
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 19 June 2024
Sec. Psycho-Oncology
Volume 15 - 2024 | https://doi.org/10.3389/fpsyg.2024.1378854
Background: The provision of audio recordings of their own medical encounters to patients, termed consultation recordings, has demonstrated promising benefits, particularly in addressing information needs of cancer patients. While this intervention has been explored globally, there is limited research specific to Germany. This study investigates the attitudes and experiences of cancer patients in Germany toward consultation recordings.
Methods: We conducted a nationwide cross-sectional quantitative online survey, informed by semi-structured interviews with cancer patients. The survey assessed participants’ attitudes, experiences and desire for consultation recordings in the future. The data was analyzed using descriptive statistics and subgroup analyses.
Results: A total of 287 adult cancer patients participated. An overwhelming majority (92%) expressed a (very) positive attitude. Overall, participants strongly endorsed the anticipated benefits of the intervention, such as improved recall and enhanced understanding. Some participants expressed concerns that physicians might feel pressured and could become more reserved in their interactions with the use of such recordings. While a small proportion (5%) had prior experience with audio recording medical encounters, the majority (92%) expressed interest in having consultation recordings in the future.
Discussion: We observed positive attitudes of cancer patients in Germany toward consultation recordings, paralleling international research findings. Despite limited experiences, participants acknowledged the potential benefits of the intervention, particularly related to recalling and comprehending information from medical encounters. Our findings suggest that the potential of the intervention is currently underutilized in German cancer care. While acknowledging the possibility of a positive bias in our results, we conclude that this study represents an initial exploration of the intervention’s potential within the German cancer care context, laying the groundwork for its further evaluation.
The provision of audio recordings of their own medical encounters to patients, termed consultation recordings, can help to address information needs of patients by improving understanding, recall, and feeling informed (van der Meulen et al., 2008; Tsulukidze et al., 2014; Barr et al., 2018; Rieger et al., 2018). High information needs are common among cancer patients (Rutten et al., 2005), especially shortly after diagnosis (Matsuyama et al., 2013). Medical consultations are the most important source of information for cancer patients (Rudolph et al., 2015). Ensuring patients receive comprehensible information is crucial, as emphasized in health policy (Bundestag, 2013). A systematic review found that patients with fulfilled information needs experience better health-related quality of life and less anxiety and depression (Husson et al., 2011). However, patients often struggle to accurately recall information provided during medical encounters, with up to 80 percent being forgotten (Ley, 1979; Kessels, 2003; Jansen et al., 2008; van der Meulen et al., 2008; Watson and Mckinstry, 2009; Sherlock and Brownie, 2014). Various reasons have been proposed, including anxiety, pain (Kessels, 2003; Rimmer, 2019) and cognitive deficits (Kessels, 2003; Janelsins et al., 2014; Pendergrass et al., 2018).
One intervention to address this issue is providing patients with consultation recordings. Several international studies have investigated this intervention, predominantly focusing on cancer patients (Tsulukidze et al., 2014), with the majority of research conducted in the United States (Tsulukidze et al., 2014; Elwyn et al., 2017; Grande et al., 2017; Barr et al., 2018, 2021; Joshi et al., 2020; Kwon et al., 2021; Smith et al., 2022), Australia (Lipson-Smith et al., 2016; Moloczij et al., 2017; Hyatt et al., 2018, 2020; Petric et al., 2021; Ryan et al., 2022), and the United Kingdom (Elwyn et al., 2015; Ivermee and Yentis, 2019; Shepherd et al., 2023). Empirical evidence supporting this intervention reveals a wide range of benefits, which help to meet information needs of patients by improving information recall (van der Meulen et al., 2008; Tsulukidze et al., 2014; Barr et al., 2018; Hyatt et al., 2018; Rieger et al., 2018; Dommershuijsen et al., 2019; Kwon et al., 2021; Petric et al., 2021; Shepherd et al., 2023), increasing feelings of being informed (Dommershuijsen et al., 2019; Hack et al., 2021), and enhancing understanding (van Bruinessen et al., 2017; Barr et al., 2018; Hyatt et al., 2018; Kwon et al., 2021; Shepherd et al., 2023). Further benefits include increased patient empowerment (Elwyn et al., 2015; Grande et al., 2017; Hyatt et al., 2020; Smith et al., 2022), facilitation of discussions with family members (Dommershuijsen et al., 2019; Hyatt et al., 2020; Kwon et al., 2021; Petric et al., 2021), heightened satisfaction with care (Pitkethly et al., 2008; Dommershuijsen et al., 2019), improvement in decision-making (Dommershuijsen et al., 2019; Kwon et al., 2021; Smith et al., 2022), and reductions in anxiety and depression (Tsulukidze et al., 2014; Rieger et al., 2018; Smith et al., 2022). Research has explored various ways of implementing this intervention, including patient-led recordings [i.e., patients asking clinicians to record with their own recording device or cell phone (Ryan et al., 2022)], covert recordings (Elwyn et al., 2015; Barr et al., 2018), or provision of recordings, for example via patient-centered smartphone apps (Hyatt et al., 2020; Barr et al., 2021). Nevertheless, the prevalence of consultation recordings for patients remains relatively low, ranging from 15 [United Kingdom (Elwyn et al., 2015)] to 18 [United States (Barr et al., 2018)] percent of patients reporting to have recorded at least one medical consultation in the past. This might be linked to barriers related to the implementation of consultation recordings. Concerns include the potential escalation of patient anxiety from hearing distressing content (Tsulukidze et al., 2014; Moloczij et al., 2017; Hyatt et al., 2018; Hack et al., 2021), a negative impact on the patient-physician relationship (Tsulukidze et al., 2014; Elwyn et al., 2015; Grande et al., 2017; Moloczij et al., 2017; van Bruinessen et al., 2017; Dommershuijsen et al., 2019), healthcare personnel feeling uneasy about being recorded (Tsulukidze et al., 2014; Moloczij et al., 2017; van Bruinessen et al., 2017; Barr et al., 2018; Ivermee and Yentis, 2019), and worries about medico-legal implications (Tsulukidze et al., 2014; Elwyn et al., 2015; Moloczij et al., 2017; van Bruinessen et al., 2017; Barr et al., 2018; Rieger et al., 2018; Ivermee and Yentis, 2019; Joshi et al., 2020; Ryan et al., 2022). Additionally, concerns were raised that consultation recordings could prolong consultations (Tsulukidze et al., 2014; Moloczij et al., 2017). However, consultation recordings have not been found to substantially extend consultation times (Hack et al., 2013; Tsulukidze et al., 2014; Petric et al., 2021). Furthermore, previous studies suggest that patients who received a consultation recording needed less phone calls and had fewer questions later on (Hack et al., 2013; Tsulukidze et al., 2014; Petric et al., 2021). Nevertheless, patients in general express a positive attitude toward consultation recordings (Barr et al., 2018; Dommershuijsen et al., 2019; Ivermee and Yentis, 2019; Hack et al., 2021; Petric et al., 2021; Smith et al., 2022), and express a desire to record consultations in the future (Elwyn et al., 2015; Barr et al., 2018; Dommershuijsen et al., 2019).
Effective implementation of interventions relies heavily on contextual factors, such as culture (Damschroder et al., 2022). However, there is limited research on consultation recordings in Germany. To assess the intervention’s feasibility in the German healthcare context, this study aimed to assess the attitudes and experiences of cancer patients in Germany toward the provision of audio recordings of medical encounters.
We report on a cross-sectional nationwide quantitative survey exploring cancer patients’ attitudes and experiences regarding consultation recordings in Germany. Reporting follows the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) (Eysenbach, 2004) (cp. Supplementary file S1).
Adult cancer patients were eligible to participate. It was planned to include 300 participants in the quantitative survey for pragmatic reasons. As we planned predominantly descriptive data analyses, no a priori power analysis was undertaken.
The development of the survey questionnaire was based on semi-structured qualitative interviews with 11 cancer patients (qualitative methods and results can be found in Supplementary file S2), qualitative interviews with people from the general public in an unpublished preliminary study by the authors, the integrative model of patient-centeredness (Scholl et al., 2014), and additional literature (Elwyn et al., 2015, 2017; Lipson-Smith et al., 2016; Moloczij et al., 2017; Hyatt et al., 2018; Joshi et al., 2020). The survey assessed the experience with, attitudes toward, and desire for consultation recordings. The first sentence of the survey’s first page described to participants what consultation recordings are. When participants indicated that they had experience with consultation recordings, they were asked further questions regarding their experience (e.g., who suggested the recording, how it was done, and with whom they shared their recording). Subsequently, participants were asked about their general attitude toward the intervention on a 6-point Likert scale, ranging from very negative (=1) to very positive (=6), followed by 45 questions with statements about the assumed benefits and concerns regarding the intervention, which were assessed on a 6-point Likert scale, ranging from completely disagree (=1) to completely agree (=6). When participants indicated that they would like to have audio recordings in the future, they were asked further questions regarding the implementation (e.g., if they would be open to record the consultation with their own phone, if they would listen to the recording, and if they would share it).
Additionally, we employed the German version of the “Affinity for Technology Interaction Short Scale (ATI-S) (Wessel et al., 2019) to evaluate participants’ proclivity for actively engaging with technical systems (Franke et al., 2019). The scale consists of 4 items using a 6-point Likert scale, ranging from completely disagree (=1) to completely agree (=6). The ATI-S showed high McDonald’s omega, factor loadings, item difficulty and discrimination, and construct validity (Wessel et al., 2019). Participants’ health literacy was assessed using the German version of the “HLS-EU-Q16” (Pelikan and Ganahl, 2017), consisting of 16 items using a 4-point Likert scale, ranging from very easy (=1) to very difficult (=4). To assess participants’ preferred role in treatment decisions, an adapted version of the “Control Preferences Scale (CPS)” (Degner et al., 1997; Rothenbacher et al., 1997; Giersdorf et al., 2003) was used. The instrument measures whether participants prefer the decision-making to be led by either the doctor, the patient, or both, assessed with one item. Additionally, demographic data (e.g., age, gender, language skills, education level) and disease-related information (e.g., cancer diagnosis, level of disease progression) were collected. The questionnaire can be found in Supplementary file S3. The questionnaire was pretested with cancer patients from the study’s advisory board, colleagues from our department, and people from the general population (n = 9).
We employed a convenience sampling method. Different recruitment strategies were used to disseminate invitations to the survey. Participants were invited via email through the distribution networks of more than a thousand self-help groups for various cancer types, and via social media. In addition, leaflets were distributed at various locations, including conferences and in-and outpatient facilities. Further details on the recruitment process can be found in Supplementary file S4. Before participating in the open online survey, participants were required to provide informed consent electronically and confirm their cancer diagnosis through self-report. The online survey was conducted between June 2022 and April 2023, utilizing the LimeSurvey platform (Limesurvey GmbH, n.d.). Participating patients had the opportunity to receive a 10 Euro incentive.
Only participants who met the inclusion criteria and completed the survey were included in the dataset for analysis. Standardized questionnaires were analyzed according to their manuals. Participants were excluded from analysis if the manuals’ criteria were not met (i.e., certain number of non-responses on questionnaire items). Responses (n = 2) to open-ended questions, which were only used in the assessment of experiences, were also included in the analyses.
Data was analyzed using SPSS 27. We primarily calculated descriptive statistics. For all items on attitudes, we calculated frequency distributions, means, standard deviations, and medians from the complete sample. For items on experience with and desire for consultation recordings, we calculated frequency distributions. In addition, we calculated descriptive statistics regarding the attitudes toward consultation recordings for three subsamples: those indicating a desire for consultation recordings, those being undecided, and those having no desire. Furthermore, two hypotheses for subgroup testing were formulated based on results from a previous study (Barr et al., 2018): (1) The attitude toward consultation recordings is more negative with higher patient age, (2) The attitude toward consultation recordings is more negative with lower education level. Regarding hypothesis 1, we compared three age groups: “18 to 39 years,” “40 to 59 years,” and “60 years and older.” Regarding hypothesis 2, we compared three groups with different education levels: “low to intermediate” (i.e., no formal degree or graduation after not more than 11 years at school), “high” (i.e., graduation after more than 11 years at school), and “very high” (i.e., college or university degree). The Jonckheere-Terpstra test, a rank-based nonparametric test, was employed to determine whether there is a statistically significant trend between the ordinal independent variables (age groups, education levels) and the ordinal dependent variable (general attitude) (Sheskin, 2011). Given the presence of two co-primary hypotheses, significance level was set to p < 0.025.
Two hundred eighty-seven participants met the inclusion criteria and completed the survey. Most participants were female (n = 213, 74.2%), between 40 and 59 years old (n = 117, 40.8%), and had a very high education level (i.e., college or university degree, n = 128, 44.6%). Breast cancer (n = 105, 36.6%) and prostate cancer (n = 28, 9.8%) were the most frequently reported diagnoses. Additional participant characteristics are presented in Table 1. Additional disease related information of the participants can be found in Table 2.
The mean of the 6-point Likert scale item on general attitudes toward consultation recordings was 5.22 (SD = 0.99; Median = 6.00), showing very positive attitudes. Most participants (n = 265, 91.9%) reported a rather positive, mostly positive or very positive attitude toward consultation recordings (see Figure 1). Table 3 presents statements regarding benefits of consultation recordings and participants’ level of agreement on a scale from completely disagree (=1) to completely agree (=6), ranked from highest to lowest mean, Supplementary file 5 includes frequency distribution graphs for all statements about potential benefits. In general, participants demonstrated high to very high agreement to the proposed benefits of consultation recordings (means from 3.87 to 5.74, medians from 4.00 to 6.00). “A consultation recording allows patients to have a better recall of the information discussed” was the item with the highest and “A consultation recording improves the trust between patients and physicians” with the lowest mean. Participants particularly exhibited very high agreement to statements regarding the influence of consultation recordings on recall (X̅=5.74; SD = 0.68; Median = 6.00) and preparation for follow-up appointments (X̅=5.55; SD = 0.86; Median = 6.00). They also concurred that consultation recordings help patients retrospectively verify correct understanding of the information (X̅=5.46; SD = 0.89; Median = 6.00). Additionally, consultation recordings were perceived to enhance the understanding of information (X̅=5.34; SD = 0.91; Median = 6.00). Furthermore, they agreed that consultation recordings are especially helpful in consultations where treatment decisions are made (X̅=5.30; SD = 1.05; Median = 6.00) and in complex and lengthy treatments (X̅=5.29; SD = 1.04; Median = 6.00).
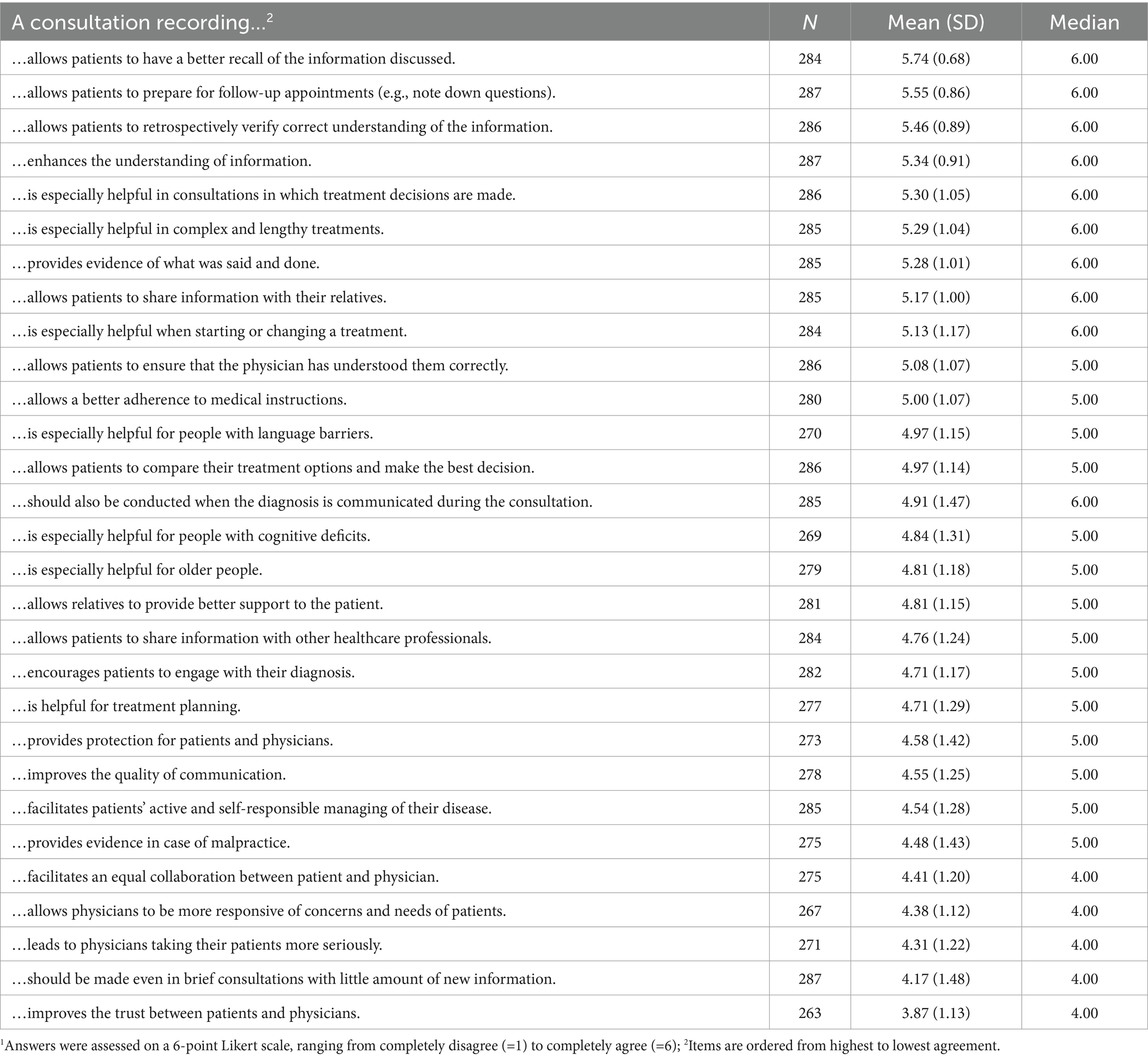
Table 3. Levels of agreement toward different statements about benefits of consultation recordings1.
However, participants somewhat agreed with the proposed concerns about consultation recordings (see Table 4 and Supplementary file S6), although this agreement was not as strong as that related to the proposed benefits. Their primary concerns centered around consultation recordings putting pressure on physicians (X̅=3.77; SD = 1.34; Median = 4.00) and physicians being reserved and less open during the consultations (X̅=3.72; SD = 1.45; Median = 4.00). Lesser concerns included the physician-patient-relationship becoming more formal (X̅=3.47; SD = 1.35; Median = 4.00) and physicians solely referring them to the consultation recording if questions arose after the consultation (X̅=3.45; SD = 1.28; Median = 3.00). Furthermore, participants expressed less concern that consultation recordings would be used as evidence against physicians (X̅=3.44; SD = 1.48; Median = 3.00) and that relatives could pressure patients into allowing them to listen to their consultation recordings (X̅=3.41; SD = 1.43; Median = 3.00).
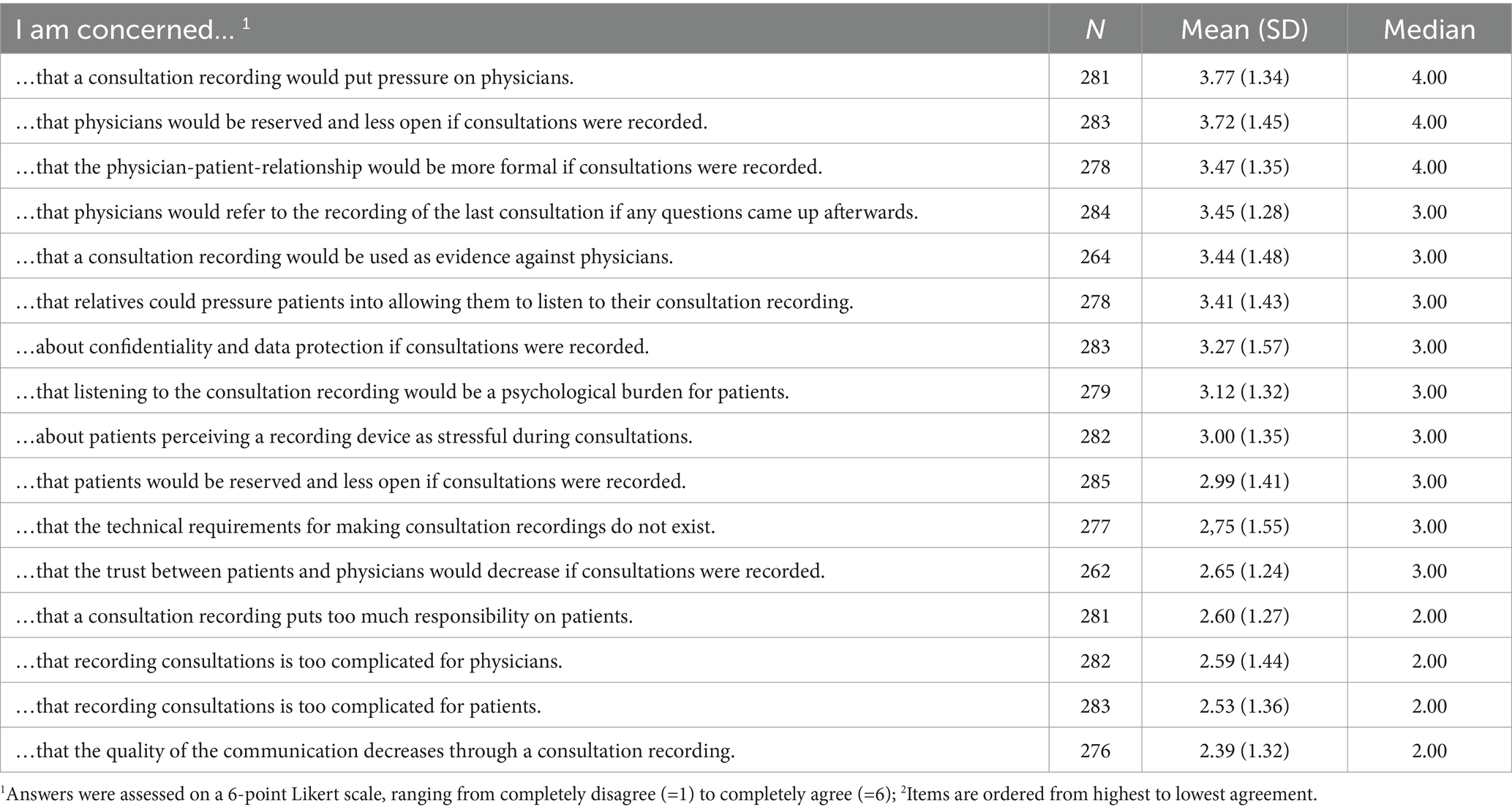
Table 4. Levels of agreement toward different statements about concerns regarding consultation recordings.
Descriptively, 18 to 39 year-old participants showed a Median of 6.00 regarding their general attitude toward consultation recordings, 40 to 59 year-olds of 5.50, and people 60 years and older of 5.00. In the Jonckheere-Terpstra test, we found a statistically significant trend toward more negative attitude with rising age in this sample (TJT = 11213.500, z = −2.838, p = 0.005).
Regarding education levels, the medians for the general attitude item in the three groups were as follows: Median = 5.00 for low to intermediate education level, Median = 6.00 for high education level, and Median = 6.00 for very high education level. The Jonckheere-Terpstra test did show no statistically significant trend in the general attitudes with rising educational level in this sample (TJT = 13275.000, z = 1.136, p < 0.256).
Fifteen participants (5.2%) reported having experience with consultation recordings. Among them, seven (46.7%) had recorded on multiple occasions and four (26.7%) covertly. For the following items, multiple answers could apply. Recordings had been initiated by patients themselves (n = 13, 86.7%) or by either a physician, a friend, or a spouse (each n = 1, 6.7%). In all instances, consultations had been recorded with a cell phone – either with the patients (n = 14, 93.3%) or the accompanying person’s (n = 2, 13.3%). Most participants (n = 14, 93.3%) had listened to the consultation recording after the encounter – either by themselves (n = 8, 57.1%), with their family (n = 4, 28.6%), their friends (n = 4, 28.6%), their spouse (n = 3, 21.4%), their physician (n = 1, 7.1%), or another person (n = 1, 7.1%).
When asked if they wanted consultation recordings in the future, 193 of the 287 participants (67.2%) answered “yes,” 73 (25.4%) answered “maybe,” and 21 (7.3%) answered “no.” Among those who answered “yes” or “maybe,” 220 (82.7%) would be open to recording the encounter with their own cell phone, while 46 (17.3%) would not. Among those who had prior experience with consultation recordings, 13 (86.7%) answered “yes” and two (13.3%) “maybe.” All of these (n = 15, 100%) would be open to recording the encounter with their own cell phone.
Two hundred twenty-seven participants (85.3%) expected they would listen to the consultation recordings, 37 (13.9%) maybe, and two (0.8%) would not. Of those expecting to listen, all (n = 227, 100.0%) (rather, mostly, or completely) agreed that they would want to listen to what their physician said, 195 (86%) to what they said themselves. Furthermore, 193 participants (72.5%) assumed that they would listen to the recording together with relatives, nine (3.4%) would let their relatives listen to the recording on their own, 40 (15.0%) would not share the recording with relatives, and 24 (9.0%) did not answer this question.
We descriptively analyzed the attitudes regarding consultation recordings separately for those wanting consultation recordings in the future (n = 193), those being undecided (n = 73), and those not wanting them (n = 21) in an explorative approach. On average, those wanting consultation recordings reported more positive general attitudes, higher agreement with potential benefits, and lower agreement with concerns. Those participants who would “maybe” want consultation recordings in the future seemed to build the middle ground, and those declining a wish for consultation recordings reported rather neutral attitudes. However, the third subsample was very small, with only 21 participants indicating no desire for consultation recordings. Detailed results are shown in Supplementary file S7.
In this initial exploration of cancer patients’ views on consultation recordings in Germany, we identified predominantly positive attitudes and high level of agreement regarding potential benefits. Concerns related to consultation recordings were also reported, albeit with less emphasis. Participants viewed encounters involving decisions about complex and burdensome treatment regimens as particularly suitable for recording. Older age was associated with less favorable attitudes toward consultation recordings in our sample. While a minority of participants in our sample had prior experiences with consultation recordings, the majority expressed interest in having consultation recordings in the future. Positive attitudes toward consultation recordings seem to be associated with a desire for future use.
In relation to participants’ positive attitudes toward consultation recordings, our findings align with existing research (Barr et al., 2018; Dommershuijsen et al., 2019; Ivermee and Yentis, 2019; Hack et al., 2021; Petric et al., 2021; Smith et al., 2022). Our study also supports previous research indicating that patients value consultation recordings as a suitable solution to the challenge of recalling and comprehending information from medical encounters (van der Meulen et al., 2008; Tsulukidze et al., 2014; van Bruinessen et al., 2017; Barr et al., 2018; Hyatt et al., 2018; Rieger et al., 2018; Dommershuijsen et al., 2019; Kwon et al., 2021; Petric et al., 2021; Shepherd et al., 2023). Consequently, we can conclude that participants would appreciate consultation recordings as a means to address their information needs. Moreover, we found that consultation recordings were expected to be particularly beneficial in contexts involving treatment decisions, which is consistent with prior research demonstrating that consultation recordings are useful for decision-making (Dommershuijsen et al., 2019; Kwon et al., 2021; Smith et al., 2022). It is noteworthy that in our sample, similar to findings from previous research (Barr et al., 2018), older patients seem to be less in favour of consultation recordings. If age is the cause of the more negative attitudes or a proxy for another cause, it needs to be evaluated in subsequent studies. At the same time, both our study and previous research suggest that consultation recordings could be particularly beneficial for older patients (Dommershuijsen et al., 2019). Nevertheless, some participants expressed concerns about consultation recordings, particularly regarding a potential negative shift in the openness of the physician and in the physician-patient-relationship. Those concerns were also found in previous research (Tsulukidze et al., 2014; Elwyn et al., 2015; Grande et al., 2017; Moloczij et al., 2017; van Bruinessen et al., 2017; Dommershuijsen et al., 2019). Nevertheless, it is worth noting that the overall level of concern about these issues was relatively low, suggesting that participants believe the benefits of consultation recordings outweigh potential disadvantages.
Only a small percentage of participants reported having prior experience with consultation recordings (either overt or covert). This highlights that consultation recordings are not yet widely utilized in Germany, consistent with findings from international studies (Elwyn et al., 2015; Barr et al., 2018). Notably, a considerable amount of those who had shared the recording did so with a relative, emphasizing the potential role of consultation recordings for facilitating discussions and information sharing with the patient’s support network. This observation aligns with findings from previous studies (Dommershuijsen et al., 2019; Hyatt et al., 2020; Kwon et al., 2021; Petric et al., 2021). Furthermore, our study revealed that in almost all cases, participants took the initiative to record the medical encounter with their own cell phone, showcasing an accessible approach to this intervention. The majority of participants also expressed a desire to have consultation recordings in the future, with most of them considering recording the encounter with their own cell phone. This underscores the potential of consultation recordings to not only improve patient outcomes such as recall and comprehension of medical information but also to promote patients’ engagement in their own healthcare, consistent with findings from previous research (Elwyn et al., 2015; Grande et al., 2017; Hyatt et al., 2020; Smith et al., 2022).
The overwhelmingly positive attitudes of our sample, coupled with the expressed desire for consultation recordings in the future, underscores its potential for the German healthcare system. However, the limited experiences of our sample suggests that this potential remains largely underutilized in German cancer care. This could be attributable to physicians in Germany being less open toward technological and digital innovations in general and viewing changes in power structure (e.g., empowering patients) as less favorable than in other countries, thus slowing the adoption of technological innovations in Germany (Safi et al., 2018; Hansen et al., 2019). Furthermore, the link between attitudes and desire to use consultation recordings warrants further exploration.
Despite comprehensive international research on consultation recordings and their well-documented benefits and effects, their applicability to the German healthcare system remains uncertain. Future research, including randomized controlled trials, should delve deeper into the effects within this context and consider diverse perspectives, such as those of relatives, health professionals, and healthcare institutions.
A major strength of our study is that it presents the first investigation of consultation recordings in the German healthcare setting, therewith closing a relevant research gap. Additional strengths include the preceding qualitative interviews that informed the development of our quantitative questionnaire. However, our study is not without limitations. First, selection bias, which limits the generalizability and validity of our results, is anticipated, particularly given that our sample was obtained through self-help groups and patient organizations. This suggests a potential bias toward a more favorable disposition toward patient-centered interventions. Additionally, our sample comprised relatively young and female participants with a high level of education. It is also presumed that due to the online recruitment of participants, individuals with lower technological competence might be underrepresented. This might have contributed to a bias toward positive attitudes about consultation recordings, which might have led to over estimating the feasibility of the intervention. Moreover, the majority of our sample consisted of individuals expressing their attitudes toward an intervention with which they lack personal experience. Second, this study focused on descriptive analyses. We therefore did not conduct power analyses, which limits the external validity of our results. Third, data collection occurred during the peak period of the COVID pandemic, when patients were often alone in medical consultations and were possibly more inclined to welcome an “additional pair of ears,” for which consultation recordings could have been used. Additional limitations include the lack of investigation into reasons for non-participation and the absence of a standardized and psychometrically sound questionnaire to assess attitudes toward consultation recordings.
In conclusion, this study represents an initial exploration of the intervention’s potential within the German cancer care context, laying the groundwork for its further evaluation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study involving humans were approved by the Psychological Ethics Committee of the Center for Psychosocial Medicine of the University Medical Center Hamburg-Eppendorf. This study were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
CT: Investigation, Writing – original draft, Formal analysis. IS: Writing – review & editing, Supervision, Project administration, Methodology, Funding acquisition, Conceptualization. PH: Writing – review & editing, Supervision, Project administration, Methodology, Formal analysis, Conceptualization, Funding acquisition.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Robert Bosch Foundation (Project number: 01000824–001) as part of the feasibility study “Patientenorientierte Krebsversorgung durch Bereitstellung von Audioaufnahmen von Arzt-Patienten-Gesprächen für Patient:innen – eine Machbarkeitsstudie.” We acknowledge financial support from the Open Access Publication Fund of UKE - Universitätsklinikum Hamburg-Eppendorf.
We thank all those who supported our study. Special acknowledgment goes to our student assistant, Marina Buzo. Additionally, we appreciate the contributions of our interns: Robert Reincke, Hannah Schmidberger, Funda Sahbudak, and Alena Schneider. We are also grateful to the members of our project advisory board, Maximilian Büttner (“Deutsche Stiftung für Junge Erwachsene mit Krebs“), Anja Coym (University Medical Center Hamburg-Eppendorf), Kerstin Hermes-Moll (“Wissenschaftliches Institut der Niedergelassenen Ärztinnen und Ärzte für Hämatologie und Medizinische Onkologie – WINHO GmbH”), Bernhard Jochheim (“Deutsche Leukämie- & Lymphom-Hilfe e.V.“), Volkmar Müller (University Medical Center Hamburg-Eppendorf), Kai Uwe Parsons-Galka (“University Cancer Center Hamburg Research Patient Advisory Board”), Georgia Schilling (“Asklepios Nordseeklinik Westerland – Rehabilitationsklinik”), and Andrea Spakowski (“Bundesverband Prostatakrebs Selbsthilfe e.V.”). We thank Stefan Zeh for pretesting the online survey, and Susanne Lezius, Svenja Wandke as well as Eva Christalle for providing advice on the quantitative data analysis. Furthermore, we thank Paul Barr for scientific advice. We also thank all collaboration partners at the University Cancer Center Hamburg and the University Medical Center Hamburg-Eppendorf as well as at the “Asklepios Tumorzentrum Hamburg,” the “Haus der Krebs-Selbsthilfe – Bundesverband e.V.,” the “Deutsche Leukämie-und Lymphom-Hilfe e.V.,” the “Deutsche Stiftung für junge Erwachsene mit Krebs,” and the Hämatologisch-Onkologische Praxis Eppendorf (HOPE).” Lastly, our gratitude is extended to all participating patients.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1378854/full#supplementary-material
Barr, P. J., Bonasia, K., Verma, K., Dannenberg, M. D., Yi, C., Andrews, E., et al. (2018). Audio−/videorecording clinic visits for patient’s personal use in the United States: cross-sectional survey. J. Med. Internet Res. 20:e11308. doi: 10.2196/11308
Barr, P. J., Haslett, W., Dannenberg, M. D., Oh, L., Elwyn, G., Hassanpour, S., et al. (2021). An audio personal health library of clinic visit recordings for patients and their caregivers (HealthPAL): user-centered design approach. J. Med. Internet Res. 23:e25512. doi: 10.2196/25512
Bundestag (2013). Gesetz zur Verbesserung der Rechte von Patientinnen und Patienten (Patientenrechtegesetz). Bundesgesetzblatt 1, 277–282.
Damschroder, L. J., Reardon, C. M., Widerquist, M. A. O., and Lowery, J. (2022). The updated consolidated framework for implementation research based on user feedback. Implement. Sci. 17:75. doi: 10.1186/s13012-022-01245-0
Degner, L. F., Sloan, J. A., and Venkatesh, P. (1997). The control preferences scale. Can. J. Nurs. Res. 29, 21–43
Dommershuijsen, L. J., Dedding, C. W. M., and Van Bruchem-Visser, R. L. (2019). Consultation recording: what is the added value for patients aged 50 years and over? A Systematic Review. Health Commun. 36, 168–178. doi: 10.1080/10410236.2019.1669270
Elwyn, G., Barr, P. J., and Castaldo, M. (2017). Can patients make recordings of medical encounters? JAMA 318, 513–514. doi: 10.1001/jama.2017.7511
Elwyn, G., Barr, P. J., and Grande, S. W. (2015). Patients recording clinical encounters: a path to empowerment? Assessment by mixed methods. BMJ Open 5:e008566. doi: 10.1136/bmjopen-2015-008566
Eysenbach, G. (2004). Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J. Med. Internet Res. 6:e34. doi: 10.2196/jmir.6.3.e34
Franke, T., Attig, C., and Wessel, D. (2019). A personal resource for technology interaction: development and validation of the affinity for technology interaction (ATI) scale. Int. J. Hum. Comput. Interact. 35, 456–467. doi: 10.1080/10447318.2018.1456150
Giersdorf, N., Loh, A., and Härter, M. (2003). “Quantitative Messverfahren des shared Decison-making” in Shared Decision-Making: Der Patient als Partner im medizinischen Entscheidungsprozess. eds. F. Scheibler and H. Pfaff (Weinheim, München: Juventa), 69–85.
Grande, S. W., Castaldo, M. G., Carpenter-Song, E., Griesemer, I., and Elwyn, G. (2017). A digital advocate? Reactions of rural people who experience homelessness to the idea of recording clinical encounters. Health Expect. 20, 618–625. doi: 10.1111/hex.12492
Hack, T. F., Ruether, J. D., Pitz, M., Thiessen, B., Degner, L. F., and Chateau, D. (2021). Impact of consultation recordings on patient-reported outcomes in patients with brain tumors: a parallel randomized controlled trial. Support Care Cancer 29, 5681–5690. doi: 10.1007/s00520-021-06038-7
Hack, T. F., Ruether, J. D., Weir, L. M., Grenier, D., and Degner, L. F. (2013). Promoting consultation recording practice in oncology: identification of critical implementation factors and determination of patient benefit. Psychooncology 22, 1273–1282. doi: 10.1002/pon.3135
Hansen, A., Herrmann, M., Ehlers, J. P., Mondritzki, T., Hensel, K. O., Truebel, H., et al. (2019). Perception of the progressing digitization and transformation of the German health care system among experts and the public: mixed methods study. JMIR Public Health Surveill. 5:e14689. doi: 10.2196/14689
Husson, O., Mols, F., and van de Poll-Franse, L. V. (2011). The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: a systematic review. Ann. Oncol. 22, 761–772. doi: 10.1093/annonc/mdq413
Hyatt, A., Lipson-Smith, R., Gough, K., Butow, P., Jefford, M., Hack, T. F., et al. (2018). Culturally and linguistically diverse oncology patients’ perspectives of consultation audio-recordings and question prompt lists. Psycho-Oncol 27, 2180–2188. doi: 10.1002/pon.4789
Hyatt, A., Lipson-Smith, R., Morkunas, B., Krishnasamy, M., Jefford, M., Baxter, K., et al. (2020). Testing consultation recordings in a clinical setting with the SecondEars smartphone app: mixed methods implementation study. JMIR Mhealth Uhealth 8:e15593. doi: 10.2196/15593
Ivermee, C., and Yentis, S. M. (2019). Attitudes of postnatal women and maternity staff toward audio recording of consent discussions. Anaesthesia 74, 1095–1100. doi: 10.1111/anae.14660
Janelsins, M. C., Kesler, S. R., Ahles, T. A., and Morrow, G. R. (2014). Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int. Rev. Psychiatry 26, 102–113. doi: 10.3109/09540261.2013.864260
Jansen, J., Butow, P. N., Van Weert, J. C. M., Van Dulmen, S., Devine, R. J., Heeren, T. J., et al. (2008). Does age really matter? Recall of information presented to newly referred patients with cancer. J. Clin. Oncol. 26, 5450–5457. doi: 10.1200/JCO.2007.15.2322
Joshi, A., Farberov, M., Demissie, S., Smith, M. C., and Elwyn, G. (2020). Attitudes of physicians to recording clinical encounters: responses to an online survey. J. Gen. Intern. Med. 35, 942–943. doi: 10.1007/s11606-019-05127-y
Kessels, R. P. C. (2003). Patients’ memory for medical information. J. R. Soc. Med. 96, 219–222. doi: 10.1258/jrsm.96.5.219
Kwon, D. H., Aggarwal, R. R., Esserman, L. J., and Belkora, J. K. (2021). Prime time for consultation audio recordings: supporting shared decision making during and after the COVID-19 era. JCO Oncol. Pract. 17, 161–163. doi: 10.1200/OP.20.00765
Ley, P. (1979). Memory for medical information. Br. J. Soc. Clin. Psychol. 18, 245–255. doi: 10.1111/j.2044-8260.1979.tb00333.x
Limesurvey GmbH (n.d.). LimeSurvey: An open source survey tool. Available at: http://www.limesurvey.org (Accessed January 29, 2024).
Lipson-Smith, R., Hyatt, A., Butow, P., Hack, T. F., Jefford, M., Hale, S., et al. (2016). Are audio recordings the answer?- a pilot study of a communication intervention for non-English speaking patients with cancer. Psycho-Oncol. 25, 1237–1240. doi: 10.1002/pon.4193
Matsuyama, R. K., Kuhn, L. A., Molisani, A., and Wilson-Genderson, M. C. (2013). Cancer patients’ information needs the first nine months after diagnosis. Patient Educ. Couns. 90, 96–102. doi: 10.1016/j.pec.2012.09.009
Moloczij, N., Krishnasamy, M., Butow, P., Hack, T. F., Stafford, L., Jefford, M., et al. (2017). Barriers and facilitators to the implementation of audio-recordings and question prompt lists in cancer care consultations: a qualitative study. Patient Educ. Couns. 100, 1083–1091. doi: 10.1016/J.PEC.2017.01.005
Pelikan, J., and Ganahl, K. (2017). Die europäische Gesundheitskompetenz-Studie: Konzept, Instrument und ausgewählte Ergebnisse. Health Literacy. Forschungsstand und Perspektiven, 1, 93–125.
Pendergrass, J. C., Targum, S. D., and Harrison, J. E. (2018). Cognitive impairment associated with Cancer: a brief review. Innov. Clin. Neurosci. 15, 36–44.
Petric, J., Sadri, B., van Essen, P., and Dean, N. R. (2021). Improving preoperative breast reconstruction consultations: a qualitative study on the impact of personalised audio-recordings. BMC Womens Health 21:389. doi: 10.1186/s12905-021-01534-8
Pitkethly, M., Mac Gillivray, S., and Ryan, R. (2008). Recordings or summaries of consultations for people with cancer. Cochrane Database Syst. Rev. 3. doi: 10.1002/14651858.CD001539.pub2
Rieger, K. L., Hack, T. F., Beaver, K., and Schofield, P. (2018). Should consultation recording use be a practice standard? A systematic review of the effectiveness and implementation of consultation recordings. Psycho-Oncol. 27, 1121–1128. doi: 10.1002/pon.4592
Rimmer, A. (2019). My patient wants to record our appointment, what should I do? BMJ 364:l1101. doi: 10.1136/bmj.l1101
Rothenbacher, D., Lutz, M. P., and Porzsolt, F. (1997). Treatment decisions in palliative cancer care: patients’ preferences for involvement and doctors’ knowledge about it. Eur. J. Cancer 33, 1184–1189. doi: 10.1016/S0959-8049(97)00034-8
Rudolph, I., Seilacher, E., Köster, M.-J., Stellamanns, J., Liebl, P., Zell, J., et al. (2015). Der Informationsbedarf von Patienten mit Krebserkrankungen in Deutschland – eine Befragung von Patienten und Angehörigen. Dtsch. Med. Wochenschr. 140, e43–e47. doi: 10.1055/s-0041-100585
Rutten, L. J. F., Arora, N. K., Bakos, A. D., Aziz, N., and Rowland, J. (2005). Information needs and sources of information among cancer patients: a systematic review of research (1980-2003). Patient Educ. Couns. 57, 250–261. doi: 10.1016/j.pec.2004.06.006
Ryan, L., Weir, K. A., Maskell, J., Bevan, L., and Le Brocque, R. (2022). ‘What are you hiding from me?’ A qualitative study exploring health consumer attitudes and experiences regarding the patient-led recording of a hospital clinical encounter. Health Expect. 25, 3096–3104. doi: 10.1111/hex.13617
Safi, S., Thiessen, T., and Schmailzl, K. J. G. (2018). Acceptance and resistance of new digital technologies in medicine: qualitative study. JMIR Res. Protoc. 7:e11072. doi: 10.2196/11072
Scholl, I., Zill, J. M., Härter, M., and Dirmaier, J. (2014). An integrative model of patient-centeredness - a systematic review and concept analysis. PLoS One 9:e107828. doi: 10.1371/journal.pone.0107828
Shepherd, S. C., Hacking, B., Wallace, L. M., Murdoch, S. E., and Belkora, J. (2023). Feeling known and informed: serial qualitative interviews evaluating a consultation support intervention for patients with high-grade glioma. Cancer Med. 12, 8652–8661. doi: 10.1002/cam4.5572
Sherlock, A., and Brownie, S. (2014). Patients’ recollection and understanding of informed consent: a literature review. ANZ J. Surg. 84, 207–210. doi: 10.1111/ans.12555
Sheskin, D. J. (2011). Handbook of parametric and nonparametric statistical procedures. New York: Chapman and Hall, CRC. doi: 10.1201/9780429186196
Smith, S. M., Stelmar, J., Lee, G., Carroll, P. R., and Garcia, M. G. (2022). Use of voice recordings in the consultation of patients seeking genital gender-affirming surgery: an opportunity for broader application throughout surgery? J. Surg. Res. 5, 618–625. doi: 10.26502/jsr.10020269
Tsulukidze, M., Durand, M. A., Barr, P. J., Mead, T., and Elwyn, G. (2014). Providing recording of clinical consultation to patients – a highly valued but underutilized intervention: a scoping review. Patient Educ. Couns. 95, 297–304. doi: 10.1016/j.pec.2014.02.007
van Bruinessen, I. R., Leegwater, B., and van Dulmen, S. (2017). When patients take the initiative to audio-record a clinical consultation. Patient Educ. Couns. 100, 1552–1557. doi: 10.1016/j.pec.2017.03.001
van der Meulen, N., Jansen, J., van Dulmen, S., Bensing, J., and van Weert, J. (2008). Interventions to improve recall of medical information in cancer patients: a systematic review of the literature. Psycho-Oncol. 17, 857–868. doi: 10.1002/pon.1290
Watson, P. W., and Mckinstry, B. (2009). A systematic review of interventions to improve recall of medical advice in healthcare consultations. J. R. Soc. Med. 102, 235–243. doi: 10.1258/jrsm.2009.090013
Keywords: cancer, consultation recordings, patient-centered care, patient information, oncology, cross-sectional online study
Citation: Topf C, Scholl I and Hahlweg P (2024) Attitudes and experiences of cancer patients toward the provision of audio recordings of their own medical encounter: a cross-sectional online survey. Front. Psychol. 15:1378854. doi: 10.3389/fpsyg.2024.1378854
Received: 30 January 2024; Accepted: 17 May 2024;
Published: 19 June 2024.
Edited by:
Andreas Dinkel, Technical University of Munich, GermanyReviewed by:
Mirjam Garvelink, St. Antonius Hospital, NetherlandsCopyright © 2024 Topf, Scholl and Hahlweg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheyenne Topf, Yy50b3BmQHVrZS5kZQ==
†These authors have contributed equally to this work and share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.