
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 27 October 2023
Sec. Health Psychology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1266059
Introduction: For middle-aged and older people, depression is a frequent and prevalent illness. The purpose of this study was to examine the moderating function of living arrangements in the mediating model as well as the mediating role of life satisfaction in the association between chronic diseases and depressive symptoms.
Methods: The China Health and Retirement Longitudinal Study (CHARLS) provided the data for this investigation (2018). Respondents were grouped according to depression status to compare the differences between middle-aged and older people with different depression statuses. The moderating effect of living arrangements and the mediating effect of life satisfaction were tested using the Bootstrap program and the simple slope approach.
Results: The population’s total prevalence of depressive symptoms was 30.3%. According to the mediating effect research, middle-aged and older people with chronic diseases experienced substantial direct effects on depressive symptoms (β = 1.011, p < 0.001). It has been established that life satisfaction has an 18.6% mediation effect between depressive symptoms and chronic diseases. Regarding the further moderating influence, it was discovered that chronic diseases had a more significant impact on the life satisfaction of middle-aged and older people who are in live alone than those who are living with others (β = 0.037, p < 0.05).
Conclusion: In middle-aged and older people, chronic diseases have a major influence on depressive symptoms. Life satisfaction mediated the relationship between chronic diseases and depressive symptoms, and living arrangements moderated the first part of the route in the mediation model. Therefore, life satisfaction and living arrangements should be important considerations to decrease the prevalence of depressive symptoms in middle-aged and older people.
The critical public health problem of depression has become a significant issue for middle-aged and older people’s mental health. Depression symptoms affect around 32 million individuals globally (World Health Organization, 2017). By 2030, it is predicted to be the main contributor to the burden of illness worldwide (Malhi and Mann, 2018). With the aging of the population, depression in the middle-aged and elderly will become relatively common. According to Li et al. (2021) 32.62% of middle-aged and older people reported having depression in 2015 and research from the China Health and Retirement Longitudinal Survey of 2018 suggested that 42.92% of middle-aged and older people in China suffer from depression (Wang et al., 2022), we can see that depression is becoming more common among middle-aged and older people. It not only lowers one’s quality of life and social functioning, but it also frequently coexists with some prevalent ailments. It is clear that in order to contribute to the effective prevention and treatment of depression, it is essential to identify the influencing factors by which middle-aged and older people experience depressive symptoms and study the link between them and depressive symptoms.
Chronic disease can impair middle-aged and older people’s self-assessed health and cognitive function, resulting in bodily dysfunction that can precipitate and worsen the start and progression of geriatric depression. A prior study found that those who had numerous medical illnesses (co-occurrence of two or more chronic noncommunicable diseases) were two to three times more likely to develop depression than people who did not have multiple medical conditions or chronic illnesses (Read et al., 2017). Chronic disease duration, the need for long-term medicine, persistent comorbidities, poor physical performance, an excessive financial burden, and a lack of spiritual support can all increase depression symptoms in older persons (Ma et al., 2015). Another study suggests a bidirectional relationship between depression and chronic disease (Pan et al., 2012). Furthermore, according to the World Health Organization’s (WHO) Global Burden of Disease research, people with chronic conditions are far more likely to suffer from depression. As a result, having a chronic disease raises the risk of developing depression symptoms.
Life satisfaction is a crucial aspect of subjective well-being and is associated with judging an individual’s quality of life (Shad et al., 2017). Patients with chronic diseases have poor health and reduced capacity to complete activities of daily life (Violán et al., 2016). A previous study showed that poor health affects the decline in life satisfaction (Chokkanathan and Mohanty, 2017). Wister et al. found that multimorbidity and chronic diseases are linked to poorer satisfaction levels (Wister et al., 2016). According to certain research, chronic respiratory illness patients had reduced life satisfaction (Hu et al., 2016; Drop et al., 2018; Tanrıverdi and Korkmaz, 2021). Additionally, another study revealed a link between poorer life satisfaction and cardiovascular disease risk factors among African-Americans participating in longitudinal research (Mendez et al., 2018). Life satisfaction is a factor in mental health and quality of life (Rosella et al., 2019). In individuals with cardiovascular disease, a strong link between life satisfaction and depression has been found (Steca et al., 2013). A previous study revealed that people with lower life satisfaction tend to be more likely to experience depressive symptoms (Mei et al., 2021), Smorti et al. found an association between depression, anxiety, and life satisfaction in the research of amyloid light chain cardiac amyloidosis (Smorti et al., 2016). Decreased life satisfaction can affect well-being, there is a risk of bad mood and subsequent development of depression or anxiety. Consequently, chronic diseases may cause reduced life satisfaction and lead to depressive symptoms due to poor mood and anxiety.
The treatment of depressive symptoms involves both personal and external environmental factors. Personal behavior modifications are the outcome of interactions between an individual and their environment (Anderies, 2014). The living arrangement reflects the structure of the family and the way family life is organized, and the structural level determines the way family members interact (Gao and Yao, 2020). Previous studies have revealed that compared to older people living with other adults, those who live alone have a greater frequency of serious chronic diseases (Park et al., 2014; Srivastava et al., 2021), a meta-analysis shows that older adults who live alone are more likely to experience depression (Xiu-Ying et al., 2012). Because of things like family structure and connections, a study has shown that older people who live with their spouse and children have greater life satisfaction than those who live alone (Kooshiar et al., 2012). Kandapan et al. found that older people’s living arrangements in India substantially impacted how satisfied they felt with their lives (Kandapan et al., 2023).
Based on the facts mentioned above, earlier research has examined the direct relationships between depressive symptoms and chronic diseases, the direct impact of living arrangements and life satisfaction on chronic disease, and depressive symptoms. Current research is sparse on how the living arrangements and life satisfaction of middle-aged and older adults affect the relationship between chronic illness and depression. Given the rising rate of multimorbidity, it is crucial to evaluate this relationship to determine how to prevent and treat depression. Depressive symptoms and mental health in middle-aged and older people may be improved by looking at the relationship between chronic diseases and depressive symptoms in middle-aged and older people and their mechanisms from the perspectives of life satisfaction and living arrangements. We provide three hypotheses for this investigation in light of those above, as seen in Figure 1.
H1: Chronic diseases directly impact middle-aged and older people’s depressive symptoms.
H2: Through the intermediate effect of life satisfaction, chronic diseases directly affect depressive symptoms in middle-aged and older people.
H3: Living arrangements moderate the mediating model of life satisfaction.
This study used the latest data from wave 4 (2018) published on the official website of the China Health and Retirement Longitudinal Study (CHARLS). The goal of CHARLS is to gather a set of high-quality microdata typical of Chinese families and people at least 45 years old and in their middle years, 19,816 respondents in a total of 12,400 households in 2018, In this study, We removed 374 outliers and ages<45, leaving 19,442 samples. We excluded samples with missing key variables (life satisfaction, living arrangements) and non-core variables (smoking, drinking) interpolation is performed using the mode, with a final sample size of 7,756 (Figure 2).
The socio-demographic variables considered in the analysis were gender (male/female), age, marital status (married/unmarried), education level (middle school and below/high school and above), annual household income (<100,000¥,100,000¥-, 300000¥-,500000¥-), living arrangements (living alone/living with other people). Smoking statuses (smoking/no smoking) and drinking statuses (drinking/no drinking) were included in the category of health behaviors.
The CHARLS database asks the middle-aged and elderly separately if they have any of the 14 chronic diseases informed by their physicians. They are defined as having a chronic disease if they have at least one condition. Each chronic disease was assigned 1 point, with higher scores indicating a greater number of chronic diseases.
The CHARLS program uses an epidemiological survey measured by the Depression Scale (CES-D). CES-D scale options consist of 4 levels: “rarely or not at all = 0,” “not too much =1,” “sometimes or half of the time = 2,” and “most of the time = 3,” with a composite score range of 0 to 30. Depressive symptoms were thought to be present in the CES-D ≥ 10 (Chen and Mui, 2014) and classified as the “depressed group”; CES-D < 10 was supposed to have no depressive symptoms and classified as a “non-depressed group,” the Cronbach’s Alpha coefficient of the CES-D scale used in CHARLS was 0. 795, and its reliability met the requirements for statistical analysis.
Life Satisfaction comes from the CHARLS survey question “Overall, are you satisfied with your life? “there are five options to answer: extremely satisfied, very satisfied, relatively satisfied, not very satisfied, and not satisfied at all, respectively, with values of 5, 4, 3, 2, and 1. The higher the score, the higher the life satisfaction.
IBM SPSS (version 26.0) was employed to analyze data. According to the depressive symptoms score, the study participants were divided into groups and conducted a single-factor analysis. If the measures did not fit the normal distribution, the median was used, and the Mann–Whitney U test was used to compare the differences between groups; otherwise, was used, and the t-test was used to compare the differences between groups. For statistical data, the number of cases (percentage) was used, and the χ2 test was used to compare the differences between groups. The Spearman correlation was utilized to investigate the relationship between the research variables. Mediation effect test using bias-corrected percentile Bootstrap method, improves the statistical test power. The design of the specific model is as follows:
In the model, Y is the dependent variable depressive symptoms, X is the independent variable chronic illness, and M is the mediating variable life satisfaction. The specific mediation effect test procedure is as follows: if a × b is significant, the mediation test result does not contain 0 at the 95% confidence interval, the mediation path exists. Conversely, a mediation effect is not significant if the 95% confidence interval of the mediation effect value contains 0. if c’ is not significant, then it is a full mediation effect, if c’ is significant then it is a partial mediation effect. If a × b is not significant, the mediator does not hold and the test is continued to see if c’ is significant, if c’ is significant, it has only a direct effect, and if c’ is not significant, it has no effect. Moderated effects were tested using the bias-corrected percentile Bootstrap method, with chronic diseases as the independent variable, depressive symptoms as the dependent variable, life satisfaction as the mediator, the product of the above variables is the interaction term for the moderating effect. When the moderating effect is significant, the simple slope test suggested by Aiken and West (1991) was employed to examine the precise moderating impact of different living arrangements.
Model 4 and Model 59 in PROCESS 3.4 developed by Hayes (2013) were used to analyze the mediating effect of life satisfaction and the moderating effect of living arrangements. A sample of 5,000 Bootstrap samples as taken and a confidence interval of 95% (95% CI) was set. The two models included adjustments for the relevant covariates (gender, age, marital status, education level, annual household income, smoking, and drinking), which may impact depressive symptoms. The statistically significant level was set at α = 0.05.
In our study, a total of 7,756 middle-aged and older people were included. The population was divided into groups based on the CES-D ≥ 10, and a single-factor analysis was carried out (Table 1). The results showed that 2,348 (30.3%) individuals had depressive symptoms. No statistically significant differences were found for depressive symptoms by age, living arrangement, smoking status, and drinking status (p > 0.05), however, there were statistically significant differences for different gender, education level, annual household income, marital status, number of chronic diseases, and life satisfaction (p < 0.001).
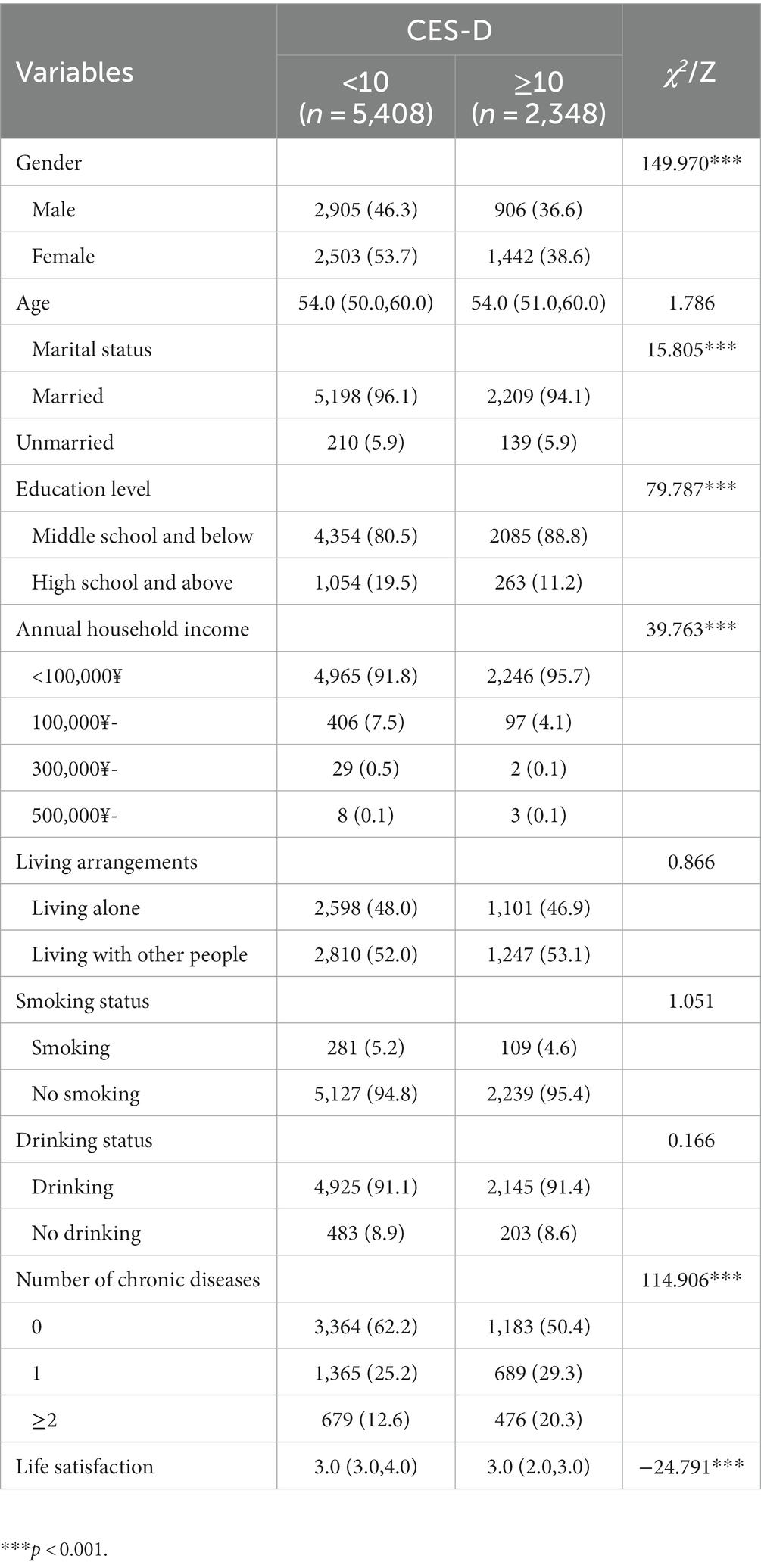
Table 1. Comparison of middle-aged and older people with depression group and without depression group at baseline.
According to the Spearman correlation analysis results, the number of chronic diseases was significantly correlated with life satisfaction and depressive symptoms (r = −0.08, p < 0.01; r = 0.15, p < 0.01). In addition, a negative correlation (r = −0.34, p < 0.01) was found between life satisfaction and depressive symptoms. The requirement of the mediating influence analysis is satisfied by this finding (Table 2). The research identified covariates for the variables in the regression analysis. (Table 3), the results showed that the variance inflation factors for these variables were less than 5, suggesting that none of these variables has covariance.
After controlling all demographic and health-related variables, the results of the mediation effect analysis showed that the total effect of chronic diseases on depressive symptoms was path c = 1.011 (p < 0.001). The indirect path had the following parameters: path a = −0.074 (p < 0.001), path b = −2.534 (p < 0.001), the indirect effect of life satisfaction was (path a × path b) = 0.188 (p < 0.001), and bootstrap 95% confidence interval did not contain 0. It suggests the validity of the mediating effect of life satisfaction. The direct effect of chronic illnesses (path c’) was 0.823, which was still significant (p < 0.001), showing that the mediating effect was partial, and the extent of the mediating effect (ab/c) was 18.6% (Table 4, Figure 3).
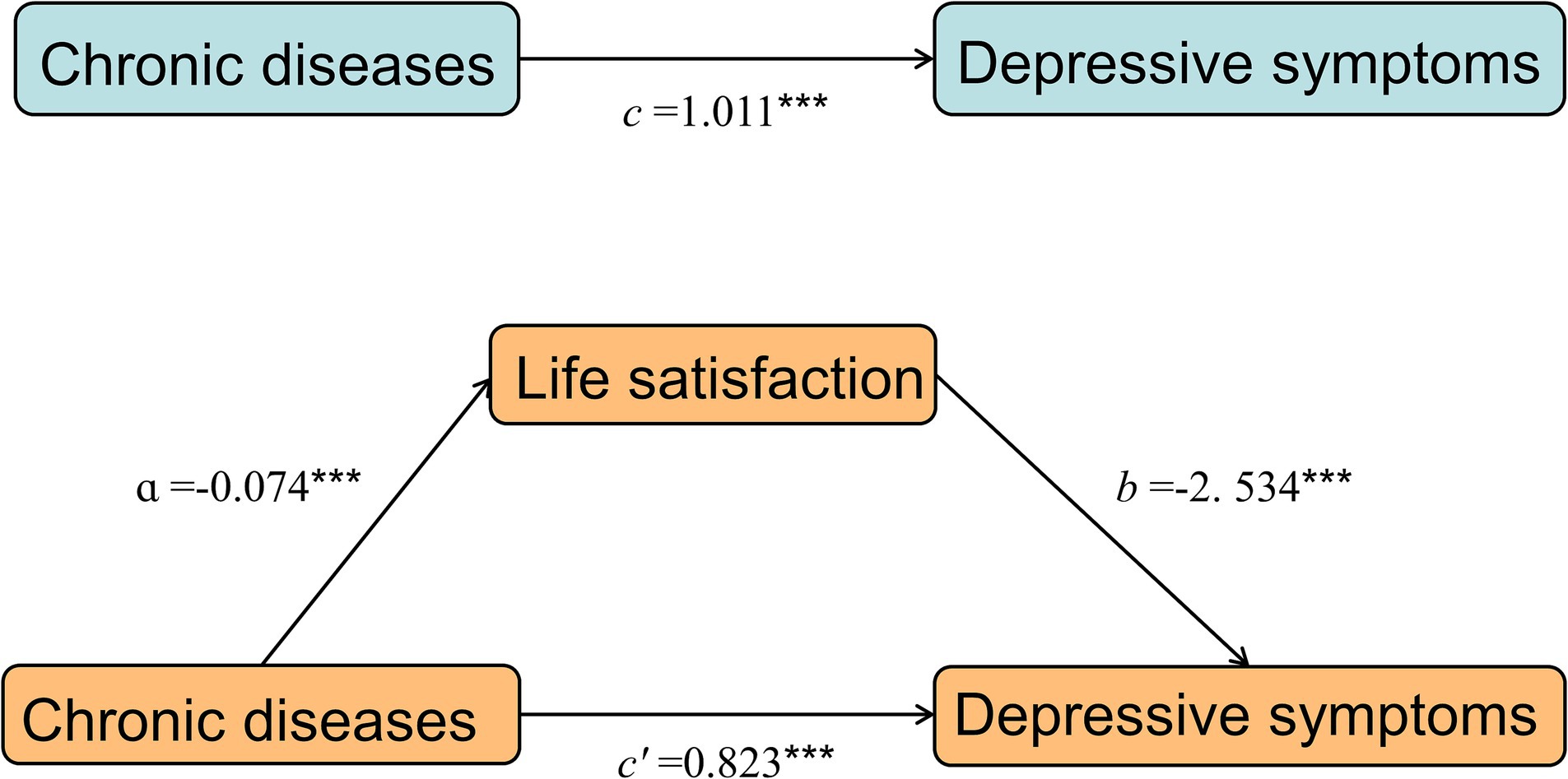
Figure 3. A mediating effect diagram. ***p < 0.001 a: Effect of the independent variable (chronic disease) on the mediating variable (life satisfaction). b: Effect of the mediating variable (life satisfaction) on the dependent variable (depressive symptoms). c: The total effect of chronic diseases on depressive symptoms. c’: The direct effect of chronic diseases.
The moderated mediation analysis indicated that the living arrangements moderated the first half of the path a (=0.037, p < 0.05) in the mediation model after controlling for demographic and health-related factors. Living arrangements moderated the relationship between chronic diseases and life satisfaction. The interaction term between chronic diseases and living arrangements predicts life satisfaction (Table 5, Figure 4). However, it did not play a moderating role in the second half of path b (=0.042, p > 0.05) or the direct path (= − 0.162, p > 0.05) in the mediation model.
A simple slope analysis of living arrangements was used to investigate to explore the effects of chronic diseases on life satisfaction among those living alone and living with other people. According to the results, with the increase in chronic disease number, the life satisfaction of people who live alone declined significantly more than that of those who live with others (simple slope, living alone: −0.13, p < 0.001, living with other people −0.10, p < 0.001) (Figure 5).
This study indicated that the population’s total prevalence of depressive symptoms was 30.3%. The prevalence of depressive symptoms is mostly higher than the results of existing studies (Jung et al., 2018; Alinaitwe et al., 2021), which may be due to differences in measurement tools and the severity of the disease. The presence of depressive symptoms is more possibly to be female, have a lower education level, and have lower annual household income than those without depressive symptoms. More than 49.6% had at least one chronic disease, and nearly 20.3% had at least two chronic diseases among those with depressive symptoms. These results are generally consistent with earlier studies (Liu et al., 2018; Li et al., 2019; Hu et al., 2022). Given that those who exhibit the aforementioned unfavorable characteristics are more likely to suffer from depressive symptoms, we need to promote mental health and pay attention to how chronic diseases affect them.
According to the results of this study, hypothesis 1 is confirmed, and there is a positive correlation between the prevalence of chronic diseases and depressive symptoms in middle-aged and older people. The severity of the depression symptoms increased with the number of chronic conditions, consistent with previous research (Seo et al., 2017; Bi et al., 2021; Zhang et al., 2022). Most chronic disease patients have diminished physical capacity, which negatively impacts everyday activities and lowers the quality of life. They might experience discomfort, anxiety, and even despair as they face challenges in their everyday lives (Tinetti et al., 2012). Some patients with chronic diseases need to accept care from family members and relatives, which adds to their psychological burden and makes them feel inferior. Another possibility is that people with chronic diseases put a significant financial strain on their families and themselves because of the lengthy treatment times and hefty medical costs. Patients who cannot take care of themselves depend on family members for care. Family members’ working hours and total family income will be reduced, and the financial burden on the family will increase (Dong et al., 2020). They were influenced by the traditional Chinese belief that most middle-aged and older adults should care for their children or grandchildren (Ma et al., 2021). Middle-aged and older people with chronic diseases who require care may feel like a burden and experience unpleasant feelings, including irritation, worry, pessimism, and despair. Therefore, enhancing chronic disease evaluation and management becomes a crucial component of preventing and treating depression in middle-aged and older people.
Hypothesis 2 is supported that the mediating effect results suggest that chronic disease can either directly impact the depressive symptoms of the middle-aged and elderly or indirectly affect their depressive symptoms through the effect of life satisfaction, which mediates the relationship between chronic diseases and depression symptoms to some extent. First, there is a direct positive predictive relationship between depressive symptoms and chronic illness. This suggests that an increase in the number of chronic diseases can put patients under additional stress. Middle-aged and older people may have more severe depressive symptoms. This study suggests that those aroused by stress typically have poor mental health (Ma et al., 2021). Second, chronic diseases can also indirectly impact depressive symptoms by lowering life satisfaction. According to earlier research, older people’s life satisfaction suffers when they have more concurrent chronic illnesses, which in turn cause depressive symptoms (Koivumaa-Honkanen et al., 2004; de Guzman et al., 2015). Chronic diseases and depressive symptoms might be connected to life satisfaction. A prior study found that older people’s life satisfaction might be decreased by less effective coping mechanisms brought on by stressful life experiences, promoting the mental health of middle-aged and older people by adopting positive stress-coping measures to ameliorate the adverse effects of stressful events (Ren et al., 2021). As a result, by successfully preventing and managing the development and progression of chronic diseases, we can not only reduce depressive symptoms in middle-aged and older people, but we can also prevent them from occurring by enhancing life satisfaction for these people, thereby enhancing their mental health.
It shows that living arrangements have a moderating effect on the association between chronic illness and life satisfaction. Based on the simple slope analysis findings, we discovered that while chronic diseases affected life satisfaction, their severity varied between middle-aged and older adults who lived with others and those who lived alone. Chronic diseases have a greater impact on the life satisfaction of middle-aged and older adults who live alone than those who live with others. A previous study has shown that living with a partner benefits role functioning in individuals with multiple chronic diseases. When middle-aged and older people living alone suffer from single or multiple chronic diseases (Müller et al., 2017), they do not have the daily care and moral support from their family members, and the pressure and solitude associated with the disease can impact their life satisfaction. Middle-aged and older adults have stronger subjective well-being and are happier with their lives when their family atmospheres are warm and harmonious and receive strong social support (Yu, 2017; Mao and Han, 2018). To increase their life satisfaction or improve chronic illness health management to lessen the incidence of depressive symptoms, it is advised to pay attention to the life satisfaction of middle-aged and older people living alone with chronic diseases.
Based on the above analysis, we should focus on depressive symptoms in middle-aged and older people with chronic diseases, increase public awareness of these conditions, and enhance the diagnostic, management, and preventative control of these illnesses. Second, we should guide middle-aged and older people with chronic diseases to maintain better living conditions and improve their life satisfaction by restoring their independent activities and living ability through standardized treatment, rehabilitation exercises, health education, and social support, reducing the impact of diseases on their lives. Third, we should care for middle-aged and elderly who live alone, understand their health and psychological needs, and strengthen their contact and social support with their families to enhance their health and reduce depressive symptoms.
There are several limitations to this study. First, this study focused mechanisms of the effect of the number of chronic conditions on depressive symptoms and did not explore different types of chronic degenerative diseases or focus on the severity of the disease. This section will be further analyzed in future studies. Second, the results of the current study revealed that life satisfaction partially mediated the association between chronic illnesses and depressive symptoms, suggesting the possibility of other mediating factors. Third, this study used cross-sectional data from 2018, which has limitations in illustrating the causal link between chronic illnesses and depressive symptoms. Consequently, we will consider utilizing longitudinal data for analysis in future research.
In the current research, chronic diseases significantly affected middle-aged and older people’s depressive symptoms, and the more chronic diseases a person had, the more severe their depressive symptoms were. Chronic diseases had a predictive influence on life satisfaction in middle-aged and older people who live alone, and life satisfaction mediated the association between chronic diseases and depressive symptoms.
Publicly available datasets were analyzed in this study. This data can be found at: http://charls.pku.edu.cn/en.
The studies involving humans were approved by the Institutional Review Board at Peking University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
ZS: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. YQL: Data curation, Investigation, Methodology, Writing – original draft. DX: Data curation, Investigation, Methodology, Writing – review & editing. YZ: Data curation, Investigation, Methodology, Writing – review & editing. YPL: Conceptualization, Supervision, Writing – review & editing. BZ: Conceptualization, Supervision, Writing – review & editing. YD: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This article was funded by the Health and Family Planning Research Talent Training Project of Fujian Province (grant number 2018-01-72).
We acknowledge the invaluable efforts made by the China Health and Retirement Longitudinal Study (CHARLS) team’s participants and staff.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CHARLS, China Health and Retirement Longitudinal Study.
Aiken, L. S., and West, S. G. (1991). Multiple regression: testing and interpreting interactions. Newbury Park. Sage Publications, Inc.
Alinaitwe, R., Birungi, C., Bangirana, P., and Nakasujja, N. (2021). Prevalence and factors associated with depressive illness in patients with tuberculosis in Mulago hospital, Kampala- Uganda: a cross sectional study. J. Psychosom. Res. 149:110591. doi: 10.1016/j.jpsychores.2021.110591
Anderies, J. M. (2014). Embedding built environments in social–ecological systems: resilience-based design principles. Build. Res. Inf. 42, 130–142. doi: 10.1080/09613218.2013.857455
Bi, Y. H., Pei, J. J., Hao, C., Yao, W., and Wang, H. X. (2021). The relationship between chronic diseases and depression in middle-aged and older adults: a 4-year follow-up study from the China health and retirement longitudinal study. J. Affect. Disord. 289, 160–166. doi: 10.1016/j.jad.2021.04.032
Chen, H., and Mui, A. C. (2014). Factorial validity of the center for epidemiologic studies depression scale short form in older population in China. Int. Psychogeriatr. 26, 49–57. doi: 10.1017/s1041610213001701
Chokkanathan, S., and Mohanty, J. (2017). Health, family strains, dependency, and life satisfaction of older adults. Arch. Gerontol. Geriatr. 71, 129–135. doi: 10.1016/j.archger.2017.04.001
de Guzman, A. B., Jurado, J. B. N., and Juson, A. J. A. (2015). Examining the structural relationship of chronic illness, physical function, life satisfaction, and social support in the development of depression among Filipino elderly in institutionalized settings. Educ. Gerontol. 41, 193–206. doi: 10.1080/03601277.2014.918836
Dong, X., Chen, L., Xu, Z., and Xu, X. (2020). An assessment of the economic burden of senile chronic diseases in China based on China health and retirement longitudinal survey. Expert Rev. Pharmacoecon. Outcomes Res. 20, 305–312. doi: 10.1080/14737167.2020.1688661
Drop, B., Janiszewska, M., Barańska, A., Kanecki, K., Nitsch-Osuch, A., and Bogdan, M. (2018). Satisfaction with life and adaptive reactions in people treated for chronic obstructive pulmonary disease. Adv. Exp. Med. Biol. 1114, 41–47. doi: 10.1007/5584_2018_242
Gao, N., and Yao, J. (2020). The effects of living arrangement on the depression of older adults. J. Nanjing Med. Univ. 2, 140–145. doi: 10.7655/NYDXBSS20200208
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press. New York.
Hu, S. X. X., Lei, W. I., Chao, K. K., Hall, B. J., and Chung, S. F. (2016). Common chronic health problems and life satisfaction among Macau elderly people. Int. J. Nurs. Sci. 3, 367–370. doi: 10.1016/j.ijnss.2016.10.004
Hu, J., Zheng, X., Shi, G., and Guo, L. (2022). Associations of multiple chronic disease and depressive symptoms with incident stroke among Chinese middle-aged and elderly adults: a nationwide population-based cohort study. BMC Geriatr. 22:660. doi: 10.1186/s12877-022-03329-4
Jung, S., Lee, S., Lee, S., Bae, S., Imaoka, M., Harada, K., et al. (2018). Relationship between physical activity levels and depressive symptoms in community-dwelling older Japanese adults. Geriatr. Gerontol. Int. 18, 421–427. doi: 10.1111/ggi.13195
Kandapan, B., Pradhan, J., and Pradhan, I. (2023). Living arrangement of Indian elderly: a predominant predictor of their level of life satisfaction. BMC Geriatr. 23:88. doi: 10.1186/s12877-023-03791-8
Koivumaa-Honkanen, H., Kaprio, J., Honkanen, R., Viinamäki, H., and Koskenvuo, M. (2004). Life satisfaction and depression in a 15-year follow-up of healthy adults. Soc. Psychiatry Psychiatr. Epidemiol. 39, 994–999. doi: 10.1007/s00127-004-0833-6
Kooshiar, H., Yahaya, N., Hamid, T. A., Abu Samah, A., and Sedaghat Jou, V. (2012). Living arrangement and life satisfaction in older Malaysians: the mediating role of social support function. PLoS One 7:e43125. doi: 10.1371/journal.pone.0043125
Li, L., Ma, M., Peng, H., Yan, Z., Wang, M., Hu, M., et al. (2021). Prevalence and associated factors of depressive symptoms in China's rural elderly. Chinese Gen. Pract. 24:3432. doi: 10.12114/j.issn.1007-9572.2021.00.577
Li, H., Zheng, D., Li, Z., Wu, Z., Feng, W., Cao, X., et al. (2019). Association of depressive symptoms with incident cardiovascular diseases in middle-aged and older Chinese adults. JAMA Netw. Open 2:e1916591. doi: 10.1001/jamanetworkopen.2019.16591
Liu, Q., Cai, H., Yang, L. H., Xiang, Y. B., Yang, G., Li, H., et al. (2018). Depressive symptoms and their association with social determinants and chronic diseases in middle-aged and elderly Chinese people. Sci. Rep. 8:3841. doi: 10.1038/s41598-018-22175-2
Ma, L., Tang, Z., Sun, F., Diao, L., Li, Y., Wang, J., et al. (2015). Risk factors for depression among elderly subjects with hypertension living at home in China. Int. J. Clin. Exp. Med. 8, 2923–2928.
Ma, Y., Xiang, Q., Yan, C., Liao, H., and Wang, J. (2021). Relationship between chronic diseases and depression: the mediating effect of pain. BMC Psychiatry 21:436. doi: 10.1186/s12888-021-03428-3
Malhi, G. S., and Mann, J. J. (2018). Depression. Lancet 392, 2299–2312. doi: 10.1016/s0140-6736(18)31948-2
Mao, X., and Han, W. J. (2018). Living arrangements and older adults' psychological well-being and life satisfaction in China: does social support matter? Fam. Relat. 67, 567–584. doi: 10.1111/fare.12326
Mei, S., Qin, Z., Yang, Y., Gao, T., Ren, H., Hu, Y., et al. (2021). Influence of life satisfaction on quality of life: mediating roles of depression and anxiety among cardiovascular disease patients. Clin. Nurs. Res. 30, 215–224. doi: 10.1177/1054773820947984
Mendez, Y. P., Ralston, P. A., Wickrama, K., Bae, D., Young-Clark, I., and Ilich, J. Z. (2018). Lower life satisfaction, active coping and cardiovascular disease risk factors in older African Americans: outcomes of a longitudinal church-based intervention. J. Behav. Med. 41, 344–356. doi: 10.1007/s10865-017-9909-0
Müller, F., Hagedoorn, M., and Tuinman, M. A. (2017). Chronic multimorbidity impairs role functioning in middle-aged and older individuals mostly when non-partnered or living alone. PLoS One 12:e0170525. doi: 10.1371/journal.pone.0170525
Pan, A., Keum, N., Okereke, O. I., Sun, Q., Kivimaki, M., Rubin, R. R., et al. (2012). Bidirectional association between depression and metabolic syndrome: a systematic review and meta-analysis of epidemiological studies. Diabetes Care 35, 1171–1180. doi: 10.2337/dc11-2055
Park, E. J., Sohn, H. S., Lee, E. K., and Kwon, J. W. (2014). Living arrangements, chronic diseases, and prescription drug expenditures among Korean elderly: vulnerability to potential medication underuse. BMC Public Health 14:1284. doi: 10.1186/1471-2458-14-1284
Read, J. R., Sharpe, L., Modini, M., and Dear, B. F. (2017). Multimorbidity and depression: a systematic review and meta-analysis. J. Affect. Disord. 221, 36–46. doi: 10.1016/j.jad.2017.06.009
Ren, Q., Jiang, C., and Jiang, S. (2021). Stressful life events and life satisfaction among Chinese older adults: the role of coping styles. Healthcare 9:1620. doi: 10.3390/healthcare9121620
Rosella, L. C., Fu, L., Buajitti, E., and Goel, V. (2019). Death and chronic disease risk associated with poor life satisfaction: a population-based cohort study. Am. J. Epidemiol. 188, 323–331. doi: 10.1093/aje/kwy245
Seo, J., Choi, B., Kim, S., Lee, H., and Oh, D. (2017). The relationship between multiple chronic diseases and depressive symptoms among middle-aged and elderly populations: results of a 2009 korean community health survey of 156,747 participants. BMC Public Health 17:844. doi: 10.1186/s12889-017-4798-2
Shad, B., Ashouri, A., Hasandokht, T., Rajati, F., Salari, A., Naghshbandi, M., et al. (2017). Effect of multimorbidity on quality of life in adult with cardiovascular disease: a cross-sectional study. Health Qual. Life Outcomes 15:240. doi: 10.1186/s12955-017-0820-8
Smorti, M., Guarnieri, S., Bergesio, F., Perfetto, F., and Cappelli, F. (2016). Anxiety and depression among amyloid light-chain cardiac amyloidosis patients: the role of life satisfaction. Eur. J. Cardiovasc. Nurs. 15, 269–275. doi: 10.1177/1474515114566737
Srivastava, S., Debnath, P., Shri, N., and Muhammad, T. (2021). The association of widowhood and living alone with depression among older adults in India. Sci. Rep. 11:21641. doi: 10.1038/s41598-021-01238-x
Steca, P., Greco, A., Monzani, D., Politi, A., Gestra, R., Ferrari, G., et al. (2013). How does illness severity influence depression, health satisfaction and life satisfaction in patients with cardiovascular disease? The mediating role of illness perception and self-efficacy beliefs. Psychol. Health 28, 765–783. doi: 10.1080/08870446.2012.759223
Tanrıverdi, Ö., and Korkmaz, M. (2021). The relationship between self-effıcacy and life satisfaction in patients with chronic obstructive pulmonary disease. J. Public Health 31, 1–8. doi: 10.1007/s10389-021-01576-0
Tinetti, M. E., Fried, T. R., and Boyd, C. M. (2012). Designing health care for the most common chronic condition--multimorbidity. JAMA 307, 2493–2494. doi: 10.1001/jama.2012.5265
Violán, C., Bejarano-Rivera, N., Foguet-Boreu, Q., Roso Llorach, A., Pons-Vigués, M., Martin Mateo, M., et al. (2016). The burden of cardiovascular morbidity in a European Mediterranean population with multimorbidity: a cross-sectional study. BMC Fam. Pract. 17:150. doi: 10.1186/s12875-016-0546-4
Wang, J., Xu, J., Nie, Y., Pan, P., Zhang, X., Li, Y., et al. (2022). Effects of social participation and its diversity, frequency, and type on depression in middle-aged and older persons: evidence from China. Front. Psych. 13:825460. doi: 10.3389/fpsyt.2022.825460
Wister, A., Kendig, H., Mitchell, B., Fyffe, I., and Loh, V. (2016). Multimorbidity, health and aging in Canada and Australia: a tale of two countries. BMC Geriatr. 16:163. doi: 10.1186/s12877-016-0341-z
World Health Organization (2017). Depression and other common mental disorders: global health estimates. America. World Health Organization
Xiu-Ying, H., Qian, C., Xiao-Dong, P., Xue-Mei, Z., and Chang-Quan, H. (2012). Living arrangements and risk for late life depression: a meta-analysis of published literature. Int. J. Psychiatry Med. 43, 19–34. doi: 10.2190/PM.43.1.b
Yu, Z. (2017). Influence of intergenerational support on the life satisfaction of the elderly and the differences between urban and rural areas: based on analysis of 7669 samples from CHARLS. J. Hunan Univ. Agric. 18, 62–69.
Keywords: life satisfaction, living arrangements, chronic diseases, depressive symptoms, mediating effect, moderating effect
Citation: Shang Z, Liu Y, Xue D, Zheng Y, Li Y, Zhang B and Dai Y (2023) The role of life satisfaction and living arrangements in the association between chronic disease and depression: a national cross-sectional survey. Front. Psychol. 14:1266059. doi: 10.3389/fpsyg.2023.1266059
Received: 24 July 2023; Accepted: 12 October 2023;
Published: 27 October 2023.
Edited by:
Sonia Brito-Costa, Polytechnic Institute of Coimbra, PortugalReviewed by:
Jose Maria De La Roca-Chiapas, University of Guanajuato, MexicoCopyright © 2023 Shang, Liu, Xue, Zheng, Li, Zhang and Dai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Dai, ZGFpeXVlODdAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.