- 1Southern Synergy, Department of Psychiatry, School of Clinical Sciences at Monash Health, Monash University, Melbourne, VIC, Australia
- 2Mindfulness-integrated Cognitive Behavior Therapy Institute, Hobart, TAS, Australia
- 3Department of Psychiatry, University of British Columbia, Vancouver, BC, Canada
- 4Mental Health Program, Monash Health, Melbourne, VIC, Australia
- 5Melbourne School of Population and Global Health, University of Melbourne, Melbourne, VIC, Australia
- 6School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC, Australia
- 7School of Primary and Allied Health Care, Monash University, Melbourne, VIC, Australia
It is important to be able to differentiate mindfulness-based programs in terms of their model, therapeutic elements, and supporting evidence. This article compares mindfulness-based cognitive therapy (MBCT), developed for relapse prevention in depression, and mindfulness-integrated cognitive behavior therapy (MiCBT), developed for transdiagnostic applications, on: (1) origins, context and theoretical rationale (why), (2) program structure, practice and, professional training (how), and (3) evidence (what). While both approaches incorporate behavior change methods, MBCT encourages behavioral activation, whereas MiCBT includes various exposure procedures to reduce avoidance, including a protocol to practice equanimity during problematic interpersonal interactions, and a compassion training to prevent relapse. MBCT has a substantial research base, including multiple systematic reviews and meta-analyses. It is an endorsed preventative treatment for depressive relapse in several clinical guidelines, but its single disorder approach might be regarded as a limitation in many health service settings. MiCBT has a promising evidence base and potential to make a valuable contribution to psychological treatment through its transdiagnostic applicability but has not yet been considered in clinical guidelines. While greater attention to later stage dissemination and implementation research is recommended for MBCT, more high quality RCTs and systematic reviews are needed to develop the evidence base for MiCBT.
Introduction
In the last 40 years, there has been an extraordinary take-up of mindfulness-based programs (MBPs) in both clinical and well-being contexts. Many different programs are now available (Creswell, 2017), and many of these have been based on, or adapted from, Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn, 1990; Crane et al., 2017). This program, created initially to address chronic pain, was inspired by Asian meditation and yogic traditions including Zen and Vipassana practices to teach about the mind–body connection. MBSR utilizes mindfulness exercises, meditation and yoga and had a focus on regulating attention (Kabat-Zinn, 1982). Subsequently, key elements of MBSR were adapted to develop Mindfulness-Based Cognitive Therapy for Depression (MBCT; Segal et al., 2002, 2013), a group intervention to promote relapse prevention in recurrent depression based on the cognitive model of depressive relapse. In contrast to MBCT, Mindfulness-integrated Cognitive Behavior Therapy (MiCBT) was developed with transdiagnostic mental health applications in mind, piloted in psychiatric populations with both moderate and severe symptoms, and designed for both individual and group contexts (Cayoun, 2011, 2015; Cayoun et al., 2019). Because it is transdiagnostic, MiCBT can also address comorbidities (Barlow et al., 2004) and it is increasingly being used to promote well-being and personal growth in the general community (Cayoun, 2015).
The aim of this paper is to inform clinicians and researchers about the unique features of MiCBT and MBCT to enable appropriate referrals and assist with decisions to pursue professional training and research pathways. As noted by Kazdin (2016), with the large number of evidence-based treatments (EBTs) now available, “a key challenge is disseminating EBTs so they are used in clinical practice. Extending EBTs to practice has enormous challenges of its own beginning with what to train among the burgeoning list of treatments.” (p. 428). It has been suggested that examining the similarities and differences between MBPs will assist in refining understanding of their respective clinical applications (Chiesa and Malinowski, 2011). To this end, the objectives of this article are to: describe and compare the origins, theoretical models, and therapeutic elements of MiCBT and MBCT to promote a deep understanding of why and how they are applied to treat their target clinical populations; to consider what their corresponding evidence base is; then consider the implications of this comparative review for clinical applications.
Origins and theory
The original naming of the three MBPs provides interesting insight into the respective developers’ initial conceptualizations. MBSR started out as “Stress Reduction and Relaxation Program” (Kabat-Zinn, 1982) as Kabat-Zinn wanted to introduce mindfulness and meditation practices to Western medical settings, and, to increase acceptability, intentionally did not explicitly emphasize their Buddhist roots. It wasn’t until the 1990s that the name “Mindfulness-Based Stress Reduction” was formally used for the program (Kabat-Zinn, 2011). Additionally, the word “stress” had already been popularized in the medical community, for whom the Buddhist use of the word “suffering” may have been less defined (Kabat-Zinn, 1990, p. 235). The original name for MBCT was ‘Attention Control Training’ (Teasdale et al., 1995) because learning to skillfully deploy one’s attention was seen as a central process to the prevention of depressive relapse (Dimidjian et al., 2010). MiCBT was initially implemented in 2001 as ‘Equanimity Training’ as an intervention for acute conditions and relapse prevention across disorders, because of the focus on developing equal interest, acceptance and non-reactivity towards body sensations regardless of their affective valence, especially during distressing experiences (Cayoun et al., 2004).
Mindfulness was defined by Kabat-Zinn as “paying attention in a particular way; on purpose, in the present moment, and non-judgmentally” (Kabat-Zinn, 1994, p. 4). This definition was adopted in the first edition of the MBCT manual (Segal et al., 2002, p. 121) but later amended to include awareness: “the awareness that emerges from paying attention, on purpose, in the present moment, and nonjudgmentally” (Segal et al., 2013, p. 132). This wording aligns with a consensus-developed definition published in 2004: “We see mindfulness as a process of regulating attention in order to bring a quality of nonelaborative awareness to current experience and the quality of relating to one’s experience within an orientation of curiosity experiential openness and acceptance. We further see mindfulness as a process of gaining insight into the nature of one’s mind and the adoption of a de-centered perspective (Safran and Segal, 1990) on thoughts and feelings” (Bishop et al., 2004, p. 230). In MiCBT, the definition of mindfulness overlapped, but includes the central role of equanimity, the non-reactive component of mindfulness, as understood in from its Buddhist roots. Accordingly, mindfulness is considered to be achieved through the development of experiential awareness and equanimity “in such a way that we can perceive our experiences, understand them and respond to them without needing to react in order to change them. This includes experiences that are taking place within the mind and body” (Cayoun, 2015).
MiCBT origins and theory
Following over a decade of conceptualization and development beginning in 1989, MiCBT (Cayoun, 2011; Cayoun et al., 2019) emerged in Australia independently, but at a similar time to the publication of the first MBCT text (Segal et al., 2002). The initial name of Equanimity Training (2001–2003) became Mindfulness-based CBT (MCBT) from 2003–2006 then finalized as MiCBT from 2006 to avoid confusion with MBCT (Cayoun, 2011). MiCBT arose from Cayoun’s interest in bringing Vipassana meditation into a scientific and clinical context to assist with transcending the sources of unnecessary suffering (Cayoun et al., 2019). MiCBT was developed as a manualized transdiagnostic psychological treatment based on an integration of mindfulness meditations (in the Burmese Vipassana lineage of Ledi Sayadaw and U Ba Khin, as taught by Satya Narayan Goenka; Hart, 1987) with cognitive and behavioral therapy principles and methods. The first formal pilot evaluation commenced in 2003 in a psychiatric hospital setting (Cayoun et al., 2004). Further piloting and refinement took place until 2010, culminating in the first published MiCBT clinical text and manualized protocol (Cayoun, 2011). The MiCBT program, while retaining its structure and content, has been revised from 8- to 10-weeks duration (Cayoun, 2011; Cayoun et al., 2019). For further details on the history of MiCBT, see Cayoun et al. (2019).
MiCBT incorporates the four types of mindfulness trainings originally taught in Buddhist teaching on “The Establishment of Mindfulness,” the Satipatthana Sutta (Ñāṇamoli and Bodhi, 2005). These include mindfulness of the body (posture and movement), body sensations (interoception and hedonic tone), mental states (e.g., moods; aversive, craving, and mindful states), and mental qualities (presence of various types of thoughts). MiCBT emphasizes the importance of developing non-reactive interoceptive awareness through mindfulness of body sensations. Interoception, the ability to sense internal signals from the body, allows the perception of hedonic tone or valence (feeling pleasant, unpleasant and neither pleasant nor unpleasant body sensations) associated with emotional experiences (Barrett, 2006; Pollatos and Schandry, 2008). As training in mindfulness of body sensations improves the capacity for interoception, one becomes increasingly emotionally aware (Gibson, 2019). It is now well documented that emotional reactivity, conscious or not, is dependent on interoceptive experience (Menon and Uddin, 2010; Uddin, 2015; Zamariola et al., 2019). Numerous studies have demonstrated that interoception is impaired to varying degrees in mental health disorders (Garfinkel and Critchley, 2013; Khalsa et al., 2018; Zamariola et al., 2019) and impaired interoceptive awareness is a major contributor to emotional reactivity (Rae et al., 2019).
Reactivity to emotional valence is expressed through craving for pleasant sensory experiences and avoidance of unpleasant ones. According to the teaching of the Goenka lineage, difficulty in managing emotional reactivity is maintained by lack of awareness that this reactive process is continually taking place (Hart, 1987). The development of wise, compassionate equanimity to all arising internal phenomena is seen as a skillful way to navigate suffering (Hart, 1987; Batchelor, 2018). In the psychological literature, equanimity has been defined as “an even-minded mental state or dispositional tendency toward all experiences or objects, regardless of their affective valence (pleasant, unpleasant or neutral) or source” (Desbordes et al., 2015, p. 4). Equanimity enables the hedonic experience to be decoupled from action choices (Hadash et al., 2016). Consequently, equanimity towards interoceptive signals facilitates emotion regulation (Füstös et al., 2013; Hadash et al., 2016).
MiCBT incorporates exposure and other behavior change techniques from CBT which have been demonstrated to be effective strategies in treating various types of anxiety and depressive disorders, and other related conditions (Barlow et al., 2004). In MiCBT, behavior change strategies incorporate operant learning principles and are guided by the co-emergence model of reinforcement (Figure 1), which underpins the program’s theoretical framework and rationale. The model describes the relationship between a stimulus event, the way this is processed cognitively, the co-arising sensations in the body and the subsequent reaction or response. This model is derived from Theravada Buddhist teachings on “the five aggregates” of information processing (Bodhi, 2003) and the neurophenomenology of behavior (see Cayoun and Shires, 2020).
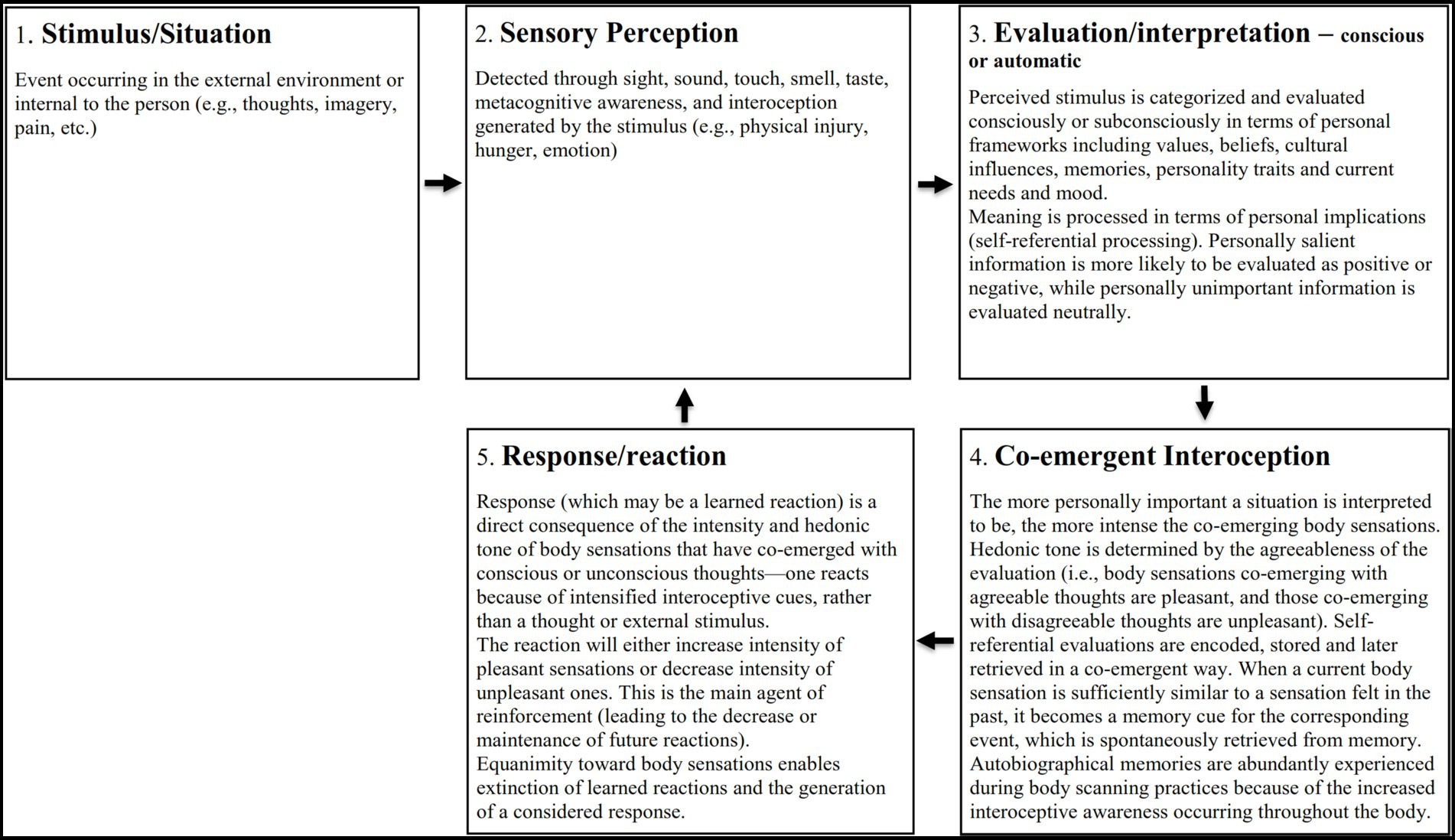
Figure 1. The co-emergence model of reinforcement in equilibrium state (Adapted from Cayoun, 2011).
Figure 1 shows the model components in their equilibrium state. In summary, a stimulus is perceived (Sensory Perception) through the senses (sight, touch, smell, taste, sound) or through awareness of thoughts or interoception, and is immediately consciously or subconsciously interpreted and evaluated (Evaluation). The stimulus is evaluated in terms of its personal significance, determined by cognitive factors such as values, beliefs, memories, personality traits, current mood, perceived needs, and culture. This causes Co-emerging Interoception of pleasant, unpleasant, or neutral body sensations to arise synchronously with evaluative thinking (see Cayoun and Shires, 2020, for discussion of neural correlates). If the co-emerging body sensations are sufficiently intense, a Reaction, (the next component of the model), is likely to occur. Reinforcement takes place if the reaction leads to a decrease in unpleasant body sensations or an increase in pleasant ones.
Hence, the model proposes that the reinforcement of behavior depends on the response to co-emerging interoception, rather than a response to the stimulus. This is theoretically consistent with learning theory (Mowrer and Klein, 2000) but differs from Skinner’s standard operant conditioning model, which assumes that “the behavior operates upon the environment to generate consequences” (Skinner, 1953, p. 65).
When well-being is disturbed, a disequilibrium state occurs, in which the Evaluation and Reaction functions predominate, causing the Sensory Perception and Co-emerging Interoception functions to be depleted. When the predominance of self-referential evaluation and reactivity becomes habitual, the disequilibrium state is established, facilitating the persistence of mental health conditions and the strengthening of reactive personality traits (Cayoun et al., 2019). The ability to pay attention to the precise nature of arising body sensations without reacting to them deepens perception of current internal experience and develops equanimity. As equanimity develops, reactivity decreases (Hadash et al., 2016) and a state of equilibrium between components can be restored. Consequently, reappraisal of beliefs about experience becomes possible. This principle is applied across the four stages of MiCBT (discussed below), where interoceptive desensitization is central to behavior change. In summary, co-emergence theory posits that cognition and interoception co-emerge bidirectionally, and being overly judgmental and reactive reduces sensory perception and interoceptive awareness, causing disequilibrium in the system, which may become learned over time and promote mental health disorders. Since interoceptive deficit and emotional hyper-and hypo-reactivity are common in emotional disorders, the development of equanimity towards interoceptive cues has transdiagnostic applicability. The co-emergence model of reinforcement is described in further detail elsewhere (Cayoun, 2011; Cayoun et al., 2019; Cayoun and Shires, 2020).
MBCT origins and theory
MBCT is focused on mental health (depression in the first iteration) and, as such, targets specific conditions, departing from the transdiagnostic approach of MBSR in which the term ‘stress’ subsumes a multitude of conditions including stress, pain and medical illness (Kabat-Zinn, 2011). MBCT was designed as an eight-week manualized group training program for prevention of depressive relapse and includes mindfulness exercises and aspects of cognitive therapy (CT) for depression (Segal et al., 2002, 2013). The mindfulness elements of MBCT are mostly adapted from MBSR which in turn, and like MiCBT, are informed by the Satipatthana meditation methods (Kabat-Zinn, 1982). The one exception to this is the 3-min breathing space exercise which was introduced in MBCT as a mini-practice to be utilized at any point throughout the day (Teasdale et al., 2014).
MBCT developed out of a quest to create a maintenance version of CT for patients in remission, building on acute-phase CT which had been shown to reduce rates of depressive relapse (Segal et al., 2002). The developers were attracted to the affective and cognitive strategies in MBSR (Dimidjian et al., 2010), in particular, the ability of the program to focus on “learning to deploy one’s attention in specific and intentional ways, a skill that seemed highly relevant to helping patients notice early warning signs of depression” (Dimidjian et al., 2010, p. 309). Furthermore, the developers were impressed by the ability of MBSR participants to develop awareness of their own thought and thinking processes, decentering from thoughts to facilitate clear-sightedness (Segal et al., 2013).
After initially unsuccessfully trialing a 20-min mindfulness practice adapted from MBSR as part of Attentional Control Training (Teasdale et al., 1995), the developers observed that MBSR also included asking participants to have a welcoming attitude towards all experience, thus extending their earlier conceptualization of decentering to encompass “even the most intense negative experiences utilizing decentering more widely and deeply than we did” (Segal et al., 2013, p. 59). This represented a significant shift from the traditional CT method of reducing difficult emotions by working to modify thoughts and solve problems to an approach that focused on changing the attitude to thoughts and all experiences. Several other techniques from CT and CBT were incorporated into MBCT including activity scheduling, thought monitoring, differentiating thoughts from facts, promoting cognitive rehearsal, becoming aware of dysfunctional attitudes, and developing an early warning system and relapse prevention plan (Segal et al., 2002).
MBCT is primarily described in terms of a cognitive theoretical perspective rather than the Buddhist-based origins of MBSR (Segal et al., 2013). The MBCT program is based on an enhancement of cognitive theory using the information-processing theory of depressive relapse (Teasdale et al., 1995) and integrating mindfulness. The Interactive Cognitive Subsystems model suggested by Barnard and Teasdale (1991) proposes a ‘central engine’ in which sensory information is either coded in a propositional (factual) way or in an implicational (self-referential) way, in terms of its personal importance. Implicational thinking in which self-oriented ruminative thinking may create negative self-schemas then prolongs depressive symptoms (Nolen-Hoeksema and Morrow, 1991; Teasdale et al., 1995).
The cognitive model of depression typically posits that symptoms of depression develop from irrational assumptions or beliefs (implicational thinking) resulting in automatic negative thoughts that are associated with unpleasant emotions (Hawton et al., 1989). Incidents can trigger a dysfunctional belief that sets in motion a vicious cycle in which the more one becomes depressed, the more one engages with and believes the depressive thoughts, establishing schematic thought patterns. Accordingly, relapse prevention was initially proposed to be accomplished by modifying the dysfunctional schema (Hawton et al., 1989). However, among populations receiving CT for depression, rates of depressive relapse continued to be high, between 30 and 40% (Lin et al., 1998; Van Weel-Baumgarten et al., 2000) and new strategies to decrease this were sought. The role of a more metacognitive mode of processing information described as distancing or ‘decentering’ from thoughts, was proposed as a possible mediator of cognitive therapy’s effects (Ingram and Hollon, 1986). It was this quest to develop a therapy that focused on cultivating decentering that led to the development of MBCT, as outlined above.
The core skills taught in MBCT are awareness of thoughts and feelings, control of attention towards thinking patterns, decentering from thoughts to prevent being caught up in them, and the ability to experience present reality as it is (Teasdale et al., 2002). This more accepting and acknowledging stance towards thoughts and the maintenance of attention (e.g., on breath) provides alternatives to elaborative, ruminating thinking. There is evidence to suggest that MBCT improves attentional capacity (Jha et al., 2007; Semple, 2010; Grossman, 2011). MBCT describes attachment and aversion as important drivers of thinking patterns (Segal et al., 2002) and in the revised protocol examines ‘feeling tone’, described as “each experience we have …automatically evokes a feeling that is pleasant, unpleasant or neutral” (Segal et al., 2013, p. 217). Feeling tone is described as subtle, and often below the conscious threshold of awareness, but key therapeutically, as pleasant feeling tone is habitually reacted to with attachment, unpleasant feeling tone with aversion, and neutral feeling tone with disconnection and boredom. MBCT focuses on aversion as it “is at the root of all the states of mind that underlie relapse in depression” (Segal et al., 2013, p. 217); the focus on aversion to unpleasant feeling tone is specifically applied to the consequences of challenging thoughts and rumination.
Program structure and practices
MiCBT program structure and practices
MiCBT is delivered in four stages. Stage 1 (personal stage) focuses on experiential-awareness and regulation of attention and emotions through mindfulness meditation; Stage 2 (exposure stage) is a behavior-regulation stage integrating mindfulness meditation with exposure methods; Stage 3 (interpersonal stage) focuses on developing mindfulness-based interpersonal skills using the tools developed in the previous two stages; Stage 4 (empathic stage) is a transpersonal regulation stage to help prevent relapse by developing a sense of interconnectedness through integrating mindfulness, compassion and ethics for the maintenance of well-being.
Practices in MiCBT, whether delivered individually or in groups, are scheduled in a specific sequence to develop metacognitive insight, interoceptive awareness, and equanimity. These skills are then used to assist with understanding the relationship between unhelpful thinking, co-emerging body sensations and consequent affective reactivity. Reflection on, and engagement with, the practices of both meditation and behavioral tasks are facilitated using Socratic questioning. Prior to the first session, a standard clinical assessment is done, commitment to self-care practices is established, targeted problems are identified, and success indicators are proposed for each issue. A week-by-week summary of the program is provided in Supplementary Table S1. To begin with, patients practice daily progressive muscle relaxation to establish a regular self-care practice and to bring awareness to body, posture, movements, and tensions throughout the day and to anchor their attention in the present. In the second session, mindfulness of breath meditation is taught to develop metacognitive awareness and insight. The practice requires sustaining attention on the sensations associated with the breath at the entrance of the nostrils, without controlling the breath in any way. Participants sit upright and are instructed to focus on the breath, noticing thoughts arising without engaging or identifying with them, calmly shifting attention back to the breath when their mind wanders (Cayoun, 2011).
From session three onwards, a series of body-scanning techniques in the ancient Theravadin tradition of U Ba Khin and Goenka are introduced, and each is practiced for a week. The purpose of these methods is to progressively increase interoceptive awareness and equanimity toward the feeling tone of body sensations. Body scanning in MiCBT is done sitting up straight and systematically surveying the body, initially vertically (from head to toe and toe to head) and then transversally (scanning from surface to internal sensations). Participants are instructed to remain alert and equanimous while experiencing body sensations as they arise, without imagining anything, visualizing body parts, seeking relaxation, or otherwise affecting the actual experience. Apart from during the first week, the experience of relaxation may occur as a by-product of equanimity. It is expected that meditators will have a range of pleasant, neutral, and unpleasant experiences as they continue with their practice (Grabovac, 2015). From session 4, exposure techniques are introduced. The first involves applying equanimity during stressful situations in daily life using the Mindfulness-based Interoceptive Exposure Task (MIET). Patients are taught to monitor arising body sensations for short periods at a time while remaining equanimous to neutralize their reactivity. The Mindfulness-based Interoceptive Signature Scale (Cayoun, 2011) is used to record their interoceptive experiences pre- and post-exposure, describing sensations in terms of their physical characteristics of mass, temperature, movement and density. Thus, the MIET cultivates both equanimity and the ability to directly experience the transient and impersonal nature of sensations, resulting in an experience-derived reappraisal of distress.
In sessions five and six, behavior change is accomplished using equanimity-based imaginal and in-vivo exposure techniques. In sessions seven and eight, these techniques are applied to assist in developing interpersonal insights and ‘mindful assertiveness’. In sessions nine and ten, compassion for oneself and others is introduced through loving kindness meditation. Compassion is defined as “the will to extend oneself for the purpose of minimizing one’s own or another’s suffering.” (Cayoun, 2017, p. 177). The practice involves pairing the pleasant flow of subtle body sensations, frequently present during body scanning at this stage of training, with compassionate thoughts towards self and others. These include positive affirmations such as “may I be peaceful,” “may I be kind to myself” and “may I share my compassion with all beings.” The pairing of pleasant body sensations with positive affirmations is in contrast with the sense of hopelessness associated with negative affirmations such as “I am useless” and “no one cares about me” which co-emerge with unpleasant sensations that can maintain depression.
Compassion training provides an ideal context for introducing ethical behavior in daily life to prevent harm to oneself and others. MiCBT explicitly teaches harm minimization within the framework of compassion training on the basis that it is not possible to be compassionate while willingly causing harm (Cayoun, 2017). This is consistent with the traditional Theravada view of ethics and compassion in which “the inclination toward kindness and compassion for others also contributes to increasingly wholesome ethical standards, since if compassion is a primary emotion in the relationship, lying, stealing, harming, or taking sexual advantage of another would be anathema” (Amaro, 2015, p. 72). Patients are invited to adopt five basic ethical challenges for a week as a behavioral experiment, and to notice any effects on their sense of well-being at an interoceptive level. In other words, they are asked to observe how it feels (internal sensations) if they behave unethically and compare this to how it feels when they deliberately inhibit the behavior. In line with the view of Kabat-Zinn (2006), ethics are understood as necessary for the development of accurate and effective mindfulness practice.
MBCT program structure and practices
As noted earlier, except for the 3-min breathing space, the mindfulness practices used in MBCT are derived from MBSR, with the rationale in MBCT linking to the cognitive model as described above (see also Supplementary Table S1). The first half of the MBCT program has its focus on mindfulness practices contextualized in terms of working “skillfully with the thoughts, emotions, and bodily sensations and emotions that create vulnerability to depressive relapse” (Dimidjian et al., 2010, p. 319). The second half of the program focuses on preventing depressive relapse, building on acceptance towards unpleasant sensations, the early detection of negative thinking, and decentering from ruminative thought patterns to reduce habitual reactivity. Skillful action for taking care of oneself is developed as an alternative response to habitual reactions to negative thoughts and low mood and the work culminates in a relapse prevention action plan. Each class is thematically organized and taught via the practices and subsequent group inquiry processes whereby learnings at each session are reflected upon and consolidated.
The first mindfulness exercise in session 1 is mindful eating (the raisin exercise), which is followed by a body scan (Segal et al., 2013), taught lying down or seated. Attention is first directed to the abdomen, then to the toes and moved up through the whole body while imagining directing the breath into and out from the different body parts, with instructions such as, “When you are ready, on an inbreath, feel or imagine the breath entering the lungs, and then passing down into the abdomen, into the left leg, the left foot, and out to the toes of the left foot. Then on the outbreath, feel or imagine the breath coming all the way back up, out of the foot, into the leg, up through the abdomen, chest, and out through the nose.” (Segal et al., 2013, pp. 122–123). Instructions include becoming aware of intense sensations and to “‘breathe in’ to them…. and… have a sense of their letting go, or releasing, on the outbreath” (Segal et al., 2013, p. 123). In session 2, a mindfulness of the breath exercise is introduced in which attention is brought to breathing at the abdominal area. A pleasant events calendar is also presented in session 2 to bring awareness to how pleasant feeling tone is experienced. In session 3, the sitting meditation incorporates mindfulness of the breath with awareness of sensations throughout the body. Mindful stretching is also introduced in session 3 as well as an unpleasant events calendar and a 3-min breathing space. The 3-min breathing space is offered as way to pause during stressful experiences during the day and turn towards the intensity of what is being experienced, instead of automatically reacting. Participants are invited to recognize and acknowledge their experience in the moment, then to bring focused attention to the breath, and finally to “expand attention to include a sense of the breath and body as a whole” (Segal et al., 2013, p. 196). Mindful stretching, mindful seeing and mindful hearing exercises are included in sessions 3 and 4. In session 4, the sitting meditation is mindfulness of sounds and thoughts, and mindful walking is also introduced. Additionally, in session 4 participants are introduced to the Automatic Thoughts Questionnaire as psychoeducation on further dis-identifying from some of the common cognitive distortions that occur in depression, by seeing them as symptoms of the illness, underscoring that thoughts are “just thoughts” and not facts.
In session 5, the working with difficulty meditation is taught in which awareness is brought to the area of strongest physical sensations evoked in the body when thinking of a difficulty, with an attitude of acceptance and openness to the sensations, intentionally letting go of any bracing or resistance. This practice is introduced as a way of letting go of aversion and cultivating an attitude of acceptance and friendliness. There is also a full day of mindfulness practice between Session 6 and 7, during which sitting and movement-based practices are alternated. The mountain meditation is introduced; this practice uses the image of a mountain to assist with feeling grounded regardless of the ‘weather systems’ that might come and go in the form of painful sensations or difficult thoughts.
In Session 6 and 7 the focus is on the relationship between thoughts, actions, and mood: in session 6, seeing moods as transitory and, in session 7, acting skillfully. MBCT invites a choice of mindfulness practices and after all have been learned, participants self-select which mediation practice to use for daily home practice. Throughout the program, the 3-min breathing space is used to apply skills learned during formal mindfulness practice into daily life, especially during times of stress or difficulty. The breathing space is used as the first step when starting to feel depressed. It is followed by asking oneself “How can I best take care of myself right now?,” to inform next actions, for example, an activity that provides a sense of pleasure or accomplishment.
In MBCT and MBSR, ethics and compassion are described as being included implicitly (Kabat-Zinn, 2011; Segal et al., 2013; Crane et al., 2017) through teachers embodying and role-modelling an ethical and kind stance as part of the program (Segal et al., 2013; Crane et al., 2017).
The possible conditions to which specific MBPs may be applicable are proposed in Table 1. Supplementary Table S1 provides a week-by-week overview of the program themes and practices used in MBCT and MiCBT.
Professional training
Professional training for both MBCT and MiCBT is rigorous and requires a substantial commitment of time and effort. Both require trainees to have clinical mental health qualification and strongly recommend ongoing development of their own meditation practice, including 5- and 7-day retreats.
MiCBT professional training
Prospective MiCBT therapists re required to complete two online courses for accreditation: a foundational course for self-implementation of MiCBT, followed by an applied course for delivery of MiCBT with patients. Each of these courses contains 10 teaching sessions of 2–3 h delivered over 12 weeks. Further supervision sessions and demonstration of the necessary competence is required to obtain MiCBT certification, available after at least 1 year of delivering MiCBT in a clinical practice setting at which time they may be added to the MiCBT Institute’s international registry of certified therapists.1 The above training program is offered through a centralized training institute located in Australia,2 with various international MiCBT Institute Chapters. Assessment criteria are outlined in the MiCBT Certification Process.3
MBCT professional training
The MBCT training program typically takes place over a 1 to 3-year period, with facilitators expected to achieve competency across all six domains of the Mindfulness-Based Interventions – Teaching Assessment Criteria (MBI-TAC) (Crane et al., 2013). MBCT training organizations are widespread – available in at least 11 countries.4 There is variation in training delivery and some training programs have moved online. There is increasing flexibility as to how training requirements are met. Training generally includes experiencing an MBCT group as a participant-observer, attending teacher training (online or traditionally as an in-person 5-day retreat) and delivering MBCT classes in a supervised capacity. There is no central certification process for MBCT, however MBCT therapists can apply to be assessed for listing on the ACCESS MBCT Register.5 Assessment criteria are outlined in the MBCT Training Pathway.6
Evidence base
MiCBT evidence base
Randomized controlled trials (RCTs) have provided evidence that MiCBT is efficacious in treating anxiety and depression in pregnant women (Yazdanimehr et al., 2016), in women with multiple sclerosis (Bahrani et al., 2017), and in men and women with type 2 diabetes (Sohrabi et al., 2022). Other studies report MiCBT to be efficacious in managing and reducing chronic pain (Cayoun et al., 2020) and increasing pain self-efficacy in patients with breast cancer (Mozafari-Motlagh et al., 2019), reducing anxiety, depression and fatigue while improving sleep quality and hope in patients with multiple sclerosis (Pouyanfard et al., 2020), reducing body image-related distress and improving emotion regulation in cancer survivors following mastectomy (Rasouli et al., 2023), reducing substance addiction compared to established treatment (Wickham, 2013), and reducing sports-anxiety and pessimism and increasing flow and adherence in competitive athletes (Scott-Hamilton et al., 2016). MiCBT was piloted in a heterogenous sample in a psychology clinic context and was equally effective when delivered in groups and individual therapy sessions (Roubos et al., 2011; cited in Cayoun et al., 2019). A recent RCT demonstrated that MiCBT was significantly more effective compared to a treatment-as-usual waitlist control group in decreasing clinical symptoms of anxiety, depression and stress and improving flourishing in a transdiagnostic group (Francis et al., 2022). Another recent study demonstrated that gene expression (IncRNA) improved in women with perinatal depression who received training in MiCBT (Wang et al., 2021). A randomized controlled study comparing the effectiveness of four treatments for obsessive compulsive disorder, MiCBT, standard CBT, Acceptance and Commitment Therapy (ACT) and Metacognitive Therapy (MT), found that while all treatments were similarly effective at mitigating symptoms from pre- to post-treatment, only the participants in the MiCBT and ACT groups maintained their gains at follow-up (Derakhtkar et al., 2022). While the evidence base for MiCBT is growing, a search through PubMed and PsycINFO in August 2023 using the search terms systematic review, meta-analysis, MiCBT, and Mindfulness-integrated cognitive behavior therapy did not identify any published systematic reviews or meta-analyses.
Clinical guidelines in Australia, the United Kingdom (UK), the United States (USA), and Canada do not mention MiCBT although CBT and MBCT are mentioned and Australian guidelines noted that there were similar effect sizes for CBT, MBCT, and IPT (Biesheuvel-Leliefeld et al., 2015). Guidelines for the treatment of anxiety proposed ‘mindfulness-based therapies’ as structured interventions for treatment-resistant panic, social, and generalized anxiety disorders (Andrews et al., 2018). These guidelines recommend treatments that have evidence-based treatment manuals and can be modified to an individual patient while attending to the therapeutic relationship.
MBCT evidence base
MBCT is currently the most widely researched MBP for mental health, and for depression in particular (Galante et al., 2013; Goldberg et al., 2019). In a search of PsychINFO, MEDLINE, Google Scholar in to August 2023 for systematic reviews and meta-analyses using key words MBCT, mindfulness-based cognitive therapy, systematic review, meta-analysis, recurrent, depression, and depressive relapse, we found one review (Coelho et al., 2007) and four meta-analyses (Piet and Hougaard, 2011; Kuyken et al., 2016; Goldberg et al., 2019; McCartney et al., 2020) that looked specifically at the efficacy of MBCT on the prevention of depressive relapse. These found advantages for its use particularly over treatment as usual, with the meta-analyses reporting moderate effect sizes. An additional systematic review looked at the management of depression with MBCT more broadly (Musa et al., 2020) and found that MBCT improved mindfulness and reduced relapse rates as well as depressive symptoms. In addition to reductions in depressive symptoms, meta-analyses from Zhang et al. (2022) and Tseng et al. (2023) also found reductions in suicidal ideation in depressed patients with large and small effect sizes, respectively. Although initial studies of MBCT suggested there may be an increased risk of relapse following MBCT for people who had experienced fewer than three episodes of depression (Teasdale et al., 2000; Helen Ma and Teasdale, 2004), a subgroup meta-analysis by McCartney et al. (2020), reported comparable results between those who had experienced more than three episodes and those who had experienced fewer than three episodes. Similarly, while the same earlier papers recommended the use of MBCT only in patients in remission from depressive episodes (Teasdale et al., 2000; Helen Ma and Teasdale, 2004), there is now an evidence base for the use of MBCT in treating current depression (Lenz et al., 2016; Goldberg et al., 2019; Liu et al., 2019; Thimm and Johnsen, 2020).
The use of MBCT with other conditions has also been studied including anxiety (Evans et al., 2008; Kim et al., 2009; Ghahari et al., 2020), bipolar disorder (Lovas and Schuman-Olivier, 2018; Xuan et al., 2020), vascular disease (Abbott et al., 2014), breast cancer (Chang et al., 2023), and chronic health conditions (Hazlett-Stevens et al., 2019; Pei et al., 2021). Meta-analyses examining the use of MBCT in populations living with bipolar disorder (Xuan et al., 2020) and chronic pain (Pei et al., 2021) found reductions in depression in between-group comparisons with moderate effect sizes. In contrast to Chang et al. (2023) meta-analysis however, Pei et al. (2021) paper did not find any statistically significant improvements in measures of pain. Though two meta-analyses reported reduction in anxiety symptoms with MBCT (Ghahari et al., 2020; Xuan et al., 2020), results varied for between-group analyses: Xuan et al. (2020) meta-analysis found no significant effects, as opposed to Ghahari et al. (2020) meta-analysis, which noted significant decreases with moderate effect sizes. A study on the implementation of MBCT in the U.K. health system suggests that MBCT has been offered to patients with a variety of other conditions including anxiety and chronic pain/fatigue for some time (Crane and Kuyken, 2013). However, guidelines for adapting MBCT (amongst other MBPs) for other conditions have been published only recently (Loucks et al., 2022).
In Australia, MBCT was endorsed by the Royal Australian and New Zealand College of Psychiatrists (RANZCP) as a preventive treatment during the maintenance phase of recurrent depression episodes (Malhi et al., 2021). In the United Kingdom, the National Collaborating Centre for Mental Health for the National Institute for Health and Care Excellence found that MBCT was recommended for individuals with a history of three or more depression episodes, who are currently stable but remain susceptible to relapse despite antidepressant medication, or who choose to discontinue antidepressant use (Royal College of Psychiatrists, 2023). In the United States, in addition to being recommended for depressive relapse prevention, MBCT was also recommended as an initial standalone depression treatment for adults, in contrast to cognitive-behavioral therapy which was recommended for use in conjunction with antidepressant medication for initial treatment (American Psychological Association, 2019). Similarly, Canada endorsed MBCT, positioning it as a second-line adjunctive treatment supported by Level 2 Evidence for acute depression, and as a first-line maintenance therapy backed by Level 1 Evidence (Parikh et al., 2016). While lacking a formal recommendation for anxiety treatment in Canada, MBCT was acknowledged as a promising approach for addressing anxiety and related disorders (Katzman et al., 2014).
Summary and clinical considerations
MiCBT and MBCT share a broadly similar approach to mental health by incorporating mindfulness with cognitive and behavioral therapies. They are each based on clear and coherent theoretical models that are conveyed throughout the programs and justify the use of practices and actions relating to the target populations. Nevertheless, the purpose, models and practices have significant differences. While MiCBT is designed to be a transdiagnostic program for acute and chronic mental health disorders, and can address comorbid symptoms, MBCT is designed for patients in remission from multiple depressive episodes, a well population with vulnerability to relapse. While MiCBT applies highly specific mindfulness practices to address the processes that precipitate and perpetuate a broad range of psychological conditions, MBCT focuses on the flexible application of a broad array of practices to one specific psychological condition, especially depression.
Co-emergence theory underpins MiCBT with initial focus on metacognitive awareness using mindfulness of the breath then a strong emphasis on interoceptive awareness and equanimity towards body sensations, using progressively refined body scanning methods to address emotional reactivity. Reactivity to unpleasant sensations that co-emerge with dysfunctional thinking patterns is an important phenomenon because it is a ‘common factor’ contributing to psychological processing across a range of mental health disorders (e.g., in depressive or anxiolytic thinking). MiCBT integrates interoceptive awareness and equanimity with Learning Theory. Applied practices target avoidance, including in interpersonal situations. MiCBT also cultivates the benefits of ethics and compassion and their relapse-prevention effects.
Cognitive theory underpins MBCT with emphasis on decentering from depression-related thoughts and feelings and averting escalating negative thinking to prevent depressive relapse. From session 6, participants choose their own selection of practices and are encouraged to embed mindfulness into their daily life. MBCT proposes that it is the regularity of practice that is critical, not which specific practice that is used as all the practices have the same end – to cultivate the “being” mode and develop the capacity to decentre from rumination to enable a wiser response too low mood.
Thus, MiCBT and MBCT are distinct treatment modalities and so require their own specific professional training. Clinically, the selection between MiCBT and MBCT may be influenced not only by diagnosis, but also by the severity of psychological symptoms and the capacity of patients to engage with the exposure and compassion methods used in MiCBT. Some clients with a significant trauma background may experience distress from extensive body scanning and skillful guidance from therapists is required. It is also possible that compassion exercises will trigger threat or grief for some people, such as those with underlying depression and adverse backgrounds (Gilbert et al., 2011; Steindl et al., 2022). Indeed, one of the reasons the developers of MBCT avoided including explicit compassion exercises such as loving kindness practices was due to the risk of triggering underlying vulnerabilities in people who struggle with depression (Segal et al., 2013, see pp. 138–139). However, in MiCBT, working with underlying vulnerabilities is central to the program, including addressing avoidance patterns associated with past trauma. Therapists are well trained to assess patients for the possibility of such experiences, prepare them for treatment and provide support as required, for example recommending individual rather than group sessions in some circumstances and pacing practice progression more slowly according to response (for details, see Cayoun et al., 2019).
In MBCT, the mindfulness exercises are introduced in a gentle and inviting manner, always deferring to a patient’s perceived capacity to do each exercise. The variety of ways that mindfulness is introduced allows for choice of exercises and with the aim of supporting long-term practice (Segal et al., 2013). This invitational stance may make it more acceptable to those who initially struggle to engage in treatments that involve more challenging exercises. Thus, it is possible that MBCT may provide a solid foundation of mindfulness before the potentially more challenging content of MiCBT. While the delivery of MiCBT is also gentle and accepting, the program is more prescriptive in terms of type and ordering of exercises. Symptoms such as avoidant or compulsive behaviors may be better addressed with the desensitization methods of MiCBT, which applies interoceptive awareness and exposure methods to address conditions such as panic disorder, obsessive compulsive disorder and post-traumatic stress disorder. As different emotional disorders may present with differing levels of sensitivity to interoceptive cues (e.g., panic disorder) the addition of equanimity to treatment can enable the management of avoidant behavior. The addition of ethics and compassion (with the loving kindness meditation) can assist with relapse prevention, preventing harm to oneself or to others. For either therapy, good client preparation before undertaking the program is essential so that potential risks and benefits are clearly understood.
Potential iatrogenic effects of MBPs have attracted increased attention since the major studies of MBCT were published. In developing non-judgmental awareness, both interventions invite participants to pay attention to unpleasant internal experiences occurring during mindfulness practice and there is a complex relationship between this process and adverse effects (Farias et al., 2020; Aizik-Reebs et al., 2021; Binda et al., 2022). A recent RCT comparing MiCBT with a wait-list control that included an examination of adverse effects did not elicit reports of any serious adverse effects (Francis et al., 2022). Mediation analysis suggested that equanimity was the most influential mediator of distress reduction and may be a protective factor against potential adverse effects. However, the current literature would not yet support a systemic comparison between the two interventions on negative effects (Farias et al., 2020). This is an area that could benefit from more precise attention in the future though the applications of measures such as the Meditation Experiences Interview (MedEx-I) (Britton et al., 2021).
The main limitation for MBCT is its single condition model - primarily major depression but also when adapted to other conditions. While single disorder MBPs will continue to uniquely meet the needs of specific populations, there is a recognized need for transdiagnostic treatment methods to extend the range of treatment possibilities and take account of comorbidities (Crane and Kuyken, 2013). For instance, using a transdiagnostic treatment protocol instead of multiple single disorder protocols can be a more resource-efficient way of treating many commonly occurring mental health conditions. In clinical settings where MBPs are delivered in groups, group recruitment can be achieved more readily, allowing more individuals to be served and wait times for treatment reduced. In addition, there are cost and time savings in terms of training clinicians in only one transdiagnostic treatment protocol, rather than in multiple single disorder protocols. Moreover, a transdiagnostic approach has the important clinical advantage of addressing comorbidity effectively.
The main limitations for MiCBT are its evidence base, which may be regarded as promising rather than established, and that it has not yet been considered in clinical guidelines. While greater attention to later stage dissemination and implementation research is recommended for single disorder protocols such as MBCT (Dimidjian et al., 2010; Goldberg et al., 2019), more quality RCTs and systematic reviews are needed to develop the evidence base for transdiagnostic MBPs such as MiCBT. Nevertheless, given the potential role for transdiagnostic MBPs, we propose that MiCBT makes a unique contribution to CBT and mindfulness-based therapies. The addition of the transdiagnostic applicability of co-emergence theory, which places importance on equanimity toward interoceptive cues in addition to metacognitive awareness, provides a strong rationale for the suite of practices and techniques in MiCBT.
Author contributions
SF: Writing – original draft, Writing – review & editing. FS: Supervision, Writing – original draft, Writing – review & editing. BC: Writing – original draft, Writing – review & editing. AG: Writing – original draft, Writing – review & editing. GM: Supervision, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
SF, BC, and AG have been paid for developing and delivering educational presentations, workshops and professional training programs for the MiCBT Institute in Australia and North America. AG has been paid for delivering MBCT educational presentations, workshops and professional training programs internationally, and provides MBCT mentorship through the UCSD Mindfulness-based Professional Training Institute and the Center for Mindfulness Studies.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1342592/full#supplementary-material
Footnotes
1. ^https://www.mindfulness.net.au/for-community/find-a-therapist/
2. ^https://www.mindfulness.net.au
3. ^https://www.mindfulness.net.au/training/micbt-professional-development-certification/
4. ^https://www.accessmbct.com/mbct-training-organisations/
5. ^https://www.accessmbct.com/
6. ^https://www.oxfordmindfulness.org/wp-content/uploads/2018/02/MBCT-Training-Pathway.pdf
References
Abbott, R. A., Whear, R., Rodgers, L. R., Bethel, A., Thompson Coon, J., Kuyken, W., et al. (2014). Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: a systematic review and meta-analysis of randomised controlled trials. J. Psychosom. Res. 76, 341–351. doi: 10.1016/j.jpsychores.2014.02.012
Aizik-Reebs, A., Shoham, A., and Bernstein, A. (2021). First, do no harm: an intensive experience sampling study of adverse effects to mindfulness training. Behav. Res. Ther. 145:103941. doi: 10.1016/j.brat.2021.103941
American Psychological Association. (2019). Clinical practice guideline for the treatment of depression across three age cohorts. Available at: https://www.apa.org/depression-guideline/guideline.pdf (Accessed August 9, 2023)
Andrews, G., Bell, C., Boyce, P., Gale, C., Lampe, L., Marwat, O., et al. (2018). Royal Australian and new Zealand College of Psychiatrists clinical practice guidelines for the treatment of panic disorder, social anxiety disorder and generalised anxiety disorder. Aust. N. Z. J. Psychiatry 52, 1109–1172. doi: 10.1177/0004867418799453
Bahrani, S., Zargar, F., Yousefipour, G., and Akbari, H. (2017). The effectiveness of mindfulness-integrated cognitive behavior therapy on depression, anxiety, and stress in females with multiple sclerosis: a single-blind randomized controlled trial. Iran. Red. Crescent. Med. J. 19:e44566. doi: 10.5812/ircmj.44566
Barlow, D. H., Allen, L. B., and Choate, M. L. (2004). Toward a unified treatment for emotional disorders. Behav. Ther. 35, 205–230. doi: 10.1016/S0005-7894(04)80036-4
Barnard, P. J., and Teasdale, J. D. (1991). Interacting cognitive subsystems: a systemic approach to cognitive-affective interaction and change. Cogn. Emot. 5, 1–39. doi: 10.1080/02699939108411021
Barrett, L. F. (2006). Valence is a basic building block of emotional life. J. Res. Pers. 40, 35–55. doi: 10.1016/j.jrp.2005.08.006
Batchelor, M. (2018). Vedanā or feeling tone: a practical and contemporary meditative exploration. Contemporary Buddhism 19, 54–68. doi: 10.1080/14639947.2018.1442142
Biesheuvel-Leliefeld, K. E., Kok, G. D., Bockting, C. L., Cuijpers, P., Hollon, S. D., Van Marwijk, H. W., et al. (2015). Effectiveness of psychological interventions in preventing recurrence of depressive disorder: meta-analysis and meta-regression. J. Affect. Disord. 174, 400–410. doi: 10.1016/j.jad.2014.12.016
Binda, D. D., Greco, C. M., and Morone, N. E. (2022). What are adverse events in mindfulness meditation? Glob. Adv. Health Med. 11, 1–3. doi: 10.1177/2164957X221096640
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., et al. (2004). Mindfulness: a proposed operational definition. Clin. Psychol. Sci. Pract. 11, 230–241. doi: 10.1093/clipsy.bph077
Bodhi, B. (2003). The connected discourses of the Buddha: a translation of the Samyutta Nikaya. Boston: Wisdom Publications.
Britton, W. B., Lindahl, J. R., Cooper, D. J., Canby, N. K., and Palitsky, R. (2021). Defining and measuring meditation-related adverse effects in mindfulness-based programs. Clin. Psychol. Sci. 9, 1185–1204. doi: 10.1177/2167702621996340
Cayoun, B.A. (2015). Mindfulness-integrated CBT for well-being and personal growth. Oxford: Wiley Blackwell
Cayoun, B. A. (2017). “The purpose, mechanisms, and benefits of cultivating ethics in mindfulness-integrated cognitive behavior therapy” in Practitioner's guide to ethics and mindfulness-based interventions. ed. C. M. Monteiro (New York: Springer), 163–192.
Cayoun, B.A., Francis, S.E., and Shires, A.G. (2019). The clinical handbook of mindfulness-integrated cognitive behavior therapy: a step-by-step guide for therapists. Hoboken: Wiley-Blackwell.
Cayoun, B., Sauvage, V., and Van Impe, M. (2004). A non-diganosis-specific application of mindfulness-based cognitive behavioural therapy (MCBT): A pilot study. Tasmania, Australia: The Hobart Clinic.
Cayoun, B. A., and Shires, A. G. (2020). Co-emergence reinforcement and its relevance to interoceptive desensitization in mindfulness and therapies aiming at transdiagnostic efficacy. Front. Psychol. 11:545945. doi: 10.3389/fpsyg.2020.545945
Cayoun, B. A., Simmons, A., and Shires, A. (2020). Immediate and lasting chronic pain reduction following a brief self-implemented mindfulness-based interoceptive exposure task: a pilot study. Mindfulness 11, 112–124. doi: 10.1007/s12671-017-0823-x
Chang, Y.-C., Tseng, T. A., Lin, G.-M., Hu, W.-Y., Wang, C.-K., and Chang, Y.-M. (2023). Immediate impact of mindfulness-based cognitive therapy (MBCT) among women with breast cancer: a systematic review and meta-analysis. BMC Womens Health 23:331. doi: 10.1186/s12905-023-02486-x
Chiesa, A., and Malinowski, P. (2011). Mindfulness-based approaches: are they all the same? J. Clin. Psychol. 67, 404–424. doi: 10.1002/jclp.20776
Coelho, H. F., Canter, P. H., and Ernst, E. (2007). Mindfulness-based cognitive therapy: evaluating current evidence and informing future research. J. Consult. Clin. Psychol. 75, 1000–1005. doi: 10.1037/0022-006X.75.6.1000
Crane, R., Brewer, J., Feldman, C., Kabat-Zinn, J., Santorelli, S., Williams, J., et al. (2017). What defines mindfulness-based programs? The warp and the weft. Psychol. Med. 47, 990–999. doi: 10.1017/S0033291716003317
Crane, R. S., Eames, C., Kuyken, W., Hastings, R. P., Williams, J. M. G., Bartley, T., et al. (2013). Development and validation of the mindfulness-based interventions – teaching assessment criteria (MBI:TAC). Assessment 20, 681–688. doi: 10.1177/1073191113490790
Crane, R. S., and Kuyken, W. (2013). The implementation of mindfulness-based cognitive therapy: learning from the UK health service experience. Mindfulness 4, 246–254. doi: 10.1007/s12671-012-0121-6
Creswell, D. J. (2017). Mindfulness interventions. Annu. Rev. Psychol. 68, 491–516. doi: 10.1146/annurev-psych-042716-051139
Derakhtkar, A., Khezrimoghadam, N., and Fazilatpour, M. (2022). The effectiveness of mindfulness-integrated cognitive behavioral therapy (MiCBT), meta-cognitive therapy (MCT), acceptance and commitment therapy (ACT), and cognitive behavioral therapy (CBT) on obsessive-compulsive disorder (OCD). Int. J. Health Sci. 8, 46–52. doi: 10.22100/ijhs.v8i2.876
Desbordes, G., Gard, T., Hoge, E. A., Hölzel, B. K., Kerr, C., Lazar, S. W., et al. (2015). Moving beyond mindfulness: defining equanimity as an outcome measure in meditation and contemplative research. Mindfulness 6, 356–372. doi: 10.1007/s12671-013-0269-8
Dimidjian, S., Kleiber, B. V., and Segal, Z. V. (2010). “Mindfulness-based cognitive therapy” in Cognitive and behavioral theories in clinical practice. eds. N. Kazantzis, M. A. Reinecke, and A. Freeman (New York: Guilford Press), 307–331.
Evans, S., Ferrando, S., Findler, M., Stowell, C., Smart, C., and Haglin, D. (2008). Mindfulness-based cognitive therapy for generalized anxiety disorder. J. Anxiety Disord. 22, 716–721. doi: 10.1016/j.janxdis.2007.07.005
Farias, M., Maraldi, E., Wallenkampf, K. C., and Lucchetti, G. (2020). Adverse events in meditation practices and meditation-based therapies: a systematic review. Acta Psychiatr. Scand. 142, 374–393. doi: 10.1111/acps.13225
Francis, S. E. B., Shawyer, F., Cayoun, B., Enticott, J., and Meadows, G. N. (2022). Group mindfulness-integrated cognitive behavior therapy (MiCBT) reduces depression and anxiety and improves flourishing in a transdiagnostic primary care sample compared to treatment-as-usual: a randomized controlled trial. Front. Psych. 13:815170. doi: 10.3389/fpsyt.2022.815170
Füstös, J., Gramann, K., Herbert, B. M., and Pollatos, O. (2013). On the embodiment of emotion regulation: interoceptive awareness facilitates reappraisal. Soc. Cogn. Affect. Neurosci. 8, 911–917. doi: 10.1093/scan/nss089
Galante, J., Iribarren, S. J., and Pearce, P. F. (2013). Effects of mindfulness-based cognitive therapy on mental disorders: a systematic review and meta-analysis of randomised controlled trials. J. Res. Nurs. 18, 133–155. doi: 10.1177/1744987112466087
Garfinkel, S. N., and Critchley, H. D. (2013). Interoception, emotion and brain: new insights link internal physiology to social behaviour. Commentary on: "anterior insular cortex mediates bodily sensibility and social anxiety" by Terasawa et al. (2012). Soc. Cogn. Affect Neurosci. 8, 231–234. doi: 10.1093/scan/nss140
Ghahari, S., Mohammadi-Hasel, K., Malakouti, S. K., and Roshanpajouh, M. (2020). Mindfulness-based cognitive therapy for generalised anxiety disorder: a systematic review and meta-analysis. East Asian Arch. Psychiatr. 30, 52–56. doi: 10.12809/eaap1885
Gibson, J. (2019). Mindfulness, interoception, and the body: a contemporary perspective. Front. Psychol. 10:2012. doi: 10.3389/fpsyg.2019.02012
Gilbert, P., McEwan, K., Matos, M., and Rivis, A. (2011). Fears of compassion: development of three self-report measures. Psychol. Psychother. 84, 239–255. doi: 10.1348/147608310x526511
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Kearney, D. J., and Simpson, T. L. (2019). Mindfulness-based cognitive therapy for the treatment of current depressive symptoms: a meta-analysis. Cogn. Behav. Ther. 48, 445–462. doi: 10.1080/16506073.2018.1556330
Grabovac, A. (2015). The stages of insight: clinical relevance for mindfulness-based interventions. Mindfulness 6, 589–600. doi: 10.1007/s12671-014-0294-2
Grossman, P. (2011). Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology's (re) invention of mindfulness: comment on Brown et al. Psychol. Assess. 23, 1034–1040. doi: 10.1037/a0022713
Hadash, Y., Segev, N., Tanay, G., Goldstein, P., and Bernstein, A. (2016). The decoupling model of equanimity: theory, measurement, and test in a mindfulness intervention. Mindfulness 7, 1214–1226. doi: 10.1007/s12671-016-0564-2
Hart, W. (1987). The art of living: Vipassana meditation as taught by SN Goenka. Onalaska (Washington, USA): Pariyatti.
Hawton, K.E., Salkovskis, P.M., Kirk, J.E., and Clark, D.M. (1989). Cognitive behaviour therapy for psychiatric problems: A practical guide. Oxford: Oxford University Press.
Hazlett-Stevens, H., Singer, J., and Chong, A. (2019). Mindfulness-based stress reduction and mindfulness-based cognitive therapy with older adults: a qualitative review of randomized controlled outcome research. Clin. Gerontol. 42, 347–358. doi: 10.1080/07317115.2018.1518282
Helen Ma, S., and Teasdale, J. D. (2004). Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. J. Consult. Clin. Psychol. 72, 31–40. doi: 10.1037/0022-006X.72.1.31
Ingram, R. E., and Hollon, S. D. (1986). “Cognitive therapy for depression from an information processing perspective” in Information processing approaches to clinical psychology. ed. R. E. Ingram (San Diego, CA: Academic Press), 259–281.
Jha, A. P., Krompinger, J., and Baime, M. J. (2007). Mindfulness training modifies subsystems of attention. Cogn. Affect. Behav. Neurosci. 7, 109–119. doi: 10.3758/CABN.7.2.109
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 4, 33–47. doi: 10.1016/0163-8343(82)90026-3
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. London: Delta.
Kabat-Zinn, J. (1994). Wherever you go there you are: Mindfulness meditation in everyday life. London: Piatkus Books.
Kabat-Zinn, J. (2006). Coming to our senses: Healing ourselves and the world through mindfulness. London: Piatkus Books.
Kabat-Zinn, J. (2011). Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Contemp. Buddhism 12, 281–306. doi: 10.1080/14639947.2011.564844
Katzman, M. A., Bleau, P., Blier, P., Chokka, P., Kjernisted, K., and Van Ameringen, M. (2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry 14, S1–S83. doi: 10.1186/1471-244X-14-S1-S1
Kazdin, A. E. (2016). Evidence-based psychosocial treatment: advances, surprises, and needed shifts in foci. Cogn. Behav. Pract. 23, 426–430. doi: 10.1016/j.cbpra.2015.11.003
Khalsa, S. S., Adolphs, R., Cameron, O. G., Critchley, H. D., Davenport, P. W., Feinstein, J. S., et al. (2018). Interoception and mental health: a roadmap. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 3, 501–513. doi: 10.1016/j.bpsc.2017.12.004
Kim, Y. W., Lee, S.-H., Choi, T. K., Suh, S. Y., Kim, B., Kim, C. M., et al. (2009). Effectiveness of mindfulness-based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depress. Anxiety 26, 601–606. doi: 10.1002/da.20552
Kuyken, W., Warren, F. C., Taylor, R. S., Whalley, B., Crane, C., Bondolfi, G., et al. (2016). Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry 73, 565–574. doi: 10.1001/jamapsychiatry.2016.0076
Lenz, A. S., Hall, J., and Bailey Smith, L. (2016). Meta-analysis of group mindfulness-based cognitive therapy for decreasing symptoms of acute depression. J. Spec. Group Work 41, 44–70. doi: 10.1080/01933922.2015.1111488
Lin, E. H., Katon, W. J., Von Korff, M., Russo, J. E., Simon, G. E., Bush, T. M., et al. (1998). Relapse of depression in primary care: rate and clinical predictors. Arch. Fam. Med. 7, 443–449. doi: 10.1001/archfami.7.5.443
Liu, J. J. W., Ein, N., and Fung, K. (2019). Mindfulness-based cognitive therapy's effect on the symptoms of currently depressed individuals: a systematic review of existing meta-analytic evidence. Can. J. Couns. Psychother. 53, 198–212.
Loucks, E. B., Crane, R. S., Sanghvi, M. A., Montero-Marin, J., Proulx, J., Brewer, J. A., et al. (2022). Mindfulness-based programs: why, when, and how to adapt? Glob. Adv. Integr. Med. Health 11, 1–12. doi: 10.1177/21649561211068805
Lovas, D. A., and Schuman-Olivier, Z. (2018). Mindfulness-based cognitive therapy for bipolar disorder: a systematic review. J. Affect. Disord. 240, 247–261. doi: 10.1016/j.jad.2018.06.017
Malhi, G. S., Bell, E., Bassett, D., Boyce, P., Bryant, R., Hazell, P., et al. (2021). The 2020 Royal Australian and new Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust. N. Z. J. Psychiatry 55, 7–117. doi: 10.1177/0004867420979353
McCartney, M., Nevitt, S., Lloyd, A., Hill, R., White, R., and Duarte, R. (2020). Mindfulness-based cognitive therapy for prevention and time to depressive relapse: systematic review and network meta-analysis. Acta Psychiatr. Scand. 143, 6–21. doi: 10.1111/acps.13242
Menon, V., and Uddin, L. Q. (2010). Saliency, switching, attention and control: a network model of insula function. Brain Struct. Funct. 214, 655–667. doi: 10.1007/s00429-010-0262-0
Mowrer, R.R., and Klein, S.B. (2000). Handbook of contemporary learning theories. London: Psychology Press
Mozafari-Motlagh, M.-R., Nejat, H., Tozandehjani, H., and Samari, A.-A. (2019). Effect of cognitive behavior therapy integrated with mindfulness on perceived pain and pain self-efficacy in patients with breast cancer. J. Nurs. Midwifery Sci. 6, 51–56. doi: 10.4103/jnms.jnms_60_18
Musa, Z. A., Kim Lam, S., Binti Mamat @ Mukhtar, F., Kwong Yan, S., Tajudeen Olalekan, O., and Kim Geok, S. (2020). Effectiveness of mindfulness-based cognitive therapy on the management of depressive disorder: systematic review. Int. J. Africa Nurs. Sci. 12:100200. doi: 10.1016/j.ijans.2020.100200
Ñāṇamoli, B., and Bodhi, B. (2005). The middle length discourses of the Buddha: A translation of the Majjhima Nikaya. Boston: Wisdom Publications.
Nolen-Hoeksema, S., and Morrow, J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta earthquake. J. Pers. Soc. Psychol. 61, 115–121. doi: 10.1037//0022-3514.61.1.115
Parikh, S. V., Quilty, L. C., Ravitz, P., Rosenbluth, M., Pavlova, B., Grigoriadis, S., et al. (2016). Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 2. Psychological treatments. Can. J. Psychiatr. 61, 524–539. doi: 10.1177/0706743716659418
Pei, J. H., Ma, T., Nan, R. L., Chen, H. X., Zhang, Y. B., Gou, L., et al. (2021). Mindfulness-based cognitive therapy for treating chronic pain: a systematic review and meta-analysis. Psychol. Health Med. 26, 333–346. doi: 10.1080/13548506.2020.1849746
Piet, J., and Hougaard, E. (2011). The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin. Psychol. Rev. 31, 1032–1040. doi: 10.1016/j.cpr.2011.05.002
Pollatos, O., and Schandry, R. (2008). Emotional processing and emotional memory are modulated by interoceptive awareness. Cogn. Emot. 22, 272–287. doi: 10.1080/02699930701357535
Pouyanfard, S., Mohammadpour, M., Parvizi Fard, A. A., and Sadeghi, K. (2020). Effectiveness of mindfulness-integrated cognitive behavior therapy on anxiety, depression and hope in multiple sclerosis patients: a randomized clinical trial. Trends Psychiatry Psychother. 42, 55–63. doi: 10.1590/2237-6089-2018-0105
Rae, C. L., Larsson, D. E., Garfinkel, S. N., and Critchley, H. D. (2019). Dimensions of interoception predict premonitory urges and tic severity in Tourette syndrome. Psychiatry Res. 271, 469–475. doi: 10.1016/j.psychres.2018.12.036
Rasouli, M., Khazaie, H., and Yarahmadi, Y. (2023). Effectiveness of mindfulness-integrated cognitive behavioural therapy (MiCBT) on body image and emotional regulation in mastectomy patients: a randomized clinical trial. Iran. J. Breast Dis. 16, 23–37. doi: 10.30699/ijbd.16.2.23
Roubos, L., Hawkins, R., and Cayoun, B.A. (2011). A comparison of group-enhanced and individual implementations of mindfulness-integrated cognitive behaviour therapy (MiCBT): An effectiveness study. Coursework master’s thesis, Cairns, QLD: James Cook University.
Royal College of Psychiatrists (2023). NICE guidelines. Available at: https://www.rcpsych.ac.uk/improving-care/nccmh/clinical-guideline-development/nice-guidelines (Accessed August 9, 2023)
Safran, J.D., and Segal, Z.V. (1990). Interpersonal process in cognitive therapy. Lanham: Jason Aronson.
Scott-Hamilton, J., Schutte, N. S., and Brown, R. F. (2016). Effects of a mindfulness intervention on sports-anxiety, pessimism, and flow in competitive cyclists. Appl. Psychol. Health Well-Being 8, 85–103. doi: 10.1111/aphw.12063
Segal, Z., Williams, J.M.G., and Teasdale, J.D. (2002). Mindfulness-based cognitive therapy for depression: a new approach to relapse prevention. New York: Guilford Press.
Segal, Z., Williams, M., and Teasdale, J. (2013). Mindfulness-based cognitive therapy for depression. New York: Guilford Press.
Semple, R. J. (2010). Does mindfulness meditation enhance attention? A randomized controlled trial. Mindfulness 1, 121–130. doi: 10.1007/s12671-010-0017-2
Sohrabi, F., Sohrabi, A., Shams-Alizadeh, N., and Cayoun, B. A. (2022). Managing type 2 diabetes and depression with mindfulness-integrated cognitive behavior therapy (MiCBT). Discov. Psychol. 2:10. doi: 10.1007/s44202-022-00026-6
Steindl, S., Bell, T., Dixon, A., and Kirby, J. N. (2022). Therapist perspectives on working with fears, blocks and resistances to compassion in compassion focused therapy. Couns. Psychother. Res. 23, 850–863. doi: 10.1002/capr.12530
Teasdale, J. D., Moore, R. G., Hayhurst, H., Pope, M., Williams, S., and Segal, Z. V. (2002). Metacognitive awareness and prevention of relapse in depression: empirical evidence. J. Consult. Clin. Psychol. 70, 275–287. doi: 10.1037/0022-006X.70.2.275
Teasdale, J. D., Segal, Z., and Williams, J. M. (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behav. Res. Ther. 33, 25–39. doi: 10.1016/0005-7967(94)e0011-7
Teasdale, J., Williams, M., and Segal, Z (2014). The mindful way workbook: An 8-week program to free yourself from depression and emotional distress. New York: Guildford Press.
Teasdale, J. D., Williams, J. M. G., Soulsby, J. M., Segal, Z. V., Ridgeway, V. A., and Lau, M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J. Consult. Clin. Psychol. 68, 615–623. doi: 10.1037//0022-006X.68.4.615
Thimm, J. C., and Johnsen, T. J. (2020). Time trends in the effects of mindfulness-based cognitive therapy for depression: a meta-analysis. Scand. J. Psychol. 61, 582–591. doi: 10.1111/sjop.12642
Tseng, H.-W., Chou, F.-H., Chen, C.-H., and Chang, Y.-P. (2023). Effects of mindfulness-based cognitive therapy on major depressive disorder with multiple episodes: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 20:1555. doi: 10.3390/ijerph20021555
Uddin, L. Q. (2015). Salience processing and insular cortical function and dysfunction. Nat. Rev. Neurosci. 16, 55–61. doi: 10.1038/nrn3857
Van Weel-Baumgarten, E. M., Schers, H., Van den Bosch, W., Van den Hoogen, H., and Zitman, F. (2000). Long-term follow-up of depression among patients in the community and in family practice settings: a systematic review. J. Fam. Pract. 49, 1113–1120.
Wang, L., Zhang, M., Zhu, H., Sun, L., Yu, B., and Cui, X. (2021). Combined identification of lnc RNA NONHSAG004550 and NONHSAT125420 as a potential diagnostic biomarker of perinatal depression. J. Clin. Lab. Anal. 35:e23890. doi: 10.1002/jcla.23890
Wickham, K. (2013). The effect of mindfulness-integrated cognitive behaviour therapy (MiCBT) on the experience of addiction. Coursework master’s thesis. Hobart, TAS: University of Tasmania.
Xuan, R., Li, X., Qiao, Y., Guo, Q., Liu, X., Deng, W., et al. (2020). Mindfulness-based cognitive therapy for bipolar disorder: a systematic review and meta-analysis. Psychiatry Res. 290:10. doi: 10.1016/j.psychres.2020.113116
Yazdanimehr, R., Omidi, A., Sadat, Z., and Akbari, H. (2016). The effect of mindfulness-integrated cognitive behavior therapy on depression and anxiety among pregnant women: a randomized clinical trial. J. Caring Sci. 5, 195–204. doi: 10.15171/jcs.2016.021
Zamariola, G., Frost, N., Van Oost, A., Corneille, O., and Luminet, O. (2019). Relationship between interoception and emotion regulation: new evidence from mixed methods. J. Affect. Disord. 246, 480–485. doi: 10.1016/j.jad.2018.12.101
Keywords: mindfulness-integrated cognitive behavior therapy, mindfulness-based cognitive therapy, mindfulness-based programs, mindfulness, depression, transdiagnostic
Citation: Francis SEB, Shawyer F, Cayoun BA, Grabovac A and Meadows G (2024) Differentiating mindfulness-integrated cognitive behavior therapy and mindfulness-based cognitive therapy clinically: the why, how, and what of evidence-based practice. Front. Psychol. 15:1342592. doi: 10.3389/fpsyg.2024.1342592
Edited by:
Valeria Cioffi, Phenomena Research Group (Italy), ItalyReviewed by:
Lucia Luciana Mosca, Scuola di Specializzazione in Psicoterapia Gestaltica Integrata (SIPGI), ItalyAlexandru I. Tiba, University of Oradea, Romania
Francesco Marino, Scuola di Specializzazione in Psicoterapia Gestaltica Integrata (SIPGI), Italy
Copyright © 2024 Francis, Shawyer, Cayoun, Grabovac and Meadows. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Frances Shawyer, ZnJhbmNlcy5zaGF3eWVyQG1vbmFzaC5lZHU=
 Sarah E. B. Francis
Sarah E. B. Francis Frances Shawyer
Frances Shawyer Bruno A. Cayoun
Bruno A. Cayoun Andrea Grabovac
Andrea Grabovac Graham Meadows
Graham Meadows