- 1Department of Kinesiology, Iowa State University, Ames, IA, United States
- 2Department of Health and Human Performance, Norwich University, Northfield, VT, United States
Middle-aged and older adults living in rural settings have been consistently less likely to report regular physical activity (PA) than those living in urban settings. While past literature has identified sociodemographic and environmental correlates of PA that may contribute to these differences, consideration of psychological correlates has been limited. A total of 95 rural and urban adults ≥50 years old provided self-reported sociodemographic information, PA level, and psychological correlates of PA including measures assessing motivation, self-efficacy, social support, and attitudes related to PA. The average participant age was 68.6 years, and most were female (62.1%) and married (70.5%). While PA level did not differ significantly between the rural and urban groups, different psychological correlates contributed significantly to separate rural and urban linear regression models considering PA status. Among rural adults, more positive attitudes toward PA, and greater PA self-efficacy and social support were associated with greater amounts of PA while for urban adults, no psychological correlates were significantly associated with PA. Psychosocial factors may be key considerations in developing more effective PA interventions in middle-aged and older adults living in rural areas.
Introduction
The benefits of regular physical activity (PA) are well documented in middle-aged and older adults (Langhammer et al., 2018; Centers for Disease Control and Prevention, 2023a). PA has an important role in helping adults preserve independence, control weight, prevent or manage chronic disease, and maintain muscle, joint and bone health (Sun et al., 2013; Langhammer et al., 2018; Eckstrom et al., 2020). PA has also been used in the prevention and management of many chronic health conditions affecting a substantial proportion of middle-aged and older adults, including cardiovascular disease, diabetes, and cancer (Anderson and Durstine, 2019). Although they can benefit from PA, middle-aged and older adults are the least physically active of any age group in the United States (Elgaddal et al., 2020), and there are further inequities in PA across many sociodemographic factors, including geographic location (Whitfield et al., 2023). Compared to urban or metropolitan older adults, fewer rural adults participate in regular PA (Cohen et al., 2018; Pelletier et al., 2021; Whitfield et al., 2023).
Several studies suggest that rural middle-aged and older adults are consistently less active than their urban counterparts (Parks et al., 2003; Martin et al., 2005; Cohen et al., 2018; Pelletier et al., 2021; Whitfield et al., 2023). However, other studies have noted higher levels of specific types of PA among adults living in more rural environments, such as recreational cycling (Arnadottir et al., 2009; Van Dyck et al., 2011; Fan et al., 2014). PA may be particularly important in rural communities, as rural adults are more likely to die from a variety of chronic diseases associated with physical inactivity including heart disease, cancer, and chronic lower respiratory disease (Centers for Disease Control and Prevention, 2023b). PA has been associated with health-related quality of life and mental health among adults living in rural areas (Hart, 2016; Smáradóttir et al., 2020). Limitations in the built environment and other structural barriers may be key drivers of rural–urban differences in PA (Brownson et al., 2009; Ferdinand et al., 2012; Sallis et al., 2020). However, improving the built environment in rural areas may not be sufficient to increase PA participation; other cultural, social, or psychological factors must be considered (Brownson et al., 2000; Trost et al., 2002; Wilcox et al., 2003; Koeneman et al., 2011; Perrin et al., 2016). Participating in regular PA is a complex behavior influenced by many factors (Trost et al., 2002; Park et al., 2015; Pelletier et al., 2021). In addition to the built environment, psychological determinants of PA, such as attitudes, expectations, beliefs, and knowledge of PA, are powerful predictors of long-term participation in PA among middle-aged and older adults (Harris et al., 2009; van Stralen et al., 2009; Kosteli et al., 2016).
While the built environment has been extensively considered in the context of PA differences between rural and urban adults, the associations of psychological factors in these contexts are unclear (Schutzer and Graves, 2004; Newson and Kemps, 2007; Kosteli et al., 2016). Psychological correlates of PA have been identified among older adults, including motivation for PA, social support for PA, and PA self-efficacy (Booth et al., 2000; Shores et al., 2009; Ayotte et al., 2010). However, comparisons of psychological correlates of PA between rural and urban adults may allow determination of specific psychological correlates that may be particularly beneficial in each setting. Identifying specific psychological correlates of PA in rural and urban older adults would allow targeted PA promotion programs for these individual populations. Thus, the purpose of this study is to assess psychological correlates of PA among rural and urban adults.
Methods
Participants
Participants were adults ≥50 years old who attended mobile health screening clinics at various locations across Iowa. Participants were invited to complete an optional PA questionnaire while waiting for their health screening. The survey probed PA participation and primary theoretical constructs underlying PA behavior (i.e., socio-ecological model, social cognitive theory, theory of planned behavior, and motives for PA). This study was approved by the Institutional Review Board and participants provided informed consent prior to data collection. Questionnaires were provided in the same order to each participant, and the questionnaires took approximately 10–15 min to administer. Participants were encouraged to contact the research team with any questions or concerns.
Rural or urban designation
The U.S. Health Resources and Services Administration guidelines (U.S. Health Resources and Services Administration, 2022), which combine US Census, Office of Management and Budget, and Rural–Urban Commuting Area classifications, were used to identify rural areas as described in previous studies (Chrisman et al., 2014; Abildso et al., 2021). Participants living in zip codes identified to be rural were assigned a “rural” label while those outside of these zip codes were assigned an “urban” label.
Primary outcome
Physical activity
The PA was measured using the Physical Activity Scale for the Elderly (PASE) (Washburn et al., 1993). The PASE is a brief instrument designed specifically to assess PA in older people over the past week. PASE is a reliable and valid measure of PA in older adults (α = 0.75) (Washburn et al., 1993, 1999).
Perceptions of an individual’s neighborhood were assessed with the Neighborhood Environment Walkability Scale (NEWS) (Saelens et al., 2003; Cerin et al., 2006). Three subscales of this measure were utilized including residential density, land use mix-access, and neighborhood satisfaction. Residential density was measured using six items inquiring about the types of buildings in an individual’s neighborhood rated on a 5-point Likert scale (“none” to “all”). Land use mix-access was assessed with seven items inquiring about access to various locations in their neighborhood (i.e., local stores, transit stops). These items are rated on a 4-point Likert scale ranging from “strongly disagree” to “strongly agree.” Finally, general neighborhood satisfaction was measured with a 17-item 5-point Likert scale. Items assessing perceptions of an individual’s neighborhood were rated from “strongly dissatisfied” to “strongly satisfied.” Internal consistencies were acceptable in the current sample (residential density α = 0.68; land use mix-access α = 0.73; neighborhood satisfaction α = 0.94).
Primary predictors
We assessed numerous psychological variables that have previously been shown to be associated with PA. We included psychological questionnaires, described in more detail below, that assessed motivation, intention, self-efficacy, barriers, enablers, social support, perceptions, and attitudes toward PA. Given the theoretical similarities between the psychological scales, a principal components analysis (PCA) was used to identify distinct psychological correlates of PA and the resulting components used as the primary predictors are described below.
Component 1: motivation for PA
Motivation for PA was assessed using the Motives for Physical Activity Measure - Revised (MPAM-R) (Ryan et al., 1997). The five motives assessed were (1) fitness, or being physically active out of the desire to be physically healthy, strong, and energetic; (2) appearance, or being active to become more physically attractive, to have defined muscles, to look better, and to achieve or maintain a desired weight; (3) competence/challenge, or being physically active because of the desire to improve at an activity, to meet a challenge, and to acquire new skills; (4) social, or being physically active in order to be with friends and meet new people; and (5) enjoyment, or being physically active because it is fun, increases happiness, and is interesting, stimulating, and enjoyable (Ryan et al., 1997). Internal consistencies were acceptable in the current sample (fitness α = 0.95; appearance α = 0.91; competence α = 0.94; social α = 0.90; enjoyment α = 0.94).
Decisional balance, or the pros and cons of PA, was determined using a 16-item questionnaire, with 10 items pertaining to pros of PA while 6 items measured cons of PA (Marcus et al., 1992). Participants rated how each item affected their decision to engage in regular PA. The pros items were summed to produce raw scores that could range from 10 to 50, while the cons items were summed to produce raw scores that could range from 6 to 30. Internal consistency was adequate in our sample (pros α = 0.97; cons α = 0.76).
Component 2: PA self-efficacy
Intention to engage in PA and perceived behavioral control of PA, concepts of the Theory of Planned Behavior, were measured using questions from a previous study involving older adults (Gretebeck et al., 2007). Perceived behavioral control was measured with 3 items rating the ease or difficulty and amount of control they had over performing PA on a Likert scale. Internal consistency was adequate in our sample (α = 0.80). Intention was measured with 2 items in which participants rated their likelihood and intention of being physically active for 30 min, 3 days/week. Higher ratings reflected greater intention to participate in PA. Internal consistency was acceptable in our sample (α = 0.91).
Self-efficacy was assessed through two measures. The Exercise Self-Efficacy Scale (McAuley, 1993) is an 8-item measure that considers the participant’s beliefs in their ability to continue exercising at a moderate intensity for 3 times/week for 40 min or more over the next month. Internal consistency was acceptable in our sample (α = 0.96). Barrier self-efficacy for PA was assessed using a 12-item scale (McAuley and Mihalko, 1998) investigating adults’ perceived capabilities to exercise three times/week for the next 3 months in the face of barriers (e.g., bad weather, lack of interest/boredom, pain, and discomfort). Internal consistency was adequate in our sample (α = 0.97).
Component 3: social support for PA
Social support for PA was assessed using a 20-item questionnaire in which participants rated how often family (5 items) and friends (15 items) engaged in acts that were supportive of PA in the past 3 months, from 1 (never) to 5 (very often) (Sallis et al., 1987). The mean of the scores were calculated, with higher scores indicating greater social support. Internal consistency was adequate in the current sample (family α = 0.94; friends α = 0.93).
Component 4: attitudes toward PA
Instrumental attitude and affective attitude regarding PA, concepts of the Theory of Planned Behavior, were measured using questions from a previous study involving older adults (Gretebeck et al., 2007). The attitude toward PA scales were measured with 8 items using a 7-point semantic differential bipolar adjective scale (from −3 to 3). Positive scores indicated a more optimistic attitude toward PA. Internal consistency was acceptable in our sample (α = 0.94).
Covariates
Participants self-reported sociodemographic and health characteristics including age, gender, education, marital status, health rating, height, and weight.
Statistical analysis
Given the theoretical similarities between the psychological scales, a principal components analysis (PCA) was used to identify distinct psychological correlates of PA. Missing data were addressed at the individual measure level, with individual measure scores imputed from the average of completed rural and urban scales. The number of imputations varied by scale: PASE: 1 (1.1%), barriers self-efficacy: 3 (3.2%), PA self-efficacy: 4 (4.2%), instrumental attitude: 9 (9.5%), affective attitude: 10 (10.5%), perceived behavioral control: 2 (2.1%), intention: 2 (2.1%), pros: 4 (4.2%), social support- family: 7 (7.4%), social support- friends: 8 (8.4%), motives- interest: 4 (4.2%), motives- competence: 3 (3.2%), motives- appearance: 4 (4.2%), motives- fitness: 4 (4.2%), and motives-social: 4 (4.2%). Imputation was performed prior to PCA analysis. As our sample size precludes inclusion of numerous covariates, demographic and health-related variables were examined for inclusion as covariates in the linear regression models based on relationships with PA using bivariate correlations. Following PCA analysis, individual linear regression models assessing the associations of the PCA components with PA level (PASE) were performed for the combined group, as well as separate rural and urban subgroups.
Results
Preliminary analysis
A PCA was performed with the summary scores of 16 measures of hypothesized correlates of PA in 95 participants. The cons of PA subscale and subjective norm item were dropped from the analysis as neither had a correlation coefficient >0.3 with any other scale, leaving 14 measures in the final PCA. The data was assessed for suitability of PCA prior to analysis. The correlation matrix demonstrated that all remaining measures had at least one correlation coefficient greater than 0.3 and the overall Kaiser–Meyer–Olkin (KMO) value was 0.84. Bartlett’s test of sphericity was statistically significant (p < 0.001), indicating data factorizability. The PCA reported four components with eigenvalues greater than one which explained 45.91, 11.32, 10.00, and 9.33% of the total variances, respectively. Scree plot visualization suggested the retention of four components (Cattell, 2023). Therefore, four components were retained.
The four-component model explained 76.56% of the total variance. A Varimax with orthogonal rotation assisted with interpretation. The interpretation of the data was consistent with identified correlates of PA with strong loadings of motivation for PA on Component 1, PA self-efficacy on Component 2, social support for PA on Component 3, and attitudes toward PA on Component 4. PCA results can be found in Table 1.
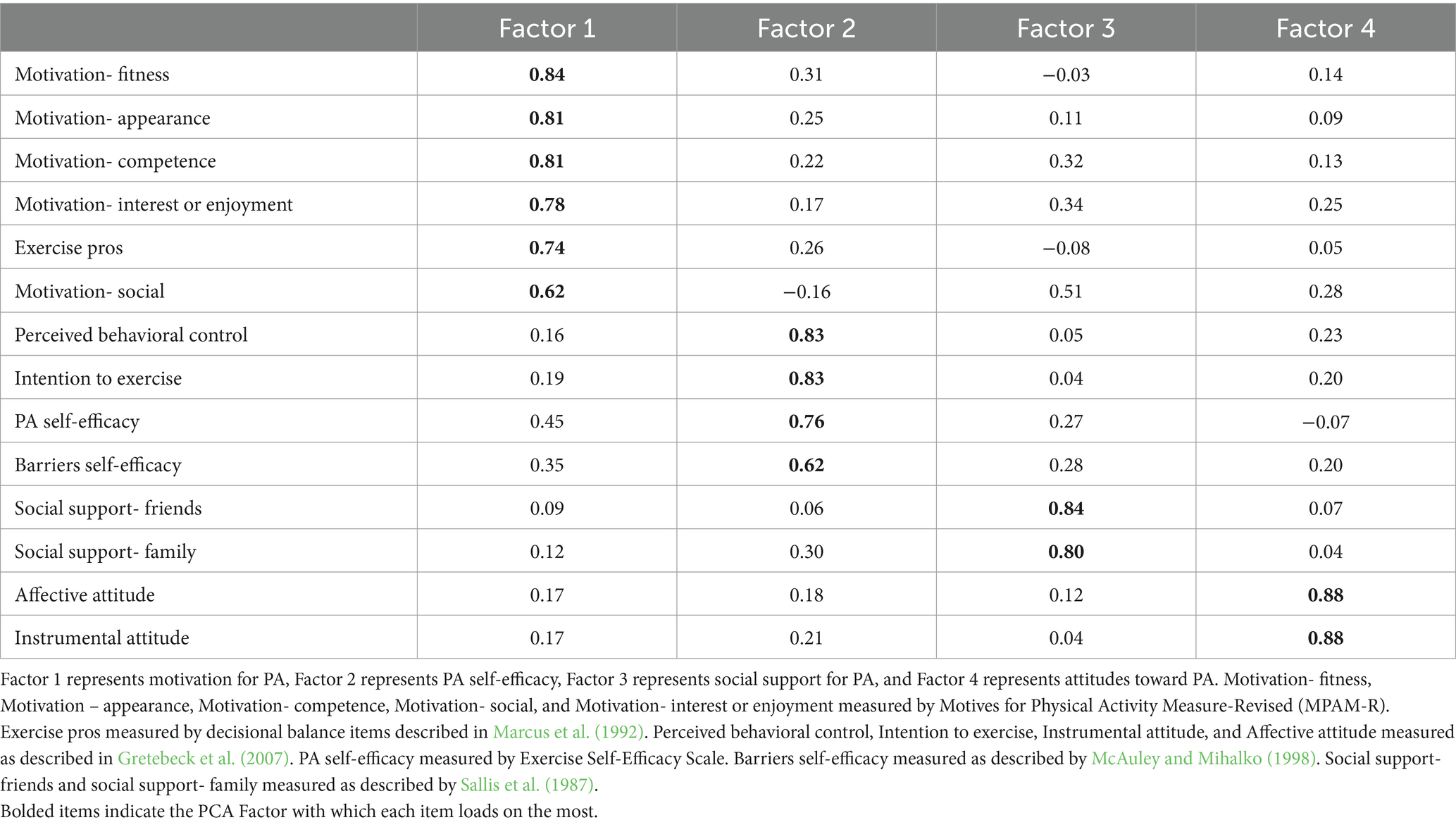
Table 1. Principal components analysis results role of psychological correlates in explaining PA in combined, rural, and urban older adults.
Bivariate correlations between PA and age, gender, education, marital status, overall health, and body mass index (by calculating weight (kg)/height (m2)) were each assessed, but only age was significantly correlated with PA [r(95) = −0.44, p < 0.001]. Therefore, only age was included as a covariate in the primary regression models.
Primary analyses
Table 2 lists baseline characteristics of the rural and urban participants. In general, urban participants were more likely to be male with greater educational attainment than rural participants. Rural participants were more likely to be married, while urban participants were more likely to be widowed. There was no significant difference in PA levels between urban and rural adults [urban M(SD) = 175.12 (82.65); rural M(SD) = 168.70 (105.69); t(93) = −0.33; p = 0.742]. Middle aged adults (<65 years old) reported higher levels of PA compared to older individuals (≥65 years old) [t(94) = 4.09; p < 0.001]. Rural adults reported more positive attitudes toward PA than urban adults, as assessed by Component 4 of the PCA [t(92) = 3.90; p < 0.001] and affective attitude [t(93) = 3.14; p = 0.002] and instrumental attitude [t(93) = 2.17; p = 0.032] subscales. Urban adults reported significantly greater PA self-efficacy [t(93) = −2.22; p = 0.029]. All other individual scale comparisons were not significant between rural and urban groups.
Results of the combined final model indicated that age [β = −0.39, t(93) = −4.24, p < 0.001] and PA self-efficacy [β = 0.29, t(93) = 3.36, p = 0.001] significantly contributed to PA level (Table 3). For the rural sample, age [β = −0.31, t(46) = −2.54, p = 0.015], self-efficacy [β = 0.28 t(46) = 2.41, p = 0.020], social support [β = 0.34, t(46) = 2.78, p = 0.008], and attitudes toward PA [β = 0.29, t(46) = 2.50, p = 0.017] were each significantly associated with PA level. In the urban sample, only age [β = −0.51, t(47) = −3.63, p < 0.001] was significantly associated with PA level. Detailed regression results can be found in Table 3.
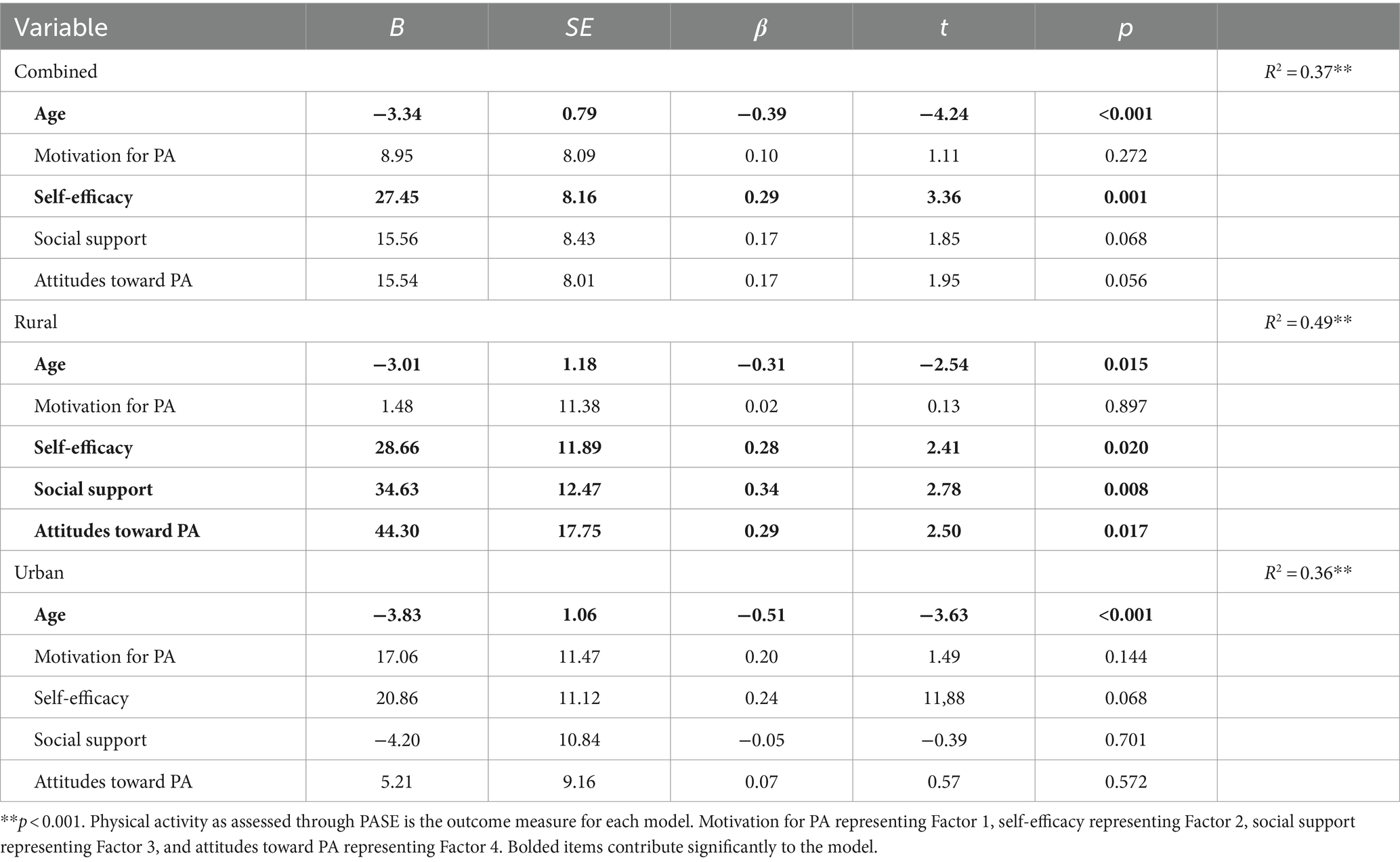
Table 3. Role of psychological correlates in explaining PA in combined, rural, and urban older adults.
Sensitivity analyses
Gender and education were explored as covariates in conjunction with age in the regression models given their established association with physical activity (Plotnikoff et al., 2004). With these added covariates, the attitudes toward PA component was also significantly associated with PA (p = 0.021) in the combined model. There were no significantly different conclusions in the rural or urban stratified models.
In an additional sensitivity analysis, we assessed associations of available neighborhood environment-related subscales with PA. Neighborhood Environment Walkability Scale (Saelens et al., 2003; Cerin et al., 2006) subscales were available for a subset of participants in our sample (residential density n = 78; land use mix-access n = 60; neighborhood satisfaction n = 89). Neither residential density, described as the perceived density of residences in an area, or land use mix-access, defined as the perceived ability to access places nearby through PA, differed between rural and urban groups [t(76) = 0.06, p = 0.949; t(58) = −0.60, p = 0.552]. However, rural adults reported greater neighborhood satisfaction than urban adults [t(87) = 2.45, p = 0.016]. Therefore, neighborhood satisfaction was included in a regression model with age and the PCA components. In the combined model, social support was significantly associated with PA in addition to age and self-efficacy. Social support (p = 0.012) and attitudes toward PA (p = 0.028) remained significant in the rural model. There were no significant predictors in the urban subsample (ps > 0.05).
Discussion
PA among rural and urban adults
This study aimed to identify psychological correlates of PA in rural and urban middle aged and older adults. Middle aged adults reported higher levels of PA compared older adults, fitting with prior literature (Spartano et al., 2019). We found similar levels of PA in rural and urban participants, which contrasts with other studies reporting that rural residents engage in less PA than their urban counterparts (Cohen et al., 2018; Pelletier et al., 2021; Whitfield et al., 2023). Possible reasons for similar PA levels in our rural and urban participants include similar perceived residential density and land use mix-access, as well as greater neighborhood satisfaction among rural participants although this was not associated with PA in any final regression models. Lack of perceived differences in location accessibility and residential density, as well as greater neighborhood satisfaction may have caused our rural subset to be more active than rural groups in previous literature (Stronegger et al., 2010; Wang et al., 2019). Age was also the strongest predictor of PA levels, and age was similar between our urban and rural samples, which has not always been the case in previous studies (Parks et al., 2003; Martin et al., 2005). Finally, while we followed HRSA rural–urban definitions, the range of populations for the rural and urban locales may not have been as extreme as in other studies. For example, the ‘urban’ zip codes in this study had an average population of 211,754 people while the rural areas averaged 25,934 people (US Census Bureau, 2010; U.S. Health Resources and Services Administration, 2022). Previous work reporting on rural–urban differences in PA has included much larger metro areas of 1–5+ million residents (US Census Bureau, 2010; Cohen et al., 2018). Thus, it is quite possible that Iowa is relatively more homogenous in its population density, which could contribute to less separation in rural and urban characteristics.
Psychological correlates of PA
Despite finding no differences in self-reported PA levels, different psychological correlates of PA were identified in stratified analyses performed with rural and urban participants. Among rural participants, greater social support, and self-efficacy, as well as more positive attitudes toward PA were associated with greater amounts of PA. This finding aligns with reports of social support barriers associated with lower PA levels among rural adults, while not urban adults (Pelletier et al., 2022). Among urban participants, however, none of the psychological correlates were significantly associated with PA. These results suggest that the association between psychological correlates and PA may differ based on rural or urban residence. Resources targeting psychological correlates of PA may be particularly impactful among rural adults, while PA may be more affected by other factors in urban adults such as the individual’s physical health and environment (Weiss et al., 2007; Sallis et al., 2012).
Interestingly, motivation for exercise, while the leading component identified by the PCA analysis accounting for nearly half of the total variance, was not significantly associated with PA in the combined, rural, or urban models conflicting with findings in prior rural and urban samples (Pelletier et al., 2022). This finding suggests that motivation, which has been viewed as a vital predictor of PA performance and public health promotion target (Teixeira et al., 2012; Molanorouzi et al., 2015), may not be the primary driver of PA behavior in middle-aged and older adults. However, our results do fit with other literature demonstrating that motivation is a weaker predictor of PA than other psychological correlates, perhaps because motivation can be transient (Ryan and Deci, 2000; Braver et al., 2014). Social cohesion has been noted among many rural communities (Avery et al., 2021), and considering group attitudes and social support may be particularly important among individuals living in rural areas. On the other hand, urban areas may have more built-in support for PA with extensive infrastructure for PA, making social support and group attitudes less important in predicting PA level among urban adults. Our results indicate that considering the environment and characteristics of the targeted population and targeting self-efficacy, social support, and attitudes toward PA may produce more effective health promotion campaigns. While many PA promotion programs have targeted the built environment and motivation for PA (Brownson et al., 2009; Ferdinand et al., 2012; Sallis et al., 2020), our findings indicate that interventions targeting self-efficacy, social support, and attitudes toward PA may be more impactful, particularly among rural adults. Further research is needed to develop these intervention programs.
Limitations
There were limitations to the present study. The study was cross-sectional, and it is possible that higher levels of PA may exert reciprocal influences on positive psychosocial correlates of PA, distinct from the impact of rural or urban setting. The sample size was limited, and our findings cannot be extrapolated to all rural and urban middle-aged and older adults. PA was self-reported, which is prone to reporting bias.
Conclusion
In summary, rural middle-aged and older adults have been consistently noted to perform less PA than their urban peers and while sociodemographic and environmental correlates have been considered in prior work, there has been little investigation of potential psychological considerations. Our findings suggest that self-efficacy, social support, and positive attitudes toward PA are significantly associated with PA in rural populations, while psychological correlates were not significantly associated with PA in urban populations. Considering these findings in identifying those at risk of low PA levels and while developing more effective and specific PA campaigns may assist in improving health in these populations. Future studies could investigate interventions targeting distinct, specific psychological correlates in rural and urban areas to assist middle-aged and older adults in increasing PA levels and health. Intervention development in improving self-efficacy, social support, and attitudes toward PA among rural adults may be particularly impactful future research. Receiving community input through focus group discussions and an iterative study design may allow identification of community factors to consider in intervention development and implementation. Evaluating community factors will allow identification of important considerations prior to implementation of costly built environment or other intensive intervention. Our results indicate that considering psychological variables rather than solely the built environment may provide impactful PA interventions, particularly among rural adults.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study involving humans was approved by the Iowa State University Institutional Review Board. The study was conducted in accordance with local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZS: Formal analysis, Methodology, Writing – original draft. AB: Formal analysis, Methodology, Supervision, Writing – review & editing. AH: Conceptualization, Investigation, Methodology, Writing – original draft. AW: Data curation, Investigation, Supervision, Writing – review & editing. JM: Methodology, Writing – review & editing. WF: Conceptualization, Data curation, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abildso, C. G., Daily, S. M., Meyer, M. R. U., Edwards, M. B., Jacobs, L., McClendon, M., et al. (2021). Environmental factors associated with physical activity in rural U.S. counties. Int J Environ Res Public Health 18:7688. doi: 10.3390/ijerph18147688
Anderson, E., and Durstine, J. L. (2019). Physical activity, exercise, and chronic diseases: a brief review. Sports Med Health Sci 1, 3–10. doi: 10.1016/j.smhs.2019.08.006
Arnadottir, S. A., Lundin-Olsson, L., and Gunnarsdottir, E. D. (2009). Are rural older Icelanders less physically active than those living in urban areas? A population-based study. Scand J Public Health 37, 409–417. doi: 10.1177/1403494809102776
Avery, E. E., Hermsen, J. M., and Kuhl, D. C. (2021). Toward a better understanding of perceptions of neighborhood social cohesion in rural and urban places. Soc Indic Res 157, 523–541. doi: 10.1007/s11205-021-02664-0
Ayotte, B. J., Margrett, J. A., and Hicks-Patrick, J. (2010). Physical activity in middle-aged and young-old adults: the roles of self-efficacy, barriers, outcome expectancies, self-regulatory behaviors and social support. J Health Psychol 15, 173–185. doi: 10.1177/1359105309342283
Booth, M. L., Owen, N., Bauman, A., Clavisi, O., and Leslie, E. (2000). Social-cognitive and perceived environment influences associated with physical activity in older Australians. Prev Med 31, 15–22. doi: 10.1006/pmed.2000.0661
Braver, T. S., Krug, M. K., Chiew, K. S., Kool, W., Andrew Westbrook, J., Clement, N. J., et al. (2014). Mechanisms of motivation-cognition interaction: challenges and opportunities. Cogn Affect Behav Neurosci 14, 2, 443–472. doi: 10.3758/s13415-014-0300-0
Brownson, R. C., Eyler, A. A., King, A. C., Brown, D. R., Shyu, Y. L., and Sallis, J. F. (2000). Patterns and correlates of physical activity among US women 40 years and older. Am J Public Health 90:264. doi: 10.2105/ajph.90.2.264
Brownson, R. C., Hoehner, C. M., Day, K., Forsyth, A., and Sallis, J. F. (2009). Measuring the built environment for physical activity: state of the science. Am. J. Prev. Med. 36, S99–S123.e12. doi: 10.1016/j.amepre.2009.01.005
Cattell, R. B. (2023). The scree test for the number of factors. Multivariate Behav Res 1, 245–276. doi: 10.1207/s15327906mbr0102_10
Centers for Disease Control and Prevention. How much physical activity do older adults need? Atlanta, GA: Centers for Disease Control and Prevention. (2023a).
Centers for Disease Control and Prevention. About Rural Health. Atlanta, GA: Centers for Disease Control and Prevention. (2023b).
Cerin, E., Saelens, B. E., Sallis, J. F., and Frank, L. D. (2006). Neighborhood environment walkability scale: validity and development of a short form. Med Sci Sports Exerc 38, 1682–1691. doi: 10.1249/01.mss.0000227639.83607.4d
Chrisman, M., Nothwehr, F., Yang, J., and Oleson, J. (2014). Perceived correlates of domain-specific physical activity in rural adults in the Midwest. J Rural Health 30, 352–358. doi: 10.1111/jrh.12065
Cohen, S. A., Greaney, M. L., and Sabik, N. J. (2018). Assessment of dietary patterns, physical activity and obesity from a national survey: rural-urban health disparities in older adults. PLoS One 13:e0208268. doi: 10.1371/journal.pone.0208268
Eckstrom, E., Neukam, S., Kalin, L., and Wright, J. (2020). Physical activity and healthy aging. Clin Geriatr Med 36, 671–683. doi: 10.1016/j.cger.2020.06.009
Elgaddal, N., Kramarow, E. A., and Reuben, C. (2020). Physical activity among adults aged 18 and over: United States. NCHS Data Brief 443, 1–8.
Fan, J. X., Wen, M., and Kowaleski-Jones, L. (2014). Rural-urban differences in objective and subjective measures of physical activity: findings from the National Health and nutrition examination survey (NHANES) 2003-2006. Prev Chronic Dis 11:E141. doi: 10.5888/pcd11.140189
Ferdinand, A. O., Sen, B., Rahurkar, S., Engler, S., and Menachemi, N. (2012). The relationship between built environments and physical activity: a systematic review. Am J Public Health 102, e7–e13. doi: 10.2105/AJPH.2012.300740
Gretebeck, K. A., Black, D. R., Blue, C. L., Glickman, L. T., Huston, S. A., and Gretebeck, R. J. (2007). Physical activity and function in older adults: theory of planned behavior. Am J Health Behav 31, 203–214. doi: 10.5993/AJHB.31.2.9
Harris, T. J., Owen, C. G., Victor, C. R., Adams, R., and Cook, D. G. (2009). What factors are associated with physical activity in older people, assessed objectively by accelerometry? Br J Sports Med 43, 442–450. doi: 10.1136/bjsm.2008.048033
Hart, P. D. (2016). Meeting recommended levels of physical activity and health-related quality of life in rural adults. J Lifestyle Med 6:1. doi: 10.15280/jlm.2016.6.1.1
Koeneman, M. A., Verheijden, M. W., Chinapaw, M. J. M., and Hopman-Rock, M. (2011). Determinants of physical activity and exercise in healthy older adults: a systematic review. Int. J. Behav. Nutr. Phys. Act. 8, 142–115. doi: 10.1186/1479-5868-8-142
Kosteli, M. C., Williams, S. E., and Cumming, J. (2016). Investigating the psychosocial determinants of physical activity in older adults: A qualitative approach. Psychol Health 31, 730–749. doi: 10.1080/08870446.2016.1143943
Langhammer, B., Bergland, A., and Rydwik, E. (2018). The importance of physical activity exercise among older people. Biomed Res Int 2018, 1–3. doi: 10.1155/2018/7856823
Marcus, B. H., Rakowski, W., and Rossi, J. S. (1992). Assessing motivational readiness and decision making for exercise. Health Psychol 11, 257–261.
Martin, S. L., Kirkner, G. J., Mayo, K., Matthews, C. E., Durstine, J. L., and Hebert, J. R. (2005). Urban, rural, and regional variations in physical activity. J Rural Health 21, 239–244. doi: 10.1111/j.1748-0361.2005.tb00089.x
McAuley, E. (1993). Self-efficacy and the maintenance of exercise participation in older adults. J Behav Med 16, 103–113. doi: 10.1007/BF00844757
McAuley, E., and Mihalko, S. L. (1998). “Measuring exercise-related self-efficacy” in Advances in sport and exercise psychology measurement. ed. J. L. Duda (Morgantown, WV: Fitness Information Technology), 371–390.
Molanorouzi, K., Khoo, S., and Morris, T. (2015). Motives for adult participation in physical activity: type of activity, age, and gender health behavior, health promotion and society. BMC Public Health 15, 1–12. doi: 10.1186/s12889-015-1429-7
Newson, R. S., and Kemps, E. B. (2007). Factors that promote and prevent exercise engagement in older adults. J Aging Health 19, 470–481. doi: 10.1177/0898264307300169
Park, S., Ahn, J., and Lee, B. K. (2015). Self-rated subjective health status is strongly associated with sociodemographic factors, lifestyle, nutrient intakes, and biochemical indices, but not smoking status: KNHANES 2007-2012. J Korean Med Sci 30, 1279–1287. doi: 10.3346/jkms.2015.30.9.1279
Parks, S. E., Housemann, R. A., and Brownson, R. C. (2003). Differential correlates of physical activity in urban and rural adults of various socioeconomic backgrounds in the United States. J Epidemiol Community Health 57, 29–35. doi: 10.1136/jech.57.1.29
Pelletier, C. A., White, N., Duchesne, A., and Sluggett, L. (2021). Barriers to physical activity for adults in rural and urban Canada: a cross-sectional comparison. SSM Popul Health 16:100964. doi: 10.1016/j.ssmph.2021.100964
Pelletier, C., White, N., Duchesne, A., and Sluggett, L. (2022). Rural-urban differences in individual and environmental correlates of physical activity in Canadian adults. Prev. Med. Rep. 30:102061. doi: 10.1016/j.pmedr.2022.102061
Perrin, A. J., Caren, N., Skinner, A. C., Odulana, A., and Perrin, E. M. (2016). The unbuilt environment: culture moderates the built environment for physical activity. BMC Public Health 16, 1–8. doi: 10.1186/s12889-016-3866-3
Plotnikoff, R. C., Mayhew, A., Birkett, N., Loucaides, C. A., and Fodor, G. (2004). Age, gender, and urban–rural differences in the correlates of physical activity. Prev Med 39, 1115–1125. doi: 10.1016/j.ypmed.2004.04.024
Ryan, R. M., and Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 55, 68–78. doi: 10.1037/0003-066X.55.1.68
Ryan, R. M., Frederick, C. M., Lepes, D., Rubio, N., and Sheldon, K. M. (1997). Intrinsic motivation and exercise adherence. Int. J. Sport Psychol. 28, 335–354.
Saelens, B. E., Sallis, J. F., Black, J. B., and Chen, D. (2003). Neighborhood-based differences in physical activity: an environment scale evaluation. Am J Public Health 93:1552. doi: 10.2105/ajph.93.9.1552
Sallis, J. F., Cerin, E., Kerr, J., Adams, M. A., Sugiyama, T., Christiansen, L. B., et al. (2020). Built Environment, Physical Activity, and obesity: findings from the international physical activity and environment network (IPEN) adult study. Annu Rev Public Health 41, 119–139. doi: 10.1146/annurev-publhealth-040218-043657
Sallis, J. F., Floyd, M. F., Rodríguez, D. A., and Saelens, B. E. (2012). Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation 125, 729–737. doi: 10.1161/CIRCULATIONAHA.110.969022
Sallis, J. F., Grossman, R. M., Pinski, R. B., Patterson, T. L., and Nader, P. R. (1987). The development of scales to measure social support for diet and exercise behaviors. Prev Med 16, 825–836.
Schutzer, K. A., and Graves, B. S. (2004). Barriers and motivations to exercise in older adults. Prev Med 39, 1056–1061. doi: 10.1016/j.ypmed.2004.04.003
Shores, K. A., West, S. T., Theriault, D. S., and Davison, E. A. (2009). Extra-individual correlates of physical activity attainment in rural older adults. J Rural Health 25, 211–218. doi: 10.1111/j.1748-0361.2009.00220.x
Smáradóttir, B. R., Kristófersson, G. K., Sigurðardóttir, Á. K., and Árnadóttir, S. (2020). Physical activity and depression among older community-dwelling adults in urban and rural areas: population based study. Laeknabladid 106, 453–459. doi: 10.17992/lbl.2020.10.600
Spartano, N. L., Lyass, A., Larson, M. G., Tran, T., Andersson, C., Blease, S. J., et al. (2019). Objective physical activity and physical performance in middle-aged and older adults. Exp. Gerontol. 119, 203–211. doi: 10.1016/j.exger.2019.02.003
Stronegger, W. J., Titze, S., and Oja, P. (2010). Perceived characteristics of the neighborhood and its association with physical activity behavior and self-rated health. Health Place 16, 736–743. doi: 10.1016/j.healthplace.2010.03.005
Sun, F., Norman, I. J., and While, A. E. (2013). Physical activity in older people: a systematic review. BMC Public Health 13, 1–17. doi: 10.1186/1471-2458-13-449
Teixeira, P. J., Carraça, E. V., Markland, D., Silva, M. N., and Ryan, R. M. (2012). Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act 9:78. doi: 10.1186/1479-5868-9-78
Trost, S. G., Owen, N., Bauman, A. E., Sallis, J. F., and Brown, W. (2002). Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc 34, 1996–2001. doi: 10.1249/01.MSS.0000038974.76900.92
U.S. Health Resources and Services Administration. Defining rural population. Rockville, MD: U.S. Health Resources & Service Administration. (2022).
US Census Bureau. Annual estimates of the resident population for counties in Iowa: April 1, 2010 to July 1, 2019 (CO-EST2019-ANNRES-19). Suitland, MD: U.S. Census Bureau (2010).
Van Dyck, D., Cardon, G., Deforche, B., and De Bourdeaudhuij, I. (2011). Urban-rural differences in physical activity in Belgian adults and the importance of psychosocial factors. J Urban Health 88, 154–167. doi: 10.1007/s11524-010-9536-3
van Stralen, M. M., de Vries, H., Mudde, A. N., Bolman, C., and Lechner, L. (2009). Determinants of initiation and maintenance of physical activity among older adults: a literature review. Health Psychol Rev 3, 147–207. doi: 10.1080/17437190903229462
Wang, Z., Qin, Z., He, J., Ma, Y., Ye, Q., Xiong, Y., et al. (2019). The association between residential density and physical activity among urban adults in regional China. BMC Public Health 19, 1279–1277. doi: 10.1186/s12889-019-7593-4
Washburn, R. A., McAuley, E., Katula, J., Mihalko, S. L., and Boileau, R. A. (1999). The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol 52, 643–651. doi: 10.1016/S0895-4356(99)00049-9
Washburn, R. A., Smith, K. W., Jette, A. M., and Janney, C. A. (1993). The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol 46, 153–162. doi: 10.1016/0895-4356(93)90053-4
Weiss, D. R., O’Loughlin, J. L., Platt, R. W., and Paradis, G. (2007). Five-year predictors of physical activity decline among adults in low-income communities: a prospective study. Int J Behav Nutr Phys Act 4, 1–7. doi: 10.1186/1479-5868-4-2
Whitfield, G. P., Carlson, S. A., Ussery, E. N., Fulton, J. E., Galuska, D. A., and Petersen, R. (2023). Trends in meeting physical activity guidelines among urban and rural dwelling adults — United States, 2008–2017. MMWR Morb Mortal Wkly Rep 68, 513–518. doi: 10.15585/mmwr.mm6823a1
Keywords: older adults, physical activity, psychological factors, rural health, urban health
Citation: Sirotiak Z, Brellenthin AG, Hariharan A, Welch AS, Meyer JD and Franke WD (2024) Psychological correlates of physical activity among adults living in rural and urban settings. Front. Psychol. 15:1389078. doi: 10.3389/fpsyg.2024.1389078
Edited by:
Pedro Forte, Higher Institute of Educational Sciences of the Douro, PortugalReviewed by:
Rafael Peixoto, Instituto Superior de Ciências Educativas, PortugalAndreia Teixeira, University of Trás-os-Montes and Alto Douro, Portugal
Copyright © 2024 Sirotiak, Brellenthin, Hariharan, Welch, Meyer and Franke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zoe Sirotiak, em1zaXJvQGlhc3RhdGUuZWR1
 Zoe Sirotiak
Zoe Sirotiak Angelique G. Brellenthin
Angelique G. Brellenthin Arjun Hariharan1
Arjun Hariharan1 Jacob D. Meyer
Jacob D. Meyer