
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 07 December 2023
Sec. Health Psychology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1325622
This article is part of the Research Topic Trauma, Attachment and Culture View all 4 articles
 Mariana Rangel Maciel1*†
Mariana Rangel Maciel1*† Vinicius Fernando Calsavara2†
Vinicius Fernando Calsavara2† Cecilia Zylberstajn1†
Cecilia Zylberstajn1† Marcelo Feijo Mello1†
Marcelo Feijo Mello1† Bruno Messina Coimbra1,3,4†
Bruno Messina Coimbra1,3,4† Andrea Feijo Mello1†
Andrea Feijo Mello1†Introduction: Attachment patterns are established during early childhood; however, extreme experiences throughout life may change this structure, either toward attachment security or insecurity. We analyzed changes in attachment dimensions in women with acute post-traumatic stress disorder (PTSD) following sexual assault, that were randomized to a 14-week treatment with either the medication sertraline or Interpersonal Psychotherapy.
Methods: Seventy-four adult women who presented significant reduction in PTSD symptoms across the trial responded to the Revised Adult Attachment Scale at baseline, on week 8 of treatment, and at the end of the trial, on week 14. We fitted a generalized linear model to explain the attachment anxiety and avoidance scores at baseline. A generalized linear mixed model investigated how attachment dimensions changed over time. Socioeconomic data, treatment type, history of childhood trauma, and PTSD severity over the 14-week period were the considered covariates.
Results: At baseline, attachment anxiety was associated with a history of early trauma. Attachment anxiety remained stable during the follow-up. Attachment avoidance, on the other hand, significantly increased from baseline to week 14. Higher avoidance was observed in patients with higher total PTSD scores and on the cluster of hyperarousal symptoms. Races other than White (black, mixed-race, or Asian) and younger age were associated with higher attachment avoidance.
Discussion: Contrary to our expectations, attachment avoidance increased during follow-up, indicating changes in the interpersonal realm beyond the symptoms of PTSD.
Sexual assault is frequent and distributed globally (Abrahams et al., 2014; World Health Organization, 2021). In Brazil, recent data show a consistent increase in rape reports over the past 10 years, from 44.000 in 2011 to 75.000 in 2022. Nonetheless, estimates indicate that only 8.5% of incidents are reported, suggesting actual numbers may reach approximately 800,000 cases annually (Cerqueira et al., 2021; Bueno et al., 2023).
There are multiple forms of sexual violence; sexual assault refers to any sexual contact or behavior without explicit consent. Rape is defined as sexual assault with penetration. Sexual assault victims are at a high risk of developing clinical and psychiatric disorders, such as post-traumatic stress disorder (PTSD), depression, substance abuse, and anxiety disorders (Elliott et al., 2004; Dworkin et al., 2017; Lake et al., 2022; Stea et al., 2023). The prevalence of PTSD after sexual assault is approximately 50%, and this type of trauma is also associated with poorer PTSD outcomes, as the disease tends to be more severe and chronic (Steenkamp et al., 2012; Elklit and Christiansen, 2013; Möller et al., 2014).
PTSD is a condition that may develop after a life-threatening experience. The traumatic event is required to consider the diagnosis; symptoms include intrusive memories of the experience, avoidance of stimuli that remind them of the event, social isolation, anhedonia, hyperarousal, irritability, sleep disturbances (Yehuda et al., 2015). Most individuals that go through life-threatening experiences do not develop PTSD. Pre-trauma characteristics, specificities of the traumatic event itself, and post-trauma factors may increase or decrease the magnitude of risk (Brewin et al., 2000). Among the pre-trauma characteristics under consideration is attachment style (Clark and Owens, 2012; Bruno et al., 2019; Marshall and Frazier, 2019).
Attachment style is one of the most extensively studied characteristics that shape how humans respond to stress. When John Bowlby developed the theory, which was later strengthened by the field research done by Mary Ainsworth and colleagues, attachment was conceptualized as a behavioral system based on early experiences with caregivers, which determined a matrix called “internal working model” – a template of how comfortable that individual would be in intimate relations, and how positive his or her views and expectations of themselves and others would predominantly be (Bowlby, 1973; Bretherton, 1992).
Observational studies in children demonstrated that attachment patterns could be described by two linear functions, anxiety and avoidance; the same functions were used to determine types of attachment behavior in adults, expanding research to other life stages (Ainsworth et al., 1978; Hazan and Shaver, 1987). Attachment anxiety refers to the degree to which a person is worried about the availability of others in times of need, resulting in hyperactivation of the attachment system; attachment avoidance refers to the difficulty in closeness and relying on others for support, leading to deactivating strategies. Securely attached individuals display low anxiety and low avoidance. The anxiety dimension can be conceptualized as a model of self, while the avoidance dimension represents as a model of others. Individuals characterized by secure attachment have a positive model of both self and others, whereas individuals with insecure attachment may have a negative model of self (anxiety), others (avoidance), or both (anxious avoidant) (Griffin and Bartholomew, 1994).
The attachment pattern established in childhood launches the individual into a developmental pathway, that tends to stability but is subject to change depending on cumulative history along the way (Sroufe and Waters, 1977). As a result, both continuity and discontinuity of attachment style across the lifespan are possible, as indicated by longitudinal studies (Sroufe, 2005; Van Assche et al., 2013; Chopik et al., 2019). The initial matrix serves as a prototype that can be later modified to a certain point, depending on experiences that follow during adult life (Pinquart et al., 2013). Severe interpersonal violence, socioeconomic disadvantage, and chronic disease can potentially increase attachment insecurity (Waters et al., 2000; Bachem et al., 2019). Evidence indicates that samples more exposed to adversities may display more frequent changes in the structure, likely due to the instability within their life circumstances and relationships (Weinfield et al., 2000, 2004).
Conversely, positive life changes and relationships and social support may help change attachment styles toward security (Travis et al., 2001; Pace et al., 2019; Slade and Holmes, 2019). Furthermore, it has been replicated that psychotherapy may enhance attachment security (Lahav and Elklit, 2016; Diamond et al., 2023) as research findings have reported attachment style changes in time-limited treatments with several psychotherapy orientations (Muller and Rosenkranz, 2009; Kinley and Reyno, 2013). The literature on psychotherapeutic treatment for PTSD offers relevant data, as improving social bonds, interpersonal relationships, and attachment are possible mechanisms through which psychotherapy may exert its effects (Ravitz et al., 2008; Coyne et al., 2018).
Secure attachment has consistently shown a link to resilience, while insecure attachment styles are identified as risk factors for developing psychopathology (Fonagy et al., 1996; Darling Rasmussen et al., 2019). In the face of stress and adversity, securely attached individuals tend to maintain emotional regulation, effectively seek social support, activate internalized representations of attachment figures, and balance emotions and cognitions in their behavior (Ensink et al., 2016). In contrast, insecurely attached individuals often experience difficulties in self-regulation, exhibit unstable relationships, display more negative affectivity, and suffer from higher levels of global distress – all risk factors for psychopathology (Mikulincer and Shaver, 2012).
The relationship between attachment and post-traumatic reactions, particularly PSTD, has been explored as a risk factor for the development of pathological reactions, alone or interacting with biological and psychological characteristics (Lim et al., 2012; Tamman et al., 2021; Jittayuthd and Karl, 2022). Attachment has been shown to interfere with the response and adherence to treatment (Forbes et al., 2010). Overall, studies indicate that insecure attachment styles are associated with a higher risk of developing PTSD and a worse prognosis of the disorder (Levy et al., 2011; Woodhouse et al., 2015; Ferrajão, 2022). Considering that the relationship of attachment and trauma is bidirectional, it is also relevant to investigate the effect of trauma and PTSD on attachment styles. This has been explored longitudinally in cohorts of veterans with PTSD (Franz et al., 2014; Mikulincer et al., 2014). Taken together, the evidence suggests that insecure attachment may function as both a risk factor for and be influenced by PTSD (Castro-Vale et al., 2020). However, there is limited evidence investigating longitudinal changes in attachment styles in patients undergoing treatment for PTSD.
In light of the documented association between PTSD, its treatment, and attachment within existing literature, our study aimed to longitudinally explore attachment dimensions over a 14-week period of post-traumatic stress disorder intervention. The research encompassed a cohort of 74 women who recently experienced sexual assault (rape or attempted rape) and received treatment using either sertraline or Interpersonal Psychotherapy adapted for PTSD (IPT-PTSD; Markowitz, 2016). We hypothesized that attachment anxiety and avoidance would be greater in patients with higher levels of childhood and adolescent trauma, with greater PTSD severity, younger age, and lower income.
Subsequently, we measured whether attachment fluctuated during follow-up and which covariates might be related to possible attachment changes. We hypothesized that attachment dimensions would shift toward security; that is, reduced avoidance and anxiety dimensions scores. Considering that IPT works on interpersonal relations as a means to improve PTSD symptoms (Lipsitz and Markowitz, 2013), we hypothesized that changes in attachment would be more prominent in the psychotherapy group. Psychiatric treatment (consultations and the use of medication sertraline) does not target attachment directly but may affect it indirectly through PTSD improvement. Other variables included in the model were: PTSD symptoms, age, history of early trauma, socioeconomic status, racial background, and marital status. These characteristics have been shown to have a possible impact on attachment styles (Ehrlich et al., 2022; Kazmierski et al., 2023).
Participants were referred to us by a women’s health hospital in São Paulo. Women admitted to this hospital with a history of sexual assault (defined as forced penetration, attempted forced penetration, or alcohol/drug-facilitated forced or attempted penetration) that had occurred one to six months prior to admission were requested to fill in the National Stressful Events Survey Short Scale for PTSD (LeBeau et al., 2014). If this screening measure was positive, they were referred to our outpatient clinic. A telephone call from our team assessed initial eligibility criteria; an appointment with psychologists or psychiatrists from the research team was then scheduled, for a full clinical evaluation and subsequent tests. From 149 women referred to our service, 34 refused to participate in the study, 38 were not eligible, and 3 could not be located. A total of 74 women diagnosed with PTSD after sexual assault were enrolled in the trial between January 2016 and April 2019. The complete study protocol has been described by Coimbra et al. (2020).
The inclusion criteria were as follows: (1) age 18–45 years; (2) sexual assault experienced 1–6 months before evaluation; (3) current PTSD diagnosis on the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998; Amorim, 2000); (4) CAPS-5 score > 26, indicating a current PTSD diagnosis; and (5) Ethics Review Board-approved signed informed consent. Exclusion criteria were as follows: (1) psychiatric or psychotherapeutic treatment for the present disorder; (2) severe suicidal risk, evaluated in a clinical interview by a trained researcher; (3) pregnancy; (4) chronic corticosteroid use; (5) unstable medical condition or neurologic disease; (6) Inability to understand the informed consent or research protocol; (7) substance use disorder within the previous six months; and (8) bipolar disorder or schizophrenia. This study was approved by the Research Ethics Committee.
The initial interview included (a) a sociodemographic questionnaire developed for the study, including age, race, relationship status, income, living conditions, and educational level; (b) Clinician-Administered Post-Traumatic Stress Disorder Scale-5 (Weathers et al., 2018); (c) Childhood Trauma Questionnaire (Bernstein et al., 1994); and (d) Revised Adult Attachment Scale – Close Relationships version (Collins and Read, 1990; Collins, 1996). The study data were stored in REDCap, a secure web-based research application.
The RAAS is a self-reported measure of adult attachment conceptually derived from Hazan and Shaver’s prototype for adult attachment (Hazan and Shaver, 1987). According to the authors, it can be scored on three (close, dependent, and anxious) or two (avoidance and anxiety) dimensions. We chose to use the latter, facilitating comparisons with other studies. There are several self-report measures of attachment, and many yield results in the form of these two dimensions (Mikulincer and Shaver, 2016). Continuous values were used for this analysis, resulting in scores ranging from 1 to 5 for each dimension. If a categorical viewpoint was used, scores above 3 would be considered positive for each dimension. Cronbach’s Alpha for anxiety, close and dependent subscales are, respectively, 0.72, 0.69 and 0.75; test–retest reliability indexes are 0.52, 0.68 and 0.72 (Collins and Read, 1990). The instrument has been validated for the Brazilian population (Teixeira et al., 2019).
PTSD symptoms were quantified using the CAPS-5. The scale generates a total score that can be summed to indicate the overall severity of the disorder; the threshold for establishing a PTSD diagnosis was 26. It comprises 20 symptom-related questions divided into four groups, one for each diagnostic cluster: five items for intrusion symptoms, two items for avoidance, seven items for alterations in cognition and mood, and six items for hyperarousal. Each symptom is quantified from 0 (absent) to 4 (extreme/incapacitating), and a severity rating of 2 or higher implies that the criteria are considered present. The CAPS-5 has demonstrated high internal consistency (α = 0.88), and high interrater and test–retest reliability coefficients (κ = 0.78 and 0.83, respectively); the correlation with other valid measures of PTSD symptoms is strong, indicating high construct validity (Weathers et al., 2018). The Portuguese version of the scale has been validated in Brazil (Oliveira-Watanabe et al., 2021).
The CTQ is a widely used retrospective, self-report measure of childhood maltreatment. Four factors are identified: physical and emotional abuse, physical neglect, emotional neglect, and sexual abuse. The instrument presents 28 items, and response to each item is rated on a 5-point Likert-type scale. Results can be analyzed for each trauma type or as a total score – a continuous total score was the measure that entered our analysis. Cronbach’s Alpha for each factor range from 0.78 to 0.94, and 0.95 for the total scale, showing high internal consistency, and test–retest reliability coefficients range from 0.80 to 0.88 (Bernstein et al., 1994). The instrument shows high convergence to interview measures of early trauma and has been translated to Portuguese (Grassi-Oliveira et al., 2006).
After inclusion, the patients were randomized to receive either IPT-PTSD (n = 38) or pharmacological treatment with sertraline (n = 36). The duration of the randomized clinical trial was 14 weeks. IPT was delivered in 14 weekly 50-min sessions following the IPT-PTSD manual (Markowitz, 2016). The sertraline dose ranged from 50 to 200 mg daily and was titrated according to the clinician’s understanding of the patient’s needs and tolerance. Appointments were scheduled at baseline and weeks 2, 4, 8, and 14. Pharmacotherapy sessions lasted 15–30 min and focused on targeting PTSD symptoms and exploring medication benefits and side effects. Both sertraline and IPT-PTSD patients could receive low-dose quetiapine (25–50 mg), risperidone (0.5–2.0 mg), or zolpidem CR (12.5 mg) for insomnia or PTSD-related psychotic symptoms.
An evaluator blinded to the treatment condition assessed patients at baseline and weeks 8 and 14. Independent appointments were scheduled for these assessments, that were performed by a psychologist who was otherwise not involved in the clinical trial. The standardized instruments used at the initial visit were repeated at weeks 8 and 14, except for the sociodemographic questionnaire and the CTQ, which were only applied at the initial visit.
The results of this clinical trial have been published and are beyond the scope of this study (Proença et al., 2022). We assessed the PTSD symptoms and attachment dimensions of the entire sample at baseline and at weeks 8 and 14 to evaluate the eventual attachment changes across treatments.
We described baseline patient characteristics as absolute and relative frequencies for qualitative variables and as the mean, standard deviation, median, and minimum and maximum for quantitative variables. Bivariate associations between two qualitative variables were assessed using Fisher’s exact test or the chi-squared test – qualitative variables used in the model were race, marital status and income (classified in two categories). Quantitative variables were compared between the two groups using the t-test if the normality assumption was satisfied; otherwise, the Mann–Whitney U test was applied. The Shapiro-Francia test was applied to evaluate the normality assumption.
Univariable and multivariable generalized linear models (GLMs) were fitted considering: (i) avoidance and (ii) anxiety dimensions as outcomes, and age, income, CTQ score, race, treatment group (SER or IPT-PTSD), relationship status, and CAPS-5 total score at baseline as covariates. We also fitted multivariable generalized linear mixed models (GLMMs) considering the attachment dimensions of anxiety and avoidance, measured by the RAAS over time, as outcomes, and the same covariates previously mentioned. In the mixed models, the CAPS-5 score was considered as a time-dependent covariate: scores from the baseline, from week 8 and week 14 were added in the model. The subjects’ random effects describing the repeated measures were considered. The presence of an interaction term between time and patient characteristics was tested using a likelihood ratio test. Sensitivity analyses were conducted by employing each of the four CAPS-5 subscales—symptoms of intrusion, avoidance, alterations in cognition and mood, and hyperarousal—as time-dependent covariates instead of using the total CAPS-5 score collected over time. The gamma distribution with identity or log-link functions was utilized to identify the factors associated with the avoidance score, whereas the normal distribution with the identity link function was used to model the anxiety score as a function of the covariates in the GLMs and GLMMs.
We chose to use valid cases in all analyses and refrained from applying imputation strategies to handle missing data. Profile analysis showed great variability in individual patterns, rendering the imputation perilous.
All hypothesis tests were two-sided with a 5% significance level. Thus, results with p-values lower than 0.05 were considered statistically significant. All statistical analyses were performed using R version 4.1 (R Core Team, 2020).
The baseline characteristics of the treatment groups are shown in Table 1. No statistically significant differences were observed between the treatment groups at baseline. Race was reported by the patients to be white (n = 32), black/mixed-race (n = 41), and Asian (n = 1). Because of the small number of patients in each distinct category, we grouped the categories Black/mixed-race and Asian, and two categories were considered for the statistical analysis.
Sexual assault was classified as rape (with penetration) in 88% of women, and in 94.6% of the cases, the aggressor was unknown to the victim. The prevalence of drug-facilitated sexual assault was 27%. Early abuse and neglect were also extensive in our sample, as indicated by the total CTQ scores in Table 1.
Of the 74 women enrolled, 48 (64.9%) completed the intermediate assessment (week 8) and 46 (62.2%) completed the clinical trial (week 14), generating attrition rates of 37.8% from baseline to week 14. The research team excluded six women, for reasons such as pregnancy, elevated suicidal risk, or initiating concomitant treatment elsewhere. Twenty-two women dropped out of study (29.7%); 15 of them did so very early in the follow-up, attending only the first or second visit. There were no statistically significant differences between completers and dropouts regarding treatment type, PTSD symptoms, attachment dimensions scores, and other baseline characteristics except for age – women who dropped out of the study were younger, with mean age 22.27 (4.60) vs. 26.10 (7.50), (p < 0.05). The RAAS was evaluated in 73 women at baseline, 25 (34.2%) at week 8, and in 45 (61.6%) women who completed the trial – one of the completers missed the evaluation visit at week 14.
The only significant association in the linear models was attachment anxiety (RAAS anxiety) and a history of early trauma (CTQ total score; p < 0.05). No significant associations were observed with attachment avoidance. The results of the fitted models are presented in Supplementary Material (Part 1).
Two multivariable mixed models were fitted to evaluate the changes in attachment dimensions across the 14 weeks of follow-up. Tables 2, 3 present the results of the multivariable generalized linear mixed models for the outcomes of attachment avoidance and anxiety, respectively. The interaction terms between time and (i) CAPS-5 scores, (ii) treatment arm, and (iii) race were tested, and no statistically significant interactions were found. Attachment anxiety did not show statistically significant variations across time and none of the examined covariates had an impact on the results. Attachment avoidance, on the other hand, increased over time (p < 0.0001); the increase was greater for patients with higher CAPS-5 scores, younger patients, and those who reported a race other than white (Black, mixed-race, or Asian).
We constructed an additional model using the CAPS-5 subscales for each cluster of PTSD symptoms instead of the total score. Other covariates remained unchanged. The only PTSD symptom cluster significantly related to attachment avoidance was hyperarousal (Cluster E). The tables that depict the results of this model are provided in Supplementary Materials, Part 2. Both groups showed a similar improvement in PTSD symptoms – see Proença et al. for the complete description of the results of the clinical trial (Proença et al., 2022).
Figures 1–3 illustrate RAAS avoidance and anxiety results across follow-up.
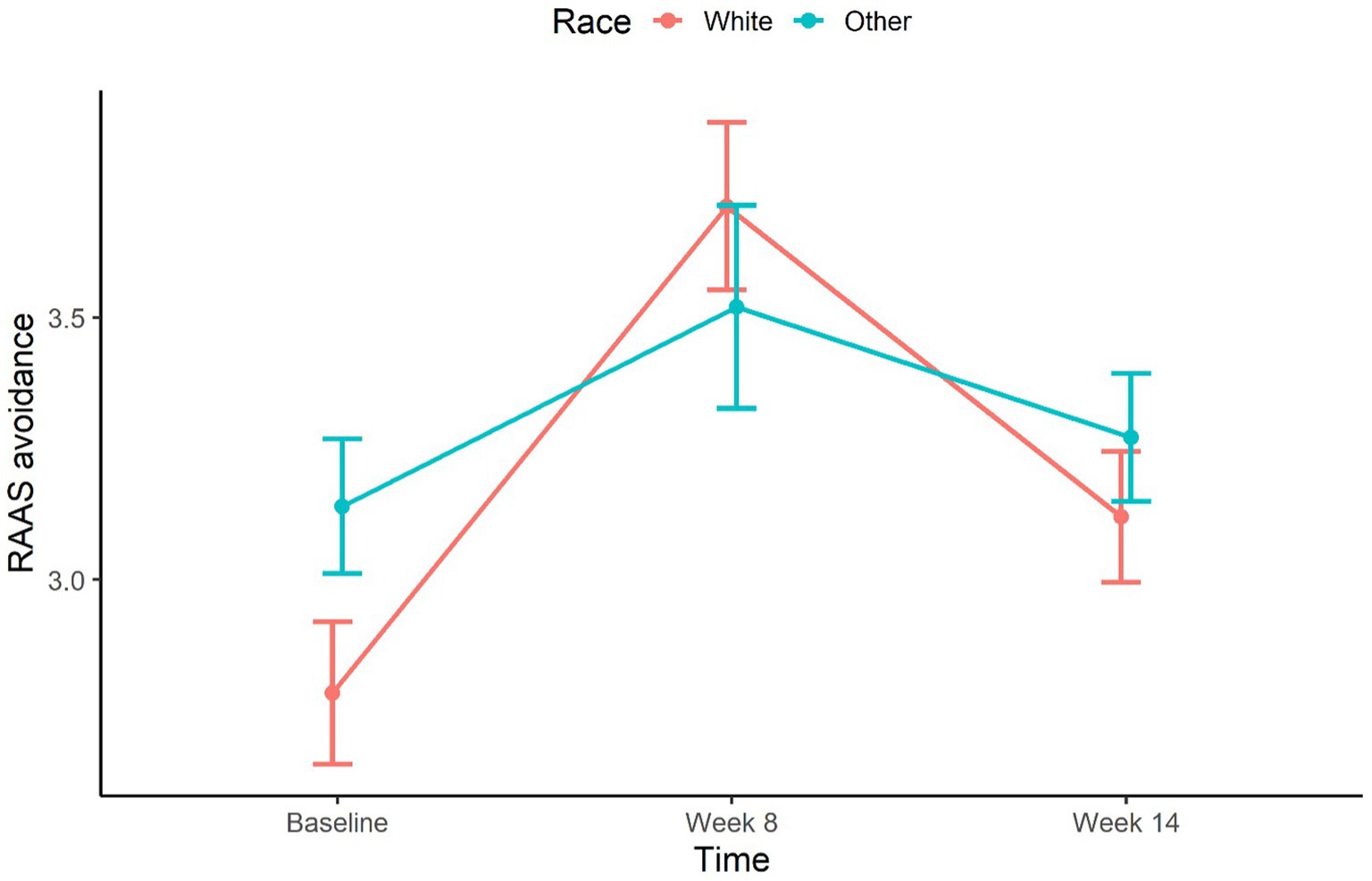
Figure 3. Mean profile of attachment avoidance over time by race. Error bars represent the standard error.
In this study, we examined attachment styles in a sample of adult women with PTSD after a recent sexual assault who were treated for 14 weeks with either IPT or sertraline. Attachment was measured at baseline and at weeks 8 and 14, as well as PTSD symptoms. Contrary to our hypothesis, attachment anxiety remained stable throughout the follow-up period, and attachment avoidance slightly increased equally in both treatment groups. This increased attachment avoidance was associated with higher PTSD severity, races other than white (Black, mixed-race, Asian), and younger age. When the PTSD symptoms were broken down into clusters, the cluster associated with increased attachment avoidance was hyperarousal (cluster E).
We found higher levels of attachment insecurity in our sample than generally reported in epidemiological data; approximately 40% presented with secure attachment at baseline, while population studies find 60% (Mickelson et al., 1997; Bakermans-Kranenburg et al., 2009). However, recent data evaluating college students in the United States indicate a possible rise in insecure attachment to levels similar to those found in our study (Konrath et al., 2014). To the best of our knowledge, there are no data on the Brazilian population. Considering that we evaluated only women who developed PTSD after sexual violence (not resilient), the higher proportion of insecure attachment is possibly a reflection of its role as a risk factor for the development of the disorder (Mikulincer et al., 2015).
The women in our study reported high levels of childhood trauma, which is strongly associated with attachment insecurity (Egeland and Sroufe, 1981). The findings regarding childhood trauma are consistent with epidemiological data from the Brazilian population (Zanoti-Jeronymo et al., 2009; Soares et al., 2016). The only characteristic that significantly explained the attachment dimensions at baseline was early trauma, which was related to attachment anxiety. None of the covariates analyzed explained attachment avoidance.
Contrary to our expectations, we did not find a decrease in attachment anxiety and/or avoidance during the follow-up period, accompanying an improvement in PTSD symptoms. The increase in attachment avoidance in our sample was associated with higher PTSD symptoms across the trial, which may reflect more severely compromised patients who were less responsive to treatment. Younger age and race other than white (black, mixed-race, and Asian) were also associated with higher attachment avoidance. Younger women could experience a greater impact on their beliefs regarding trust and comfort in proximity to others after experiencing severe interpersonal trauma. Regarding race, it has been discussed in the literature that differences in attachment might be mediated by socioeconomic status rather than ethnic or racial background (Bakermans-Kranenburg et al., 2004); in Brazil, however, adversities faced by black/mixed-race population also include higher violence exposure, difficulties in accessing healthcare, and other impacts of structural racism (Instituto Brasileiro de Geografia e Estatística (IBGE), 2019; Oliveira et al., 2020; Cerqueira et al., 2021).
It is worth investigating whether attachment avoidance confers an evolutionary advantage to individuals or groups. Social defense theory posits that, in dangerous settings, the sense of security may increase vulnerability by postponing the recognition or reaction to threats, and insecure attachment strategies – either activating the attachment system, as seen in anxiously attached individuals, or deactivating the system, as seen in avoidant individuals – could increase the chances of survival (Ein-Dor et al., 2010). Violence against women is a major health problem in Brazil and worldwide, and enduring this unsafe environment may require adaptive behavior (Mesman et al., 2016). Further research in the mental health and social sciences must explore these hypotheses.
This study has several limitations. Attrition rates were significant: there were almost 30% of actual dropouts, most of them in the first weeks of treatment. Adherence in PTSD studies is challenging, as the symptoms themselves may hinder the patients’ ability to attend treatment; previous evidence has reported that younger age is associated with higher dropout rates in PTSD studies, which is consistent with our findings (Hale et al., 2019). Our evaluation was limited to women who experienced sexual assault and subsequently developed PTSD, excluding those who did not develop PTSD. Thus, our study focused on individuals following trajectories of either disease and recovery or evolution toward chronicity, rather than examining resilience to trauma. Therefore, we were unable to determine whether the attachment pattern found at baseline was affected by an acute PTSD diagnosis, rather than reflecting long-term characteristics. We assessed attachment through a self-report measure; this type of assessment has been extensively used in the field, particularly because of its feasibility over interview measures, although these methods emphasize different phenomena, and their psychometric properties have been questioned (Maunder and Hunter, 2009; Ravitz et al., 2010; Justo-Núñez et al., 2022). It is also possible that the self-reported measures at all time points were affected by the experience of severe interpersonal trauma. Longitudinal studies with representative samples of the Brazilian population may be more suitable for investigating attachment patterns and trajectories across the lifespan.
Another limitation of our study lies in the relatively narrow timeframe, potentially limiting our ability to detect attachment changes. The treatment targeted improvements in PTSD symptoms and not changes in attachment, particularly in the sertraline group, where patients received medication and psychiatric treatment as usual. Nevertheless, short-term interventions in psychotherapy studies, such as CBT for panic disorder (Zalaznik et al., 2019; Lange et al., 2021) and IPT for depression in adolescents and adults (Bernecker et al., 2014; Gunlicks-Stoessel et al., 2017) have shown alterations in attachment. A pilot study of 29 veterans treated for PTSD with IPT observed improvement in separation anxiety symptoms, which can be considered a proxy for insecure attachment (Milrod et al., 2020). Despite our focus on interpersonal relations and social support within the IPT-PTSD treatment group, we could not observe changes in the dimensions of attachment style structure.
One of the biggest strengths of this study is the homogeneity of our sample, particularly considering the trauma type – few PTSD studies with civilian populations have investigated a single type of violence. Research on attachment and PTSD in developing countries is scarce, and this is to our knowledge the first study investigating this association in Brazil. Exploring attachment, rather than limiting it to diagnostic criteria, expands our understanding of the psychological functioning in traumatized individuals. Considering the high rates of urban violence and childhood adversities, further exploration of attachment patterns in the Brazilian population may be crucial for tailoring specific interventions for violence-related disorders.
We assessed anxiety and avoidance dimensions representing attachment styles in adult women undergoing a 14-week PTSD treatment following recent sexual assault. Both IPT-PTSD and sertraline effectively reduced PTSD symptoms; however, attachment avoidance levels increased over time while attachment anxiety remained stable. Our results indicate that difficulties in the interpersonal realm after severe interpersonal trauma should be investigated and addressed independently from the diagnosis, as they may pose a heavy and lasting burden on these women.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Universidade Federal de São Paulo Ethics Comitee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MRM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. VC: Formal analysis, Methodology, Writing – review & editing. CZ: Data curation, Writing – review & editing. MFM: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Visualization, Writing – review & editing. BC: Conceptualization, Formal analysis, Project administration, Supervision, Visualization, Writing – review & editing. AM: Conceptualization, Formal analysis, Funding acquisition, Investigation, Resources, Supervision, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Fundação de Apoio à Pesquisa do Estado de São Paulo (FAPESP), Project number 2014/12559–5; Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), under Grant 303389/2016–8; and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES), Finance Code 001.
The authors wish to thank the individuals who contributed to this project: Bruna Nicoletta, Luciana Porto, Janaína Cruz, Nina Valente, Mary Yeh, Fernando Grecco, Flavia Strumpf, Paula Serafim, Thays Mello, Rosaly Braga (in memorian), Euthymia Prado, Camila Matsuzaka, and Ana Teresa D’Elia, and the staff and participants in the treatment trial.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1325622/full#supplementary-material
Abrahams, N., Devries, K., Watts, C., Pallitto, C., Petzold, M., Shamu, S., et al. (2014). Worldwide prevalence of non-partner sexual violence: a systematic review. Lancet 383, 1648–1654. doi: 10.1016/S0140-6736(13)62243-6
Ainsworth, M. D. S., Blehar, M. C., Waters, E., and Wall, S. (1978). Patterns of attachment: a psychological study of the strange situation Lawrence Erlbaum Associates.
Amorim, P. (2000). Mini International Neuropsychiatric Interview (MINI): validação de entrevista breve para diagnóstico de transtornos mentais. Rev. Bras. Psiquiatr. 22, 106–115. doi: 10.1590/S1516-44462000000300003
Bachem, R., Levin, Y., and Solomon, Z. (2019). Trajectories of attachment in older age: interpersonal trauma and its consequences. Attach Hum. Dev. 21, 352–371. doi: 10.1080/14616734.2018.1479871
Bakermans-Kranenburg, M. J., Van IJzendoorn, M. H., and Kroonenberg, P. M. (2004). Differences in attachment security between African American and white children: ethnicity or socio-economic status? Infant Behav. Dev. 27, 417–433. doi: 10.1016/j.infbeh.2004.02.002
Bakermans-Kranenburg, M. J., and van IJzendoorn, M. H. (2009). The first 10,000 adult attachment interviews: distributions of adult attachment representations in clinical and non-clinical groups. Attach Hum. Dev. 11, 223–263. doi: 10.1080/14616730902814762
Bernecker, S. L., Constantino, M. J., Pazzaglia, A. M., Ravitz, P., and Mcbride, C. (2014). Patient interpersonal and cognitive changes and their relation to outcome in interpersonal psychotherapy for depression. J. Clin. Psychol. 70, 518–527. doi: 10.1002/jclp.22038
Bernstein, D. P., Fink, L., Handeisman, L., Foote, J., Lovejoy, M., Wenzel, K., et al. (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am. J. Psychiatr. 151, 1132–1136. doi: 10.1176/ajp.151.8.1132
Bretherton, I. (1992). The origins of attachment theory: John Bowlby and Mary Ainsworth. Dev. Psychol. 28, 759–775. doi: 10.1037/0012-1649.28.5.759
Brewin, C. R., Andrews, B., and Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 68, 748–766. doi: 10.1037/0022-006X.68.5.748
Bruno, J., Machado, J., Ferreira, Y., Munsch, L., Silès, J., Steinmetz, T., et al. (2019). Impact of attachment styles in the development of traumatic symptoms in French women victims of sexual violence. Sexologies. 28, 25–30. doi: 10.1016/j.sexol.2018.04.005
Bueno, S., Bohnenberger, M., Martins, J., and Sobral, I. (2023). “A explosão da violência sexual no Brasil” in 17o Anuário Brasileiro de Segurança Pública (São Paulo: Fórum Brasileiro de Segurança Pública), 154–161.
Castro-Vale, I., Severo, M., Carvalho, D., and Mota-Cardoso, R. (2020). Vulnerability factors associated with lifetime posttraumatic stress disorder among veterans 40 years after war. Healthcare 8 359, 1–13. doi: 10.3390/healthcare8040359
Cerqueira, D., Ferreira, H., Bueno, S., Palmieri Alves, P., Sérgio de Lima, R., Marques, D., et al. (2021). Atlas da Violência 2021. Relatório Institucional 1–104, 1–104. doi: 10.38116/riatlasdaviolencia2021
Chopik, W. J., Edelstein, R. S., and Grimm, K. J. (2019). Longitudinal changes in attachment orientation over a 59-year period. J. Pers. Soc. Psychol. 116, 598–611. doi: 10.1037/pspp0000167
Clark, A. A., and Owens, G. P. (2012). Attachment, personality characteristics, and posttraumatic stress disorder in U.S. Veterans of Iraq and Afghanistan. J Trauma Stress. 25, 657–664. doi: 10.1002/jts.21760
Coimbra, B. M., Yeh, M., D’Elia, A. T., Maciel, M. R., Carvalho, C. M., Milani, A. C., et al. (2020). Posttraumatic stress disorder and neuroprogression in women following sexual assault: protocol for a randomized clinical trial evaluating allostatic load and aging process acceleration. JMIR Res Protoc 9:e19162. doi: 10.2196/19162
Collins, N. L. (1996). Working models of attachment: implications for explanation, emotion, and behavior. J. Pers. Soc. Psychol. 71, 810–832. doi: 10.1037/0022-3514.71.4.810
Collins, N. L., and Read, S. J. (1990). Adult attachment, working models, and relationship quality in dating couples. J. Pers. Soc. Psychol. 58, 644–663. doi: 10.1037/0022-3514.58.4.644
Coyne, A. E., Constantino, M. J., Ravitz, P., and McBride, C. (2018). The interactive effect of patient attachment and social support on early alliance quality in interpersonal psychotherapy. J. Psychother. Integr. 28, 46–59. doi: 10.1037/int0000074
Darling Rasmussen, P., Storebø, O. J., Løkkeholt, T., Voss, L. G., Shmueli-Goetz, Y., Bojesen, A. B., et al. (2019). Attachment as a Core feature of resilience: a systematic review and Meta-analysis. Psychol. Rep. 122, 1259–1296. doi: 10.1177/0033294118785577
Diamond, D., Keefe, J. R., Hörz-Sagstetter, S., Fischer-Kern, M., Doering, S., and Buchheim, A. (2023). Changes in attachment representation and personality Organization in Transference-Focused Psychotherapy. Am. J. Psychother. 76, 31–38. doi: 10.1176/appi.psychotherapy.20220018
Dworkin, E. R., Menon, S. V., Bystrynski, J., and Allen, N. E. (2017). Sexual assault victimization and psychopathology: a review and meta-analysis. Clin. Psychol. Rev. 56, 65–81. doi: 10.1016/j.cpr.2017.06.002
Egeland, B., and Sroufe, L. A. (1981). Attachment and early maltreatment. Child Dev. 52:44. doi: 10.2307/1129213
Ehrlich, K. B., Yu, T., Sadiq, A., and Brody, G. H. (2022). Neighborhood poverty, allostatic load, and changes in cellular aging in African American young adults: the moderating role of attachment. Attach Hum. Dev. 24, 339–352. doi: 10.1080/14616734.2021.1976934
Ein-Dor, T., Mikulincer, M., Doron, G., and Shaver, P. R. (2010). The attachment paradox: how can so many of us (the insecure ones) have no adaptive advantages? Perspect. Psychol. Sci. 5, 123–141. doi: 10.1177/1745691610362349
Elklit, A., and Christiansen, D. M. (2013). Risk factors for posttraumatic stress disorder in female help-seeking victims of sexual assault. Violence Vict. 28, 552–568. doi: 10.1891/0886-6708.09-135
Elliott, D. M., Mok, D. S., and Briere, J. (2004). Adult sexual assault: prevalence, symptomatology, and sex differences in the general population. J. Trauma. Stress. 17, 203–211. doi: 10.1023/B:JOTS.0000029263.11104.23
Ensink, K., Begin, M., Normandin, L., Biberdzic, M., Vohl, G., and Fonagy, P. (2016). Maternal reflective functioning and child internalising and externalising difficulties in the context of child sexual abuse. Le fonctionnement reflexif maternel et les symptomes interiorises et exteriorises d’enfants victimes d’une agression sexuelle. 7, 117–133. doi: 10.3402/ejpt.v7.30611
Ferrajão, P. (2022). Attachment mediates the impact of previous trauma on posttraumatic symptoms during the COVID-19 pandemic. Psychol. Trauma. Advance online publication. doi: 10.1037/tra0001312
Fonagy, P., Leigh, T., Steele, M., Steele, H., Kennedy, R., Mattoon, G., et al. (1996). The relation of attachment status, psychiatric classification, and response to psychotherapy. J. Consult. Clin. Psychol. 64, 22–31. doi: 10.1037/0022-006X.64.1.22
Forbes, D., Parslow, R., Fletcher, S., McHugh, T., and Creamer, M. (2010). Attachment style in the prediction of recovery following group treatment of combat veterans with post-traumatic stress disorder. J. Nerv. Ment. Dis. 198, 881–884. doi: 10.1097/NMD.0b013e3181fe73fa
Franz, C. E., Lyons, M. J., Spoon, K. M., Hauger, R. L., Jacobson, K. C., Lohr, J. B., et al. (2014). Post-traumatic stress symptoms and adult attachment: a 24-year longitudinal study. Am. J. Geriatr. Psychiatry 22, 1603–1612. doi: 10.1016/j.jagp.2014.02.003
Grassi-Oliveira, R., Stein, L. M., and Pezzi, J. C. (2006). Tradução e validação de conteúdo da versão em português do Childhood Trauma Questionnaire. Rev. Saude Publica 40, 249–255. doi: 10.1590/S0034-89102006000200010
Griffin, D. W., and Bartholomew, K. (1994). Models of the self and other: fundamental dimensions underlying measures of adult attachment. J. Pers. Soc. Psychol. 67, 430–445. doi: 10.1037/0022-3514.67.3.430
Gunlicks-Stoessel, M., Westervelt, A., Reigstad, K., Mufson, L., and Lee, S. (2017). The role of attachment style in interpersonal psychotherapy for depressed adolescents. Psychother. Res. 29, 78–85. doi: 10.1080/10503307.2017.1315465
Hale, A. C., Bohnert, K. M., Ganoczy, D., and Sripada, R. K. (2019). Predictors of treatment adequacy during evidence-based psychotherapy for PTSD. Psychiatr. Serv. 70, 367–373. doi: 10.1176/appi.ps.201800361
Hazan, C., and Shaver, P. (1987). Romantic love conceptualized as an attachment process. J. Pers. Soc. Psychol. 52, 511–524. doi: 10.1037/0022-3514.52.3.511
Instituto Brasileiro de Geografia e Estatística (IBGE) (2019).VDesigualdades sociais por cor ou raça no Brasil. Estudos e Pesquisas - Informação Demográfica e Socioeconômican. Rio de Janeiro. 41, 1–12. ISBN 978-85-240-4513-4
Jittayuthd, S., and Karl, A. (2022). Rejection sensitivity and vulnerable attachment: associations with social support and PTSD symptoms in trauma survivors. Eur. J. Psychotraumatol. 13:2027676. doi: 10.1080/20008198.2022.2027676
Justo-Núñez, M., Morris, L., and Berry, K. (2022). Self-report measures of secure attachment in adulthood: a systematic review. Clin. Psychol. Psychother. 29, 1812–1842. doi: 10.1002/cpp.2756
Kazmierski, K. F. M., Borelli, J. L., and Rao, U. (2023). Multidimensional discrimination distress, controlling parenting, and parent–adolescent attachment relationships: racial/ethnic differences. J. Soc. Issues 79, 334–359. doi: 10.1111/josi.12525
Kinley, J. L., and Reyno, S. M. (2013). Attachment style changes following intensive short-term group psychotherapy. Int. J. Group Psychother. 63, 53–75. doi: 10.1521/ijgp.2013.63.1.53
Konrath, S. H., Chopik, W. J., Hsing, C. K., and O’Brien, E. (2014). Changes in adult attachment styles in American college students over time. Personal. Soc. Psychol. Rev. 18, 326–348. doi: 10.1177/1088868314530516
Lahav, Y., and Elklit, A. (2016). The cycle of healing - dissociation and attachment during treatment of CSA survivors. Child Abuse Negl. 60, 67–76. doi: 10.1016/j.chiabu.2016.09.009
Lake, A. M., Goleva, S. B., Samuels, L. R., Carpenter, L. M., and Davis, L. K. (2022). Sex differences in health conditions associated with sexual assault in a large hospital population. Complex Psychiatry 8, 80–89. doi: 10.1159/000527363
Lange, J., Goerigk, S., Nowak, K., Rosner, R., and Erhardt, A. (2021). Attachment style change and working Alliance in panic disorder patients treated with cognitive behavioral therapy. Psychotherapy 58, 206–218. doi: 10.1037/pst0000365
LeBeau, R., Mischel, E., Resnick, H., Kilpatrick, D., Friedman, M., and Craske, M. (2014). Dimensional assessment of posttraumatic stress disorder in DSM-5. Psychiatry Res. 218, 143–147. doi: 10.1016/j.psychres.2014.03.032
Levy, K. N., Ellison, W. D., Scott, L. N., and Bernecker, S. L. (2011). Attachment style. J. Clin. Psychol. 67, 193–203. doi: 10.1002/jclp.20756
Lim, B. H., Adams, L. A., and Lilly, M. M. (2012). Self-worth as a mediator between attachment and posttraumatic stress in interpersonal trauma. J. Interpers. Violence 27, 2039–2061. doi: 10.1177/0886260511431440
Lipsitz, J. D., and Markowitz, J. C. (2013). Mechanisms of change in interpersonal therapy (IPT). Clin. Psychol. Rev. 33, 1134–1147. doi: 10.1016/j.cpr.2013.09.002
Marshall, E. M., and Frazier, P. A. (2019). Understanding posttrauma reactions within an attachment theory framework. Curr Opin Psychol. 25, 167–171. doi: 10.1016/j.copsyc.2018.08.001
Markowitz, J. C. (2016). Interpersonal psychotherapy for posttraumatic stress disorder. New York: Oxford University Press.
Maunder, R. G., and Hunter, J. J. (2009). Assessing patterns of adult attachment in medical patients. Gen. Hosp. Psychiatry 31, 123–130. doi: 10.1016/j.genhosppsych.2008.10.007
Mesman, J., Van Ijzendoorn, M. H., and Sagi-Schwartz, A. (2016). “Cross-cultural patterns of attachment: universal and cultural dimensions” in Handbook of attachment: theory, research, and clinical applications. eds. J. Cassidy and P. Shaver (New York: The Guilford Press), 852–853.
Mickelson, K. D., Kessler, R. C., and Shaver, P. R. (1997). Adult attachment in a nationally representative sample. J. Pers. Soc. Psychol. 73, 1092–1106. doi: 10.1037/0022-3514.73.5.1092
Mikulincer, M., and Shaver, P. R. (2012). An attachment perspective on psychopathology. World Psychiatry 11, 11–15. doi: 10.1016/j.wpsyc.2012.01.003
Assche, L.Van, Luyten, P., Bruffaerts, R., Persoons, P., van de Ven, L., and Vandenbulcke, M. (2013). Attachment in old age: theoretical assumptions, empirical findings and implications for clinical practice. Clin. Psychol. Rev. 33, 67–81. doi: 10.1016/j.cpr.2012.10.003
Mikulincer, M., and Shaver, P. R. (2016). Attachment in adulthood: structure, dynamics, and change. New York and London: The Guilford Press.
Mikulincer, M., Shaver, P. R., and Solomon, Z. (2015). “An attachment perspective on traumatic and posttraumatic reactions” in Future directions in post-traumatic stress disorder prevention, diagnosis, and treatment. eds. M. P. Safir, H. S. Wallach, and A. S. Rizzo (New York: Springer), 79–96.
Mikulincer, M., Solomon, Z., Shaver, P. R., and Ein-Dor, T. (2014). Attachment-related consequences of war captivity and trajectories of posttraumatic stress disorder: a 17-year longitudinal study. J. Soc. Clin. Psychol. 33, 207–228. doi: 10.1521/jscp.2014.33.3.207
Milrod, B., Keefe, J. R., Choo, T., Arnon, S., Such, S., Lowell, A., et al. (2020). Separation anxiety in PTSD: a pilot study of mechanisms in patients undergoing IPT. Depress. Anxiety 37, 386–395. doi: 10.1002/da.23003
Möller, A. T., Bäckström, T., Söndergaard, H. P., and Helström, L. (2014). Identifying risk factors for PTSD in women seeking medical help after rape. PLoS One 9, 1–9. doi: 10.1371/journal.pone.0111136
Muller, R. T., and Rosenkranz, S. E. (2009). Attachment and treatment response among adults in inpatient treatment for posttraumatic stress disorder. Psychotherapy: theory. Research, Practice, Training 46, 82–96. doi: 10.1037/a0015137
Oliveira, R. G. de, Cunha, A. P. da, Gadelha, A. G., dos, S., Carpio, C. G., Oliveira, R. B., et al. (2020). Desigualdades raciais e a morte como horizonte: considerações sobre a COVID-19 e o racismo estrutural. Cad Saude Publica 36, 1–14. doi: 10.1590/0102-311x000150120
Oliveira-Watanabe, T. T., Ramos-Lima, L. F., Zylberstajn, C., Calsavara, V., Coimbra, B. M., Maciel, M. R., et al. (2021). Validation of the Brazilian-Portuguese version of the clinician administered post traumatic stress disorder Scale-5. Front. Psych. 12:614735. doi: 10.3389/fpsyt.2021.614735
Pace, C. S., Di Folco, S., Guerriero, V., and Muzi, S. (2019). Late-adopted children grown up: a long-term longitudinal study on attachment patterns of adolescent adoptees and their adoptive mothers. Attach Hum. Dev. 21, 372–388. doi: 10.1080/14616734.2019.1571519
Pinquart, M., Feußner, C., and Ahnert, L. (2013). Meta-analytic evidence for stability in attachments from infancy to early adulthood. Attach Hum. Dev. 15, 189–218. doi: 10.1080/14616734.2013.746257
Proença, C. R., Markowitz, J. C., Coimbra, B. M., Cogo-Moreira, H., Maciel, M. R., Mello, A. F., et al. (2022). Interpersonal psychotherapy versus sertraline for women with posttraumatic stress disorder following recent sexual assault: a randomized clinical trial. Eur. J. Psychotraumatol. 13:1–14. doi: 10.1080/20008066.2022.2127474
R Core Team (2020). R: A language and environment for statistical computing. Vienna, Austria: R Development Core Team.
Ravitz, P., Maunder, R., Hunter, J., Sthankiya, B., and Lancee, W. (2010). Adult attachment measures: a 25-year review. J. Psychosom. Res. 69, 419–432. doi: 10.1016/j.jpsychores.2009.08.006
Ravitz, P., Maunder, R., and McBride, C. (2008). Attachment, contemporary interpersonal theory and IPT: an integration of theoretical, clinical, and empirical perspectives. J. Contemp. Psychother. 38, 11–21. doi: 10.1007/s10879-007-9064-y
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., et al. (1998). The Mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry. 59, 34–57.
Slade, A., and Holmes, J. (2019). Attachment and psychotherapy. Curr. Opin. Psychol. 25, 152–156. doi: 10.1016/j.copsyc.2018.06.008
Soares, A. L. G., Howe, L. D., Matijasevich, A., Wehrmeister, F. C., Menezes, A. M. B., and Gonçalves, H. (2016). Adverse childhood experiences: prevalence and related factors in adolescents of a Brazilian birth cohort. Child Abuse Negl. 51, 21–30. doi: 10.1016/j.chiabu.2015.11.017
Sroufe, L. A. (2005). Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach Hum. Dev. 7, 349–367. doi: 10.1080/14616730500365928
Sroufe, L. A., and Waters, E. (1977). Attachment as an organizational construct. Child Dev. 48:1184. doi: 10.2307/1128475
Stea, T., Steigen, A., Dangmann, C., Granrud, M., and Bonsaksen, T. (2023). Associations between exposure to sexual abuse, substance use, adverse health outcomes, and use of youth health services among Norwegian adolescents. BMC Public Health 23:1330. doi: 10.1186/s12889-023-16261-y
Steenkamp, M. M., Dickstein, B. D., Salters-Pedneault, K., Hofmann, S. G., and Litz, B. T. (2012). Trajectories of PTSD symptoms following sexual assault: is resilience the modal outcome? J. Trauma. Stress. 25, 469–474. doi: 10.1002/jts.21718
Tamman, A. J. F., Wendt, F. R., Pathak, G. A., Krystal, J. H., Montalvo-Ortiz, J. L., Southwick, S. M., et al. (2021). Attachment style moderates polygenic risk for posttraumatic stress in United States military veterans: results from the National Health and resilience in veterans study. Biol. Psychiatry 89, 878–887. doi: 10.1016/j.biopsych.2020.09.018
Teixeira, R. C. R., Ferreira, J. H. B. P., and Howat-Rodrigues, A. B. C. (2019). Collins and Read revised adult attachment scale (RAAS) validity evidence. Psico 50:e29567. doi: 10.15448/1980-8623.2019.2.29567
Travis, L. A., Bliwise, N. G., Binder, J. L., and Horne-Moyer, H. L. (2001). Changes in clients’ attachment styles over the course of time-limited dynamic psychotherapy. Psychotherapy: theory. Research, Practice, Training 38, 149–159. doi: 10.1037/0033-3204.38.2.149
Waters, E., Merrick, S., Treboux, D., Crowell, J., and Albersheim, L. (2000). Attachment security in infancy and early adulthood: a twenty-year longitudinal study. Child Dev. 71, 684–689. doi: 10.1111/1467-8624.00176
Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., et al. (2018). The clinician-administered PTSD scale for DSM–5 (CAPS-5): development and initial psychometric evaluation in military veterans. Psychol. Assess. 30, 383–395. doi: 10.1037/pas0000486
Weinfield, N. S., Sroufe, L. A., and Egeland, B. (2000). Attachment from infancy to early adulthood in a high-risk sample: continuity, discontinuity, and their correlates. Child Dev. 71, 695–702. doi: 10.1111/1467-8624.00178
Weinfield, N. S., Whaley, G. J. L., and Egeland, B. (2004). Continuity, discontinuity, and coherence in attachment from infancy to late adolescence: sequelae of organization and disorganization. Attach Hum. Dev. 6, 73–97. doi: 10.1080/14616730310001659566
Woodhouse, S., Ayers, S., and Field, A. P. (2015). The relationship between adult attachment style and post-traumatic stress symptoms: a meta-analysis. J. Anxiety Disord. 35, 103–117. doi: 10.1016/j.janxdis.2015.07.002
World Health Organization (2021). Violence against women prevalence estimates, 2018: global, regional and national prevalence estimates for intimate partner violence against women and global and regional prevalence estimates for non-partner sexual violence against women. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO.
Yehuda, R., Hoge, C. W., McFarlane, A. C., Vermetten, E., Lanius, P. P., Nievergelt, C. M., et al. (2015). Post-traumatic stress disorder. Nat Rev Dis Primers 1. 15057, 1–22. doi: 10.1038/nrdp.2015.57
Zalaznik, D., Weiss, M., and Huppert, J. D. (2019). Improvement in adult anxious and avoidant attachment during cognitive behavioral therapy for panic disorder. Psychother. Res. 29, 337–353. doi: 10.1080/10503307.2017.1365183
Keywords: post-traumatic stress disorder, attachment, interpersonal psychotherapy, treatment, sexual assault
Citation: Maciel MR, Calsavara VF, Zylberstajn C, Mello MF, Coimbra BM and Mello AF (2023) Changes in attachment dimensions during the treatment of acute post-traumatic stress disorder in sexually assaulted Brazilian women. Front. Psychol. 14:1325622. doi: 10.3389/fpsyg.2023.1325622
Received: 23 October 2023; Accepted: 23 November 2023;
Published: 07 December 2023.
Edited by:
Pia Tohme, Lebanese American University, LebanonReviewed by:
Hady Naal, American University of Beirut, LebanonCopyright © 2023 Maciel, Calsavara, Zylberstajn, Mello, Coimbra and Mello. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mariana Rangel Maciel, bWFyaWFuYXJtYWNpZWxAZ21haWwuY29t
†ORCID: Mariana Rangel Maciel https://orcid.org/0000-0002-1428-3553
Vinicius Fernando Calsavara https://orcid.org/0000-0003-2332-5863
Cecilia Zylberstajn https://orcid.org/0000-0002-3906-9641
Marcelo Feijo Mello https://orcid.org/0000-0002-0475-4729
Bruno Messina Coimbra https://orcid.org/0000-0001-5092-9625
Andrea Feijo Mello https://orcid.org/0000-0001-8498-7751
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.