
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 10 September 2024
Sec. Psychology for Clinical Settings
Volume 15 - 2024 | https://doi.org/10.3389/fpsyg.2024.1382272
Background: Dying in a preferred place is important for a good death. Currently, no study has evaluated the extent to which the preferences for the place of death (PoD) are met among terminal cancer patients in China. This study examined the congruence between the preferred and actual PoD and its predictors among terminal cancer patients in China.
Methods: Between 2015 and 2023, 845 terminal cancer patients from four tertiary hospitals in Wuhan, China, were enrolled and followed till death. Face-to-face surveys at baseline and telephone-based interviews in the last month of patients’ lives were combined to learn patients’ preferred PoD. Data on patients’ actual PoD were collected from families within 1 month after patients’ death.
Results: Of the 410 patients who died, 62.7% of them died in hospitals. The agreement between patients’ preferred and actual PoD was fair (κ = 0.221). The congruence between patients’ preferred and actual PoD was 63.0, 36.6%, and 0 for hospital death, home death, and hospice facility/nursing home death separately. Patients were more likely to die in their preferred places if their preferred place and family caregivers’ belief of patients’ preferred PoD was congruent (odds ratio [OR] = 6.464, p = 0.001), or if caregivers had a medically related occupation (OR = 4.577, p = 0.003); if patients were hospitalized at least twice in the last month of life (OR = 0.422, p = 0.000), or the quality of care received by patients in the last 48 h was rated good by the families (OR = 0.373, p = 0.011), patients were less likely to die in their preferred places.
Conclusion: The congruence between patients’ preferred and actual PoD was fair. Advance care planning (ACP) needs to be popularized in China, and the quality of care in hospice facilities and nursing homes should be improved. The necessary policy support for hospice care should be made to respect cancer patients’ end-of-life (EoL) care preferences in China.
Despite increased life expectancy and complete cures that are conceivable for many kinds of cancer, it is still the leading cause of death in 57 countries, including China (Bray et al., 2021). Terminal cancer patients occupy a large proportion of people who can benefit from hospice care focusing on easing suffering and improving quality of life at the EoL stage (Smith et al., 2012). One essential part of hospice care is to respect patients’ preferences for the place where they are cared for, spend the rest life, and die finally (Davies and Higginson, 2004). Previous literature has indicated most cancer patients all over the world preferred to die at home (Gomes et al., 2013; Teno and Curtis, 2016; Lee and Lee, 2022; Cohen et al., 2015), while the actual PoD did not necessarily match the preferred PoD. Various complications and unbearable pain may force patients and families to give up home care and seek more care from medical institutions (Kain and Eisenhauer, 2016), resulting in repeated hospitalizations and an increasing likelihood of hospital death.
Currently, more and more countries have taken steps to promote dying in preferred places through hospice care programs and ACP interventions (Van Beek et al., 2013; Driller et al., 2022), whereas such services remain relatively nascent, especially in China (Wu et al., 2016). The limited financial support, less mature management guidelines, insufficient hospice wards, and inadequate professional staff cannot satisfy the increasing needs for hospice care (Yin et al., 2017). According to the latest report on the quality of death worldwide in 2021, China ranked 53rd among 81 countries (Finkelstein et al., 2022). With a gradual increase in the incidence and mortality of cancer (Bray et al., 2021), it is necessary to promote the quality of death of terminal cancer patients in China. The congruence between the preferred and actual PoD indeed serves as a significant indicator of the quality of death (Peláez-Cantero et al., 2023).
Exploring the congruence between patients’ preferred and actual PoD as well as the associated factors can address the facilitators and barriers to the compliance of patients’ PoD preferences. Then relevant interventions can be made to follow patients’ EoL care preferences, thus promoting patients’ quality of EoL care. Nowadays, most studies related to this topic focused on the preferences for PoD (Vidal et al., 2022; Alsirafy et al., 2019; Malhotra et al., 2021; Yeung, 2020; Chen et al., 2014; Kuo et al., 2017; Gu et al., 2015; Leng et al., 2022), the actual PoD (Lee and Lee, 2022; Puechl et al., 2019; Lin et al., 2017; Tang, 2002; Lee et al., 2014; Li et al., 2020; Ding et al., 2023), or patient-family congruence on the preferred PoD (Tang et al., 2010; Tang et al., 2005; Tang et al., 2008) separately. Only very few studies explored the congruence between patients’ preferred and actual PoD among cancer patients in Brazil (n = 190) (Valentino et al., 2023) and Sweden (n = 242) (Nilsson et al., 2023). While in China, Tang et al.’s study found a poor to slight agreement between the preferred and actual PoD among 127 advanced cancer patients in Taiwan, but this study was conducted 20 years ago (Tang and McCorkle, 2003), and the policy development related to palliative care was very different between Taiwan China and China. Given the paucity of information and limited published data on the congruence between patients’ preferred and actual PoD among advanced cancer patients in China, this study sought to investigate the preferences for PoD in a cohort of relatively large-sample of different terminal cancer patients in China, to follow the patients until their death to measure the congruence between their preferred and actual PoD. Factors associated with the congruence between the preferred and actual PoD as well as the agreement in preferred PoD between patient-family caregiver dyads were also explored.
A prospective cohort study was adopted between January 2015 and August 2023 to collect data from terminal cancer patients in Wuhan, China, through face-to-face interviews and telephone-based surveys with questionnaires.
Terminal cancer patient-family caregiver dyads were recruited from four tertiary hospitals in Wuhan, China, via a convenience sampling method. Our research team members contacted the nursing administrators of four hospitals and explained the purpose and procedures of the study. The eligibility criteria for the participants included patients diagnosed with terminal cancer, unresponsive to curative therapy, competent in cognition, whose estimated life expectancy was less than 6 months, and during hospitalization. Family members identified as the primary caregivers to be involved in patients’ EoL care, able to communicate coherently, aged 18 and older, were also recruited. The exclusion criteria specified patients or caregivers who were not Chinese.
Given that most Chinese work from Monday to Friday and rest on weekends in a week, it will be less busy on weekends, so the data were collected at 9–12 a.m. and 2–5 p.m. on weekends from 1 January 2015 to 31 August 2023 to allow more flexibility and respondence. After the eligibility screening in the oncology department, terminal cancer patients and family caregivers who signed informed consent or gave oral consent were face-to-face interviewed separately in an intimate room by a trained research nurse first to collect their socio-demographic information and patients’ preferred PoD. The follow-up telephone interview took place in the last month of the patients’ lives, estimated by the physician in charge to learn the patients’ preference for PoD again. At last, within 1 month after the patients’ death, families were interviewed about patients’ reception of hospice care and actual PoD by phone.
Ethical approval of the research protocol was granted by the institutional review board of Huazhong University of Science and Technology [registration number: [2019]IEC(S198)] as well as all the institutional review boards of the participating hospitals. All participants were informed of their voluntary participation in the study and their right to refuse to participate and withdraw from the study at any time, and all information was kept confidential.
Patient-caregiver dyads’ general characteristics, such as age, gender, and the relationship between patients and caregivers (spouse, son/daughter, parents, sibling, and others), were collected at baseline. Patients’ disease conditions, such as types of cancer and the date diagnosed as cancer were also collected.
Patients’ preferred PoD was investigated twice during a baseline face-to-face survey and follow-up telephone interview by asking them “Where is your preferred place to spend your last days of life?.” Response categories were “home,” “hospital,” “hospice facility,” “nursing home,” “relative’s home” and “other places.” Besides, family caregivers’ belief of the patients’ preferred PoD was asked by the item, “Where do you think the patient would like to spend his/her last days of life?,” with the same response categories as that of the patients’ question.
Patients’ actual PoD was obtained from family caregivers within 1 month after patients’ death. Additionally, patients’ conditions approaching death, such as whether had pain and dyspnea and whether received hospice care, were also collected from families. We also asked families to rate the quality of care that the patients received within 48 h before death and the patients’ quality of death.
The congruence was rated as “congruent” if the patients’ last reported preferred PoD was the same as their actual PoD (answered by the family caregivers). Otherwise, it was rated as “not congruent.”
Data analysis was calculated with SPSS 24.0 (SPSS Inc., Chicago, IL) (IBM Corp, 2012). Descriptive statistics were used for participants’ characteristics. The κ statistic was used to assess the agreement between patients’ preferred and actual PoD, with values ≤0 as indicating no agreement, 0.01–0.20 as none to slight, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1.00 as almost perfect agreement (McHugh, 2012). Binary logistic regression models were applied to identify how significant variables were associated with the congruence. Differences at a p-value of <0.05 were demonstrated as statistically significant. An OR with a 95% confidence interval (CI) was calculated for each outcome variable.
A total of 1,229 patient-caregiver dyads met the inclusion criteria, but 328 dyads refused to participate in the study, and 56 dyads did not complete the questionnaire, leaving 845 dyads to complete baseline tests, with a response rate of 68.8%. During the follow-up period, 84 patients were still alive until the end of the study, 125 dyads refused to continue to participate in the survey, and 226 dyads were lost to follow-up due to the unavailable phone number, leaving 410 patients who died during the study period (Figure 1).
The baseline characteristics of 845 dyads are presented in Table 1. Approximately half (52.3%) of the patients were male, with a median age of 54.1 years old. The most common type of cancer was lung cancer (27.5%), followed by breast cancer (17.7%), head and neck cancer (14.6%), intestinal cancer (13.0%), and gastric carcinoma (8.2%); and cancer had lasted for approximately an average of 422 days from diagnosis to study enrollment. Family caregivers were mostly the patients’ spouses (59.2%), followed by sons or daughters (27.9%). Approximately half of them were female (55.0%) with an average age of 47.2 years old.
Most dying patients had pain (69.0%) and did not receive hospice care (89.1%). A total of 27.6% of the family caregivers rated the quality of care received by patients in the last 48 h as good, while 55.4% of them thought patients’ quality of death was good (Table 2).
For patients’ preferred PoD, the home was selected by most patients (83.7%) in the baseline interview but decreased (68.1%) in the follow-up interview in the last month of their life. The percentage of the preference for dying in hospitals and hospice facilities increased from 9.3 to 24.4% and from 0.7 to 6.1%, respectively, in the two interviews. Additionally, the agreement in patients’ preferred PoD in patient-caregiver dyads was both fair in the baseline interview (κ = 0.211, p = 0.000) and in the follow-up interview (κ = 0.267, p = 0.000) (Table 3).
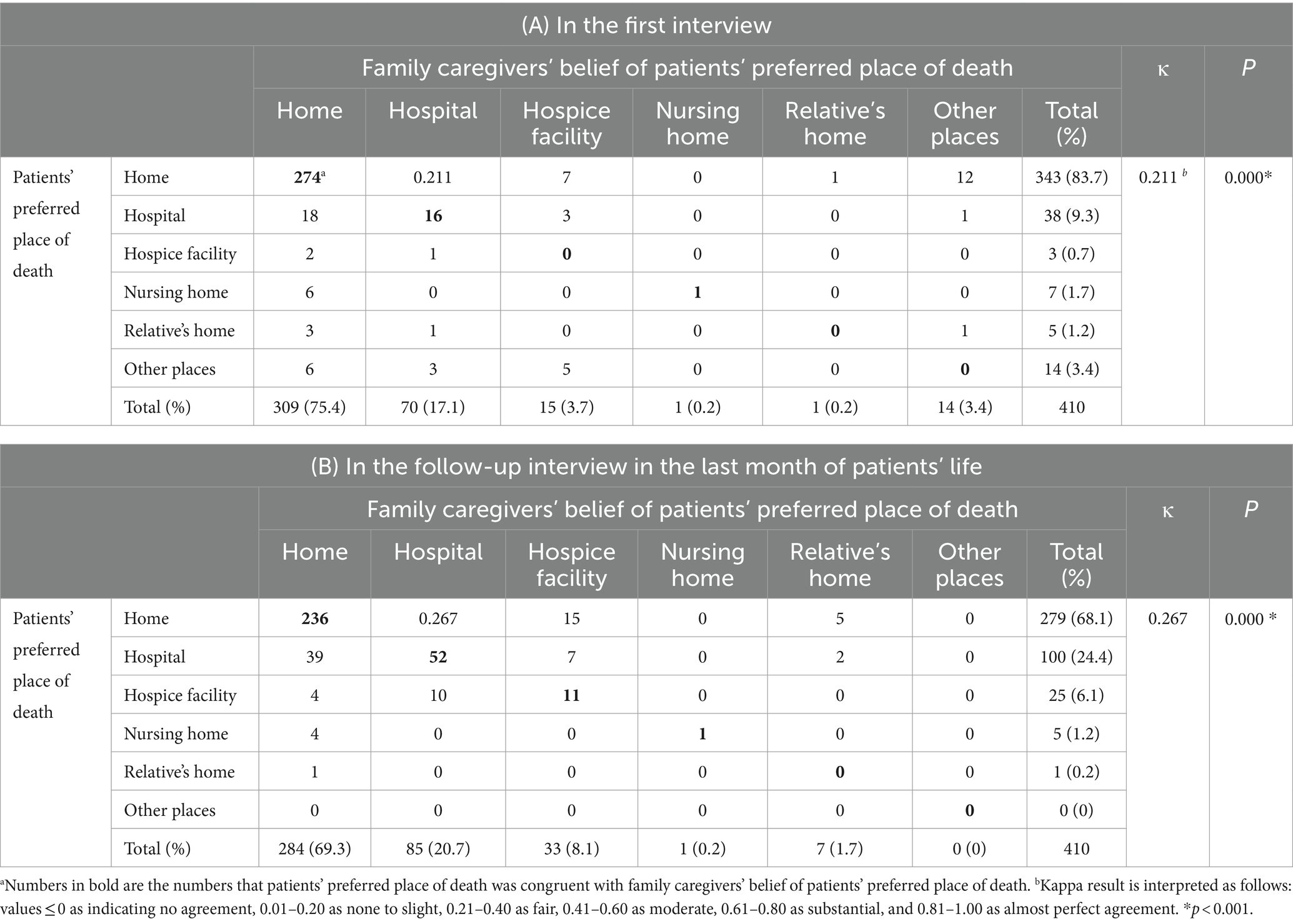
Table 3. Patients’ preferred place of death and congruence between patient-family caregiver dyads (n = 410).
For patients’ actual PoD, most patients died in hospitals (62.7%), followed by home (36.1%) and on the way to hospitals (1.2%). The congruence between patients’ preferred and actual PoD was 63.0, 36.6%, and 0 for hospital death, home death, and hospice facilities/nursing homes/relative’s home death separately (Figure 2). In summary, the agreement between patients’ preferred and actual PoD was fair (κ = 0.221, p = 0.000) (Table 4).
The congruence between patients’ preferred and actual PoD was more likely to be achieved when patients’ preferred PoD and family caregivers’ belief of patients’ preferred PoD was congruent (OR = 6.464, p = 0.001), or caregivers had a medical-related occupation (OR = 4.577, p = 0.003); if hospitalizations occurred at least twice in the last month of patients’ lives (OR = 0.422, p = 0.000), or the quality of care received by the patients in the last 48 h was good rated by the family caregivers (OR = 0.373, p = 0.011), patients were less likely to die in their preferred places (Table 5).

Table 5. Predictors of the congruence between patients’ preferred and actual place of death (n = 410).
Consistent with previous findings (Agar et al., 2008; Hinton, 1994), our study found that terminal cancer patients’ preferences for home death decreased, while the preference for dying in hospitals or hospice facilities increased as death approached. When dying is approaching, preparation for symptom control related to dying is required (National Cancer Center and National Hospice Center, 2020), while families are less confident in offering quality home care (Gao et al., 2013). In addition, this study also collected data during the COVID-19 pandemic. Considering the limited professional support outside hospitals during the COVID-19 wave, no wonder many people wanted to go to hospitals for symptom control (Lucijanic et al., 2023). Hospice care aims at relieving patients’ bad sufferings and helping them acquire a relatively comfortable dying process with dignity (Kumar et al., 2017), but such services are mostly provided in hospitals in China as professional hospice facilities are in great shortage in most areas of China, including Wuhan (Lu et al., 2018). Patients and families believe hospitals are more reliable to deal with discomfort symptoms than other settings (Li et al., 2020). Suggesting hospice services need to be expanded, not only in hospitals and hospice facilities but also provide hospice at home or nursing homes under potential legislation for dying patients to make flexible choices of preferred PoD.
The agreement between patients’ preferred and actual PoD was fair. A total of 63.0% of those patients preferred hospital death and 36.6% of those preferred home death ultimately died in their preferred places, but the percentage was 0 for those who preferred dying in hospice facilities/nursing homes. Impacted by the Chinese principle of filial piety, compared with those patients who preferred to die in other places, patients’ wishes for hospital death were more likely to be met, as their families were more likely to make all efforts to prolong the patients’ life (Ling et al., 2020). For the home death preference, patients and families who acknowledged the Chinese proverb “falling leaves return to their roots” were more likely to return home when death was approaching (Li et al., 2020). The preference for hospice death or nursing home death was difficult to follow due to the unawareness and inaccessibility to hospice services (Wu et al., 2016; Yin et al., 2017). Additionally, hospice care fees are only partially covered by medical insurance in China (China Health Insurance, 2020); families need to pay for hospice care out of their pocket, while 57.4% of patients’ family financial status was not adequate in our study, which may be another reason why the percentage was 0 for those who preferred dying in hospice facilities/nursing homes. Additionally, the COVID-19 pandemic might also influence the changes in PoD. Shibata et al. found home death appeared in a strong uptrend while hospital death exhibited downward trends after 2019 (Shibata et al., 2024), as many were without any option stuck at home despite their wishes to be in hospital or hospice, leading to a decreased congruence between preferred and actual PoD. The fair agreement between the preferred and actual PoD suggests a need to establish and utilize community-or home-based hospice services and increase the reimbursement of hospice care under potentially considering legislation to support advance directives.
If patients’ preferred PoD and family caregivers’ belief of the patient’s preferred PoD was the same, patients were more likely to die in their preferred places. Previous literature has indicated that the inconsistent gap between patients and their surrogates regarding EoL care preferences can be decreased through ACP (Ke et al., 2021); in addition, ACP indeed helps patients receive care concordant with their preferences (Detering et al., 2010). Given the fact that ACP remains unfamiliar to the public and has not been regulated by legislation in China (Zhang et al., 2021), it is urgent to establish relevant policies or guidelines to promote the awareness and development of ACP in China, to increase the congruence between patients and caregivers about patients’ PoD preferences, and thus to promote the compliance of patients’ EoL care preferences.
If the family caregivers engaged in the medical-related work, patients were more likely to die in their preferred places. Family-centered decision-making process is admired in Asian culture (Haley et al., 2002). Family caregivers with medically related occupations may tend to occupy the leading position in the decision-making process and are more willing to initiate death topics with patients (Itzhaki et al., 2016), which may make them know more about the patient’s preferred PoD. Furthermore, they might be more aware that satisfying patients’ preferences was an essential indicator of the quality of good death (Peláez-Cantero et al., 2023); thus, they were more prone to respect and follow patients’ preferences. This highlights that detailed ACP or EoL care discussions should be started earlier to promote the families’ awareness of patients’ EoL preferences.
When patients were hospitalized at least twice in the last month of life, they were less likely to die in their preferred places. The more hospitalizations suggest patients may suffer more emergent symptoms that need to be addressed. Under the healthcare background in China, hospitals, especially tertiary hospitals, are the priority for patients and families to seek professional help, as most community hospitals or nursing homes can only offer basic medical care to various patients (Gu et al., 2015). Other reasons may include the less utilization of hospice facilities (Lu et al., 2018), insufficient medical resources, and weaker professional competence of nursing home staff (Gu et al., 2015), leading the patients to go to hospitals for treatment. It is important to reallocate and balance the medical services among hospitals, hospice facilities, and nursing homes, to make patients receive timely treatment in their preferred PoD.
If family caregivers considered patients had received high-quality care in the last 48 h, patients were less likely to die in their preferred places compared to those who acquired low-quality care or did not receive care. Caregivers may wish the high-quality care to last till the last moment of patients’ lives, resulting in increasing numbers of hospital deaths, whatever the patients’ preferred PoD was. For the patients who received high-quality care in hospitals in the last 48 h, they might change their preference from other places to hospital death, but this actual “last” preference was unknown to us as almost all the patients were unconscious or could not express normally at this EoL stage, suggesting to note and update patients’ EoL care preferences more dynamically. It is urgent to set up more hospice facilities in China to provide high-quality care not only in hospitals but also to improve the quality of care in hospice facilities, nursing homes, and at home, thus meeting patients’ EoL care preferences with flexibility.
Our study provides insight into the congruence of patients’ preferred and actual PoD and the factors of it, as well as the agreement in patients’ preferred PoD in patient-caregiver dyads among terminal cancer patients in China for the first time with a relatively large sample size, which will help to improve compliance of patients’ EoL care preferences. There are several limitations. First, a convenience sampling method was used to recruit participants from four tertiary hospitals in Wuhan, China, possibly limiting the findings to be generalized to patients in primary or secondary hospitals, and in communities or medical care facilities. Second, patients’ preferred PoD interviewed in their last month of life may not be totally the same as the preference in the last few hours. Future research with a mixed method in different facilities could be carried out to provide more information on the congruence of patients’ preferred and actual PoD.
This study provides insight into the congruence between preferred and actual PoD among terminal cancer patients living in China and further highlights that if patients’ preferred PoD and family caregivers’ belief of patients’ preferred PoD was congruent, or family caregivers occupied a medical-related job, patients would tend to die in their preferred places. There are opportunities to promote the compliance of patients’ EoL care preferences, but this will require popularizing ACP and improving the quality of care not only in hospitals but also in hospice facilities and nursing homes. Policies or laws about hospice care should be made to respect patients’ rights in China, thus improving the quality of EoL care for terminal cancer patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the institutional review board of Huazhong University of Science and Technology. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
HL: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. PN: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. BW: Writing – review & editing. JL: Investigation, Writing – original draft. JF: Investigation, Writing – original draft.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Natural Science Foundation of China (Grant No. 71904056).
The authors gratefully appreciate all the participating patients and their family members, as well as the medical staff of the participating hospitals.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Agar, M., Currow, D. C., Shelby-James, T. M., Plummer, J., Sanderson, C., and Abernethy, A. P. (2008). Preference for place of care and place of death in palliative care: are these different questions? Palliat. Med. 22, 787–795. doi: 10.1177/0269216308092287
Alsirafy, S. A., Hammad, A. M., Ibrahim, N. Y., Farag, D. E., and Zaki, O. (2019). Preferred place of death for patients with incurable Cancer and their family caregivers in Egypt. Am. J. Hosp. Palliat. Care 36, 423–428. doi: 10.1177/1049909118813990
Bray, F., Laversanne, M., Weiderpass, E., and Soerjomataram, I. (2021). The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer 127, 3029–3030. doi: 10.1002/cncr.33587
Chen, C. H., Lin, Y.-C., Liu, L.-N., and Tang, S. T. (2014). Determinants of preference for home death among terminally ill patients with cancer in Taiwan: a cross-sectional survey study. J. Nurs. Res. 22, 37–44. doi: 10.1097/jnr.0000000000000016
China Health Insurance. (2020). 2020 medical insurance catalog adjustment results released! National Medical Insurance Bureau: dynamic adjustment mechanism is basically completed. Available online at: https://www.zgylbx.com/index.php?m=content&c=index&a=show&catid=6&id=37369 (Accessed October 10, 2023)
Cohen, J., Pivodic, L., Miccinesi, G., Onwuteaka-Philipsen, B. D., Naylor, W. A., Wilson, D. M., et al. (2015). International study of the place of death of people with cancer: a population-level comparison of 14 countries across 4 continents using death certificate data. Br. J. Cancer 113, 1397–1404. doi: 10.1038/bjc.2015.312
Davies, E., and Higginson, I. J. (2004). Palliative care: The solid facts. Copenhagen, DK: World Health Organization.
Detering, K. M., Hancock, A. D., Reade, M. C., and Silvester, W. (2010). The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 340:c 1345. doi: 10.1136/bmj.c1345
Ding, X.-S., Qi, J.-L., Liu, W.-P., Yin, P., Wang, L.-J., Song, Y.-Q., et al. (2023). Trends and determinants of place of death among Chinese lymphoma patients: a population-based study from 2013-2021. Am. J. Cancer Res. 13, 4246–4258
Driller, B., Talseth-Palmer, B., Hole, T., Strømskag, K. E., and Brenne, A.-T. (2022). Cancer patients spend more time at home and more often die at home with advance care planning conversations in primary health care: a retrospective observational cohort study. BMC Palliat. Care 21:61. doi: 10.1186/s12904-022-00952-1
Finkelstein, E. A., Bhadelia, A., Goh, C., Baid, D., Singh, R., Bhatnagar, S., et al. (2022). Cross country comparison of expert assessments of the quality of death and dying 2021. J. Pain Symptom Manag. 63, e419–e429. doi: 10.1016/j.jpainsymman.2021.12.015
Gao, W., Ho, Y. K., Verne, J., Glickman, M., and Higginson, I. J. (2013). Changing patterns in place of cancer death in England: a population-based study. PLoS Med. 10:e1001410. doi: 10.1371/journal.pmed.1001410
Gomes, B., Calanzani, N., Gysels, M., Hall, S., and Higginson, I. J. (2013). Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat. Care 12:7. doi: 10.1186/1472-684x-12-7
Gu, X., Cheng, W., Cheng, M., Liu, M., and Zhang, Z. (2015). The preference of place of death and its predictors among terminally ill patients with cancer and their caregivers in China. Am. J. Hosp. Palliat. Care 32, 835–840. doi: 10.1177/1049909114542647
Haley, W. E., Allen, R. S., Reynolds, S., Chen, H., Burton, A., and Gallagher-Thompson, D. (2002). Family issues in end-of-life decision making and end-of-life care. Am. Behav. Sci. 46, 284–298. doi: 10.1177/000276402236680
Hinton, J. (1994). Can home care maintain an acceptable quality of life for patients with terminal cancer and their relatives? Palliat. Med. 8, 183–196. doi: 10.1177/026921639400800302
Itzhaki, M., Hildesheimer, G., Barnoy, S., and Katz, M. (2016). Family involvement in medical decision-making: perceptions of nursing and psychology students. Nurse Educ. Today 40, 181–187. doi: 10.1016/j.nedt.2016.03.002
Kain, D. A., and Eisenhauer, E. A. (2016). Early integration of palliative care into standard oncology care: evidence and overcoming barriers to implementation. Curr. Oncol. 23, 374–377. doi: 10.3747/co.23.3404
Ke, L. S., Hu, W.-Y., Chen, C.-Y., Liu, C.-Y., and Chiu, T.-Y. (2021). A quasi-experimental evaluation of advance care planning improves consistency between elderly individuals and their surrogates regarding end-of-life care preferences: development and application of a decision aid with cartoon pictures. Patient Educ. Couns. 104, 815–825. doi: 10.1016/j.pec.2020.09.027
Kumar, P., Wright, A. A., Hatfield, L. A., Temel, J. S., and Keating, N. L. (2017). Family perspectives on hospice care experiences of patients with Cancer. J. Clin. Oncol. 35, 432–439. doi: 10.1200/JCO.2016.68.9257
Kuo, T.-L., Lin, C.-H., Jiang, R.-S., Yen, T.-T., Wang, C.-C., and Liang, K.-L. (2017). End-of-life care for head and neck cancer patients: a population-based study. Support Care Cancer 25, 1529–1536. doi: 10.1007/s00520-016-3555-x
Lee, L.-C., Hu, C.-C., Loh, E.-W., and Hwang, S. F. (2014). Factors affecting the place of death among hospice home care cancer patients in Taiwan. Am. J. Hosp. Palliat. Care 31, 300–306. doi: 10.1177/1049909113487427
Lee, E. J., and Lee, N.-R. (2022). Factors associated with place of death for terminal cancer patients who wished to die at home. Medicine (Baltimore) 101:e30756. doi: 10.1097/MD.0000000000030756
Leng, A., Maitland, E., Wang, S., Nicholas, S., Lan, K., and Wang, J. (2022). Preferences for end-of-life care among patients with terminal Cancer in China. JAMA Netw. Open 5:e228788. doi: 10.1001/jamanetworkopen.2022.8788
Li, Z., Jiang, S., Xu, C., Lu, F., He, R., Pan, Z., et al. (2020). Determinants of place of death for end-stage cancer patients: evidence from China. Int. J. Qual. Health Care 32, 41–47. doi: 10.1093/intqhc/mzz064
Lin, H.-Y., Kang, S.-C., Chen, Y.-C., Chang, Y.-C., Wang, W.-S., and Lo, S.-S. (2017). Place of death for hospice-cared terminal patients with cancer: a nationwide retrospective study in Taiwan. J. Chin. Med. Assoc. 80, 227–232. doi: 10.1016/j.jcma.2016.10.009
Ling, M., Wang, X., Ma, Y., and Long, Y. (2020). A review of the current state of hospice care in China. Curr. Oncol. Rep. 22:99. doi: 10.1007/s11912-020-00959-y
Lu, Y., Gu, Y., and Yu, W. (2018). Hospice and palliative Care in China: development and challenges. Asia Pac. J. Oncol. Nurs. 5, 26–32. doi: 10.4103/apjon.apjon_72_17
Lucijanic, M., Marelic, D., Stojic, J., Markovic, I., Sedlic, F., Kralj, I., et al. (2023). Predictors of prolonged hospitalization of COVID-19 patients. Eur Geriatr Med 14, 511–516. doi: 10.1007/s41999-023-00787-w
Malhotra, C., Koh, L. E., Teo, I., Ozdemir, S., Chaudhry, I., and Finkelstein, E. (2021). A prospective cohort study of stability in preferred place of death among patients with stage IV Cancer in Singapore. J. Natl. Compr. Cancer Netw. 20, 20–28. doi: 10.6004/jnccn.2020.7795
McHugh, M. L. (2012). Interrater reliability: the kappa statistic. Biochem Med 22, 276–282. doi: 10.11613/BM.2012.031
National Cancer Center and National Hospice Center. (2020) Guide to the provision of hospice services for hospice agencies. Available at: https://www.hospice.go.kr/pain/archivesView.do?brd_no=96940 (Accessed September 28, 2023).
Nilsson, J., Bergström, S., Hållberg, H., Berglund, A., Bergqvist, M., and Holgersson, G. (2023). Prospective study of preferred versus actual place of death among Swedish palliative Cancer patients. Am. J. Hosp. Palliat. Care. doi: 10.1177/10499091231213640
Peláez-Cantero, M. J., Morales-Asencio, J. M., Navarro-Mingorance, Á., Madrid-Rodriguez, A., Tavera-Tolmo, Á., Escobosa-Sánchez, O., et al. (2023). End of life in patients attended by pediatric palliative care teams: what factors influence the place of death and compliance with family preferences? Eur. J. Pediatr. 182, 2369–2377. doi: 10.1007/s00431-023-04870-z
Puechl, A. M., Chino, F., Havrilesky, L. J., Davidson, B. A., and Chino, J. P. (2019). Place of death by region and urbanization among gynecologic cancer patients: 2006-2016. Gynecol. Oncol. 155, 98–104. doi: 10.1016/j.ygyno.2019.07.013
Shibata, M., Otsuka, Y., Hagiya, H., Koyama, T., Kashiwagi, H., and Otsuka, F. (2024). Changes in the place of death before and during the COVID-19 pandemic in Japan. PLoS One 19:e0299700. doi: 10.1371/journal.pone.0299700
Smith, T. J., Temin, S., Alesi, E. R., Abernethy, A. P., Balboni, T. A., Basch, E. M., et al. (2012). American society of clinical oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J. Clin. Oncol. 30, 880–887. doi: 10.1200/JCO.2011.38.5161
Tang, S. T. (2002). Influencing factors of place of death among home care patients with cancer in Taiwan. Cancer Nurs. 25, 158–166. doi: 10.1097/00002820-200204000-00013
Tang, S. T., Chen, C. C.-H., Tang, W.-R., and Liu, T.-W. (2010). Determinants of patient-family caregiver congruence on preferred place of death in Taiwan. J. Pain Symptom Manag. 40, 235–245. doi: 10.1016/j.jpainsymman.2009.12.018
Tang, S. T., Liu, T.-W., Lai, M.-S., and McCorkle, R. (2005). Discrepancy in the preferences of place of death between terminally ill cancer patients and their primary family caregivers in Taiwan. Soc. Sci. Med. 61, 1560–1566. doi: 10.1016/j.socscimed.2005.02.006
Tang, S. T., Liu, T.-W., Tsai, C.-M., Wang, C.-H., Chang, G.-C., and Liu, L.-N. (2008). Patient awareness of prognosis, patient-family caregiver congruence on the preferred place of death, and caregiving burden of families contribute to the quality of life for terminally ill cancer patients in Taiwan. Psychooncology 17, 1202–1209. doi: 10.1002/pon.1343
Tang, S. T., and McCorkle, R. (2003). Determinants of congruence between the preferred and actual place of death for terminally ill cancer patients. J. Palliat. Care 19, 230–237. doi: 10.1177/082585970301900403
Teno, J. M., and Curtis, J. R. (2016). Family perspectives on aggressive Cancer care near the end of life. JAMA Oncol. 2, 957–958. doi: 10.1001/jamaoncol.2016.0441
Valentino, T. C. O., Paiva, C. E., de Oliveira, M. A., Hui, D., Bruera, E., Julião, M., et al. (2023). Preference and actual place-of-death in advanced cancer: prospective longitudinal study. BMJ Support. Palliat. Care. doi: 10.1136/spcare-2023-004299
Van Beek, K., Woitha, K., Ahmed, N., Menten, J., Jaspers, B., Engels, Y., et al. (2013). Comparison of legislation, regulations and national health strategies for palliative care in seven European countries (results from the Europall research group): a descriptive study. BMC Health Serv. Res. 13:275. doi: 10.1186/1472-6963-13-275
Vidal, M., Rodriguez-Nunez, A., Hui, D., Allo, J., Williams, J. L., Park, M., et al. (2022). Place-of-death preferences among patients with cancer and family caregivers in inpatient and outpatient palliative care. BMJ Support. Palliat. Care 12, e501–e504. doi: 10.1136/bmjspcare-2019-002019
Wu, Y., Li, L., Su, H., Yao, X., and Wen, M. (2016). Hospice and palliative care: development and challenges in China. Clin. J. Oncol. Nurs. 20, E16–E19. doi: 10.1188/16.CJON.E16-E19
Yeung, N. Y. (2020). Expectation of the place of care and place of death of terminal cancer patients in Hong Kong: a hospital based cross-sectional questionnaire survey. Ann Palliat Med. 9, 4534–4548. doi: 10.21037/apm.2019.09.17
Yin, Z., Li, J., Ma, K., Ning, X., Chen, H., Fu, H., et al. (2017). Development of palliative Care in China: a tale of three cities. Oncologist 22, 1362–1367. doi: 10.1634/theoncologist.2017-0128
Keywords: cancer, place of death, congruence, hospice care, quality of death
Citation: Lin H, Ni P, Wu B, Liao J and Fu J (2024) The congruence between the preferred and actual places of death among terminal cancer patients in China. Front. Psychol. 15:1382272. doi: 10.3389/fpsyg.2024.1382272
Received: 20 March 2024; Accepted: 26 August 2024;
Published: 10 September 2024.
Edited by:
Vittorio Lenzo, University of Catania, ItalyReviewed by:
Xiao Feng Xie, Sichuan University, ChinaCopyright © 2024 Lin, Ni, Wu, Liao and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ping Ni, bmlwaW5nQGh1c3QuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.