
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 27 June 2024
Sec. Health Psychology
Volume 15 - 2024 | https://doi.org/10.3389/fpsyg.2024.1390442
This article is part of the Research Topic Behaviors, Bias, and Decision-Making in Health View all 13 articles
 Ting Liu1†
Ting Liu1† Weifen Meng1†
Weifen Meng1† Wenlong Wang2
Wenlong Wang2 Guomin Sun1
Guomin Sun1 Xi Chen1
Xi Chen1 Yan Lu3
Yan Lu3 Weiping Qin4
Weiping Qin4 Yan Wang1
Yan Wang1 Lu Zhang4
Lu Zhang4 SuHua Zheng1*
SuHua Zheng1*Objective: To investigate the factors that influence health literacy (HL) among Chinese patients with rheumatoid arthritis (RA) and furnish theoretical underpinnings for the development of intervention strategies aimed at enhancing patients’ quality of life.
Methods: From May 2022 to December 2022, a comprehensive survey was conducted among both outpatients and inpatients diagnosed with (RA) in a tertiary hospital in China. The survey utilized various instruments, including a general information questionnaire, a chronic disease patient health literacy scale, the Health Assessment Questionnaire-Disability Index (HAQ-DI), the Chinese-translated Rheumatoid Arthritis Self-Efficacy Scale, the Chinese-translated Rheumatoid Arthritis Stigma Scale, and the Chinese-translated Compliance Questionnaire for Rheumatology Treatments.
Results: The average scores of HL, self-efficacy, medication adherence, and disability index were 83.54 ± 17.43, 84.91 ± 14.37, 70.16 ± 11.24, and 0.26 ± 0.44, respectively. HL in Chinese RA patients was negatively correlated with age, erythrocyte sedimentation rate (ESR), number of tender joints, number of swollen joints, and disease activity, while positively correlated with self-efficacy and medication adherence. Age, disease activity, disability index, self-efficacy, and medication adherence are predictive factors of HL, and a predictive model has been initially constructed.
Conclusion: In the management of RA, healthcare professionals should develop and implement effective intervention measures by focusing on improving medication adherence, enhancing patients’ self-efficacy, improving patients’ physical function, and reducing disease activity. This will help enhance the health literacy and promote clinical outcomes in RA patients.
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by inflammatory arthritis. In China, the prevalence of RA ranges from 0.35 to 0.45%, with an estimated total RA patient count of approximately 5 million, exhibiting a significant male-to-female ratio of 1:4 (Yu et al., 2023). Extensive research has revealed that joint diseases constitute one of the primary sources of physical disability, with RA occupying the topmost position in terms of disability rates (Bai et al., 2020). This high disability rate is attributed to the unclear etiology of RA and the absence of effective curative measures (Brown et al., 2024). Moreover, the scarcity of preventive research and delayed interventions serve as significant factors that contribute to the unfavorable prognosis of RA (Abbasi, 2017).
Health literacy (HL) is a cognitive and social skill that determines an individual’s motivation and ability to access, understand, and apply information to promote and maintain health (Nutbeam, 2008). Research has shown that HL is a crucial factor in health outcomes (Stormacq et al., 2020). Low HL among RA patients can lead to poor medication adherence and an increased risk of misinterpretation of medical advice (Nakayama et al., 2015). HL is not merely a lack of knowledge and skills; it also involves making correct health decisions through self-awareness (Zhuang et al., 2023). Studies have found that the proportion of HL in RA patients ranges from 7 to 42% (Loke et al., 2012). Many factors contribute to low HL in RA patients, including low education levels, a lack of reading habits, as well as race, income, and age-related factors (Martin et al., 2013). A study conducted in a nursing outpatient clinic in Germany revealed a significant association between high HL and low disease activity as well as high quality of life across various dimensions (Hirsh et al., 2019). A cross-sectional study of 110 RA patients found that low HL was associated with joint dysfunction (Caplan et al., 2014). A study in Ontario, Canada, showed that poor HL can lead to poor medication adherence (Gong et al., 2015).
In the early stages, most domestic and international scholars investigated the influencing factors of HL primarily from demographic characteristics. As cross-sectional studies have progressed, social and psychological factors have become hot topics of discussion (Stoll et al., 2024). However, correlation research remains comparatively scarce, and comprehensive, large-scale cross-sectional studies encompassing multiple factors are still pending. The consequence of low HL is suboptimal clinical outcomes, which ultimately impedes the progression toward high-quality healthcare. Therefore, the focus of research has shifted to how to identify the influencing factors of low HL in RA patients from multiple dimensions and perspectives. In terms of psychological factors, a higher level of HL has been linked to patient confidence (Jang et al., 2024). Hence, this study includes the self-efficacy of RA patients in a cross-sectional study on HL. Additionally, patients’ symptoms, disease activity, physical function, and self-management capabilities have also become areas of our focus. Meanwhile, as the commonly used functional HL scales have not undergone reliability and validity testing in the Chinese RA population, this study employs a chronic disease HL scale that is suitable for the Chinese population. The aim of this study is to explore factors significantly associated with HL in RA patients, reveal potential predictors of HL in Chinese RA patients, and initially develop a predictive model. This will provide theoretical support for medical professionals to accurately identify RA patients with low HL levels, develop targeted intervention measures, and improve health outcomes.
A convenience sampling method was adopted to recruit RA patients from the outpatient and inpatient departments of the rheumatology and immunology division in Changzhou, China, from May 2022 to December 2022. Inclusion criteria were: ages ranging from 18 to 79; diagnosed with RA according to the 1987 American College of Rheumatology (ACR) classification criteria; normal cognitive ability and clear expression skills; disease duration greater than 6 months. Exclusion criteria were: severe personal or family changes affecting the patient’s emotional well-being during the survey period; presence of severe diseases (such as heart failure, renal insufficiency, respiratory failure, severe infection, etc.) and extra-articular manifestations of RA; and the presence of other autoimmune diseases. The survey was conducted by a nurse from the Chronic Rheumatic Disease Management Center. After obtaining the patients’ informed consent, all questionnaires were distributed to the patients, and uniform instructions were provided for any issues encountered during completion. The questionnaires were collected on the spot, and strict confidentiality measures were implemented to protect the participants’ privacy. A total of 172 participants were surveyed in this study, and 172 valid questionnaires were recovered, with a 100% response rate. This study was approved by the Ethics Committee of our hospital with the approval number [2021] KY025-01.
The HL Management Scale (HeLMS), which was developed by Australian scholars, was translated and revised by Sun (2012) in China. The scale comprises 24 items and is divided into 4 dimensions. The total score is 120 points, and a higher score indicates a higher level of HL. Patients scoring 80% or above are defined as having high HL. The Cronbach’s alpha coefficient of this scale ranges from 0.857 to 0.947, indicating good internal consistency of the scale.
This scale was translated into Chinese by Zhu et al. (2013). It comprises 19 items, utilizing a 4-point scoring method. The CCQR score is calculated using the formula: (sum of scores for each item-19) /0.57. A score of 80 or above indicates good compliance. The intra-class correlation coefficient for the CCQR score is 0.994 (95% confidence interval: 0.990, 0.997).
This scale was adapted into Chinese by Chinese scholars Li et al. (2019). It consists of 25 items, with scores ranging from 1 to 5, and a total score ranging from 25 to 125. A higher score indicates a stronger sense of self-efficacy. The Cronbach’s α coefficient for this scale is 0.751.
This scale was revised by Geng et al. (2022). It uses a 4-point Likert scale, with a total score ranging from 20 to 80. A higher score indicates a more severe stigma. The Cronbach’s α coefficient for this scale is 0.90. The confirmatory factor analysis showed RMSEA = 0.09, CFI = 0.94, and TLI = 0.93.
Consisting of 20 items, this scale is used to assess the physical function of RA patients. Scores are categorized as mild (total score ≤ 1), moderate (1 < total score ≤ 2), and severe (2 < total score ≤ 3). The scale exhibits good reliability and validity, making it suitable for evaluating physical function limitations in RA patients (Fries et al., 1980).
Data analysis was conducted using SPSS 19.0 software. Descriptive statistical analysis was performed using means, standard deviations (SDs), medians, quartiles, absolute frequencies, and relative frequencies. Pearson’s correlation coefficient was used to explore the relationship between quantitative variables. Due to the inability to determine normal distribution previously, the Kruskal-Wallis test was used to determine the effect of variables on HL. Linear regression analysis was used to explore predictive associations among variables. A p-value of <0.05 indicates statistical significance.
The Harman single-factor test was used to assess the common method deviation in the samples. The results indicate that the interpretation rate of the first factor is 15.5%, which is significantly below the critical threshold of 40% (Podsakoff et al., 2003), thus suggesting that there is no significant common methodological bias in the data from this sample.
A total of 172 RA patients who met the inclusion criteria were surveyed, and 172 valid questionnaires were returned (response rate of 100%). The majority of RA patients were female, 72.67% were urban residents, and their ages ranged from 46 to 59 years, with a median age of 53 years. Most patients had a morning stiffness level of 1 (69.19%). Specific information on the patients is presented in Table 1.
The average scores for health literacy, stigma of illness, medication adherence, self-efficacy, and disability index were (83.54 ± 17.43), (54.51 ± 9.68), (70.16 ± 11.24), (84.91 ± 14.37), and (0.26 ± 0.44) respectively. Table 2 presents the detailed results.
As shown in Figure 1, The Spearman’s rank correlation coefficient was calculated to determine the relationship between HL (represented by HL_T) of RA patients and demographic and clinical variables. The results revealed that HL had a significant negative correlation with age (r = −0.63, p < 0.001), ESR (r = −0.19, p < 0.05), joint pain score (r = −0.16, p < 0.05), joint swelling score (r = −0.22, p < 0.01), and DAS28 (r = −0.21, p < 0.01), while it had a significant positive correlation with Total_SEFF (r = 0.45, p < 0.001) and CCQRT (r = 0.37, p < 0.001). The disease duration, pain score (VAS), PGA, and stigma score showed no significant correlation with HL and were not included in subsequent analyses.
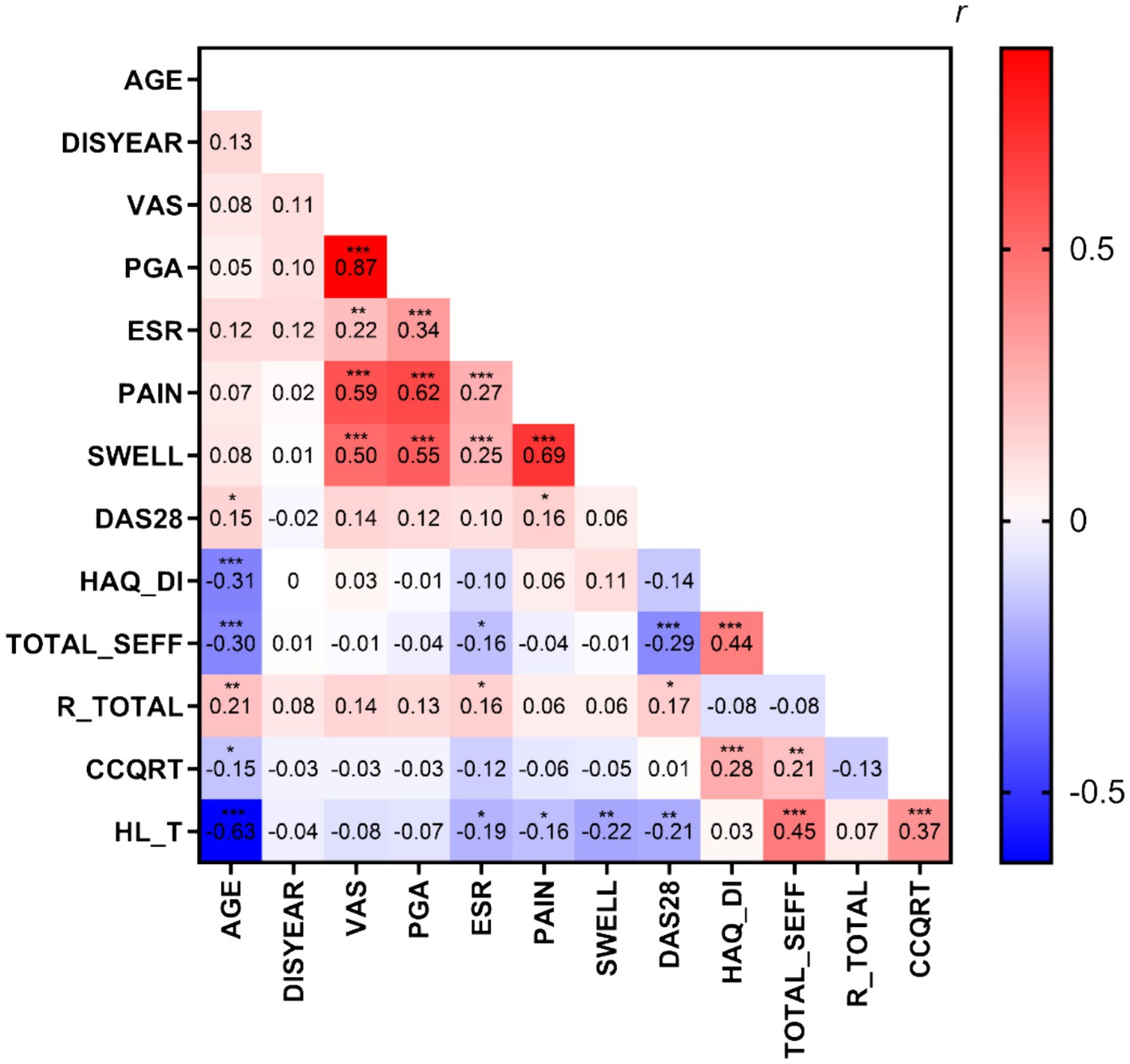
Figure 1. The heatmap of correlations between variables. DISYEAR, illness duration (month); ESR, erythrocyte sedimentation rate; pain, the total joint pain count; SWELL, the total joint swelling count; DAS28,disease activity index; HAQ-DI, total score of HAQ-DI; TOTAL_SEFF, total score of C-RASE; R_TOTAL, total score of C-ISMI-RA; CCQRT, total score of CCQR; HL_T, total score of HL Scale for chronic patients. *p < 0.05, **p < 0.01, ***p < 0.001.
The results of the univariate analysis indicated that there were statistically significant differences in HL among patients with respect to age, disease activity (DAS28), self-efficacy, and treatment compliance (p < 0.05). Although HAQ did not have a significant correlation with HL (F = 1.44, p = 0.15), it was still included in the subsequent analysis for clinical consideration, as shown in Table 3.
To determine which factors best predict HL, a stepwise multiple linear regression analysis was performed (Table 4). Spearman’s rank correlation coefficient was calculated to distinguish the relationships between these factors and HL (represented by HL_T score). Age, DAS28, HAQ_DI, self-efficacy, and CCQRT values were identified as predictors of HL. These predictors yielded a statistically significant model (F = 48.96, p ≤ 0.001), explaining 77% of the variation in the dependent variable (adjusted R2 = 0.765). The final equation is: HL = 64.67–0.82*Age - 4.20*DAS28 + 12.29*HAQ_DI + 0.46*TOTAL_SEFF +0.51*CCQRT.
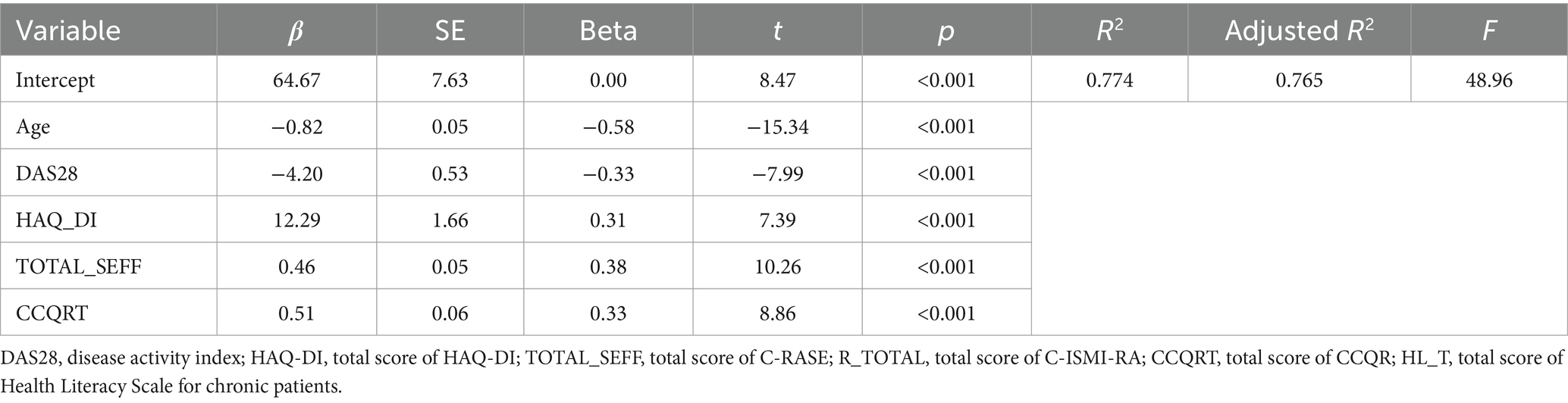
Table 4. Multiple linear regression analysis explaining the variance of HL in RA patients (n = 172).
The average HL score for RA patients in China is (83.54 ± 17.43), indicating a moderate level. Although it is still lower than the diabetic patients (Qin and Xu, 2016), significant progress has been made in the “Healthy China 2030” strategy. An effective way to improve HL among RA patients is to implement chronic disease management. China started relatively late in this regard, but China’s still actively exploring a chronic rheumatic disease management model that suits its national conditions. HL emphasizes active acquisition, critical thinking, and ultimately using the obtained information to make healthy decisions and solve problems. Foreign studies (Hirsh, 2016) have shown that low education levels can affect HL levels. In this study, 75% of the participants had an education level below high school, which created certain obstacles in accessing and utilizing health information, and may be a reason why the HL score of RA patients is at a moderate level.
Self-efficacy refers to individuals’ confidence or belief in their ability to achieve specific behavioral goals in a particular domain (Cepukiene and Puzeriene, 2024). The average score of self-efficacy for RA patients in this study was (84.91 ± 14.37), indicating that it is consistent with a cross-sectional study in Spain (Cantero-Tellez et al., 2023). The results of the multivariate analysis show that self-efficacy is a predictor of HL among RA patients. RA patients with higher HL levels are more likely to be aware of the relationship between current behaviors and health outcomes, which plays an important role in adopting and maintaining healthy behaviors (Liu et al., 2024). The study by Cantero-Tellez et al. has proven that individuals with high self-efficacy are more likely to adopt positive health behaviors (Cantero-Tellez et al., 2023). HL, self-efficacy, and their levels are closely related to health outcomes and quality of life. Enhancing self-efficacy and improving HL among RA patients, as well as changing unhealthy lifestyles, can contribute significantly to improving their quality of life.
The proportion of medication adherence among RA patients ranges from 30 to 93% (Omair et al., 2022). Some studies have shown that low HL in RA patients is associated with poor medication adherence (Contreras-Yanez et al., 2021). In this study, there was a positive correlation between self-efficacy and medication adherence (p < 0.01), which is consistent with the findings of Lavsa’s research (Lavsa et al., 2011). Simultaneously, there was also a positive correlation between disability index and medication adherence (p < 0.001), in line with Nagafusa’s study (Nagafusa et al., 2023). Multivariate analysis revealed that medication adherence is a predictor of HL. Gomez-Galicia and colleagues reported that low HL is associated with poor self-reported medication adherence among RA patients (Gomez-Galicia et al., 2022). Hirsh et al. (2020) pointed out that patients with low HL encounter difficulties in reading medication labels and prescriptions. Additional research has shown that patients with low levels of light physical activity and self-efficacy tend to have severe joint deformities and more functional limitations (Contreras-Yanez et al., 2021 Park et al., 2024). In this study, medication adherence and self-efficacy both affect HL among RA patients, but we do not know whether these two factors directly impact HL or if one factor indirectly affects HL through the other. This remains to be further explored in the future. However, it is certain that interventions targeting HL can improve patients’ long-term medication adherence, increase treatment engagement, and enhance skills in medication management.
In this study, the mean value of the Health Assessment Questionnaire Disability Index (HAQ-DI) was 0.26 ± 0.44, indicating mild functional disability. Univariate regression analysis showed no significant correlation between HAQ-DI and HL. However, based on clinical judgment, HAQ-DI was included in the multiple regression analysis, suggesting its potential as a predictor of HL. This may be related to the data sources, since most of the data came from chronic rheumatic disease management centers. Domestic experts believe that to address physical dysfunction among RA patients in China, more attention should be paid to elderly patients and those with high disease activity (Zhou et al., 2018). Currently, there are few studies on the relationship between physical dysfunction and HL, but some research has shown a close relationship between low HL and cognitive impairment (Han et al., 2015). Therefore, we hypothesize that the disability index may predict HL among RA patients, and that there may be an underlying relationship with cognitive impairment, which requires further validation.
Age (52.62 ± 12.25) and the average DAS28 score (4.48 ± 1.59) were also significant negative factors for HL. Among the recruited age range, older age was associated with lower HL. These findings are similar to previous studies (Buchbinder et al., 2006), which suggest that reading, writing, and cognitive abilities decline as patients age (Fraenkel et al., 2006). HL emphasizes the ability to read, write, access information, communicate, and understand. In terms of disease activity, higher DAS28 scores were associated with lower HL, possibly because patients experience recurrent disease episodes and poor control, leading to a complete loss of confidence in self-management. They may perceive the disease as an incurable cancer and shut themselves off from all disease-related information. Therefore, controlling the disease in a stable state is of utmost importance to improve HL.
This study shows that in Chinese RA patients, HL is negatively correlated with age, ESR, the number of tender joints, the number of swollen joints, and disease activity score (DAS28), while positively correlated with self-efficacy and medication adherence. A preliminary prediction model for HL has been established, providing a theoretical basis for healthcare professionals to develop targeted strategies to effectively enhance functional, critical, and interactive HL levels, strengthen patients’ ability to access self-disease management information, and improve their quality of life (Nutbeam and Lloyd, 2021). However, there are some limitations to this study. Although our research initially established a prediction model for HL in RA patients, covering a broad range, we still need to expand the sample size and conduct a multi-center study to validate the model in the future. Moreover, a longer follow-up time would be beneficial to further validate the model.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Ethics Committee of Changzhou Second People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
TL: Writing – original draft, Writing – review & editing, Data curation. WM: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. WW: Formal analysis, Project administration, Writing – original draft, Writing – review & editing. GS: Data curation, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. XC: Data curation, Investigation, Resources, Writing – original draft, Writing – review & editing. YL: Supervision, Visualization, Writing – original draft, Writing – review & editing. WQ: Writing – original draft, Writing – review & editing, Investigation. YW: Data curation, Resources, Supervision, Writing – original draft, Writing – review & editing. LZ: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. SZ: Supervision, Validation, Writing – review & editing, Writing – original draft.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. We thanked the support by Connotation Construction Special Nursing Discipline Support of Nanjing Medical University (No.2022–26); Beijing Bethune Public Charitable Foundation (TY149EN); General project of nursing scientific research in Changzhou Second People’s Hospital (2019HYB006).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbasi, J. (2017). To prevent rheumatoid arthritis, look past the joints to the gums. JAMA 317, 1201–1202. doi: 10.1001/jama.2017.0764
Bai, B., Chen, M., Fu, L., Liu, H., Jin, L., Wei, T., et al. (2020). Quality of life and influencing factors of patients with rheumatoid arthritis in Northeast China. Health Qual. Life Outcomes 18:119. doi: 10.1186/s12955-020-01355-7
Brown, P., Pratt, A. G., and Hyrich, K. L. (2024). Therapeutic advances in rheumatoid arthritis. BMJ 384:e070856. doi: 10.1136/bmj-2022-070856
Buchbinder, R., Hall, S., and Youd, J. M. (2006). Functional health literacy of patients with rheumatoid arthritis attending a community-based rheumatology practice. J. Rheumatol. 33, 879–886
Cantero-Tellez, R., Martin Mateos, A., Cuesta Garcia, C., Cruz Gambero, L., Garcia Orza, S., and Valdes, K. (2023). The predictive value of self-efficacy in the evolution of rheumatoid arthritis and its relationship with pain and function. Reumatol Clin 19, 549–554. doi: 10.1016/j.reumae.2023.02.010
Caplan, L., Wolfe, F., Michaud, K., Quinzanos, I., and Hirsh, J. M. (2014). Strong association of health literacy with functional status among rheumatoid arthritis patients: a cross-sectional study. Arthritis Care Res. 66, 508–514. doi: 10.1002/acr.22165
Cepukiene, V., and Puzeriene, E. (2024). Examining pain severity in women with rheumatoid arthritis: the impact of pain self-efficacy and perceived partner's emotional support. Health Psychol. Rep. 12, 14–25. doi: 10.5114/hpr/167803
Contreras-Yanez, I., Lavielle, P., Clark, P., and Pascual-Ramos, V. (2021). Markers of disease severity and positive family history are associated to significant risk perception in rheumatoid arthritis, while compliance with therapy is not: a cross-sectional study in 415 Mexican outpatients. Arthritis Res. Ther. 23:61. doi: 10.1186/s13075-021-02440-y
Fraenkel, L., Rabidou, N., and Dhar, R. (2006). Are rheumatologists' treatment decisions influenced by patients' age? Rheumatology 45, 1555–1557. doi: 10.1093/rheumatology/kel144
Fries, J. F., Spitz, P., Kraines, R. G., and Holman, H. R. (1980). Measurement of patient outcome in arthritis. Arthritis Rheum. 23, 137–145. doi: 10.1002/art.1780230202
Geng, Y. Q., Sun, G. M., Liu, T., Zhang, Z. Y., Gao, B., and Han, Z. Y. (2022). Reliability and validity test of the Chinese version of rheumatoid arthritis stigma scale. Chin J Rheumatol. 26, 683–689. doi: 10.3760/cma.j.cn141217-20211027-00435
Gomez-Galicia, D. L., Aguilar-Castillo, J., Garcia-Garcia, C., Moctezuma-Rios, J. F., Alvarez-Hernandez, E., Medrano-Ramirez, G., et al. (2022). Qualitative validation of audiovisual educational material for use on rheumatoid arthritis patients. Rheumatol. Int. 42, 2049–2059. doi: 10.1007/s00296-021-04921-4
Gong, Z., Haig, S. L., Pope, J. E., Rohekar, S., Rohekar, G., LeRiche, N. G., et al. (2015). Health literacy rates in a population of patients with rheumatoid arthritis in southwestern Ontario. J. Rheumatol. 42, 1610–1615. doi: 10.3899/jrheum.141509
Han, S. D., Boyle, P. A., James, B. D., Yu, L., and Bennett, D. A. (2015). Poorer financial and health literacy among community-dwelling older adults with mild cognitive impairment. J. Aging Health 27, 1105–1117. doi: 10.1177/0898264315577780
Hirsh, J., Wood, P., Keniston, A., Boyle, D., Quinzanos, I., Caplan, L., et al. (2020). Universal health literacy precautions are associated with a significant increase in medication adherence in vulnerable rheumatology patients. ACR Open Rheumatol 2, 110–118. doi: 10.1002/acr2.11108
Hirsh, J., Wood, P., Keniston, A., Peng, M., Ramaswami, S., Caplan, L., et al. (2019). Limited health literacy and patient confusion about rheumatoid arthritis patient global assessments and model disease states. Arthritis Care Res. 71, 611–619. doi: 10.1002/acr.23692
Hirsh, J. M. (2016). The challenge and opportunity of capturing patient reported measures of rheumatoid arthritis disease activity in vulnerable populations with limited health literacy and limited English proficiency. Rheum. Dis. Clin. N. Am. 42, 347–362. doi: 10.1016/j.rdc.2016.01.006
Jang, G. Y., Chang, S. J., and Noh, J. H. (2024). Relationships among health literacy, self-efficacy, self-management, and HbA1c levels in older adults with diabetes in South Korea: a cross-sectional study. J. Multidiscip. Healthc. 17, 409–418. doi: 10.2147/JMDH.S448056
Lavsa, S. M., Holzworth, A., and Ansani, N. T. (2011). Selection of a validated scale for measuring medication adherence. J Am Pharm Assoc 51, 90–94. doi: 10.1331/JAPhA.2011.09154
Li, X. W., Hang, C., Sun, L., Zhou, Q., Zhou, L., and Geng, Y. Q. (2019). Reliability and validity analysis of Chinese version of rheumatoid arthritis self-efficacy scale. Chin J Rheumatol. 23, 228–232. doi: 10.3760/cma.j.issn.1007-7480.2019.04.003
Liu, R., Zhao, Q., Yu, M., Chen, H., Yang, X., Liu, S., et al. (2024). Measuring general health literacy in Chinese adults: validation of the HLS (19)-Q12 instrument. BMC Public Health 24:1036. doi: 10.1186/s12889-024-17977-1
Loke, Y. K., Hinz, I., Wang, X., Rowlands, G., Scott, D., and Salter, C. (2012). Impact of health literacy in patients with chronic musculoskeletal disease--systematic review. PLoS One 7:e40210. doi: 10.1371/journal.pone.0040210
Martin, R. W., McCallops, K., Head, A. J., Eggebeen, A. T., Birmingham, J. D., and Tellinghuisen, D. J. (2013). Influence of patient characteristics on perceived risks and willingness to take a proposed anti-rheumatic drug. BMC Med. Inform. Decis. Mak. 13:89. doi: 10.1186/1472-6947-13-89
Nagafusa, T., Mizushima, T., Suzuki, M., and Yamauchi, K. (2023). Comprehensive relationship between disease activity indices, mTSS, and mHAQ and physical function evaluation and QOL in females with rheumatoid arthritis. Sci. Rep. 13:21905. doi: 10.1038/s41598-023-49380-y
Nakayama, K., Osaka, W., Togari, T., Ishikawa, H., Yonekura, Y., Sekido, A., et al. (2015). Comprehensive health literacy in Japan is lower than in Europe: a validated Japanese-language assessment of health literacy. BMC Public Health 15:505. doi: 10.1186/s12889-015-1835-x
Nutbeam, D. (2008). The evolving concept of health literacy. Soc. Sci. Med. 67, 2072–2078. doi: 10.1016/j.socscimed.2008.09.050
Nutbeam, D., and Lloyd, J. E. (2021). Understanding and responding to health literacy as a social determinant of health. Annu. Rev. Public Health 42, 159–173. doi: 10.1146/annurev-publhealth-090419-102529
Omair, M. A., Alshehri, M. M., Altokhais, N. A., Aljanobi, G. A., El Dessougi, M. I., AlHarthi, A., et al. (2022). Exploring factors influencing medication compliance in Saudi rheumatoid arthritis patients: a Nationwide cross-sectional survey-results from the COPARA study. Patient Prefer. Adherence 16, 1105–1114. doi: 10.2147/PPA.S363477
Park, H. Y., Lee, J. I., Park, Y. J., and Lim, S. H. (2024). Phase angle as a marker of physical function in non-Sarcopenic rheumatoid arthritis. Medicina 60:355. doi: 10.3390/medicina60030355
Podsakoff, P. M., Mac Kenzie, S. B., Lee, J. Y., and Podsakoff, N. P. (2003). Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 88, 879–903. doi: 10.1037/0021-9010.88.5.879
Qin, L., and Xu, H. (2016). A cross-sectional study of the effect of health literacy on diabetes prevention and control among elderly individuals with prediabetes in rural China. BMJ Open 6:e011077. doi: 10.1136/bmjopen-2016-011077
Stoll, N., Dey, M., Norton, S., Adas, M., Bosworth, A., Buch, M. H., et al. (2024). Understanding the psychosocial determinants of effective disease management in rheumatoid arthritis to prevent persistently active disease: a qualitative study. RMD Open 10:e004104. doi: 10.1136/rmdopen-2024-004104
Stormacq, C., Wosinski, J., Boillat, E., and Van den Broucke, S. (2020). Effects of health literacy interventions on health-related outcomes in socioeconomically disadvantaged adults living in the community: a systematic review. JBI Evid Synth 18, 1389–1469. doi: 10.11124/JBISRIR-D-18-00023
Sun, H. L., (2012). Research on Health Literacy Scale for Patients with Chronic Diseases and Its Initial Application. Fudan University.
Yu, F., Chen, H., Li, Q., Tao, M., Jin, Z., Geng, L., et al. (2023). Secular trend of mortality and incidence of rheumatoid arthritis in global, 1990-2019: an age period cohort analysis and joinpoint analysis. BMC Pulm. Med. 23:356. doi: 10.1186/s12890-023-02594-2
Zhou, Y., Wang, X., An, Y., Zhang, X., Han, S., Li, X., et al. (2018). Disability and health-related quality of life in Chinese patients with rheumatoid arthritis: a cross-sectional study. Int. J. Rheum. Dis. 21, 1709–1715. doi: 10.1111/1756-185X.13345
Zhu, G. H., Wang, Y. Z., and Tong, Z. W. (2013). Reliability and Validity of Chinese Compliance Questionnaire for Rheumatology. Chin. J. Gene. Prac. 16, 2803–2805. doi: 10.3969/j.issn.1007-9572.2013.08.081
Keywords: rheumatoid arthritis, health literacy, self-efficacy, medication adherence, disability index
Citation: Liu T, Meng W, Wang W, Sun G, Chen X, Lu Y, Qin W, Wang Y, Zhang L and Zheng S (2024) A cross-sectional study of predictive factors of health literacy among rheumatoid arthritis patients in China. Front. Psychol. 15:1390442. doi: 10.3389/fpsyg.2024.1390442
Received: 23 February 2024; Accepted: 10 June 2024;
Published: 27 June 2024.
Edited by:
Paola Iannello, Catholic University of the Sacred Heart, ItalyReviewed by:
Liang Huang, Minnan Normal University, ChinaCopyright © 2024 Liu, Meng, Wang, Sun, Chen, Lu, Qin, Wang, Zhang and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: SuHua Zheng, MjY5MTk3MjEyQHFxLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.