- 1Psychology, Central Luzon State University, Munoz, Philippines
- 2Department of Psychology, De La Salle University, Manila, Philippines
Social support has been associated with improved mental health; however, the mechanisms underlying this relationship remain unclear. This study aimed to explore whether perceived stress mediate the relationship between social support and positive affect, anxiety, and depression. Drawing from Lazarus and Folkman’s stress and coping theory, the study emphasized the influential role of social support in appraising stressful events. A cross-sectional survey was conducted online among 426 Filipino adults during the peak of the COVID-19 pandemic. Participants completed measures including the Multidimensional Scale of Perceived Social Support (MSPSS), the Perceived Stress Scale-10 (PSS-10), the Positive Affect subscale of PANAS, and the Depression and Anxiety subscales of DASS-21. The hypotheses of the study were tested using mediation analysis. Consistent with the hypotheses, perceived stress significantly mediated the relationship between family and significant other support with positive affect, anxiety, and depression. Family and significant other support decreased perceived stress, increasing positive affect, and decreasing anxiety and depression. On the other hand, perceived stress did not mediate the relationship between friend support and positive affect, anxiety, and depression. Implications and future research directions are discussed.
Introduction
Social support encompasses feeling loved, valued, and part of a network that offers mutual assistance (Cobb, 1976; Sarason et al., 1987; Wills, 1991). Many studies highlight its protective role in mental health. Yet, the precise ways it impacts mental well-being remain unclear. This gap offers an opportunity for exploration, especially amid the COVID-19 pandemic.
Numerous studies during the pandemic noted increased stress, physical issues, fatigue, loneliness, depression, and anxiety (Brailovskaia et al., 2021; Mansueto et al., 2021; Alhakami et al., 2023). In the Philippines, Tee et al. (2020) and Montano and Acebes (2020) reported widespread mental health concerns during strict quarantines. This crisis reignites interest in understanding how social support boosts mental well-being, given its consistent association with better mental health.
This study delves into how social support benefits mental health amid the COVID-19 pandemic, aiming to uncover insights for future interventions promoting long-term well-being. Anchored in Lazarus and Folkman’s stress and coping theory, the research highlights how social support shapes stress assessment and influences mental health. Understanding these underlying mechanisms is crucial, especially given the current prevalence of mental health issues, and can guide the development of interventions leveraging social support for improved mental wellbeing.
Social support
Social support, a multidimensional concept, is typically measured in terms of either the structure (number of relationships) or the functions (like informational, instrumental, and emotional) of social networks (Wills, 1991). Perceived support, the perception of available help, often has a more significant impact on mental health than received support (Kessler and McLeod, 1985; Thoits, 1985; Wethington and Kessler, 1986). Research also shows that social support can stem from various sources like family, friends, or pets (Allen et al., 2002; Ford et al., 2007), and can benefit mental and physical health in both stressful and non-stressful times (Cohen and Wills, 1985).
Social support and mental health
Numerous studies highlight social support’s protective role in mental health. For depression, research underscores the significance of parental support for children, while adults benefit from spouses, family, and friends (Gariepy et al., 2016; Mohd et al., 2019). Low support relates to higher depression, anxiety, and self-harm during pregnancy (Bedaso et al., 2021). Those with weaker support face difficulties in depression recovery and social functioning (Wang et al., 2018). Anxiety among informal carers shows a negative link with perceived support (Priego-Cubero et al., 2023). Social support positively influences well-being in international students and children (Chu et al., 2010; Bender et al., 2019). University students’ well-being and LGB youth’s adjustment tie to perceived support (Watson et al., 2019; Cobo-Rendón et al., 2020). Family support strongly predicts well-being among senior students (Gülaçtı, 2010). Amid COVID-19, higher social support links to lower depression, anxiety, and stress (Grey et al., 2020; Qi et al., 2020; Xiao et al., 2020; Ghafari et al., 2021; Liu et al., 2021).
The Stress and coping theory (Lazarus and Folkman, 1984) provides a framework to understand the pivotal role of social support in mental health. The theory suggests that social support significantly shapes how we perceive and handle stress. It acts as a crucial resource when facing challenges, impacting our stress levels. When we feel supported and equipped to cope, stress tends to diminish. Thus, an event’s perceived stress is not solely inherent; our evaluation, influenced by our perceived social support, greatly shapes how we perceive it. A robust support system can alleviate the overwhelming nature of specific events. Therefore, increasing social support is more likely to decrease perceived stress.
Perceived stress and mental health
Perceived stress, shaped by how individuals appraise situations and their coping abilities (Lazarus and Folkman, 1984), strongly correlates with mental health outcomes such as anxiety, depression, and harmful behaviors (Liu and Alloy, 2010; Skipworth, 2011; Neese et al., 2013; Zhang et al., 2014; Konstantopoulou et al., 2020; Pieh et al., 2020; Salari et al., 2020; Huang and Zhao, 2021; Puertas-Gonzalez et al., 2023). Epidemiological studies confirm that facing more stressful events and consistently reporting high perceived stress over extended periods are linked to poorer mental health and increased mortality (Epel et al., 2018). The COVID-19 has been a significant stressor impacting mental health, with rising anxiety and depression rates (Courtet et al., 2020; Luo et al., 2020; Pieh et al., 2020; Salari et al., 2020; Huang and Zhao, 2021; Litwin and Levinsky, 2021; Hüfner et al., 2022; Mansueto et al., 2022). Anxiety, a response to stress, shows a strong link to perceived stress, activating similar brain regions (Konstantopoulou et al., 2020; Gijón Puerta et al., 2022). Perceived stress significantly contributes to depression and harmful behaviors like substance abuse (Skipworth, 2011; Neese et al., 2013; Zhang et al., 2014; Reger et al., 2020). Notably, higher positive affect, vital for wellbeing, correlates negatively with perceived stress (Kun, 2013; Eden et al., 2020; Lades et al., 2020; Rackoff and Newman, 2020; Yang and Ma, 2020; Klaiber et al., 2021; Stieger et al., 2021; Zacher and Rudolph, 2021).
Social support and perceived stress
Previous studies highlight social support’s impact on perceived stress. Özer et al. (2021) linked increased family support to lower stress levels, explaining 11% of stress variance. Ekmen et al. (2021) found family and significant other support significantly reduce stress, with stress partially mediating life satisfaction. McLean et al. (2023) among college students reaffirmed this link: more support meant lower stress. Social support not only directly affects stress but also indirectly influences overall satisfaction by shaping stress perception. This underscores the pivotal role of social support in reducing perceived stress levels.
In summary, empirical evidence consistently indicates a positive link between greater social support and improved mental health outcomes. Further, previous studies have highlighted that social support contributes to mental well-being by diminishing perceived stress. Theoretically rooted in Lazarus and Folkman’s stress and coping theory, social support is recognized as a pivotal factor influencing how individuals perceive and manage stress, consequently impacting mental health. Thus, this study investigates the indirect influence of social support on mental health, specifically through its impact on perceived stress.
This study significantly contributes to advancing our understanding of the intricate interplay between social support, perceived stress, and mental health. By exploring the indirect effect of social support on mental health through perceived stress, it expands upon existing theories and models. Traditionally, the association between social support and mental health has been acknowledged, but this study delves deeper. It elucidates the mechanism by which social support operates, highlighting its role in influencing an individual’s perception and management of stress. The integration of Lazarus and Folkman’s stress and coping theory into this framework offers a theoretical underpinning, illustrating how social support acts as a crucial resource in shaping stress appraisal, subsequently impacting mental health outcomes.
By specifically investigating the pathway through perceived stress, this study bridges gaps in understanding how social support exerts its influence. It augments existing theories by elucidating a more nuanced pathway, shedding light on the nuanced dynamics between social support, stress perception, and mental health outcomes. This deeper understanding can pave the way for more targeted interventions. Understanding the indirect influence of social support on mental health through its impact on perceived stress holds significant clinical relevance. By delving into this relationship, clinicians and practitioners can gain insights into potential intervention strategies. Recognizing the pivotal role of social support in mitigating perceived stress and, consequently, improving mental health outcomes, clinicians can develop targeted approaches.
This comprehension allows for the enhancement of support systems tailored to individuals experiencing high stress levels, thereby potentially reducing the risk of mental health issues. By addressing and bolstering social support perceptions, interventions can be designed to not only alleviate perceived stress but also potentially prevent or ameliorate mental health conditions. This study’s findings may serve as a foundation for developing more effective, nuanced interventions that harness the power of social connections to promote mental wellbeing.
The current study
Social support has been associated with improved mental health; however, the mechanisms underlying this relationship remain unclear. Hence, this study aimed to investigate whether perceived stress mediate the relationship between social support and mental health outcomes.
This study is based on Lazarus and Folkman’s stress and coping theory, which emphasizes the crucial role of social support as a valuable resource that influences how individuals perceive stressful events. According to this theory, an event is considered stressful when its demands exceed the individual’s available resources, leading to heightened levels of stress. However, if individuals perceive an event as manageable and believe they have the necessary resources to handle it effectively, their experience of stress tends to decrease. A key factor that affects the appraisal process is the presence of strong social support. Having a reliable support network can significantly shape how individuals perceive stressful events. Social support can take various forms, including emotional support, practical assistance, informational guidance, and companionship. When individuals have access to these forms of support, they are more likely to view the event as less stressful. In essence, the appraisal of stressfulness depends not only on the objective nature of the event but also on the individual’s subjective evaluation of their available resources, including social support. A robust support system can contribute to perceiving certain events as less daunting, thereby positively impacting mental health outcomes, and reducing the likelihood of negative psychological consequences.
Building upon Lazarus and Folkman’s stress and coping theory and considering the existing body of research regarding the impact of social support on mental health and its correlation with perceived stress, this study posits the following hypotheses:
1. Social support is positively associated with positive affect and negatively associated with anxiety, and depression symptoms.
2. Social support is negatively associated with perceived stress.
3. Perceived stress is negatively associated with positive affect and positively associated with anxiety and depression symptoms.
4. Perceived stress mediates the association between social support with positive affect, anxiety, and depression.
Conceptual model
The mediation model is a statistical framework that enables researchers to explore the indirect impact of an independent variable on a dependent variable through a mediator. In this study, the independent variable is social support, the dependent variables comprise mental health outcomes such as positive affect, anxiety, and symptoms of depression, and the proposed mediator is perceived stress.
The proposed mediation model is grounded in Lazarus and Folkman’s stress and coping theory (1984), which emphasizes the crucial role of social support in how individuals evaluate stressful events. Overall, the mediation model posits that social support will have indirect effect on mental health outcomes through a pathway involving perceived stress. Specifically, the model suggests that social support will reduce perceived stress, leading to an increase in positive affect and a decrease in anxiety and depression. Figure 1 presents the schematic presentation of the conceptual model.
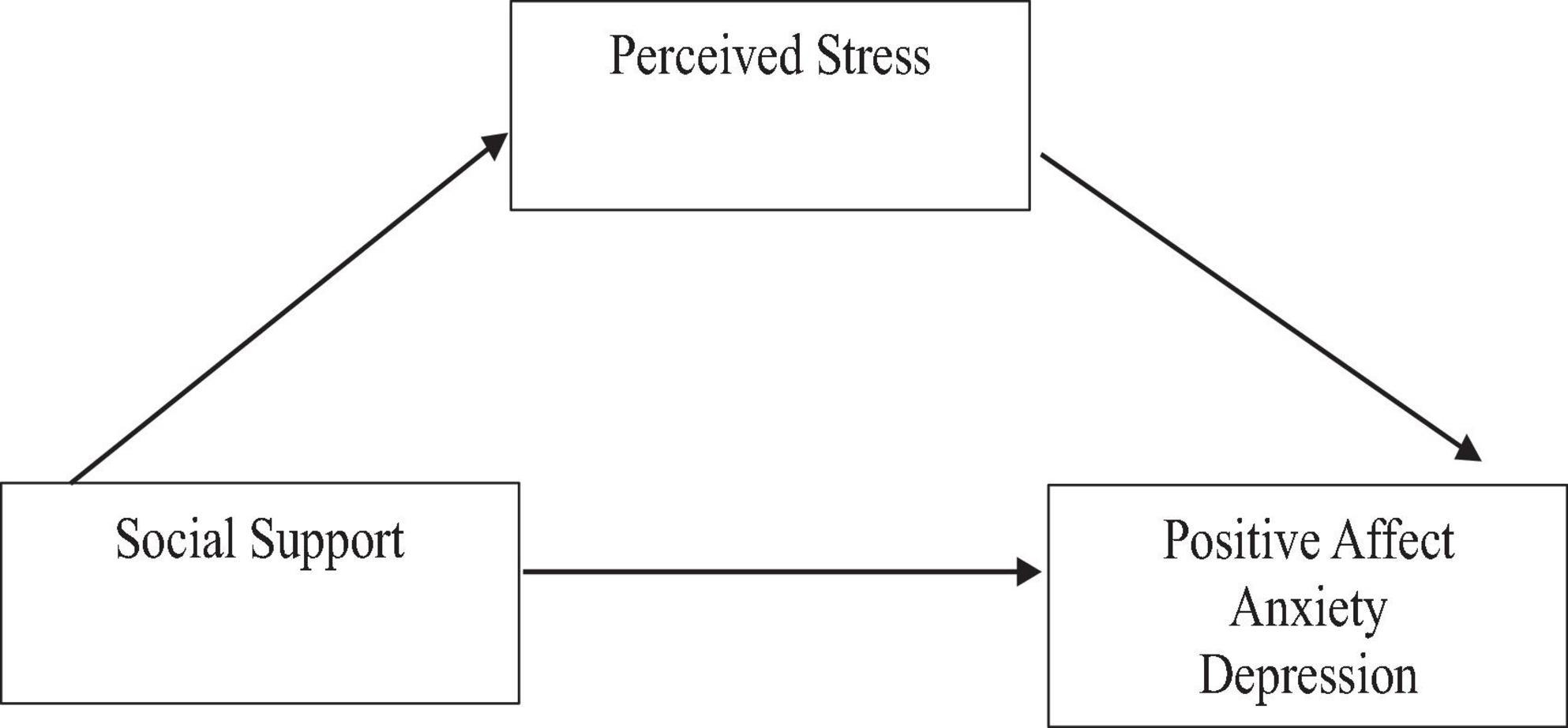
Figure 1. Hypothesized simple mediation model of the relations among social support and mental health and the mediating role of perceived stress.
Materials and methods
Research design
This study utilized a correlational design to explore how perceived stress mediates the relationship between social support and various indicators of mental health, including positive affect, anxiety, and depression. The primary objective was to investigate the potential mechanisms that explain how social support positively influences mental health outcomes.
Participants
Participants were 426 Filipino adults presently residing in the Philippines. The participants had a mean age of 28.40 years old (age range: 18 - 64 years old, SD = 10.19). Majority of them were females (74.2%), single (80.3%) and were living with their families (88.5%). Most of them were college graduate (48.4%) followed by high school graduates (26.3%) and college students (11.7%). The participants were recruited online, via referral from acquaintances, or through the participants’ referrals themselves. Informed consent was first obtained before answering the research questionnaires.
Measures
Multidimensional Scale of Perceived Social Support (MSPSS)
The MSPSS (Zimet et al., 1988) is a tool designed to assess perceived social support from friends, family, and significant others. It comprises 12 items, with 4 items dedicated to each subscale. The scale has demonstrated robust psychometric properties, including excellent internal consistency (Cronbach’s alpha = 0.95) and strong test-retest reliability (intraclass correlation coefficient [ICC] = 0.91), with kappa values ranging from 0.62 to 0.71. Concurrent validity is evidenced by a negative correlation with perceived stress and a significant positive correlation with rewarding feelings (Wang et al., 2021). In the present study, Cronbach’s alpha for the overall scale is 0.88, and for the subscales, it is 0.91 for significant others, 0.87 for family, and 0.85 for friends. Participants provide responses on a Likert scale ranging from 1 (absolutely disagree) to 7 (absolutely agree), with a higher score indicating greater perceived social support.
Perceived Stress Scale-10 (PSS-10)
The PSS-10 (Cohen et al., 1983) was used to assess participants perceived COVID-19 stress levels. The PSS-10 comprises ten items that are rated on a Likert scale ranging from 0 (never) to 4 (very often). The composite score can range from 0 to 40, with higher scores indicating greater perceived stress. The PSS-10 has demonstrated good reliability and validity, with reported Cronbach’s alphas ranging from 0.78 to 0.91 and test-retest reliability coefficients ranging from 0.55 to 0.85 (Cohen et al., 1983; Mitchell et al., 2008). For the present study, a modified version of the PSS-10 was utilized, adapted from the study of Zhang et al. (2021), to reflect perceived stress levels specifically related to the COVID-19 pandemic. The original PSS items were modified to start with the phrase “Since the COVID-19 has occurred,” with an example item being “Since the COVID-19 has occurred, how often have you been upset because of something that happened unexpectedly?”
Positive and Negative Affect Schedule (PANAS)
The PANAS (Watson et al., 1988) is composed of two 10-item mood scales that assess both positive and negative affect. For this study, only the positive affect subscale was utilized, as the negative affect was already measured by the DASS-21. Participants were asked to rate the degree to which they have experienced each emotion during a specified period, using a 5-point scale ranging from 1 (not at all) to 5 (very much). The internal consistency reliability of the PANAS scales ranges from.86 to.90 for positive affect and from.84 to.87 for negative affect, indicating good reliability. The Cronbach alpha for the positive affect subscale was 0.89 in this study. Díaz-García et al. (2020) additionally affirmed the suitability of the PANAS when administered online and endorsed its applicability in clinical settings.
Depression, Anxiety, and Stress Scales (DASS-21)
The DASS-21 (Lovibond and Lovibond, 1995) are a self-report assessment tool designed to measure levels of anxiety and depression, as well as stress. The items on the DASS-21 are rated on a 4-point scale, with 0 indicating that an item did not apply to the respondent at all and 3 indicating that an item applied to the respondent very much or most of the time. The internal consistency of the DASS-21 scales has been found to be good to excellent in previous research studies, as measured by Cronbach’s alpha (Lovibond and Lovibond, 1995). The validity of the DASS-21 has also been demonstrated consistently. In this study, the stress subscale of the DASS-21 was not included since perceived stress was the predictor variable under consideration. The Cronbach alpha for this study was 0.96. The DASS21 also exhibited strict longitudinal invariance, and the subscales also displayed adequate reliability in the two time points. The results are the first demonstration of longitudinal invariance with a Filipino sample and provide evidence that DASS-21 can be useful in both screening and in monitoring severity of different categories of symptoms over time, particularly among school-based Filipino youth (Simon and Bernardo, 2022).
Procedure
This study utilized a cross-sectional online survey to collect data between July 21, 2021 and August 5, 2021. The Ethics Committee for Psychological Research was contacted to obtain permission for conducting the survey. Before completing the measures, informed consent was obtained from each participant, and they completed the measures using Google Forms, which ensured anonymity and confidentiality. The survey comprised different measures, including a sociodemographic questionnaire, the Multidimensional Scale of Perceived Social Support (MSPSS), the Perceived Covid-19 Stress Scale-10 (PSS-10), the Positive affect subscale of the Positive and Negative Affect Schedule (PANAS), and the Depression and Anxiety subscales of DASS-21.
Ethical considerations
The procedures undertaken in this study involving human participants followed the ethical standards set forth by the institutional research committee. Ethics approval was obtained prior to data collection, and participants provided informed consent before completing the measures. The informed consent form contained comprehensive information on the nature and objectives of the study, as well as the requirements expected of the participants. Participants were also assured of the confidentiality and anonymity of their responses. The form indicated the researcher’s contact information in case a respondent experienced lingering discomfort from the survey questions or had further questions related to the study. Furthermore, only the researcher had access to the data obtained from the online surveys, which was stored in a password-protected personal laptop. Data was retained after publication to allow the researcher to address any inquiries about the results and will be deleted a few years after publication.
Data analysis
Preliminary analyses included checking the assumptions of normality, linearity, and homoscedasticity. Descriptive statistics were calculated for all measures, and the evaluation of the relationships between the variables was performed using the Pearson - r correlation analysis. The bootstrapping method, involving resampling from the data with replacement to create multiple datasets, encompasses the computation of correlations and the examination of correlation coefficient distributions. This technique provides an empirical estimate of the statistical distribution, thereby improving our comprehension of the variability in the targeted statistic. Its application was instrumental in addressing errors stemming from multiple bivariate correlation analyses. The analyses of the mediation effects, were conducted using the IBM SPSS Statistics 25 software and the PROCESS plug-in version 4.0. To test the hypothesis that perceived stress mediated the relationship between social support with positive affect, anxiety, and depression, the bootstrap method was used for the analysis of the effect of mediation (Model 4), with a sample size of 5000. The mediation effect test was considered significant when it did not contain zero under the 95% confidence interval (CI), and the significance level was set at p ≤ 0.05. In the mediation analysis, potential confounders were included as covariates. This involves statistically controlling for the influence of these variables to isolate the direct and indirect effects of the independent variable on the dependent variable through the mediator.
Results
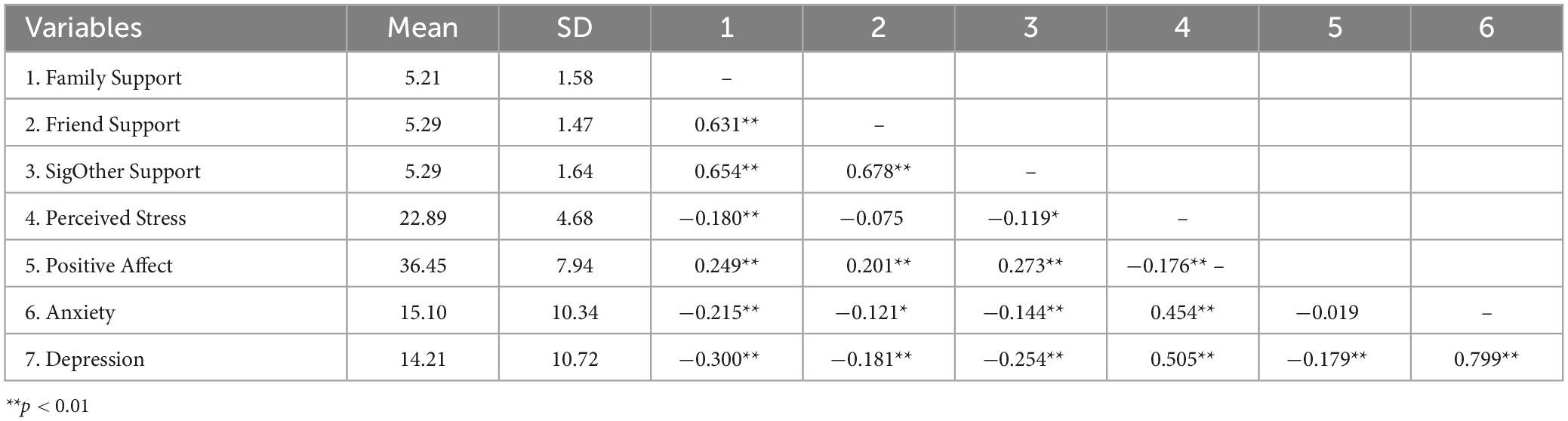
Table 1 presents the descriptive statistics and bivariate correlations among this study’s variables. Most participants (61.3%) reported a high level of social support from their family, friends, and significant others. In terms of perceived stress, most participants reported moderate levels (78.2%), with a smaller portion indicating high levels (20%), while only 1.9% reported experiencing low stress. Furthermore, most participants reported an average level of positive affect, with an average score of 36.45. However, a significant number of participants (65%) reported experiencing moderate to severe anxiety symptoms, and 49.7% reported moderate to severe depression symptoms.
Results of the correlation analysis revealed significant associations between social support and mental health outcomes. Family support displayed a weak yet statistically significant positive correlation with positive affect (r = 0.25, p ≤ 0.01), indicating that heightened family support is linked to increased positive affect. Conversely, family support exhibited weak negative relationships with anxiety (r = −0.22, p ≤ 0.01) and depression (r = −0.30, p ≤ 0.01), suggesting that greater family support corresponds to reduced levels of anxiety and depression. Furthermore, family support demonstrated a weak negative relationship with perceived stress (r = −0.18, p ≤ 0.01), implying that individuals perceiving stronger family support tend to experience lower perceived stress levels.
Similarly, support from significant others exhibited a weak but statistically significant positive relationship with positive affect (r = 0.27, p ≤ 0.01) and displayed low negative relationships with anxiety (r = −0.14, p ≤ 0.01) and depression (r = −0.25, p ≤ 0.01). These results indicate that enhanced support from significant others is associated with increased positive affect and reduced levels of anxiety and depression. Notably, this form of support also showed a low negative relationship with perceived stress (r = −0.12, p ≤ 0.01) suggesting that individuals perceiving stronger support from significant other tend to experience lower perceived stress levels.
Further, friend support exhibited a weak positive relationship with positive affect (r = 0.20, p ≤ 0.01) and displayed weak negative relationships with anxiety (r = −0.12, p ≤ 0.05) and depression (r = −0.18, p ≤ 0.05). However, no significant relationship was observed between friend support and perceived stress. These findings reveal the distinct roles of different sources of social support in shaping individuals’ mental health, with family and significant other support appearing to have a more substantial impact compared to friend support.
To address the question of whether social support predicts positive affect, anxiety, and depression, the findings indicate the following: Based on the total effects, family support demonstrated a significant and positive prediction of positive affect (Figure 2), and a significant negative prediction of anxiety, and depression (Figures 3, 4). Similarly, support from significant other demonstrated a significant and positive prediction of positive affect (Figure 5), and a significant negative prediction of anxiety, and depression (Figures 6, 7). Further, friend support demonstrated a significant and positive prediction of positive affect (Figure 8), and a significant negative prediction of anxiety, and depression (Figures 9, 10).
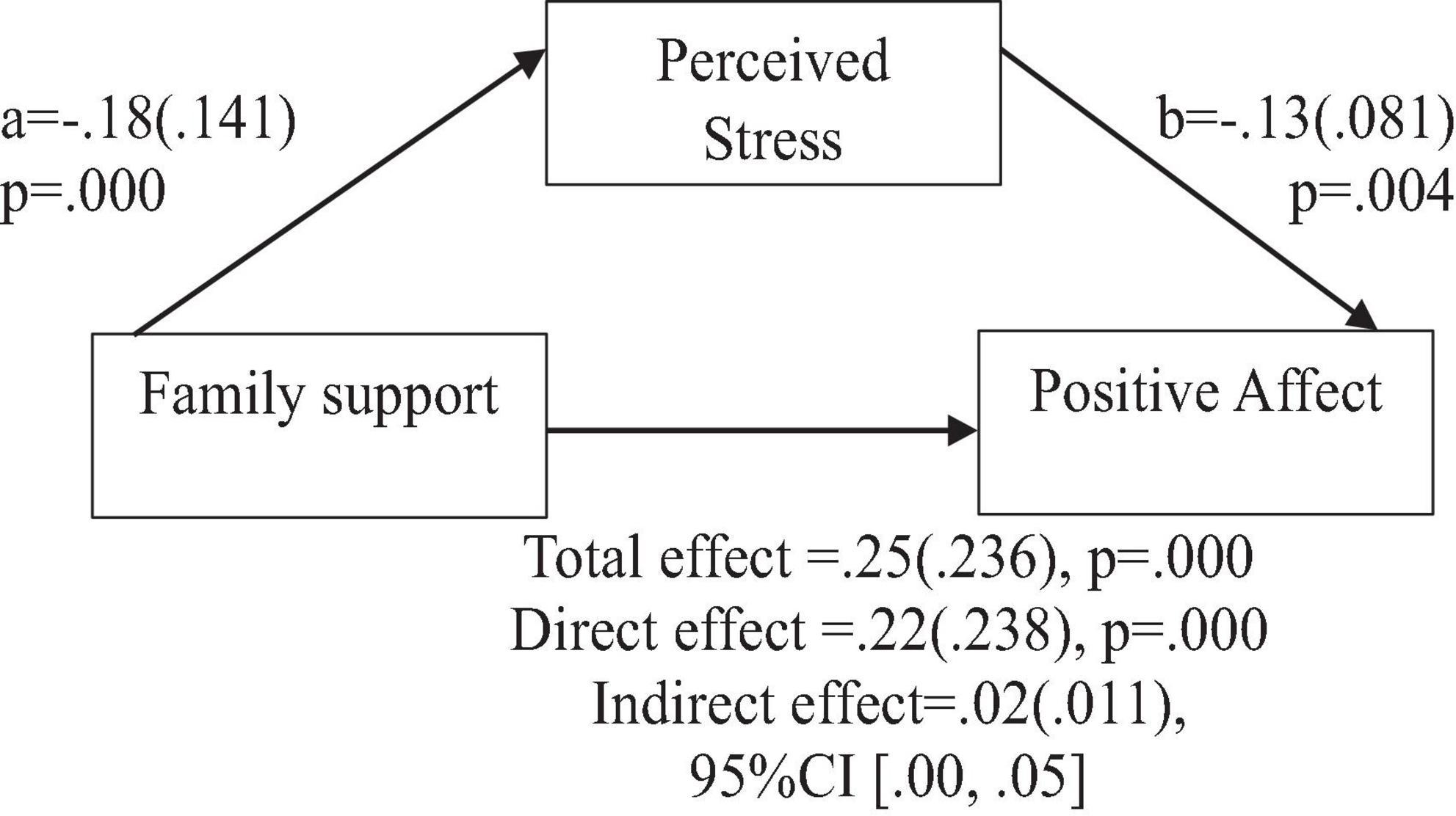
Figure 2. Family support predicts positive affect indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
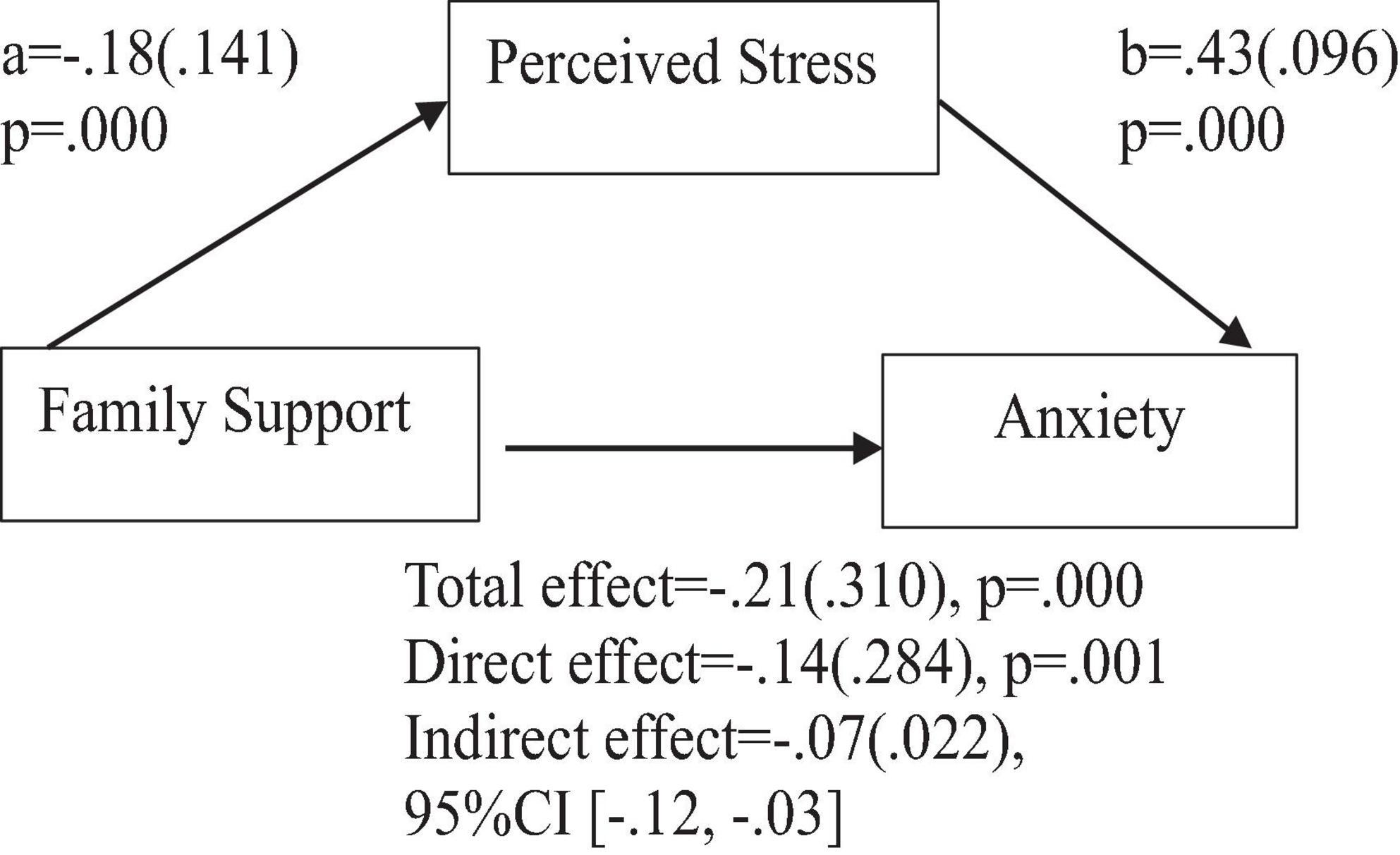
Figure 3. Family support predicts anxiety indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
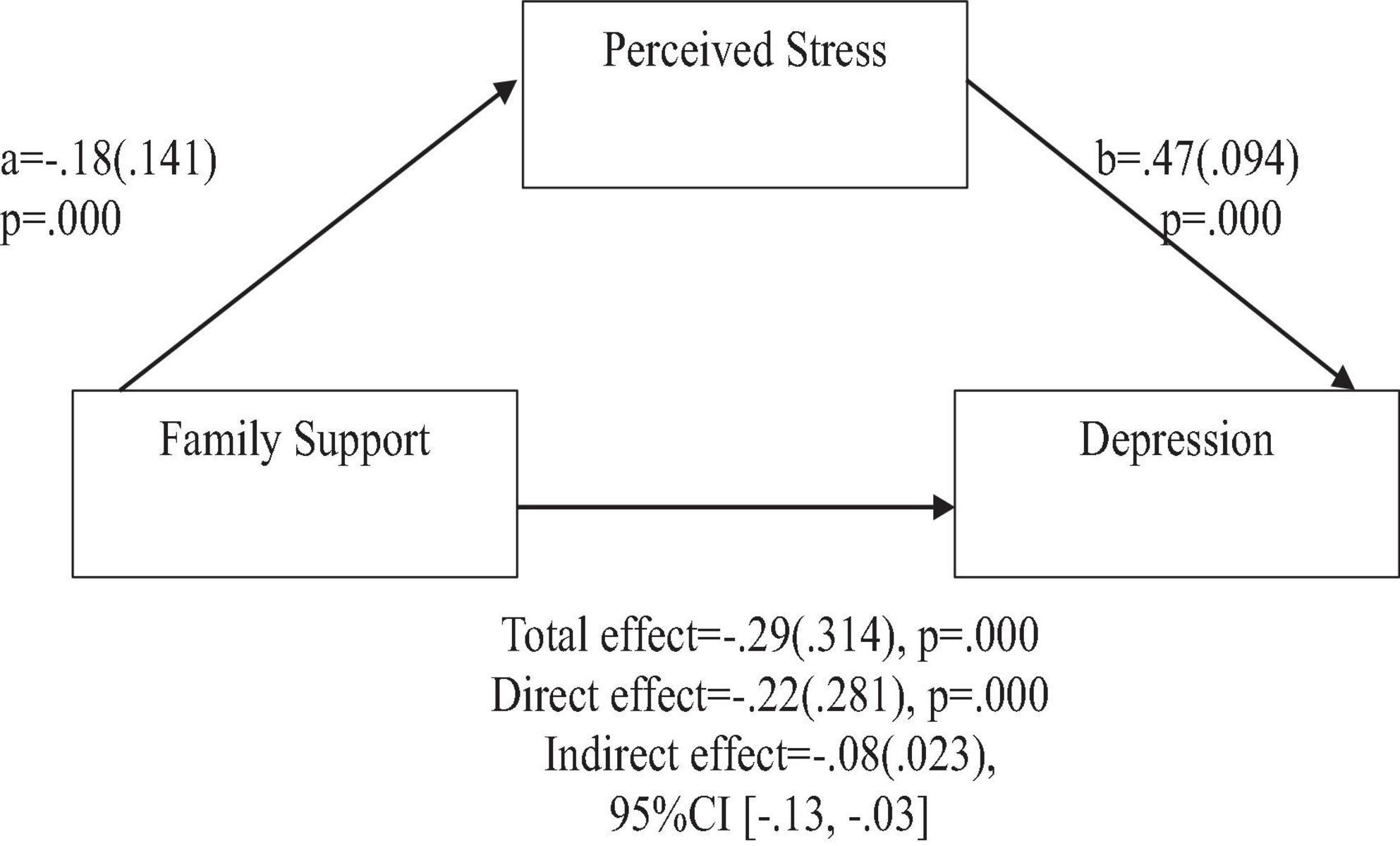
Figure 4. Family support predicts depression indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
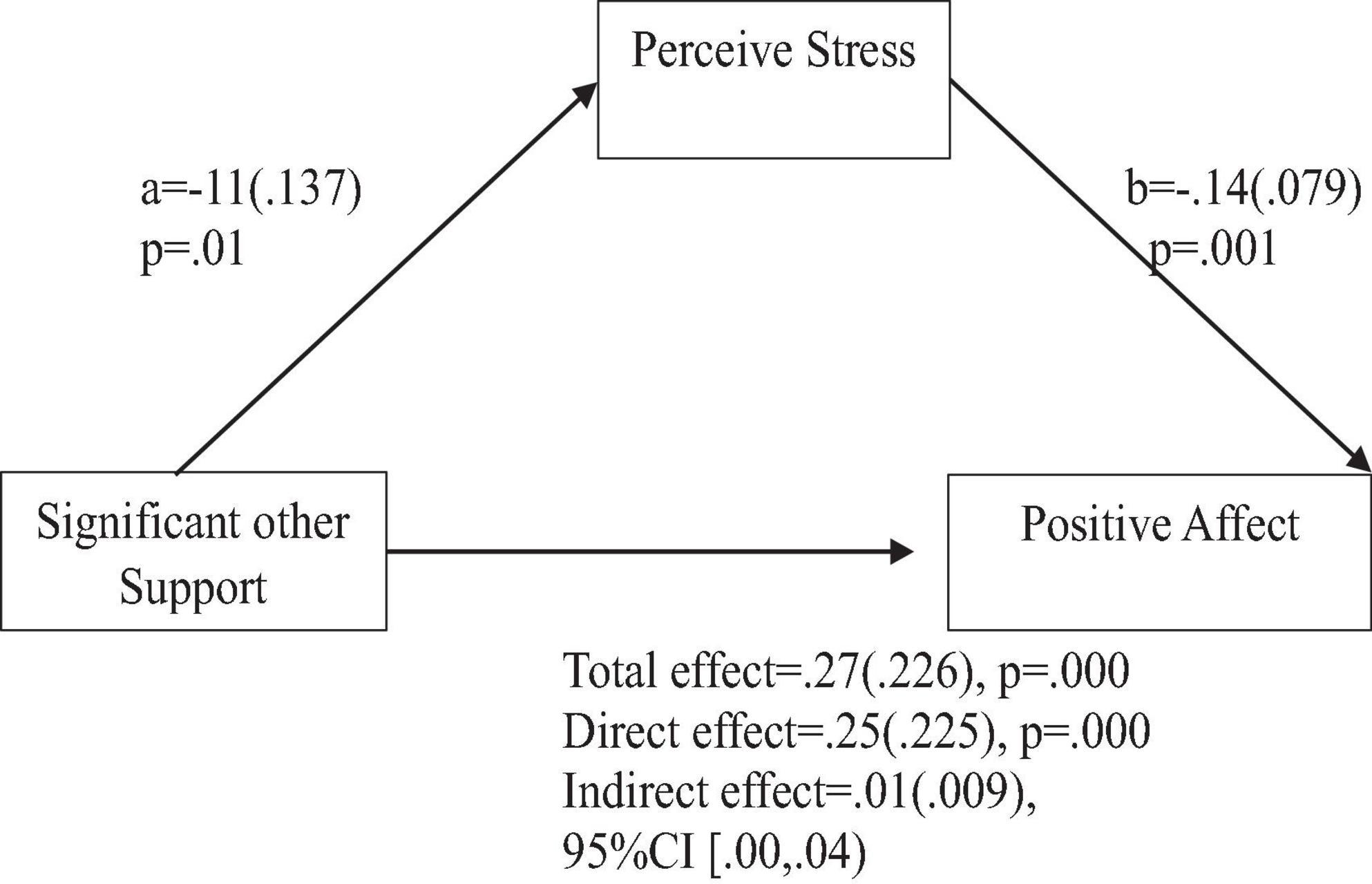
Figure 5. Support from significant other predicts positive affect indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
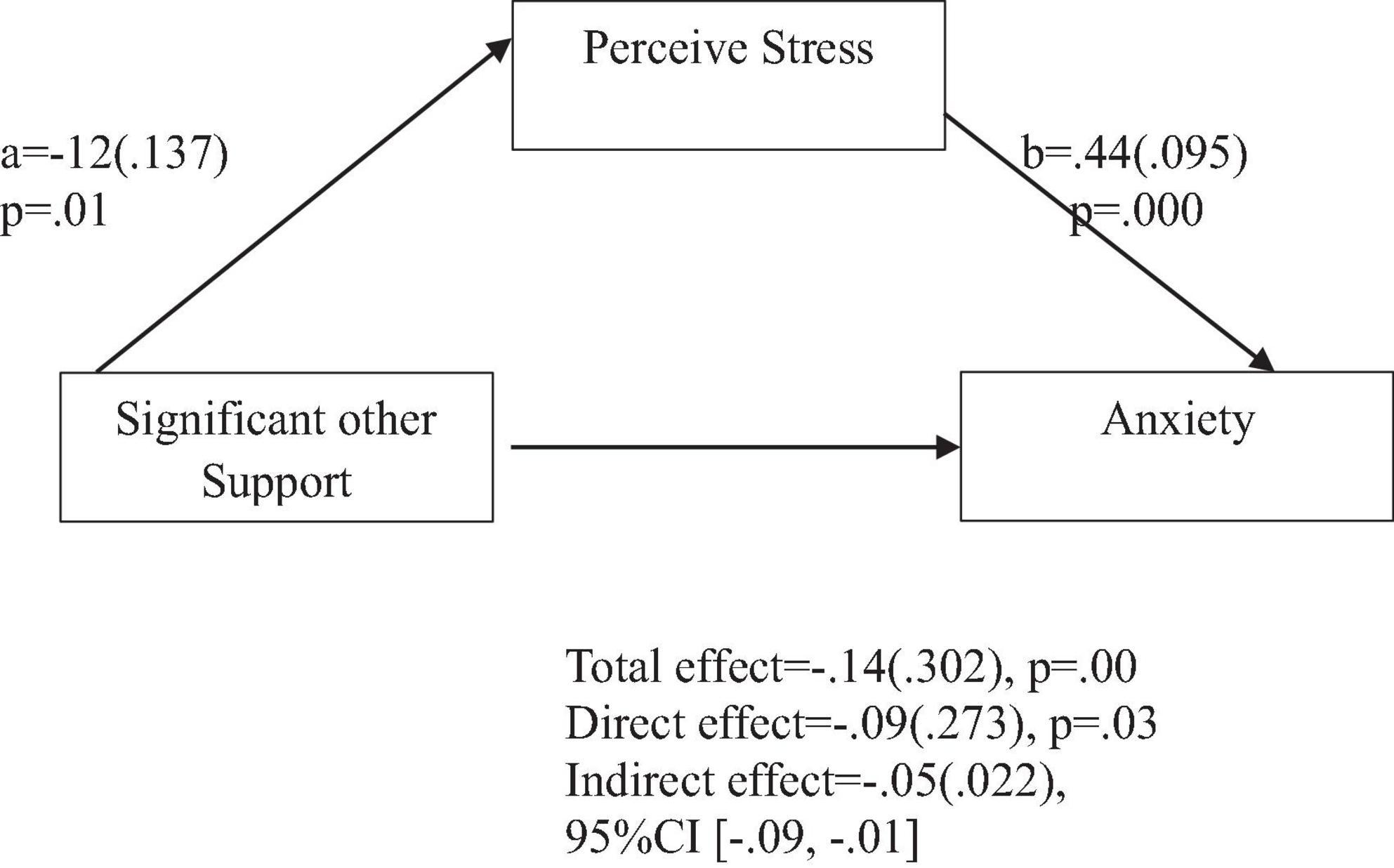
Figure 6. Support from significant other predicts anxiety indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
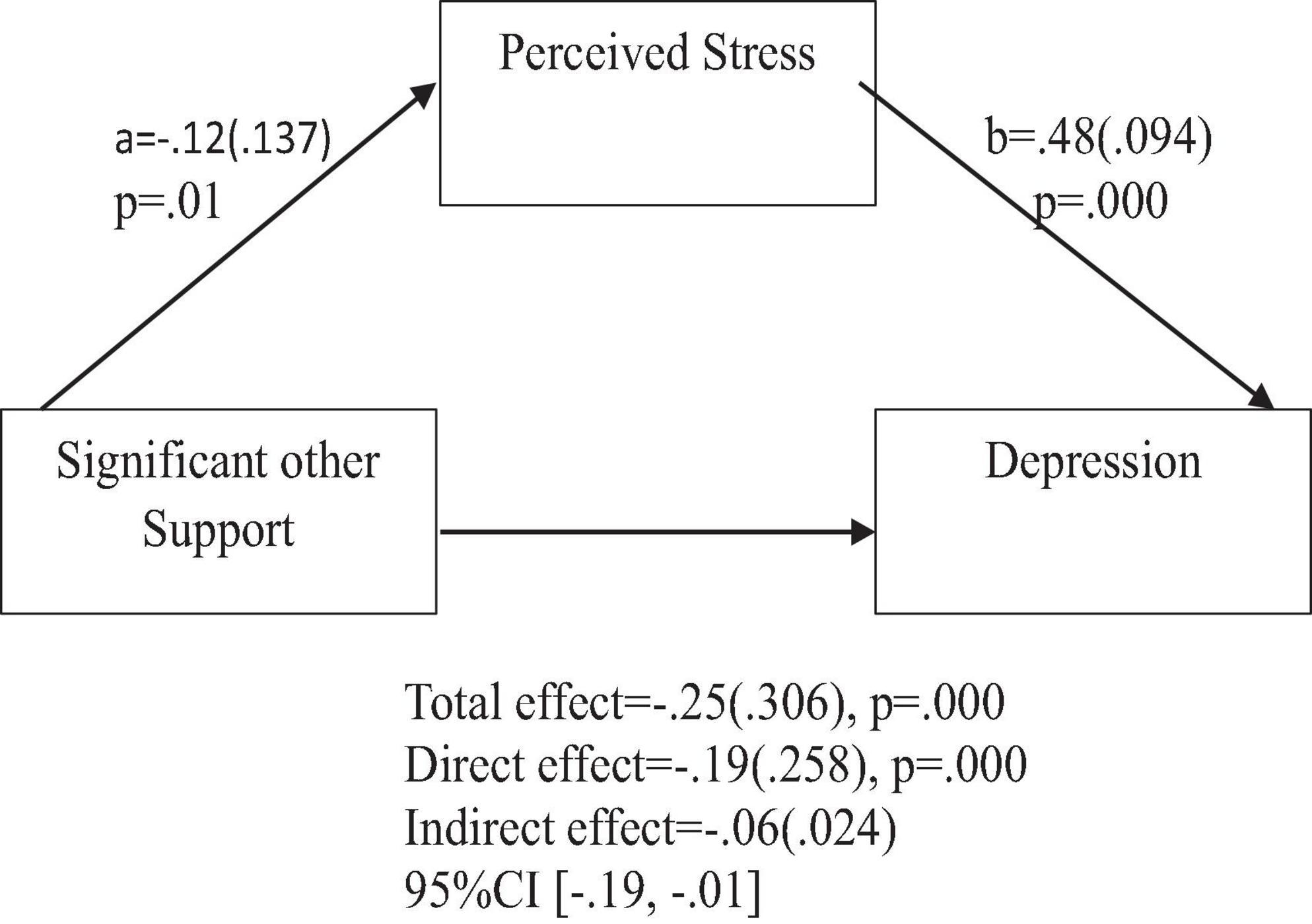
Figure 7. Support from significant other predicts depression indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
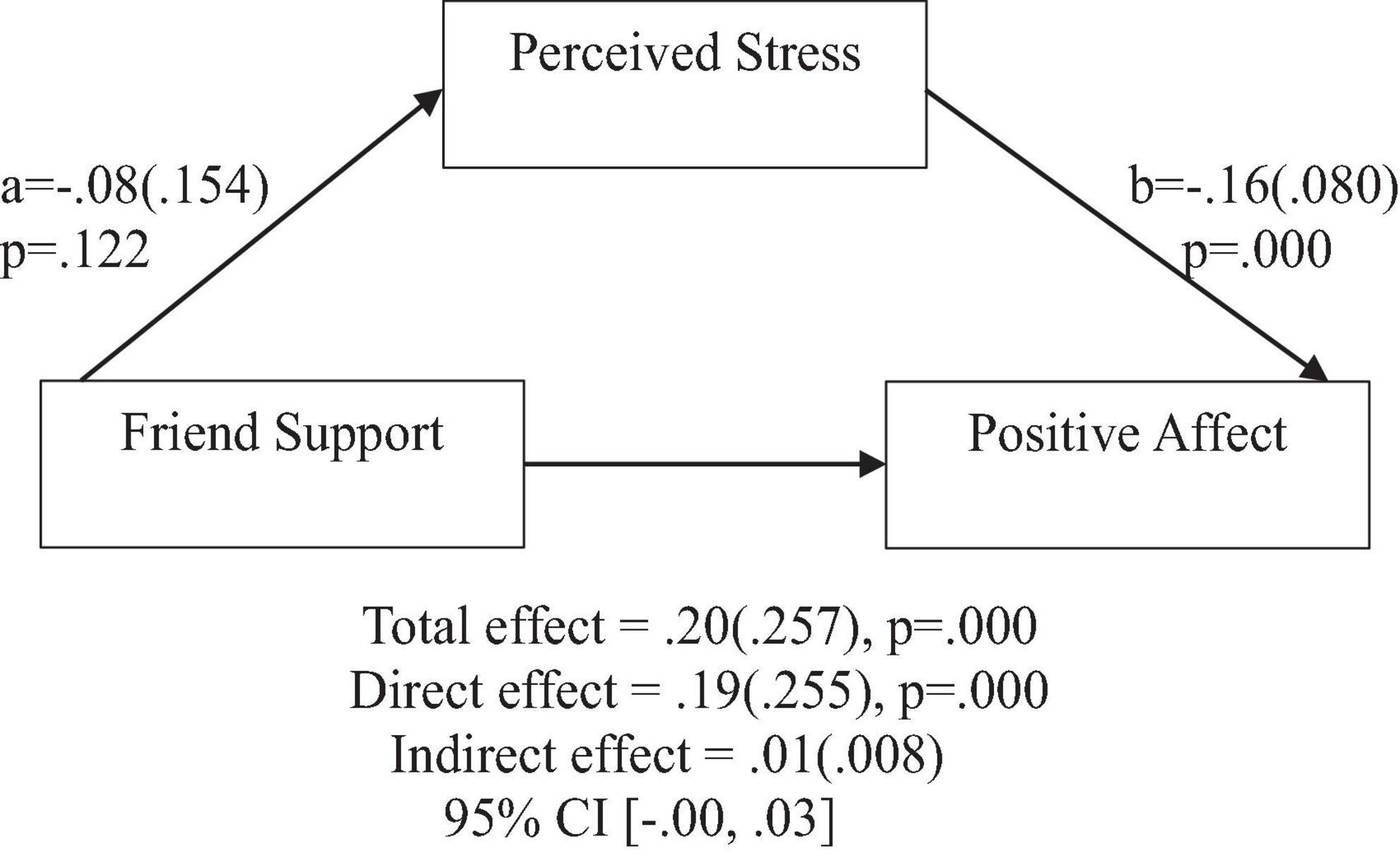
Figure 8. Friend support does not predict positive affect indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
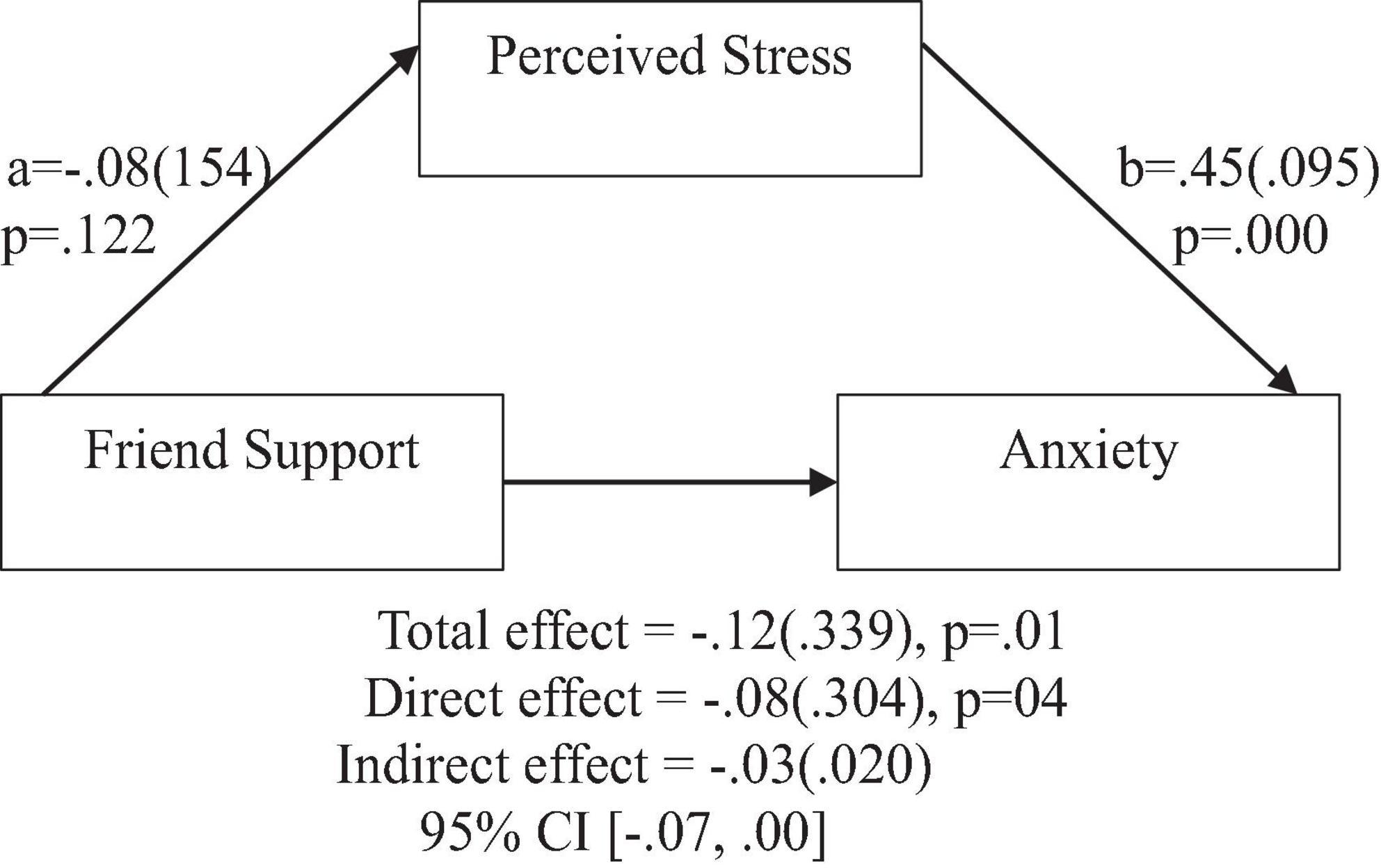
Figure 9. Friend support does not predict anxiety indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
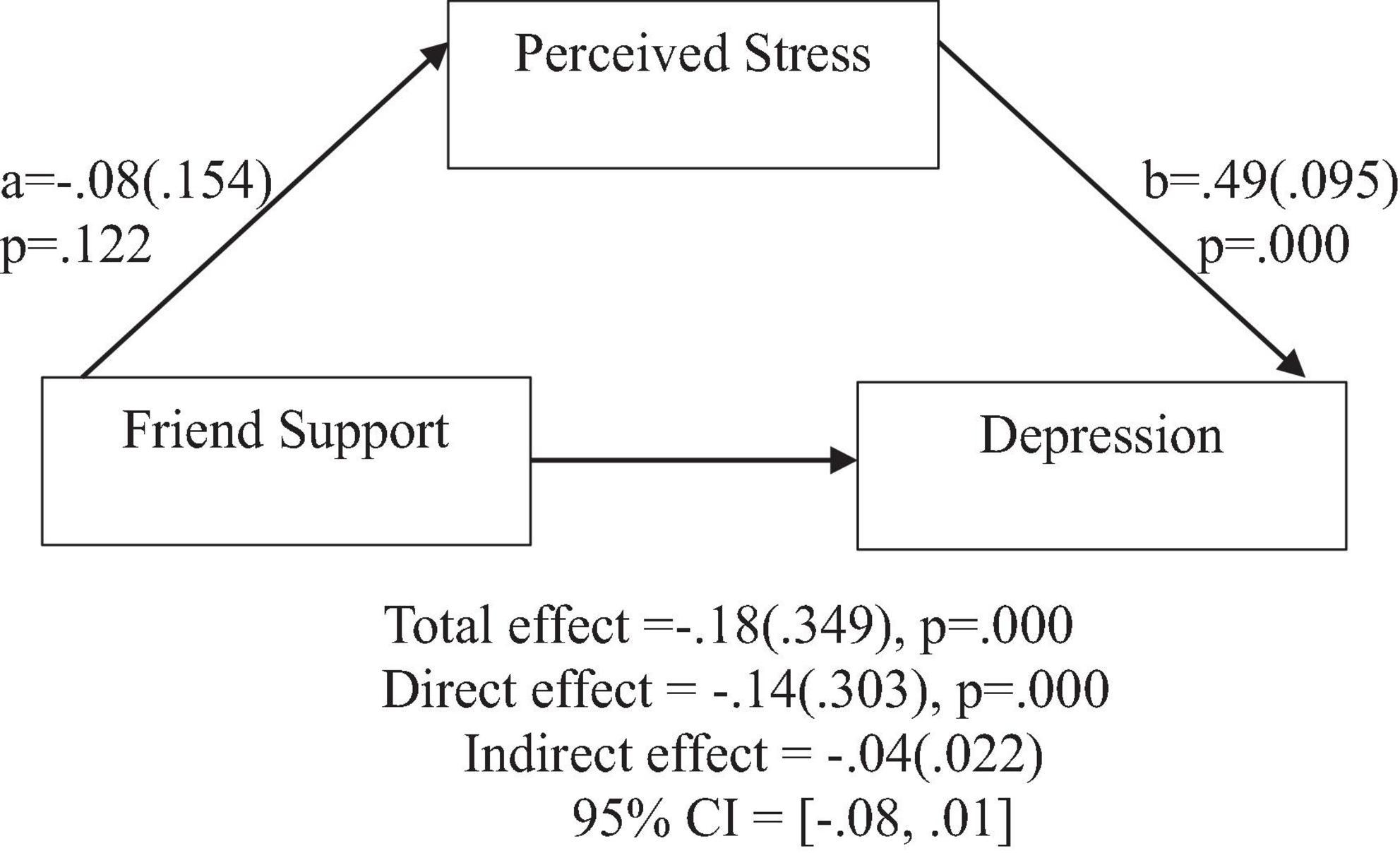
Figure 10. Friend support does not predict depression indirectly through perceived stress. Coefficients are standardized with standard error in parentheses.
When considering perceived stress as mediator, the direct effects of family support on positive affect, anxiety, and depression remained significant (Figures 2–4). Similarly, after accounting for perceived stress as mediator, the direct effect of support from significant other on positive affect, anxiety and depression remained significant (Figures 5–7). Furthermore, the direct effects of friend support on positive affect, anxiety, and depression were significant (Figures 8–10).
The study assessed the mediating role of perceived stress on the relationship between family support and positive affect, anxiety, and depression. Figure 2 revealed a significant indirect effect of family support on positive affect through perceived stress [β = 0.02(0.010)], 95% CI [0.00, 0.05]. Family support negatively predicted perceived stress (a = −0.18, p = 0.000), which in turn negatively predicted positive affect (b = −0.13, p = 0.004). Similarly, the study also found a significant indirect effect of family support on anxiety through perceived stress [β = −0.07(0.022), 95% CI (−0.12, −0.03)]. Family support negatively predicted perceived stress (a = −0.18, p = 0.000), which in turn positively predicted anxiety (b = 0.43, p = 0.000). Furthermore, the study also found a significant indirect effect of family support on depression through perceived stress [β = 0.08(0.023), 95% CI (−0.13, −0.03)]. Family support negatively predicted perceived stress (a = −0.18, p = 0.000), which in turn positively predicted depression (b = 0.47, p = 0.000).
The study also assessed the mediating role of perceived stress on the relationship between support from significant other and positive affect, anxiety, and depression. Figure 5 revealed a significant indirect effect of support from significant other on positive affect through perceived stress [β = 0.01(0.009), 95% CI (0.00,0.04)]. Support from significant other negatively predicted perceived stress (a = −0.11, p = 0.01), which in turn negatively predicted positive affect (b = −0.14, p = 0.001). Similarly, the study also found a significant indirect effect of support from significant other on anxiety through perceived stress [β = −0.05(0.022), 95% CI (−0.09, −0.01)]. Support from significant other negatively predicted perceived stress (a = −0.12, p = 0.01), which in turn positively predicted anxiety (b = 0.44, p = 0.000). Furthermore, the study also found a significant indirect effect of support from significant other on depression through perceived stress [β = −0.06(0.023), 95% CI (−0.19, −0.01)]. Significant other support negatively predicted perceived stress (a = −0.12, p = 0.01), which in turn positively predicted depression (b = 0.48, p = 0.000).
In contrast, friend support was found to have no significant indirect effect through perceived stress on positive affect [β = 0.01(0.008), 95% CI (−0.00,0.03)], anxiety [β = −0.03(0.020), 95% CI (−0.07,0.00)], and depression [β = −0.04(0.022), 95% CI (−0.08,0.01)].
Discussion
Social support and mental health outcomes
The current study substantiates the hypothesis that social support, emanating from diverse sources such as family, friends, and significant others, is positively correlated with positive affect and inversely associated with symptoms of anxiety and depression. In essence, heightened perceived social support corresponds to increased positive affect and diminished anxiety and depression symptoms. These findings resonate with prior and more recent research conducted across various cultural and demographic settings (Chu et al., 2010; Gülaçtı, 2010; Gariepy et al., 2016; Wang et al., 2018; Bender et al., 2019; Mohd et al., 2019; Watson et al., 2019; Alshehri et al., 2020; Cobo-Rendón et al., 2020; Grey et al., 2020; Xiao et al., 2020; Özmete and Pak, 2020; Bedaso et al., 2021; Ghafari et al., 2021; Liu et al., 2021; Yildirim and Aziz, 2023; Yıldırım and Green, 2023; Yıldırım et al., 2023; Green et al., 2024).
These compelling findings underscore social support as a pivotal resource stemming from an individual’s social network. This resource manifests in various forms, encompassing emotional, instrumental, and informational support, each catering to distinct needs. Notably, emotional support cultivates a profound sense of love and care, assuring individuals of available assistance when needed. Access to emotional support fosters a secure and accepting environment, facilitating the expression, and processing of emotions. This openness enables individuals to share concerns, vent feelings, and receive empathetic understanding. The impact of emotional support on mental health outcomes is profound, aiding individuals in coping with emotions and bolstering overall well-being. Instrumental support emerges as another influential dimension of social support, offering practical assistance, resources, and guidance in navigating stressors. This facet equips individuals with the tools necessary to effectively confront challenging situations, highlighting the tangible and practical role of social support in mitigating adversity. Additionally, social support extends to informational support, providing valuable information, advice, or feedback. The diverse types and functions of social support thus afford individuals the opportunity to meet various human needs, ultimately contributing to enhanced mental well-being and a reduction in negative mental health consequences.
From a pragmatic perspective, these discoveries hold significant clinical implications. Mental health interventions ought to transcend individual focus, acknowledging the wider social context. Therapeutic strategies that actively engage and harness the support of family, friends, and significant others may demonstrate greater efficacy in fostering positive mental health outcomes. Moreover, interventions could be customized to target forms of support in accordance with individual needs. The integration of these insights into clinical practice shows potential for crafting more holistic and impactful interventions, ultimately playing a role in enhancing mental well-being across varied populations.
Social support and perceived COVID-19 stress
Consistent with the study’s hypothesis, this research found that social support (from family, friends, and significant others) is negatively associated with perceived stress, indicating that social support decreases perceived stress. These results align with prior studies conducted in diverse cultural and demographic backgrounds (Ekmen et al., 2021; Özer et al., 2021; McLean et al., 2023; Yıldırım and Green, 2023).
Drawing on Lazarus and Folkman’s stress and coping theory, the study illuminates the influential role of social support in shaping our stress perceptions. In the face of challenging events, stress intensifies when we feel overwhelmed and lack coping resources. Conversely, a belief in having adequate support to navigate such events tends to alleviate stress. Social support, manifesting in emotional assistance, practical aid, guidance, and companionship, plays a vital role in this evaluation process. Access to these forms of support enhances our ability to perceive events as less stressful, emphasizing that stressfulness is not solely determined by the event itself but also by our personal evaluations, including the strength of our social support network.
Clinically, these findings underscore the potential of integrating social support interventions into mental health strategies, especially for individuals experiencing heightened stress, such as during a global pandemic. Therapeutic approaches that actively involve and cultivate social support networks emerge as powerful tools in alleviating perceived stress. Mental health practitioners are encouraged to incorporate assessments of social support systems into their evaluations, identifying areas for enhancement and tailoring interventions accordingly.
Healthcare practitioners should acknowledge the stress-alleviating benefits of social support and advise individuals to enhance their social connections, cultivate a sense of community, and promote transparent communication within their social networks. This comprehensive approach recognizes the intricate interplay between individual and social factors, offering a more thorough and effective clinical framework for addressing stress during a global health crisis and beyond.
Perceived stress, positive affect, anxiety, and depression
Consistent with the study’s hypothesis, the findings revealed a negative association between perceived stress and positive affect, indicating that individuals reporting higher levels of perceived stress exhibited lower levels of positive affect. Furthermore, the study demonstrated that perceived stress was a positive predictor of anxiety and depression, suggesting that heightened levels of perceived stress corresponded to an increased likelihood of experiencing symptoms related to anxiety and depression. These outcomes align with earlier investigations conducted across diverse cultural and demographic contexts (Pieh et al., 2020; Salari et al., 2020; Huang and Zhao, 2021).
The interpretation of these results draws on Lazarus and Folkman’s stress and coping theory. According to this theory, the inverse correlation between perceived stress and positive affect stems from viewing the stressor, in this case, the COVID-19 pandemic, as a threat to one’s well-being, thereby diminishing positive emotional states. Similarly, the positive association between perceived stress and anxiety and depression aligns with the theory’s proposition that unmanaged stress can lead to emotional distress.
Lazarus and Folkman’s stress and coping theory (1984) prove instrumental in comprehending the impact of perceived stress on positive affect, anxiety, and depression in the context of the current study, which focuses on the COVID-19 pandemic as a potential stressor. Recognized as a health emergency, the pandemic embodies characteristics such as harm, life threatening aspects, unpredictability, constraints, trauma, and chronicity, all fulfilling the criteria of a stressor (Wheaton and Montazer, 2017). Additionally, government-mandated mitigating measures add another layer of stress. The nature and demands of the pandemic contribute to prolonged stress experiences, potentially resulting in mental health challenges, as indicated by the study’s findings.
Moreover, the observed decline in positive affect or overall well-being during the pandemic may be attributed to disruptions in activities traditionally associated with enhanced well-being. Activities like outdoor exercising (Reed and Ones, 2006), walking (Hanson and Jones, 2015), and exposure to natural environments (Bowler et al., 2010) are known to promote wellbeing. The pandemic, due to governmental measures aimed at minimizing the virus’s spread, compromises these activities, adversely affecting people’s positive affect.
In a clinical context, these findings emphasize the critical significance of acknowledging and addressing perceived stress as a prominent factor that influences mental health outcomes. Clinicians are encouraged to integrate stress management strategies into their interventions, aiming to alleviate the adverse impact on positive affect and diminish the likelihood of anxiety and depression symptoms. Moreover, a nuanced comprehension of the distinct stressors linked to the pandemic, notably the disruption of activities known to promote well-being, enables targeted interventions to enhance overall mental well-being in the face of challenging circumstances.
Furthermore, as elucidated earlier, healthcare practitioners should recognize and leverage the stress-alleviating benefits inherent in social support. This entails not only acknowledging the role of social connections but actively incorporating strategies to enhance and capitalize on these supportive networks. Such an approach aligns with the multifaceted nature of mental health interventions, integrating both stress management and social support strategies to create a more comprehensive and effective clinical framework.
Perceived stress as a mediator between the association of social support and mental health outcomes
The outcomes of the present study offer robust support for the hypothesis that perceived stress operates as a pivotal mediator in the relationship between social support from family and significant others and key mental health outcomes, including positive affect, anxiety, and depression. This empirical investigation establishes a clear pathway through which social support exerts its influence, illuminating the role of perceived stress as a critical factor in the enhancement of positive affect and the mitigation of anxiety and depression.
The mediation analyses conducted in this study provide compelling evidence that both family and significant other support possess the potential to elevate positive affect by attenuating perceived stress levels. This suggests that the impact of social support on fostering a positive emotional state operates, at least in part, through the reduction of perceived stress. Furthermore, the findings underscore the effectiveness of family and significant other support in alleviating symptoms of anxiety and depression, emphasizing the role of perceived stress as a key mediator in this relationship. These insights emphasize the nuanced dynamics between social support, perceived stress, and mental health outcomes.
As elucidated earlier, encountering challenging events can induce a sense of overwhelm and resource inadequacy, leading to heightened stress levels. However, the presence of a robust support system, encompassing emotional support, practical assistance, guidance, and companionship, emerges as a buffer against these stressors. Notably, this study highlights the subjective evaluation of stressfulness, suggesting that it is not solely the nature of the events but also the perceived availability of a social support network that shapes our stress experience. Access to social support transforms daunting events into more manageable challenges, thereby significantly contributing to improved mental health outcomes. The study underscores the instrumental role of social support in reshaping individuals’ perceptions of stress and, consequently, their mental well-being.
Finally, the intriguing observation of the absence of an indirect influence of friend support on mental health through perceived stress warrants careful consideration. This observation gains added significance when contextualized within the unique challenges posed by the COVID-19 pandemic. The implementation of stringent mitigation measures, such as social distancing and quarantine, may have substantially restricted opportunities for interpersonal interactions with friends. This altered social landscape likely accounts for the non-significant impact of friend support on mental health through perceived stress. However, it prompts further exploration into alternative mechanisms that may more effectively elucidate the intricate dynamics of how friend support influences mental health outcomes, especially in the context of unprecedented challenges like a global pandemic.
In sum, this study advances our understanding of the nuanced relationships between social support, perceived stress, and mental health outcomes. The identified role of perceived stress as a mediator adds a layer of complexity to our comprehension of how social support operates to shape positive affect and alleviate symptoms of anxiety and depression. These findings carry significant clinical implications, underscoring the importance of incorporating interventions that target perceived stress into mental health strategies, with a particular focus on enhancing social support from family and significant others. Recognizing and fortifying these dynamics can contribute to more effective clinical approaches that address the multifaceted nature of mental health challenges.
Limitations of the study
The present study’s findings should be interpreted in light of several limitations. Firstly, the cross-sectional design inherently limits the establishment of definitive causality among the study’s variables. Future research endeavors may explore longitudinal designs to ascertain conclusive causality among the variables under investigation. Secondly, the data collected and analyzed relied on self-reported measures, which introduces the possibility of common-method bias. To address this concern, future studies could incorporate additional measures, such as behavioral observations. Thirdly, the online data collection method employed in this study may have implications for the sample characteristics, potentially limiting the generalizability of the findings. To address this issue, future research could explore alternative data collection methods to include individuals who lack internet access. Nevertheless, despite these limitations, the findings of this study significantly contribute to our understanding of human social support and its mechanisms of effects during the Covid-19 pandemic. Moreover, the findings offer valuable empirical evidence that supports the stress and coping theory proposed by Lazarus and Folkman.
Theoretical implications
The findings of this study carry significant theoretical implications, offering added empirical support for the application of the Stress and Coping Theory (Lazarus and Folkman, 1984) within the context of Filipino adults. Moreover, the study extends this theory by providing evidence for the mechanisms through which social support influences mental health outcomes. By shedding light on the potential mechanisms underlying the positive correlation between social support and favorable mental health outcomes, as well as the inverse relationship with negative mental health outcomes, this research contributes to our understanding of the intricate dynamics at play. Notably, the study highlights perceived stress as a pivotal mediating factor in the connection between familial and significant other support and positive affect, anxiety, and depression. These findings emphasize the critical role of reducing perceived stress as a mechanism through which familial and significant other support can positively impact individuals’ mental well-being. However, it is noteworthy that in this study, perceived stress did not act as a mediating factor in the relationship between friend support and positive affect, anxiety, and depression. This suggests the necessity for further investigation, as alternative mechanisms may provide a more accurate explanation for this association. The absence of a mediating role for perceived stress in the friend support relationship underscores the complexity of social support dynamics and prompts exploration into additional factors contributing to mental health outcomes within the context of friendships.
Practical implications
From a clinical standpoint, these results hold significant meaning and carry practical implications. Mental health professionals should not only prioritize the assessment of social support networks but also consider the specific mediating role of perceived stress in family and significant other relationships. Recognizing the nuanced dynamics of social support can inform tailored interventions aimed at reducing perceived stress and enhancing positive mental health outcomes. The study’s observation of differing mediation patterns with friend support emphasizes the need for a comprehensive understanding of various social support sources, guiding clinicians to explore diverse mechanisms that influence mental health outcomes in different relational contexts.
Recommendation
Based on the conclusions derived from this study, several recommendations can be proposed for future research and clinical practice. Firstly, a more comprehensive understanding can be attained by exploring the effects of different types of social support and the moderators influencing these effects. Conducting longitudinal studies is imperative for investigating the lasting impacts of social support on mental health outcomes. Such studies will provide the opportunity to explore more definitive causal relationships among the variables under investigation. In clinical practice, it is vital for mental health professionals to evaluate social support networks and their impact on perceived stress, enabling personalized interventions. Tailoring interventions to capitalize on the distinctive advantages of various sources of social support is crucial considering their differing effects. Delving into the interactions between social support and variables like cultural context or individual differences is essential for a more nuanced understanding. Addressing these recommendations in future research can augment our comprehension of the role of social support in mental health, while in clinical practice, targeted interventions can be developed to foster positive mental health outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the De La Salle University, Manila, Philippines. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing−original draft, Writing− review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The author conveys her gratitude to her dissertation panel, who provided significant guidance and assistance in completing this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alhakami, A., Salem, V., Alateeq, D., Nikčević, A. V., Marci, T., Palmieri, S., et al. (2023). The Arab COVID-19 Anxiety Syndrome Scale (C-19ASS): COVID-19 anxiety syndrome and psychological symptoms in the Saudi Arabian population. Clin. Psychol. Psychotherapy 30, 1083–1094. doi: 10.1002/cpp.2860
Allen, K., Blascovich, J., and Mendes, W. B. (2002). Cardiovascular reactivity and the presence of pets, friends, and spouses: the truth about cats and dogs. Psychosom. Med. 64, 727–739.
Alshehri, N. A., Yildirim, M., and Vostanis, P. (2020). Saudi adolescents’ reports of the relationship between parental factors, social support, and mental health problems. Arab J. Psychiatry 31, 130–143.
Bedaso, A., Adams, J., Peng, W., and Sibbritt, D. (2021). The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod. Health 18, 1–23.
Bender, M., van Osch, Y., Sleegers, W., and Ye, M. (2019). Social support benefits psychological adjustment of international students: Evidence from a meta-analysis. J. Cross-Cult. Psychol. 50, 827–847.
Bowler, D. E., Buyung-Ali, L. M., Knight, T. M., and Pullin, A. S. (2010). A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health 10:456. doi: 10.1186/1471-2458-10-456
Brailovskaia, J., Cosci, F., Mansueto, G., Miragall, M., Herrero, R., Baños, R. M., et al. (2021). The association between depression symptoms, psychological burden caused by Covid-19 and physical activity: An investigation in Germany, Italy, Russia, and Spain. Psychiatry Res. 295:113596. doi: 10.1016/j.psychres.2020.113596
Chu, P. S., Saucier, D. A., and Hafner, E. (2010). Meta-analysis of the relationships between social support and well-being in children and adolescents. J. Soc. Clin. Psychol. 29, 624–645.
Cobb, S. (1976). Social support as a moderator of life stress. Psychosom. Med. 38, 300–314. doi: 10.1097/00006842-197609000-00003
Cobo-Rendón, R., López-Angulo, Y., Pérez-Villalobos, M. V., and Díaz-Mujica, A. (2020). Perceived social support and its effects on changes in the affective and eudaimonic well-being of Chilean university students. Front. Psychol. 11:590513. doi: 10.3389/fpsyg.2020.590513
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396. doi: 10.2307/2136404
Cohen, S., and Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bull. 98, 310–357. doi: 10.1037/0033-2909.98.2.310
Courtet, P., Olié, E., Debien, C., and Vaiva, G. (2020). Keep socially (but not physically) connected and carry on: preventing suicide in the age of COVID-19. J. Clin. Psychiatry 81:20com13370. doi: 10.4088/JCP.20com13370
Díaz-García, A., González-Robles, A., Mor, S., Mira, A., Quero, S., García-Palacios, A., et al. (2020). Positive and Negative Affect Schedule (PANAS): Psychometric properties of the online Spanish version in a clinical sample with emotional disorders. BMC Psychiatry 20:56. doi: 10.1186/s12888-020-2472-1
Eden, A. L., Johnson, B. K., Reinecke, L., and Grady, S. M. (2020). Media for Coping During COVID-19 Social Distancing: Stress, Anxiety, and Psychological Well-Being. Front. Psychol. 11:577639. doi: 10.3389/fpsyg.2020.577639
Ekmen, E., Koçak, O., Solmaz, U., Kopuz, K., Younis, M. Z., and Orman, D. (2021). How does the social support affect refugees’ life satisfaction in Turkey? Stress as a mediator, social aids and coronavirus anxiety as moderators. Sustainability 13:12727.
Epel, E. S., Crosswell, A. D., Mayer, S. E., Prather, A. A., Slavich, G. M., Puterman, E., et al. (2018). More than a feeling: A unified view of stress measurement for population science. Front. Neuroendocrinol. 49:146–169. doi: 10.1016/j.yfrne.2018.03.001
Ford, M. T., Heinen, B. A., and Langkamer, K. L. (2007). Work and family satisfaction and conflict: a meta-analysis of cross-domain relations. J. Appl. Psychol. 92:57. doi: 10.1037/0021-9010.92.1.57
Gariepy, G., Honkaniemi, H., and Quesnel-Vallee, A. (2016). Social support and protection from depression: systematic review of current findings in Western countries. Br. J. Psychiatry 209, 284–293.
Ghafari, R., Mirghafourvand, M., Rouhi, M., and Osouli Tabrizi, S. (2021). Mental health and its relationship with social support in Iranian students during the COVID-19 pandemic. BMC Psychol. 9:81. doi: 10.1186/s40359-021-00589-4
Gijón Puerta, J., Galván Malagón, M. C., Khaled Gijón, M., and Lizarte Simón, E. J. (2022). Levels of stress, anxiety, and depression in university students from Spain and Costa Rica during periods of confinement and virtual learning. Educ. Sci. 12:660. doi: 10.3390/educsci12100660
Green, Z. A., Çiçek, I., and Yıldırım, M. (2024). The relationship between social support and uncertainty of COVID-19: The mediating roles of resilience and academic self-efficacy. Psihologija [Epub ahead of print]. doi: 10.2298/PSI220903002G
Grey, I., Arora, T., Thomas, J., Saneh, A., Tohme, P., and Abi-Habib, R. (2020). The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 293:113452.
Gülaçtı, F. (2010). The effect of perceived social support on subjective well-being. Procedia Soc. Behav. Sci. 2, 3844–3849.
Hanson, S., and Jones, A. (2015). Is there evidence that walking groups have health benefits? A systematic review and meta-analysis. Br. J. Sports Med. 49, 710–715.
Huang, Y., and Zhao, N. (2021). Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychol. Health Med. 26, 23–34.
Hüfner, K., Tymoszuk, P., Ausserhofer, D., Sahanic, S., Pizzini, A., Rass, V., et al. (2022). Who is at risk of poor mental health following coronavirus disease-19 outpatient management? Front. Med. 9:792881. doi: 10.3389/fmed.2022.792881
Kessler, R. C., and McLeod, J. D. (1985). Social support and mental health in community samples. London: Academic Press.
Klaiber, P., Wen, J. H., DeLongis, A., and Sin, N. L. (2021). The ups and downs of daily life during COVID-19: Age differences in affect, stress, and positive events. J. Gerontol. Series B 76, e30–e37. doi: 10.1093/geronb/gbaa096
Konstantopoulou, G., Iliou, T., Karaivazoglou, K., Iconomou, G., Assimakopoulos, K., and Alexopoulos, P. (2020). Associations between (sub) clinical stress- and anxiety symptoms in mentally healthy individuals and in major depression: a cross-sectional clinical study. BMC Psychiatry 20:428. doi: 10.1186/s12888-020-02836-1
Kun, A. (2013). “Health, stress, well-being and positive affectivity,” in Psychology, eds J. Soos and I. Takacs (Budapest: BME GTK).
Lades, L. K., Laffan, K., Daly, M., and Delaney, L. (2020). Daily emotional well-being during the COVID-19 pandemic. Br. J. Health Psychol. 25, 902–911.
Lazarus, R. S., and Folkman, S. (1984). Stress, appraisal, and coping. Berlin: Springer publishing company.
Litwin, H., and Levinsky, M. (2021). Social networks and mental health change in older adults after the Covid-19 outbreak. Aging Mental Health 26, 1–6. doi: 10.1080/13607863.2021.1902468
Liu, C., Huang, N., Fu, M., Zhang, H., Feng, X. L., and Guo, J. (2021). Relationship between risk perception, social support, and mental health among general Chinese population during the COVID-19 pandemic. Risk Manage. Healthcare Policy 14, 1843–1853. doi: 10.2147/RMHP.S302521
Liu, R. T., and Alloy, L. B. (2010). Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clin. Psychol. Rev. 30, 582–593. doi: 10.1016/j.cpr.2010.04.010
Lovibond, S. H., and Lovibond, P. F. (1995). Depression Anxiety Stress Scales (DASS–21, DASS–42) [Database record]. Washington, DC: APA PsycTests, doi: 10.1037/t01004-000
Luo, M., Guo, L., Yu, M., and Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and public–A systematic review and meta-analysis. Psychiatry Res. 291:113190. doi: 10.1016/j.psychres.2020.113190
Mansueto, G., Lopes, F. L., Grassi, L., and Cosci, F. (2021). Impact of COVID-19 outbreak on Italian healthcare workers versus general population: Results from an online survey. Clin. Psychol. Psychother. 28, 1334–1345. doi: 10.1002/cpp.2644
Mansueto, G., Palmieri, S., Marino, C., Caselli, G., Sassaroli, S., Ruggiero, G. M., et al. (2022). The Italian COVID-19 Anxiety Syndrome Scale: Investigation of the COVID-19 anxiety syndrome and its association with psychological symptoms in an Italian population. Clin. Psychol. Psychother. 29, 1972–1990. doi: 10.1002/cpp.2767
McLean, L., Gaul, D., and Penco, R. (2023). Perceived Social Support and Stress: A study of 1st year students in Ireland. Int. J. Mental Health Addict. [Epub ahead of print]. doi: 10.1007/s11469-021-00710-z
Mitchell, A. M., Crane, P. A., and Kim, Y. (2008). Perceived stress in survivors of suicide: psychometric properties of the Perceived Stress Scale. Res. Nurs. Health 31, 576–585. doi: 10.1002/nur.20284
Mohd, T. A. M. T., Yunus, R. M., Hairi, F., Hairi, N. N., and Choo, W. Y. (2019). Social support and depression among community dwelling older adults in Asia: A systematic review. BMJ Open 9, e026667. doi: 10.1136/bmjopen-2018-026667
Montano, R. L. T., and Acebes, K. M. L. (2020). Covid stress predicts depression, anxiety and stress symptoms of Filipino respondents. Int. J. Res. Bus. Soc. Sci. 9, 78–103.
Neese, A. L., Pittman, L. D., and Hunemorder, R. (2013). Depressive symptoms and somatic complaints among Zambian adolescents: Associations with stress and coping. J. Res. Adolesc. 23, 118–127. doi: 10.1111/j.15327795.2012.00834.x
Özer, O., Özkan, O., Budak, F., and Özmen, S. (2021). Does social support affect perceived stress? A research during the COVID-19 pandemic in Turkey. J. Hum. Behav. Soc. Environ. 31, 134–144.
Özmete, E., and Pak, M. (2020). The relationship between anxiety levels and perceived social support during the pandemic of COVID-19 in Turkey. Soc. Work Public Health 35, 603–616.
Pieh, C., Budimir, S., and Probst, T. (2020). The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychos. Res. 136:110186. doi: 10.1016/j.jpsychores.2020.110186
Priego-Cubero, E., Orgeta, V., López-Martínez, C., and del-Pino-Casado, R. (2023). The relationship between social support and anxiety symptoms in informal carers: A systematic review and meta-Aaalysis.”. J. Clin. Med 12:1244.
Puertas-Gonzalez, J. A., Marino-Narvaez, C., Romero-Gonzalez, B., Vilar-Lopez, R., and Peralta Ramirez, M. I. (2023). Resilience, stress, and anxiety in pregnancy before and throughout the pandemic: a structural equation modelling approach. Curr. Psychol. 42, 22013–22023. doi: 10.1007/s12144-022-03305-6
Qi, M., Zhou, S. J., Guo, Z. C., Zhang, L. G., Min, H. J., Li, X. M., et al. (2020). The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. J. Adolesc. Health 30:1e5.
Rackoff, G. N., and Newman, M. G. (2020). Reduced positive affect on days with stress exposure predicts depression, anxiety disorders, and low trait positive affect 7 years later. J. Abnorm. Psychol. 129, 799–809. doi: 10.1037/abn0000639
Reed, J., and Ones, D. S. (2006). The effect of acute aerobic exercise on positive activated affect: A meta-analysis. Psychol. Sport and Exerc. 7, 477–514.
Reger, M. A., Stanley, I. H., and Joiner, T. E. (2020). Suicide mortality and coronavirus disease 2019—a perfect storm. JAMA Psychiatry 77, 1093–1094. doi: 10.1001/jamapsychiatry.2020.1060
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., et al. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and metanalysis. Globaliz. Health 16, 1–11. doi: 10.1186/s12992-020-00589-w
Sarason, B. R., Shearin, E. N., Pierce, G. R., and Sarason, I. G. (1987). Interrelations of social support measures: Theoretical and practical implications. J. Pers. Soc. Psychol. 52:813.
Simon, P. D., and Bernardo, A. B. I. (2022). Longitudinal measurement invariance of the Depression Anxiety Stress Scale (DASS-21) in Filipino adolescents. Trans. NAST PHL 44:2557. doi: 10.57043/transnastphl.2022.2557
Skipworth, K. (2011). Relationship between perceived stress and depression in college students. Master’s thesis, Arizona: Arizona State University.
Stieger, S., Lewetz, D., and Swami, V. (2021). Emotional well-being under conditions of lockdown: An experience sampling study in Austria during the COVID-19 pandemic. J. Happ. Stud. 1–18. doi: 10.1007/s10902-020-00337-2
Tee, M. L., Tee, C. A., Anlacan, J. P., Aligam, K. J. G., Reyes, P. W. C., Kuruchittham, V., et al. (2020). Psychological impact of COVID-19 pandemic in the Philippines. J. Affect. Disord. 277, 379–391.
Thoits, P. A. (1985). Social support and psychological well-being: Theoretical possibilities. In Social support: Theory, research and applications. Dordrecht: Springer Netherlands, 51–72.
Wang, D., Zhu, F., Xi, S., Niu, L., Tebes, J. K., Xiao, S., et al. (2021). Psychometric properties of the Multidimensional Scale of Perceived Social Support (MSPSS) among family caregivers of people with schizophrenia in China. Psychol. Res. Behav. Manage. 14, 1201–1209. doi: 10.2147/PRBM.S320126
Wang, J., Mann, F., Lloyd-Evans, B., Ma, R., and Johnson, S. (2018). Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry 18:5. doi: 10.1186/s12888-018-1736-5
Watson, D., Clark, L. A., and Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. J. Pers. Soc. Psychol. 54:1063.
Watson, R. J., Grossman, A. H., and Russell, S. T. (2019). Sources of social support and mental health among LGB youth. Youth Soc. 51, 30–48.
Wethington, E., and Kessler, R. C. (1986). Perceived support, received support, and adjustment to stressful life events. J. Health Soc. Behav. 27, 78–89.
Wheaton, B., and Montazer, S. (2017). “Studying stress in the twenty-first century: An update of stress concepts and research,” in A handbook for the study of mental health: Social contexts, theories, and systems, eds T. L. Scheid and T. N. Brown (London: University of the Aegean). doi: 10.1111/eci.13748
Wills, T. A. (1991). “Social support and interpersonal relationships,” in Prosocial behavior, ed. M. S. Clark (London: Sage Publications, Inc), 265–289.
Xiao, H., Zhang, Y., Kong, D., Li, S., and Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 26, e923549–e923541. doi: 10.12659/MSM.923549
Yang, H., and Ma, J. (2020). How an epidemic outbreak impacts happiness: Factors that worsen (vs. protect) emotional well-being during the coronavirus pandemic. Psychiatry Res. 289:113045. doi: 10.1016/j.psychres.2020.113045
Yildirim, M., and Aziz, I. A. (2023). Turkish validation of the Psy-Flex Scale and its association with resilience and social support. Environ. Soc. Psychol. 8:263.
Yıldırım, M., and Green, Z. A. (2023). Social support and resilience mediate the relationship of stress with satisfaction with life and flourishing of youth. Br. J. Guid. Counsel. [Epub ahead of print]. doi: 10.1080/03069885.2023.2172551
Yıldırım, M., Turan, M., Albeladi, N., Crescenzo, P., Rizzo, A., Nucera, G., et al. (2023). Resilience and perceived social support as predictors of emotional well-being. J. Health Soc. Sci. 8, 59–75. doi: 10.19204/2023/rsln5
Zacher, H., and Rudolph, C. W. (2021). Individual differences and changes in subjective wellbeing during the early stages of the COVID-19 pandemic. Am. Psychol. 76:50. doi: 10.1037/amp0000702
Zhang, B., Yan, X., Zhao, F., and Yuan, F. (2014). The relationship between perceived stress and adolescent depression: The roles of social support and gender. Soc. Indic. Res. 123, 501–518. doi: 10.1007/s11205-014-0739-y
Zhang, X., Zou, R., Liao, X. X., Bernardo, A. B. I., Du, H., Wang, Z., et al. (2021). Perceived stress, hope, and health outcomes among medical staff in China during the COVID-19 pandemic. Front. Psychiatry 11:588008. doi: 10.3389/fpsyt.2020.588008
Keywords: social support, perceived stress, mental health, and COVID-19 pandemic, mediation analysis
Citation: Acoba EF (2024) Social support and mental health: the mediating role of perceived stress. Front. Psychol. 15:1330720. doi: 10.3389/fpsyg.2024.1330720
Received: 31 October 2023; Accepted: 31 January 2024;
Published: 21 February 2024.
Edited by:
Murat Yildirim, Ağrı İbrahim Çeçen University, TürkiyeReviewed by:
Giovanni Mansueto, University of Florence, ItalySagrario Gomez-Cantarino, University of Castilla La Mancha, Spain
Copyright © 2024 Acoba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Evelyn F. Acoba, YWNvYmFldmVseW5AZ21haWwuY29t
 Evelyn F. Acoba
Evelyn F. Acoba