- 1University “Giustino Fortunato” of Benevento, Benevento, Italy
- 2Universitas Mercatorum of Rome, Rome, Italy
Introduction
Fragile X syndrome (FXS) is a rare genetic disease caused by mutations in the fifth untranslated region of the FMRI gene situated on the Xq27.3 site, resulting in an expansion of cytosine–guanine–guanine (CGG) trinucleotide repeats. Typically, the CGG segment is repeated between 5 and 40 times in the normally developed population. Conversely, it is usually repeated over 200 times in FXS (i.e., full mutation). Individuals whose CGG repletion is comprised between 55 and 200 times present the premutation (Symons et al., 2003; Crawford et al., 2020; Marschik et al., 2022). The disease affects ~1 in 2,500 male individuals and 1 in 4,000–6,000 female individuals (Oliver et al., 2017). The excessive CGG repeats cause the FMR1 gene to be methylated, resulting in reduced production of the protein FMRP. Because the FXS is an X-linked neurodevelopmental disorder, it is more likely to be observed in male individuals than in female individuals (Adams and Oliver, 2011; Alusi et al., 2022). It represents the most known inherited cause of intellectual disabilities (IDs). Approximately 60% of FXS individuals present an autism spectrum disorder (ASD) comorbidity, while attention deficit hyperactivity (ADHD) is commonly observed in 70% of people with FXS (Kenny et al., 2022; Shaffer et al., 2023). The phenotype is characterized by an elongated face, a high-arched palate, large ears, muscular hypotonia, connective tissue dysplasia, mitral valve prolapse, and joint hypermobility (Cregenzán-Royo et al., 2022). Beyond cognitive impairments, language delays are commonly acknowledged. Adaptive skills are negatively affected, and social abnormalities are frequently observed (Van der Lei and Kooy, 2022). Behavioral difficulties, including poor eye contact, self-injury, aggression, and stereotypic, repetitive, and pervasive behaviors, are additionally reported (Marlborough et al., 2021; Niescier and Lin, 2021). Anxiety is also documented in FXS, with over 80% of the male subjects meeting the criteria for one anxiety disorder and over 60% of male subjects meeting the criteria for multiple anxiety disorders (Alusi et al., 2022; Chen Y. S. et al., 2022). The most frequent categories of anxiety disorders detectable in FXS are selective mutism and specific and/or social phobia. Approximately 60% of the male subjects with FXS show clinically relevant traits of social anxiety (Aishworiya et al., 2022; Chen C. C. et al., 2022).
Anxiety disorders are commonly recognized, with an approximate prevalence of 12 months in 18% of the general population. Children, adolescents, and adults with ID are at least four times more likely to meet the criteria for anxiety than those without ID (Tolmacheva et al., 2022). People with genetic diseases face a higher risk (Kat et al., 2022). Social anxiety is defined as a specific anxiety disorder that evidences persistent features of fear in social contexts (Kat et al., 2022). Exposure to unfamiliar people or environmental conditions is additionally included (Edwards et al., 2022). Eventual scrutiny by others and avoidance of social circumstances are embedded (Protic et al., 2022). Social anxiety represents one of the most common anxiety disorders, with a 12-month prevalence of 7% in the general population and a highly increased rate in people with rare genetic diseases. For instance, in individuals with FXS, as reported above, ~60% meet the diagnostic criteria of social anxiety. The rate is 35 times higher if compared with other idiopathic IDs (DaWalt et al., 2022).
Crawford (2023) suggested a conceptual model of social anxiety in FXS, including five constructs associated with it, namely, (a) physiological arousal, (b) sensory sensitivity, (c) emotion dysregulation, (d) cognitive flexibility, and (e) intolerance of uncertainty. The model emphasizes a multilevel pathway to social anxiety based on a biologically aroused state that, combined with sensory sensitivity, predisposes people with FXS to an inability to manage negative emotions. Consequently, the acceleration of physical processes compromises the capacity to regulate the deceleration of emotional responses. Built on this state of arousal and emotion, the model conceptualizes that individuals with FXS are unable to shift attention away from threatening stimuli, and an intolerance for the uncertainty of everyday life events or circumstances considered threatening is evidenced. A hierarchical element was postulated. Thus, emotional dysregulation is downstream of physiological excessive arousal, while sensory sensitivity, cognitive inflexibility, and intolerance to uncertainty are downstream of emotion dysregulation. This situation may be viewed as deleterious for the individuals' quality of life, with an increased burden on parents and caregivers, and their healthcare might be significantly hampered (Gabis et al., 2023; Klusek et al., 2023; Prior et al., 2023; Wall et al., 2023). To tackle this issue, one may envisage technology-aided interventions and/or artificial intelligence-based setups (Stasolla et al., 2017; Movaghar et al., 2022).
Within new technologies, extended reality (XR) includes computer-generated environments merging the physical and virtual worlds and/or creating an entirely virtual experience for users. XR encompasses the intersection of three different technologies, such as augmented reality (AR), virtual reality (VR), and mixed reality (MR). By merging the aforementioned technologies, XR provides users with a broad range of immersive opportunities across real- and virtual-based environments (Ren et al., 2023). Among AI-based programs, reinforcement learning (RL) as part of machine learning conceives an artificially intelligent agent capable of constantly interacting with the user and being reinforced by him/her; it is capable of constructive learning and can continuously calibrate the difficulty of the task for the user (Nissan et al., 2023). Although highly promising and constituting an invaluable educational and rehabilitative resource, the use of such technologies in neurodevelopmental disorders or developmental disabilities is quite sparse (Pires et al., 2022). Specifically, by inserting FXS, XR, and RL as keywords in Scopus and even merging their combinations, no records were found.
In line with the above, the objective of this opinion paper was to propose a new diagnostic tool and a plausible rehabilitative strategy to promote the healthcare of individuals with FXS and reduce the burden on parents and caregivers. In addition to an assessment tool to differentiate emotion regulation and tolerance to social anxiety, we suggest a combined strategy between XR and RL to promote constructive engagement in individuals with FXS (Stasolla et al., 2014a,b). In the following sections, we first describe and detail the functioning of XR and RL; subsequently, we argue for the combination of both as an assessment tool and a rehabilitative approach. The implications were critically discussed.
Extended reality
A wide range of terms are commonly used to summarize different virtual reality and related technologies that represent simulated real worlds built through computers, mobile devices, and wearable devices (Chen and Geschwind, 2022; Tan et al., 2022). XR is an umbrella term that encompasses all categories of real and virtual environments. Thus, AR, MR, and VR represent different modalities with different features. However, a considerable level of overlap may be found in the literature. Accordingly, non-experts may easily confound and use interchangeably one with the other (Park et al., 2022). For practical reasons, we avoid explaining each specific technology. Rather, by examining the existing literature, we found six records including XR and developmental disabilities (Camfield et al., 2016; Evans, 2018; Ropar et al., 2018; Stevens, 2018; AlMusawi et al., 2019; Park et al., 2022), and only two records using XR and neurodevelopmental disorders (Atkinson et al., 2003; Kim and Koh, 2016). Nevertheless, those technologies were largely and successfully adopted for developmental disabilities and neurodevelopmental disorders (Atkinson et al., 2003; Kim and Koh, 2016; MintzHemed and Melosh, 2023; Wu et al., 2023). Their use may be considered a crucial and invaluable resource because those technologies provide high levels of ecological validity (i.e., with situations similar to real life) and provide researchers and clinicians with practical knowledge through behavioral tracking and experimental control (Liu et al., 2022; Perera et al., 2022). Matched with serious games (SRs), those technologies may easily pursue educational, funny, diagnostic, and rehabilitative purposes (Hossain et al., 2016; Ávila et al., 2017; Maio et al., 2022a). By merging FXS and XR in Scopus, no records were found, suggesting that further research in this specific area was warranted. For example, one may argue that the healthcare and quality of life of individuals with FXS may be relevantly improved and the burden of parents and caregivers similarly reduced (Celesti et al., 2022; Maio et al., 2022b).
Reinforcement learning
Constantly interacting with the participant and calibrating the difficulty of a proposed activity or task to the individual's skills and performances, as part of machine learning, may be considered crucial for the success of an assessment or a rehabilitative strategy. Currently, computerized systems frequently include specific processes with progressive difficulties throughout sessions. Usually, those difficulties increase step by step according to predefined rules evaluated by a neuropsychologist who assesses the participants' performance. For example, such computerized systems daily adapt to the activities and increase the difficulty whenever a predefined threshold is reached. However, the order in which the specific parameters of the task are modified is fixed. Therefore, the characteristics of the unique participant are almost ignored. Thus, the peculiarities of the participants are neglected (Zini et al., 2022).
Broadly speaking, the basic concept is that in computerized systems, an RL AI agent is linked to a unique participant for each suggested activity or task. Thus, the agent continuously interacting with the participant while the exercise is running will be able to provide a rigorously tailored and customized difficulty, which is optimal for the unique participant. The agent is capable of learning from the specific performance of the participant through algorithms and parameters that are continuously adapted to the performance. A customized policy for each participant will be targeted, considering the ongoing performance. Specifically, the individuals' performance while completing the task plays the role of highly positive reinforcement useful to progressively enhance a policy by modifying the values of the parameters over time. Accordingly, the difficulty of the activity or task is optimized. That is, the task can be adapted individually, and the policy adopted to vary the parameters and to optimize the intervention can be independently learned for each participant (Coronato et al., 2020).
In light of the above, one may consider the combined integration between XR and RL. It may be conceived as an invaluable technological resource because the artificially intelligent agent may personalize the difficulty of the activities and/or tasks for the user, while the XR setups may enable an immersive environment similar to real life. The integration and combination of different technologies have been recently postulated and suggested by Stasolla et al. (2022, 2023a,b). Next to the positive outcomes for the participant, one may reasonably argue on the reduction of both caregivers' and families' burdens (Lopez-Vargas et al., 2019; Stasolla et al., 2021; Teriö et al., 2022). The innovative characteristic may be emphasized by the combined integration of both technologies, whose application and implementation may be adopted for both assessment and rehabilitative objectives in the early stages of social anxiety among FXS individuals. Furthermore, the emotional and cognitive competencies of individuals with FXS might be accurately investigated (Raspa et al., 2017; Bartholomay et al., 2019).
How should it work
The convergence of extended reality (XR) and reinforcement learning (RL) for the betterment of health and reduction of social anxiety in individuals with fragile X syndrome necessitates a multifaceted approach that integrates cutting-edge technologies and a profound understanding of the syndrome itself (Pons et al., 2022).
Initiating the process with an exhaustive exploration of fragile X syndrome lays the groundwork for an enhanced comprehension of its symptoms, risk factors, and the intricate challenges faced by those affected. Following this, the development of a three-dimensional virtual reality (VR) or mixed reality (MR) environment comes into play, aimed at replicating authentic social scenarios. These scenarios could encompass interactions with others, work-related situations, or even gaming scenarios. Integration of sensors within the virtual environment is then employed to capture biometric data, including heart rate, perspiration, and facial expressions during individuals' engagements within the virtual realm. The implementation of RL agents follows suit, designed to perpetually monitor the amassed biometric data. These agents discern instances when an individual with fragile X syndrome exhibits indications of social anxiety (Dechant et al., 2017).
Upon the detection of social anxiety, RL agents step in with personalized interventions. This may involve offering tailored suggestions, facilitating relaxation exercises, or adjusting the intensity of social interactions within the virtual environment to align with the individual's specific needs. A pivotal aspect involves continuous learning by RL agents, allowing them to adapt and refine their responses based on the outcomes of interactions over time. Therapeutic involvement is also woven into the fabric of this approach, with mental health professionals or therapists seamlessly integrated into the virtual environment. Their role is to provide direct support and counseling as necessary. The process includes a robust system for the evaluation and improvement of individuals' progress, utilizing biometric sensor feedback to collect data on mental health advancements over time (Yao et al., 2020).
An emphasis on ethics and privacy underscores the importance of stringent privacy policies and ethical considerations, empowering individuals to control their data and participate in the virtual environment. To ensure a comprehensive and ethical framework, interdisciplinary collaboration is pivotal. Experts in medicine, psychology, artificial intelligence, ethics, and XR development collectively contribute to shaping this holistic approach. In essence, the overarching goal of merging XR and RL is to forge a secure and personalized environment for individuals grappling with fragile X syndrome. The ultimate aim is to champion mental health and alleviate social anxiety. However, it is crucial to underscore that this innovative approach necessitates further research and technological advancements to transition from concept to practical and effective reality (Warin, 2022).
Considering the multilevel pathway model suggested by Crawford (2023) above, an optimal starting point for an artificial agent working according to RL rules usually comes from a fully randomized policy criterion. That is, an initial identical probability is assigned to all considered actions that the agent can carry out. The parameters are identified by the five basic elements acknowledged by the model. An identical initial probability is randomly assigned to each parameter/element of the model. Two different outcomes are sought: (a) a successful consequence is empirically recorded because an optimal policy has been designed with a long interaction between the participant and the system or (b) a failure is detected because an initial poor effect of the learning process is planned and frustration by the participant is empirically documented (Ciampi et al., 2022). To overcome this issue, one may envisage an association between category policies and exercises or tasks. The category policy should include a probability of actions that is not the ideal one but very close to it if compared to the fully randomized policy. Starting from the task category policy, an individualized participant–agent interaction would be fostered, and the accuracy of the ideal personalized policies can be programmed (Stasolla and Di Gioia, 2023).
XR-based setups may enable, on the other hand, an individual with FXS to have a fully immersive experience similar to real life. For instance, different experimental conditions eliciting different emotions can be built. Based on the participants' preferences (Lancioni et al., 2022), one may consider different scenarios rigorously adapted to the individual level of social functioning (i.e., including cognitive, emotional, and motor functioning). For FXS individuals with severe to profound intellectual disabilities, one may design a basic recognition of facial expressions, representing different emotions. The participant would be required to correctly identify the solicited emotion in each trial. For individuals with moderate intellectual disabilities, one may consider request and choice access to preferred items eliciting different emotions. A hierarchical system requesting different choices to be performed by the participant would be proposed (Lancioni et al., 2008b, 2022). For individuals with mild cognitive impairment, one may propose cognitive tasks or exercises mediated and supported by customized technology (Hocking et al., 2023).
The opportunities detailed above may be helpful to easily pursue a dual goal. An assessment of individuals who are at risk of social anxiety may be reached. A rehabilitative strategy can be adopted to promote constructive engagement, positive participation, and functional occupation (Stasolla et al., 2014a). Different solutions tailored to the participants functioning and preferences might be encouraged (Caffò et al., 2016). In summary, in a unique session of intervention, a combined solution of XR and RL would provide the participant with an optimal technological solution depending on the global functioning of the participant, and at the same time, the artificially intelligent agent would constantly calibrate the difficulty of the task. With the illustrative examples detailed above, one can differentiate between an individual who is capable of managing his/her emotional states and an individual who is at risk of social anxiety (i.e., social value). Once differentiated, one might propose a rehabilitative intervention with further experimental conditions (i.e., see above) to promote adaptive responding and constructive engagement in individuals with FXS (Caffò et al., 2016; Raspa et al., 2020; Ellis et al., 2021). To enhance the reader's ability to follow the logic with each possible outcome, we inserted a graphical representation of the proposed functioning in Figure 1.
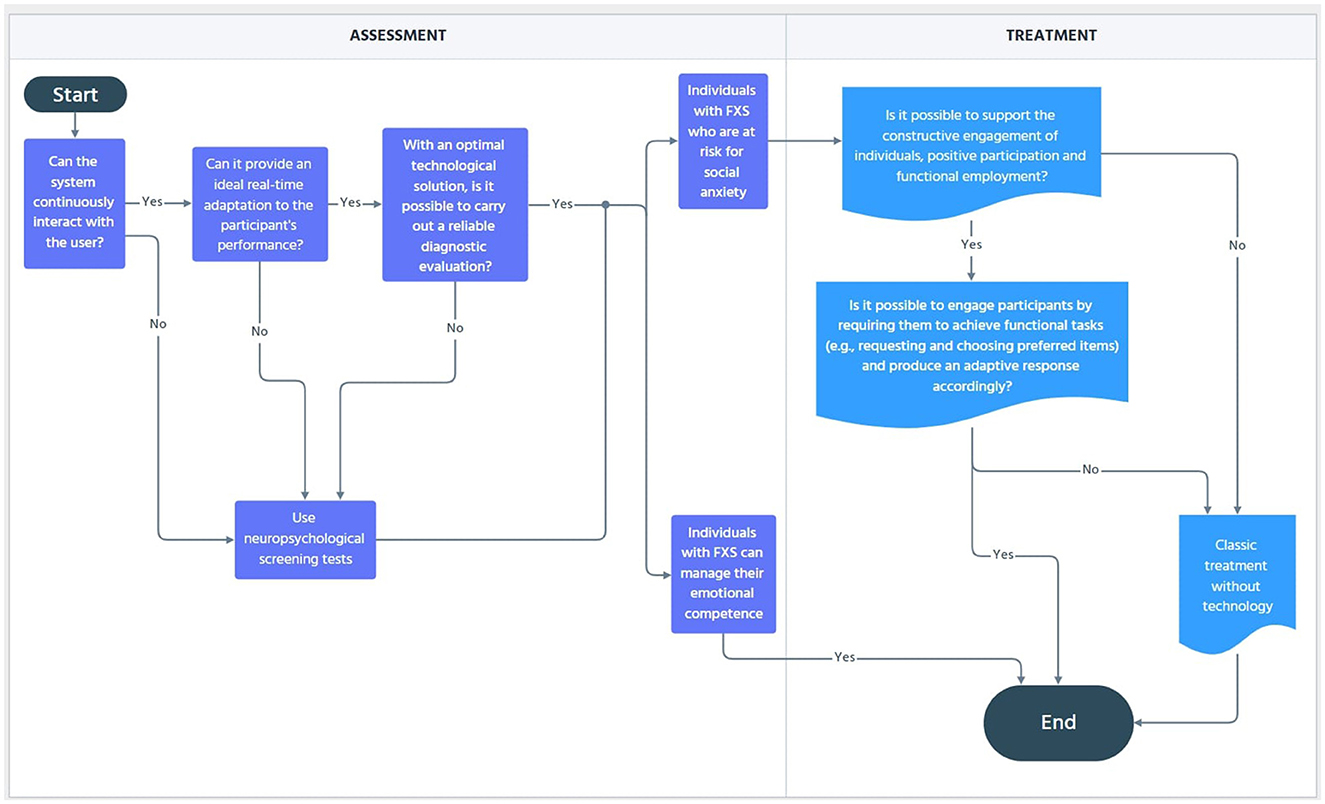
Figure 1. Flow chart diagram of the process for reaching the proposed assessment and recovery objectives.
Discussion
We proposed a combined technology integrating XR and RL in a unique intervention with a dual purpose: (a) the assessment and (b) the rehabilitation of cognitive and emotional competencies in individuals with FXS. Regarding social anxiety, we described the model suggested by Crawford (2023). Moreover, we argued about the combined mechanism aimed at identifying cognitive and emotional skills in individuals with FXS. Finally, we detailed a new diagnostic tool and a new rehabilitative strategy for assessment and recovery objectives. We provided some illustrative examples to identify people with FXS who are capable of independently managing their emotions and individuals with FXS who are at risk of developing social anxiety. Furthermore, depending on the individual's functioning, we presented different possible scenarios and/or experimental conditions. The proposal may suggest the following considerations.
First, a new assessment tool was tentatively structured. The system may be considered valuable because by continuously interacting with the user, it can provide an ideal adaptation in real-time to the performance of the participant. With an optimal technological solution, a reliable diagnostic evaluation could be made. One may argue that an early assessment, eventually supported by neuropsychological screening, can be carried out. It could be viewed as critical to differentiate between individuals with FXS who could manage their emotional competence mediated by coping strategies and individuals with FXS who were at risk of social anxiety (Lancioni et al., 2009a,b, 2010; Tarver et al., 2021; Crawford et al., 2023; Jones et al., 2023).
Second, based on a rehabilitative point of view, one may support the individual's constructive engagement, positive participation, and functional occupation. Thus, by involving the participants in social and/or emotional conditions as described above, people with FXS and ID may be requested to achieve functional tasks (e.g., request and choice of preferred items) and produce an adaptive response accordingly (Lancioni et al., 2009a, 2010).
Third, the participants' quality of life may be significantly improved, and families' or caregivers' burdens may be similarly reduced. One may argue that the healthcare of individuals with FXS can be favorably supported. However, the integration in clinical settings was recently conceptualized (Jones et al., 2023) should be carefully evaluated. Furthermore, its suitability in daily contexts (e.g., home and educational environments) should be additionally considered.
Fourth, clinical and social validity should also be included. For example, social validation procedures involving external experts such as neurologists, psychologists, parents of children with developmental disabilities, physiotherapists, and/or speech/occupational therapists are warranted. External validity, including systematic comparisons with idiopathic disabilities or other developmental disabilities, should be viewed as mandatory (Lancioni et al., 2004, 2007, 2008a, 2009a; Stasolla et al., 2014a).
Limitations and future research
Despite the beneficial perspectives, caution is highly recommended. Thus, different limitations can be recognized. First, empirical data in our proposed combination between XR and RL are currently missing. Systematic investigations of FXS individuals are mandatory. Either group comparisons or longitudinal single-subject-based studies, as well as several clinical trials, should be conducted. Second, both assessment and rehabilitative goals should be addressed daily. Third, the acceptability of young and older adults with FXS should be considered. Fourth, suitability and sustainability in daily settings should be a research priority. Fifth, affordability in daily contexts should be adequately evaluated. Sixth, the proposed tool should be carefully assessed through a large sample of participants, including other idiopathic ID and/or different genetic diseases (e.g., Angelman, Cornelia de those with Lange, and Rett syndromes). Seventh, it should be noted that FXS is also associated with hypersensitivity to sensory stimuli, and this could impose some challenges while also providing opportunities by altering the amount of XR sensory stimulation. To overcome this issue, one may argue that the combined RL and VR may provide individuals with FXS in a highly continuous and rigorously customized and tailored fashion. Thus, an adapted and updated version of Crawford's Model (Crawford, 2023) may be envisaged. A sixth parameter, including a further detailed customized sensitivity, may be embedded. The RL-based agent would calibrate the individual's sensitivity to such a parameter. An optimal VR setup would be adopted. Further evaluations might be assessed with neuropsychological and neurophysiological measures (e.g., event-related potentials, neural oscillations, and animal models). Outcomes of clinical trials, profiles, and developmental trajectories may additionally indicate the degree of sensitivity (Budimirovic et al., 2017; Sinclair et al., 2017; Jenner et al., 2023).
In light of the above, future research perspectives should include the following topics: (a) to empirically investigate the use of a combined XR and RL tool to evaluate emotional competence and social anxiety in FXS, (b) to assess the suitability and sustainability on environmental, financial, and human resources, (c) to consider affordability through social validation procedures, including psychologists, neurologists, clinicians, researchers, and caregivers as external and expert raters, and (d) gradually carry out systematic reviews and meta-analysis within this specific framework.
Conclusion
A combined integration between XR and RL was suggested to pursue the dual objective of evaluation and rehabilitation in FXS individuals. An early assessment with the combined technology may be viewed as critical to preventing social anxiety and emotional dysregulation. Additionally, the combined technology can be used as a useful rehabilitative strategy, providing a continuous and rigorously tailored adaptation to the activity's complexity. A systematic matching between different technologies (e.g., assistive technology, telerehabilitation, and VR) has been recently proposed (García et al., 2021).
An adequate evaluation of the personalized options for each use is warranted. A remote supervised control may be implemented (Bernini et al., 2023a). Specific adaptations, suitability investigations, and satisfaction experiences should be relevantly issued within this framework (Bernini et al., 2023b).
Author contributions
FS: Conceptualization, Writing – original draft. AP: Writing – review & editing. MD: Supervision, Writing – review & editing. EC: Supervision, Writing – review & editing. AZ: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adams, D., and Oliver, C. (2011). The expression and assessment of emotions and internal states in individuals with severe or profound intellectual disabilities. Clin. Psychol. Rev. 31, 293–306. doi: 10.1016/j.cpr.2011.01.003
Aishworiya, R., Protic, D., and Hagerman, R. (2022). Autism spectrum disorder in the fragile X premutation state: possible mechanisms and implications. J. Neurol. 269, 4676–4683. doi: 10.1007/s00415-022-11209-5
AlMusawi, A. M. J., Shebib, H. S. S., Musawy, A. K., and Bekheet, H. N. (2019). Corruption and its economic and social impacts on Iraq's economy developmental reality. Int. J. Innov. Creat. Chan. 8, 297–310.
Alusi, G., Berry-Kravis, E., Nelson, D., Orefice, L. L., and Booker, S. A. (2022). Emerging therapeutic strategies for fragile X syndrome: QandA. ACS Chem. Neurosci. 13, 3544–3546. doi: 10.1021/acschemneuro.2c00674
Atkinson, J., Braddick, O., Anker, S., Nardini, M., Bellugi, U., Rose, F. E., et al. (2003). Extending the ≪dorsal stream vulnerability hypothesisa≫: spatial reorientation and motion and form coherence in children and adults with Williams syndrome. J. Vision 3, 287a. doi: 10.1167/3.9.287
Ávila, C., Manso, L., de Castro, P. B. G., and Núñez, P. (2017). ‘VRComponent': a virtual reality software for neuro-rehabilitation with robotics technologies. Biosyst. Biorob. 15, 1327–1332. doi: 10.1007/978-3-319-46669-9_217
Bartholomay, K. L., Lee, C. H., Bruno, J. L., Lightbody, A. A., and Reiss, A. L. (2019). Closing the gender gap in fragile X syndrome: review on females with FXS and preliminary research findings. Brain Sci. 9, 10011. doi: 10.3390/brainsci9010011
Bernini, S., Gerbasi, A., Panzarasa, S., Quaglini, S., Ramusino, M. C., Costa, A., et al. (2023a). Outcomes of a computer-based cognitive training (CoRe) in early phases of cognitive decline: a data-driven cluster analysis. Sci. Rep. 13, 2175. doi: 10.1038/s41598-022-26924-2
Bernini, S., Panzarasa, S., Quaglini, S., Costa, A., Picascia, M., Cappa, S. F., et al. (2023b). HomeCoRe system for telerehabilitation in individuals at risk of dementia: a usability and user experience study. Front. Med. 10, e1129914. doi: 10.3389/fmed.2023.1129914
Budimirovic, D. B., Berry-Kravis, E., Erickson, C. A., Hall, S. S., Hessl, D., Reiss, A. L., et al. (2017). Updated report on tools to measure outcomes of clinical trials in fragile X syndrome. J. Neurodev. Disord. 9, 14. doi: 10.1186/s11689-017-9193-x
Caffò, A. O., Lopez, A., Spano, G., Saracino, G., Stasolla, F., Ciriello, G., et al. (2016). The role of pre-morbid intelligence and cognitive reserve in predicting cognitive efficiency in a sample of Italian elderly. Aging Clin. Exp. Res. 28, 1203–1210. doi: 10.1007/s40520-016-0580-z
Camfield, P., Camfield, C., and Nolan, K. (2016). Helping families cope with the severe stress of dravet syndrome. Can. J. Neurol. Sci. 43, S9–12. doi: 10.1017/cjn.2016.248
Celesti, A., Cimino, V., Naro, A., Portaro, S., Fazio, M., Villari, M., et al. (2022). Recent considerations on gaming console based training for multiple sclerosis rehabilitation. Med. Sci. 10, 10013. doi: 10.3390/medsci10010013
Chen, C. C., Chen, H. R., and Wang, T. Y. (2022). Creative situated augmented reality learning for astronomy curricula. Educ. Technol. Soc. 25, 148–162.
Chen, G. T., and Geschwind, D. H. (2022). Challenges and opportunities for precision medicine in neurodevelopmental disorders. Adv. Drug Del. Rev. 191, e114564. doi: 10.1016/j.addr.2022.114564
Chen, Y. S., Guo, L., Han, M., Zhang, S. M., Chen, Y. Q., Zou, J., et al. (2022). Cerebellum neuropathology and motor skill deficits in fragile X syndrome. Int. J. Dev. Neurosci. 82, 557–568. doi: 10.1002/jdn.10217
Ciampi, M., Coronato, A., Naeem, M., and Silvestri, S. (2022). An intelligent environment for preventing medication errors in home treatment. Expert Syst. Appl. 193, e116434. doi: 10.1016/j.eswa.2021.116434
Coronato, A., Naeem, M., De Pietro, G., and Paragliola, G. (2020). Reinforcement learning for intelligent healthcare applications: a survey. Artif. Intellig. Med. 109, e101964. doi: 10.1016/j.artmed.2020.101964
Crawford, H. (2023). Social anxiety in neurodevelopmental disorders: the case of fragile X syndrome. Am. J. Intell. Dev. Disabil. 128, 302–318. doi: 10.1352/1944-7558-128.4.302
Crawford, H., Abbeduto, L., Hall, S. S., Hardiman, R., Hessl, D., Roberts, J. E., et al. (2020). Fragile X syndrome: an overview of cause, characteristics, assessment and management. Paediat. Child Health. 30, 400–403. doi: 10.1016/j.paed.2020.08.007
Crawford, H., Oliver, C., Groves, L., Bradley, L., Smith, K., Hogan, A., et al. (2023). Behavioural and physiological indicators of anxiety reflect shared and distinct profiles across individuals with neurogenetic syndromes. Psychiatry Res. 326, 115278. doi: 10.1016/j.psychres.2023.115278
Cregenzán-Royo, O., Brun-Gasca, C., and Fornieles-Deu, A. (2022). Behavior Problems and social competence in fragile X syndrome: a systematic review. Genes. 13, 280. doi: 10.3390/genes13020280
DaWalt, L. S., Fielding-Gebhardt, H., Fleming, K. K., Warren, S. F., and Brady, N. (2022). Change in behavior problems from childhood through adolescence for children with fragile X syndrome. J. Autism Dev. Disord. 52, 4056–4066. doi: 10.1007/s10803-021-05270-8
Dechant, M. J., Trimpl, S., Wolff, C., and Mühlberger, A. (2017). Potential of virtual reality as a diagnostic tool for social anxiety: a pilot study. Comput. Hum. Behav. 76, 128–134. doi: 10.1016/j.chb.2017.07.005
Edwards, G., Jones, C., Pearson, E., Royston, R., Oliver, C., Tarver, J., et al. (2022). Prevalence of anxiety symptomatology and diagnosis in syndromic intellectual disability: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 138, e104719. doi: 10.1016/j.neubiorev.2022.104719
Ellis, K., Moss, J., Stefanidou, C., Oliver, C., and Apperly, I. (2021). The development of early social cognitive skills in neurogenetic syndromes associated with autism: Cornelia de Lange, fragile X and Rubinstein–Taybi syndromes. Orphanet J. Rare Dis. 16, 488. doi: 10.1186/s13023-021-02117-4
Evans, G. (2018). Assessing clients with a serious physical illness or disability for psychodynamic counselling. Dual Real. Search Mean. Psychodyn. Therapy Phys. Ill People. doi: 10.4324/9780429474033-2
Gabis, L. V., Shaham, M., Attia, O. L., Kowal, T., David, S., Banet-Levi, Y., et al. (2023). An escalating continuum of learning and attention difficulties from premutation to full mutation in female carriers of FMR1 expansion. Front. Neurol. 14, e1135630. doi: 10.3389/fneur.2023.1135630
García, T. P., Garabal-Barbeira, J., Trillo, P. P., Figueira, O. V., Díaz, C. N., Loureiro, J. P., et al. (2021). A framework for a new approach to empower users through low-cost and do-it-yourself assistive technology. Int. J. Environ. Res. Public Health. 18, 1–17. doi: 10.3390/ijerph18063039
Hocking, J., Oster, C., Maeder, A., and Lange, B. (2023). Design, development, and use of conversational agents in rehabilitation for adults with brain-related neurological conditions: a scoping review. JBI Evid. Synth. 21, 326–372. doi: 10.11124/JBIES-22-00025
Hossain, M. S., Hardy, S., Alamri, A., Alelaiwi, A., Hardy, V., Wilhelm, C., et al. (2016). AR-based serious game framework for post-stroke rehabilitation. Multimedia Syst. 22, 659–674. doi: 10.1007/s00530-015-0481-6
Jenner, L., Richards, C., Howard, R., and Moss, J. (2023). Heterogeneity of autism characteristics in genetic syndromes: key considerations for assessment and support. Curr. Dev. Disord. Rep. 10, 132–146. doi: 10.1007/s40474-023-00276-6
Jones, R. B., Hussain, F., Agha, S. S., Weavers, B., Lucassen, M., Merry, S., et al. (2023). Digital technologies to support adolescents with depression and anxiety: review. BJPsych Adv. 29, 239–253. doi: 10.1192/bja.2022.3
Kat, R., Arroyo-Araujo, M., de Vries, R. B. M., Koopmans, M. A., de Boer, S. F., Kas, M. J. H., et al. (2022). Translational validity and methodological underreporting in animal research: a systematic review and meta-analysis of the Fragile X syndrome (Fmr1 KO) rodent model. Neurosci. Biobehav. Rev. 139, e10722. doi: 10.1016/j.neubiorev.2022.104722
Kenny, A., Wright, D., and Stanfield, A. C. (2022). EEG as a translational biomarker and outcome measure in fragile X syndrome. Transl. Psychiatry. 12, 34. doi: 10.1038/s41398-022-01796-2
Kim, H. J., and Koh, H. Y. (2016). Impaired reality testing in mice lacking phospholipase Cβ1: Observed by persistent representation-mediated taste aversion. PLoS ONE. 11. E0146376. doi: 10.1371/journal.pone.0146376
Klusek, J., Will, E., Moser, C., Hills, K., Thurman, A. J., Abbeduto, L., et al. (2023). Predictors, parental views, and concordance across diagnostic sources of autism in male youth with fragile X syndrome: clinical best estimate and community diagnoses. Res. Child Adoles. Psychopathol. 51, 989–1004. doi: 10.1007/s10802-023-01044-1
Lancioni, G., O'Reilly, M., Singh, N., Green, V., Chiapparino, C., Pace, D., et al. (2010). Use of microswitch technology and a keyboard emulator to support literacy performance of persons with extensive neuro-motor disabilities. Dev. Neurorehabil. 13, 248–257. doi: 10.3109/17518423.2010.485596
Lancioni, G. E., Belardinelli, M. O., Chiapparino, C., Angelillo, M. T., Stasolla, F., Singh, N. N., et al. (2008a). Learning in post-coma persons with profound multiple disabilities: two case evaluations. J. Dev. Phys. Disabil. 20, 209–216. doi: 10.1007/s10882-008-9105-9
Lancioni, G. E., Belardinelli, M. O., Stasolla, F., Singh, N. N., O'Reilly, M. F., Sigafoos, J., et al. (2008b). Promoting engagement, requests and choice by a man with post-coma pervasive motor impairment and minimally conscious state through a technology-based program. J. Dev. Phys. Disabil. 20, 379–388. doi: 10.1007/s10882-008-9104-x
Lancioni, G. E., O'Reilly, M. F., Singh, N. N., Sigafoos, J., Didden, R., Oliva, D., et al. (2009a). Persons with multiple disabilities accessing stimulation and requesting social contact via microswitch and VOCA devices: new research evaluation and social validation. Res. Dev. Disabil. 30, 1084–1094. doi: 10.1016/j.ridd.2009.03.004
Lancioni, G. E., O'Reilly, M. F., Singh, N. N., Stasolla, F., Manfredi, F., Oliva, D., et al. (2004). Adapting a grid into a microswitch to suit simple hand movements of a child with profound multiple disabilities. Perceptual Motor Skills. 99, 724–728. doi: 10.2466/pms.99.2.724-728
Lancioni, G. E., Singh, N. N., O'Reilly, M. F., Sigafoos, J., Alberti, G., Chiariello, V., et al. (2022). A microswitch-aided program to enable people with extensive multiple disabilities to control environmental stimulation through different responses. Front. Psychiatry. 13, e1073650. doi: 10.3389/fpsyt.2022.1073650
Lancioni, G. E., Singh, N. N., O'Reilly, M. F., Sigafoos, J., Chiapparino, C., Stasolla, F., et al. (2007). Enabling a young man with minimal motor behavior to manage independently his leisure television engagement. Perceptual Motor Skills. 105, 47–54. doi: 10.2466/pms.105.1.47-54
Lancioni, G. E., Singh, N. N., O'Reilly, M. F., Sigafoos, J., Green, V., Chiapparino, C., et al. (2009b). A voice-detecting sensor and a scanning keyboard emulator to support word writing by two boys with extensive motor disabilities. Res. Dev.Disabil. 30, 203–209. doi: 10.1016/j.ridd.2008.03.001
Liu, Y., Liu, T., and Ma, Q. (2022). Immersive virtual reality teaching in colleges and universities based on vision sensors. Wireless Commun. Mobile Comput. 2022, 5790491. doi: 10.1155/2022/5790491
Lopez-Vargas, P., Tong, A., Crowe, S., Alexander, S. I., Caldwell, P. H. Y., Campbell, D. E., et al. (2019). Research priorities for childhood chronic conditions: a workshop report. Arch. Dis. Childhood. 104, 237–245. doi: 10.1136/archdischild-2018-315628
Maio, R., Alves, J., Marques, B., Dias, P., and Lau, N. (2022b). Exploring an augmented reality serious game for motorized wheelchair control. P B, E P, curatori. ACM International Conference Proceeding Series.
Maio, R., Marques, B., Alves, J., Santos, B. S., Dias, P., Lau, N., et al. (2022a). An augmented reality serious game for learning intelligent wheelchair control: comparing configuration and tracking methods. Sensors. 22, 7788. doi: 10.3390/s22207788
Marlborough, M., Welham, A., Jones, C., Reckless, S., and Moss, J. (2021). Autism spectrum disorder in females with fragile X syndrome: a systematic review and meta-analysis of prevalence. J. Neurodev. Disord. 13, 28. doi: 10.1186/s11689-021-09362-5
Marschik, P. B., Widmann, C. A. A., Lang, S., Kulvicius, T., Boterberg, S., Nielsen-Saines, K., et al. (2022). Emerging verbal functions in early infancy: lessons from observational and computational approaches on typical development and neurodevelopmental disorders. Adv. Neurodevelop. Disord. 6, 369–388. doi: 10.1007/s41252-022-00300-7
MintzHemed, N., and Melosh, N. A. (2023). An integrated perspective for the diagnosis and therapy of neurodevelopmental disorders – From an engineering point of view. Adv. Drug Deliv. Rev. 194, 114723. doi: 10.1016/j.addr.2023.114723
Movaghar, A., Page, D., Brilliant, M., and Mailick, M. (2022). Advancing artificial intelligence-assisted pre-screening for fragile X syndrome. BMC Med. Inform. Decision Mak. 22. doi: 10.1186/s12911-022-01896-5
Niescier, R. F., and Lin, Y. C. (2021). The potential role of AMPA receptor trafficking in autism and other neurodevelopmental conditions. Neuroscience 479, 180–191. doi: 10.1016/j.neuroscience.2021.09.013
Nissan, N., Hertz, U., Shahar, N., and Gabay, Y. (2023). Distinct reinforcement learning profiles distinguish between language and attentional neurodevelopmental disorders. Behav. Brain Funct. 19, 6. doi: 10.1186/s12993-023-00207-w
Oliver, C., Licence, L., and Richards, C. (2017). Self-injurious behaviour in people with intellectual disability and autism spectrum disorder. Curr. Opin. Psychiatry 30, 97–101. doi: 10.1097/YCO.0000000000000313
Park, S. B., Ju, Y., Kwon, H., Youm, H., Kim, M. J., Chung, J., et al. (2022). Effect of a cognitive function and social skills-based digital exercise therapy using iot on motor coordination in children with intellectual and developmental disability. Int. J. Environ. Res. Public Health. 19, 6499. doi: 10.3390/ijerph192416499
Perera, K. T., Gamage, A. I. U., Jawahir, M. H., Dias, G. K. A., and Sandaruwan, K. D. (2022). Augmented Reality Supported Self-help Interventions for Psychological and Physiological Acute Stress. LNNS. 359, 662–679. doi: 10.1007/978-3-030-89880-9_49
Pires, G., Cruz, A., Jesus, D., Yasemin, M., Nunes, U. J., Sousa, T., et al. (2022). A new error-monitoring brain-computer interface based on reinforcement learning for people with autism spectrum disorders. J. Neural Eng. 19, aca798. doi: 10.1088/1741-2552/aca798
Pons, P., Navas-Medrano, S., and Soler-Dominguez, J. L. (2022). Extended reality for mental health: current trends and future challenges. Front. Comp. Sci. 4, 1034307. doi: 10.3389/fcomp.2022.1034307
Prior, D., Win, S., Hassiotis, A., Hall, I., Martiello, M. A., Ali, A. K., et al. (2023). Behavioural and cognitive-behavioural interventions for outwardly directed aggressive behaviour in people with intellectual disabilities. Cochrane Datab. Syst. Rev. 2023. doi: 10.1002/14651858.CD003406.pub5
Protic, D. D., Aishworiya, R., Salcedo-Arellano, M. J., Tang, S. J., Milisavljevic, J., Mitrovic, F., et al. (2022). Fragile X syndrome: from molecular aspect to clinical treatment. Int. J. Mol. Sci. 23, 41935. doi: 10.3390/ijms23041935
Raspa, M., Paquin, R. S., Brown, D. S., Andrews, S., Edwards, A., Moultrie, R., et al. (2020). Preferences for accessing electronic health records for research purposes: views of parents who have a child with a known or suspected genetic condition. Value Health. 23, 1639–1652. doi: 10.1016/j.jval.2020.06.016
Raspa, M., Wheeler, A. C., and Riley, C. (2017). Public health literature review of fragile X syndrome. Pediatrics. 139, S153–S171. doi: 10.1542/peds.2016-1159C
Ren, X., Wu, Q., Cui, N., Zhao, J., and Bi, H. Y. (2023). Effectiveness of digital game-based trainings in children with neurodevelopmental disorders: a meta-analysis. Res. Dev. Disabil. 133, e104418. doi: 10.1016/j.ridd.2022.104418
Ropar, D., Greenfield, K., Smith, A. D., Carey, M., and Newport, R. (2018). Body representation difficulties in children and adolescents with autism may be due to delayed development of visuo-tactile temporal binding. Dev. Cogn. Neurosci. 29, 78–85. doi: 10.1016/j.dcn.2017.04.007
Shaffer, R. C., Reisinger, D. L., Schmitt, L. M., Lamy, M., Dominick, K. C., Smith, E. G., et al. (2023). Systematic review: emotion dysregulation in syndromic causes of intellectual and developmental disabilities. J. Am. Acad. Child Adoles. Psychiatry. 62, 518–557. doi: 10.1016/j.jaac.2022.06.020
Sinclair, D., Oranje, B., Razak, K. A., Siegel, S. J., and Schmid, S. (2017). Sensory processing in autism spectrum disorders and Fragile X syndrome-From the clinic to animal models. Neurosci. Biobehav. Rev. 76, 235–253. doi: 10.1016/j.neubiorev.2016.05.029
Stasolla, F., Bernini, S., Bottiroli, S., Koumpouros, Y., Wadhera, T., Akbar, K., et al. (2023a). Editorial: the integration of the technology in clinical settings among neurological populations. Front. Psychol. 14, e1145982. doi: 10.3389/fpsyg.2023.1145982
Stasolla, F., Damiani, R., and Caffò, A. O. (2014a). Promoting constructive engagement by two boys with autism spectrum disorders and high functioning through behavioral interventions. Res. Autism Spect. Disord. 8, 376–380. doi: 10.1016/j.rasd.2013.12.020
Stasolla, F., and Di Gioia, M. (2023). Combining reinforcement learning and virtual reality in mild neurocognitive impairment: a new usability assessment on patients and caregivers. Front. Aging Neurosci. 15, e1189498. doi: 10.3389/fnagi.2023.1189498
Stasolla, F., Lopez, A., Akbar, K., Vinci, L. A., and Cusano, M. (2023b). Matching assistive technology, telerehabilitation, and virtual reality to promote cognitive rehabilitation and communication skills in neurological populations: a perspective proposal. Technologies. 11, 20043. doi: 10.3390/technologies11020043
Stasolla, F., Matamala-Gomez, M., Bernini, S., Caffò, A. O., and Bottiroli, S. (2021). Virtual reality as a technological-aided solution to support communication in persons with neurodegenerative diseases and acquired brain injury during COVID-19 pandemic. Front. Public Health. 8, 635426. doi: 10.3389/fpubh.2020.635426
Stasolla, F., Perilli, V., and Damiani, R. (2014b). Self monitoring to promote on-task behavior by two high functioning boys with autism spectrum disorders and symptoms of ADHD. Res. Autism Spectr. Disord. 8, 472–479. doi: 10.1016/j.rasd.2014.01.007
Stasolla, F., Perilli, V., Damiani, R., and Albano, V. (2017). Assistive technology to promote occupation and reduce mouthing by three boys with fragile X syndrome. Dev. Neurorehabil. 20, 185–193. doi: 10.3109/17518423.2015.1133724
Stasolla, F., Vinci, L. A., and Cusano, M. (2022). The integration of assistive technology and virtual reality for assessment and recovery of post-coma patients with disorders of consciousness: a new hypothesis. Front. Psychol. 13, e905811. doi: 10.3389/fpsyg.2022.905811
Stevens, R. (2018). “Social augmented reality,” in Proceedings of the 5th European Conference on Social Media, ECSM 2018 (Limerick), 312–317.
Symons, F. J., Clark, R. D., Hatton, D. D., Skinner, M., and Bailey, J.r. D. B. (2003). Self-injurious behavior in young boys with fragile X syndrome. Am. J. Med. Genet. 118A, 115–121. doi: 10.1002/ajmg.a.10078
Tan, Q. P., Huang, L., Xu, D., Cen, Y., and Cao, Q. (2022). Serious game for VR road crossing in special needs education. Electronics. 11, 62568. doi: 10.3390/electronics11162568
Tarver, J., Pearson, E., Edwards, G., Shirazi, A., Potter, L., Malhi, P., et al. (2021). Anxiety in autistic individuals who speak few or no words: a qualitative study of parental experience and anxiety management. Autism. 25, 429–439. doi: 10.1177/1362361320962366
Teriö, M., Pérez-Rodríguez, R., Guevara, T., Valdes-Aragonés, M., Kornevs, M., Bjälevik-Chronan, S., et al. (2022). Preventing frailty with the support of a home-monitoring and communication platform among older adults—a study protocol for a randomised-controlled pilot study in Sweden. Pilot Feasibil. Stud. 8, 190. doi: 10.1186/s40814-022-01147-4
Tolmacheva, E. N., Fonova, E. A., and Lebedev, I. N. (2022). X-linked CNV in pathogenetics of intellectual disability. Russ. J. Genet. 58, 1193–1207. doi: 10.1134/S102279542210009X
Van der Lei, M. B., and Kooy, R. F. (2022). Therapeutic potential of GABAA receptor subunit expression abnormalities in fragile X syndrome. Expert Rev. Precision Med. Drug Dev. 7, 105–120. doi: 10.1080/23808993.2021.2008168
Wall, C. A., Shic, F., Varanasi, S., and Roberts, J. E. (2023). Distinct social attention profiles in preschoolers with autism contrasted to fragile X syndrome. Autism Res. 16, 340–354. doi: 10.1002/aur.2857
Warin, C. (2022). “Vision: usable privacy for XR in the era of the metaverse,” in Proceedings of the 2022 (New York, NY).
Wu, X., Deng, H., Jian, S., Chen, H., Li, Q., Gong, R., et al. (2023). Global trends and hotspots in the digital therapeutics of autism spectrum disorders: a bibliometric analysis from 2002 to 2022. Front. Psychiatry 14, e1126404. doi: 10.3389/fpsyt.2023.1126404
Yao, H., de Siqueira, A. G., Foster, A., Galynker, I. I., and Lok, B. C. (2020). Toward automated evaluation of empathetic responses in virtual human interaction systems for mental health scenarios. In: Proceedings of the 20th ACM International Conference on Intelligent Virtual Agents.
Keywords: fragile X syndrome, healthcare, artificial intelligence, technologies, quality of life, reinforcement learning (IRL)
Citation: Stasolla F, Passaro A, Di Gioia M, Curcio E and Zullo A (2023) Combined extended reality and reinforcement learning to promote healthcare and reduce social anxiety in fragile X syndrome: a new assessment tool and a rehabilitative strategy. Front. Psychol. 14:1273117. doi: 10.3389/fpsyg.2023.1273117
Received: 23 August 2023; Accepted: 30 November 2023;
Published: 20 December 2023.
Edited by:
Donovan Jones, Charles Sturt University, AustraliaReviewed by:
Roberto Galvez, University of Illinois at Urbana-Champaign, United StatesRebecca Shaffer, Cincinnati Children's Hospital Medical Center, United States
Copyright © 2023 Stasolla, Passaro, Di Gioia, Curcio and Zullo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fabrizio Stasolla, Zi5zdGFzb2xsYUB1bmlmb3J0dW5hdG8uZXU=
 Fabrizio Stasolla
Fabrizio Stasolla Anna Passaro
Anna Passaro Mariacarla Di Gioia
Mariacarla Di Gioia Enza Curcio
Enza Curcio Antonio Zullo
Antonio Zullo