- 1School of Psychology, Arden University, Coventry, United Kingdom
- 2Department of Psychology, Bangor University, Bangor, United Kingdom
- 3Clinical Neuropsychology Unit, Centre for Human Neuroscience and Neuropsychology, Faculty of Psychology, Diego Portales University, Santiago, Chile
- 4Brainkind, Sussex, United Kingdom
- 5Medicine, Health & Life Science Faculty, Swansea University, Swansea, United Kingdom
- 6North Wales Brain Injury Service, Betsi Cadwaladr University Health Board, Colwyn Bay, United Kingdom
Introduction: Group interventions are carried out routinely across neuropsychological rehabilitation services, to improve understanding of brain injury and aspects of impairment. Treatment provided in a group modality can bring additional perceived benefits, such as co-operative learning. However, there are very few studies which explore patient perceptions and experiences of such interventions. In the present study we investigated the experience of attending a group-based educational intervention for the consequences of acquired brain injury (ABI), which had a strong focus on emotion and emotion regulation.
Methods: Using qualitative semi-structured interviews (approximately 20 minutes), the study explores the lived experience of participating in the seven-session programme, the better to identify the perceived efficacy, salience and value of individual elements. Twenty participants with ABI took part in individual interviews, after completion of the group programme (the Brain Injury Solutions and Emotions Programme, BISEP). The study adopted a descriptive phenomenological philosophy, which focuses on lived experience to explore a phenomenon (i.e. the experience of BISEP). As regards methods, the study employed thematic analysis to cluster experiences into themes of meaning.
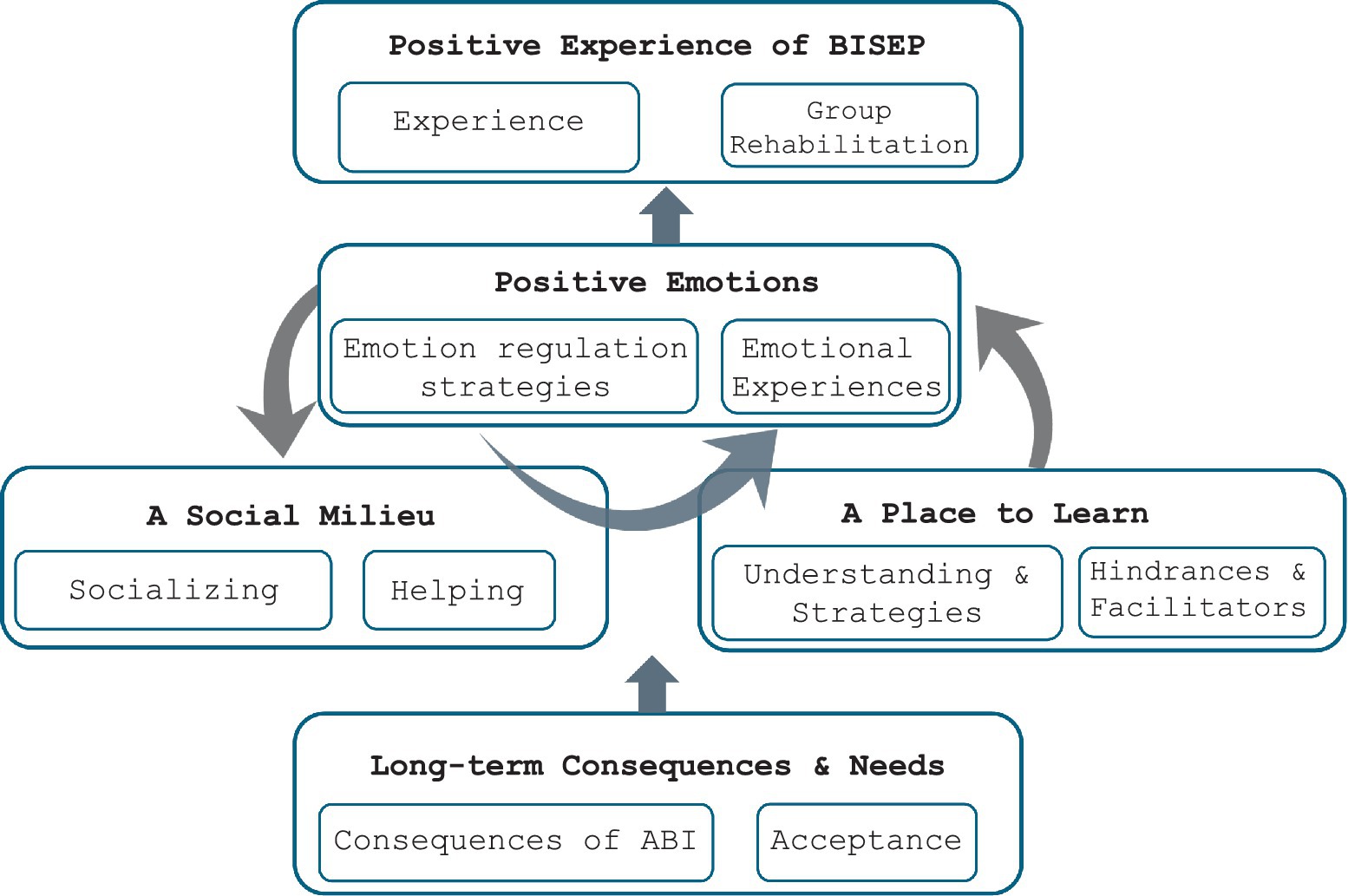
Results: Five themes were identified: (1) ‘Long term consequences and psychological needs’, which related to the persistent nature of direct consequences of injury and adjustment, and how these result in a need for interventions such as BISEP. (2) ‘Positive experiences of participating in the programme’, referred to participants’ overall experience of the programme and valued elements within it. The remaining themes referred to the programme as (3) a social milieu; (4) a place to learn; and (5) a place to promote positive emotional experiences.
Discussion: Similar to previous studies, many people reported high acceptability and perceived value of the group programme, and its role in facilitating adjustment and understanding of injury. Of particular importance was the opportunity to socialise with people who “can all relate”, in line with a growing emphasis on social rehabilitation. The findings especially highlight the relevance of emotion-focused group programmes for ABI, promoting emotion regulation, and practical tools that are delivered optimistically. Further implications for practice and future research include to focus on long term rehabilitation, a social milieu, and strategies to support adjustment.
Introduction
Neuropsychological rehabilitation has increasingly been focusing on adjustment and acceptance, consistent with an ‘emotional turn’, where feelings are placed at the heart of formulation (Wilson et al., 2009; Wilson and Gracey, 2009; Bowen et al., 2010; McDonald, 2017). Group interventions are promising vehicles to promote understanding of injury, psychological adjustment, and improve aspects of impairment (Psaila and Gracey, 2009; Patterson et al., 2016; Wilson, 2017). Evidence points to their efficacy for a range of targeted outcomes, such as cognitive impairment and coping skills (Backhaus et al., 2010; Patterson et al., 2016, for a review). However, there has been only modest qualitative research capturing the perceptions and experiences of patients to inform group intervention development and evaluation (Patterson et al., 2016).
Within neuropsychological rehabilitation, holistic approaches have received much attention in the literature (see Ben-Yishay, 2000; Ben-Yishay and Daniels-Zide, 2000; Trexler, 2000; Wilson et al., 2009; Ben-Yishay and Diller, 2011), and are effective (Cicerone et al., 2008; Turner-Stokes et al., 2015). Traditionally, holistic approaches involve very intense provision of individual and group interventions, to increase understanding and self-awareness, and address the cognitive, behavioral, and emotional consequences of ABI as a whole, providing compensation strategies to help manage difficulties (Ben-Yishay, 2000; Trexler, 2000; Wilson et al., 2009). Despite their efficacy, the service intensity and the high staff-to-patient ratio means that holistic programs are often expensive and time-limited.
In recognition that subjective experiences play an important role in recovery, contemporary holistic approaches also address embodied perspectives of consciousness (see Lo et al., 2023 for review). Embodiment in this context refers to how survivors experience and perceive the world through their ‘lived body’ – including emotions, sensations, perceptions, and all aspects of self-awareness within a physical body (Merleau-Ponty, 1962; Lo et al., 2023). A phenomenologically-informed neurorehabilitation approach considers individual experience, the body, and the entire surrounding environment relevant for recovery. For example, rehabilitation of gait disturbances in a music environment for people with Parkinson’s disease has shown promising motor, cognitive, and socio-affective outcomes (Schiavio and Altenmüller, 2015), and a case study of a woman with ABI receiving rehabilitation on a therapy ball (as opposed to a chair) demonstrating greater cognitive and behavioral performances (Martínez-Pernía et al., 2016). See Martínez-Pernía (2020) for a detailed account of experiential neurorehabilitation based on an embodied perspective. Despite its clinical relevance, such an experiential approach to rehabilitation has not yet widely transformed standard practice.
Due to the chronic nature of brain injury, survivors can experience difficulties for many years, highlighting the continued role of rehabilitation in the community (Coetzer, 2008; Turner-Stokes et al., 2015). However, the provision of neuropsychological rehabilitation in the chronic phase has been an area of little emphasis in the wider field. There are some reports that holistic approaches can be adapted to overcome barriers in low resource and long-term community settings (e.g., Coetzer, 2008; See Balchin et al., 2017, for a handbook on this topic). The North Wales Brain Injury Service (NWBIS), UK, one program which follows the philosophical foundations of the holistic model, have published extensively on this topic. NWBIS provides rehabilitation in a long-term, ‘slow stream’, out-patient setting, and provides individual rehabilitation and group interventions (Coetzer et al., 2003; Coetzer, 2008; Coetzer et al., 2018). Group-based treatment in such services typically consist of several weekly sessions, run over the course of three-weeks to three months (Patterson et al., 2016). Psycho-education about brain injury, compensation strategies for cognitive difficulties, and facilitation of emotional adjustment and awareness, are provided holistically within one program.
Interventions are carried out routinely in groups across rehabilitation settings (Tyerman and Hucker, 2016). Many, however, adopt a ‘home-grown’ approach, where interventions have been developed by clinicians at services, but are typically not evaluated empirically. Additionally, several published guides can be used to facilitate group programs (e.g., Van den Broek and Dayus, 2002; Powell, 2013; Winson et al., 2017), however these are not always evidence-based and do not have associated empirical data. The existing evidence-base for empirically-evaluated group interventions is complex, with large variation in their targeted outcome, setting and duration of delivery, intervention content, and methodological rigor (Patterson et al., 2016). Considered together, quantitative evidence suggests that group-based treatment is an effective intervention approach (Patterson et al., 2016), however further research is required to establish a more robust evidence-base.
The majority of evaluated group interventions have focused on cognitive difficulties (Patterson et al., 2016). Some have also focused on adjustment and coping (e.g., Bradbury et al., 2008; Backhaus et al., 2010), and group programs with a multidisciplinary focus (e.g., Malec, 2001). In addition to targeted outcomes, there are other benefits to group environments in ABI rehabilitation (Winson et al., 2017, p. 9). For instance, they provide an opportunity for co-operative learning, and are valued by patients and carers (Couchman et al., 2014). Providing group rehabilitation also simultaneously provides an opportunity for increasing self-awareness and social support (Anson and Ponsford, 2006; Lundqvist et al., 2010), and developing social connections with other survivors to help fight social isolation after ABI (Salas et al., 2018). There are, however, few evaluations of group programs which consider multiple aspects of ABI consequences, with an underlying holistic philosophical approach. More research is, therefore, necessary to ensure that such interventions are acceptable, efficacious, and an appropriate use of limited service resources.
A scoping review of group interventions in neuropsychological rehabilitation especially noted an absence of qualitative research, that consider participants’ perceptions of group processes and elements of intervention (Patterson et al., 2016). Understanding the ‘user experience’, or participants’ subjective accounts, in the delivery of neuropsychological interventions are key to develop and improve group programs. Qualitative research has been crucial in developing an understanding of the wider context of the rehabilitation experience (Wain et al., 2008; Levack et al., 2010; Graff et al., 2018). One patient’s account captured the discrepancy between a lack of improvement on empirical measurements and the feelings of having improved (Wain et al., 2008). This indicates the value and clinical relevance of qualitative patient accounts and experiences in refining services and interventions.
One aspect of ABI consequences that seems particularly important to include in group programs is emotion regulation (ER). This is because difficulties with emotion management, or emotion dysregulation, may be a key transdiagnostic factor of emotional difficulties after ABI (Shields et al., 2016), and have been identified as a common consequence of focal and diffuse brain injury (Bechara, 2004; Beer and Lombardo, 2007; Obonsawin et al., 2007). ER refers to processes which can influence emotion type, their intensity, and how they are experienced and expressed (Gross and Thompson, 2007). The most popular model of ER, the Process Model, includes five ER strategies, that can be implemented at key time points (Gross and Thompson, 2007; Gross, 2013). These are: (1) situation selection: choosing settings which give rise to desirable, or undesirable, emotions before the event; (2) situation modification: taking steps which change the external environment to alter the emotional impact of the situation; (3) attentional deployment: changing attentional focus, often by focusing on more desirable internal scenarios, (4) cognitive change (reappraisal): changing the meaning of a situation to alter its emotional impact, (5) response modulation: altering emotional response tendencies once they have been elicited (Gross and Thompson, 2007; Werner and Gross, 2010; Gross, 2015).
Many group interventions include an element of ER (Patterson et al., 2016, for review; Winson et al., 2017), including interventions with a Cognitive Behavior Therapy (CBT) focus (e.g., Bradbury et al., 2008; Aboulafia-Brakha et al., 2013). However, there is little consistency in the operational definitions of ER, and CBT-based interventions require appropriately trained facilitators. The available studies of targeted ER interventions appear to be growing, but still remain sparse, and with much variation in their theoretical approaches and success (Cantor et al., 2014; Tornås et al., 2016). An example of a successful ER group program is that developed by Tsaousides et al. (2017). This 24-session, web-based, group intervention conceptualized ER based on the Process Model, and involved training on specific ER strategies. Significant and continued improvement was found on the primary outcome measure of ER difficulties. However, publicly-funded services may not have the resources to carry out 24-sessions of video-conferencing, or allocate clinician time to run interventions that focus exclusively on ER. A potential avenue for such settings would be to incorporate a theoretically sound framework of ER in holistic education-based group interventions, alongside the traditional topics that are commonly seen in such programs.
Little is known about patients’ experiences of ER training provided in a group format. There are, however, a few exceptions to this. For example, Tsaousides et al. (2017) included very brief qualitative feedback interviews in their online ER intervention, and found that participants considered the program to be relevant, and enjoyed connecting with other survivors. This is an important finding, because both experience and engagement in rehabilitation programs are indicated as crucial components for outcomes (Paolucci et al., 2012; Williams et al., 2019). Though it is an individualized intervention, Karagiorgou et al. (2018) noted how Positive Psychotherapy, and specific components such as making a note of ‘Three Good Things’ in a day, facilitated positive personal growth. Due to the distressing nature of emotional difficulties after ABI (Ownsworth and Fleming, 2005; Levack et al., 2010), it is especially important to address these issues in interventions, and understand the experience and meaning of participating in such group programs and their perceived role in outcomes.
Qualitative accounts have proven important in developing our understanding of which elements are important for various rehabilitation outcomes, from patients’ perspectives (Couchman et al., 2014; Graff et al., 2018). This includes which perceived factors or experiences have positive or negative effects on motivation for rehabilitation, for example adequate provision of information, versus a lack of information or transparency from professionals (Maclean et al., 2000; Graff et al., 2018). In a meta-synthesis of qualitative research, external support (such as that provided by rehabilitation programs) was considered especially important for recovery (Levack et al., 2010). Specifically, survivors discussed the value of learning about the injury, and the ‘normalising’ effect of interacting with other survivors in community settings (Levack et al., 2010).
A number of interesting themes were identified, following the qualitative analysis of a multifamily group therapy (Couchman et al., 2014). The attendees expressed a sense of social connection, the enhancement of a sense of self-identity, and the knowledge and understanding which came from the interactions with other members. This is important, because it highlights the value of the group environment, and how the informal learning which comes from it was seen as more informative than the content of the intervention. Giving patients an opportunity to participate in rehabilitation activities with other survivors may bring therapeutic gains in terms of support and guidance, social interaction, and engagement (Patterson et al., 2016, for a review).
From a phenomenological standpoint, Martin et al. (2015) interviewed survivors of ABI to understand their lived experiences of life goals in inpatient neurorehabilitation. The authors acknowledge the importance of exploring the voices and perceptions of those with lived experience as a route to challenge our assumptions of and understand person-centered rehabilitation. For instance, they found that participants felt that rehabilitation targeted instrumental activities, but they desired social connectedness as a central life goal. An important clinical consideration developed from such a phenomenological approach is the need to consider the milieu and strategies to support social connection (Martin et al., 2015). Similarly, Panday et al. (2022) investigated patient perspectives within rehabilitation from a phenomenological philosophy, and found that autonomy, adjustment, and identity are important elements for recovery.
Phenomenology is a philosophy, methodology, and method; and refers to a subjective dimension, a focus on participants’ lived experiences of a phenomenon, and interprets an individual’s consciousness (Giorgi and Giorgi, 2003; Christensen et al., 2017; Gill, 2020; Sinfield et al., 2023) There is a variation of phenomenology types (e.g., transcendental, embodied), but Husserl’s descriptive phenomenology is involved with the description of lived experiences as a representation of a phenomenon and maintains no priori assumptions or deductive logic procedures (Willis et al., 2016). Descriptive phenomenology remains close to participants’ original experiences and meanings to understand phenomena, and thus does not seek to interpret meanings (c.f. interpretive phenomenology). Given this closeness to lived experience and people’s voices, descriptive phenomenology has been especially insightful across a range of person-centered healthcare research (e.g., Greenfield and Jensen, 2012; Shorey and Ng, 2022 for reviews). A grounding in descriptive phenomenology as an epistemological framework can lend itself to a range of analysis approaches, including thematizing meaning via thematic analysis (Sundler et al., 2019 for detailed guide).
There are three novel elements in the present study. The first is using descriptive phenomenology as a guiding philosophy to understand the lived experience of participating in a holistically-influenced group program in a low-intensity, long-term, community rehabilitation setting (i.e., the phenomenon of interest). Second, is the focus on participants’ experiences as a route to identify valued elements, perceived efficacy (or inefficacy) and acceptability (or unacceptability) of the program. Third, is to understand participants’ experience of the emotion and emotion-regulation focus of the intervention (which was based upon the over-arching theoretical Process Model [Gross and Thompson, 2007; Gross, 2013]). The present study aimed to describe participants’ lived experience of a newly developed education and skills-based group intervention (The Brain Injury Emotion and Solutions Program [BISEP]), which emphasized ER, alongside several aspects ABI consequences and psycho-education provided holistically.
Methods
Design and data analysis
The Standards for Reporting Qualitative Research (SRQR) proposed by O’Brien et al. (2014) are followed. The present qualitative study was underpinned and guided by a descriptive phenomenological philosophy, meaning that our epistemological position is that an individual’s reality (or ‘lifeworld’) is experienced through their consciousness, and we recognize the challenges that come with a focus on an objective reality. We chose this as a guiding philosophy because it was appropriate to address the risk of bias in the present study, due to the group facilitator also conducting the interviews and analysing the data. In line with this philosophy, the researcher’s goal is transcendental subjectivity – that is, the researcher’s biases are assessed through ‘bracketing’ (see Gearing, 2004) and reduction. Phenomenological reduction involves keeping at bay one’s pre-assumptions and theories, and instead stays close to the described phenomenon – this was especially important in the context that the researcher/interviewer was familiar with each individual. Bracketing involves setting aside certain elements (e.g., internal suppositions). We endeavored to set aside our knowledge of the participants’, our perceptions of how they interacted with the program, and any theories and knowledge regarding group interventions, with a pragmatic bracketing approach. A loose pragmatic approach to bracketing was employed, as some argue that completely putting aside assumptions is not possible and some assumptions are part of understanding (see Sundler et al., 2019, for review). A descriptive philosophy underpinning was also chosen because of its emphasis on ‘the lifeworld’ – the lived experience of participants in the present study must be interpreted in line with their subjectivity, interactions, and the ‘world’ of the phenomenon of interest (the group program and the physical and emotional space in which it happens).
Descriptive phenomenology was used to describe and articulate the essential features of the phenomenon of interest (experiences of and during the group rehabilitation program). We let the principles of openness, reflexivity, and questioning pre-understanding guide the entire process (i.e., following suggestions of thematic analysis for descriptive phenomenology by Sundler et al., 2019). The data was then analyzed using thematic analysis (Braun and Clarke, 2006; Maguire and Delahunt, 2017). Thematic analysis is considered an appropriate method for a variety of qualitative research questions, across a range of epistemologies (Nowell et al., 2017). We follow the thematic analysis for descriptive phenomenology guide by Sundler et al. (2019), which follows and inductive approach which is grounded in the data and experience of participants, and involved searching for patterns of meanings and their complexity (not necessarily their frequency) and how these can be organized into themes.
Interviews were conducted in person, and audio-recorded on a Dictaphone. The recording was immediately transferred to a password protected computer after the session, and deleted from the device. After transcribing the interviews verbatim, the first step was data familiarization. This was done by the first (LR) and second author (CS) reading and re-reading the transcripts in an open-minded manner to avoid confirmation bias when familiarizing with the data. Next, the transcripts were exported into an Excel spreadsheet. Preliminary codes were generated to identify the essence of the data or meanings, in three waves. Fifty percent of the data was double coded by two independent coders (LR and CS), who first coded one interview before meeting to discuss the codes. They then independently coded four additional interviews before meeting to discuss and agree on codes once more. Finally, they independently coded five more interviews and met to discuss any disagreements or discrepancies. During each wave of coding checks, the coders discussed the inclusion and exclusion criteria, and how the meanings represented by the codes, as a form of data validation. The second coder acted as a critical friend, whereby the first author’s reflections, perceptions, and potential biases were discussed and critiqued. The remaining 50 % of the interviews, which were shorter in duration, were then single coded by the first author before zooming in and back out again to continue checking for any biases or preconceptions.
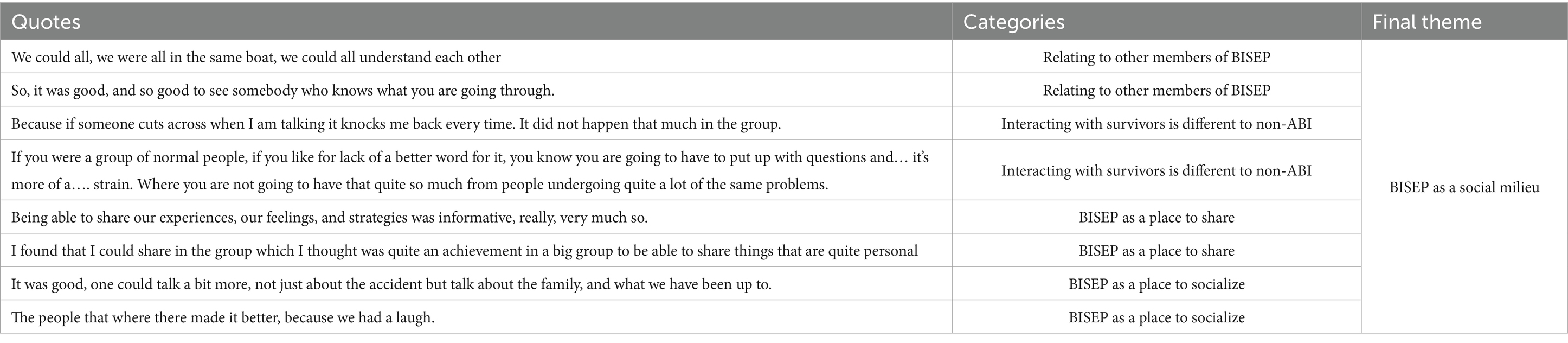
The next phase involved searching for broad patterns among the meanings and structuring categories, with a particular focus on those relating to participants’ experience of and within the group program, and its elements. The emerging categories were modified using the constant-comparison approach, where researchers compared newly uncovered and pre-existing codes. These categories were then clustered into derived themes and sub-themes. Using triangulation. All themes and underlying interview extracts were discussed, reviewed, and refined by both coders, and triangulation of the data was achieved with the inclusion of 7 participant reviewers who confirmed the themes were justified interpretations of their transcripts. Finally, themes were allocated names which were reflective of the lived experiences, and example transcripts were chosen. No qualitative analysis software was used on the data, so that coders could remain closer to the data. See Table 1 for example of theme development process.
Participants
In total, twenty participants with ABI were invited to take part (17 men, 3 women), after first being approached over the telephone approximately two-weeks following attendance of a group psych-education program at the North Wales Brain Injury Service (NWBIS), Betsi Cadwaladr University Health Board (BCUHB). These twenty participants were from three separate but consecutive waves of BISEP (n = 8, n = 7, n = 5). The average age of the group was 50 (SD = 10.24, range 26–67). The average time since injury was 7 years (SD = 7.54, range 9 months – 32 years). Seven participants had suffered a cerebrovascular accident (CVA), 11 a traumatic brain injury (TBI), one who had an ABI following encephalitis, and one who sustained a hypoxic brain injury. All participants agreed to take part, and nobody withdrew from the study. The over-representation of men in the sample is reflective of the neurorehabilitation environment within NWBIS and within rehabilitation more generally (Frost et al., 2013).
Procedure
The study was granted Ethical Approval by BCUHB (224613) and the School of Psychology, Bangor University. Participants were invited to attend the 7-session psycho-education group intervention, the Brain Injury Solutions and Emotions Program (BISEP). The program was facilitated by the first author (LR), and an additional member of the clinical team at NWBIS. The co-facilitator was kept constant as much as was possible. Each session lasted two hours, with a 15 min break approximately half-way.
Participants from three separate waves of BISEP took part in face-to-face qualitative feedback sessions, approximately 2 weeks after completing the program. It has been suggested that a minimum of twelve participants are required for data saturation (Guest et al., 2006), however, in the present study, data-saturation was judged to have been achieved through constant-comparison and analysis of data until no new themes emerged (N = 20). Interviews were carried out in a quiet room at Bangor University or NWBIS, and in patients’ homes in cases where travel was difficult. Only the researcher and participant were present for the sessions. The interviews lasted approximately 20 min (M = 18.52, SD = 6.38), were audio-recorded, and transcribed verbatim. A semi-structured interview format with prompts was used, i.e., “What are your thoughts on the BISEP?,” “What did you value most?,” “Are there any aspects that could be improved?,” “Has the program helped you understand how to manage your emotions better- in what way?,” “Have you used things from the sessions in your day to day life?.” Session-by-session prompting was used to assist participants’ recall. A collaborative interview approach with scaffolding was used, to help participants develop narratives (Paterson and Scott-Findlay, 2002; Carlsson et al., 2007, for a review). The questions were selected to be as open as possible, and the interview protocol was pilot tested with the first two participants. No changes were made to the protocol following the pilot testing, and data included in the present study. For interview protocol and additional prompts, see Appendix.
The intervention – the Brain Injury Solutions and Emotions Program (BISEP)
BISEP, like all such group programs, has general elements, such as increasing awareness and understanding of injury, and facilitating adjustment. Strategies and compensation methods are also offered to help with common difficulties (e.g., problem solving and executive function, memory, and fatigue). Uniquely, the program is designed to have a strong emphasis on emotion, ER, and promoting positivity, and these elements are thus threaded throughout the entire program.
BISEP consists of: (1) an introductory session, (2) a session on anatomy and mechanisms of injury, (3) a session on emotional changes, (4) emotion regulation, (5) problem solving, (6) memory, and finally (7) fatigue. Participants receive a workbook every session, which includes the content, skill building and group exercises, and discussion prompts.
In the ‘Emotion Regulation’ session, ER strategies from the Process Model (situation selection, situation modification, attentional deployment, and cognitive change1) are conceptualized as ones to use ‘before’ (situation selection), ‘during’ (situation modification, attentional deployment), and ‘after’ (cognitive change) an emotional event. The positive element is threaded throughout the entire program, and includes the ‘Three Good Things’ intervention from the field of Positive Psychology (Seligman et al., 2005), as a daily homework. This involves making a note of three things that go well each day with a short causal explanation.
Researchers’ reflexivity
The research was led by the first author (LR), who also conducted the interviews. LR, a female PhD student, had previous experience of qualitative research with people with ABI. She also received further training by the third and fifth authors (RC and OT), who have decades experience of clinical research with ABI participants. LR and CS coded the data, and CS, a clinical neuropsychologist, had previous experience of conducting qualitative studies with survivors of ABI. As mentioned, CS acted as a critical friend through the coding process, ensuring that we stayed close to the data. Finally, research themes and interpretations were scrutinized by SB through collaborative reflexivity with the first author, to ensure methodological rigor and challenge any underlying assumptions. No theme changes were required as a result of this process.
An important consideration was that the interviews were conducted by the BISEP facilitator (LR). The participants were, therefore, familiar with the researcher, and she would have known all participants for a period of 12 weeks (from group intervention recruitment/invites and pre-discussions, to the end of the 7 week program). This may have influenced the methodological rigor. In particular, participants may not have disclosed negative comments or critiques, or exaggerated the positive elements. However, an existing bond may have facilitated a conversational style of interviewing, that is recommended for participants with brain injury (Paterson and Scott-Findlay, 2002). The participants were informed that all their experiences and feedback were important for the evaluation, including constructive comments. All effort was made to encourage participants to feel comfortable disclosing issues. We also mitigated this by having a second coder (CS) who was not part of the service or the groups, and the fourth author (SB) who was external to the project to scrutinize the themes. As part of bracketing, the first author reflected and noted any assumptions, current knowledge, biases, and expectations based on her experience of running the groups and her subject expertise, and reflected on these within supervision. All effort was made to step away from these, and to interview and analyze the data from the position of an ‘unknower’, e.g., by asking prompting questions based on what is said in the moment and not any context or knowledge.
Results
Five themes of meaning were identified in the data, each consisting of two sub-themes. See Figure 1 for visual representation. The names associated with the quotes provided have been changed to protect participants’ identities.
Theme one: long term consequences and needs of ABI survivors
This core theme (experienced by all participants but one) was related to the persistent nature of post-injury impairment, and how these result in a need for interventions such as the group program BISEP. The data show that in the early phases post-injury (9–24 months) or even in the chronic phase many decades following the injury, an ABI tends to affect every-day functioning in similar ways. Though the long-term consequences of ABI survivors were not directly related to the group program experience of environment, the presence of this experience in participants’ accounts was overwhelming, and highlighted their need for support (such as group intervention).
Two sub-themes were identified. The first related to the experiences of direct consequences of a brain injury, described by the majority of participants. This included cognitive impairments, fatigue, and difficulties with communication. Such difficulties resulted in some individuals having to “take a step back” from engaging in social activities. As described by Emyr:
“… if someone cuts across when I am talking, it knocks me back every time […], so you tend to take a step back from everything because that happens. And like I said, when I am tired and when I have to really think to get the right words and things like that, it really tires me, so I take a step back.”
And as described by Peredur:
“The real problems are the ones I’m giving a good example of at the moment… That’s… communicating and… The main part of my brain, all the thinking bits, go on fairly normally… Unaffected… erm… and … so, I can sit in a chair and think about something and pretty effective at doing it, it’s only when making sense of it when trying to get it out.”
The most common ABI consequence experienced by participants related to emotional changes and ER difficulties. Many participants reported experiencing low mood, or feeling “so sad.” A number also described how anxiety or “panic” made it difficult to engage in previously enjoyed leisure activities. Difficulty with managing emotions, or using maladaptive ways of coping, were also present in the data.
“James: I’ve just, because I’m disabled, and I think about what I was like, before…
LR: So, when this sort of thing happens what do you do?
James: Go for a walk. Seems to be the only thing… I’ve got loads of things to do but I cannot do them. But bad things too, like having a drink. I had given up before this happened to me […] I do not drink much but I have started drinking again, it’s an escape really.”
The second sub-theme related to the process of acceptance and adjusting to the long-term consequences described above (experienced by more than half of the participants). The dramatic change in functioning and identity from pre-injury levels, challenged participants’ ways of living, and was a common theme from participants early after injury to the chronic phase. This adjustment was described as analogous to a ‘journey’. For Emyr, the stark contrast to his pre-injury function, was difficult for him to “get over.”
“I always go back to the same place in my head. Thinking about years ago, and the type of work I did in a day. In the past, if someone had called me saying there was a job in Scotland I would have just gone straight away there. Those things I miss. Those are the things I cannot get over at this time. It’s all behind me.”
And for Gethin:
“I was angry last year, I was… angry… why did it happen to me to start with, and angry it was taking me so long to recover. But this year, I’ve had to accept, and I have accepted, that it is going to take time. And maybe never get back to the way I used to be anyway […] Any progress I look forward to it like.”
Other participants were objectively further on in their time since injury, but seemed earlier in their process of acceptance. For example, Huw:
“I cannot accept it. It’s… do not know… I could do without it. It stopped me in my tracks.”
Theme two: positive experience of participating in BISEP
A second core theme related to participants’ general positive experience of participating in the program, and various valued elements which contributed to this experience (mentioned by all participants). Group members’ accounts especially reflect the relevance of group programs within neurorehabilitation.
Two sub-themes were, again, identified. The first related to the positive experiences of BISEP and various elements of the program. Some group members’ experienced that it took “time to get into it.” As participants relaxed in each other’s company many reported that they began to both “enjoy” and “benefit” from it. BISEP was a place where they felt positive, “safe,” free of judgment, and a place where they could benefit in terms of recovery.
Cai: “We were there in our safe zone, nobody could judge us on anything, and we had a great time.”
For a smaller number of participants, BISEP was a place where they experienced a sense of “achievement” toward the activities or end-of-program party, or developed “confidence.”
Bevan: “… you think you have achieved something because you have done your little bit, and everyone else has done their little bit, so you can buzz off eachother.”
The positive overall experience of BISEP appeared to become an important part of their routine, and something to “look forward to” each week. Half of the group members referred to the role of the facilitators, and their personalities, as especially important for a positive BISEP experience, and “encourages people to think in [a positive] way.”
As Iolo describes:
“I think the group, I’d give it like a ten out of ten – it’s fantastic. Really everything about it, the people who run it, the personalities, the warmth, the knowledge, the care, the empathy as well […] People really bonded over the humour, and it was all because the whole group was run in such a positive way on every level. […] There was always this positive- it’s just walking in that room each week was like walking into a warm, sunny day.”
These positive experiences of BISEP stood in contrast to participants’ experiences of acute care, and highlight the smaller sub-theme (described by half of the participants), The relevance of group rehabilitation programmes. Many participants expressed negative experiences of acute care, and a disconnect when returning to adjust in their community. In the face of these negative reflections, participants emphasized the relevance of group rehabilitation programs such as BISEP. Emyr expressed that there is a need for more rehabilitation resources in “Cymraeg” [the Welsh language], in particular. Individuals expressed that there is a need for the program to “continue,” and participants would like more opportunities to take part in groups. Consider the case of Rhys:
“Get another one sorted. Sort another one as soon as possible. Do anything. And even if a group is set up again, I would attend the meeting.”
And Angharad:
“I just think, well, we are so lucky to have it. I think it should be… we are though, honestly. You know how the NHS is, it struggles massively, and how lucky are we to be able to have something like that.”
Theme three: BISEP was a social milieu
The third major theme related to the therapeutic function of socializing with other ABI survivors, within the context of the group rehabilitation program. This was reported by all participants.
The first sub-theme related to the experience and value of socializing. Participants valued the opportunity to be among people that were “in the same boat,” and could, therefore, “understand” much of their experience. This opportunity to “share” with people who can “relate,” in a setting of mutual understanding, was of greater value to many participants than any other component of BISEP. This appeared to be “reassuring” and brought a sense of normality to the group. For one participant, however, comparison to others was a difficult part of relating to other survivors, and contributed to negative emotional experiences.
For Gethin, the biggest value of BISEP was sharing with people who could relate to the effects of brain injury:
“Gethin: Exchanging stories with the other people really. Yeah, we all have something in common, that’s the main point. […] Especially from the invisible injury side. Because we can all relate to each other in that respect.”
Similarly, for Cai:
“LR: What did you value most?
Cai: Erm… I would probably say, what jumps out of my mind, would be sitting down with people who have been through brain trauma like I have, and looking at them and listening to their stories, I would not say comparing them to mine but thinking: ‘He’s going through exactly the same thing as I did, and about the same time as I did’. I might be years on from what they are going through now. I also think that erm…staying in touch with some of them characters and helping them, if they had a bad day, or if I had a bad day and vice versa. That camaraderie that you can sort of get from a group like that is invaluable.”
BISEP opened the possibility for people to “enjoy a social setting in a managed way.” That is, the positive experience of interacting with members of BISEP stood in stark contrast to their experiences of people who do not have a brain injury. Some participants reported difficult experiences of interacting with people. As described by Morgan, “People that do not know that you have cracked your head, they look at you and they treat you like you are a bit of a, I do not know, a bit stupid.” Peredur and Emyr both experienced pressures to act “normal” from people in the ‘outside’, which were substantially reduced when interacting with people in BISEP:
Emyr: “I could tell people ‘I’ve had a brain injury’, but it just is not the same as if someone had broken a finger or arm, it just does not ever go away. And people from outside think ‘Oh, he looks ok now, he must be better, he is better now’. But it is not like that… So, in the groups, you come across people who understand, and are the same.”
A smaller sub-theme, reported by few of the participants, was the opportunity to help other group members through sharing their experiences. For these participants, being in a position where they could help somebody else resulted in a positive emotional response. Helping others, or being able to “contribute” to the group, appeared to serve a positive function.
For example, the case of Lewis:
“I sort of tried to help, what I’ve learned to pass on to them […] It was good for me. Made me feel good, put it that way. I’d come home and I’d think ‘Yes I’ve helped somebody today’. Whatever shape or form it took, you have still done a good thing. And I like that. So, doing that for them, was good for me.”
Theme four: BISEP was a place to learn
A key theme, reported by all participants consisted of the learning which took place during BISEP, and the many dimensions of that learning process. Two sub-themes were identified. The first, developing an understanding of ABI and learning strategies to manage difficulties, was experienced by the majority of participants.
Participants’ narratives suggest that they experienced the content as “very informative” and “relevant.” For many, they experienced BISEP as a place to learn about “how the brain works,” and through developing an understanding of brain injury they became “less confused” about their situation.
Angharad: “Even though I knew bits from [previous career in medicine], I did not know it for me. I had never put me in that brain.”
Participants also discussed learning specific “strategies” to help manage difficulties. The patients especially valued suggestions about “tools for every-day life,” and that adopting strategies could make “life easier.” Not only did participants value the learning which came from the content and the facilitator, but participants were able to learn from each other. Survivors were seen as a source of help similar to that provided by professionals.
In the case of Aled:
Aled: The information definitely was comprehensive and very informative. I’ve taken on board quite a few of the strategies. And the strategies I’ve picked up off different clients. We were able to learn off each other and take information off each other. There’s so many different things you have mentioned that I’ve implemented really to make life easier for yourself. And it certainly does make life easier, and much more comfortable within yourself doing different things, having adopted strategies.”
The second sub-theme related to things that hindered or facilitated learning in BISEP, described by three-quarters of participants. ABI consequences, such as difficulty with memory, or concentrating, could act as barriers to learning or engaging during BISEP. Related to this, three participants stated that there was “too much information” in sessions for it all to be digested. However, some participants described implicit learning which they may not be able to explicitly recall on the spot, but if a situation were to arise, they might implement learned material “automatically.” Consider, for example, the case of Cai who experienced that: “in every meeting, you learn something, you might learn something subconsciously or consciously.”
Participants also suggested that certain existing elements of the program facilitated learning, and helped compensate for challenges with the learning process. One such element was the use of 3D models of the brain and skull during the session about anatomy, to enhance experiential learning. Another essential component of BISEP that half of the participants found helpful was the handouts/booklets that they received with each session. These acted as a transitional resource, so that participants could “refer back to” and “refresh” their memories. This resource also allowed learning to continue even after BISEP has finished. Finally, some participants suggested that they would like even more sessions to go through things further, or to have an opportunity to revisit.
For Arwyn:
“As I’ve said before, I often refer to the notes I’ve been given, and I refer to the notes that I personally take to refresh my memory, and also to think in different ways. Because… sometimes things do not occur to you at that particular time, but if you appraise, and go over what you have learned, you are more likely to find something that will stimulate you or present a strategy or whatever. It’s an on-going thing really.”
These experiences of learning through the BISEP program demonstrate how knowledge is experienced as powerful for emotional healing post-injury, yet participants require significant support through learning resources and memory aids.
Theme five: BISEP promoted positive emotional experiences
The final theme related to the emotional changes experienced through participating in BISEP, described by all the group members. For many, the program was associated with enhanced positive emotions, fewer experiences of negative emotions, and increased ability to “manage” emotional difficulties in daily life.
Two-sub themes were identified. The first, emotion regulation strategies, related to the use of strategies to manage emotional difficulties in daily life. Of the ER strategies included in BISEP, thinking of “positive things” was the most commonly reported helpful strategy, which was related to the ‘Three Good Things’ activity. Making a note of good things each day got “people to talk and focus on the good,” and “engaged positive thought.” The important thing, however, was the positive effect of doing this activity on mood, which appeared to continue following the program. For many, doing this helped them to “notice positive things” after BISEP, and encouraged “positive thinking.”
Twelve participants discussed the benefits of using ER strategies based on the Process Model, conceptualized in BISEP as tools to use ‘Before’, ‘During’, and ‘After’. The data indicated that the in the moment (‘During’) strategies were especially useful for many participants. This mainly consisted of distracting activities such as “going for a walk” to improve low mood, or “moving away” from overwhelming or anxiety-inducing situations. The ‘Before’ strategies seemed particularly salient for the few people who discussed them. By thinking things through beforehand, they could “foresee [their] situation and predict where it’s going.” Finally, a small number of participants described the benefits of the ‘After’ strategy of reappraisal for “turning a negative into a positive.” The ‘stop’ element was especially important for five participants.
As described by Rhian, “And with the S.O.S […] I would practice it. I say things to my mum that makes for a bad atmosphere, because I’ve got no filter. But now I try to stop and think. And that has made me think, if you do just stop and think, I can stop that bad atmosphere. And it’s stupid that it has taken me until now.”
For Robin, the ‘stop’ allowed him to “buy some time” which helped him deal with difficult situations.
The second sub-theme related to the emotional experiences that were related to the generic elements, and the philosophical approach, of BISEP. Participating in the program appeared to have beneficial effects on attendees’ emotional well-being, with one reporting “feeling better” after BISEP. For some individuals, they felt “less aggressive” after the group, or “less critical” of themselves and their progress.
As described by Iolo:
Ermm … It’s helped me to be more aware of my emotions. And it’s helped me try and work through those emotions […] Ermm… things like even feeling low or whatever. I’ve got the dog. I do something positive. Think of something positive, focus on the positive. If I’m feeling low, the group helped me to feel the positive, getting up in the morning and being alive. It’s so important. The group helped you to look at that, remember that, focus on that. […] So, when bad emotions come along hopefully the positive will pull you out. So, yeah in that way yeah, definitely. […] But, the shopping one is probably most important […] Since I took the advice on shopping: Go to the shop, at a quieter time, go to a quieter shop. That was the -… things went a lot smoother for me in the shop. I still had my panic moments where I’ve forgotten and… Once I panic, I forget and I just want to get out […] the important thing is I have reduced my chances of having problems by doing things, and adapting when I do things, how I do things. I actually did not do that one week. And I went to a shop at a busy time…Thinking I can do this now, I can do it. And I went in and I was totally overwhelmed […] And it was absolutely awful, Because I did not follow these things. So, my problems have not changed really. But my ability to manage the problems has changed.”
In sum, through the implementation of ER tools, developed in the BISEP group, a transfer could be seen into activities of daily living. For these participants, managing emotional reactions to post-injury challenges was key, and opened up an availability in survivors to compromise for the benefit of managing these emotional reactions.
Discussion
To our knowledge, the present study is the first to directly explore participants’ experiences of and within a group program which specifically addresses ER (among other topics common in group psycho-education programs), and the core components that were valued by attendees. Using a descriptive phenomenology philosophy, the present study focused on lived experience and participants’ worldview within the group rehabilitation space. The discussion presents the patterns of meaning derived from individual’s experiences.
Long-term difficulties need long-term support
Participants’ experiences emphasize the chronic nature of ABI in the long-term, consistent with previous literature (Hoofien et al., 2001; Dikmen et al., 2003; Colantonio et al., 2004; Salas et al., 2018; Dams-O'Connor et al., 2023). The findings also suggest that participants frequently disengage, or take a “step back,” from leisure pursuits and socializing, as a means of coping with the long-term difficulties (Fleming et al., 2011; Kersey et al., 2019, for a review), and may indicate a potential mechanism to address social isolation in rehabilitation. A recurrent element in the interviews was that survivors were at various stages of adjusting to changes in identity, or are on a different part of the ‘journey’ of acceptance, similar to themes identified by Couchman et al. (2014), and in a meta-synthesis by Villa et al. (2021). Interestingly, emphasizing the metaphor of a ‘journey’ might, in itself, be a tool which has important clinical implications (Huang and Aaker, 2019).
The persistent nature of participants’ difficulties, sometimes decades after the injury, highlight the important role of long-term community rehabilitation services (Wade, 2003; Coetzer et al., 2018; Norman et al., 2023), and group programs, in assisting patients with the adjustment process (Lundqvist et al., 2010; Lexell et al., 2013). The findings also contribute to the idea that addressing how survivors experience their ‘new self’ in rehabilitation might generate more positive adjustment (Gracey et al., 2008; Carroll and Coetzer, 2011). Together, this theme highlights the need for continued support, for example in the form of group programs, in the longer term.
Experiences of valued elements
Participants experienced socializing with, and relating to, other survivors appeared to be a powerful, therapeutic experience (c.f. Salas et al., 2018). Being able to “share,” and relate to the experiences of people “in the same boat,” was something which connected the group members, and facilitated a sense of unity or cohesion, similar to previous studies (Lexell et al., 2013; Couchman et al., 2014; Salas et al., 2018). Existing holistic approaches traditionally include some emphasis on social interaction within rehabilitation (Gracey et al., 2010). Douglas et al. (2015) describe the need to emphasize social and relational approaches in neurorehabilitation, and promoting a sense of meaning and belonging after ABI. Participants’ interviews extend this idea by highlighting the potential benefit of developing a social milieu in promoting positive emotional experiences and a sense of connectedness (i.e., the feeling that they are “not alone”).
Participants experienced BISEP as a platform for learning to take place, consistent with previous literature (Lexell et al., 2013; Couchman et al., 2014). Attendees valued learning tools, or “strategies,” that could be used in their daily lives to manage various difficulties (e.g., memory, fatigue). This contributes to a well-established literature on compensation strategies (Wilson, 2000; Tsaousides and Gordon, 2009). Participants especially appreciated the strategies that they “picked up off different clients,” and the data suggests that other survivors can be a source of help similar to that provided by professionals.
Some participants experienced the consequences of ABI as barriers to learning in the program (e.g., “sometimes things did not sink in”). Rehabilitation has many ways to address difficulties in learning and memory following brain injury (Wilson et al., 1994; Evans et al., 2000; Kessels and Haan, 2003; Fish and Brentnall, 2016). The data from the present study especially suggest that experiential learning is provides a more positive learning experience, and that providing survivors with handouts or booklets is particularly valued, and allows learning to continue following program completion.
The final perceived important elements were the ER strategies, and positive philosophy of BISEP. The participants especially valued the ‘Three Good Things’ activity to manage low mood, and promote positive thinking. Previous literature has also indicated how making a note of ‘good things’ can help promote positive feelings (Andrewes et al., 2014; Karagiorgou et al., 2018), further highlighting the relevance of this activity in neurorehabilitation (Evans, 2011). Further, due to its simplicity it may be an especially beneficial tool for people with ABI.
In the context of the strategies based upon the Process Model (Gross, 2013), the ‘During’ strategies were frequently experienced as effective for managing emotional difficulties in daily life. These ‘in the moment’ tools are based upon ‘situation modification’ (modifying the external environment to manage emotional responses) and ‘attentional deployment’ (changing the internal environment to more favorable thoughts). Participants’ experienced these as useful for improving low mood, and managing anxiety or overwhelming situations. This is consistent with evidence in neurologically healthy participants, indicating that attentional deployment may be useful for those low in cognitive resources (Lohani and Isaacowitz, 2014; Sheppes et al., 2014).
Additionally, some participants described the relevance of the ‘Before’ strategies: the forward-thinking approach of ‘situation selection’. Through “analysing” and predicting the potential difficulties of various situations, participants reported being better able to manage their difficulties in daily life. This provides further evidence that situation selection may be particularly effective for people who struggle to regulate their emotions (Webb et al., 2018).
The ‘After’ strategies (reappraisal in the Process Model), was only explicitly described by three participants. However, there is some overlap between thinking of the positives generally with ‘Three Good Things’, and using positive things to change the meaning of a situation (as in reappraisal). However, reappraisal is a cognitively effortful strategy; which research suggests is difficult for patients with ABI (Salas Riquelme et al., 2014; Rowlands et al., 2019). It is possible that this strategy remains difficult to use, even after training, and that ‘Three Good Things’ may be a simpler approach to promote positive thinking.
Participants reported positive emotional experiences and changes, that were related to generic elements of the program. This emphasizes the role that a group program, with a positive philosophical approach, can have in improving emotional well-being following brain injury. The present study’s findings provide further support that group rehabilitation programs can be a promising vehicle to promote adaptive ER and emotional well-being (Tornås et al., 2016; Tsaousides et al., 2017).
Acceptability of BISEP and the role of Group Interventions
BISEP was perceived as a valuable, beneficial, and a positive experience, similar to previous studies of group programs (Lexell et al., 2013; Couchman et al., 2014). The narrative especially suggests that enjoying the sessions played a central role in engagement, and participants’ motivation to attend the program until it was completed (“I’m sad to see it end”). The positive experience of participating in BISEP allowed participants to “benefit” in terms of their recovery (similar to Lexell et al., 2013; Couchman et al., 2014). A final point which deserves attention is the facilitators’ role in fostering the positive rehabilitation experience. This contributes to well-established qualitative evidence, which points to the therapeutic relationship as a potential mechanism to promote rehabilitation engagement (Bright et al., 2015; Lawton et al., 2016), and demonstrates that it is not only what clinicians do that is important, but how they do it (Kayes and McPherson, 2012; Bright et al., 2015; Bishop et al., 2019).
Survivors described the relevance of group programs, such as BISEP, for community rehabilitation services. The lack of information provided at the organizational level in acute services resulted in feelings of disconnect after returning home, something which has been reported elsewhere (Piccenna et al., 2016; Abrahamson et al., 2017; Graff et al., 2018). The limited level of information provided to participants highlights how community services broadly, and group programs specifically, can help with progression through the rehabilitation pathway.
Limitations
The results of the present study are promising. A potential limitation, however, is that the interviewer (LR) was also the person who facilitated the program. The impact of this was minimized by emphasizing the potential benefits of constructive criticism to improving the program for future, and taking time at the beginning of the session to reassure and create a sense of safety and receptiveness to all feedback. The researcher also used bracketing to aim to reduce any preconceived ideas or biases, and the second coder was not part of the BISEP program. Further mitigation was sought through including author SB to scrutinize the themes, and making use of clinical and academic supervision to support the reflectivity and bracketing process.
Future research would benefit from having an interviewer who was not the facilitator of the program and not involved in the service or program development, and to conduct interviews at an additional time point to track changes over time. It would also be interesting to interview family members or care-givers, to obtain an additional perspective. These aspects were beyond the scope of the current research project. An additional limitation is that the individuals who completed BISEP chose to enroll on a group program. The results would then be less generalizable to all survivors of ABI. Future research may benefit from unpacking people’s motivations for group rehabilitation and how this relates to their experience.
Clinical and theoretical implications
Participant experiences suggest several important clinical implications. (1) Build long term: The findings provide clear support of the role of ‘slow stream’ holistic rehabilitation services in the long term, to help survivors with issues related to adjustment, acceptance, and identity. Services may benefit from ensuring a longer term pathway of care, and the literature may benefit from further research into models of rehabilitation and its barriers and enablers, in the chronic phase (2) A social space: The data highlight the importance of group programs in forming a “safe” and relational space, where participants can experience the therapeutic benefits of socializing with similar others. Additionally, by placing the focus of rehabilitation programs in the relational space between people, it provides a platform to learn from their peers, in addition to the formal content. There has been a growing literature on social connection and its relevance for rehabilitation. Continued research, in particular through a lived experience lens, would benefit the field. (3) Provide strategies: Suggesting practical tools and strategies may be a promising approach in rehabilitation programs. This is not a new idea in neurorehabilitation, but further research may be warranted to explore the perceived and objective efficacy of various tools. (4) Focus on positives: The present study suggests that BISEP (and other group programs) are promising vehicles for promoting positive emotional experiences, and adaptive ER skills. Participants especially noted the relevance of the ‘Three Good Things’ activity, in addition to the underlying principle of ‘promoting a positive outlook’ across all sessions.
Conclusion
The majority of rehabilitation research has focused on post-acute services and individualized treatment (e.g., Cicerone et al., 2011). The present findings suggest that group programs are not simply an expedient tool to save money or clinician time. Group interventions, such as BISEP, have perceived benefits through the powerful therapeutic effect of shared experience. Patients identified therapeutic gains which the clinician themselves could not provide, but only facilitate. Finally, traditional rehabilitation interventions have tended to focus on cognitive impairment. The emphasis on emotion regulation and optimism had benefits which are arguably more important in patients’ lives. In sum, rehabilitation services may benefit from placing an emphasis on group programs, continued treatment in the chronic phase, and simple, practical tools that are delivered optimistically.
Data availability statement
The datasets presented in this article are not readily available, because service and patient consent was not given to sharing full transcripts. Requests to access data should be directed to bHJvd2xhbmRzQGFyZGVuLmFjLnVr.
Ethics statement
The present study, involving humans, was approved by Bangor University Ethics Committee and NHS Betsi Cadwaladr University Health Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LR: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. CS: Formal analysis, Methodology, Writing – review & editing. RC: Conceptualization, Project administration, Supervision, Writing – review & editing. SB: Formal analysis, Writing – review & editing. OT: Conceptualization, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by a PhD studentship for the first author (LR) – KESS 2 Scholarship through the Welsh Government via EU Social Fund.
Acknowledgments
The authors would like to thank all participants for generously offering their time and sharing their experiences.
Conflict of interest
RC was employed by the North Wales Brain Injury Service, Betsi Cadwaladr University Health Board, Colwyn Bay, UK at the time of data collection.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^Response modulation was not included in BISEP, as this strategy involves the regulation of emotional expressions not experience per se. There is also evidence that this strategy can be used maladaptively (Gross and John, 2003), and describing when/how to use it in an adaptive way might be confusing for patients.
References
Aboulafia-Brakha, T., Greber Buschbeck, C., Rochat, L., and Annoni, J. M. (2013). Feasibility and initial efficacy of a cognitive-behavioural group programme for managing anger and aggressiveness after traumatic brain injury. Neuropsychol. Rehabil. 23, 216–233. doi: 10.1080/09602011.2012.747443
Abrahamson, V., Jensen, J., Springett, K., and Sakel, M. (2017). Experiences of patients with traumatic brain injury and their carers during transition from in-patient rehabilitation to the community: a qualitative study. Disabil. Rehabil. 39, 1683–1694. doi: 10.1080/09638288.2016.1211755
Andrewes, H. E., Walker, V., and O’Neill, B. (2014). Exploring the use of positive psychology interventions in brain injury survivors with challenging behaviour. Brain Inj. 28, 965–971. doi: 10.3109/02699052.2014.888764
Anson, K., and Ponsford, J. (2006). Evaluation of a coping skills group following traumatic brain injury. Brain Inj. 20, 167–178. doi: 10.1080/02699050500442956
Backhaus, S. L., Ibarra, S. L., Klyce, D., Trexler, L. E., and Malec, J. F. (2010). Brain injury coping skills group: a preventative intervention for patients with brain injury and their caregivers. Arch. Phys. Med. Rehabil. 91, 840–848. doi: 10.1016/j.apmr.2010.03.015
Balchin, R., Coetzer, R., Salas, C., and Webster, J. (2017). Addressing brain injury in under-resourced settings: a practical guide to community-centred approaches. London: Psychology Press.
Bechara, A. (2004). Disturbances of emotion regulation after focal brain lesions. Int. Rev. Neurobiol. 62, 159–193. doi: 10.1016/S0074-7742(04)62006-X
Beer, J. S., and Lombardo, M. V. (2007). “Insights into emotion regulation from neuropsychology” in Handbook of emotion regulation. ed. J. J. Gross (New York: The Guilford Press), 69–86.
Ben-Yishay, Y. (2000). “Postacute neuropsychological rehabilitation” in International handbook of neuropsychological rehabilitation (Boston, MA: Springer), 127–135.
Ben-Yishay, Y., and Daniels-Zide, E. (2000). Examined lives: outcomes after holistic rehabilitation. Rehabil. Psychol. 45, 112–129. doi: 10.1037/0090-5550.45.2.112
Ben-Yishay, Y., and Diller, L. (2011). Handbook of holistic neuropsychological rehabilitation: Outpatient rehabilitation of traumatic brain injury. New York: Oxford University Press.
Bishop, M., Kayes, N., and McPherson, K. (2019). Understanding the therapeutic alliance in stroke rehabilitation. Disabil. Rehabil. 43, 1074–1083. doi: 10.1080/09638288.2019.1651909
Bowen, C., Yeates, G., and Palmer, S. (2010). A relational approach to rehabilitation: Thinking about relationships after brain injury. London: Karnac books.
Bradbury, C. L., Christensen, B. K., Lau, M. A., Ruttan, L. A., Arundine, A. L., and Green, R. E. (2008). The efficacy of cognitive behavior therapy in the treatment of emotional distress after acquired brain injury. Arch. Phys. Med. Rehabil. 89, S61–S68. doi: 10.1016/j.apmr.2008.08.210
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101. doi: 10.1191/1478088706qp063oa
Bright, F. A., Kayes, N. M., Worrall, L., and McPherson, K. M. (2015). A conceptual review of engagement in healthcare and rehabilitation. Disabil. Rehabil. 37, 643–654. doi: 10.3109/09638288.2014.933899
Cantor, J., Ashman, T., Dams-O'Connor, K., Dijkers, M. P., Gordon, W., Spielman, L., et al. (2014). Evaluation of the short-term executive plus intervention for executive dysfunction after traumatic brain injury: a randomized controlled trial with minimization. Arch. Phys. Med. Rehabil. 95, 1–9.e3. doi: 10.1016/j.apmr.2013.08.005
Carlsson, E., Paterson, B. L., Scott-Findlay, S., Ehnfors, M., and Ehrenberg, A. (2007). Methodological issues in interviews involving people with communication impairments after acquired brain damage. Qual. Health Res. 17, 1361–1371.
Carroll, E., and Coetzer, R. (2011). Identity, grief and self-awareness after traumatic brain injury. Neuropsychol. Rehabil. 21, 289–305. doi: 10.1080/09602011.2011.555972
Christensen, M., Welch, A., and Barr, J. (2017). Husserlian descriptive phenomenology: a review of intentionality, reduction and the natural attitude. J. Nurs. Educ. Pract. 7, 113–118. doi: 10.5430/jnep.v7n8p113
Cicerone, K. D., Langenbahn, D. M., Braden, C., Malec, J. F., Kalmar, K., Fraas, M., et al. (2011). Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch. Phys. Med. Rehabil. 92, 519–530. doi: 10.1016/j.apmr.2010.11.015
Cicerone, K. D., Mott, T., Azulay, J., Sharlow-Galella, M. A., Ellmo, W. J., Paradise, S., et al. (2008). A randomized controlled trial of holistic neuropsychologic rehabilitation after traumatic brain injury. Arch. Phys. Med. Rehabil. 89, 2239–2249. doi: 10.1016/j.apmr.2008.06.017
Coetzer, B. R., Vaughan, F. L., Roberts, C. B., and Rafal, R. (2003). The development of a holistic, community based neurorehabilitation service in a rural area. J. Cogn. Rehabil. 21, 4–15.
Coetzer, R. (2008). Holistic neuro-rehabilitation in the community: is identity a key issue? Neuropsychol. Rehabil. 18, 766–783. doi: 10.1080/09602010701860266
Coetzer, R., Roberts, C., Turnbull, O. H., and Vaughan, F. L. (2018). Neuropsychoanalytically informed psychotherapy approaches to rehabilitation: the North Wales brain injury service–Bangor University experience 1998–2018. Neuropsychoanalysis 20, 3–13. doi: 10.1080/15294145.2018.1478747
Colantonio, A., Ratcliff, G., Chase, S., Kelsey, S., Escobar, M., and Vernich, L. (2004). Long term outcomes after moderate to severe traumatic brain injury. Disabil. Rehabil. 26, 253–261. doi: 10.1080/09638280310001639722
Couchman, G., McMahon, G., Kelly, A., and Ponsford, J. (2014). A new kind of normal: qualitative accounts of multifamily group therapy for acquired brain injury. Neuropsychol. Rehabil. 24, 809–832. doi: 10.1080/09602011.2014.912957
Dams-O'Connor, K., Juengst, S. B., Bogner, J., Chiaravalloti, N. D., Corrigan, J. D., Giacino, J. T., et al. (2023). Traumatic brain injury as a chronic disease: insights from the United States traumatic brain injury model systems research program. The Lancet Neurol. 22, 517–528. doi: 10.1016/S1474-4422(23)00065-0
Dikmen, S. S., Machamer, J. E., Powell, J. M., and Temkin, N. R. (2003). Outcome 3 to 5 years after moderate to severe traumatic brain injury. Arch. Phys. Med. Rehabil. 84, 1449–1457. doi: 10.1016/S0003-9993(03)00287-9
Douglas, J., Drummond, M., Knox, L., and Mealings, M. (2015). “Rethinking social-relational perspectives in rehabilitation: traumatic brain injury as a case study” in Rethinking rehabilitation theory and practice. eds. K. McPherson, B. Gibson, and A. Leplege (Boca Raton: CRC Press), 137–162.
Evans, J. J. (2011). Positive psychology and brain injury rehabilitation. Brain Impairment 12, 117–127. doi: 10.1375/brim.12.2.117
Evans, J. J., Wilson, B. A., Schuri, U., Andrade, J., Baddeley, A., Bruna, O., et al. (2000). A comparison of “errorless” and “trial-and-error” learning methods for teaching individuals with acquired memory deficits. Neuropsychol. Rehabil. 10, 67–101. doi: 10.1080/096020100389309
Fish, J., and Brentnall, S. (2016). “Memory” in The brain injury rehabilitation workbook. eds. R. Winson, B. A. Wilson, and A. Bateman (New York, NY: Guilford Press), 68–85.
Fleming, J., Braithwaite, H., Gustafsson, L., Griffin, J., Collier, A. M., and Fletcher, S. (2011). Participation in leisure activities during brain injury rehabilitation. Brain Inj. 25, 806–818. doi: 10.3109/02699052.2011.585508
Frost, R. B., Farrer, T. J., Primosch, M., and Hedges, D. W. (2013). Prevalence of traumatic brain injury in the general adult population: a meta-analysis. Neuroepidemiology 40, 154–159. doi: 10.1159/000343275
Gearing, R. E. (2004). Bracketing in research: a typology. Qual. Health Res. 14, 1429–1452. doi: 10.1177/1049732304270394
Gill, M. J. (2020). “Phenomenological approaches to research” in Qualitative analysis: Eight approaches. eds. N. Mik-Meyer and M. Jarvinen (London: Sage), 73–94.
Giorgi, A., and Giorgi, B. (2003). “The descriptive phenomenological psychological method” in Qualitative research in psychology: Expanding perspectives in methodology and design. eds. P. Camic, J. Rhodes, and L. Yardley (Washington, DC: American Philosophical Association), 243–273.
Gracey, F., Palmer, S., Rous, B., Psaila, K., Shaw, K., O'Dell, J., et al. (2008). “Feeling part of things”: personal construction of self after brain injury. Neuropsychol. Rehabil. 18, 627–650. doi: 10.1080/09602010802041238
Gracey, F., Yeates, G., Palmer, S., and Psaila, K. (2010). “The psychological support group” in Neuropsychological rehabilitation. Theory, models, therapy and outcome. eds. B. Wilson, F. Gracey, J. Evans, and A. Bateman (Cambridge: Cambridge University Press), 123–136.
Graff, H. J., Christensen, U., Poulsen, I., and Egerod, I. (2018). Patient perspectives on navigating the field of traumatic brain injury rehabilitation: a qualitative thematic analysis. Disabil. Rehabil. 40, 926–934. doi: 10.1080/09638288.2017.1280542
Greenfield, B., and Jensen, G. M. (2012). Phenomenology: a powerful tool for patient-centered rehabilitation. Phys. Ther. Rev. 17, 417–424. doi: 10.1179/1743288X12Y.0000000046
Gross, J. J. (2015). Emotion regulation: Current status and future prospects. Psychol. Inq. 26, 1–26
Gross, J. J., and John, O. P. (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 85:348.
Gross, J. J., and Thompson, R. A. (2007). “Emotion regulation: conceptual foundations” in Handbook of emotion regulation. ed. J. J. Gross (New York: Guilford Press), 3–24.
Guest, G., Bunce, A., and Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods 18, 59–82. doi: 10.1177/1525822X05279903
Hoofien, D., Gilboa, A., Vakil, E., and Donovick, P. J. (2001). Traumatic brain injury (TBI) 10? 20 years later: a comprehensive outcome study of psychiatric symptomatology, cognitive abilities and psychosocial functioning. Brain Inj. 15, 189–209. doi: 10.1080/026990501300005659
Huang, S. C., and Aaker, J. (2019). It’s the journey, not the destination: how metaphor drives growth after goal attainment. J. Pers. Soc. Psychol. 117, 697–720. doi: 10.1037/pspa0000164
Karagiorgou, O., Evans, J. J., and Cullen, B. (2018). Post-traumatic growth in adult survivors of brain injury: a qualitative study of participants completing a pilot trial of brief positive psychotherapy. Disabil. Rehabil. 40, 655–659. doi: 10.1080/09638288.2016.1274337
Kayes, N. M., and McPherson, K. M. (2012). Human technologies in rehabilitation: ‘who’ and ‘how’ we are with our clients. Disabil. Rehabil. 34, 1907–1911. doi: 10.3109/09638288.2012.670044
Kersey, J., Terhorst, L., Wu, C. Y., and Skidmore, E. (2019). A scoping review of predictors of community integration following traumatic brain injury: a search for meaningful associations. J. Head Trauma Rehabil. 34, E32–E41. doi: 10.1097/HTR.0000000000000442
Kessels, R. P., and Haan, E. H. (2003). Implicit learning in memory rehabilitation: a meta-analysis on errorless learning and vanishing cues methods. J. Clin. Exp. Neuropsychol. 25, 805–814. doi: 10.1076/jcen.25.6.805.16474
Lawton, M., Haddock, G., Conroy, P., and Sage, K. (2016). Therapeutic alliances in stroke rehabilitation: a meta-ethnography. Arch. Phys. Med. Rehabil. 97, 1979–1993. doi: 10.1016/j.apmr.2016.03.031
Levack, W. M., Kayes, N. M., and Fadyl, J. K. (2010). Experience of recovery and outcome following traumatic brain injury: a metasynthesis of qualitative research. Disabil. Rehabil. 32, 986–999. doi: 10.3109/09638281003775394
Lexell, E. M., Alkhed, A. K., and Olsson, K. (2013). The group rehabilitation helped me adjust to a new life: experiences shared by persons with an acquired brain injury. Brain Inj. 27, 529–537. doi: 10.3109/02699052.2013.765598
Lohani, M., and Isaacowitz, D. M. (2014). Age differences in managing response to sadness elicitors using attentional deployment, positive reappraisal and suppression. Cognit. Emot. 28, 678–697. doi: 10.1080/02699931.2013.853648
Lo, T. L. T., Lee, J. L. C., and Ho, R. T. H. (2023). Recovery beyond functional restoration: a systematic review of qualitative studies of the embodied experiences of people who have survived a stroke. BMJ Open 13:e066597. doi: 10.1136/bmjopen-2022-066597
Lundqvist, A., Linnros, H., Orlenius, H., and Samuelsson, K. (2010). Improved self-awareness and coping strategies for patients with acquired brain injury—a group therapy programme. Brain Inj. 24, 823–832. doi: 10.3109/02699051003724986
Maclean, N., Pound, P., Wolfe, C., and Rudd, A. (2000). Qualitative analysis of stroke patients' motivation for rehabilitation. BMJ 321, 1051–1054. doi: 10.1136/bmj.321.7268.1051
Maguire, M., and Delahunt, B. (2017). Doing a thematic analysis: a practical, step-by-step guide for learning and teaching scholars. AISHE-J 9.
Malec, J. F. (2001). Impact of comprehensive day treatment on societal participation for persons with acquired brain injury. Arch. Phys. Med. Rehabil. 82, 885–895. doi: 10.1053/apmr.2001.23895
Martin, R., Levack, W. M., and Sinnott, K. A. (2015). Life goals and social identity in people with severe acquired brain injury: an interpretative phenomenological analysis. Disabil. Rehabil. 37, 1234–1241. doi: 10.3109/09638288.2014.961653
Martínez-Pernía, D. (2020). Experiential neurorehabilitation: A neurological therapy based on the enactive paradigm. Front. Psychol. 11:505199.
Martínez-Pernía, D., Huepe, D., Huepe-Artigas, D., Correia, R., García, S., and Beitia, M. (2016). Enactive approach and dual-tasks for the treatment of severe behavioral and cognitive impairment in a person with acquired brain injury: a case study. Front. Psychol. 7:220100. doi: 10.3389/fpsyg.2016.01712
McDonald, S. (2017). Emotions are rising: the growing field of affect neuropsychology. J. Int. Neuropsychol. Soc. 23, 719–731. doi: 10.1017/S1355617717000844
Norman, A., Curro, V., Holloway, M., Percuklievska, N., and Ferrario, H. (2023). Experiences of individuals with acquired brain injury and their families interacting with community services: a systematic scoping review. Disabil. Rehabil. 45, 739–751. doi: 10.1080/09638288.2022.2043465
Nowell, L. S., Norris, J. M., White, D. E., and Moules, N. J. (2017). Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods 16:160940691773384. doi: 10.1177/1609406917733847
O’Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A., and Cook, D. A. (2014). Standards for reporting qualitative research: a synthesis of recommendations. Acad. Med. 89, 1245–1251. doi: 10.1097/ACM.0000000000000388
Obonsawin, M. C., Jefferis, S., Lowe, R., Crawford, J. R., Fernandez, J., Holland, L., et al. (2007). A model of personality change after traumatic brain injury and the development of the brain injury personality scales. J. Neurol. Neurosurg. Psychiatry 78, 1239–1247. doi: 10.1136/jnnp.2004.052654
Ownsworth, T., and Fleming, J. (2005). The relative importance of metacognitive skills, emotional status, and executive function in psychosocial adjustment following acquired brain injury. J. Head Trauma Rehabil. 20, 315–332. doi: 10.1097/00001199-200507000-00004
Panday, J., Velikonja, D., Moll, S. E., and Harris, J. E. (2022). Experiences of inpatient rehabilitation from the perspective of persons with acquired brain injury. Disabil. Rehabil. 44, 5539–5548. doi: 10.1080/09638288.2021.1938706
Paolucci, S., Di, A. V., Massicci, R., Traballesi, M., Bureca, I., Matano, A., et al. (2012). Impact of participation on rehabilitation results: a multivariate study. Eur. J. Phys. Rehabil. Med. 48, 455–466
Paterson, B., and Scott-Findlay, S. (2002). Critical issues in interviewing people with traumatic brain injury. Qual. Health Res. 12, 399–409. doi: 10.1177/104973202129119973
Patterson, F., Fleming, J., and Doig, E. (2016). Group-based delivery of interventions in traumatic brain injury rehabilitation: a scoping review. Disabil. Rehabil. 38, 1961–1986. doi: 10.3109/09638288.2015.1111436
Piccenna, L., Lannin, N. A., Gruen, R., Pattuwage, L., and Bragge, P. (2016). The experience of discharge for patients with an acquired brain injury from the inpatient to the community setting: a qualitative review. Brain Inj. 30, 241–251. doi: 10.3109/02699052.2015.1113569
Powell, T. J. (2013). The brain injury workbook: Exercises for cognitive rehabilitation. 2nd Edn. London: Speechmark Pub. Limited.
Psaila, K., and Gracey, F. (2009). “The mood management group” in In neuropsychological rehabilitation: Theory, models, therapy and outcome. eds. B. A. Wilson, F. Gracey, J. J. Evans, and A. Bateman (Cambridge, UK: Cambridge University Press), 112–123.
Rowlands, L., Coetzer, R., and Turnbull, O. H. (2019). Good things better? Reappraisal and discrete emotions in acquired brain injury. Neuropsychol. Rehabil. 30, 1947–1975. doi: 10.1080/09602011.2019.1620788
Salas, C. E., Casassus, M., Rowlands, L., Pimm, S., and Flanagan, D. A. (2018). “Relating through sameness”: a qualitative study of friendship and social isolation in chronic traumatic brain injury. Neuropsychol. Rehabil. 28, 1161–1178. doi: 10.1080/09602011.2016.1247730
Salas Riquelme, C. E., Turnbull, O. H., and Gross, J. J. (2014). Reappraisal generation after acquired brain damage: the role of laterality and cognitive control. Front. Psychol. 5:242. doi: 10.3389/fpsyg.2014.00242
Schiavio, A., and Altenmüller, E. (2015). Exploring music-based rehabilitation for parkinsonism through embodied cognitive science. Front. Neurol. 6:162903. doi: 10.3389/fneur.2015.00217
Seligman, M. E. P., Steen, T. A., Park, N., and Peterson, C. (2005). Positive psychology progress: Empirical validation of interventions. Am. Psychol. 60, 410–421.
Sheppes, G., Brady, W. J., and Samson, A. C. (2014). In (visual) search for a new distraction: the efficiency of a novel attentional deployment versus semantic meaning regulation strategies. Front. Psychol. 5:346. doi: 10.3389/fpsyg.2014.00346
Shields, C., Ownsworth, T., O'Donovan, A., and Fleming, J. (2016). A transdiagnostic investigation of emotional distress after traumatic brain injury. Neuropsychol. Rehabil. 26, 410–445. doi: 10.1080/09602011.2015.1037772
Shorey, S., and Ng, E. D. (2022). Examining characteristics of descriptive phenomenological nursing studies: a scoping review. J. Adv. Nurs. 78, 1968–1979. doi: 10.1111/jan.15244
Sinfield, G., Goldspink, S., and Wilson, C. (2023). Waiting in the wings: the enactment of a descriptive phenomenology study. Int J Qual Methods 22:16094069231207012. doi: 10.1177/16094069231207012
Sundler, A. J., Lindberg, E., Nilsson, C., and Palmér, L. (2019). Qualitative thematic analysis based on descriptive phenomenology. Nurs. Open 6, 733–739. doi: 10.1002/nop2.275
Tornås, S., Løvstad, M., Solbakk, A. K., Schanke, A. K., and Stubberud, J. (2016). Goal management training combined with external cuing as a means to improve emotional regulation, psychological functioning, and quality of life in patients with acquired brain injury: a randomized controlled trial. Arch. Phys. Med. Rehabil. 97, 1841–1852.e3. doi: 10.1016/j.apmr.2016.06.014
Trexler, L. E. (2000). “Empirical support for neuropsychological rehabilitation” in International handbook of neuropsychological rehabilitation. Critical issues in neuropsychology. eds. A. L. Christensen and B. P. Uzzell (Boston, MA: Springer).
Tsaousides, T., and Gordon, W. A. (2009). Cognitive rehabilitation following traumatic brain injury: assessment to treatment. Mount Sinai J. Med. 76, 173–181. doi: 10.1002/msj.20099
Tsaousides, T., Spielman, L., Kajankova, M., Guetta, G., Gordon, W., and Dams-O'Connor, K. (2017). Improving emotion regulation following web-based group intervention for individuals with traumatic brain injury. J. Head Trauma Rehabil. 32, 354–365. doi: 10.1097/HTR.0000000000000345
Turner-Stokes, L., Pick, A., Nair, A., Disler, P. B., and Wade, D. T. (2015). Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database Syst. Rev. 2015:CD004170. doi: 10.1002/14651858.CD004170.pub3
Tyerman, A., and Hucker, R. (2016). Community brain injury rehabilitation services benchmarking exercise. Buckinghamshire Healthcare NHS Trust: United Kingdom.
Van den Broek, M. D., and Dayus, B. (2002). Head injury education: A group therapy manual. Oxon: Speechmark Pub. Limited.
Villa, D., Causer, H., and Riley, G. A. (2021). Experiences that challenge self-identity following traumatic brain injury: a meta-synthesis of qualitative research. Disabil. Rehabil. 43, 3298–3314. doi: 10.1080/09638288.2020.1743773
Wade, D. (2003). Community rehabilitation, or rehabilitation in the community? Disabil. Rehabil. 25, 875–881. doi: 10.1080/0963828031000122267
Wain, H. R., Kneebone, I. I., and Billings, J. (2008). Patient experience of neurologic rehabilitation: a qualitative investigation. Arch. Phys. Med. Rehabil. 89, 1366–1371. doi: 10.1016/j.apmr.2007.11.050
Webb, T. L., Lindquist, K. A., Jones, K., Avishai, A., and Sheeran, P. (2018). Situation selection is a particularly effective emotion regulation strategy for people who need help regulating their emotions. Cognit. Emot. 32, 231–248. doi: 10.1080/02699931.2017.1295922
Werner, K., and Gross, J. J. (2010). “Emotion regulation and psychopathology: a conceptual framework” in Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. eds. A. M. Kring and D. M. Sloan (New York, NY: The Guilford Press), 13–37.
Williams, M. W., Rapport, L. J., Hanks, R. A., and Parker, H. A. (2019). Engagement in rehabilitation therapy and functional outcomes among individuals with acquired brain injuries. Disabil. Rehabil. 43, 33–41. doi: 10.1080/09638288.2019.1613682
Willis, D. G., Sullivan-Bolyai, S., Knafl, K., and Cohen, M. Z. (2016). Distinguishing features and similarities between descriptive phenomenological and qualitative description research. West. J. Nurs. Res. 38, 1185–1204. doi: 10.1177/0193945916645499
Wilson, B. A. (2000). Compensating for cognitive deficits following brain injury. Neuropsychol. Rev. 10, 233–243. doi: 10.1023/A:1026464827874
Wilson, B. A., Baddeley, A., Evans, J., and Shiel, A. (1994). Errorless learning in the rehabilitation of memory impaired people. Neuropsychol. Rehabil. 4, 307–326. doi: 10.1080/09602019408401463
Wilson, B. A., and Gracey, F. (2009). “Background and theory. Towards a comprehensive model of neuropsychological rehabilitation” in Neuropsychological rehabilitation: Theory, models, therapy and outcome. eds. B. A. Wilson, F. Gracey, J. J. Evans, and A. Bateman (Cambridge, UK: Cambridge University Press), 1–22.
Wilson, B. A. (2017). “General introduction” in The brain injury rehabilitation workbook. eds. W. Winson, B. A. Wilson, and A. Bateman (New York, NY: Guilford Press), 1–15.
Wilson, B., Gracey, F., Evans, J., and Bateman, A. (2009). Neuropsychological rehabilitation: Theory, models, therapy and outcome. New York, NY: Cambridge University Press.
Winson, W., Wilson, B. A., and Bateman, A. (2017). The brain injury rehabilitation workbook. New York, NY: Guilford Press.
Appendix A
Semi-structured interview protocol
The interviewee used the following questions and additional memory prompts to explore group members’ experience of BISEP. Scaffolding was used when necessary to assist patients in developing a narrative and expressing their ideas.
• What are your thoughts on BISEP?
• Content – Session by session reminder prompts
• ‘Three Good Things’ activity
• Party
• What did you value most?
• Are there any aspects that you think could be improved?
• Has the program helped you understand how to manage your emotions better? In
• what way?
• ‘Before’, ‘During’, and ‘After’ strategies o ‘Three Good Things’ activity
• Have you used things from the sessions in your day to day life?
• Recap of main ideas/strategies from each session
• Do you have any additional comments?
Keywords: brain injury, groups, neurorehabilitation, social, emotion regulation, qualitative
Citation: Rowlands L, Salas C, Coetzer R, Buckland S and Turnbull OH (2024) “We can all relate”: patient experience of an emotion-oriented group intervention after Acquired Brain Injury. Front. Psychol. 15:1384080. doi: 10.3389/fpsyg.2024.1384080
Edited by:
Nicolò Zarotti, Manchester Centre for Clinical Neurosciences, United KingdomReviewed by:
David Martínez-Pernía, Adolfo Ibáñez University, ChileKhalida Akbar, Durban University of Technology, South Africa
Copyright © 2024 Rowlands, Salas, Coetzer, Buckland and Turnbull. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leanne Rowlands, bHJvd2xhbmRzQGFyZGVuLmFjLnVr
 Leanne Rowlands
Leanne Rowlands Christian Salas
Christian Salas Rudi Coetzer2,4,5,6
Rudi Coetzer2,4,5,6