
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol., 07 August 2024
Sec. Pediatric Psychology
Volume 15 - 2024 | https://doi.org/10.3389/fpsyg.2024.1380826
This article is part of the Research TopicPsychological Implications of Preterm BirthView all 12 articles
Objective: Early psychosocial interventions for preterm infants and their parents are diverse. This study aimed to structure the knowledge on psychosocial parent–infant interventions and to identify gaps in the intervention studies.
Methods: We included studies on early (during first year of life) psychosocial parent–infant interventions with parent–infant relationship outcomes after preterm birth (< 37 weeks). We excluded studies that did not focus on preterm infants, failed to indicate the studied intervention and outcomes, were not written in English, were not controlled or peer-reviewed studies, or did not provide essential information for eligibility. The search included studies published between January 2000 and March 2024 in PubMed and PsycINFO. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed in reporting. Psychosocial parent–infant intervention studies were classified adapting the International Classification of Health Interventions (ICHI) and the Template for Intervention Description and Replication (TIDieR).
Results: The included 22 studies reported data from 18 different interventions with preterm infants (< 37 weeks). Studies excluded preterm infants with health risks (19/22, 86%), with very low gestational age and/or birth weight (7/22, 32%), and/or mothers with psychosocial risks (14/22, 64%). Of the 18 interventions, 12 (67%) were classified as counseling, 3 (17%) as emotional support, 2 (11%) as psychotherapeutic, and 1 (6%) as educational. The parent–child relationship was assessed using 30 different methods and varying time points up to 18 months of age. Most studies (17/22, 77%) reported positive changes in the parent–child relationship favoring the intervention group.
Conclusion: We identified four types of interventions to influence parenting behavior; the most used was counseling. All four intervention types showed positive effects on parent–infant relationships, although the preterm populations studied were selective, the effects were evaluated using different methods, and the follow-up periods were short. These findings indicate a need for studies with standardized methods, longer follow-up, and less-restricted preterm populations to develop guidelines for all families with preterm infants.
Preterm birth (< 37 weeks of gestation) is a stressor for infant brain development (Krugers et al., 2017) and may relate to adverse neurodevelopmental (Bhutta et al., 2002; Aarnoudse-Moens et al., 2013) and socioemotional outcomes in later life (Bhutta et al., 2002; Aarnoudse-Moens et al., 2009; Woodward et al., 2009; Burnett et al., 2011; D’Onofrio et al., 2013; Johnson and Marlow, 2013). The lower the gestational age of the infant at birth, the higher the risk for developmental problems (Elgen et al., 2012; Arpi and Ferrari, 2013), hospital readmissions, and special care (Clark et al., 2008; Larroque et al., 2008; Athalye-Jape et al., 2022). Therefore, children born preterm are fragile and need a good environment to overcome early challenges and develop well.
A preterm birth is also a challenge to transition to parenthood. It interrupts the psychological preparation for the birth, leads often to early separation from the infant, and can include psychologically stressful or even traumatic situations during labor or the neonatal intensive care unit (NICU) care of the infant (Miles and Holditch-Davis, 1997; Jotzo and Poets, 2005; Melnyk et al., 2006; Forcada-Guex et al., 2011; Baum et al., 2012; Yaari et al., 2019). Earlier studies have shown that preterm birth also relates to stress and elevated mental health symptoms in parents, which, in turn, may negatively affect the parent–infant relationship (Forcada-Guex et al., 2011; Meijssen et al., 2011; Shah et al., 2011; Korja et al., 2012; Gerstein and Poehlmann-Tynan, 2015; Hoffenkamp et al., 2015a; Ionio et al., 2017; Gerstein et al., 2019). Together, infant fragility and challenges to early parenthood can create a complex negative circle of prematurity.
A well-functioning family relationships are a protective factor for the development of a fragile preterm infant (Miceli, 2000; Gross et al., 2001; Treyvaud et al., 2012; Aarnoudse-Moens et al., 2013; Gerstein and Poehlmann-Tynan, 2015; Faure et al., 2017). The optimal time to intervene in family relationships is during early months of an infant’s life and parenthood, as this is a sensitive period in infant development and the biopsychological processes of parenthood (Givrad et al., 2021). Therefore, the interventions supporting parenting and the parent–infant relationships (Muller-Nix and Forcada-Guex, 2009; Zeanah, 2009; Meijssen et al., 2011; Benzies et al., 2013; Gerstein and Poehlmann-Tynan, 2015; Givrad et al., 2021) should be important part of modern neonatal care.
There is evidence available that interventions supporting parenting or specifically emotional parent–infant relationships during NICU stay and/or the early months after discharge lead to positive health outcomes (Benzies et al., 2013; Evans et al., 2014; Yrjölä et al., 2022). In particular, interventions that include direct support for the parents or focus on the parent–infant interaction have been shown to improve outcomes such as parents’ mental well-being, child rearing attitudes, and the socioemotional and cognitive development of prematurely born children (Nordhov et al., 2010; Landsem et al., 2014, 2020; Welch et al., 2015; Vohr et al., 2017). A meta-analytic review showed that 8 out of 17 different psychosocial parent–infant interventions that were tested in randomization-controlled trials and published up to 2007 were effective in improving the quality of the parent–infant relationship. These eight interventions (Mother Infant Transaction Program, State Modulation, Nursing Systems Toward Effective Parenting-Preterm, Infant Behavioral Assessment and Intervention Program, Guided Participation, Kangaroo Holding, Traditional Holding, and an individualized family-based intervention) focused mainly on cue-based and responsive parental care (Evans et al., 2014).
However, a recent systematic review of early interventions for parenting in NICU found only small and short-term effects on parental sensitivity and stress compared with usual care or basic educational guidance, possibly because of diversity, implementation failure, or methodological bias (Lavallée et al., 2021). The structural framework of psychosocial parent–infant interventions in the preterm context has also been shown to be very heterogeneous, leaving uncertainties about their effectiveness and understanding of what works for whom (Benzies et al., 2013; Cho et al., 2013; Evans et al., 2014; Puthussery et al., 2018; Givrad et al., 2021; Lavallée et al., 2021). There have been no attempts to address this heterogeneity of intervention studies, for example, whether there are different types of interventions, and if fathers or different family structures were taken into consideration. There may be different subgroups of parents and infants and thereby a need for different approaches. For example, children born very preterm are at risk for different mental and behavioral disorders than children born preterm with later gestational age (Leppänen et al., 2023) and even for out-of-home placement during early years (Alenius et al., 2020). In the group of very preterm infants maternal psychosocial factors play an important role in the actualization or mitigation of these risks (Leppänen et al., 2023). Identifying appropriate interventions for different risk groups among NICU infants and families would be important.
A detailed understanding of the structural frameworks of the interventions and the level of support they provide would be especially beneficial for the planning of health care services (Castelpietra et al., 2017). However, no model has been designed for comparing and analyzing the differences between psychosocial parent–infant interventions for preterm infants and parents. Therefore, the aim of this scoping review was to provide more structured knowledge of early psychosocial parent–infant interventions that aim to promote parent–infant relationships during the first year after preterm birth. Specifically, we intended to explore the content of the interventions according to the theories, aims, implementation, and settings of the interventions and to study the parent–infant relationship outcomes. As described earlier, psychosocial parent–infant interventions vary a lot structurally; thus, we aimed to analyze the psychosocial parent–infant interventions in detail by using classification systems to identify potential different intervention types and describe parent–infant relationship outcomes. Furthermore, we aimed to summarize the evidence and identify potential gaps in the interventions and their implementation to benefit future research and health care services for parents with preterm infants.
In this scoping review, the systematic search and reporting followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for scoping reviews (Page et al., 2021). The literature search was conducted for articles published from January 2000 to March 2020 and later for articles published April 2020 to March 2024.
We included studies describing early (between birth and first year) psychosocial parent–infant (psychotherapy and parental) interventions for parent(s) and preterm-born infants (< 37 weeks of gestation) with studied outcomes in the parent–infant relationship and which were written in English. We excluded studies if the infants were not preterm (i.e., were born >37 weeks), did not trial interventions for parents and infants, or did not provide parent–infant relationship outcomes.
We reviewed the literature from 2000 to 2024 to examine the psychosocial parent–infant interventions and the parent–infant relationship outcomes of children born preterm in the 21st century, when neonatal care has reached an advanced stage. As earlier reviews did not search for psychotherapy/psychotherapeutic interventions, we included these as well. Only publications in English were included. We excluded studies that did not follow randomization control or study-control settings or essential information about the intervention to assess eligibility. Because we wanted to focus clearly on psychosocial interventions, we excluded interventions that promoted only physical closeness or one aspect of care, such as skin-to-skin contact. We also removed duplicates.
We searched the electronic databases PubMed and PsycINFO for all published data from January 2000 to March 2020. The search strategy comprised the following MESH headings or keywords: Premature Birth, Infant, Psychotherapy, Parent Infant Psychotherapy, and Parent Intervention. Searches were done in PubMed using the following criteria: “Premature Birth/psychology” [Mesh] OR “Infant, Premature/psychology” [Mesh] AND “Psychotherapy” [Mesh] OR “Parent Infant psychotherapy” [All Fields] OR “Parent Intervention” [All Fields] AND ((“2000/01/01” [PDAT]: “2020/03/01” [PDAT]) AND English[lang]). In PsycINFO, we used “Premature Birth” OR “Infant, Premature” AND “Psychotherapy” OR “Parent Infant psychotherapy” OR “Parent Intervention” Published Date: 20000101–20,200,331; Peer Reviewed; Publication Type: Peer Reviewed Journal; English; Age Groups: Childhood (birth−12 years); Population Group: Human; and Document Type: Journal Article. The number of all included and excluded articles of the literature search is provided in Figure 1, built according to the PRISMA guidelines (2021). Because reporting of the results took a long time, a complementary and identical search was done for all published data from April 2020 to March 2024. Studies were also identified from the reference lists of the screened manuscripts. The first author screened potential studies (n = 2,770) using the content analysis of the study abstracts and screened for eligibility by reading the manuscripts (n = 111). There were 8 studies identified through citations and were screened for eligibility. After screening, potential studies were scrutinized in greater depth through the reading of 74 manuscripts by the first author, with help of the coauthors, to examine the study methods, participants, inclusion/exclusion criteria, interventions (theory, aim, and implementation), outcomes, and results to conclude whether each study was eligible. In another search, the first author screened potential studies (n = 641) and scrutinized 21 of these studies, 4 of which were assessed in detail for eligibility with the help of the coauthors.
For different types of early psychosocial parent–infant interventions, we chose four index terms from the International Classification of Health Interventions (ICHI): Parents in Health Intervention.1 The four main types chosen were: (1) “Education to influence parenting behavior”—Providing information to improve knowledge and influence behavior concerning patterns of interaction between a parent and their child/children, including the nature and degree of monitoring and supervision; involvement and engagement; discipline; nurturing; and the expression of affection. (2) “Counseling about parenting behavior”—Providing therapeutic and/or supportive communication in relation to behavior concerning patterns of interaction between a parent and their child/children, including the nature and degree of monitoring and supervision; involvement and engagement; discipline; nurturing; and the expression of affection. (3) “Emotional support for parenting behaviors”—Providing comfort, empathy, or motivational support to the person regarding behavior concerning patterns of interaction between a parent and their child/children, including the nature and degree of monitoring and supervision; involvement and engagement; discipline; nurturing; and the expression of affection. (4) “Psychotherapy for parenting behaviors”—providing therapeutic communication, based upon the systematic application of psychological theory, in relation to behavior concerning patterns of interaction between a parent and their child/children, including the nature and degree of monitoring and supervision; involvement and engagement; discipline; nurturing; and the expression of affection. In this manuscript, we use abbreviated versions of the models’ names: education, counseling, emotional support, and psychotherapy.
To categorize the interventions into the four different intervention types, we looked at the aims and theoretical backgrounds of the interventions but especially the implementation in terms of what was done, how it was done and who did it. In addition, whether there was a focus on reading infants’ cues or providing emotional support to parents or on the parent–infant relationship or psychotherapeutic approach. The ICHI definitions were applied to the practice with preterm infants (see results and discussion for examples).
All authors of this paper studied the psychosocial parent–infant interventions separately and used a common Microsoft Excel model to capture each intervention’s theory and content. A consensus (a minimum of two reviewers) was then reached to assign each study to one of the four intervention categories.
However, there were still details in the implementation of the interventions that separated the 18 individual interventions from each other, and we added the subtype classification to structure this information. This classification is shown in Table 1, which presents the four main types and the six subtypes. The first author used the Template for Intervention Description and Replication (TIDieR) checklist (Hoffmann et al., 2014) to structure the studied interventions using more detailed qualitative and structural information. The TIDieR checklist’s details, such as name, why (theory, aim), what (materials/counseling, general/individualized), who (intervention provider’s education/training), and how (implementation, e.g., online/face-to-face), as well as where, when, and how much (environment, frequency) and how well the planned compared to the actual work done were described, were used for subtype classification. We also described the parent–infant relationship outcomes of the studies, and in relation to early parental psychosocial parent–infant intervention types. Data are available on request.
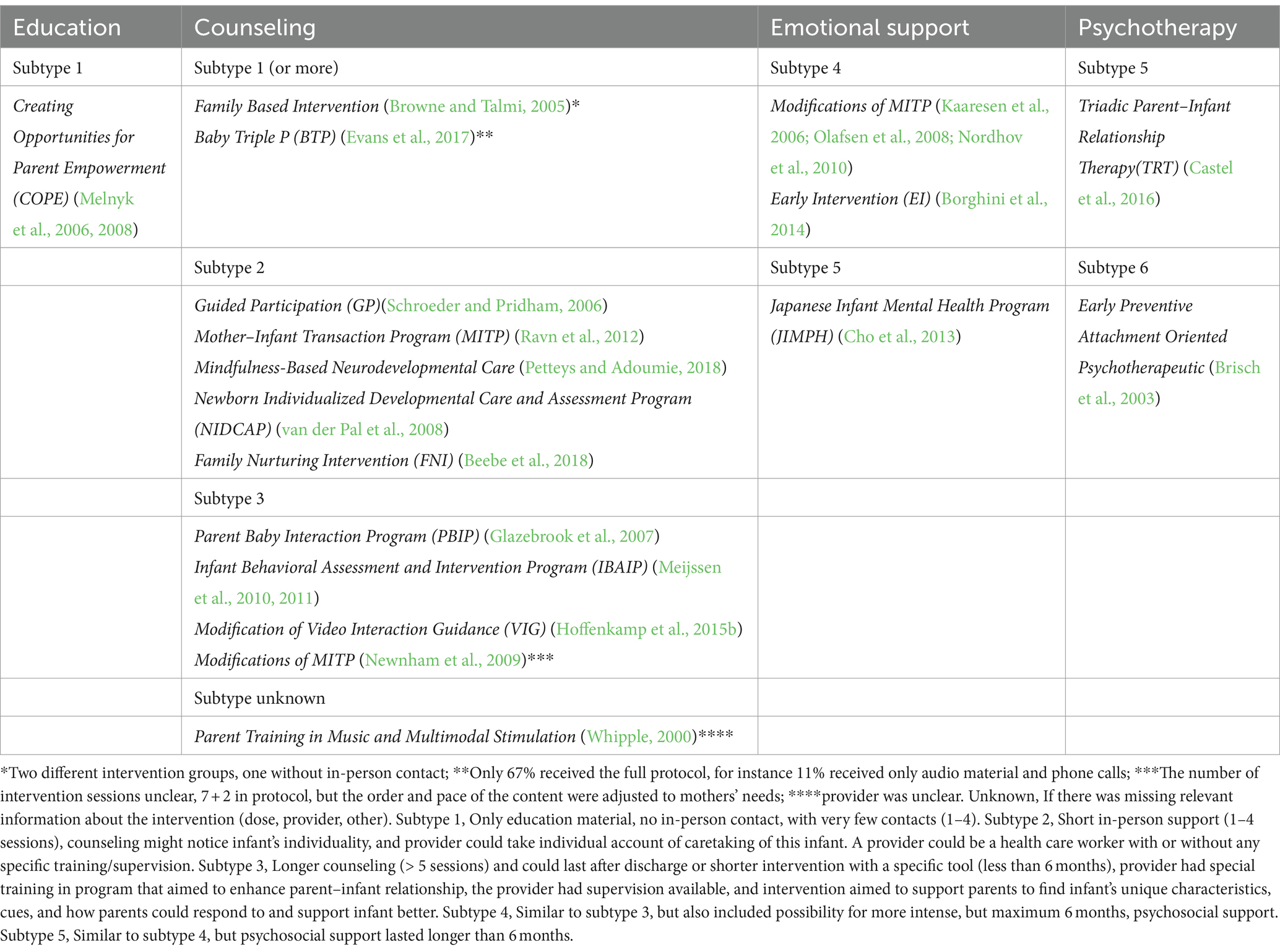
Table 1. Classification of early psychosocial parent–infant interventions to influence parenting behaviors.
We describe the selection of sources for evidence in the flow diagram shown in Figure 1.
This review included 22 studies, with 17 (Whipple, 2000; Brisch et al., 2003; Melnyk et al., 2006, 2008; Olafsen et al., 2008; van der Pal et al., 2008; Newnham et al., 2009; Meijssen et al., 2010, 2011; Nordhov et al., 2010; Ravn et al., 2012; Borghini et al., 2014; Hoffenkamp et al., 2015b; Castel et al., 2016; Evans et al., 2017; Beebe et al., 2018; Petteys and Adoumie, 2018) identified from PsycINFO and/or PubMed and 5 (Browne and Talmi, 2005; Kaaresen et al., 2006; Schroeder and Pridham, 2006; Glazebrook et al., 2007; Cho et al., 2013) identified through citation search in relevant articles. Two of the interventions were trialed with two different studies and parent–infant relationship outcomes (Melnyk et al., 2006, 2008; Meijssen et al., 2010, 2011), and one intervention was trialed three times (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010). Thus, there were 18 different early psychosocial parent–infant interventions but 22 studies with parent–infant relationship outcomes (Table 2). Out of all 22 studies, 19 (86.4%) were randomized-controlled studies and 3 (13.6%) were case–control studies. All included studies were quantitative with gathering and analysis of qualitative data. In total, 1,964 infants with their mothers and in some cases with their fathers were included in the final analyses (both the study and control). There were 128/1,964 term-born infants as controls, and the rest of the children were preterm-born infants (study and control). The inclusion and exclusion criteria of the studies, the participation of mothers and fathers, the content of the interventions, and outcomes related to the parent–infant relationship were themes that were studied and are presented in Table 2.
The studies defined prematurity by gestational age (GA) and/or birth weight in these local cohorts (Table 2). In most of the studies, GA was defined simply as <37 weeks (15/22, 68.2%), but five (22.7%) of these studies excluded immature infants of <26 weeks (Melnyk et al., 2006, 2008; Beebe et al., 2018), < 28 weeks (Castel et al., 2016), and < 30 weeks (Ravn et al., 2012) of GA. However, 6/22 (27.3%) of the studies included only very preterm infants (very low birth weight or very low GA) (Brisch et al., 2003; Glazebrook et al., 2007; Van der Pal et al., 2008; Meijssen et al., 2010, 2011; Evans et al., 2017). One (4.5%) study included only extremely low GA infants (≤ 29 weeks) (Schroeder and Pridham, 2006). Moreover, 19/22 (86.4%) of the studies excluded infants because of health impairment other than prematurity (listed in Table 2; Whipple, 2000; Browne and Talmi, 2005; Kaaresen et al., 2006; Melnyk et al., 2006, 2008; Schroeder and Pridham, 2006; Glazebrook et al., 2007; Olafsen et al., 2008; van der Pal et al., 2008; Newnham et al., 2009; Meijssen et al., 2010, 2011; Nordhov et al., 2010; Ravn et al., 2012; Cho et al., 2013; Borghini et al., 2014; Castel et al., 2016; Evans et al., 2017; Beebe et al., 2018). Furthermore, 14/22 (64.0%) of the studies excluded infants and mothers if there was any adversity in the mother’s psychosocial situation (Whipple, 2000; Browne and Talmi, 2005; Melnyk et al., 2006, 2008; Schroeder and Pridham, 2006; van der Pal et al., 2008; Newnham et al., 2009; Meijssen et al., 2010, 2011; Ravn et al., 2012; Borghini et al., 2014; Castel et al., 2016; Evans et al., 2017; Beebe et al., 2018). Only a few studies systematically included fathers in the interventions (Kaaresen et al., 2006; Melnyk et al., 2006, 2008; Olafsen et al., 2008; van der Pal et al., 2008; Nordhov et al., 2010; Hoffenkamp et al., 2015b; Castel et al., 2016). Additionally, all of the studies required that parents could communicate in the official language of the country where the study was performed.
All of the interventions provided psychosocial parent–infant intervention for mothers, and the father participated in 11/22 (50%) of the studies (Table 2). Intervention was provided only during hospital stay in eight (36.4%) of the studies (i.e., seven of the interventions, 38.9%) (Browne and Talmi, 2005; Melnyk et al., 2006, 2008; Schroeder and Pridham, 2006; van der Pal et al., 2008; Hoffenkamp et al., 2015b; Beebe et al., 2018; Petteys and Adoumie, 2018). Three (13.6%) studies implemented interventions only after discharge (i.e., 2/18 interventions, 11.1%) (Meijssen et al., 2010, 2011; Borghini et al., 2014). Interventions were provided longitudinally in 12 (54.5%) of the studies (i.e., 9/18 interventions, 50.0%) (Brisch et al., 2003; Kaaresen et al., 2006; Melnyk et al., 2006, 2008; Glazebrook et al., 2007; Olafsen et al., 2008; Newnham et al., 2009; Nordhov et al., 2010; Ravn et al., 2012; Cho et al., 2013; Castel et al., 2016; Evans et al., 2017). The number of in-person sessions in the analyzed interventions varied during hospital stay, up to 10 (13/22 studies gave exact numbers, their mean number of sessions = 3.4) and after discharge, up to 22 (15/22 studies gave exact numbers, mean = 3.1). These variations in the number of intervention sessions seem to be related not only to the intervention per se but also to the health of the infant or other conditions, such as hospital transfers. Only one of the interventions lasted over a year (18 months) (Castel et al., 2016).
To gain an overview, most of the interventions based their theory on preterm infants’ need for sensitive regulation by parents (12/22 (54.5%) studies; 10/18 (55.5%) interventions) (Whipple, 2000; Browne and Talmi, 2005; Melnyk et al., 2006, 2008; Glazebrook et al., 2007; van der Pal et al., 2008; Newnham et al., 2009; Meijssen et al., 2010, 2011; Ravn et al., 2012; Beebe et al., 2018; Petteys and Adoumie, 2018). The interventions also considered one or more of the following aspects in their background and planning of the intervention: parental stress (2/22 (9.0%) studies; 2/18 (11.1%) interventions) (Glazebrook et al., 2007; Petteys and Adoumie, 2018), parental representations (1/22 (2.5%); 1/18 (5.5%)) (Schroeder and Pridham, 2006), the importance of the parent–infant relationship for the development of the child (6/22 (27.3%); 4/18 (22.2%) interventions) (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010; Cho et al., 2013; Hoffenkamp et al., 2015b; Evans et al., 2017), the parent–infant relationship in general (2/22 (9.0%); 2/18 (11.1%)) (Cho et al., 2013; Beebe et al., 2018), and multimodal psychotherapeutic theory (3/22 (13.6%) studies; 3/18 (16.7%) interventions) (Brisch et al., 2003; Borghini et al., 2014; Castel et al., 2016). In almost all the studies (19 (86.4%) of the studies and 15 (83.3%) of the interventions), the provider of the intervention was a staff member (a nurse, a physiotherapist, or a clinical psychologist) or an individual from a research team with education in intervention. Only one intervention was delivered by a psychotherapist who worked with a nurse (Brisch et al., 2003). In two studies, the provider was not clearly stated in the manuscript (Whipple, 2000; Newnham et al., 2009).
All early psychosocial parent–infant interventions were first classified into four main types: the education type included one (4.5%) intervention that was trialed twice with different outcomes; counseling included 12 interventions (67%); emotional support included three interventions (17%), in which one was trialed three times; and two interventions were classified as psychotherapy (11.1%).
One multimodal music therapy intervention (Whipple, 2000) described the intervention but did not clearly indicate the type of provider used, and we classified the study type as unclear. One (5.6%) education intervention (Melnyk et al., 2006, 2008), which was trialed twice and had three contacts before discharge and one after discharge, was implemented with written and audiotaped material only, and was classified as subtype 1. Two of the interventions (11.1%) had variation in delivery of the intervention (two different intervention groups and in others only 67% received the full protocol, and the remaining studies used other methods, e.g., phone calls and video presentations) (Browne and Talmi, 2005; Evans et al., 2017) and were therefore classified according to the lowest subtype used in the intervention, as subtype 1. We classified five (27.8% of the interventions) counseling interventions (Schroeder and Pridham, 2006; van der Pal et al., 2008; Ravn et al., 2012; Beebe et al., 2018; Petteys and Adoumie, 2018) as subtype 2 because they included up to four personal intervention sessions with individual approaches. Subtype 3 included all methods used in subtypes 1–2, in addition to providing over five sessions, being based on a specific theory, and training providers to implement the intervention, covering four counseling interventions (22.2%) (Glazebrook et al., 2007; Newnham et al., 2009; Meijssen et al., 2010, 2011; Hoffenkamp et al., 2015b). Subtype 4 offered a possibility for longer psychosocial support than in subtype 3, but for less than 6 months; there were two emotional support interventions suitable for this subtype (11.1%) (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010; Borghini et al., 2014). Subtype 5 included longer psychosocial support than in subtypes 1–4; there was one emotional support and one psychotherapy intervention that fulfilled these criteria (11.1%) (Cho et al., 2013; Castel et al., 2016). One intervention contained individual psychotherapy sessions for parents and specific parent–infant care but also multilevel support and peer support, and we classified it as subtype 6 (5.6% of the interventions) (Brisch et al., 2003).
Almost half of the studies (10/22, 46.0%) reported parent–infant relationship outcomes for both parents and child (Whipple, 2000; Kaaresen et al., 2006; Melnyk et al., 2006, 2008; Olafsen et al., 2008; van der Pal et al., 2008; Nordhov et al., 2010; Hoffenkamp et al., 2015b; Castel et al., 2016; Petteys and Adoumie, 2018), while the remaining studies reported outcomes for either mother or child only. Moreover, parent–infant relationship outcomes were studied by 30 different methods (Table 2) by observations (16/22, 76.7%) (Whipple, 2000; Brisch et al., 2003; Browne and Talmi, 2005; Melnyk et al., 2006, 2008; Schroeder and Pridham, 2006; Glazebrook et al., 2007; Newnham et al., 2009; Meijssen et al., 2010, 2011; Ravn et al., 2012; Cho et al., 2013; Borghini et al., 2014; Evans et al., 2014; Hoffenkamp et al., 2015b; Beebe et al., 2018) and/or questionnaires (19/22, 86.4%) (Whipple, 2000; Browne and Talmi, 2005; Kaaresen et al., 2006; Melnyk et al., 2006, 2008; Schroeder and Pridham, 2006; Glazebrook et al., 2007; Olafsen et al., 2008; van der Pal et al., 2008; Newnham et al., 2009; Meijssen et al., 2010, 2011; Nordhov et al., 2010; Ravn et al., 2012; Cho et al., 2013; Evans et al., 2014; Hoffenkamp et al., 2015b; Castel et al., 2016; Petteys and Adoumie, 2018). Assessments of the intervention outcomes had varying time points: during neonatal intensive care (1/22, 4.5%) (Petteys and Adoumie, 2018); straight after intervention session (2/22, 9.0%) (Whipple, 2000; Schroeder and Pridham, 2006); days to weeks after discharge (2/22, 9.0%) (Melnyk et al., 2006, 2008); 1 month after discharge (1/22, 4.5%) (Browne and Talmi, 2005); at the age of 3 months (1/22, 4.5%) (Glazebrook et al., 2007), 4 months (2/22, 9.0%) (Borghini et al., 2014; Beebe et al., 2018), 6 months (4/22, 18.2%) (Newnham et al., 2009; Meijssen et al., 2010; Ravn et al., 2012; Hoffenkamp et al., 2015b), 9 months (1/22, 4.5%) (Castel et al., 2016), 12 months (3/22, 13.6%) (van der Pal et al., 2008; Ravn et al., 2012; Evans et al., 2014), or 18 months (3/22, 13.6%) (Brisch et al., 2003; Meijssen et al., 2011; Castel et al., 2016), or 24 to 36 months of corrected age (3/22, 13.6%) (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010). Many of the studies (17/22, 77.3%) reported at least some positive change in the intervention compared to controls.
This type included only one intervention but was trialed twice by Melnyk et al. (2006, 2008). They reported results about this COPE intervention with audiovisual or written material on preterm infants and parenting. This RCT study with 260 families found a positive effect of the intervention on better interaction behavior between mother and father, mothers’ decreased stress concerning the infant and environment, and mothers’ and fathers’ better beliefs about infants compared to controls. The parent–infant outcomes were assessed during NICU care and about 1 week before discharge. The interaction behavior was measured using the Index of Parental Behavior in the NICU. The study did not include infants with very low gestational age (< 26 weeks) or severe handicapping conditions, or twins or multiples, and mothers had to be over 17 years.
This type included 12 interventions in which one intervention was trialed twice. Nine out of 13 studies (69.2%) and 8 of 12 interventions (66.7%) classified to this type reported some positive changes in the parent–infant relationship: improved parent–infant interaction (Whipple, 2000; Browne and Talmi, 2005; Newnham et al., 2009; Meijssen et al., 2010, 2011; Hoffenkamp et al., 2015b; Beebe et al., 2018), lessened parental stress (Browne and Talmi, 2005; Newnham et al., 2009; Petteys and Adoumie, 2018), improved maternal attunement to infant and adaptability (Schroeder and Pridham, 2006), or bonding and increased time spent with the infant during hospital stay (Whipple, 2000) compared to controls and assessed before or at six months or less. In three following counseling interventions, there were both positive and unchanged parent–infant relationship outcomes. In Meijssen et al.’s (2010, 2011) studies, the mothers’ behavior improved, but their representation of attachment did not change. In a study by Hoffenkamp et al. (2015a), the intervention improved sensitive behavior and bonding but not intrusive behavior or stress. In a study by Evans et al. (2017), there were no changes in observed interaction or in attachment at 6 weeks, but attachment at 12 months was better than in controls. Of these studies, 8/13 (61.5%) (Browne and Talmi, 2005; Schroeder and Pridham, 2006; Newnham et al., 2009; Meijssen et al., 2010, 2011; Hoffenkamp et al., 2015b; Beebe et al., 2018; Petteys and Adoumie, 2018) were RCT, and one of the studies (7.1%) (Whipple, 2000) was a case–control study. The size of the study cohorts varied between N = 16–112 in nine studies with positive parent–infant outcomes (Whipple, 2000; Browne and Talmi, 2005; Schroeder and Pridham, 2006; Newnham et al., 2009; Meijssen et al., 2010, 2011; Hoffenkamp et al., 2015b; Beebe et al., 2018; Petteys and Adoumie, 2018). Of these nine studies, one (11.1%) excluded very preterm (Beebe et al., 2018) and six (66.7%) sick preterm infants (Whipple, 2000; Browne and Talmi, 2005; Newnham et al., 2009; Meijssen et al., 2010, 2011; Beebe et al., 2018). and two (22.2%) mothers of young age (Browne and Talmi, 2005; Schroeder and Pridham, 2006) and four (44.4%) with health problems (Newnham et al., 2009; Meijssen et al., 2010, 2011; Beebe et al., 2018). However, three of the studies included only very preterm infants (Schroeder and Pridham, 2006; Meijssen et al., 2010, 2011). Interventions included 1–6 sessions (Whipple, 2000; Browne and Talmi, 2005; Schroeder and Pridham, 2006; Newnham et al., 2009; Hoffenkamp et al., 2015b; Petteys and Adoumie, 2018) or individually varied numbers of sessions (Beebe et al., 2018). The follow-up lasted until NICU discharge (Whipple, 2000; Petteys and Adoumie, 2018) or until one month after discharge (Browne and Talmi, 2005), 36 weeks of GA (Schroeder and Pridham, 2006), four months (Beebe et al., 2018) or six months of age (Newnham et al., 2009; Meijssen et al., 2010, 2011; Hoffenkamp et al., 2015b). Parent–infant relationship evaluation was assessed by questionnaires (Whipple, 2000; Browne and Talmi, 2005; Schroeder and Pridham, 2006; Newnham et al., 2009; Petteys and Adoumie, 2018) and observations (Whipple, 2000; Browne and Talmi, 2005; Schroeder and Pridham, 2006; Newnham et al., 2009; Meijssen et al., 2010, 2011; Hoffenkamp et al., 2015b; Beebe et al., 2018).
In total, 4/13 (30.8%) of these studies (i.e., 4/12 (33.3%) interventions) found no difference in interaction, responsiveness, attachment, or parenting stress (Glazebrook et al., 2007; van der Pal et al., 2008; Ravn et al., 2012; Evans et al., 2017) or found negative results in parent–infant relationship outcomes in parenting stress, how the mother experienced the infant, and maternal attachment (Ravn et al., 2012; Evans et al., 2017). The cohorts included 106–242 parent–infant pairs. In the studies with negative or no difference, all four studies excluded sick preterm infants (Glazebrook et al., 2007; van der Pal et al., 2008; Ravn et al., 2012; Evans et al., 2017), and in 3/4 (75%) of the studies mothers with health issues were excluded (van der Pal et al., 2008; Ravn et al., 2012; Evans et al., 2017). However, three (75%) of the studies included only very preterm infants (Glazebrook et al., 2007; van der Pal et al., 2008; Evans et al., 2017). The interventions included seven (Ravn et al., 2012) or varying numbers of intervention sessions (Glazebrook et al., 2007; van der Pal et al., 2008) or had no-person but material delivery (Evans et al., 2017). The follow-up lasted until 3 months in one study (Glazebrook et al., 2007) and about 12 months of age of the child in the remaining three studies (75%) (van der Pal et al., 2008; Ravn et al., 2012; Evans et al., 2017). Outcomes were evaluated by questionnaire in all four studies (Glazebrook et al., 2007; van der Pal et al., 2008; Ravn et al., 2012; Evans et al., 2017) and by observation of the parent–infant relationship in three-quarters of the studies (Glazebrook et al., 2007; Ravn et al., 2012; Evans et al., 2017).
This type included three different interventions in which one was trialed three times. All of the studies and interventions in this group (100%) had a positive result in parent–infant relationship outcomes (in sensitivity of mother, co-operation of the infant, interaction, less stress, and attitudes toward the infant) among 4- and 24-month-old children (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010; Cho et al., 2013; Borghini et al., 2014). In one study, there were positive changes in observed interactions but no changes in parental stress (Cho et al., 2013). Three out of five of these studies (60%) (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010; Borghini et al., 2014) were RCT and one (Cho et al., 2013) was a case–control study. The size of the study cohorts varied between 66 and 214. All five studies excluded unhealthy preterm infants (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010; Cho et al., 2013; Borghini et al., 2014) but included all gestational ages, and 4/5 of the studies excluded mothers with young age or health problems (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010; Borghini et al., 2014). The number of intervention sessions varied between five and six (Cho et al., 2013; Borghini et al., 2014), and there were more sessions at home after discharge (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010). The follow-up period varied from 4 to 36 months of age. The parent–infant relationship was assessed by questionnaires in 4/5 of the studies (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010; Cho et al., 2013) and by observation in 2/5 of the studies (Cho et al., 2013; Borghini et al., 2014).
This type included two different interventions and separate studies. One study (50%) found a positive correlation to the parent–infant relationship (Castel et al., 2016). Parents in this study (Castel et al., 2016) reported less stress after intervention at 18 months than those in the control group. There was no other parent–infant relationship outcome measure in this study. The study included 84 parent–infant pairs; the infants were preterm (GA 28–36 weeks, excluding the most preterm infants) without congenital anomaly or other disability, and the mothers were over 18 years, without psychiatric disease. This high-frequency intervention (22 sessions) aimed to improve triadic relationships through parental stress alleviation, supporting their confidence and emotional expression and parents in the control group. In a study by Brisch et al. (2003), there were 87 parent–infant pairs; the infants were only very preterm (<1,500 grams and GA ≤ 35 weeks), surviving beyond the intervention. This multimodal psychotherapeutic intervention included group therapy, individual attachment-oriented psychotherapy sessions for mother and father, one home intervention session to promote parental self-compliance within 1 week after discharge, and, at 3 months, parental sensitivity training for infants’ cues. The mother’s attachment to the infant was evaluated at 14 months. There were no differences between controls and mothers in the intervention (Brisch et al., 2003).
The aim of this scoping review was to provide structured knowledge of early psychosocial parent–infant interventions that seek to promote parent–infant relationships after preterm birth. We also aimed to summarize the evidence considering parent–infant relationships and identify potential gaps in existing interventions and/or in the used outcomes. Previous reviews on psychosocial parent–infant interventions have shown heterogeneity (Benzies et al., 2013; Evans et al., 2014; Givrad et al., 2021) but have not provided answers on how the variation in psychosocial parent–infant interventions could be understood.
To analyze and impose a structure on the content of the interventions, we classified the studied interventions into four main types and six subtypes, adapting existing intervention classification models, namely the International Classification for Health Interventions (ICHI) by the World Health Organization and the Template for Intervention Description and Replication (TIDieR) checklist for better reporting of interventions. Based on the classification, the most common type of early psychosocial parent–infant intervention to influence parenting behavior was found to be counseling, followed by emotional support. The least common types were psychotherapy for parenting behavior and education to influence parental behavior. Positive intervention effects on the parent–infant relationship were reported in 16 of 22 studies, particularly in single education (Melnyk et al., 2006, 2008), in 8/13 of the counseling interventions (Whipple, 2000; Browne and Talmi, 2005; Schroeder and Pridham, 2006; Newnham et al., 2009; Meijssen et al., 2010, 2011; Hoffenkamp et al., 2015b; Beebe et al., 2018; Petteys and Adoumie, 2018), in 3/3 of the emotional support interventions in which one was trialed three times (Kaaresen et al., 2006; Olafsen et al., 2008; Nordhov et al., 2010; Cho et al., 2013; Borghini et al., 2014), and in 1/2 of the psychotherapy interventions (Castel et al., 2016). Our results are in line with earlier studies on the positive outcomes of parental interventions (Benzies et al., 2013; Evans et al., 2014).
ICHI definitions of different types of early parent–infant psychosocial interventions were applied to the practice with preterm infants, and the following examples are from analyzed and classified interventions. These were applicable to intervention targeted at preterm infants and their parents. Education interventions concentrated on educating parents of the typical characteristics in preterm infants and how parents can participate in their infants’ care. Counseling about parenting behavior provided individual observations and guidance for parents on how to see cues in their own preterm infant and how to consider cues when interacting with their child. Emotional support for parenting behavior promoted parents’ mental health and parent–infant interaction and psychotherapy for parenting behavior focused on dyadic/triadic relationships through emotional sharing, supporting relationships and the mental health of parents, and promoting understanding of the infant’s development. Psychotherapeutic elements such as individual or group sessions were offered to deal with experiences during the birth of the child or an individual’s own childhood.
This study included 22 studies with 18 different early psychosocial parent–infant interventions, in which about half were implemented longitudinally, starting on the NICU and lasting after discharge. The studies used 30 different outcome measures of the parent–infant relationship, measured mainly after hospital discharge (21/22) and up to 18 months of age.
We identified multiple gaps in studies on early psychosocial parent–infant interventions, especially those related to the populations included in the interventions. In total, 86.4% of the studies excluded parent–infant pairs because of some health impairment in the infant (Whipple, 2000; Browne and Talmi, 2005; Kaaresen et al., 2006; Melnyk et al., 2006, 2008; Schroeder and Pridham, 2006; Glazebrook et al., 2007; Olafsen et al., 2008; van der Pal et al., 2008; Newnham et al., 2009; Meijssen et al., 2010, 2011; Nordhov et al., 2010; Ravn et al., 2012; Cho et al., 2013; Borghini et al., 2014; Castel et al., 2016; Evans et al., 2017; Beebe et al., 2018) and/or health or other adverse sociological risk in the mother (64.0%) (Whipple, 2000; Browne and Talmi, 2005; Melnyk et al., 2006, 2008; Schroeder and Pridham, 2006; van der Pal et al., 2008; Newnham et al., 2009; Meijssen et al., 2010, 2011; Ravn et al., 2012; Borghini et al., 2014; Castel et al., 2016; Evans et al., 2017; Beebe et al., 2018). Thus, the effectiveness of most the intervention is not studied with the preterm infants and their parents with high or multiple risk factors. In future intervention studies these groups would require more attention, because typically multiple risk factor exposure is more harmful than singular risk exposure for child development (Evans et al., 2013; Leppänen et al., 2023). Further, all of the studies required parents to be able to communicate in the official language of the country where the study was performed, thereby likely excluding recently immigrated populations. Fathers were not evaluated for inclusion criteria as mothers, which may be one of the explanations why mothers and fathers seemed to benefit differently from the interventions.
In the reviewed interventions, there were extreme but also moderate preterm infants, which may have influenced the results. The environment (neonatal intensive care unit) where preterm infants may be for quite a long time before discharge may be a challenge for psychosocial care. A need for other treatments and the transfer of infants was reported to affect implementation in some interventions (Newnham et al., 2009; Evans et al., 2017), and these kinds of prematurity and intensive care-related factors may have resulted in the observed variations in the number of sessions implemented. In 18 individual interventions, there were 30 different parent–infant outcome measures at varying age points of the infants, which makes comparison of the results difficult. In these studies, the parent–infant outcomes were often not the primary outcomes of the studies and therefore likely to be underpowered. In the future, the power of parent-infant outcomes should be considered when designing an intervention study and at least adequately discussed in the reports. Evans et al. (2014) described the contents of early psychosocial intervention and statistically compared outcome variables between study and control groups. They found that part of the interventions, especially those with education/counseling of cues and how to interact with infants, seemed to be beneficial for parent–infant relationships. However, both interventions and outcome methods, as well as follow-up times, have varied strongly in reviewed and earlier studies, details have been missing, and numbers have been small in studies, leaving uncertainties (Benzies et al., 2013; Givrad et al., 2021). A recent systematic review by Lavallée et al. (2021) on early parenting intervention after preterm birth on parental sensitivity and parental stress before and after 6 months of age found mostly low or very low quality of evidence. They discussed that this could be explained by implementation failure, risk of bias, the small number of participants, and substantial heterogeneity (Lavallée et al., 2021), which is in line with our observations.
The most common type of early psychosocial parent–infant intervention in our study was counseling about parenting behavior (13/22 of the studies and 12/18 of the interventions). This kind of intervention provides therapeutic and/or supportive communication in relation to behavior concerning patterns of interaction between a parent and their child/children. Nine out of 13 (69.2%) studies of the counseling type reported some significant effects on the parent–infant relationship (improvements in parent–infant interaction bonding, less parental stress, increased time spent with the child during hospital stay compared to controls), with outcomes assessed within the first 6 months of infant age. The remaining 4 of 13 studies and of 12 interventions did not report any positive intervention effects. The studies with less positive outcome results seemed to differ in that they had larger cohorts and longer follow-ups compared to studies with positive outcomes. Two of the studies with counseling interventions excluded very preterm infants, and six included only this population. Based on the subtype categories, it appears that the moderate-dose counseling interventions (subtypes 1 to 3) had a positive but maybe short effect on the parent–infant relationship. However, among the counseling interventions, intervention components, such as the amount of training/supervision of the intervention providers or the length of the intervention, did not seem to influence the results. This is interesting but may be explained by missing information about the extent to which the participants receive the intervention as intended. Intervention studies in the future, even those using an RCT design, should monitor adherence during the intervention delivery and report it (Giovanazzi et al., 2022). In three counseling interventions (in addition to one emotional intervention) that included several different measures and age points, only some of the outcomes were positive for the intervention (Meijssen et al., 2010, 2011; Hoffenkamp et al., 2015b; Evans et al., 2017). It would be important for further studies to identify the measures that are sensitive for measuring the effect of a short counseling intervention on the parent–infant relationship. Furthermore, it is important to report negative results to avoid intervention causing harmful effects.
The next most common intervention type found was emotional support to influence parenting, caretaking, or interaction, where 5/5 and 3/3 of individual interventions and studies had a positive result in parent–infant relationship outcome (e.g., improvements in maternal sensitivity, co-operation skill of the child, interaction, less parenting stress, and attitudes toward the child) assessed between 4 and 24 months of age. Emotional support provides comfort, empathy, or motivational support to the person regarding behavior concerning patterns of interaction between a parent and their child/children. Many of the emotional support interventions included the possibility of more intense and/or longer-lasting psychosocial support than the counseling interventions did (Subtype 4). All interventions included also sessions after discharge, and also very and extreme preterm infants were included to these emotional interventions. Furthermore, all emotional support interventions included providers who received education for intervention delivery. The providers, if they were staff members, also collaborated or were supported by a specialist, such as a psychologist. NICU staff have reported that they experience the provision of emotional support to parents as a demanding task (Turner et al., 2014). Therefore, it is crucial to have a specialist with appropriate education who can collaborate on or support the delivery of parenting interventions with emotional support. Although some studies have reported less stress, one of the studies did not find an intervention effect on parenting stress (Cho et al., 2013). The outcomes were assessed between 4 and 36 months of the child’s age, utilizing mostly RCT study designs and relative sample sizes. Based on this scoping review, all interventions classified as emotional support interventions were all shown to be effective. However, we cannot conclude why these interventions were all effective. Thus, our conclusion is that there is a need for studies that compare different types of interventions rather than only studying the effect of one intervention at a time. Furthermore, the active ingrediencies of the interventions should be reported in detail and impact mechanisms of interventions studied, not only the outcomes.
Less common intervention types were education and psychotherapy, with 2/22 (9.0%) of the studies and 2/18 (7.7%) of the interventions being psychotherapy and 1/18 (5.5%) being education-based. Education aims to improve knowledge to influence behavior concerning patterns of interaction between a parent and their child/children, including the nature and degree of monitoring and supervision, involvement and engagement, discipline, nurturing, and the expression of affection. An education intervention study by Melnyk et al. (2006, 2008) delivered education materials to parents but had a positive effect on parent–infant interaction as it diminished stress and improved parents’ representations of their child/children at 1 week before discharge. Unfortunately, no later outcomes were reported. This intervention also excluded most preterm infants. One of two psychotherapy interventions by Castel et al. (2016) reported less parental stress when a child was 18 months old. There were no other outcomes assessed, although that intervention lasted until 18 months and with an educated provider and background theory of the interventions to improve triadic relationships (between mother, father, and infant). Thus, the quality of the parent–infant or triadic interaction was not evaluated as an outcome in the study. In another psychotherapeutic intervention study by Brisch et al. (2003), only the attachment quality of the child was evaluated after a very multimodal intervention that could have also eased parental stress and anxiety, and improved parental representations, which were evaluated in other studies. Although child attachment was a well-founded choice for the main outcome of this intervention with an attachment-oriented approach, the narrow choice of outcomes may leave invisible some of the important effects. This study found that effect was only present in a subgroup of preterm infants, those with neurologic delay seemed to benefit from the intervention (Brisch et al., 2003). Both psychotherapeutic interventions included only very preterm infants, although not extremely preterm infants (< 28 weeks) (Castel et al., 2016). It may be that preterm infants and their parents with comorbidities, psychotherapeutic interventions are appropriate.
We found some constraints in the reviewed studies that may affect the generalization of the results. We do not know how the exclusion of mothers and infants with additional risks has influenced the studied outcome. However, some of the different intervention types showed that some subgroups benefited more from interventions than other parents in the study. Hoffenkamp et al. (2015a) reported that mothers who were traumatized benefited more from video-based interaction guidance than those who were not. And above discussed finding by Brisch et al. (2003), that if an infant had a neurological impairment, intervention improved maternal attachment, which is line with earlier results on attachment study By Korja et al. (2012) on preterm infants and parents. Prematurity per se might not be a risk for attachment. Overall, future interventions should pay more attention to subgroups of preterm infants and parents who may be at even greater risk of parent–infant relationship problems than preterm infants and parents without comorbidities. Previous reviews have also recommended the identification of families at risk (Benzies et al., 2013; Evans et al., 2014; Givrad et al., 2021). Psychosocial risks are known to accumulate in families with preterm infants and influence the outcomes of preterm-born children (Schothorst et al., 2007; Nosarti et al., 2012; Leppänen et al., 2023). However, adequate parent–infant emotional interaction can be protective (Yrjölä et al., 2022). Therefore, when infants and parents with cumulative risks are included in intervention trials, interventions should be tailored to meet the different and probably targeted needs of the families.
The included studies used over 30 different outcome measures; some seemed to fit well with the content of the intervention, while others did not. Pilot studies should be used to identify the sensitive outcomes of an intervention to ensure a better choice of outcomes. Standardized outcome sets could also be co-created between researchers and parents. Only 5/18 (Kaaresen et al., 2006; Glazebrook et al., 2007; Olafsen et al., 2008; Meijssen et al., 2010, 2011; Nordhov et al., 2010; Hoffenkamp et al., 2015b) of the interventions clearly reported the parent–infant relationship outcome as the primary outcome in their study. Another identified gap in previous research is related to the lack of knowledge about the intervention’s effects on fathers. In the future, the inclusion of fathers in the intervention studies should be encouraged, and the content of the intervention should be modified based on existing knowledge about early fatherhood. Further, the intervention effect on the father–infant relationship could be analyzed separately in a review.
Our goal was to include various types of interventions in this scoping review; however, our inclusion criteria, as stipulated in the study methodology, necessitated the exclusion of many interventions, which might have influenced the overall picture of early parental interventions. As we aimed to scope the field broadly and to identify existing gaps, we did not follow any specific quality assessment tool for the inclusion of studies. This may have influenced our observations.
We could not extract all details from a few manuscripts for classification, even though we searched the data—for example, we searched earlier publications on the intervention—and this might have influenced how we classified the interventions. As there were no readily available classification systems, our system provides a pilot for the development of other classifications in future studies. We excluded interventions that included only skin-to-skin care to concentrate more on psychological support. Skin-to-skin care per se has been reported as beneficial for parents and infants (Neu and Robinson, 2010; Holditch-Davis et al., 2014). We used only PubMed and PsycINFO as data sources; extension to other databases and gray literature could have expanded the picture of what kind of early psychosocial parent–infant interventions there might be. For example, in a recent complementary search we identified new types of interventions, including online/app-based interventions for parents, but these were excluded. Generally, this study could not consider other social and health care services offered to families in each NICU, hospital district, and community that might supplement interventions but were not studied in this scoping review. In the future, there is a need to describe all levels of support in different phases and environments. This field has no established terms (i.e., types and subtypes), and we used new terms compared to earlier reviews (Benzies et al., 2013; Evans et al., 2014).
This scoping review study provided systematic information on studies of early psychosocial parent–infant intervention in the context of neonatal intensive care. The included interventions were classified using the ICHI, provided by the World Health Organization, and their implementation was evaluated using the TIDieR structure for reporting interventions. The most common intervention types in the studies were consultation about parenting and emotional support for parenting. Psychotherapy and education intervention types were less common. All types of interventions were shown to be beneficial for the parent–infant relationship, particularly in populations of preterm infants, without accumulating risk factors and with short-term follow-up times. But we think that in future studies, it would be of great benefit to conduct fidelity analyses of the intervention delivery (Ibrahim and Sidani, 2016) to understand how well the intervention succeeded.
Due to the heterogeneity of the outcomes and interventions used, it is hard to make comparisons between the interventions. To obtain reliable and comparable data, standardized study protocols (e.g., time of measurement and length of follow-up) and outcome measures are needed in the future. It would be important to have a long-term follow-up to study whether early outcomes are maintained. For example, synchronicity between child and parent may be a potential stable factor to measure (Feldman, 2012). The biomarkers of parenting could also be interesting proximal outcomes of parenting interventions in NICU context (Hajal and Loo, 2021). There is also a need for more intervention studies that include subpopulations of preterm infants and their parents with accumulating risks. However, it is important to carefully consider the type of intervention that is appropriate for these subpopulations. It may be that emotional support and psychotherapeutic types of interventions involving multiprofessional collaboration are more likely to be beneficial for families with accumulation risks than education or consultation. This study may help NICU professionals understand the differences between various psychosocial interventions for parenting. It may also have implications for the development of health care services for families with preterm infants.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
ML: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. RK: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. PR: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. SA-B: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. ML received study funding from the Finnish Brain Foundation and the Foundation for Pediatrics Research and Social Affairs and Health of Finland. The funders had no role in the design and conduct of the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Aarnoudse-Moens, C. S. H., Weisglas-Kuperus, N., Duivenvoorden, H. J., Oosterlaan, J., and van Goudoever, J. B. (2013). Neonatal and parental predictors of executive function in very preterm children. Acta Paediatr. 102, 282–286. doi: 10.1111/apa.12101
Aarnoudse-Moens, C. S. H., Weisglas-Kuperus, N., van Goudoever, J. B., and Oosterlaan, J. (2009). Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 124, 717–728. doi: 10.1542/peds.2008-2816
Alenius, S., Kajantie, E., Sund, R., Nurhonen, M., Näsänen-Gilmore, P., Vääräsmäki, M., et al. (2020). Out-of-home care placements of children and adolescents born preterm: a register-based cohort study. Paediatr. Perinat. Epidemiol. 34, 38–47. doi: 10.1016/j.jpeds.2022.09.032
Arpi, E., and Ferrari, F. (2013). Preterm birth and behaviour problems in infants and preschool-age children: a review of the recent literature. Dev. Med. Child Neurol. 55, 788–796. doi: 10.1111/dmcn.12142
Athalye-Jape, G., Lim, M., Nathan, E., and Sharp, M. (2022). Outcomes in extremely low birth weight (≤500 g) preterm infants: a Western Australian experience. Early Hum. Dev. 167:105553. doi: 10.1016/j.earlhumdev.2022.105553
Baum, N., Weidberg, Z., Osher, Y., and Kohelet, D. (2012). No longer pregnant, not yet a mother: giving birth prematurely to a very-low-birth-weight baby. Qual. Health Res. 22, 595–606. doi: 10.1177/1049732311422899
Beebe, B., Myers, M. M., Lee, S. H., Lange, A., Ewing, J., Rubinchik, N., et al. (2018). Family nurture intervention for preterm infants facilitates positive mother–infant face-to-face engagement at 4 months. Dev. Psychol. 54, 2016–2031. doi: 10.1037/dev0000557
Benzies, K. M., Magill-Evans, J. E., Hayden, K., and Ballantyne, M. (2013). Key components of early intervention programs for preterm infants and their parents: a systematic review and meta-analysis. BMC Pregnancy Childbirth 13:S10. doi: 10.1186/1471-2393-13-S1-S10
Bhutta, A. T., Cleves, M. A., Casey, P. H., Cradock, M. M., and Anand, K. J. S. (2002). Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA 288:728. doi: 10.1001/jama.288.6.728
Borghini, A., Habersaat, S., Forcada-Guex, M., Nessi, J., Pierrehumbert, B., Ansermet, F., et al. (2014). Effects of an early intervention on maternal post-traumatic stress symptoms and the quality of mother–infant interaction: the case of preterm birth. Infant Behav. Dev. 37, 624–631. doi: 10.1016/j.infbeh.2014.08.003
Brisch, K. H., Bechinger, D., Betzler, S., and Heinemann, H. (2003). Early preventive attachment-oriented psychotherapeutic intervention program with parents of a very low birthweight premature infant: results of attachment and neurological development. Attach Hum. Dev. 5, 120–135. doi: 10.1080/1461673031000108504
Browne, J. V., and Talmi, A. (2005). Family-based intervention to enhance infant–parent relationships in the neonatal intensive care unit. J. Pediatr. Psychol. 30, 667–677. doi: 10.1093/jpepsy/jsi053
Burnett, A. C., Anderson, P. J., Cheong, J., Doyle, L. W., Davey, C. G., and Wood, S. J. (2011). Prevalence of psychiatric diagnoses in preterm and full-term children, adolescents, and young adults: a meta-analysis. Psychol. Med. 41, 2463–2474. doi: 10.1017/S003329171100081X
Castel, S., Creveuil, C., Beunard, A., Blaizot, X., Proia, N., and Guillois, B. (2016). Effects of an intervention program on maternal and paternal parenting stress after preterm birth: a randomized trial. Early Hum. Dev. 103, 17–25. doi: 10.1016/j.earlhumdev.2016.05.007
Castelpietra, G., Salvador-Carulla, L., Almborg, A.-H., Fernandez, A., and Madden, R. (2017). Working draft: classifications of interventions in mental health care. An expert review. Eur. J. Psychiatry 31, 127–144. doi: 10.1016/j.ejpsy.2017.10.001
Cho, Y., Hirose, T., Tomita, N., Shirakawa, S., Murase, K., Komoto, K., et al. (2013). Infant mental health intervention for preterm infants in Japan: promotions of maternal mental health, mother–infant interactions, and social support by providing continuous home visits until the corrected infant age of 12 months. Infant Ment. Health J. 34, 47–59. doi: 10.1002/imhj.21352
Clark, C. A. C., Woodward, L. J., Horwood, L. J., and Moor, S. (2008). Development of emotional and behavioral regulation in children born extremely preterm and very preterm: biological and social influences. Child Dev. 79, 1444–1462. doi: 10.1111/j.1467-8624.2008.01198.x
D’Onofrio, B. M., Class, Q. A., Rickert, M. E., Larsson, H., Långström, N., and Lichtenstein, P. (2013). Preterm birth and mortality and morbidity: a population-based quasi-experimental study. JAMA Psychiatry 70:1231. doi: 10.1001/jamapsychiatry.2013.2107
Elgen, S. K., Leversen, K. T., Grundt, J. H., Hurum, J., Sundby, A. B., Elgen, I. B., et al. (2012). Mental health at 5 years among children born extremely preterm: a national population-based study. Eur. Child Adolesc. Psychiatry 21, 583–589. doi: 10.1007/s00787-012-0298-1
Evans, T., Boyd, R. N., Colditz, P., Sanders, M., and Whittingham, K. (2017). Mother-very preterm infant relationship quality: RCT of baby triple P. J. Child Fam. Stud. 26, 284–295. doi: 10.1007/s10826-016-0555-x
Evans, G. W., Li, D., and Whipple, S. S. (2013). Cumulative risk and child development. Psychol. Bull. 139, 1342–1396. doi: 10.1037/a0031808
Evans, T., Whittingham, K., Sanders, M., Colditz, P., and Boyd, R. N. (2014). Are parenting interventions effective in improving the relationship between mothers and their preterm infants? Infant Behav. Dev. 37, 131–154. doi: 10.1016/j.infbeh.2013.12.009
Faure, N., Habersaat, S., Harari, M. M., Müller-Nix, C., Borghini, A., Ansermet, F., et al. (2017). Maternal sensitivity: a resilience factor against internalizing symptoms in early adolescents born very preterm? J. Abnorm. Child Psychol. 45, 671–680. doi: 10.1007/s10802-016-0194-0
Feldman, R. (2012). Parent-infant synchrony: a biobehavioral model of mutual influences in the formation of affiliative bonds: parent–infant synchrony. Monogr. Soc. Res. Child Dev. 77, 42–51. doi: 10.1111/j.1540-5834.2011.00660.x
Forcada-Guex, M., Borghini, A., Pierrehumbert, B., Ansermet, F., and Muller-Nix, C. (2011). Prematurity, maternal posttraumatic stress and consequences on the mother–infant relationship. Early Hum. Dev. 87, 21–26. doi: 10.1016/j.earlhumdev.2010.09.006
Gerstein, E. D., Njoroge, W. F. M., Paul, R. A., Smyser, C. D., and Rogers, C. E. (2019). Maternal depression and stress in the neonatal intensive care unit: associations with mother−child interactions at age 5 years. J. Am. Acad. Child Adolesc. Psychiatry 58, 350–358.e2. doi: 10.1016/j.jaac.2018.08.016
Gerstein, E. D., and Poehlmann-Tynan, J. (2015). Transactional processes in children born preterm: influences of mother-child interactions and parenting stress. J. Fam. Psychol. 29, 777–787. doi: 10.1037/fam0000119
Giovanazzi, A., Jones, K., Carr, R. M., Fairhurst, C. M., Backhouse, M. R., and Adamson, J. A. (2022). Current practice in the measurement and interpretation of intervention adherence in randomised controlled trials: a systematic review. Contemp. Clin. Trials 118:106788. doi: 10.1016/j.cct.2022.106788
Givrad, S., Hartzell, G., and Scala, M. (2021). Promoting infant mental health in the neonatal intensive care unit (NICU): a review of nurturing factors and interventions for NICU infant-parent relationships. Early Hum. Dev. 154:105281. doi: 10.1016/j.earlhumdev.2020.105281
Glazebrook, C., Marlow, N., Israel, C., Croudace, T., Johnson, S., White, I. R., et al. (2007). Randomised trial of a parenting intervention during neonatal intensive care. Arch. Dis. Child Fetal Neonatal Ed. 92, F438–F443. doi: 10.1136/adc.2006.103135
Gross, S. J., Mettelman, B. B., Dye, T. D., and Slagle, T. A. (2001). Impact of family structure and stability on academic outcome in preterm children at 10 years of age. J. Pediatr. 138, 169–175. doi: 10.1067/mpd.2001.111945
Hajal, N. J., and Loo, S. K. (2021). Emerging biomarkers for child & family intervention studies: a review of EEG studies of parenting. Biol. Psychol. 166:108200. doi: 10.1016/j.biopsycho.2021.108200
Hoffenkamp, H. N., Braeken, J., Hall, R. A. S., Tooten, A., Vingerhoets, A. J. J. M., and van Bakel, H. J. A. (2015a). Parenting in complex conditions: does preterm birth provide a context for the development of less optimal parental behavior? J. Pediatr. Psychol. 40, 559–571. doi: 10.1093/jpepsy/jsv007
Hoffenkamp, H. N., Tooten, A., Hall, R. A. S., Braeken, J., Eliëns, M. P. J., Vingerhoets, A. J. J. M., et al. (2015b). Effectiveness of hospital-based video interaction guidance on parental interactive behavior, bonding, and stress after preterm birth: a randomized controlled trial. J. Consult. Clin. Psychol. 83, 416–429. doi: 10.1037/a0038401
Hoffmann, T. C., Glasziou, P. P., Boutron, I., Milne, R., Perera, R., Moher, D., et al. (2014). Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 348:g1687. doi: 10.1136/bmj.g1687
Holditch-Davis, D., White-Traut, R. C., Levy, J. A., O’Shea, T. M., Geraldo, V., and David, R. J. (2014). Maternally administered interventions for preterm infants in the NICU: Effects on maternal psychological distress and mother–infant relationship. Infant Behav. Dev. 37, 695–710. doi: 10.1016/j.infbeh.2014.08.005
Ibrahim, S., and Sidani, S. (2016). Intervention fidelity in interventions: an integrative literature review. Res. Theory Nurs. Pract. 30, 258–271. doi: 10.1891/1541-6577.30.3.258
Ionio, C., Lista, G., Mascheroni, E., Olivari, M. G., Confalonieri, E., Mastrangelo, M., et al. (2017). Premature birth: complexities and difficulties in building the mother-child relationship. J. Reprod. Infant Psychol. 35, 509–523. doi: 10.1080/02646838.2017.1383977
Johnson, S., and Marlow, N. (2013). Growing up after extremely preterm birth: lifespan mental health outcomes. Semin. Fetal Neonatal Med. 19, 97–104. doi: 10.1016/j.siny.2013.11.004
Jotzo, M., and Poets, C. F. (2005). Helping parents cope with the trauma of premature birth: an evaluation of a trauma-preventive psychological intervention. Pediatrics 115, 915–919. doi: 10.1542/peds.2004-0370
Kaaresen, P. I., Ronning, J. A., Ulvund, S. E., and Dahl, L. B. (2006). A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics (Evanston) 118, e9–e19. doi: 10.1542/peds.2005-1491
Korja, R., Latva, R., and Lehtonen, L. (2012). The effects of preterm birth on mother-infant interaction and attachment during the infant’s first two years. Acta Obstet. Gynecol. Scand. 91, 164–173. doi: 10.1111/j.1600-0412.2011.01304.x
Krugers, H. J., Arp, J. M., Xiong, H., Kanatsou, S., Lesuis, S. L., Korosi, A., et al. (2017). Early life adversity: lasting consequences for emotional learning. Neurobiol. Stress 6, 14–21. doi: 10.1016/j.ynstr.2016.11.005
Landsem, I. P., Handegård, B. H., Tunby, J., Ulvund, S. E., and Rønning, J. A. (2014). Early intervention program reduces stress in parents of preterms during childhood: a randomized controlled trial. Trials 15:387. doi: 10.1186/1745-6215-15-387
Landsem, I. P., Handegård, B. H., and Ulvund, S. E. (2020). Temperamental development among preterm born children. An RCT follow-up study. Children 7:36. doi: 10.3390/children7040036
Larroque, B., Ancel, P.-Y., Marret, S., Marchand, L., André, M., Arnaud, C., et al. (2008). Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): A longitudinal cohort study. Lancet 371, 813–820. doi: 10.1016/S0140-6736(08)60380-3
Lavallée, A., De Clifford-Faugère, G., Ballard, A., and Aita, M. (2021). Parent–infant interventions to promote parental sensitivity during NICU hospitalization: systematic review and meta-analysis. J. Early Interv. 43, 361–382. doi: 10.1177/1053815121991928
Leppänen, M., Pape, B., Ripatti, L., Karukivi, M., Haataja, L., and Rautava, P. (2023). Burden of mental, behavioral, and neurodevelopmental disorders in the Finnish most preterm children: a national register study. Eur. Child Adolesc. Psychiatry 2023:2172. doi: 10.1007/s00787-023-02172-1
Meijssen, D., Wolf, M.-J., Koldewijn, K., Houtzager, B. A., van Wassenaer, A., Tronick, E., et al. (2010). The effect of the infant behavioral assessment and intervention program on mother-infant interaction after very preterm birth: effect of an early intervention on mother-infant interaction after very preterm birth. J. Child Psychol. Psychiatry 51, 1287–1295. doi: 10.1111/j.1469-7610.2010.02237.x
Meijssen, D., Wolf, M.-J., van Bakel, H., Koldewijn, K., Kok, J., and van Baar, A. (2011). Maternal attachment representations after very preterm birth and the effect of early intervention. Infant Behav. Dev. 34, 72–80. doi: 10.1016/j.infbeh.2010.09.009
Melnyk, B. M., Crean, H. F., Feinstein, N. F., and Fairbanks, E. (2008). Maternal anxiety and depression after a premature infant’s discharge from the neonatal intensive care unit: explanatory effects of the creating opportunities for parent empowerment program. Nurs. Res. 57, 383–394. doi: 10.1097/NNR.0b013e3181906f59
Melnyk, B. M., Feinstein, N. F., Alpert-Gillis, L., Fairbanks, E., Crean, H. F., Sinkin, R. A., et al. (2006). Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the creating opportunities for parent empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics 118, e1414–e1427. doi: 10.1542/peds.2005-2580
Miceli, P. J. (2000). Brief report: birth status, medical complications, and social environment: individual differences in development of preterm, very low birth weight infants. J. Pediatr. Psychol. 25, 353–358. doi: 10.1093/jpepsy/25.5.353
Miles, M. S., and Holditch-Davis, D. (1997). Parenting the prematurely born child: pathways of influence. Semin. Perinatol. 21, 254–266. doi: 10.1016/S0146-0005(97)80067-5
Muller-Nix, C., and Forcada-Guex, M. (2009). Perinatal assessment of infant, parents, and parent-infant relationship: prematurity as an example. Child Adolesc. Psychiatr. Clin. N. Am. 18, 545–557. doi: 10.1016/j.chc.2009.02.008
Neu, M., and Robinson, J. (2010). Maternal holding of preterm infants during the early weeks after birth and dyad interaction at six months. J Obstet Gynecol Neonatal Nurs 39, 401–414. doi: 10.1111/j.1552-6909.2010.01152.x
Newnham, C. A., Milgrom, J., and Skouteris, H. (2009). Effectiveness of a modified mother–infant transaction program on outcomes for preterm infants from 3 to 24 months of age. Infant Behav. Dev. 32, 17–26. doi: 10.1016/j.infbeh.2008.09.004
Nordhov, S. M., Kaaresen, P. I., Rønning, J. A., Ulvund, S. E., and Dahl, L. B. (2010). A randomized study of the impact of a sensitizing intervention on the child-rearing attitudes of parents of low birth weight preterm infants. Scand. J. Psychol. 2010:805. doi: 10.1111/j.1467-9450.2009.00805.x
Nosarti, C., Reichenberg, A., Murray, R. M., Cnattingius, S., Lambe, M. P., Yin, L., et al. (2012). Preterm birth and psychiatric disorders in young adult life. Arch. Gen. Psychiatry 69:1374. doi: 10.1001/archgenpsychiatry.2011.1374
Olafsen, K. S., Kaaresen, P. I., Handegård, B. H., Ulvund, S. E., Dahl, L. B., and Rønning, J. A. (2008). Maternal ratings of infant regulatory competence from 6 to 12 months: influence of perceived stress, birth-weight, and intervention. Infant Behav. Dev. 31, 408–421. doi: 10.1016/j.infbeh.2007.12.005
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Petteys, A. R., and Adoumie, D. (2018). Mindfulness-based neurodevelopmental care: impact on NICU parent stress and infant length of stay; a randomized controlled pilot study. Adv. Neonatal Care 18, E12–E22. doi: 10.1097/ANC.0000000000000474
Puthussery, S., Chutiyami, M., Tseng, P. C., Kilby, L., and Kapadia, J. (2018). Effectiveness of early intervention programs for parents of preterm infants: A meta-review of systematic reviews. BMC Pediatrics 18:223. doi: 10.1186/s12887-018-1205-9
Ravn, I. H., Smith, L., Smeby, N. A., Kynoe, N. M., Sandvik, L., Bunch, E. H., et al. (2012). Effects of early mother–infant intervention on outcomes in mothers and moderately and late preterm infants at age 1 year: a randomized controlled trial. Infant Behav. Dev. 35, 36–47. doi: 10.1016/j.infbeh.2011.09.006
Schothorst, P. F., Swaab-Barneveld, H., and van Engeland, H. (2007). Psychiatric disorders and MND in non-handicapped preterm children: prevalence and stability from school age into adolescence. Eur. Child Adolesc. Psychiatry 16, 439–448. doi: 10.1007/s00787-007-0617-0
Schroeder, M., and Pridham, K. (2006). Development of relationship competencies through guided participation for mothers of preterm infants. J Obstet Gynecol Neonatal Nurs 35, 358–368. doi: 10.1111/j.1552-6909.2006.00049.x
Shah, P. E., Clements, M., and Poehlmann, J. (2011). Maternal resolution of grief after preterm birth: implications for infant attachment security. Pediatrics (Evanston) 127, 284–292. doi: 10.1542/peds.2010-1080
Treyvaud, K., Inder, T. E., Lee, K. J., Northam, E. A., Doyle, L. W., and Anderson, P. J. (2012). Can the home environment promote resilience for children born very preterm in the context of social and medical risk? J. Exp. Child Psychol. 112, 326–337. doi: 10.1016/j.jecp.2012.02.009
Turner, M., Chur-Hansen, A., and Winefield, H. (2014). The neonatal nurses’ view of their role in emotional support of parents and its complexities. J. Clin. Nurs. 23, 3156–3165. doi: 10.1111/jocn.12558
Van der Pal, S., Maguire, C. M., Le Cessie, S., Veen, S., Wit, J. M., Walther, F. J., et al. (2008). Parental stress and child behavior and temperament in the first year after the newborn individualized developmental care and assessment program. J. Early Interv. 30, 102–115. doi: 10.1177/1053815107313485
Vohr, B., McGowan, E., McKinley, L., Tucker, R., Keszler, L., and Alksninis, B. (2017). Differential effects of the single-family room neonatal intensive care unit on 18- to 24-month Bayley scores of preterm infants. J. Pediatr. 185, 42–48.e1. doi: 10.1016/j.jpeds.2017.01.056
Welch, M. G., Firestein, M. R., Austin, J., Hane, A. A., Stark, R. I., Hofer, M. A., et al. (2015). Family nurture intervention in the neonatal intensive care unit improves social-relatedness, attention, and neurodevelopment of preterm infants at 18 months in a randomized controlled trial. J. Child Psychol. Psychiatry 56, 1202–1211. doi: 10.1111/jcpp.12405
Whipple, J. (2000). The effect of parent training in music and multimodal stimulation on parent-neonate interactions in the neonatal intensive care unit. J. Music. Ther. 37, 250–268. doi: 10.1093/jmt/37.4.250
Woodward, L. J., Moor, S., Hood, K. M., Champion, P. R., Foster-Cohen, S., Inder, T. E., et al. (2009). Very preterm children show impairments across multiple neurodevelopmental domains by age 4 years. Arch. Dis. Child Fetal Neonatal Ed. 94:339. doi: 10.1136/adc.2008.146282
Yaari, M., Treyvaud, K., Lee, K. J., Doyle, L. W., and Anderson, P. J. (2019). Preterm birth and maternal mental health: longitudinal trajectories and predictors. J. Pediatr. Psychol. 44, 736–747. doi: 10.1093/jpepsy/jsz019
Yrjölä, P., Myers, M. M., Welch, M. G., Stevenson, N. J., Tokariev, A., and Vanhatalo, S. (2022). Facilitating early parent-infant emotional connection improves cortical networks in preterm infants. Sci. Transl. Med. 14:eabq4786. doi: 10.1126/scitranslmed.abq4786
Keywords: preterm born infant, psychosocial intervention, parent-infant relationship, parent-infant interaction, parenting a child with disabilities
Citation: Leppänen M, Korja R, Rautava P and Ahlqvist-Björkroth S (2024) Early psychosocial parent–infant interventions and parent–infant relationships after preterm birth–a scoping review. Front. Psychol. 15:1380826. doi: 10.3389/fpsyg.2024.1380826
Received: 02 February 2024; Accepted: 19 July 2024;
Published: 07 August 2024.
Edited by:
Livio Provenzi, University of Pavia, ItalyReviewed by:
Laura Cordolcini, Eugenio Medea (IRCCS), ItalyCopyright © 2024 Leppänen, Korja, Rautava and Ahlqvist-Björkroth. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marika Leppänen, bWFyaWthLmxlcHBhbmVuQHV0dS5maQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.