I feel uncomfortable or fearful sensations”), the ability to have emotional reactions as a result of negative sensations (e.g., “I worry if I feel pain or uncomfortable sensations”), the ability to regulate attention regarding multiple sensations (e.g., “I can focus sensations on my body, even when there are many distractions around me”), the ability to be aware of the relationship between bodily and affective states (e.g., “I can feel changes in my body when I am happy”), the ability to pay attention to bodily states to regulate psychological distress (e.g., “I can use my breath to help me stay calm and relaxed), the ability to feel one’s bodily sensations to make decisions (e.g., “I listen to my body to help me choose what to do”), and the experience of one’s body as safe and trustworthy (e.g., “I feel that my body is a safe place). Some subscales measure direct experience with the body, others are associated with the assessment of cognitive processes, such as self-regulation (Ferentzi et al., 2020). The total score is calculated between 0 and 160 (Valenzuela-Moguillansky and Reyes-Reyes, 2015) and the reliability for the eight subscales (Mehling et al., 2012) is between 0.66 and 0.87.
The Italian version of the metacognitions questionnaire (MCQ-30)
MCQ-30 is a questionnaire with 30 items distributed on a 5-point Likert scale (from “not at all agree” to “completely agree”) (Quattropani et al., 2014). It measures dysfunctional metacognition processes regarding vulnerability and maintenance of emotional disorders through five categories: (1) positive beliefs regarding worry, describing the positive evaluation of worry as being functional for planning and solving problems (6 items, e.g., “I need to worry in order to work better”); (2) negative beliefs regarding uncontrollable and dangerous aspects, assessing the negative interpretation of worry due to thoughts considered uncontrolled (6 items, e.g.: “When I start worrying, I cannot stop”); (3) cognitive confidence, in order to explore concerns related to the effectiveness of one’s memory (6 items, e.g., “I do not trust my memory”); (4) the need to control thoughts, which assesses the belief that some thoughts need to be controlled and suppressed (6 items, e.g., “I should keep my thoughts under control all the time”); (5) cognitive self-awareness, which assesses the tendency to constantly pay attention to one’s thought processes (6 items, e.g., “I am constantly aware of my thoughts”). MCQ-30 shows good psychometric properties with reference to satisfactory internal consistency, convergent validity, and good test–retest reliability (Laghi et al., 2020).
Dissociative experiences scale (DES)
DES is a self-report questionnaire composed of 28 items that measures the likelihood of having dissociative thinking and post-traumatic stress disorder (PTSD) (Bernstein and Putnam, 1986). Measured on a 10-point scale (from “never” to “always”), each item describes a type of experience that each subject might have had. Studies show that subjects with scores above 15 need more exploration as they are often linked to dissociative diagnoses; a score of 30 suggests a good possibility of dissociative thinking and PTSD; finally, scores above 40 indicate high likelihood of a dissociative identity disorder (Kianpoor et al., 2012). Factor analysis reports three factorial structures (Burch, 1995) that include depersonalization and derealization (e.g., feeling that our body does not belong to us), amnestic dissociation (e.g., finding new objects that one does not remember buying), and imaginal involvement (e.g., being in a familiar environment but recognizing it as strange) (Renard et al., 2012). In reference to psychometric properties, Frischholz et al. (1992) report good concurrent and criterion validity, while Olsen and Beck (2012) show high internal consistency scores with Cronbach’s alpha of 0.7.
The Pittsburgh sleep quality index (PSQI)
PSQI is a self-administered questionnaire that measures sleep quality and quantity in 1 month (Buysse et al., 1989). The test consists of 19 items that address seven components; specifically: subjective quality and latency of sleep, duration, usual sleep efficiency, sleep disturbances, use of appropriate sleep medications, and schedules referred to sleep dysfunctionality. There are also five additional questions completed by the partner of the participant subject, but which are not then calculated in the final scoring. The Global Sleep Quality scale reports Cronbach’s alpha of 0.83. Furthermore, a Global Sleep Quality score greater than five discriminates between good and poor sleepers with a diagnostic sensitivity of 89.6 percent and specificity of 86.5 percent (Buysse et al., 1991). Finally, the literature evidences the reliability and validity of the PSQI in different populations (Beck et al., 2004).
Hospital and anxiety depression scale (HADS)
HADS is a 14-item compost questionnaire on a 4-point Likert scale (0–3) to measure emotional distress (e.g., anxiety and depression) in a patient population without psychiatric symptoms (Zigmond and Snaith, 1983). The total score (0–42) results from the sum of the scores obtained in each of the two individual subscales; the first subscale is about anxiety symptoms (7 items), while the second one regards depressive symptoms (7 items) (Zigmond and Snaith, 1983). The higher the score obtained, the higher the values found in reference to anxiety and depression; values with scores of 10 and above indicate the need for clinical intervention (Zilliacus et al., 2011; LoMartire et al., 2020). Studies designed to measure the applicability of this test to different populations (Bjelland et al., 2002; Cosco et al., 2012; Norton et al., 2013) show good reliability (Bjelland et al., 2002; Zigmond and Snaith, 1983) in both the general population and in samples of patients with chronic diseases (Lynch et al., 2011; Woolrich et al., 2006).
Functional assessment of cancer therapy—breast cancer (FACT-B), version 4
The FACT-B is a self-administered scale comprising 36 items designed to assess Quality of Life (27 items) (Cella et al., 1993; Di Bella et al., 2018) and specific aspects related to breast cancer, including body image and sexual satisfaction (9 items) (Bichoo et al., 2021). It evaluates different domains of Quality of Life, such as physical, emotional, and relational aspects. Participants rate their level of agreement on a 5-point Likert scale (ranging from “not at all” to “very much”) based on their experiences over the past 7 days. Higher scores indicate a better Quality of Life across all the domains explored (Deepa et al., 2020).
Objectified body consciousness scale (I-OBCS)
I-OBCS is a questionnaire consisting of 24 items from the original English version by McKinley and Hyde (1996). Participants are asked to indicate their degree of agreement on a 7-point Likert scale (from 1: very disagree to 7: very agree). I-OBCS measures surveillance attitudes toward the body, control beliefs about one’s physical appearance, and body shame (Boursier et al., 2020). Dakanalis et al. (2017) report good construct validity, high internal consistency, and test–retest reliability.
Data analysis and sample size
The sample size required for the present study was calculated using G∗Power 3.1.9.2 software (Faul et al., 2007), for an analysis of variance with repeated measures (ANOVA) with interaction. The primary endpoint will be the difference between the two experimental groups (i.e., between-subjects factor) in the improvement of the overall MAIA scale score at pre-intervention (T0), post-intervention (T1), and follow-up (T2) times. To detect a weak-median effect size (i.e., partial η2 = 0.04), the required sample size is 40 (i.e., 20 participants in each experimental group). The type I error rate (α) was set at 0.05 (two-sided) and the power (1 - β) was set at 0.90. The collected data will be analyzed using the statistical analysis software Statistical Package for Social Science (SPSS, version 27.0).
Adherence to the intervention will be monitored and reported in the results, and data from participants who do not adhere will be managed using an intention-to-treat analysis.
The data collected in this study will be analyzed using repeated measures ANOVA to compare the outcomes between the experimental and control groups across the three time points. The primary analysis will focus on changes in the overall MAIA scale scores, allowing us to evaluate the main effects of time and group as well as the interaction between these factors. Secondary exploratory analyses will include repeated measures ANOVAs on the individual MAIA subscales and additional psychological outcomes such as anxiety, depression, and body image perception. Effect sizes and confidence intervals will be reported alongside p-values to offer a comprehensive understanding of the observed effects.
Disadvantages or undesirable effects
No inconveniences or undesirable effects are expected for research participants. It will be the responsibility of the researchers to inform on the first presentation sheet of the study the possibilitỳ for participants to discontinue participation in the research at any time, without having to give any explanation and without incurring any possible negative consequences.
Description of participants
The present study is aimed at women 18 years of age or older who have had breast cancer in the past. Participants will be recruited by email and will be informed about both the objectives and methods of the research. Regarding the questionnaires, a code will be assigned to render the collected data in a pseudonymous form. Firstly, each participant will be assigned a unique alphanumeric code, which will be used to identify them throughout the study. This code will replace any personally identifiable information in all study documents and databases, ensuring anonymity. Secondly, all data will be stored in a secure database protected by strong passwords, accessible only to authorized personnel directly involved in the study. Adherence to the study with informed consent will be requested prior to the administration of the questionnaires. Study participation is completely free, voluntary, and free of charge. All participants will have the option to discontinue the research at any time without the need to provide any explanation.
Author contributions
VS: Writing – original draft. SP: Writing – original draft. CM: Writing – original draft. KM: Writing – original draft. GP: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abrahams, H. J. G., Gielissen, M. F. M., Verhagen, C. A. H. H. V. M., and Knoop, H. (2018). The relationship of fatigue in breast cancer survivors with quality of life and factors to address in psychological interventions: a systematic review. Clin. Psychol. Rev. 63, 1–11. doi: 10.1016/j.cpr.2018.05.004
Barrett, L. F. (2017). How emotions are made: The secret life of the brain. Boston, MA: Houghton Mifflin Harcourt.
Beck, S. L., Schwartz, A. L., Towsley, G., Dudley, W., and Barsevick, A. (2004). Psychometric evaluation of the Pittsburgh sleep quality index in cancer patients. J. Pain Symptom Manag. 27, 140–148. doi: 10.1016/j.jpainsymman.2003.12.002
Bernstein, E. M., and Putnam, F. W. (1986). Development, reliability, and validity of a dissociation scale. J. Nerv. Ment. Dis. 174, 727–735
Bichoo, R. A., Mishra, A., Lal, P., Gyan, C., Agarwal, G., Agarwal, A., et al. (2021). Quality of life (QoL) in postmenopausal breast Cancer patients receiving adjuvant hormonal therapy. Indian J. Surg., 1–7. doi: 10.1007/s12262-021-02766-6
Bjelland, I., Dahl, A. A., Haug, T. T., and Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale: an updated literature review. J. Psychosom. Res. 52, 69–77. doi: 10.1016/s0022-3999(01)00296-3
Boursier, V., Gioia, F., and Griffiths, M. D. (2020). Selfie-engagement on social media: pathological narcissism, positive expectation, and body objectification–which is more influential? Addict. Behav. Rep. 11:100263. doi: 10.1016/j.abrep.2020.100263
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Berman, S. R., and Kupfer, D. J. (1989). The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Hoch, C. C., Yeager, A. L., and Kupfer, D. J. (1991). Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh sleep quality index (PSQI). Sleep 14, 331–338
Carlson, L. E., Speca, M., Patel, K. D., and Goodey, E. (2004). Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom. Med. 65, 571–581. doi: 10.1097/01.psy.0000074003.35911.41
Cella, D. F., Tulsky, D. S., Gray, G., Sarafian, B., Linn, E., Bonomi, A., et al. (1993). The functional assessment of Cancer therapy scale: development and validation of the general measure. J. Clin. Oncol. 11, 570–579
Cosco, T. D., Doyle, F., Ward, M., and McGee, H. (2012). Latent structure of the hospital anxiety and depression scale: a 10-year systematic review. J. Psychosom. Res. 72, 180–184. doi: 10.1016/j.jpsychores.2011.06.008
Czamanski-Cohen, J., Wiley, J. F., Sela, N., Caspi, O., and Weihs, K. (2019). The role of emotional processing in art therapy (REPAT) for breast cancer patients. J. Psychosoc. Oncol. 37, 586–598. doi: 10.1080/07347332.2019.1590491
Dakanalis, A., Timko, A. C., Clerici, M., Riva, G., and Carrà, G. (2017). Objectified body consciousness (OBC) in eating psychopathology: construct validity, reliability, and measurement invariance of the 24-item OBC scale in clinical and nonclinical adolescent samples. Assessment 24, 252–274. doi: 10.1177/1073191115602553
de Jong, M., Lazar, S. W., Hug, K., Mehling, W. E., Hölzel, B. K., Sack, A. T., et al. (2016). Effects of mindfulness-based cognitive therapy on body awareness in patients with chronic pain and comorbid depression. Front. Psychol. 7:967. doi: 10.3389/fpsyg.2016.00967
Deepa, K. V., Gadgil, A., Löfgren, J., Mehare, S., Bhandarkar, P., and Roy, N. (2020). Is quality of life after mastectomy comparable to that after breast conservation surgery? A 5-year follow up study from Mumbai, India. Qual Life Res 29, 683–692. doi: 10.1007/s11136-019-02351-1
Di Bella, O., Cocchiara, R. A., De Luca, A., Frusone, F., Aceti, V., Sestili, C., et al. (2018). Functional assessment of Cancer therapy questionnaire for breast Cancer (FACT-B+ 4): Italian version validation. Clin. Ter. 169, e151–e154. doi: 10.7417/T.2018.2071
Durosini, I., Triberti, S., Sebri, V., Giudice, A. V., Guiddi, P., and Pravettoni, G. (2021). Psychological benefits of a sport-based program for female Cancer survivors: the role of social connections. Front. Psychol. 12:751077. doi: 10.3389/fpsyg.2021.751077
Farb, N., Daubenmier, J., Price, C. J., Gard, T., Kerr, C., Dunn, B. D., et al. (2015). Interoception, contemplative practice, and health. Front. Psychol. 6:763. doi: 10.3389/fpsyg.2015.00763
Faul, F., Erdfelder, E., Lang, A. G., and Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 39, 175–191. doi: 10.3758/BF03193146
Ferentzi, E., Olaru, G., Geiger, M., Vig, L., Köteles, F., and Wilhelm, O. (2020). Examining the factor structure and validity of the multidimensional assessment of interoceptive awareness. J. Pers. Assess., 1–10.
Fioretti, C., Mazzocco, K., and Pravettoni, G. (2017). “Psychological support in breast cancer patients: a personalized approach” in Breast cancer. (Eds.) Veronesi, U., Goldhirsch, A., Veronesi, P., Gentilini, O., Leonardi, M. Cham: Springer.
Fischer, R., Messner, M., and Pollatos, O. (2017). Mindfulness, interoception, and the body: a measurement challenge. Mindfulness 8, 1074–1082.
Fissler, M., Winnebeck, E., Schroeter, T., Gummersbach, M., Huntenburg, J. M., Gaertner, M., et al. (2016). An investigation of the effects of brief mindfulness training on self-reported interoceptive awareness, the ability to decenter, and their role in the reduction of depressive symptoms. Mindfulness 7, 1170–1181. doi: 10.1007/s12671-016-0559-z
Frischholz, E. J., Braun, B. G., Sachs, R. G., Schwartz, D. R., Lewis, J., Shaeffer, D., et al. (1992). Construct validity of the dissociative experiences scale: II. Its relationship to hypnotizability. Am. J. Clin. Hypn. 35, 145–152
Giommi, F. (2006). Introduzione: al di là del pensiero, attraverso il pensiero in Segal ZV, Williams JMG, Teasdale JD. Mindfulness.
Glynn, B. A., Khoo, E. L., MacLeay, H. M. L., Duong, A., Cantave, R., and Poulin, P. A. (2020). Exploring Cancer patients’ experiences of an online mindfulness-based program: a qualitative investigation. Mindfulness 1, 1666–1677. doi: 10.1007/s12671-020-01380-z
Guu, S. F., Chao, Y. P., Huang, F. Y., Cheng, Y. T., Ng, H. Y. H., Hsu, C. F., et al. (2023). Interoceptive awareness: MBSR training alters information processing of salience network. Front. Behav. Neurosci. 17:1008086. doi: 10.3389/fnbeh.2023.1008086
Henderson, V. P., Massion, A. O., Clemow, L., Hurley, T. G., Druker, S., and Hébert, J. R. (2013). A randomized controlled trial of mindfulness-based stress reduction for women with early-stage breast cancer receiving radiotherapy. Integr. Cancer Ther. 12, 404–413. doi: 10.1177/1534735412473640
Higgins, E. T. (1987). Self-discrepancy: a theory relating self and affect. Psychol. Rev. 94, 319–340
Kabat-Zinn, J. (1979). Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. Delta Trade Paperbacks.
Kabat-Zinn, J. (1997). Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life. Hachette Books.
Kabat-Zinn, J. (2016). Mindfulness for Beginners: Reclaiming the Present Moment—and Your Life. Sounds True.
Kianpoor, M., Ghanizadeh, A., and Badiei, H. (2012). The relationship between dissociative experiences and the success of treatment through abstinence from opioid-use disorders. Zahedan J. Res. Med. Sci. 14, 56–60. doi: 10.1016/j.jsat.2020.108195
Laghi, F., Pompili, S., Bianchi, D., Lonigro, A., and Baiocco, R. (2020). Dysfunctional metacognition processes as risk factors for drunkorexia during adolescence. J. Addict. Dis. 38, 291–300. doi: 10.1080/10550887.2020.1756709
Lengacher, C. A., Johnson-Mallard, V., Post-White, J., Moscoso, M. S., Jacobsen, P. B., Klein, T. W., et al. (2009). Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-oncology: journal of the psychological, social and behavioral dimensions of. Cancer 18, 1261–1272. doi: 10.1002/pon.1529
LoMartire, R., Äng, B. O., Gerdle, B., and Vixner, L. (2020). Psychometric properties of short Form-36 health survey, EuroQol 5-dimensions, and hospital anxiety and depression scale in patients with chronic pain. Pain 161, 83–95. doi: 10.1097/j.pain.0000000000001700
Luiggi-Hernandez, J. G., Woo, J., Hamm, M., Greco, C. M., Weiner, D. K., and Morone, N. E. (2018). Mindfulness for chronic low back pain: a qualitative analysis. Pain Med. 19, 2138–2145. doi: 10.1093/pm/pnx197
Lynch, J., Moore, M., Moss-Morris, R., and Kendrick, T. (2011). Are patient beliefs important in determining adherence to treatment and outcome for depression? Development of the beliefs about depression questionnaire. J. Affect. Disord. 133, 29–41. doi: 10.1016/j.jad.2011.03.019
Male, D. A., Fergus, K. D., and Cullen, K. (2016). Sexual identity after breast cancer: sexuality, body image, and relationship repercussions. Curr. Opin. Support. Palliat. Care 10, 66–74. doi: 10.1097/SPC.0000000000000184
McGannon, K. R., Berry, T. R., Rodgers, W. M., and Spence, J. C. (2016). Breast cancer representations in Canadian news media: a critical discourse analysis of meanings and the implications for identity. Qual. Res. Psychol. 13, 188–207. doi: 10.1080/14780887.2016.1145774
McKinley, N. M., and Hyde, J. S. (1996). The objectified body consciousness scale: development and validation. Psychol. Women Q. 20, 181–215. doi: 10.1111/j.1471-6402.1996.tb00467.x
Mehling, W. E., Chesney, M. A., Metzler, T. J., Goldstein, L. A., Maguen, S., Geronimo, C., et al. (2017). A 12-week integrative exercise program improves self-reported mindfulness and interoceptive awareness in war veterans with posttraumatic stress symptoms. J. Clin. Psychol. 74, 554–565. doi: 10.1002/jclp.22549
Mehling, W. E., Gopisetty, V., Daubenmier, J., Price, C. J., Hecht, F. M., and Stewart, A. (2009). Body awareness: construct and self-report measures. PLoS One 4:e5614. doi: 10.1371/journal.pone.0005614
Mehling, W. E., Price, C., Daubenmier, J. J., Acree, M., Bartmess, E., and Stewart, A. (2012). The multidimensional assessment of interoceptive awareness (MAIA). PLoS One 7:e48230. doi: 10.1371/journal.pone.0048230
Norton, S., Cosco, T., Doyle, F., Done, J., and Sacker, A. (2013). The hospital anxiety and depression scale: a meta confirmatory factor analysis. J. Psychosom. Res. 74, 74–81. doi: 10.1016/j.jpsychores.2012.10.010
Olsen, S. A., and Beck, J. G. (2012). The effects of dissociation on information processing for analogue trauma and neutral stimuli: a laboratory study. J. Anxiety Disord. 26, 225–232. doi: 10.1016/j.janxdis.2011.11.003
Pardos-Gascón, E. M., Narambuena, L., Leal-Costa, C., and Van-der Hofstadt-Román, C. J. (2021). Differential efficacy between cognitive-behavioral therapy and mindfulness-based therapies for chronic pain: systematic review. Int. J. Clin. Health Psychol. 21:100197. doi: 10.1016/j.ijchp.2020.08.001
Penlington, C. (2019). Exploring a compassion-focused intervention for persistent pain in a group setting. Br. J. Pain 13, 59–66. doi: 10.1177/2049463718772148
Pérez-Peña, M., Notermans, J., Desmedt, O., Van der Gucht, K., and Philippot, P. (2022). Mindfulness-based interventions and body awareness. Brain Sci. 12:285. doi: 10.3390/brainsci12020285
Pidgeon, A. M., and Appleby, L. (2014). Investigating the role of dispositional mindfulness as a protective factor for body image dissatisfaction among women. Curr. Res. Psychol. 5:96.
Pintado, S., and Andrade, S. (2017). Randomized controlled trial of mindfulness program to enhance body image in patients with breast cancer. Eur. J. Integr. Med. 12, 147–152. doi: 10.1016/j.eujim.2017.05.009
Quattropani, M. C., Lenzo, V., Mucciardi, M., and Toffle, M. E. (2014). Psychometric properties of the Italian version of the short form of the metacognitions questionnaire (MCQ-30). BPA Appl. Psychol. Bull. 62.
Reibel, D. K., Greeson, J. M., Brainard, G. C., and Rosenzweig, S. (2001). Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen. Hosp. Psychiatry 23, 183–192. doi: 10.1016/s0163-8343(01)00149-9
Renard, S. B., Pijnenborg, M., and Lysaker, P. H. (2012). Dissociation and social cognition in schizophrenia spectrum disorder. Schizophr. Res. 137, 219–223. doi: 10.1016/j.schres.2012.02.001
Schell, L. K., Monsef, I., Wöckel, A., and Skoetz, N. (2019). Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst. Rev. 3:CD011518. doi: 10.1002/14651858.CD011518.pub2.30916356
Sebri, V., Durosini, I., Mazzoni, D., and Pravettoni, G. (2022). Breast Cancer survivors’ motivation to participate in a tailored physical and psychological intervention: a qualitative thematic analysis. Behav. Sci. 12:271.
Sebri, V., Durosini, I., and Pravettoni, G. (2023). How to address the body after breast cancer? A proposal for a psychological intervention focused on body compassion. Front. Psychol. 13:1085837. doi: 10.3390/bs12080271
Sebri, V., and Pravettoni, G. (2023). Tailored psychological interventions to manage body image: an opinion study on breast Cancer survivors. Int. J. Environ. Res. Public Health 20:2991. doi: 10.3390/ijerph20042991
Sebri, V., Triberti, S., and Pravettoni, G. (2021). The self’s choice: priming attentional focus on bodily self promotes loss frequency bias. Curr. Psychol., 1–12. doi: 10.1007/s12144-021-01400-8
Segal, Z. V., Williams, J. M. G., and Teasdale, J. D. (2014). Mindfulness. Al di là del pensiero, attraverso il pensiero. nuova edizione ampliata e aggiornata con tredici tracce audio di meditazioni guidate. Torino: Bollati Boringhieri Editore.
Tate, K. J., Newbury-Birch, D., and McGeechan, G. J. (2018). Asystematic review of qualitative evidence of cancer patients’ attitudes to mindfulness. Eur. J. Cancer Care 27:e12783. doi: 10.1111/ecc.12783
Tuthill, J. C., and Azim, E. (2018). Proprioception. Curr. Biol. 28, R194–R203. doi: 10.1016/j.cub.2018.01.064
Valenzuela-Moguillansky, C., and Reyes-Reyes, A. (2015). Psychometric properties of the multidimensional assessment of interoceptive awareness (MAIA) in a Chilean population. Front. Psychol. 6:120. doi: 10.3389/fpsyg.2015.00120
Visser, A., de Witte, T., Speckens, A. E., Prins, J. B., and Van Laarhoven, H. W. (2015). A qualitative analysis of experiences of patients with metastatic breast cancer participating in a mindfulness-based intervention. Palliat. Med. 29, 182–183. doi: 10.1177/0269216314546206
Weng, H. Y., Feldman, J. L., Leggio, L., Napadow, V., Park, J., and Price, C. J. (2021). Interventions and manipulations of interoception. Trends Neurosci. 44, 52–62. doi: 10.1016/j.tins.2020.09.010
Woolrich, R. A., Kennedy, P., and Tasiemski, T. (2006). A preliminary psychometric evaluation of the hospital anxiety and depression scale (HADS) in 963 people living with a spinal cord injury. Psychol. Health Med. 11, 80–90. doi: 10.1080/13548500500294211
Zigmond, A. S., and Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370
Zilliacus, E. M., Meiser, B., Lobb, E. A., Kelly, P. J., Barlow-Stewart, K., Kirk, J. A., et al. (2011). Are videoconferenced consultations as effective as face-to-face consultations for hereditary breast and ovarian cancer genetic counseling? Genet. Med. 13, 933–941. doi: 10.1097/GIM.0b013e3182217a19
Keywords: mindfulness-based stress reduction, breast cancer survivors, interoception, body image, psychological intervention
Citation: Sebri V, Pizzoli SFM, Marzorati C, Mazzocco K and Pravettoni G (2024) Interoception and body image in breast cancer patients: a mindfulness-based stress reduction protocol. Front. Psychol. 15:1394355. doi: 10.3389/fpsyg.2024.1394355
Edited by:
Ada Ghiggia, University of Trieste, ItalyReviewed by:
Ciro Conversano, University of Pisa, ItalyHaydee Verduzco-Aguirre, National Institute of Medical Sciences and Nutrition Salvador Zubirán, Mexico
Copyright © 2024 Sebri, Pizzoli, Marzorati, Mazzocco and Pravettoni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Valeria Sebri, dmFsZXJpYS5zZWJyaUBnbWFpbC5jb20=
 Valeria Sebri
Valeria Sebri Silvia Francesca Maria Pizzoli
Silvia Francesca Maria Pizzoli Chiara Marzorati
Chiara Marzorati Ketti Mazzocco
Ketti Mazzocco Gabriella Pravettoni
Gabriella Pravettoni