- 1Department of Social and Behavioural Medicine, Faculty of Medicine, Pavol Jozef (PJ) Safarik University in Kosice, Kosice, Slovakia
- 2Department of Organisation and Management of Pharmacy, Faculty of Pharmacy, Comenius University in Bratislava, Bratislava, Slovakia
- 3Biomedical Research Centre of the Slovak Academy of Sciences, Bratislava, Slovakia
- 4Institute for Prevention and Intervention, St. Elisabeth University of Health and Social Work, Bratislava, Slovakia
- 5Faculty of Nursing and Medical Professional Studies, Slovak Health University, Bratislava, Slovakia
Introduction: Increasing overweight and obesity rates represent one of the global public health challenges. COM-B is a theoretical model used to identify areas to target to achieve behavior change. It identifies three factors that are needed for any behavior to occur: capability, opportunity, and motivation. We aimed to assess the potential facilitators and barriers to behavior change in weight management using the COM-B.
Methods: The study included 139 people with overweight and obesity (mean age 48.81 ± 14.49 years; 64.5% female; body mass index 32.64 ± 6.51 kg/m2; waist-to-height ratio 0.62 ± 0.10) from primary care settings. All participants completed the Brief Measure of Behavior Change (COM-B), the General Self-Efficacy Scale (GSE), the Rosenberg Self-esteem Scale (RSE), and the Overall Evaluation of Health (OEH). Multiple linear regression was performed to analyse the data.
Results: The associations between sociodemographic and clinical variables and COM-B domains attenuated or were no longer significant when psychological resources were added to the regression models. Self-efficacy was identified as a stronger facilitator of health behavior change (p < 0.001) when compared to self-esteem (p < 0.05). No associations between automatic motivation and psychological resources were identified, however. Automatic motivation was found to be associated with higher age, being in a relationship, and better health.
Discussion: Behavioral interventions for weight management should specifically target different components of COM-B. Self-efficacy and self-esteem may play a significant role in individual capabilities, opportunities, and reflective motivation and should be included in tailored public health interventions. Health programs targeting younger and single people, and people with chronic conditions may help to promote sustainable behavior change.
Introduction
Obesity/overweight represents one of the global health problems in the 21st century. Based on the latest estimates, obesity affects nearly 25% of European adults, and combined overweight and obesity affects nearly 60% of all adults in Europe (World Obesity Federation, 2021; WHO Regional Office for Europe, 2022). By 2025 the prevalence of obesity in some EU countries may reach 30–43% (Pineda et al., 2018). Obesity/overweight rates have tripled in the past 30 years and continue to increase globally which is associated with a concomitant rise in health care and economic costs (Anekwe et al., 2020; WHO, 2021). Moreover, many obesity-related comorbidities lead to a decreased life expectancy (Anekwe et al., 2020).
Behavioral risk factors such as poor nutritional habits and physical inactivity cause 50% of all deaths in Slovakia, which is significantly above the EU average of 39% (OECD, 2019). Obesity rates in Slovakia are higher than the EU average (OECD, 2023), and obesity rates by education and income in Slovakia were also found to be larger than in the rest of the EU (OECD, 2019, 2021, 2023). Nevertheless, obesity as the second leading cause of preventable death does not receive prioritization in healthcare and public health interventions according to its prevalence and impact (De Lorenzo et al., 2020; World Obesity Federation, 2021). Thus, preventive strategies and effective weight management remain the most important challenges in public health (World Obesity Federation, 2021).
Behavioral insights currently represent one of the WHO/Europe flagship initiatives to improve the population's health (WHO, 2022). Current studies show that although caloric restriction-based interventions are effective in promoting weight reduction, long-term adherence to behavioral change should be supported (Hassapidou et al., 2023). Understanding human behavior can offer powerful insights to support health-protective changes in people's daily lives (WHO, 2022). Health behavior change interventions are crucial in obesity management, due to their focus on individuals' ability to self-regulate their health (Teixeira and Marques, 2017). Michie et al. (2014) proposed the “Capability, Opportunity, Motivation and Behaviour” (COM-B) as a theoretical model to guide understanding of behavior in different contexts, identify areas to target in order to enable behavior change and provide a basis for designing behavioral interventions in health management. Origins of COM-B can be found in health behavior models such as the theory of planned behavior, self-determination theory, transtheoretical model, or the health action process approach while meta-analyses show that these health behavior models can explain up to 37% of the variance in human behavior (Keyworth et al., 2020).
COM-B model defines behavior as the result of the interaction between the following components: physical and psychological capability (C), social and physical opportunity (O), and automatic and reflective motivation (M) (West and Michie, 2020).
It seems that health literacy alone is rarely sufficient to change an individual's behavior. Rather, psychological, social, and environmental factors, together with personal motivation (Kelly and Barker, 2016), or the effects of psychological factors on self-regulatory processes for overcoming lifestyle barriers should be considered (Annesi, 2020).
Thus, the understanding of COM-B domains allows for a more organized and efficient approach when considering barriers to health change in counseling people with overweight/obesity and how this knowledge can be applied in a healthcare setting (Sooknarine-Rajpatty et al., 2020). Application of the COM-B model considering core aspects of patient engagement is crucial to ensure the real impact of interventional programs can be achieved (Zheng et al., 2022). COM-B domains were also found to be predictive in long-term health-related behavior (Armitage and Munro, 2023) with current studies showing the explanatory potential and efficiency of COM-B components in the management of physical activity (Shoneye et al., 2020; Brierley et al., 2021; Kandel et al., 2021; Willmott et al., 2021; Niven et al., 2022; Gu et al., 2023; Huynh et al., 2023), and nutrition (Chater et al., 2020; Crowley et al., 2020; Shoneye et al., 2020; Kandel et al., 2021; Willmott et al., 2021) in the general population and people with overweight/obesity.
The study by Johnson et al. (2020) showed that self-efficacy and the COM-B domains are the key factors to allow personal tailoring of intervention techniques. Perceived self-efficacy facilitates goal-setting, effort investment, persistence in facing barriers, and recovery from setbacks (Schwarzer and Jerusalem, 1995). Psychological resources such as self-efficacy or self-esteem may also play a role in the process of making lifestyle changes (Wang and Veugelers, 2008; Dahlberg et al., 2022) and were identified as ideal targets for the maintenance of health behavior in high-income countries (Silveira et al., 2021). Low self-efficacy was found to be associated with sub-optimal self-care (Herber et al., 2017), and lower motivation and commitment to goals (Bandura, 1998), while low self-esteem was found to be associated with an inactive lifestyle (Wang and Veugelers, 2008). However, some current studies assessed the role of self-esteem and self-efficacy in weight management with inconclusive results (Olander et al., 2013; Jebeile et al., 2021; Björkman et al., 2022).
Health policies, services, and communication are frequently planned and administered without a thorough understanding of the drivers and barriers people face (WHO, 2022). Research on weight management omits factors that may affect human behavior (Ellis et al., 2019) and recent interventions focus mainly on dietary intake and a sedentary lifestyle although their success has been limited (Spinosa et al., 2019). Despite the overarching framework of the COM-B model to guide intervention development, there is a lack of quantitative studies that evaluate the mechanisms of action in COM-B (e.g., Keyworth et al., 2020) and its use and understanding in weight management is still scarce. Although information exists regarding specific behaviors associated with efficient weight management, far less is known about the role of psychological factors in determining if these health behaviors will be performed and maintained (Coms ´ a et al., 2023). Thus, our study aimed to assess the role of potential facilitators and barriers to weight-related behavior change using the COM-B model to identify and reflect on areas to target to achieve efficient weight management. We aimed to assess the association between sociodemographic variables, clinical variables, self-esteem, self-efficacy and COM-B domains in people with overweight and obesity.
Materials and methods
Participants
We included 139 people with overweight and obesity [64.5% females; 35.5% males; mean age 48.81 ± 14.49 years; body mass index (BMI) 32.64 ± 6.51 kg/m2; waist-to-height ratio (WHtR) 0.62 ± 0.10]. Participants were recruited by general practitioners (GPs) from outpatient clinical settings that covered all regions of Slovakia. The study sample consisted of consecutive patients who visited their GPs for routine medical examinations, preventive check-ups, or prescriptions of medication. The participants were included based on overall overweight and obesity (using BMI) and central obesity (using WHtR) scores. Exclusion criteria were a BMI of ≤ 24.99, and a WHtR of ≤ 0.49 which is not associated with central obesity or health risks (Ashwell and Gibson, 2016), the inability to speak the Slovak language, and being < 18 years of age. Additionally, people with major comorbidities such as cognitive impairment (e.g., due to dementia or stroke), current major psychiatric diagnoses (e.g., psychotic disorders, major depression), or diagnosis of terminal disease were also excluded by GP.
Procedure
The study design was cross-sectional. Data collection consisted of self-reported questionnaires and measurements of patient height, weight, and waist circumference. Patients filled in the questionnaires at their own pace at home. Questionnaires were translated from the English language to the Slovak language following the standard procedure. First, two independent bilingual translators, one also an expert in psychology translated the questionnaires. Then, a forward-backwards translation was conducted. Differences between the original and the back translation were discussed by the research team in order to optimize the translation (International Test Commission, 2017). Informed consent was obtained from all individual participants included in the study. Participation in the study was entirely voluntary with no incentives offered for participation in the research. The study was approved by the Ethics Committee of Comenius University in Bratislava (approval no. EK 02/2020). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Data were collected between October 2020 and August 2021.
Measures
Self-efficacy
The 10-item General Self-efficacy Scale (GSE) reflects an optimistic self-belief (Schwarzer and Jerusalem, 1995) that one can perform novel, difficult tasks, or successfully cope with adversity in various domains of human functioning. The score ranges from 10 to 40 points and a higher score implies a higher level of internal-stable attributions of success (Schwarzer and Jerusalem, 1995). Cronbach's alpha in our sample was 0.93.
Self-esteem
The level of self-esteem was assessed using the Rosenberg Self-esteem Scale (RSE). RSE is a 10-item scale anchored at 4 points indicating a level of self-esteem. The total score ranges from 10 to 40 points, with a higher score indicating higher levels of self-esteem (Rosenberg, 1965). Cronbach's alpha in our sample was 0.85.
Capabilities, opportunities, and motivations
To assess barriers and facilitators in health-behavior change we used the Brief measure of capabilities, opportunities, and motivations (COM-B) which represents a valid questionnaire based on the COM-B model (Keyworth et al., 2020) that is used to estimate health-related behavior (e.g., Niven et al., 2022; Armitage et al., 2023). The COM-B model proposes that for someone to engage in a particular behavior at a given moment must have the physical and psychological capability, the social and physical opportunity to perform the behavior and, in addition, want or need to perform the behavior more than any other competing behaviors. Motivation includes all brain processes that guide behavior and covers basic drives and automatic processes such as habits, or impulses as well as reflective processes such as plans, intentions, or choices (West and Michie, 2020). The measure comprises six items designed to assess physical capability, psychological capability, physical opportunity, social opportunity, reflective motivation, and automatic motivation. Participants were asked to rate their ability and willingness to change their health-related behavior on an eleven-point scale (0 strongly disagree to 10 strongly agree). Health-related behavior change was defined as healthy nutrition and physical activity. Cronbach's alpha in our sample was 0.86.
Self-rated health
To assess the self-rated health the Overall Evaluation of Health (OEH) instrument was used. The OEH is a 100 mm visual analog scale on which the participant marks a line at the point that most closely reflects his/her self-rated health at present. The OEH score ranges from 0 to 100, with a higher score indicating better self-rated health (EURIDISS, 1990).
Sociodemographic and clinical variables
Sociodemographic data (age, sex, education, relationship status, household income) were collected using a questionnaire. Household income was categorized as low (lower than the “minimum wage”, i.e., under the poverty line), middle (at least “minimum wage” but less than double minimum wage), and high (twice the “minimum wage” and higher) income.1 Additional health information on clinical data such as the presence of chronic diseases was obtained from patients using a questionnaire. Data on weight, height, and waist circumference were assessed by healthcare professionals. The measures were taken barefoot with indoor clothes using an electronic scale for body weight, tape, and a wall-mount stadiometer. We calculated BMI in kg/m2 using weight and height measures. The waist-to-height ratio (WHtR) was used to assess central obesity. The WHtR of each participant was obtained by dividing waist circumference by height.
Statistical analyses
Statistical analyses consisted of descriptive analyses of all key variables under study, followed by linear regression analysis (enter method) to assess the explained variance of COM-B domains. The order of variables included in the model was as follows: (1) age, sex, (2) education, income, relationship status, (3) presence of chronic disease, self-rated health, WHtR, (4) self-esteem, and (5) self-efficacy. Power analysis revealed that the statistical power for multivariate analysis exceeds 88% at α = 0.05 and medium effect size. The statistical power for bivariate analysis was 0.98 at α = 0.05 and medium effect size (Faul et al., 2009). A p-value of < 0.05 was considered to be statistically significant. All analyses were performed using the Statistical Package for the Social Sciences (IBM SPSS 26). Multicollinearity was assessed using the variance inflation factor (VIF < 2.5). A p-value of < 0.05 was considered statistically significant.
Results
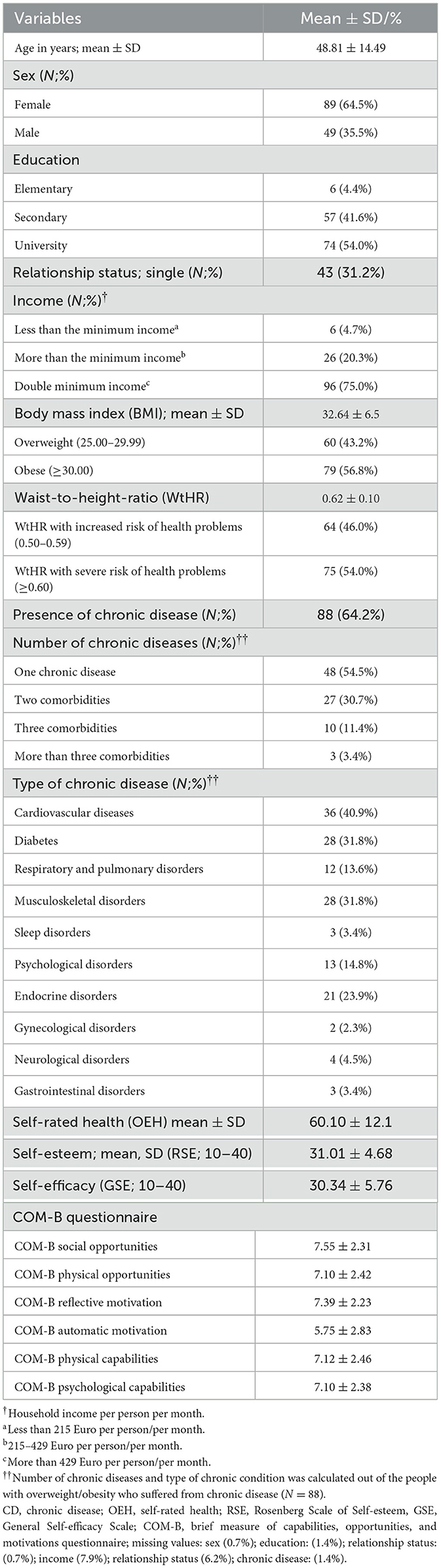
The basic description of the sample is shown in Table 1 (N = 139). The participants averaged 48.81 ± 14.49 years of age with the majority of females (64.5%) with a mean BMI of 32.64 ± 6.5 and WHtR of 0.62 ± 0.10. A total of 56.8% of participants had overall obesity and 54% were at severe risk of weight-related health problems. A total of 64.2% of participants suffered from chronic conditions with cardiovascular disease being the most prevalent (40.9%). The mean level of automatic motivation (5.75 ± 2.83) was lower than in other assessed COM-B domains.
Regression analyses showed that self-efficacy was a statistically significant contributor to overall explained variance in all final models except for the Automatic Motivation model. In this model, having a partner (β = 0.18; p < 0.05), and the presence of chronic disease (β = 0.24; p < 0.05), were significantly contributing to the overall explained variance. Higher age yielded a significant contribution also in the final model of Automatic Motivation (β = 0.21; p < 0.05) and Psychological Capabilities (β = 0.25; p < 0.01). Sex retained its significant contribution through each step of the analyses in the Physical Capabilities model (β = −0.18; p < 0.05 in the final iteration). Self-efficacy was most strongly associated with reflective motivation (β = 0.52; p < 0.001), followed by psychological capability (β = 0.44; p < 0.001) and physical capability (β = 0.43; p < 0.001). The associations between self-esteem, social opportunities, reflective motivation and physical capabilities were weaker but still significant (p < 0.05). Social opportunities and reflective motivation domains were associated with psychological factors, while sociodemographic and clinical variables were not significant. No significant associations between income, education, waist-to-height ratio and COM-B domains were identified. Detailed results of regression analyses are shown in Table 2.
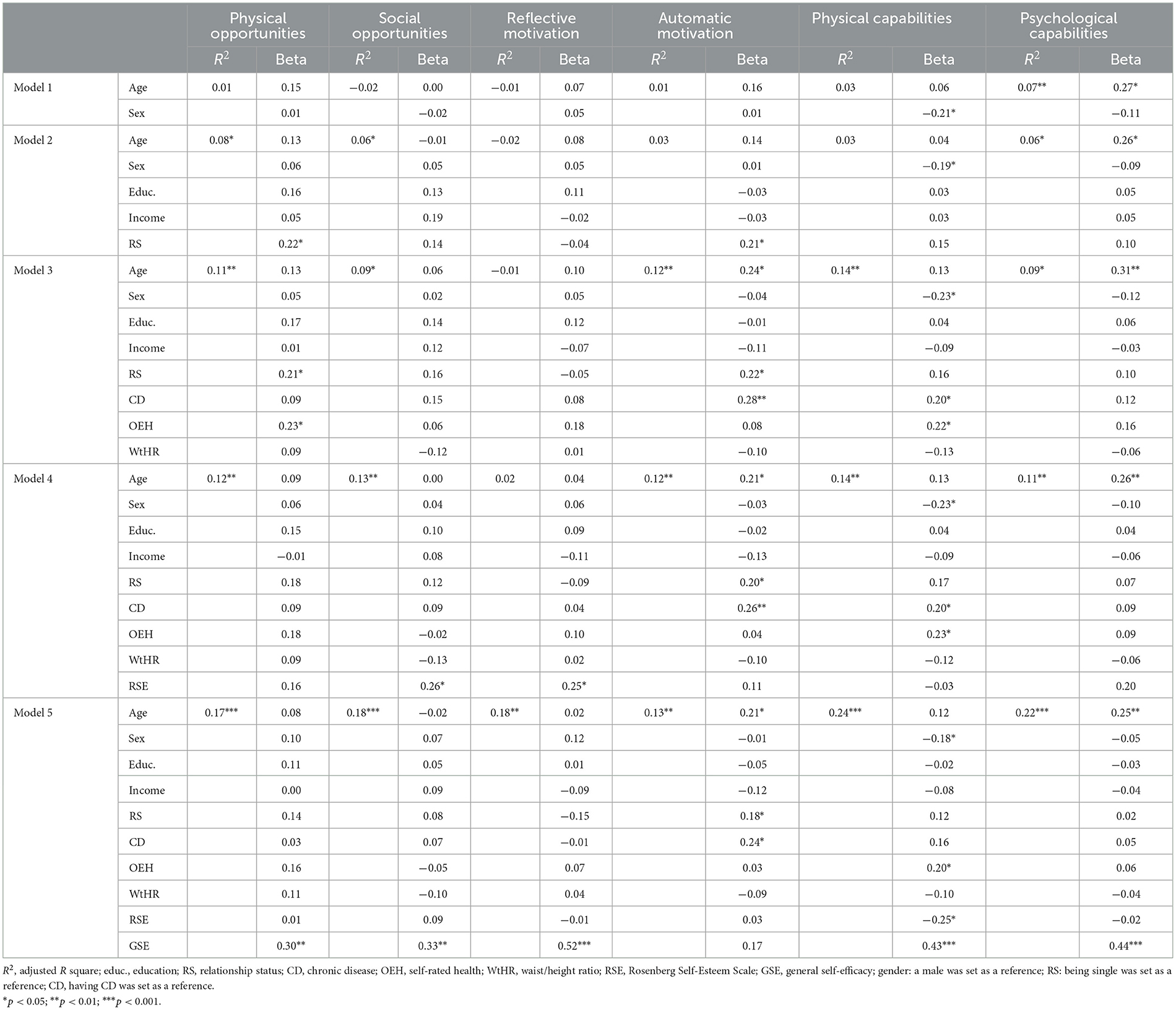
Table 2. Regression analyses of six components of the COM-B regressed on sociodemographic, clinical, and psychological variables.
Discussion
Physical capabilities, psychological capabilities, and automatic motivation domains were associated with higher age, female sex, having a partner, absence of chronic diseases, and better self-rated health. However, these associations between sociodemographic and clinical variables and COM-B domains attenuated or were no longer significant when psychological resources were added to the regression models. Self-efficacy was identified as a stronger facilitator of health behavior change when compared to self-esteem. Automatic motivation was found to be associated with higher age, being in a relationship, and better health. No association between automatic motivation and psychological resources was identified. Total explained variances in the final models varied from 13 to 24%.
Our study identified a significant association between all COM-B domains, except automatic motivation. These findings are in line with previous studies showing a significant association between self-efficacy, action orientation (Schwarzer and Jerusalem, 1995), reflective action control (Rothman et al., 2009), and motivation (Bandura, 1998). Furthermore, it is assumed, that as self-efficacy reflects beliefs about capabilities it may overlap with reflective motivation (e.g., Whittal et al., 2021). Previous research also identified self-efficacy as a mechanism of action by which interventions “work” in promoting behavior change (Werner et al., 2020). Therefore, the premise that self-efficacy may increase individuals' capabilities, opportunities, and reflective motivation can be used to develop intervention strategies.
We further found that the level of automatic motivation was the lowest in our sample when compared to other COM-B domains. Automatic motivation is needed to maintain health behavior change in the long term as it reflects habit strength (Gardner et al., 2022). However, previous studies also identified challenges in translating initial behavioral changes into long-standing habits (Rothman et al., 2009; Dunton et al., 2021). Thus, we may assume that people with overweight and obesity are more strongly motivated to health behavior change by conscious decision-making while their habit strength is weaker. Making behavior habitual, such that people automatically act in associated contexts due to learned context-response associations, offers a mechanism for maintaining new, desirable behaviors even when conscious motivation wanes (Gardner et al., 2022). It is therefore crucial to identify intervention strategies that would help to increase automatic motivation in people with overweight and obesity.
Success in long-term weight management depends partly on psychological factors (Oikarinen et al., 2023) and the importance of self-efficacy in predicting health intention and health behavior, is well-recognized (Sheeran et al., 2016; Zhang et al., 2019). We found no association between automatic motivation and intervention-prone psychological resources measured as self-esteem and self-efficacy, however. Previous studies showed that low self-efficacy was found to be associated with low motivation and lower commitment to goals (Bandura, 1998), low automaticity including poor intentional habit building (Stojanovic et al., 2021), and multiple concomitant eating behaviors that prevent successful weight management (Oikarinen et al., 2023). However, the lack of the association between self-efficacy and automatic motivation identified in our study is in line with previous findings that self-efficacy may be an important, but not sufficient condition for initiating long-lasting behavior change (e.g., Rothman et al., 2009). Moreover, people may overestimate their capabilities and only realize the difficulty in implementing lasting behavior change when it comes to real activity, also known as implementation dip in self-efficacy (Bandura and Locke, 2003).
Based on the results of our study it also seems that automatic motivation is lower in younger people with overweight/obesity. Older age may offer sufficient time to prevent unhealthy aging and to establish new daily routines to increase health behavior (Schoufour et al., 2021). As our data were collected during the COVID-19 pandemic we may also assume that older people might have been more worried about COVID-related complications (Barber and Kim, 2021) and thus been more strongly motivated to develop habitual health-related behaviors. However, current studies showed the opposite direction and identified younger people as more prone to lifestyle change during the pandemic (Barber and Kim, 2021; Oliveira et al., 2022). Thus, future studies are needed to shed more on the role of age in habitual change.
Based on our findings it also seems that in people affected by overweight and obesity, the presence of a chronic disease may play a more significant role in the low level of experienced automatic motivation, compared to psychological factors. The strength of automatic (e.g., habit-based) mechanisms was identified as a strong predictor of behavior change in people with chronic conditions and an intervention target for chronic illness self-management; while assessing it in practice settings may effectively detect poor to existing treatment and lifestyle regimens (Phillips et al., 2016). Diagnosis of a serious health condition should lead to the recognition of a problem, which represents an initial stage of change (Prochaska et al., 2005). Although we may assume that chronic disease may be a trigger for habitual health-related behavior change, previous studies found little evidence that severe chronic diseases such as cancer, diabetes, lung disease, or heart disease (Newsom et al., 2012; Williams et al., 2013) motivates health-protective changes and concluded that the vast majority of people newly diagnosed with a chronic condition do not adopt healthier behaviors (Newsom et al., 2012).
We also identified a significant association between automatic motivation and having a partner. The same was true for the association between relationship status and physical opportunities domain. No significant association between relationship status and psychological or physical capabilities, or the level of experienced reflective motivation, was identified. Thus, we may assume that having a partner seems to be positively associated with instrumental support—including physical opportunity (e.g., fewer time constraints, accessible childcare) (e.g., Ellis et al., 2019) and automatization of these processes in weight management, while emotional support of a partner seems to be negligible. It should be considered that the majority of our sample were females who globally do 75–83% of household chores and child or elderly care (The World Bank, 2018; Perez, 2019; Rubiano Matulevich and Viollaz, 2019) and thus may report having less leisure time when compared to males (Perez, 2019; Rubiano Matulevich and Viollaz, 2019). As the data were collected during the COVID-19 pandemic we may also assume that the increase in the gender gap in leisure time might have been highlighted (Yerkes et al., 2020; Clark et al., 2021) and people, especially women might have lacked opportunities for implementing sustainable weight management strategies with lack of instrumental support from the partner.
Based on our findings personalized interventions focusing on addressing poor health, younger people, and people without spouse/partner may help to promote behavior change via the automatization of motivation processes among adults with overweight and obesity. Our study suggests that intensive efforts are needed to maintain lifestyle improvements in this population.
We further found a lack of physical capabilities to make lifestyle changes to be associated with the presence of chronic disease, poor self-rated health, and low self-efficacy. We also found that the female sex was associated with lower physical capabilities to make lifestyle changes. These findings may be explained by poorer physical functioning reported by women compared to men identified in previous studies (Von Bonsdorff et al., 2011; Sialino et al., 2022), as well as barriers such as aspects of the built environment that may create gender gap in activity (Althoff et al., 2017) and decrease the functional capability of females (Satariano and Maus, 2017).
Surprisingly, an association between low self-esteem and higher physical capabilities reappeared when self-efficacy was added to the final model. This result may be explained by differences in sex, as physical capabilities are the only domain of the COM-B model that shows a significant contribution of sex to the overall explained variance in all stages of regression analyses. Adding self-efficacy to the model may point toward a closer association between self-efficacy and self-esteem in males compared to females, especially in the physical capabilities domain. These results need further investigation as a lower proportion of male participants may statistically impair these particular findings.
Better psychological capabilities were significantly associated with older age. Thus, it seems that lower age undermines psychological capabilities in people with overweight and obesity. However, this association was no longer significant when self-efficacy was added to the model. Self-efficacy was strongly associated also with psychological capabilities, while no association between self-esteem and psychological capabilities was observed.
No significant associations between education, income, waist-to-height ratio and COM-B domains were identified. As the difference in obesity rates by education and income in Slovakia are larger than in the rest of the EU (OECD, 2019, 2021), and the prevalence of behavioral risk factors was found to be higher among people with the lowest levels of education and income (OECD, 2023) more studies are needed to shed more light on the role of sociodemographic variables in overweight and obesity.
Strengths and limitations
To our best knowledge, this is one of the first studies providing important insight into the factors enabling or inhibiting health behavior change to increase physical activity and healthy nutrition amongst adults with overweight and obesity using the COM-B model. To identify people with overweight and obesity, we used Body Mass Index (BMI) as one of the most widespread measures (e.g., Khanna et al., 2022) used in population studies (Garvey and Mechanick, 2020). However, it needs to be considered that the use of the BMI falls short in considering differences in body composition and the contribution of body fat to overall body weight (Pasco et al., 2014) and does not reflect differences in body composition according to the individual's age, sex (Gallagher et al., 1996), ethnicity-specific cutoffs (Caleyachetty et al., 2021), or obesity-related complications at the individual level (Garvey and Mechanick, 2020). Thus, we used also the WtHR of ≥0.5 as the main inclusion criterion for our study which led to the exclusion of three participants with BMI ≥ 25.0. Central obesity was also used as a control variable in multiple linear regression due to the collinearity between the waist-to-height ratio and BMI.
A brief measure of the COM-B questionnaire was previously used in the current studies that addressed health-related behavior (e.g., Niven et al., 2022; Armitage et al., 2023). The assessment of automatic motivation measured by COM-B is based on the Self-Report Habit Index, the most commonly used habit measure in health psychology, which measures behavior XY as “something that a person does automatically”. As the Self-Report Habit Index was found to be loaded on the same factor as did an instigation variant, whereas an execution variant was found to be loaded on a separate factor, there is also the possibility that we addressed habitual instigation, rather than its execution (Gardner et al., 2019). Thus, future research should be aimed at better understanding the contribution of automatic motivation to behavior frequency. As data were collected during the COVID-19 pandemic there is a possibility that our findings could be influenced by this global crisis and adopted measures. For example, physical opportunities, as well as social opportunities, might have been significantly limited by restrictions such as social distancing or lack of open public places (Porter et al., 2022). Although most of the current studies describe habitual processes including automatic motivation as a predictor of behavior change, the study by Spence et al. (2021) showed that physical opportunity and reflective motivation were the most consistent predictors of behavior change during COVID-19. Finally, as obesity/overweight tends to be higher among minority racial/ethnic groups (Dolinska et al., 2007), future research should aim to recruit an ethnically diverse sample of people with overweight/obesity.
Implications for practice and future research
Obesity rates in Slovakia are on the rise and higher than the EU average. Low fruit and vegetable intake and insufficient physical activity of 30–40% of Slovak inhabitants represent another salient problem in health management (Maciejewski et al., 2021; World Obesity Federation, 2021; OECD, 2023). In addition, the health status of the Slovak population lags behind the EU average (OECD, 2019, 2021, 2023) while about half of the deaths in Slovakia can be associated with behavioral risk factors, including dietary risks and low levels of physical activity, which is higher than the EU average of two in five deaths (Maciejewski et al., 2021; OECD, 2021, 2023). Thus, it is crucial to identify the behavioral, social, and cultural factors that influence human behavior to provide more evidence-based, effective, and people-centered services and policies for effective health change (WHO, 2022).
From a clinical perspective, understanding patients' deficits or shortcomings, as well as resources and strengths may help to increase the self-care and management of the patient. Based on the results of our findings it seems that different types of interventions should specifically target different components of COM-B, with self-efficacy identified as the stronger facilitator of behavior change when compared to self-esteem. Self-efficacy may be improved using behavior change techniques such as goal setting and self-monitoring (Silveira et al., 2021). These findings can be implemented in interventional programs using Cognitive Behavioral Therapy or Acceptance and Commitment Therapy-based interventions that target people with overweight and obesity and may help to support efficient weight management and sustain regular engagement in behavioral change (Zhang et al., 2018; Cattivelli et al., 2021).
Although much remains to be done to equip interventionists with effective techniques for the enhancement of self-esteem or self-efficacy, it should be acknowledged that our findings confirm the assumptions that strong capabilities, opportunities, reflective motivation, and high self-efficacy may be an important, but not sufficient, condition for initiating behavior change as they are not always translated into action (e.g., Webb and Sheeran, 2006; Rothman et al., 2009). Thus, future research should shed more light on the possible deficits in automatic motivation, as well as the inability to manage the lack of habitual change through psychological interventions aimed at self-esteem and self-efficacy identified in our study.
As habit has been proposed as a means to promote the long-term maintenance of behavior (Gardner and Rebar, 2019), it needs to be considered that even when people successfully initiate the recommended changes, the gains are often transient as few of the traditional behavior change strategies have built-in mechanisms for maintenance (Gardner et al., 2012). Current studies using COM-B also show the necessity of supporting long-term adherence to behavior change in weight management (Hassapidou et al., 2023). Brief advice from a physician, nurse, or nutrition specialist on how to change, and engage automatic processes, may offer a valuable alternative with the potential for long-term impact and offers a useful option in the behavior change toolkit (Gardner et al., 2012). Based on our findings, to promote habitual change special attention should be paid to people affected by overweight and obesity of younger age, without a spouse or partner, and with chronic conditions. More research is needed on how automatic and reflective systems interact to promote or derail a positive health behavior change. Longitudinal studies on the changes in automatic motivation are needed as it is necessary to recognize that habit forms with multiple cue-behavioral response repetitions, and may follow a non-linear trajectory (Gardner et al., 2022).
Conclusion
Behavioral interventions for weight management should specifically target different components of COM-B. Self-efficacy and self-esteem may play a significant role in individual capabilities, opportunities, and reflective motivation and should be included in tailored public health interventions. The results indicate deficits in automatic motivation, as well as the inability to manage the lack of habitual change through psychological interventions aimed at self-esteem and self-efficacy. It seems that health programs focusing on addressing poor health, younger people, and people without a partner or spouse may help to promote sustainable behavior change among people affected by overweight and obesity.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Comenius University in Bratislava (approval no. EK 02/2020). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
VT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Writing—original draft. DM: Conceptualization, Writing—review & editing. LF: Data curation, Writing—review & editing. JB: Writing—review & editing. PM: Data curation, Writing—review & editing. ZK: Writing—review & editing, Conceptualization. IN: Conceptualization, Supervision, Writing—review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Scientific Grant Agency of the Ministry of Education, Science, Research, and Sport of the Slovak Republic under Grant no. VEGA 1/0748/22.
Acknowledgments
We would like to thank all people who participated in this research. We would like to express our gratitude to all general practitioners, nurses, and public health professionals for the recruitment of patients.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^Ministry of Labour, Social Affairs and Family of the Slovak Republic (2022). Available online at: https://www.employment.gov.sk/en/family-social-assistance/material-need-assistance/subsistence-minimum.html.
References
Althoff, T., Sosič, R., Hicks, J. L., King, A. C., Delp, S. L., and Leskovec, J. (2017). Large-scale physical activity data reveal worldwide activity inequality. Nature 547, 336–339. doi: 10.1038/nature23018
Anekwe, C. V., Jarrell, A. R., Townsend, M. J., Gaudier, G. I., Hiserodt, J. M., and Stanford, F. C. (2020). Socioeconomics of obesity. Curr. Obes. Rep. 9, 272–279. doi: 10.1007/s13679-020-00398-7
Annesi, J. J. (2020). Psychosocial correlates of emotional eating and their interrelations: implications for obesity treatment research and development. J. Prim. Prev. 41, 105–125. doi: 10.1007/s10935-020-00580-6
Armitage, C. A., and Munro, K. J. (2023). Can the capabilities, opportunities and motivations model predict behavior one year later?. Health Psychol. 42:270. doi: 10.1037/hea0001269
Armitage, C. J., Keyworth, C., Gartland, N., Coleman, A., Fishwick, D., Johnson, S., et al. (2023). Identifying targets for interventions to support public use of face coverings. Br. J. Health Psychol. 28, 208–220. doi: 10.1111/bjhp.12620
Ashwell, M., and Gibson, S. (2016). Waist-to-height ratio as an indicator of ‘early health risk': simpler and more predictive than using a ‘matrix' based on BMI and waist circumference. BMJ Open 6:e010159. doi: 10.1136/bmjopen-2015-010159
Bandura, A. (1998). Health promotion from the perspective of social cognitive theory. Psychol. Health. 13, 623–649. doi: 10.1080/08870449808407422
Bandura, A., and Locke, E. A. (2003). Negative self-efficacy and goal effects revisited. J. Appl. Psychol. 1:87. doi: 10.1037/0021-9010.88.1.87
Barber, S. J., and Kim, H. (2021). COVID-19 worries and behavior changes in older and younger men and women. J Gerontol. Ser. B 76, e17–e23. doi: 10.1093/geronb/gbaa068
Björkman, S., Wallengren, O., Laurenius, A., Eliasson, B., and Larsson, I. (2022). Locus of control and self-efficacy in relation to 12-month weight change after non-surgical weight loss treatment in adults with severe obesity–A clinical cohort study. Obes. Med. 32:100409. doi: 10.1016/j.obmed.2022.100409
Brierley, M. L., Smith, L. R., Bailey, D. P., Every, S. A., Staines, T. A., and Chater, A. M. (2021). Perceived influences on reducing prolonged sitting in police staff: a qualitative investigation using the Theoretical Domains Framework and COM-B model. BMC Public Health 21, 1–12. doi: 10.1186/s12889-021-12019-6
Caleyachetty, R., Barber, T. M., Mohammed, N. I., Cappuccio, F. P., Hardy, R., Mathur, R., et al. (2021). Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. Lancet Diabetes Endocrinol. 9, 419–426. doi: 10.1016/S2213-8587(21)00088-7
Cattivelli, R., Guerrini Usubini, A., Manzoni, G. M., Vailati Riboni, F., Pietrabissa, G., Musetti, A., et al. (2021). ACTonfood. Acceptance and commitment therapy-based group treatment compared to cognitive behavioral therapy-based group treatment for weight loss maintenance: an individually randomized group treatment trial. Int. J. Environ. Res. Public Health 18:9558. doi: 10.3390/ijerph18189558
Chater, A. M., Smith, L., Ferrandino, L., Wyld, K., and Bailey, D. P. (2020). Health behaviour change considerations for weight loss and type 2 diabetes: nutrition, physical activity and sedentary behaviour. Pract. Diabetes 37, 228–231. doi: 10.1002/pdi.2311
Clark, S., McGrane, A., Boyle, N., Joksimovic, N., Burke, L., Rock, N., et al. (2021). “You're a teacher you're a mother, you're a worker”: gender inequality during COVID-19 in Ireland. Gender Work Organ 28, 1352–1362. doi: 10.1111/gwao.12611
Coms ´ a, L. T., David, O. A., and David, D. O. (2023). Relevant psychological factors in weight management. How to think and behave to lose weight and maintain it for good. J. Ration Emot. Cogn. Behav. Ther. 41, 176–192. doi: 10.1007/s10942-022-00455-1
Crowley, J., Ball, L., and Hiddink, G. J. (2020). Nutrition care by primary-care physicians: advancing our understanding using the COM-B framework. Public Health Nutr. 23, 41–52. doi: 10.1017/S1368980019003148
Dahlberg, K., Bylund, A., Stenberg, E., and Jaensson, M. (2022). An endeavour for change and self-efficacy in transition: patient perspectives on postoperative recovery after bariatric surgery–a qualitative study. Int. J. Qual. Stud. Health Wellbeing 17:2050458. doi: 10.1080/17482631.2022.2050458
De Lorenzo, A., Romano, L., Di Renzo, L., Di Lorenzo, N., Cenname, G., and Gualtieri, P. (2020). Obesity: a preventable, treatable, but relapsing disease. Nutrition 71:110615. doi: 10.1016/j.nut.2019.110615
Dolinska, S., Kudlackova, M., and Ginter, E. (2007). The prevalence of female obesity in the world and in the Slovak Gypsy women. Bratisl. Lek. Listy 108, 207–211.
Dunton, G., Rothman, A. J., Leventhal, A. M., and Intille, S. S. (2021). How intensive longitudinal data can stimulate advances in health behavior maintenance theories and interventions. Transl. Behav. Med. 11, 281–286. doi: 10.1093/tbm/ibz165
Ellis, K., Pears, S., and Sutton, S. (2019). Behavioural analysis of postnatal physical activity in the UK according to the COM-B model: a multimethods study. BMJ Open 9:e028682. doi: 10.1136/bmjopen-2018-028682
EURIDISS (1990). European research on incapacitating diseases and social support. Int. J. Health Sci. 1, 217–228.
Faul, F., Erdfelder, E., Buchner, A., and Lang, A. G. (2009). Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods 41, 1149–1160. doi: 10.3758/BRM.41.4.1149
Gallagher, D., Visser, M., Sepulveda, D., Pierson, R. N., Harris, T., and Heymsfield, S. B. (1996). How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups?. Am. J. Epidemiol. 143, 228–239. doi: 10.1093/oxfordjournals.aje.a008733
Gardner, B., Lally, P., and Wardle, J. (2012). Making health habitual: the psychology of ‘habit-formation' and general practice. Br. J. Gen. Pract. 62, 664–666. doi: 10.3399/bjgp12X659466
Gardner, B., and Rebar, A. L. (2019). “Habit formation and behavior change,” in Oxford Research Encyclopedia of Psychology.
Gardner, B., Rebar, A. L., and Lally, P. (2019). A matter of habit: recognizing the multiple roles of habit in health behaviour. Br. J. Health Psychol. 24, 241–249. doi: 10.1111/bjhp.12369
Gardner, B., Rebar, A. L., and Lally, P. (2022). How does habit form? Guidelines for tracking real-world habit formation. Cogent. Psychol. 9:2041277. doi: 10.1080/23311908.2022.2041277
Garvey, W. T., and Mechanick, J. I. (2020). Proposal for a scientifically correct and medically actionable disease classification system (ICD) for obesity. Obesity 28, 484–492. doi: 10.1002/oby.22727
Gu, Y., Zhou, R., Kong, T., Zhang, W., Chen, Y., Wang, C., et al. (2023). Barriers and enabling factors in weight management of patients with nonalcoholic fatty liver disease: a qualitative study using the COM-B model of behaviour. Health Expect. 26, 355–365. doi: 10.1111/hex.13665
Hassapidou, M., Vlassopoulos, A., and Kalliostra, M. (2023). European Association for the Study of Obesity Position Statement on Medical Nutrition Therapy for the Management of Overweight and Obesity in Adults Developed in Collaboration with the European Federation of the Associations of Dietitians. Obes. Facts. 16, 11–28. doi: 10.1159/000528083
Herber, O. R., Bücker, B., Metzendorf, M. I., and Barroso, J. (2017). A qualitative meta-summary using Sandelowski and Barroso's method for integrating qualitative research to explore barriers and facilitators to self-care in heart failure patients. Eur. J. Cardiovasc. Nurs. 16, 662–677. doi: 10.1177/1474515117711007
Huynh, T. L., Silveira, S. L., and Motl, R. W. (2023). Physical activity behavior in persons newly diagnosed with multiple sclerosis: Applying the Capability–Opportunity–Motivation–Behavior (COM-B) model. Mult. Scler. Relat. Disord. 69:104432. doi: 10.1016/j.msard.2022.104432
International Test Commission (2017). ITC Guidelines for Translating and Adapting Tests, 2nd Edn. Available online at: www.InTestCom.org (accessed January 11, 2024).
Jebeile, H., Cardel, M. I., Kyle, T. K., and Jastreboff, A. M. (2021). Addressing psychosocial health in the treatment and care of adolescents with obesity. Obesity 29, 1413–1422. doi: 10.1002/oby.23194
Johnson, M., Judah, G., Cunningham, D., and Olander, E. K. (2020). Individualised physical activity and physiotherapy behaviour change intervention tool for breast cancer survivors using self-efficacy and COM-B: feasibility study. Eur. J. Physiother. 24, 119–128. doi: 10.1080/21679169.2020.1804616
Kandel, P., Lim, S., Pirotta, S., Skouteris, H., Moran, L. J., and Hill, B. (2021). Enablers and barriers to women's lifestyle behavior change during the preconception period: a systematic review. Obes. Rev. 22:e13235. doi: 10.1111/obr.13235
Kelly, M. P., and Barker, M. (2016). Why is changing healthrelated behaviour so difficult? Public Health 136, 109–116. doi: 10.1016/j.puhe.2016.03.030
Keyworth, C., Epton, T., Goldthorpe, J., Calam, R., and Armitage, C. J. (2020). Acceptability, reliability, and validity of a brief measure of capabilities, opportunities, and motivations (“COM-B”). Br. J. Health Psychol. 25, 474–501. doi: 10.1111/bjhp.12417
Khanna, D., Peltzer, C., and Kahar, P. (2022). MS Body mass index (BMI): a screening tool analysis. Cureus 14:22119. doi: 10.7759/cureus.22119
Maciejewski, G., Kita, P., Ozimek, I., and Szlachciuk, J. (2021). Typology of consumers according to the declared consumption of food products and non-alcoholic beverages. Polish and Slovakian Case Studies. Agronomy 11:2141. doi: 10.3390/agronomy11112141
Michie, S., Atkins, L., West, R., Ramage-Morin, P., Kaplan, M. S., and Bernier, J. (2014). The Behaviour Change Wheel. A Guide to Designing Interventions, 1st Edn. Great Britain: Silverback Publishing, 1003–1010.
Newsom, J. T., Huguet, N., McCarthy, M. J., Ramage-Morin, P., Kaplan, M. S., Bernier, J., et al. (2012). Health behavior change following chronic illness in middle and later life. J. Gerontol. B Psychol. Sci. Soc. Sci. 67, 279–288. doi: 10.1093/geronb/gbr103
Niven, A., Baker, G., Almeida, E. C., Fawkner, S. G., Jepson, R., Manner, J., et al. (2022). “Are we working (too) comfortably?”: understanding the nature of and factors associated with sedentary behaviour when working in the home environment. Occup. Health Sci. 7, 71–88. doi: 10.21203/rs.3.rs-1362673/v1
OECD (2019). State of Health in the EU. Slovak Republic. Country Health Profile 2019. Available online at: https://www.oecd.org/slovakia/slovak-republic-country-health-profile-2019-c1ae6f4b-en.htm (accessed May 3, 2023).
OECD (2021). State of Health in the EU. Slovak Republic. Country Health Profile 2021. Available online at: https://www.oecd.org/publications/slovak-republic-country-health-profile-2021-4ba546fe-en.htm (accessed May 3, 2023).
OECD (2023). State of Health in the EU. Slovak Republic. Country Health Profile 2023. Available online at: https://eurohealthobservatory.who.int/publications/m/slovakia-country-health-profile-2023 (accessed January 11, 2024).
Oikarinen, N., Jokelainen, T., Heikkil,ä, L., Nurkkala, M., Hukkanen, J., Salonurmi, T., et al. (2023). Low eating self-efficacy is associated with unfavorable eating behavior tendencies among individuals with overweight and obesity. Sci. Rep. 13:7730. doi: 10.1038/s41598-023-34513-0
Olander, E. K., Fletcher, H., Williams, S., Atkinson, L., Turner, A., and French, D. P. (2013). What are the most effective techniques in changing obese individuals' physical activity self-efficacy and behaviour: a systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 10, 1–15. doi: 10.1186/1479-5868-10-29
Oliveira, M. R., Sudati, I. P., and Konzen, V. D. M. (2022). Covid-19 and the impact on the physical activity level of elderly people: a systematic review. Exp. Gerontol. 159:111675. doi: 10.1016/j.exger.2021.111675
Pasco, J. A., Holloway, K. L., Dobbins, A. G., Kotowicz, M. A., Williams, L. J., and Brennan, S. L. (2014). Body mass index and measures of body fat for defining obesity and underweight: a cross-sectional, population-based study. BMC Obes. 1, 1–7. doi: 10.1186/2052-9538-1-9
Perez, C. C. (2019). Invisible women: Exposing Data Bias in a World Designed for Men. New York, NY: Abrams Press, 432.
Phillips, L. A., Cohen, J., Burns, E., Abrams, J., and Renninger, S. (2016). Self-management of chronic illness: the role of ‘habit' versus reflective factors in exercise and medication adherence. Int. J. Behav. Med. 39, 1076–1091. doi: 10.1007/s10865-016-9732-z
Pineda, E., Sanchez-Romero, L. M., Brown, M., Jaccard, A., Jewell, J., and Galea, G. (2018). Forecasting future trends in obesity across Europe: the value of improving surveillance. Obes. Facts 11, 360–371. doi: 10.1159/000492115
Porter, L., Cox, J. S., Wright, K. A., Lawrence, N. S., and Gillison, F. B. (2022). The impact of COVID-19 on the eating habits of families engaged in a healthy eating pilot trial: a thematic analysis. Health Psychol. Behav. Med. 10, 241–261. doi: 10.1080/21642850.2022.2043750
Prochaska, J. O., Prochaska, J. M., Trafton, J. A., and Gordon, W. P. (2005). An update on maximum impact practices from a transtheoretical approach. Best Pract. Behav. Manag. Chron. Dis. 1, 1–16.
Rosenberg, M. (1965). Rosenberg self-esteem scale (RSE). Acceptance and commitment therapy. Meas. Pack. 61, 18. doi: 10.1037/t01038-000
Rothman, A. J., Sheeran, P., and Wood, W. (2009). Reflective and automatic processes in the initiation and maintenance of dietary change. Ann. Behav. Med. 38, 4–17. doi: 10.1007/s12160-009-9118-3
Rubiano Matulevich, E. C., and Viollaz, M. (2019). “Gender differences in time use: allocating time between the market and the household,” in World Bank Policy Res. Work. Pap. (8981) (Washington, DC: The World Bank), 53.
Satariano, W. A., and Maus, M. (2017). Aging, Place, and Health: A Global Perspective. Burlington, MA: Jones and Bartlett Learning, 378.
Schoufour, J. D., Tieland, M., Barazzoni, R., Allouch, S. B., van der Bie, J., Boirie, Y., et al. (2021). The relevance of diet, physical activity, exercise, and persuasive technology in the prevention and treatment of sarcopenic obesity in older adults. Front. Nutr. 8:661449. doi: 10.3389/fnut.2021.661449
Schwarzer, R., and Jerusalem, M. (1995). Generalized self-efficacy scale. J. Weinman, S. Wright, M. Johnston, Measures in health psychology: A user's portfolio. Causal Control Beliefs 35:37. doi: 10.1037/t00393-000
Sheeran, P., Maki, A., Montanaro, E., Avishai-Yitshak, A., Bryan, A., Klein, W. M. P., et al. (2016). The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Health Psychol. 35, 1178–1188. doi: 10.1037/hea0000387
Shoneye, C. L., Mullan, B., Begley, A., Pollard, C. M., Jancey, J., and Kerr, D. A. (2020). Design and development of a digital weight management intervention (ToDAy): qualitative study. JMIR mHealth uHealth 8:e17919. doi: 10.2196/17919
Sialino, L. D., Picavet, H. S. J., Wijnhoven, H. A. H., Loyen, A., Verschuren, W. M. M., Visser, M., et al. (2022). Exploring the difference between men and women in physical functioning: how do sociodemographic, lifestyle-and health-related determinants contribute? BMC Geriatr. 22, 1–9. doi: 10.1186/s12877-022-03216-y
Silveira, S. L., Riemann-Lorenz, K., Heesen, C., and Motl, R. W. (2021). Current and long-term physical activity among adults with multiple sclerosis in the United States: COM-B variables as explanatory factors. IJBM 28, 561–574. doi: 10.1007/s12529-020-09946-w
Sooknarine-Rajpatty, J. B., Auyeung, A., and Doyle, F. A. (2020). Systematic review protocol of the barriers to both physical activity and obesity counselling in the secondary care setting as reported by healthcare providers. Int. J. Environ. Res. Public Health 17:1195. doi: 10.3390/ijerph17041195
Spence, J. C., Rhodes, R. E., McCurdy, A., Mangan, A., Hopkins, D., and Mummery, W. K. (2021). Determinants of physical activity among adults in the United Kingdom during the COVID-19 pandemic: The DUK-COVID study. Br. J. Health Psychol. 26, 588–605. doi: 10.1111/bjhp.12497
Spinosa, J., Christiansen, P., Dickson, J. M., Lorenzetti, V., and Hardman, C. A. (2019). From socioeconomic disadvantage to obesity: the mediating role of psychological distress and emotional eating. Obesity 27, 559–564. doi: 10.1002/oby.22402
Stojanovic, M., Fries, S., and Grund, A. (2021). Self-efficacy in habit building: how general and habit-specific self-efficacy influence behavioral automatization and motivational interference. Front. Psychol. 12:643753. doi: 10.3389/fpsyg.2021.643753
Teixeira, P. J., and Marques, M. M. (2017). Health behavior change for obesity management. Obes. Facts 10, 666–673. doi: 10.1159/000484933
The World Bank (2018). Women Economic Empowerment Study. Available online at: https://documents1.worldbank.org/curated/en/861491551113547855/pdf/134846-WP-PUBLIC-march-2-WB-Women-Study-EN.pdf (accessed March 9, 2023).
Von Bonsdorff, M. B., Rantanen, T., Sipilä, S., Salonen, M. K., Kajantie, E., Osmond, C., et al. (2011). Birth size and childhood growth as determinants of physical functioning in older age. Am. J. Epidemiol. 174:1336. doi: 10.1093/aje/kwr270
Wang, F., and Veugelers, P. J. (2008). Self-esteem and cognitive development in the era of the childhood obesity epidemic. Obes. Rev. 9, 615–623. doi: 10.1111/j.1467-789X.2008.00507.x
Webb, T. L., and Sheeran, P. (2006). Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol. Bull. 132:249. doi: 10.1037/0033-2909.132.2.249
Werner, H., Young, C., Hakeberg, M., and Wide, U. (2020). A behavioural intervention for young adults with dental caries, using acceptance and commitment therapy (ACT): treatment manual and case illustration. BMC Oral Health 20, 1–8. doi: 10.1186/s12903-020-01213-4
West, R., and Michie, S. (2020). A Brief Introduction to the COM-B Model of Behaviour and the PRIME Theory of Motivation. Qeios Ltd. London (UK).
Whittal, A., Atkins, L., and Herber, O. R. (2021). What the guide does not tell you: reflections on and lessons learned from applying the COM-B behavior model for designing real life interventions. Transl. Behav. Med. 11, 1122–1126. doi: 10.1093/tbm/ibaa ,116
WHO (2021). Obesity and Overweight (2021). Available online at:https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed May 3, 2023).
WHO (2022). Setting up a Behavioural Insights Unit - WHO Launches a Set of Considerations to Support Countries. Available online at: https://www.who.int/europe/news/item/12-05-2022-setting-up-a-behavioural-insights-unit—who-launches-a-set-of-considerations-to-support-countries (accessed March 13, 2023).
WHO Regional Office for Europe (2022). WHO European Regional Obesity Report 2022. Available online at: https://apps.who.int/iris/bitstream/handle/10665/353747/9789289057738-eng.pdf?sequence=1andisAllowed=y (accessed March 9, 2023).
Williams, K., Steptoe, A., and Wardle, J. (2013). Is a cancer diagnosis a trigger for health behaviour change? Findings from a prospective, population-based study. Br. J. Cancer 108, 2407–2412. doi: 10.1038/bjc.2013.254
Willmott, T. J., Pang, B., and Rundle-Thiele, S. (2021). Capability, opportunity, and motivation: an across contexts empirical examination of the COM-B model. BMC Public Health 21:1014. doi: 10.1186/s12889-021-11019-w
World Obesity Federation (2021). COVID-19 and Obesity: The 2021 Atlas. Available online at: http://s3-eu-west-1.amazonaws.com/wof-files/2722_WOF_-_COVID-19_and_Obesity-The_2021_Atlas_WEB.pdf (accessed March 9, 2023).
Yerkes, M. A., André, S. C. H., Besamusca, J. W., Kruyen, P. M., Remery, C. L. H. S., van der Zwan, R., et al. (2020). ‘Intelligent'lockdown, intelligent effects? Results from a survey on gender (in) equality in paid work, the division of childcare and household work, and quality of life among parents in the Netherlands during the Covid-19 lockdown. PLoS ONE 15:e0242249. doi: 10.1371/journal.pone.0242249
Zhang, C. Q., Leeming, E., Smith, P., Chung, P. K., Hagger, M. S., and Hayes, S. C. (2018). Acceptance and commitment therapy for health behavior change: a contextually-driven approach. Front. Psychol. 11:2350. doi: 10.3389/fpsyg.2017.02350
Zhang, C. Q., Zhang, R., Schwarzer, R., and Hagger, M. S. (2019). A meta-analysis of the health action process approach. Health Psychol. 38, 623–637 doi: 10.1037/hea0000728
Keywords: COM-B, obesity, overweight, weight management, behavior change
Citation: Timkova V, Minarikova D, Fabryova L, Buckova J, Minarik P, Katreniakova Z and Nagyova I (2024) Facilitators and barriers to behavior change in overweight and obesity management using the COM-B model. Front. Psychol. 15:1280071. doi: 10.3389/fpsyg.2024.1280071
Received: 19 August 2023; Accepted: 05 February 2024;
Published: 22 February 2024.
Edited by:
Mohsen Saffari, Baqiyatallah University of Medical Sciences, IranReviewed by:
Ewelina Czenczek-Lewandowska, University of Rzeszow, PolandGiorgia Varallo, University of Parma, Italy
Copyright © 2024 Timkova, Minarikova, Fabryova, Buckova, Minarik, Katreniakova and Nagyova. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Iveta Nagyova, aXZldGEubmFneW92YUB1cGpzLnNr
 Vladimira Timkova
Vladimira Timkova Daniela Minarikova2
Daniela Minarikova2 Zuzana Katreniakova
Zuzana Katreniakova Iveta Nagyova
Iveta Nagyova