
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Psychol., 01 December 2023
Sec. Mindfulness
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1287891
Objective: This study aimed to evaluate the effects of self-help mindfulness-based cognitive therapy (MBCT-SH) on mindfulness, symptom change, and suicidal ideation in patients with depression.
Methods: For this randomized controlled study, 97 patients were randomly assigned to either the MBCT-SH (n = 48) or control (n = 49) group. The Five Facet Mindfulness Questionnaire (FFMQ), Hamilton Depression Rating Scale (HAMD-24), and Suicide Attitude Questionnaire (SAQ) were used to assess mindfulness, depression symptoms, and suicidal ideation, respectively, at baseline (T0), intervention week 4 (T1), intervention week 8 (T2), and 3-month follow-up (T3). The groups were also compared on treatment costs and readmission rates at a 6-month follow-up.
Results: In the MBCT-SH group, 46 of 48 participants (96%) completed the eight-week program. At T0, there were no statistically significant between-group differences in demographics, clinical characteristics, FFMQ, HAMD-24, or SAQ. Nor were there statistically significant differences on the HAMD-24 or SAQ between the MBCT-SH and control groups at T1 (p = 0.18 and p = 0.59, respectively), while mindfulness was significantly higher in the MBCT-SH group (t = 2.383, p = 0.019). At T2, there were significant between-group differences on the FFMQ, HAMD-24, and SAQ, all of which remained significant at T3. At the 6-month follow-up, per capita treatment costs were 5,298 RMB lower in the MBCT-SH group compared with the control group, while their readmission rates (6.1% and 4.2%, respectively) did not differ significantly.
Conclusion: These findings support the feasibility and effectiveness of MBCT-SH among patients with depression.
Clinical trial registration: http://www.chictr.org.cn, ChiCTR2300077850.
Depression is a mental illness characterized by low mood, sadness, and a sense of emptiness (American Psychiatric Association, 1980) that affects about 280 million people worldwide (Ortega et al., 2022) and contributes greatly to the global disease burden. In China, the lifetime prevalence of depression is 6.9%, and the 12-month prevalence is 3.6% (Huang et al., 2019). Depression is distinct from typical mood fluctuations and short-term emotional responses to everyday challenges. Especially when recurrent, moderate or severe depression can become a serious health issue that causes patient suffering and impacts their work, school and relationship functioning.
At its worst, depression can lead to suicide. Among completed suicides, 43–50% can be attributed to depression (Slama et al., 2011), and depression causes one of the highest suicide rates among psychiatric disorders. These patients see suicidal behavior as a solution, to escape psychological pain (Campos et al., 2017). Clinical depression treatment focuses primarily on pharmacotherapy, which can improve clinical symptoms and reduce suicide incidence. Yet suicide risk may remain during antidepressant treatment, and some patients have residual symptoms; thus, there are limitations to single drug therapy (Yuan et al., 2020). In recent years, patients with depression have also benefited from concurrent physical therapy and psychotherapy. However, even with a variety of treatments, some patients have persistent symptoms and do not fully recover (Pigott et al., 2010). Therefore, optimal depression treatments still need to be explored.
Mindfulness-based cognitive therapy (MBCT) was first proposed in 2003 (Morgan, 2003) as a novel approach to preventing depression relapse. MBCT is typically an eight-week group intervention of mindfulness-based stress reduction and cognitive behavioral therapy (Wright and Beck, 1983; Kabat-Zinn, 1990). Multiple studies have shown that MBCT can significantly reduce both current depression symptoms and relapse risk and related symptoms in patients who are in remission from depression (Cladder-Micus et al., 2018; Zemestani and Fazeli, 2020; Wang et al., 2022). While MBCT can be beneficial for depression recovery, several factors have limited its implementation. First, available space can limit group size. Second, time demands can reduce participation rates. Third, intensive face-to-face training may increase negative emotions in patients with depression. Thus, novel ways to address these limitations, and facilitate more patients with depression who can benefit from MBCT, are needed.
Self-help MBCT (MBCT-SH) is an internet-based intervention in which participants conduct self-help mindfulness training with a mobile device (e.g., smartphone, computer) and audio-visual materials. While self-help mindfulness interventions have been confirmed as efficacious (Zernicke et al., 2013; Lever Taylor et al., 2014; Kvillemo et al., 2016), and online MBCT-SH is attracting increasing attention, it is still in the exploratory stage. Few studies have evaluated the effectiveness of MBCT-SH in patients with depression. As such, the aim of this randomized controlled study was to determine the effects of MBCT-SH on mindfulness, symptom change, and suicidal ideation in patients with depression.
As illustrated by Figure 1, for this randomized controlled trial comparing MBCT-SH and control groups of Chinese patients with depression, participants were assessed at baseline (T0), intervention week 4 (T1), intervention week 8 (T2), and 3-month follow-up (T3).
Power was calculated using G*Power (Faul et al., 2007); with p = 0.05 and power 80%, 86 participants were needed to detect effect sizes comparable to those reported in a similar mindfulness-based intervention study (Perez-Blasco et al., 2013). Accounting for a potential 10% attrition during follow-up, we sought to include at least 95 participants.
Inclusion criteria were: depression diagnosis based on associate chief- and psychiatrist-evaluated DSM-IV diagnostic criteria, through administration of the Chinese version of the mini international neuropsychiatric interview; age 18–60 years; total Hamilton Depression Rating Scale (HAMD-24) score ≥ 8; ability to communicate in Chinese; normal reading and communication abilities; able to sign written informed consent.
Exclusion criteria were: meeting the DSM-IV Axis I disorder diagnostic criteria for another psychiatric disorder; suffering from a severe physical disease, central nervous system disease, or substance abuse; inability to use a smartphone or computer; already regularly practice mindfulness meditation.
Participants were recruited from the psychological counseling clinic, psychiatry clinic, and psychiatric inpatient department at the Second Affiliated Hospital of Guangxi Medical University. Potential participants were informed about the study and signed informed consent. The study was conducted from June 2021 to December 2022.
Participants were randomly assigned at a 1:1 ratio to either the MBCT-SH or control group. Patients in both groups received conventional therapy; patients in the MBCT-SH group also received the eight-week MBCT-SH program.
The intervention was implemented according to the translated MBCT manual for depression (Morgan, 2003). Prior to training, participants in the MBCT-SH group were trained in the use of mindfulness exercises, including the participant manual and MBCT audio exercises. The participant manual included the MBCT definition, weekly training schedule, exercise instructions, and information about commitment to the training program. MBCT-SH group participants were also trained to use the audio and manual by MBCT-certified instructors with extensive experience in mindfulness training.
Participants were encouraged to practice 30–45 min daily, 3–5 days per week. The eight-week MBCT-SH program is shown in Table 1. A researcher also introduced the daily training content and following week’s training project through a WeChat group every Monday. Participants needed to be willing to record and share their feelings about the program through WeChat, email, or phone.
Control group participants received conventional therapy only. They were disallowed from participating in any type of mindfulness program during the study. They were invited to attend the MBCT-SH program upon completion of their study participation.
The HAMD-24, developed by Hamilton in 1960 (Hamilton, 1960), is widely used to evaluate depression symptom severity in adults. The 24 items are each rated on a four-point scale, and total scores are interpreted as follows: ≤7, no depression; >8 to ≤20, mild depression; >20 to ≤35, moderate depression; and > 35, severe depression.
The Suicide Attitude Questionnaire (SAQ), developed by Xiao et al. (1999), is used to evaluate attitudes and views towards suicide. The scale consists of four dimensions: understanding the nature of suicidal behavior; attitude toward suicide; attitude toward the family of the suicide; and attitude toward euthanasia. SAQ scores are interpreted as follows: ≤2.5, positive attitude toward suicide; >2.5 to <3.5, ambivalence or neutrality; and ≥ 3.5, negative attitude toward suicide.
The Five Facet Mindfulness Questionnaire (FFMQ), developed by Baer et al. (2006), includes: observing; describing; non-judging of inner experience; acting with awareness; and non-reactivity to inner experience. Each of the 39 items are rated on a five-point scale.
SPSS 24.0 software was used for data analyses. Descriptive statistics are used to describe the participant characteristics and assess levels of depression, suicide attitude, and mindfulness. Continuous variables were analyzed by t-test and categorical variables by χ2 test, to test for between-group differences at T0. Between-group comparison measures were first assessed for normality. Data conforming to the normal distribution were tested by independent samples t-tests. Paired samples t-tests were used to compare within-groups, and repeated measures ANOVAs were used to test for changes in indices. p < 0.05 was considered statistically significant.
Ninety-seven of 105 potential participants signed informed consent and 8 were excluded. The 97 participants were randomized to the MBCT-SH (n = 48) or control (n = 49) group.
The average participant age was 30.06 (standard deviation [SD] = 11.82) years. The participants were overwhelmingly female, and more than half were college-educated. Most had moderate depression. At T0, there were no statistically significant between-groups differences in demographic or clinical characteristics (Table 2).
As shown in Figure 2 and Table 3, repeated measures ANOVA showed significant main FFMQ effects of group (F = 7.905, p = 0.006) and time (F = 30.054, p < 0.001). There was also a significant interaction between group and time (F = 16.657, p < 0.001). Therefore, simple effects analyses were carried out, comparing groups based on time. There was not a significant between-groups difference at T0, indicating comparability at baseline. However, between-groups differences at T1, T2, and T3 were statistically significant, with higher MBCT-SH group scores compared with control group scores. Within-group comparisons showed that the MBCT-SH group differed significantly between T1, T2, and T3 compared with T0, and between T1 and T3 compared with T2. The control group did not differ significantly across any time points.
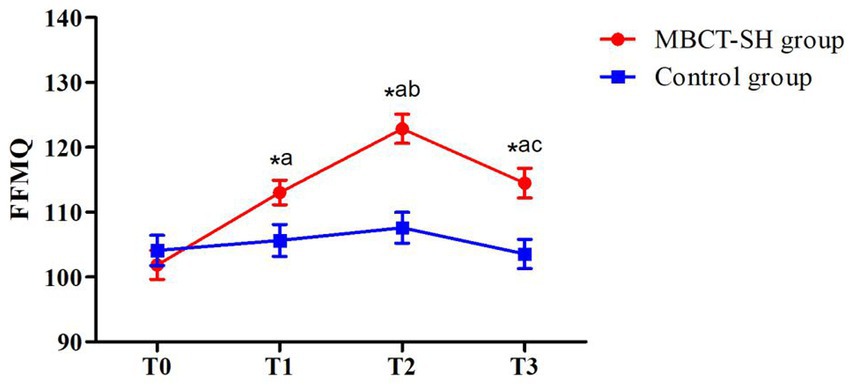
Figure 2. Mean FFMQ scores from T0 to T3 in MBCT-SH and control groups. ap < 0.05 vs. T0; bp < 0.05 vs. T1; cp < 0.05 vs. T2; FFMQ, five-facets of mindfulness.
There were significant HAMD-24 score difference effects for group (F = 11.011, p = 0.001) and time (F = 36.812, p<0.001). There was also an interaction between group and time (F = 15.050, p<0.001). Therefore, simple effects analyses were conducted, comparing between-group on time. As shown in Figure 3 and Table 4, there was no significant between-groups difference at T0, indicating that the groups were comparable. Nor was there a significant between-groups difference at T1. At T2 and T3, MBCT-SH group scores were significantly lower compared with the control group. Within-groups comparisons showed that the MBCT-SH group had significant differences between T1, T2, and T3 compared with T0, and between T2 and T3 compared with T1. There were no significant control group differences across any time points.
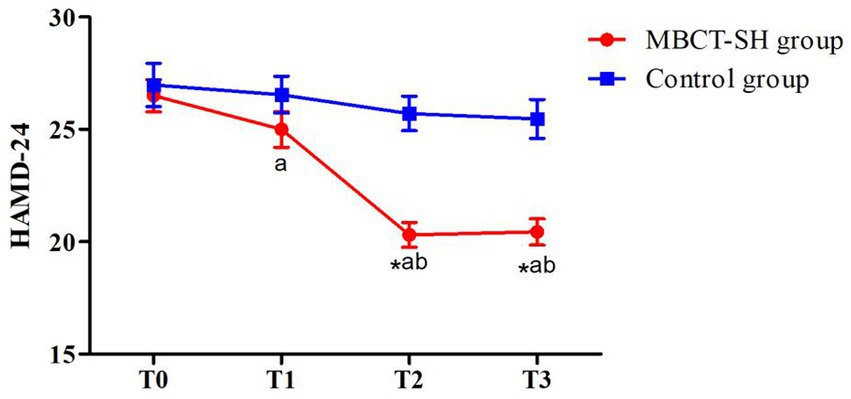
Figure 3. Mean HAMD-24 scores from T0 to T3 in MBCT-SH and control groups. ap < 0.05 vs. T0; bp < 0.05 vs. T1; cp < 0.05 vs. T2; HAMD-24, Hamilton depression scale-24.
As shown in Figure 4 and Table 5, repeated measures ANOVA showed significant main SAQ effects for group (F = 3.433, p = 0.067) and time (F = 8.937, p < 0.001). There was also an interaction between group and time (F = 7.968, p < 0.001). Therefore, simple effects analyses were carried out, comparing between groups based on the time factor. There was not a significant between-groups difference at T0, indicating that the groups were comparable at baseline. Nor was there a significant between-groups difference at T1. However, the groups differed significantly at T2 and T3, when MBCT-SH group scores were significantly lower compared with the control group. Within-group comparisons showed that the MBCT-SH group differed significantly at T2 and T3 compared with T0, and between T2 and T3 compared with T1. The control group showed no significant differences across time points.
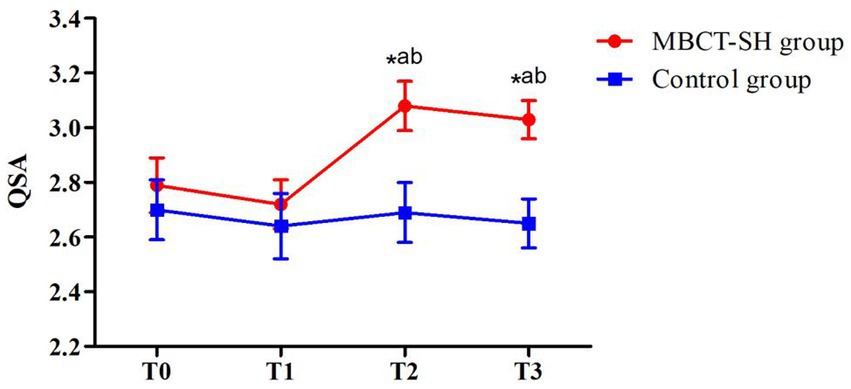
Figure 4. Mean SAQ scores from T0 to T3 in MBCT-SH and control groups. ap < 0.05 vs. T0; bp < 0.05 vs. T1; cp < 0.05 vs. T2; SAQ, suicide attitude questionnaire.
We also compared treatment costs and readmission rates between the groups at a 6-month follow-up. At that time, per capita treatment costs were 5,298 RMB lower in the MBCT-SH group compared with the control group. MBCT-SH and control group readmission rates, 6.1% and 4.2%, respectively, did not differ significantly (p > 0.05).
Previous studies (Zhang et al., 2018; Yu et al., 2019) have shown that traditional MBCT intervention training reduces non-inpatient enthusiasm and compliance, because of inflexible meeting times and locations. This study tested a novel self-help internet-based MBCT training program, in which patients could flexibly adjust training content and timing according to their needs, and without affecting their daily life. Self-help training can also reduce patient financial burden by lowering treatment costs, transportation costs, lost income, and other expenses.
Herein, 46 of 48 participants (96%) completed both the four-week MBCT self-help program and eight-week follow-up. Participants also showed a high level of adherence to MBCT-SH, similar to traditional MBCT (Cavanagh et al., 2013). Participants herein actively accepted MBCT-SH, perhaps due to its accessibility, and possibly because 62.50% of the sample was female. Previous studies have shown that females are more interested in participating in mindfulness training programs (Bränström et al., 2012). To the best of our knowledge, few studies have assessed self-help MBCT in patients with depression. In a similar study of self-help MBCT in students, the participation rate was 95% (Lever Taylor et al., 2014), close to that herein.
Herein, control group participants received conventional therapy, while the MBCT-SH group received an additional eight weeks of MBCT-SH training. As shown in Table 3, MBCT-SH group FFMQ scores were significantly higher than the control group at T1, T2, and T3 (all p < 0.05). Compared with T0, mindfulness in the intervention group increased by mid-intervention (T1) and was higher post-intervention (T2). This indicates that patients with depression can gradually form a stronger sense of mindfulness through MBCT-SH training. Furthermore, longer training leads to stronger mindfulness. Previous studies have shown that mindfulness levels among patients with depression rise significantly after MBCT training (Key et al., 2017; Shenefelt, 2018). However, the levels herein were slightly lower than in similar studies (Kong et al., 2020). This may have been because MBCT herein was self-help rather than traditional, thus participants could independently determine their training intensity and the researcher did not intervene overly.
There were significant between-group HAMD-24 score differences at T1, T2, and T3 (all p < 0.05). After eight weeks of MBCT-SH training, participants’ depression symptoms decreased from moderate to mild. This suggests that MBCT-SH may reduce depression symptoms, similar to traditional MBCT (Joormann and Davanzato, 2010; Peng and Pang, 2018). Our findings also suggest that depression symptom severity and mindfulness are inversely related. A primary psychological characteristic of patients with depression is that they pay excessive attention to negative emotions (Leppänen, 2006). Several studies (Ives-Deliperi et al., 2013; Yang et al., 2016; Lifshitz et al., 2019) have shown that the mechanism by which MBCT improves depressive symptoms is by reducing patient attention to negative emotions through the attention control network system and emotion regulation brain areas. MBCT may both influence brain function and change brain structure (Hölzel et al., 2011). Our findings support the value of MBCT-SH for use by patients with depression.
Mindfulness can inversely predict suicide risk (Mohammadkhani et al., 2015), with higher levels of mindfulness related to lower suicide risk. In other words, mindfulness may have a protective effect by reducing suicide risk (Chesin et al., 2016). Herein, it was interesting that while no significant differences in suicidal ideation were found between the groups at mid-intervention (T1), they differed significantly both post-intervention (T2) and at later follow-up (T3). Dimidjian et al. (2014) found that the longer participants took part in MBCT training, the higher their level of mindfulness became, and the lower their suicidal ideation. Consistent with this, four weeks of MBCT-SH appeared to be insufficient. At mid-intervention, patients with depression appeared to lack sufficient mindfulness levels to reduce suicidal ideation.
Herein, MBCT-SH was effective for improving mindfulness and reducing depression symptoms and suicidal ideation. This effect was most obvious at the end of the full eight-week program and was still observed at the 3-month follow-up. Training simultaneously reduced financial burden among patients with depression.
MBCT-SH herein was an internet-based intervention in which participants self-trained in mindfulness using a mobile device (e.g., smartphone, computer), combined with audio-visual materials. The main differences between MBCT-SH and traditional MBCT are that the former lacks: (1) face-to-face classes; (2) a required specific place and time for practice; and (3) group contact among participants. The advantages of MBCT-SH thus include its lower cost, ease of access to learning content, self-regulation of practice time and space, higher level of relaxation, and independence to choose exercise content. MBCT-SH is not without disadvantages, including that the researcher cannot observe the participant’s learning response and the lack of communication among group members.
There were also several study limitations. First, three follow-up months may have been insufficient; future studies should conduct longer-term follow-up to evaluate the persistence of MBCT-SH effects. Second, the scales used to evaluate the effects of MBCT-SH were quantitative; future studies could incorporate qualitative objectives. Finally, that the sample was exclusively patients with depression may have limited the generalizability of its findings.
MBCT-SH improves mindfulness, depression symptoms, and suicidal ideation in patients with depression.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of the Second affiliated hospital of Guangxi Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
YM: Writing – original draft. ZL: Investigation, Writing – original draft. MC: Data curation, Writing – review & editing. HD: Data curation, Investigation, Writing – review & editing. RL: Project administration, Writing – review & editing. MY: Project administration, Resources, Writing – review & editing. HH: Project administration, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by funds from the Scientific Research Project of Guangxi Health Commission (Z20201402).
We thank the patients who took part in this study. Our sincerest gratitude also to the Mental Health Center of the Second Affiliated Hospital of Guangxi Medical University, China.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
American Psychiatric Association (1980). Diagnostic and statistical manual of mental disorders. Essentials Pain Med 51, 4–8.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., and Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment 13, 27–45. doi: 10.1177/1073191105283504
Bränström, R., Kvillemo, P., and Moskowitz, J. T. (2012). A randomized study of the effects of mindfulness training on psychological well-being and symptoms of stress in patients treated for cancer at 6-month follow-up. Int. J. Behav. Med. 19, 535–542. doi: 10.1007/s12529-011-9192-3
Campos, R. C., Gomes, M., Holden, R. R., Piteira, M., and Rainha, A. (2017). Does psychache mediate the relationship between general distress and suicide ideation? Death Stud. 41, 241–245. doi: 10.1080/07481187.2016.1251510
Cavanagh, K., Strauss, C., Cicconi, F., Griffiths, N., Wyper, A., and Jones, F. (2013). A randomised controlled trial of a brief online mindfulness-based intervention. Behav. Res. Ther. 51, 573–578. doi: 10.1016/j.brat.2013.06.003
Chesin, M., Interian, A., Kline, A., Benjamin-Phillips, C., Latorre, M., and Stanley, B. (2016). Reviewing mindfulness-based interventions for suicidal behavior. Arch. Suicide Res. 20, 507–527. doi: 10.1080/13811118.2016.1162244
Cladder-Micus, M. B., Speckens, A. E. M., Vrijsen, J. N., Donders, T., Becker, E. S., and Spijker, J. (2018). Mindfulness-based cognitive therapy for patients with chronic, treatment-resistant depression: a pragmatic randomized controlled trial. Depress. Anxiety 35, 914–924. doi: 10.1002/da.22788
Dimidjian, S., Beck, A., Felder, J. N., Boggs, J. M., Gallop, R., and Segal, Z. V. (2014). Web-based mindfulness-based cognitive therapy for reducing residual depressive symptoms: an open trial and quasi-experimental comparison to propensity score matched controls. Behav. Res. Ther. 63, 83–89. doi: 10.1016/j.brat.2014.09.004
Faul, F., Erdfelder, E., Lang, A. G., and Buchner, A. (2007). G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. doi: 10.3758/bf03193146
Hamilton, M. (1960). A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. doi: 10.1136/jnnp.23.1.56
Hölzel, B. K., Carmody, J., Vangel, M., Congleton, C., Yerramsetti, S. M., Gard, T., et al. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 191, 36–43. doi: 10.1016/j.pscychresns.2010.08.006
Huang, Y., Wang, Y., Wang, H., Liu, Z., Yu, X., Yan, J., et al. (2019). Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 6, 211–224. doi: 10.1016/S2215-0366(18)30511-X
Ives-Deliperi, V. L., Howells, F., Stein, D. J., Meintjes, E. M., and Horn, N. (2013). The effects of mindfulness-based cognitive therapy in patients with bipolar disorder: a controlled functional MRI investigation. J. Affect. Disord. 150, 1152–1157. doi: 10.1016/j.jad.2013.05.074
Joormann, J., and Davanzato, C. (2010). Emotion regulation in depression: examining the role of cognitive processes. Cognit. Emot. 24, 913–939. doi: 10.1080/02699931003784939
Kabat-Zinn, J. (1990). Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. NY: Delacorte.
Key, B. L., Rowa, K., Bieling, P., McCabe, R., and Pawluk, E. J. (2017). Mindfulness-based cognitive therapy as an augmentation treatment for obsessive-compulsive disorder. Clin. Psychol. Psychother. 24, 1109–1120. doi: 10.1002/cpp.2076
Kong, Y. Z., Hang, L., Liu, Q., Hen, M., and Fu, X. (2020). Effect of group mindfulness-based cognitive therapy on somatic symptoms and sleep in depressive disorder. Chinese. J. Health Psychol. 28, 1144–1148. doi: 10.13342/j.cnki.cjhp
Kvillemo, P., Brandberg, Y., and Bränström, R. (2016). Feasibility and outcomes of an internet-based mindfulness training program: a pilot randomized controlled trial. JMIR Ment Health 3:e33. doi: 10.2196/mental.5457
Leppänen, J. M. (2006). Emotional information processing in mood disorders: a review of behavioral and neuroimaging findings. Curr. Opin. Psychiatry 19, 34–39. doi: 10.1097/01.yco.0000191500.46411.00
Lever Taylor, B., Strauss, C., Cavanagh, K., and Jones, F. (2014). The effectiveness of self-help mindfulness-based cognitive therapy in a student sample: a randomised controlled trial. Behav. Res. Ther. 63, 63–69. doi: 10.1016/j.brat.2014.09.007
Lifshitz, M., Sacchet, M. D., Huntenburg, J. M., Thiery, T., Fan, Y., Gärtner, M., et al. (2019). Mindfulness-based therapy regulates brain connectivity in major depression. Psychother. Psychosom. 88, 375–377. doi: 10.1159/000501170
Mohammadkhani, P., Khanipour, H., Azadmehr, H., Mobramm, A., and Naseri, E. (2015). Trait mindfulness, reasons for living and general symptom severity as predictors of suicide probability in males with substance abuse or dependence. Iran. J. Psychiatry 43, 381–390. doi: 10.1038/icb.1965.71
Morgan, D. (2003). Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. Psychother. Res. 13, 123–125. doi: 10.1080/713869628
Ortega, M. A., Fraile-Martínez, Ó., García-Montero, C., Alvarez-Mon, M. A., Lahera, G., Monserrat, J., et al. (2022). Nutrition, epigenetics, and major depressive disorder: understanding the connection. Front. Nutr. 9:867150. doi: 10.3389/fnut.2022.867150
Peng, F., and Pang, R. (2018). Effect of mindfulness-based cognitive therapy on depressive symptoms and quality of life in patients with depression. Medical Clin. Res. 35, 1133–1135. doi: 10.3969/j.issn.1671-7171.2018.06.032
Perez-Blasco, J., Viguer, P., and Rodrigo, M. F. (2013). Effects of a mindfulness-based intervention on psychological distress, well-being, and maternal self-efficacy in breast-feeding mothers: results of a pilot study. Arch. Womens Ment. Health 16, 227–236. doi: 10.1007/s00737-013-0337-z
Pigott, H. E., Leventhal, A. M., Alter, G. S., and Boren, J. J. (2010). Efficacy and effectiveness of antidepressants: current status of research. Psychother. Psychosom. 79, 267–279. doi: 10.1159/000318293
Shenefelt, P. D. (2018). Mindfulness-based cognitive hypnotherapy and skin disorders. Am. J. Clin. Hypn. 61, 34–44. doi: 10.1080/00029157.2017.1419457
Slama, F., Merle, S., Ursulet, G., Charles-Nicolas, A., and Ballon, N. (2011). Prevalence of and risk factors for lifetime suicide attempts among Caribbean people in the French West Indies. Psychiatry Res. 190, 271–274. doi: 10.1016/j.psychres.2011.08.007
Wang, J., Ren, F., Gao, B., and Yu, X. (2022). Mindfulness-based cognitive therapy in recurrent mdd patients with residual symptoms: alterations in resting-state theta oscillation dynamics associated with changes in depression and rumination. Front. Psych. 13:818298. doi: 10.3389/fpsyt.2022.818298
Wright, J. H., and Beck, A. T. (1983). Cognitive therapy of depression: theory and practice. Hospital and community psychiatry 34:1119.
Xiao, S., Yang, H., Dong, Q., and Yang, D. (1999). A study on the reliability and validity of the suicide attitude questionnaire. Chinese J. Mental Health 4, 250–251.
Yang, C. C., Barrós-Loscertales, A., Pinazo, D., Ventura-Campos, N., Borchardt, V., Bustamante, J. C., et al. (2016). State and training effects of mindfulness meditation on brain networks reflect neuronal mechanisms of its antidepressant effect. Neural Plast. 2016:9504642. doi: 10.1155/2016/9504642
Yu, S., Xu, W., and Liu, X. (2019). A controlled study of mindfulness training intervening negative emotions and perceived stress in individuals. Chinese Ment Health J 33, 273–278. doi: 10.3969/j.issn.1000-6729.2019.04.006
Yuan, Z., Chen, Z., Xue, M., Zhang, J., and Leng, L. (2020). Application of antidepressants in depression: a systematic review and meta-analysis. J. Clin. Neurosci. 80, 169–181. doi: 10.1016/j.jocn.2020.08.013
Zemestani, M., and Fazeli, N. Z. (2020). Effectiveness of mindfulness-based cognitive therapy for comorbid depression and anxiety in pregnancy: a randomized controlled trial. Arch. Womens Ment. Health 23, 207–214. doi: 10.1007/s00737-019-00962-8
Zernicke, K. A., Campbell, T. S., Speca, M., McCabe-Ruff, K., Flowers, S., Dirkse, D. A., et al. (2013). The eCALM trial-eTherapy for cancer applying mindfulness: online mindfulness-based cancer recovery program for underserved individuals living with cancer in Alberta: protocol development for a randomized wait-list controlled clinical trial. BMC Complement. Altern. Med. 13:34. doi: 10.1186/1472-6882-13-34
Zhang, G., Yang, L., Duan, D., Shi, Y., and Zhao, X. (2018). Effects of mindfulness relaxation training on perioperative psychological stress response and sleep quality in elderly patients with coronary heart disease undergoing PCI. Chinese J. Nurs. 53, 1463–1467. doi: 10.3761/j.issn.0254-1769.2018.12.011
Keywords: self-help mindfulness-based cognitive therapy, depression, mindfulness, suicidal ideation, randomized controlled study
Citation: Mo Y, Lei Z, Chen M, Deng H, Liang R, Yu M and Huang H (2023) Effects of self-help mindfulness-based cognitive therapy on mindfulness, symptom change, and suicidal ideation in patients with depression: a randomized controlled study. Front. Psychol. 14:1287891. doi: 10.3389/fpsyg.2023.1287891
Received: 03 September 2023; Accepted: 09 November 2023;
Published: 01 December 2023.
Edited by:
Jose Miguel Mestre, University of Cádiz, SpainReviewed by:
Olle Jane Sahler, University of Rochester, United StatesCopyright © 2023 Mo, Lei, Chen, Deng, Liang, Yu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rong Liang, bGlhbmcyMjNAc2luYS5jb20=; Miaoyu Yu, eXVsaXV5dTAxQHNpbmEuY29t; Huiqiao Huang, aHVhbmdodWlxaWFvbm5AMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.