
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 19 July 2024
Sec. Health Psychology
Volume 15 - 2024 | https://doi.org/10.3389/fpsyg.2024.1363527
 Awatif Alrasheeday1
Awatif Alrasheeday1 Maha Ali Alsaeed2
Maha Ali Alsaeed2 Bushra Alshammari3*
Bushra Alshammari3* Farhan Alshammari4
Farhan Alshammari4 Asia Saad Alrashidi3
Asia Saad Alrashidi3 Turki Ahmed Alsaif5
Turki Ahmed Alsaif5 Soha Kamel Mahmoud6,7
Soha Kamel Mahmoud6,7 Dolores I. Cabansag3
Dolores I. Cabansag3 Ma Venus Borja3
Ma Venus Borja3 Ahmad R. Alsayed8
Ahmad R. Alsayed8 Omaima Mohamed Elalem6,9
Omaima Mohamed Elalem6,9 Shaimaa Mohamed Nageeb5
Shaimaa Mohamed Nageeb5 Rania Abd-Elnaby Allam10
Rania Abd-Elnaby Allam10 Tahani Nasser Alhejaili11
Tahani Nasser Alhejaili11 Haneen Fahad Alsulami12
Haneen Fahad Alsulami12 Bahia Galal Abd Elrazik Siam3,13
Bahia Galal Abd Elrazik Siam3,13Background: COVID-19 has probably contributed to sleep disturbance among nurses, especially those working at emergency departments (EDs). Sleep disorders in nurse managers can negatively impact their health and impair work performance and decision-making. This study aimed to explore the quality of sleep among nurses working in EDs and its influencing factors during the COVID-19 pandemic.
Method: In this study, a cross-sectional design was employed to assess the sleep quality of nurses working in EDs during the COVID-19 pandemic. The research recruited a convenience sample of emergency nurses, who were selectively sourced from four hospitals in Hail City. This recruitment occurred over the period from April to July 2022. Descriptive data analysis was conducted using SPSS, with the significance level set at 0.05.
Results: Among the 216 participants in the study, the majority (55.6%) were aged between 30 and 39 years, and 73.6% were female. Additionally, 64.4% were married, while 69.4% had a bachelor’s degree, 20% held a diploma, and the remaining had a master’s degree. Notably, a significant 81.5% of the nurses reported poor sleep quality, as assessed by the Pittsburgh Sleep Quality Index (PSQI), with an overall mean score of 10.55 indicating poor sleep. The study highlighted that poor sleep quality among nurses was linked to being female, being married, and not exercising regularly. Better sleep was associated with nurses who manage fewer patients per shift and have adequate monthly income.
Conclusion: The prevalence of poor sleep quality among Emergency nurses during the COVID-19 pandemic is high. There is a pressing need for targeted interventions to enhance sleep quality among ED nurses. Improving sleep quality is not only essential for the wellbeing of these nurses but is also likely to contribute to better patient care.
The COVID-19 pandemic, which emerged as a global health crisis in late 2019, profoundly impacted health worldwide. By early 2022, the World Health Organization (WHO) reported a significant rise in global COVID-19 cases, with a sharp increase in reported cases, totaling approximately 23.5 million weekly (World Health Organization, 2024). The COVID-19 pandemic heightened stress, anxiety, and uncertainty due to increased cases and hospitalizations. These factors significantly impact sleep, causing disturbances, disrupted routines, and changes in work environments, particularly affecting frontline workers like nurses in Eds (Madkhali et al., 2022; Guerrera et al., 2024). The surge in patient numbers overwhelmed healthcare systems, especially in EDs, increasing the workload for nurses. This resulted in longer, irregular hours and disrupted sleep patterns, leading to sleep problems, anxiety, and depression (Pollard et al., 2020).
Quality sleep is crucial for nurses in high-stress environments like EDs; it is essential for maintaining physical and mental wellbeing, cognitive function, and overall quality of life (Abraham et al., 2017; Zeng et al., 2020). Nurses regularly face numerous work-related pressures, including heavy workloads, the need to manage interactions with patients and their families, shift work, and overtime (Bae and Fabry, 2014; Alshammari et al., 2022). Sleep problems among nurses, including insomnia, insufficient sleep, deprivation, and poor quality, are prevalent, with rates ranging from 57 to 83% (Qiu et al., 2020) and up to 50% worldwide experience short sleep durations (Furihata et al., 2020; Stimpfel et al., 2020). Low-quality sleep will not only affect their health and wellbeing but also has significant implications for patient care and safety as it can impair cognitive functions such as memory, attention, and decision-making, which are critical in the fast-paced and often high-stakes environment of an ED.
The unique stressors of the COVID-19 pandemic, including the fear of virus contraction, treating severely ill patients, and witnessing suffering, contribute to increased stress and anxiety among ED nurses (Fawaz et al., 2020). The pandemic also alters ED working conditions, with added complexities like personal protective equipment (PPE) and infection control protocols, impacting nurses’ physical exhaustion and sleep quality (Fawaz et al., 2020; Hoedl et al., 2021). The nature of shift work, especially night shifts inherent in emergency nursing, significantly affects the sleep quality of ED nurses. This, combined with rotating schedules, can disrupt circadian rhythms, leading to shift work sleep disorder. The pandemic’s demand for extended and irregular shifts further exacerbates these disruptions, impacting sleep quality (Dong et al., 2020).
Several factors influence their sleep quality, including gender, marital status, exercise habits, monthly income, and patient load (Krueger and Friedman, 2009). Female nurses often report poorer sleep quality due to the additional societal and domestic responsibilities they bear, which increase their stress levels (Almeida et al., 2020). Marital status also impacts sleep quality, with various statuses such as being single, married, divorced, or widowed influencing stress and sleep patterns differently (Troxel et al., 2007). Regular physical exercise is known to improve sleep quality by reducing stress and anxiety (Kredlow et al., 2015). Financial stability, indicated by higher monthly income, is associated with better sleep quality due to reduced financial stress and access to comfortable living conditions (Du et al., 2021). Lastly, the number of patients a nurse is responsible for during a shift significantly affects their stress levels, which in turn impacts sleep quality, with higher patient loads leading to increased stress and poorer sleep (Aiken et al., 2002). These factors, particularly in the context of nurses, need to be thoroughly explored to understand their impact on sleep quality. Poor sleep quality not only affects nurses directly but also has broader implications for healthcare systems and patient care. Studies show that sleep issues can reduce productivity, potentially lowering nursing care standards (Dong et al., 2017). Sleep-deprived nurses may struggle to maintain attention and vigilance, crucial for patient safety and effective care delivery (Stimpfel et al., 2020), increasing the risk of errors, a significant concern in EDs (Wardle-Pinkston et al., 2019).
The research aims to provide valuable insights into the pandemic’s impact on healthcare workers, specifically focusing on the sleep quality of ED nurses. It seeks to inform strategies for supporting their health and wellbeing by addressing the challenges they face during the pandemic (Alshammari et al., 2023). Additionally, the study aims to contribute to the broader discourse on healthcare worker support during crises, emphasizing the necessity of systemic changes to ensure their wellbeing, considering their integral role in healthcare systems.
Aim of the study: This study aimed to explore the quality of sleep among nurses working in EDs and its influencing factors during the COVID-19 pandemic.
Research questions:
1. What is the level of sleep quality among nurses working in the EDs during COVID-19 Pandemic?
2. What are the factors influencing sleep quality among nurses working in the EDs during COVID-19 Pandemic?
Research hypothesis
H1: Female gender has a significant association with lower sleep quality among nurses working in the ED during the COVID-19 pandemic.
H2: Being married has a significant association with lower sleep quality among nurses working in the ED during the COVID-19 pandemic.
H3: Regular physical exercise is positively associated with the sleep quality of nurses working in the ED during the COVID-19 pandemic.
H4: Monthly income is positively associated with the sleep quality of nurses working in the ED during the COVID-19 pandemic.
H5: The number of patients a nurse is responsible for during a night shift is negatively associated with sleep quality.
A cross-sectional descriptive study design was employed to assess the sleep quality and its influencing factors among nurses working in ED during the COVID-19 pandemic. All staff nurses working in the EDs were invited to participant in this research. Data collection took place between April and July 2022.
The sample was recruited from four government hospitals in Hail City, namely King Salman Specialist Hospital, Sharaf Hospital, Hail General Hospital, and King Khaled Hospital. These selected hospitals are government-run medical facilities that offer complimentary services and emergency treatment exclusively to Saudi nationals facing health issues. Each of these hospitals has the capacity to accommodate hundreds of patients across various specialties, including oncology, cardiology, obesity, and neurology. Additionally, they are equipped with Intensive Care Units (ICUs) and specialized units for burns, endoscopy, surgery, day surgery, and physiotherapy. Furthermore, they house various specialized and support service sections to cater to a broad spectrum of healthcare needs.
In this study, we approached a convenience sample of 330 nurses. Of these, 216 ED nurses completed the survey. Eligibility for participation was limited to registered nurses who were actively employed on a full-time basis in the EDs, had a minimum of one year of work experience, and expressed their willingness to participate in the study. The study excluded nurses who were not regular staff of the ED but were only covering shifts in the ED, in addition to newly hired nurses and intern nurses.
In the selected hospitals, gatekeepers, who were the head nurses, played a crucial role in identifying eligible nurses for the study. These gatekeepers were responsible for distributing the participation link, generated via Google Forms, to these selected nurses. This link led to a page where the nurses found an invitation to participate, along with an information sheet and a consent form. Upon providing their consent, the nurses gained access to the survey. They could then complete and submit the questionnaire at their convenience. The questionnaire takes 10 min to complete.
To ensure data accuracy in the questionnaires, all items were set as required to guarantee response completeness. Additionally, each IP address or device was limited to a single submission to prevent duplicate responses, thus maintaining the integrity and reliability of the data.
An English language, self-administered questionnaire was utilized to collect data, consisting of four parts:
Part I: This section gathers the sociodemographic data of the study subjects, including gender, age, educational level, marital status, and the number of children in the household.
Part II: This part focuses on professional and work-related information, including monthly income, professional rank, number of work hours per week, number of night shifts per month, and the number of patients under their care during a shift.
Part III: This section addressed daily activities related to the sleep quality of the nurses, including questions about smoking status, tea/coffee consumption, and exercise habits.
Part IV: This section incorporates the Pittsburgh Sleep Quality Index (PSQI), an English version adopted from Buysse et al. (1989). The PSQI is a self-rated scale used to assess the nurses’ sleep quality and sleep disturbances over a one-month interval. The PSQI has nineteen items make up seven sub-dimensions: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficacy, sleep disturbance, use of sleep medication, and daytime dysfunction, each scored 0 (no difficulty) to 3 (severe difficulty). The component scores are summed to produce a global score (range 0 to 21). Higher scores indicate poor sleep quality. A systematic review and meta-analysis study confirmed that the PSQI demonstrated strong reliability and validity, as well as intermediate structural validity, in a variety of samples (Mollayeva et al., 2016). This indicates that the tool serves its intended purpose (Aiken et al., 2002). Nurses who scored five or more on the PSQI global score were classified as having poor sleep, while those who scored less than five were judged to have normal sleep.
The collected data were tabulated and statistically analyzed using the statistical package for social science (SPSS) advanced statistics, version 26. Continuous variables were presented using mean and standard deviation (SD), while categorical variables were expressed as frequency and percentage. t-tests and one-way analysis of variance (ANOVA) were used to examine the association between sleep quality mean scores and categorical variables with two groups (t-test) or more than two groups ANOVA. Multiple linear regression was used for multivariate analyses with the PSQI as the dependent variable, including only significant independent variables in the model and excluding non-significant ones. All tests were conducted at the 0.05 level of statistical significance. In cases of missing data, any responses with incomplete data, whether entirely or partially missing, were excluded from the analyses.
Ethical approval for the study was obtained from the Institutional Review Board (IRB), represented by the Health Cluster in Hail city [registered with the King Abdullah City for Science and Technology (KACS) in the KSA, under the registration number H-08-L-074, with Approval No: 2022-23]. Informed consent was obtained from all participants prior to their engagement in the study. In this research, every participant was briefed on the study’s aims and benefits before they filled out the questionnaire. Their freedom to choose to be part of the study was assured, and confidentiality of their information was guaranteed, with usage limited strictly to research purposes. The survey used were anonymous, ensuring they couldn’t be linked back to the individuals who filled them. The survey didn’t include any identifying details like names or contact info. To enhance the protection of participants’ anonymity, all responses were collected, merged, and then summarized in the final report.
Table 1 shows that most of the respondents (55.6%) aged between 30 and 39 years old, with an overall mean (SD) of 33.1 (6.6). A higher proportion were females (73.6%), married (64.4%), had bachelor’s degrees (69.4%), almost two-thirds of the nurses (42.1%) earned a monthly salary of 6,000–8,000 Saudi Riyal and 47.2% of them were having one to three dependents. Regarding their working status, the results show that the majority of nurses were registered nurses (56.5%), 46.3 of them had night shifts at least 7 times a month, 47.7 % worked for at least 45 h a week, and 56.9 % of them had less than 30 patients admitted per shift. As regards the health-related factors; 44.0 % of the studied nurses had normal BMI, 77.3 % of them took tea and coffee daily, slightly more than half practice smoking daily (50.9%). However, 6.9% of them never smoke, and 58.8% of them were sometimes practicing exercise.
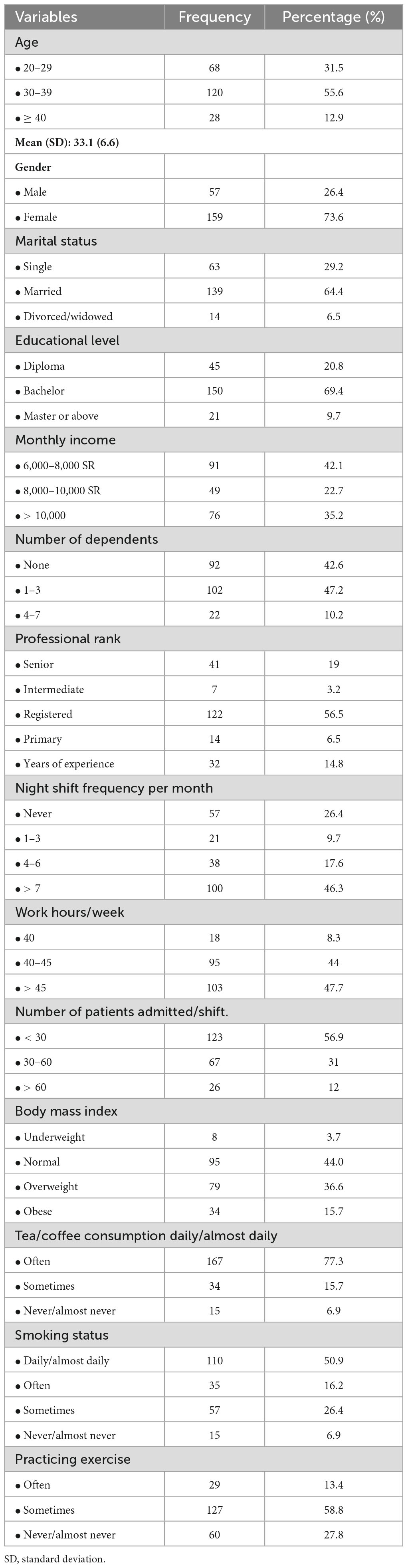
Table 1. Percentage distribution of the studied nurses based on their sociodemographic, work status, and health-related factors (N. 216).
Table 2 reveals that highest mean scores of the PSQI components were for Component 5 (sleep disturbances), Component 1 (subjective sleep quality), Component 3 (sleep duration), and Component 4 (habitual sleep efficiency), with a global mean score of 10.55. It was also notable that the score for the use of sleep medications among nurses is relatively low (1.44), suggesting a relatively infrequent reliance on pharmacological aids for sleep. The mean score for daytime disfunction was 0.42, indicating relatively high efficiency of daily work among the participants even with poor sleep quality.
Figure 1 illustrates that 81.5% of the participants were categorized as having poor sleep quality according to the PSQI scale. Conversely, only 18.5% of them demonstrated normal sleep quality.
As shown in Table 3, the overall mean scores of the PSQI were significantly associated with gender, marital status, monthly income, patient load per shift, and practicing exercise. Female nurses, those who had moderate income, who had higher number of admitted patients per shift, and those who never practice exercise had higher mean PSQI scores indicative of poorer sleep quality compared to other categories (p-value < 0.05). However, there were no significant differences in sleep quality across other variables.
Table 4 Presents that The PSQI of the studied subjects was best predicted by gender, income, and workload (number of patients in the charge of night shift).
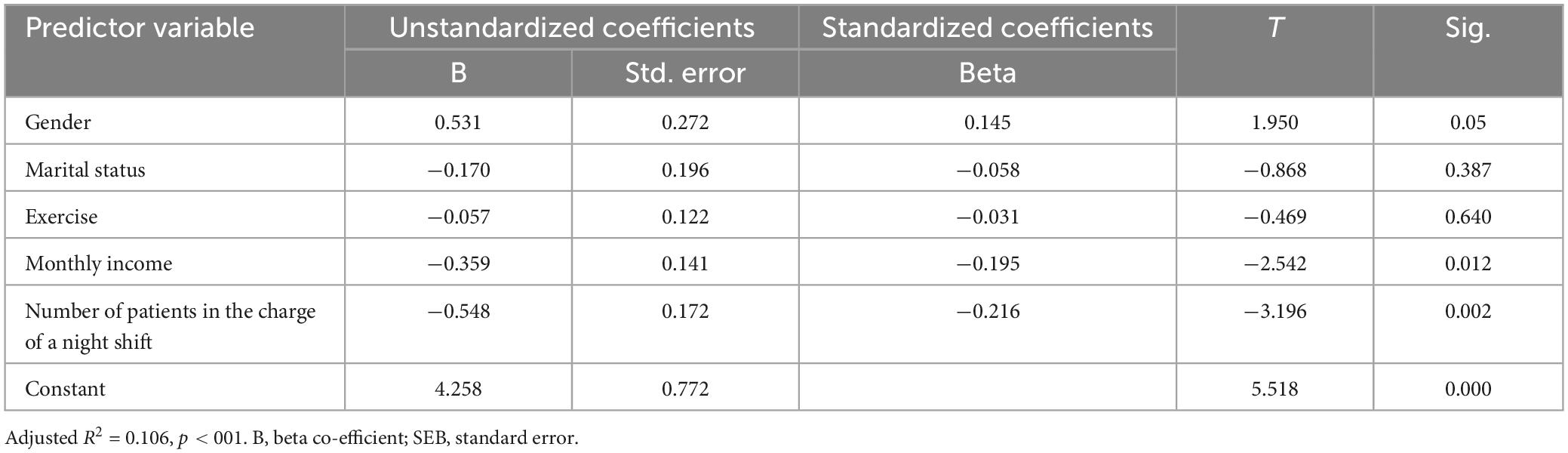
Table 4. Multiple linear regression analyses for some predictor variables and PSQI scores of the studied group.
This study aims to investigate the sleep quality of Saudi emergency nurses during the COVID-19 pandemic and identify the factors influencing it. Sleeping problems are common among nurses and could have a variety of unpleasant effects. A change in sleep quality might impair productivity and lower the standard of nursing care (Dong et al., 2020).
The findings of the current study showed that a majority of respondents (81.5%) experienced poor sleep quality (Figure 1), with a global mean PSQI score of 10.55 (Table 2), indicative of poor sleep quality among nurses. This finding is consistent with findings from other studies, including those by Furihata et al. (2020), Khatony et al. (2020), Qiu et al. (2020), Stimpfel et al. (2020), and Vadi et al. (2022), all of which reported the poor sleep quality is a common problem among nurses. Further supporting this, Dong et al. (2017) found that 64% of nurses reported sleep disturbances within the nursing profession.
The sleep quality among the nurses in this study was found to be associated with gender, as female nurses exhibiting higher instances of poor sleep quality. This observation aligns with the findings of Cattani et al. (2021), who also reported an association between sleep quality and gender. Similarly, Alharbi et al. (2021) noted that being female was linked to poorer sleep. Additionally, Yilmaz et al. (2021), concluded that female nurses were more prone to experiencing poor sleep quality. The observed findings can be interpreted through various ways. Female nurses often have to balance their professional duties with familial caregiving responsibilities (Yilmaz et al., 2021). This dual role can elevate stress levels and limit the time available for restful sleep (DePasquale et al., 2019). Another explanation is the hormonal changes associated with the menstrual cycle, pregnancy, and menopause can profoundly affect sleep patterns, as noted by Baker and Lee (2022). Societal and cultural expectations can influence sleep quality. In many cultures, women face additional pressures that can lead to increased stress and disrupted sleep (Knutson, 2013). Additionally, some studies have proposed that women are generally more likely than men to recognize and report problems associated with sleep disturbances (Knutson, 2013).
Furthermore, a link was found between sleep quality and monthly income, where emergency nurses earning lower salaries experienced more sleep difficulties. This finding aligns with Gao et al. (2022) research, which identified low monthly income as a contributing factor to poor sleep quality in most participants. Similarly, a study conducted in Jordan by Suleiman et al. (2020) established a positive correlation between the amount of salary and sleep quality, further emphasizing the impact of income on sleep. The findings can be attributed to several factors. Financial stress from lower income can increase anxiety and worry, adversely affecting sleep. Additionally, lower income often limits access to a conducive sleep environment, potentially resulting in less comfortable living conditions and exposure to disruptive factors like noise and inadequate temperature control (Johnson et al., 2018).
Besides personal factors, the study found that the quantity of patients a nurse managed per shift associated negatively with their sleep quality (the higher the number of patients, the higher PSQI scores and poor sleep). This aligns with findings from a French longitudinal cohort study by Badahdah et al. (2020), which connected sleep issues to both intensive labor and extended workdays. Supporting this, research by Dong et al. (2017) and Dong et al. (2020) suggests that primary and registered nurses are particularly prone to sleep disorders. Factors such as longer working hours and the patient load per shift were also identified as contributors to reduced sleep quality. Dealing with more patients, especially in an ED setting, often involves managing critical and high-stress situations. This can lead to emotional and mental fatigue, which makes it harder to unwind and achieve restful sleep.
Our study’s results show that sleep quality was not significantly associated with sociodemographic factors such as age, education level, and professional rank. This aligns with findings by Johnson et al. (2018) and Segon et al. (2022), who also reported no significant correlation between age, educational status, and sleep deprivation. In addition, Badahdah et al. (2020) and Wang et al. (2021) observed no substantial link between poor sleep quality and professional rank in their research.
The current findings indicate a statistically significant difference in the PSQI total scores among nurses in relation to their exercise habits. This might be due to the stress-reducing effects of exercise, which in turn could improve sleep quality. This observation is consistent with the studies by Strand et al. (2013) and Chen et al. (2022), which noted that the frequency of exercise positively influenced the sleep quality of nurses.
Our study’s results indicate that there was no significant association between poor sleep quality and habits like smoking or consuming tea and coffee. This contrasts with the findings of Strand et al. (2013), Omar et al. (2022), and Sayik et al. (2022), who observed that both smokers and tea/coffee drinkers tended to have lower overall PSQI-mean scores, suggesting poorer sleep quality. This difference in findings could be attributed to factors such as the timing and quantity of smoking or caffeine consumption. Specifically, consuming caffeine later in the day may have a more significant impact on sleep compared to morning intake. This variable, which can crucially affect sleep quality, might not have been consistently accounted for across different studies. Additionally, it’s noteworthy that our study did not measure these aspects, which could further explain the variation in results.
In relation to predictor variables of sleep quality, the present study showed that sleep quality among the studied subjects was best predicted by gender, income, and workload (number of patients in the charge of night shift), answering research question (2). These findings were in the same line with (Kim-Godwin et al., 2021), who pointed out that the nurses working full time (t = 2.41, p = 0.02), showed poor overall sleep quality. While these findings contradicted (Chen et al., 2022) who revealed that nurse managers’ sleep quality can be greatly affected by demographic characteristics such as their ages and exercise regularity.
This study has several limitations that should be considered. Firstly, the cross-sectional nature of the research design prevents the establishment of cause-and-effect relationships. Secondly, focusing on a specific government institution in the northern region of Saudi Arabia raises concerns regarding selection bias, thus limiting the generalizability of the findings. Additionally, exclusively including emergency nurses, may not accurately reflect the experiences of nurses in other specialties or departments, cautioning against extrapolating these findings to a broader nursing population. Furthermore, the study did not account for some potentially relevant factors, such as the psychological impact of the COVID-19 pandemic, individual health conditions, or personal coping mechanisms, which might influence sleep quality. Moreover, there is a possibility that some observed disturbances may be normative rather than solely attributable to the pandemic. Factors beyond the pandemic, such as societal stressors and individual circumstances, may contribute to sleep disruptions during the study period. Therefore, we encourage future research to explore these complexities further, ensuring a nuanced understanding of sleep disturbances in the context of both pandemics and broader societal influences. Finally, the study failed to explore the influence of COVID-related stress on sleep quality among nurses. This overlooks a crucial aspect of their wellbeing, particularly in high-stress environments like EDs during the pandemic. Future research should examine this association to provide a more comprehensive understanding of nurses’ sleep patterns.
The study reveals a high prevalence of poor sleep quality among emergency nurses during the COVID-19 pandemic. Factors such as gender, marital status, monthly income, the number of patients managed per shift, and exercise habits significantly associated with poor sleep quality in this group. These findings underline the multifaceted nature of sleep disturbances in a high-stress healthcare environment and emphasize the need for targeted interventions to address these issues. Healthcare institutions should consider implementing policies and programs aimed at improving sleep quality among nurses. This could include scheduling reforms to reduce overwork, stress reduction workshops, and health promotion activities that encourage exercise. Creating a support system within the workplace to address the unique challenges faced by different demographic groups, such as female nurses or those with lower incomes, is also crucial.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval for the study was obtained from the Institutional Review Board (IRB), represented by the Health Cluster in Hail city [registered with the King Abdullah City for Science and Technology (KACS) in the KSA, under the registration number H-08-L-074, with Approval No: 2022-23]. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
AwA: Writing – original draft, Writing – review & editing. MA: Writing – original draft, Writing – review & editing. BA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. FA: Writing – original draft, Writing – review & editing. AsA: Writing – original draft, Writing – review & editing. TAA: Writing – original draft, Writing – review & editing. SM: Writing – original draft, Writing – review & editing. DC: Writing – original draft, Writing – review & editing. MB: Writing – original draft, Writing – review & editing. AhA: Writing – original draft, Writing – review & editing. OE: Writing – original draft, Writing – review & editing. SN: Writing – original draft, Writing – review & editing. RA: Writing – original draft, Writing – review & editing. TNA: Writing – original draft, Writing – review & editing. HA: Writing – original draft, Writing – review & editing. BS: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.
The authors declare that financial support was received for the research, authorship, and/or publication of this article. This research has been funded by the Scientific Research Deanship at University of Hail-Saudi Arabia through project number BA-22 038.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abraham, O., Pu, J., Schleiden, L. J., and Albert, S. M. (2017). Factors contributing to poor satisfaction with sleep and healthcare seeking behavior in older adults. Sleep Health 3, 43–48.
Aiken, L., Clarke, S., Sloane, D., Sochalski, J., and Silber, J. (2002). Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 288, 1987–1993.
Alharbi, A. S., Alshahrani, S. M., Alsaadi, M. M., Al-Jahdali, H. H., Wali, S. O., and BaHammam, A. S. (2021). Sleep quality and insomnia during the COVID-19 lockdown among the Saudi public: A cross-sectional study. Saudi Med. J. 42:384.
Almeida, M., Shrestha, A., Stojanac, D., and Miller, L. (2020). The impact of the COVID-19 pandemic on women’s mental health. Arch. Womens Ment. Health 23, 741–748.
Alshammari, B., AlEnazy, A., Alshammari, F., Madkhali, N., and Al-Masaeed, M. (2022). Investigation of the level and factors influencing emergency department nurses fatigue: A case study of the Saudi Arabian context. Healthcare 10:1294.
Alshammari, B., Alkubati, S. A., Pasay-An, E., Alrasheeday, A., Alshammari, H. B., Asiri, S. M., et al. (2023). Sleep quality and its affecting factors among Hemodialysis patients: A Multicenter cross-sectional study. Healthcare 11:2536.
Badahdah, A. M., Khamis, F., and Al Mahyijari, N. (2020). Sleep quality among health care workers during the COVID-19 pandemic. J. Clin. Sleep Med. 16, 1635–1635.
Bae, S.-H., and Fabry, D. (2014). Assessing the relationships between nurse work hours/overtime and nurse and patient outcomes: Systematic literature review. Nurs. Outlook 62, 138–156.
Baker, F. C., and Lee, K. A. (2022). Menstrual cycle effects on sleep. Sleep Med. Clin. 17, 283–294.
Buysse, D., Reynolds, C., Monk, T., Berman, S., and Kupfer, D. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213.
Cattani, A. N., Silva, R. M., Beck, C. L. C., Miranda, F. M. D. A., Dalmolin, G. L., and Camponogara, S. (2021). Evening work, sleep quality and illness of nursing workers. Acta Paulista Enfermagem 34:843.
Chen, R., Fang, P., Tan, L., Li, J., and Yu, L. (2022). Factors associated with sleep quality among nurse managers during regular prevention and control of the COVID-19 in China: A cross-sectional study. BMC Nurs. 21:363. doi: 10.1186/s12912-022-01149-w
DePasquale, N., Sliwinski, M. J., Zarit, S. H., Buxton, O. M., and Almeida, D. M. (2019). Unpaid caregiving roles and sleep among women working in nursing homes: A longitudinal study. Gerontologist 59, 474–485.
Dong, H., Zhang, Q., Sun, Z., Sang, F., and Xu, Y. (2017). Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry 17:241. doi: 10.1186/s12888-017-1402-3
Dong, H., Zhang, Q., Zhu, C., and Lv, Q. (2020). Sleep quality of nurses in the emergency department of public hospitals in China and its influencing factors: A cross-sectional study. Health Q. Life Outcomes 18, 1–9.
Du, C., Wang, W., Hsiao, P., Ludy, M., and Tucker, R. (2021). Insufficient sleep and poor sleep quality completely mediate the relationship between financial stress and dietary risk among higher education students. Behav. Sci. 11:69.
Fawaz, M., Anshasi, H., and Samaha, A. (2020). Nurses at the front line of COVID-19: Roles, responsibilities, risks, and rights. Am. J. Trop. Med. Hyg. 103:1341.
Furihata, R., Saitoh, K., Suzuki, M., Jike, M., Kaneita, T. O., Buysse, D. J., et al. (2020). A composite measure of sleep health is associated with symptoms of depression among Japanese female hospital nurses. Compr. Psychiatry 97:152151.
Gao, C., Wang, L., Tian, X., and Song, G.-M. (2022). Sleep quality and the associated factors among in-hospital nursing assistants in general hospital: A cross-sectional study. Heliyon 8:e09393.
Guerrera, C. S., Boccaccio, F. M., Varrasi, S., Platania, G. A., Coco, M., Pirrone, C., et al. (2024). Narrative review on insomnia and hypersomnolence within major depressive disorder and bipolar disorder: A proposal for a novel psychometric protocol. Neurosci. Biobehav. Rev. 158:105575.
Hoedl, M., Eglseer, D., and Bauer, S. (2021). Associations between personal protective equipment and nursing staff stress during the COVID-19 pandemic. J. Nurs. Manag. 29, 2374–2382.
Johnson, D. A., Billings, M. E., and Hale, L. (2018). Environmental determinants of insufficient sleep and sleep disorders: Implications for population health. Curr. Epidemiol. Rep. 5, 61–69.
Khatony, A., Zakiei, A., Khazaie, H., Rezaei, M., and Janatolmakan, M. (2020). International nursing: A study of sleep quality among nurses and its correlation with cognitive factors. Nurs. Admin. Q. 44, E1–E10.
Kim-Godwin, Y., Lee, M., Logan, J., and Liu, X. (2021). Factors influencing sleep quality among female staff nurses during the early COVID-19 pandemic in the United States. Int. J. Environ. Res. Public Health 18:4827.
Knutson, K. L. (2013). Sociodemographic and cultural determinants of sleep deficiency: Implications for cardiometabolic disease risk. Soc. Sci. Med. 79, 7–15.
Kredlow, M., Capozzoli, M., Hearon, B., Calkins, A., and Otto, M. (2015). The effects of physical activity on sleep: A meta-analytic review. J. Behav. Med. 38, 427–449.
Krueger, P. M., and Friedman, E. M. (2009). Sleep duration in the United States: A cross-sectional population-based study. Am. J. Epidemiol. 169, 1052–1063.
Madkhali, N. A., Ameri, A., Al-Naamani, Z. Y., Madkhali, M. A., Alshammari, B., and ALMeqbali, M. A. (2022). Has the COVID-19 pandemic affected the psychological state of Arab cancer patients? Curr. Psychol. 21, 1–12.
Mollayeva, T., Thurairajah, P., Burton, K., Mollayeva, S., Shapiro, C. M., and Colantonio, A. (2016). The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 25, 52–73.
Omar, D., Hassan, O., and Hani, B. (2022). Sleep quality and its determinants among nurses during COVID-19 pandemic. Egypt J. Occup. Med. 46, 75–92.
Pollard, C. A., Morran, M. P., and Nestor-Kalinoski, A. L. (2020). The COVID-19 pandemic: A global health crisis. Physiol. Genom. 52, 549–557.
Qiu, D., Yu, Y., Li, R.-Q., Li, Y.-L., and Xiao, S.-Y. (2020). Prevalence of sleep disturbances in Chinese healthcare professionals: A systematic review and meta-analysis. Sleep Med. 67, 258–266.
Sayik, D., Acikgoz, A., and Kaya, S. (2022). Anxiety and sleep quality levels of emergency medical personnel and factors affecting them during the coronavirus disease-2019 pandemic/COVID-19 pandemisinde acil servis calisanlarinin anksiyete ve uyku kalitesi duzeyleri ve etkileyen faktorlerin belirlenmesi. J. Turk. Sleep Med. 9, 27–37.
Segon, T., Kerebih, H., Gashawu, F., Tesfaye, B., Nakie, G., and Anbesaw, T. (2022). Sleep quality and associated factors among nurses working at comprehensive specialized hospitals in Northwest, Ethiopia. Front. Psychiatry 13:931588. doi: 10.3389/fpsyt.2022.931588
Stimpfel, A. W., Fatehi, F., and Kovner, C. (2020). Nurses’ sleep, work hours, and patient care quality, and safety. Sleep Health 6, 314–320.
Strand, L. B., Laugsand, L. E., Wisløff, U., Nes, B. M., Vatten, L., and Janszky, I. (2013). Insomnia symptoms and cardiorespiratory fitness in healthy individuals: The Nord-Trøndelag health study (HUNT). Sleep 36, 99–108.
Suleiman, K., Hijazi, Z., Kalaldeh, M. A., and Sharour, L. A. (2020). Factors associated with sleep quality among emergency nurses in Jordan. Sleep Vigil. 4, 11–16.
Troxel, W. M., Robles, T. F., Hall, M., and Buysse, D. J. (2007). Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Med. Rev. 11, 389–404.
Vadi, S., Shah, S., Bajpe, S., George, N., Santhosh, A., Sanwalka, N., et al. (2022). Mental health indices of intensive care unit and emergency room frontliners during the severe acute respiratory syndrome coronavirus 2 pandemic in India. Indian J. Crit. Care Med. 26:100.
Wang, B., Lu, Q., Sun, F., and Zhang, R. (2021). The relationship between sleep quality and psychological distress and job burnout among Chinese psychiatric nurses. Ind. Health 59, 427–435.
Wardle-Pinkston, S., Slavish, D. C., and Taylor, D. J. (2019). Insomnia and cognitive performance: A systematic review and meta-analysis. Sleep Med. Rev. 48:101205.
Yilmaz, M., Kıraç, Y., and Sahin, M. K. (2021). Sleep quality and related factors in a sample of Turkish healthcare workers during the COVID-19 pandemic: A cross-sectional study. Int. J. Clin. Pract. 75:e14813.
Keywords: emergency nurses, factors, sleep quality, COVID-19, sleep disturbances
Citation: Alrasheeday A, Alsaeed MA, Alshammari B, Alshammari F, Alrashidi AS, Alsaif TA, Mahmoud SK, Cabansag DI, Borja MV, Alsayed AR, Elalem OM, Nageeb SM, Allam RA-E, Alhejaili TN, Alsulami HF and Siam BGAE (2024) Sleep quality among emergency nurses and its influencing factors during COVID-19 pandemic: a cross-sectional study. Front. Psychol. 15:1363527. doi: 10.3389/fpsyg.2024.1363527
Received: 30 December 2023; Accepted: 03 July 2024;
Published: 19 July 2024.
Edited by:
Changiz Mohiyeddini, Oakland University William Beaumont School of Medicine, United StatesReviewed by:
Claudia Savia Guerrera, Department of Biomedical and Biotechnological Science, ItalyCopyright © 2024 Alrasheeday, Alsaeed, Alshammari, Alshammari, Alrashidi, Alsaif, Mahmoud, Cabansag, Borja, Alsayed, Elalem, Nageeb, Allam, Alhejaili, Alsulami and Siam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bushra Alshammari, YnUuYWxzaGFtbWFyaUB1b2guZWR1LnNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.